Abstract
Purpose
To attempt to determine whether group audiologic rehabilitation (AR) content affected psychosocial outcomes.
Method
A randomized controlled trial with at least 17 participants per group was completed. The 3 treatment groups included a communication strategies training group, a communication strategies training plus psychosocial exercise group, and an informational lecture plus psychosocial exercise group. Evaluations were conducted preclass, postclass, and 6-months postclass; they included hearing loss–related and generic quality of life scales, and a class evaluation form.
Results
All treatment groups demonstrated short- and long-term improvement on the hearing loss–related quality of life scale. Minimal differences were measured across treatment groups. A significant difference was observed between the lecture plus psychosocial exercise group and the communication strategies training group for 1 hearing loss–related quality of life subscale. Better outcomes were measured for the 2 groups with psychosocial exercises versus the communication strategies training group on 1 generic quality of life subscale. The results for the class evaluation did not discriminate among the treatment groups.
Conclusions
Class content had only a minimal influence on treatment outcomes. Recommended AR class content includes a mix of interventions including information, training, and psychosocial exercises.
Keywords: audiologic rehabilitation, hearing loss, psychosocial
The purpose of group audiologic rehabilitation (AR) programs is to provide information, training, and psychosocial support. Adult-onset hearing loss changes the predictability of everyday life and may cause social uncertainty, fear, anxiety, and increased sensitivity to difficult situations (Hogan, 2001). A supportive group is an ideal venue to take a psychosocial approach to AR: A psychosocial approach is one in which participants can begin to understand and accept their feelings about hearing loss and the problems associated with hearing loss (Noble, 1996). With the help of others facing similar problems, the group participants can begin to practice new skills necessary for successful communication. Once the feelings and problems associated with hearing loss are understood and new strategies are learned, AR class participants may learn to accept their new normal and begin to use strategies to improve their communication in everyday situations (Hogan, 2001).
Recently, Hawkins (2005) used an evidence-based practice approach to review the effectiveness of counseling-based adult group AR programs. He looked for studies in which adults with hearing loss participated in a group class that included communication strategies, personal adjustment counseling, information about hearing and hearing devices, and/or group counseling. Hawkins found 12 studies which evaluated AR programs that used a randomized controlled trial and a quasi-experimental or nonintervention cohort design. Hawkins concluded that there were potential short-term benefits from adult AR groups. These benefits included reduced hearing handicap, improved self-perceived quality of life, and improved use of communication strategies. Unfortunately, only limited research demonstrated long-term benefits.
It is important to note that not all of the patients in the studies that Hawkins (2005) reviewed demonstrated benefits as a result of the group classes. This may have been due to the actual AR content taught in the classes, the demographic characteristics of participants in the programs, or the effectiveness of the outcome measures used (Preminger, 2007). The purpose of the present investigation is to determine whether class content influences outcomes.
Table 1 shows a review of nine of the studies cited by Hawkins (2005), plus an additional study (Hickson, Worrall, & Scarinci, 2007) in which the following criteria were met: (a) There was at least one treatment group and one control (or placebo) group, (b) the content in the group AR class was described, and (c) outcomes were measured with questionnaires that had known psychometric properties. The class content was fairly similar across the 10 studies. Nine programs included informational lectures about hearing loss, hearing aids, and other related topics. Nine of the programs included instruction and role-playing in the use of communication strategies (e.g., see Kaplan, Bally, & Garretson, 1985; Tye-Murray, 1997). Additional content included speechreading and/or auditory training (seven studies), assistive device demonstrations (five studies), and stress reduction techniques (four studies). Finally, while not stated, it is likely that all 10 programs included discussions aimed at alleviating the psychosocial affects of hearing loss. Whereas time may not have been set aside explicitly for these discussions, they often occur during informational lectures and during communication strategy instruction. In all 10 studies, treatment groups who received group AR demonstrated significant posttreatment versus pretreatment improvements on a questionnaire or standardized scale. In seven of the 10 studies, treatment groups who received group AR demonstrated significantly more improvement on hearing loss–related quality of life scales than control groups who did not participate in group AR.
Table 1.
Summary of content and outcomes in group audiologic rehabilitation (AR) studies cited by Hawkins (2005).
| Reference | Participants | Content | Outcome measures | Results |
|---|---|---|---|---|
| Abrams et al. (1992) |
N = 31; 100% new HA users; VA patients; 100% male |
Control 1: No attention Control 2: HA only Treatment: HA plus group AR (lectures, speechreading, communication strategies, assistive devices) |
HHIE (pre- and posttreatment) | Treatment group had significantly greater reduction in hearing handicap in comparison with both control groups. |
| Abrams et al. (2002) |
N = 102; 100% new HA users; VA patients; 64% male |
Control: HA Treatment: HA plus group AR (lectures, speechreading, communication strategies, assistive devices) |
Overall quality of life (pre- and posttreatment) |
Both groups showed significant improvement on the mental component subscale. |
| Andersson, Melin, Scott, & Lindberg (1995) |
N = 20; 100% experienced HA users; 70% male |
Control: No attention Treatment: Group AR (lectures, communication strategies, relaxation skills) |
Structured interviews; daily ratings of HA; HCA (pre- and posttreatment) |
Treatment group improved significantly in relaxation (observed in videos) and improved daily ratings of HA satisfaction compared to controls; no difference across groups on HCA. |
| Beynon et al. (1997) |
N = 47; new HA users; no gender data available |
Control: HA Treatment: HA plus group AR (lectures, HA use, speechreading, communication strategies, stress reduction, psychosocial discussions) |
QDS (pre- and posttreatment) | Treatment group had significantly larger reduction in hearing handicap than controls. |
| Chisolm et al. (2004) |
N = 106; 100% new HA users: VA patients; 64% male |
Control: Routine HA orientation Treatment: Routine HA orientation plus group AR (lectures, communication strategies, assistive device use) |
CPHI (pre- and posttreatment and at 1 year) |
Treatment group had better CPHI outcomes posttreatment and at 6 months posttreatment compared to control group; no difference between groups at 1 year. |
| Hallberg & Barrenas (1994) |
N = 38; 7.5% HA users, noise-induced hearing loss patients; 100% male |
Control: No attention Treatment: Group AR with significant others (lectures, psychosocial discussions, assistive devices, stress reduction) |
3 hearing loss–related quality of life scales (pre- and posttreatment and 4 months posttreatment) |
Treatment group had significantly more improvement in perceived hearing handicap posttreatment compared to controls; no difference between groups 4 months later. |
| Hickson et al. (2007) |
N = 178; 54% experienced HA users, 46% nonusers; 45% male |
Placebo group: Informational lectures Treatment: Group AR (identification of communication problems, group problem solving, and communication strategy practice) |
5 quality of life scales, 3 of which were hearing loss–related (pretreatment, posttreatment, and 6 months posttreatment) |
Compared to pretreatment scores, treatment group showed significant improvement on 4 of the quality of life scales that were maintained at 6 months posttreatment. No significant differences in posttreatment improvement between treatment group and placebo group. |
| Norman et al. (1995) |
N = 124; 100% new HA users, National Health Service; 50% male |
Control: HA Treatment: HA plus group AR (lectures, speechreading training, communication strategies, relaxation techniques, psychosocial discussions) |
Questionnaire, HA rating diary (pre- and posttreatment) |
Treatment group had significantly higher HA satisfaction than controls; no difference across groups in residual disability or handicap. |
| Preminger (2003) |
N = 25; 100% experienced HA users; private practice patients; 52% male |
Control: Group AR for people with hearing loss (lectures, speechreading, auditory training, communication strategies, psychosocial discussion) Treatment: Group AR for people with hearing loss and significant others (content revised for inclusion of significant others) |
HHIE, HHIA, CSOA (pre- and posttreatment) |
Treatment group had significantly greater reduction in hearing handicap than control group; no difference in improvement between groups on CSOA. |
| Smaldino & Smaldino (1988) |
N = 40; 100% new HA users; 48% male |
Control: basic HA orientation Treatment 1: HA orientation plus instruction about learning style Treatment 2: HA orientation plus group AR (lectures, auditory training, speechreading training, communication strategies) plus instruction about learning style Treatment 3: HA orientation plus group AR (same content as Treatment 2) |
HPI (pre- and posttreatment) | Signification improvement on HPI following intervention for Treatment 2 and Treatment 3 groups; no change on HPI for control and Treatment 1 groups. |
Note. HA = hearing aid; VA = participants who were recruited through the Louisville Veterans Affairs (VA) Medical Center; HHIE = Hearing Handicap Inventory for the Elderly (Ventry & Weinstein, 1982); HCA = Hearing Coping Assessment (Andersson, Melin, Lindberg, & Scott, 1995); QDS = Quantified Denver Scale (Schow & Nerbonne, 1980); CPHI = Communication Profile for the Hearing Impaired (Demorest & Erdman, 1987); HHIA = Hearing Handicap Inventory for Adults (Newman et al., 1990); CSOA = Communication Scale for Older Adults (Kaplan et al., 1997); HPI = Hearing Performance Inventory (Giolas et al., 1979).
The actual content of the group AR classes was explicitly varied in only one study included in Table 1. In the Hickson et al. (2007) study, performance on quality of life scales was compared between a treatment group and a placebo group. The treatment group completed the Active Communication Education (ACE) program (Hickson & Worrall, 2003) in which group participants identified specific communication difficulties, identified skills to improve communication in specific environments, and practiced the new skills. The placebo group attended five informational lectures covering communication-related topics (e.g., communication and technology). There were no significant differences in posttreatment benefits between the two groups for three hearing loss–related quality of life scales and two general quality of life scales (Hickson et al., 2007).
Two additional studies listed in Table 1 did include slight treatment variations across the treatment groups. In one study, the second treatment group received new hearing aids, hearing aid orientation, a traditional group AR program, and an individual session discussing participants’ individual learning styles, while the third treatment group received the same treatment as the second treatment group minus the discussion of individual learning styles (Smaldino & Smaldino, 1988). Although the actual class content was not varied in this study, the expectation was that individuals who had knowledge of their individual learning styles could apply this to the group AR experience. The results did not show any difference in outcomes across these two treatment groups (Smaldino & Smaldino, 1988). In the other study, individuals with hearing loss in both the control group and the treatment groups attended traditional group AR classes, while the participants in the treatment group attended the classes with a significant other (Preminger, 2003). The class content was similar across classes; however, some of the actual content was varied to accommodate the inclusion of significant others. For example, while both types of classes included role-playing communication strategy exercises, the control class participants role-played with the instructors while the treatment class participants role-played with their significant others. In this study, class content (and significant other participation) did influence results: Individuals who participated with their significant others demonstrated significantly greater improvement in hearing loss–related quality of life than those who participated alone.
Psychosocial Benefits of the Group Experience
It seems likely that AR groups can be designed to maximize the psychosocial benefits provided. We can look to the field of psychology to develop AR groups who provide psychosocial support and explicit psychosocial exercises. Support groups have been used to help individuals deal with social problems and to cope with illness; they provide a forum for participants to learn about their medical condition and to meet others who face similar circumstances (Stewart, Davidson, Meade, Hirth, & Weld-Viscount, 2001; Weber, Roberts, & McDougall, 2000). We can also consider coping mechanisms when designing psychosocial activities. Coping can be defined as the cognitive and behavioral efforts to manage stress as a result of a condition such as hearing loss (Lazarus & Folkman, 1984; Ryden, Karlsson, Sullivan, & Torgerson, 2003). One way to categorize coping is in terms of problem-focused and emotion-focused coping (Lazarus & Folkman, 1984). Problem-focused coping focuses on managing the problem (e.g., defining the problem, generating alternative solutions, weighing the alternatives, and choosing among them), whereas emotion-focused coping is achieved by managing one’s own emotional response to a problem (e.g., avoidance, minimization, and positive comparisons; Lazarus & Folkman, 1984).
The psychosocial exercises in the present study were developed based on the work of Hogan (2001). Hogan developed group exercises in which participants may learn to recognize the feelings that often accompany hearing loss (e.g., fear, guilt, anxiety, worry, sadness, grief, anger, frustration, and a loss of intimacy). In a group environment, participants may begin to recognize and accept the feelings that accompany hearing loss as they realize that others with hearing loss also experience these feelings. Hogan postulated that after participants begin to accept the feelings that accompany hearing loss, they may begin to take action to deal with the communication difficulties that they face. The psychosocial exercises in the current study were developed to foster emotion-focused coping in the participants.
In a recent study, the use of psychosocial exercises was manipulated in an evaluation of group AR benefit (Preminger & Ziegler, 2008). One group of adult hearing aid users participated in a group AR program consisting of auditory-only and auditory-visual speech perception training, while a second group of participants completed the same training plus psychosocial exercises designed to assist participants in the acceptance of hearing loss and hearing-related problems. As a result of training, no significant group changes were measured for tests of auditory-only or auditory-visual speech perception. Both training groups demonstrated a significant posttraining improvement on the Emotional subscale of the Hearing Handicap Inventory (HHI) for the Elderly and for Adults (Newman, Weinstein, Jacobson, & Hug, 1990; Ventry & Weinstein, 1982) that was not displayed by a control group of individuals who were evaluated on multiple occasions. However, neither training group demonstrated significantly more improvement on the total HHI scale in comparison with the control group in which participants received multiple evaluations but no treatment.
The present study is an extension of the Preminger and Ziegler (2008) study. Three groups of participants were evaluated in a randomized controlled trial: One group received training activities focusing on communication strategies, one group received communication strategy training activities plus psychosocial exercises, and one group received informational lectures and psychosocial exercises. Because no true control group was evaluated, the results of the current study were used to compare the three different treatment methods; the results did not determine whether any of the treatment groups were better than no treatment. All participants were evaluated with a hearing loss–specific quality of life scale and a generic quality of life scale, and all participants completed a class evaluation form. The purpose of this study was to determine whether group AR content affected the outcomes. It was hypothesized that individuals who participated in AR classes that included both training and psychosocial activities would demonstrate better outcomes as compared to those measured in individuals who participated in AR classes that contained only training exercises or that contained psychosocial activities and no training exercises.
Method
Participants
This study was approved by the institutional review board at the University of Louisville in Louisville, KY. Experienced hearing aid users (at least 3 months’ experience) between the ages of 55 and 75 years were invited to participate in the study. Participants were recruited primarily from the Louisville Veterans Affairs (VA) Medical Center and also from a private practice associated with the program in audiology at the University of Louisville. Volunteers were screened and met these predetermined criteria before study enrollment: (a) a score of at least 20 on the HHI (Newman et al., 1990; Ventry & Weinstein, 1982); (b) corrected binocular visual acuity of at least 20/40 (Hardick, Oyer, & Irion, 1970); (c) scores within the normal range on the Mini-Mental State Examination (Folstein, Folstein, & McHugh, 1975); and (d) Synthetic Sentence Identification-Ipsilateral Competing Message test scores at levels appropriate for the degree of hearing loss and no more than 20% poorer than scores on the Northeastern University Auditory Test No. 6 (NU-6) word list (Stach, Spretnjak, & Jerger, 1990; Yellin, Jerger, & Fifer, 1989). See Preminger and Ziegler (2008) for a more extensive discussion of the screening criteria.
Although a power analysis was not completed for any of the outcome measures used in the present study, a power analysis had been completed for a speech perception measure used in the Preminger and Ziegler study (2008) which determined that a sample size of 16 per group was necessary to achieve 80% power with a one-sided alpha = .05. As this study was an extension of the Preminger and Ziegler study, a sample size of at least 16 per group was required. Fifty-two participants were randomly assigned to one of three groups: (a) a communication strategies training group (ComStrat; n = 18), (b) a communication strategies training plus psychosocial exercises group (ComStrat + PS; n = 17), and (c) a group in which no training was given but time was spent on informational lectures and psychosocial exercises (Info + PS; n = 17). There was no attempt to balance participants across the treatment groups based on any of the baseline characteristics. Participants were randomly assigned to each treatment group based on their preferred class meeting times. Participants were given class meeting times and no information about the class content. (They were not told that class content varied according to treatment group or meeting time.)
Demographic data for each treatment group are shown in Table 2. Demographic characteristics were compared across groups using a one-way analysis of variance (ANOVA) for the ordinal data (age, years of hearing aid use, preclass HHI scores, and better ear pure-tone average), using a chi-square test for the percentage data (percentage male and percentage recruited via the VA Medical Center), and using the Kruskal–Wallis test for the categorical data (highest educational level achieved and median income level). Probability values associated with each test are shown in Table 2. There were no significant differences in participant characteristics at the baseline visit. It should be noted that the majority of participants were recruited from the Louisville VA Medical Center; thus, they were predominately male.
Table 2.
Demographic characteristics of participants.
| Characteristic | Info + PS | ComStrat | ComStrat + PS | Statistical difference |
|---|---|---|---|---|
| N | 17 | 18 | 17 | |
| Age | 68.8 (6.7) | 68.8 (6.2) | 70.0 (7.1) | F(2, 49) = 0.172, p = .842 |
| HA use | 8.5 (10.6) | 10.9 (12.6) | 10.7 (9.6) | F(2, 48) = 0.249, p = .781 |
| HHI | 63.7 (20.4) | 64.4 (22.9) | 53.1 (17.8) | F(2, 49) = 1.664, p = .200 |
| Better ear PTA | 42.8 (19.7) | 47.9 (15.8) | 40.2 (15.5) | F(2, 49) = 0.914, p = .407 |
| % male | 88% | 83% | 94% | χ2(2, N = 52) = 0.997, p = .607 |
| % VA | 82% | 78% | 94% | χ2(2, N = 52) = 1.892, p = .388 |
| Education | Some college | Some college | Some college | χ2(2, N = 52) = 2.769, p = .837 |
| Income | $18–$42K | $43–$83K | $43–$83K | χ2(2, N = 52) = 3.683, p = .885 |
Note. Mean values with standard deviations in parentheses are shown for the ordinal data: age (in years), years of HA use, preclass Hearing Handicap Index (HHI) scores, and better ear pure-tone average (PTA; 0.5, 1.0, and 2.0 kHz); percentages are shown for percentage male and percentage recruited via the VA; and median values are shown for the categorical data: highest educational level achieved (5 categories: less than high school, some high school, high school graduate, some college, or college graduate) and median income level (4 categories: <$18K, $18–$42K, $43K–$83K, or <$83K). Info + PS = informational lectures plus psychosocial activities group; ComStrat = communication strategies group; ComStrat + PS = communication strategies plus psychosocial activities group.
Four individuals dropped out of the study. Their demographic characteristics are described in Table 3. These individuals were scheduled to participate in a class and completed the preclass evaluation but did not attend the initial class session. The most common reason for dropping out was an inability to attend the scheduled AR classes. These four individuals are not included in Table 2 or in any of the data analyses. Two individuals completed the preclass and post-class evaluations as well as the 6-week AR class but did not complete the 6-month evaluation; they did not respond to requests to schedule the last evaluation. One participant was in the ComStrat group, and the other was in the Info + PS group. These two participants were included in the data analyses.
Table 3.
Demographic characteristics of individuals who dropped out of the study.
| Age | Gender | VA? | PTA | HHI score | HA use (years) |
|---|---|---|---|---|---|
| 75 | Male | No | 35 | 48 | 2 |
| 68 | Male | Yes | 58 | 52 | 10 |
| 74 | Male | No | 72 | 74 | 25 |
| 62 | Male | Yes | 40 | 36 | 2 |
Note. VA? = whether the participant was recruited via the VA Medical Center.
Outcome Measures
Three questionnaires were used as outcome measures: a measure of hearing loss–related quality of life, a measure of generic quality of life, and a questionnaire designed specifically for this project. The quality of life measures were used for two reasons. First, these types of questionnaires are designed to measure the activity limitations and participation restrictions that individuals encounter as a result of hearing loss; thus, they are appropriate for measuring the outcomes of AR (Gagné, 2009). Second, quality of life questionnaires have frequently been used as outcome measures in other studies measuring the efficacy of AR groups (e.g., see Table 1), thus allowing for easier comparison of results across studies. The questionnaire designed for this project was included to sample content areas not addressed by the quality of life measures.
Quality of life
The HHI for the Elderly and the HHI for Adults were used to measure hearing loss–related quality of life (Newman et al., 1990; Ventry & Weinstein, 1982). These questionnaires measure social and emotional functioning as they relate to hearing loss. As they differ by only three of the 25 items (two social and one emotional), results were collapsed across the two forms. These scales have been shown to have adequate internal consistency, test–retest reliability, and criterion-related validity (Newman et al., 1990; Newman, Weinstein, Jacobson, & Hug, 1991; Ventry & Weinstein, 1982; Weinstein, Spitzer, & Ventry, 1986).
The World Health Organization Disability Assessment Schedule II (WHODAS II) was used to measure generic quality of life. This comprehensive quality of life scale was designed to measure the participation restrictions and activity limitations imposed by illness or disability. The 36-item questionnaire contains six subscales: Understanding and Communicating (U&C), Getting Along With People (GAWP), Participation in Society (PIS), Getting Around (GA), Life Activities (LA), and Self-Care (SC). The WHODAS II has been shown to have adequate psychometric properties in adults with hearing loss (Chisolm, Abrams, McArdle, Wilson, & Doyle, 2005) and to be responsive to AR (in regard to hearing aid use, see McArdle, Chisolm, Abrams, Wilson, & Doyle, 2005).
Only three of the six WHODAS II subscales include questions related to speech communication. These are the U&C subscale, in which three of the six items pertain to communication (e.g., one item that did not focus on communication: “In the last week how much difficulty did you have in concentrating on doing something for 10 minutes?”); the GAWP subscale, in which all five questions are indirectly related to communication (e.g., “In the last week how much difficulty did you have in getting along with people who are close to you?”); and the PIS subscale, in which seven (out of eight) items are indirectly related to communication (e.g., “In the last week how much of a problem did you have joining in community activities [e.g., festivities or religious or other activities] in the same way as anyone else can?”). The items in the remaining three subscales focus primarily on physical activities (e.g., in the GA subscale: “In the last week how much difficulty did you have standing up from sitting down?”), maintaining a home (e.g., in the LA subscale: “In the last week how much difficulty did you have in doing your most important household tasks well?”), and activities of daily living (e.g., in the SC subscale: “In the last week how much difficulty did you have in getting dressed?”). Results for the SC subscale are not reported because all participants lived in the community and thus did not report difficulties in self-care (i.e., eating, bathing, dressing, or living independently).
Class evaluation form
A class evaluation form was completed by all participants. This form was designed to measure the perceived benefit of the training and the psychosocial exercises received in the classes. A copy of the class evaluation is shown in Appendix A.
AR Classes
Classes were held in conference rooms located in three audiology practices throughout the Louisville area. The rooms were configured to maximize auditory and visual speech perception. Noise was kept to a minimum, and lighting was maximal. Handouts and projected slides were used to encourage the use of context. See Appendix B for an outline of the material covered in the three different types of AR classes.
Communication strategies exercises
Communication strategies training included both anticipatory strategies and repair strategies. Exercises were adapted from Tye-Murray (1997) and from Kaplan et al. (1985). Additional exercises were developed to demonstrate the importance of concentration, context, and speechreading. Exercises followed one of three formats:
Participants were given handouts and asked to answer questions regarding a specified topic (e.g., participants were asked to identify the key words in a sentence or to identify the desired seat in a typical classroom).
Concepts were demonstrated and then discussed (e.g., the concept of context was demonstrated by asking participants to answer questions about a paragraph presented in noise; in high-context situations, the topic of the paragraph was given prior to reading the paragraph, and in low-context situations, the topic was not given).
Participants were given the opportunity to practice repair strategies both with the instructors and with the other members in the class.
In communication strategies training, multiple solutions were available for most identified problems. Class members were asked to offer solutions, and the group evaluated their merits. When appropriate, the instructor offered solutions that were not identified by the participants.
Psychosocial exercises
The psychosocial exercises described in Preminger and Ziegler (2008) were used in the present experiment. The exercises were designed to encourage discussion of (a) the problems, feelings, attitudes, and emotions associated with hearing loss; (b) other people’s reactions to their hearing loss; and (c) the impact of hearing loss on personal and professional relationships (Hogan, 2001). See Appendix B for a list of topics. To minimize variability across group sessions, the instructors used a list of predetermined questions and prompts when leading a structured discussion about each topic.
Informational lectures
Slide presentations of 1-hr duration were developed. See Appendix B for a list of topics. Discussion and questions were encouraged.
Procedures
See Appendix B for an outline of the procedures and content used in each of the three AR class types. All AR classes met once per week over a 6-week period. At least 1 hr was spent each week on the training exercises in the two training groups, approximately 1 hr was spent on the informational lectures in the Info + PS group, and approximately 30 min were spent each week on the psychosocial exercises in the two + PS group classes. All participants completed at least five of the six classes.
All questionnaires (HHI, WHODAS II, and class evaluation) were administered in a paper-and-pencil format. The participant completed the scales in the presence of the examiner, who was available to answer any questions and ensure that all questions were answered. Participants were evaluated within a 2-week time period prior to the first class, within a 2-week period after the completion of the course, and 6 months after the courses were completed. At each visit, the questionnaires were completed along with pure-tone hearing threshold testing. Hearing threshold levels were monitored so that individuals with fluctuating hearing threshold levels could be excluded from the study. At each evaluation, participants were evaluated with auditory-only and auditory-visual speech perception measures; these results are not reported here.
To identify treatment effects, the baseline, posttreatment, and 6-months questionnaire data were examined with repeated measures ANOVAs (RM-ANOVA). Separate analyses were calculated for each scale and subscale. In each analysis, there was one between-group factor (treatment group: ComStrat, ComStrat + PS, and Info + PS) and one within-group factor (visit: baseline, postclass, and at 6 months). To measure both short-term and long-term treatment effects, the within-subjects contrasts were evaluated specifically for the baseline versus the postclass visit and the baseline versus 6-month visit. If only short-term treatment effects were observed, this would suggest that treatment benefit was not maintained at 6 months. If only long-term training effects were observed, this would suggest that participants needed time following the group classes to appreciate and implement the activities and exercises.
Follow-up tests were conducted for RM-ANOVA results where a significant Visit × Treatment Group interaction was observed based on a Type I error rate of 10%. This relaxed error rate was used due to the small sample size. Follow-up tests were conducted on difference scores (baseline vs. post-class or baseline vs. 6 months), as change in quality of life over time was the metric of interest. The Bonferroni adjustment was used to keep the experimentwise error rate below 5%.
Again, because the sample size was small, effect size was calculated for each treatment group using Cohen’s d (Cohen, 1998) for the baseline versus postclass means and for the baseline versus 6-month means. The standard deviations from the baseline measurement were used rather than the pooled standard deviations to prevent overestimation of the effect size (Dunlop, Cortina, Vaslow, & Burke, 1996). Effect size is a useful measure of the practical significance of a treatment; it measures the magnitude of the relationship between the independent and dependent variables and is not influenced by sample size (Meline & Schmitt, 1997). An effect size of 0.2 is considered small, 0.5 is considered medium, and 0.8 is considered large (Cohen, 1998). Cohen explained that these guidelines should be used with caution and that interpretation is best when compared to effect sizes for similar variables. Recent research has reported effect sizes for the HHI total and two WHODAS II subscales in a group of 176 VA patients when the scales were administered 2 weeks prior to hearing aid fitting and again 8 weeks after the hearing aid fitting (McArdle et al., 2005). Using inferential statistics (RM-ANOVA), significant improvements were measured for these scales and subscales between the baseline and post–hearing aid fitting visits. This study reported effect sizes of 0.74 for the HHI total score, 0.2 for the WHODAS II total, 0.52 for the U&C subscale, and 0.13 for the PIS subscale (McArdle et al., 2005). The authors did caution that the effect size of 0.13 for the PIS subscale was quite small and might not be clinically meaningful.
Results
Hearing Loss–Related Quality of Life
Results for the HHI are shown in Table 4, and results of the RM-ANOVAs are shown in Table 5; significant interactions are shown in Figures 1–4. Scores are reported in terms of hearing handicap, with a lower score indicating a reduced hearing handicap (or improved hearing loss–related quality of life). All treatment groups demonstrated mean preclass performance between 50 and 60 on the HHI scale. All groups showed significant short-term and long-term treatment effects; the RM-ANOVAs showed significant time effects with no significant interactions with group. Although an overall treatment effect was observed on the HHI, Visit × Treatment Group interactions may be explored to determine whether short-term and long-term effects differed across the three groups.
Table 4.
Mean quality of life scores (with standard deviations) and effect sizes.
| Subscales and groups |
Baseline | Postclass visit | 6-month visit | Effect size: Baseline vs. postclass visit |
Effect size: Baseline vs. 6-month visit |
|---|---|---|---|---|---|
| HHI: Total | |||||
| ComStrat | 64.4 (22.9) | 54.2 (24.5) | 58.6 (24.9) | 0.445* | 0.253* |
| ComStrat + PS | 53.1 (17.8) | 39.1 (20.7) | 39.2 (23.4) | 0.787** | 0.787** |
| Info + PS | 63.8 (20.4) | 48.0 (21.7) | 43.8 (21.0) | 0.775** | 0.98*** |
| HHI: Social | |||||
| ComStrat | 31.2 (10.0) | 27.3 (10.9) | 28.2 (11.5) | 0.390* | 0.300* |
| ComStrat + PS | 27.1 (9.3) | 20.4 (9.0) | 21.4 (11.0) | 0.720** | 0.613** |
| Info + PS | 30.5 (11.1) | 24.6 (20.0) | 23.5 (9.2) | 0.532** | 0.631** |
| HHI: Emotional | |||||
| ComStrat | 33.2 (13.5) | 26.9 (14.1) | 30.4 (13.9) | 0.467* | 0.210* |
| ComStrat + PS | 25.7 (10.5) | 18.7 (12.5) | 17.8 (13.4) | 0.667** | 0.752** |
| Info + PS | 33.2 (10.6) | 23.4 (12.3) | 20.3 (12.5) | 0.925*** | 1.217*** |
| WHODAS II: Total | |||||
| ComStrat | 24.9 (18.4) | 26.4 (20.6) | 28.6 (19.3) | −0.082 | −0.201† |
| ComStrat + PS | 21.6 (17.9) | 21.1 (15.2) | 19.5 (17.6) | 0.028 | 0.117 |
| Info + PS | 21.3 (16.0) | 18.9 (16.8) | 17.9 (12.3) | 0.150 | 0.213* |
| WHODAS II: U&C | |||||
| ComStrat | 29.2 (18.9) | 28.6 (20.8) | 32.4 (20.1) | 0.0317 | −0.0175 |
| ComStrat + PS | 21.2 (17.5) | 24.1 (14.4) | 21.8 (17.4) | −0.166 | −0.034 |
| Info + PS | 22.4 (15.5) | 21.5 (18.94) | 18.1 (15.7) | 0.058 | 0.277* |
| WHODAS II: GAWP | |||||
| ComStrat | 23.61 (20.3) | 26.9 (21.7) | 32.8 (25.3) | −0.162 | −0.453† |
| ComStrat + PS | 25.5 (17.6) | 21.1 (18.0) | 18.1 (17.7) | 0.250* | 0.421* |
| Info + PS | 23.5 (22.1) | 18.6 (21.8) | 19.8 (17.7) | 0.225* | 0.170 |
| WHODAS II: PIS | |||||
| ComStrat | 26.6 (20.5) | 28.9 (19.8) | 34.4 (21.0) | −0.112 | −0.380† |
| ComStrat + PS | 23.0 (20.2) | 20.1 (18.6) | 18.4 (20.0) | 0.144 | 0.228* |
| Info + PS | 26.5 (20.7) | 21.6 (19.1) | 22.1 (15.5) | 0.237* | 0.213* |
| WHODAS II: GA | |||||
| ComStrat | 26.4 (27.7) | 31.3 (32.4) | 27.1 (29.2) | −0.163 | −0.025 |
| ComStrat + PS | 25.7 (24.7) | 28.7 (25.8) | 26.5 (26.7) | −0.119 | −0.031 |
| Info + PS | 23.9 (24.2) | 22.1 (24.9) | 24.1 (21.9) | 0.073 | −0.009 |
| WHODAS II: LA | |||||
| ComStrat | 27.2 (27.8) | 26.1 (29.7) | 24.7 (25.6) | 0.038 | 0.094 |
| ComStrat + PS | 21.2 (24.2) | 20.6 (22.5) | 20.0 (21.5) | 0.026 | 0.052 |
| Info + PS | 21.2 (25.5) | 20.0 (21.5) | 21.8 (22.4) | 0.051 | −0.025 |
Note. WHODAS II = World Health Organization Disability Assessment Schedule II; U&C = Understanding and Communicating; GAWP = Getting Along With People; PIS = Participation in Society; GA = Getting Around; LA = Life Activities.
= small effect size;
= medium effect size;
= large effect size;
= small negative effect size.
Table 5.
Short-term (baseline visit vs. postclass visit) and long-term (baseline visit vs. 6-month visit) repeated measures analysis of variance results for HHI scale and subscales and WHODAS II scale and subscales.
| Interactions | HHI: Total | HHI: Social | HHI: Emotional |
|---|---|---|---|
| Visit | |||
| Baseline vs. postclass | F(1, 49) = 26.8, p < .001* | F(1, 49) = 17.9, p < .001* | F(1, 49) = 29.1, p < .001* |
| Baseline vs. 6-month | F(1, 49) = 33.4, p < .001* | F(1, 49) = 17.9, p < .001* | F(1, 49) = 35.4, p < .001* |
| Visit × Subgroup | |||
| Baseline vs. postclass | F(2, 49) = 0.41, p = .666 | F(2, 49) = 0.42, p = .659 | F(2, 49) = 0.58, p = .562 |
| Baseline vs. 6-month | F(2, 49) = 1.79, p = .178 | F(2, 49) = 0.49, p = .615 | F(2, 49) = 2.97, p = .061+ |
|
| |||
| WHODAS II Total | WHODAS II U&C | WHODAS II GAWP | |
|
| |||
| Visit | |||
| Baseline vs. postclass | F(1, 49) = 0.18, p = .670 | F(1, 49) = 0.07, p = .789 | F(1, 49) = 1.25, p = .269 |
| Baseline vs. 6-month | F(1, 49) = 0.00, p = .954 | F(1, 49) = 0.01, p = .922 | F(1, 49) = 0.07, p = .798 |
| Visit × Subgroup | |||
| Baseline vs. postclass | F(2, 49) = 0.91, p = .410 | F(2, 49) = 0.43, p = .656 | F(2, 49) = 2.15, p = .127 |
| Baseline vs. 6-month | F(2, 49) = 1.81, p = .174 | F(2, 49) = 0.74, p = .482 | F(2, 49) = 4.62, p = .015* |
|
| |||
| WHODAS II | PIS WHODAS II GA | WHODAS II LA | |
|
| |||
| Visit | |||
| Baseline vs. postclass | F(1, 49) = 1.01, p = .321 | F(1, 49) = 0.96, p = .331 | F(1, 49) = 0.19, p = .664 |
| Baseline vs. 6-month | F(1, 49) = 0.03, p = .864 | F(1, 49) = 0.09, p = .772 | F(1, 49) = 0.29, p = .592 |
| Visit × Subgroup | |||
| Baseline vs. postclass | F(2, 49) = 1.40, p = .256 | F(2, 49) = 0.97, p = .386 | F(2, 49) = 0.01, p = .993 |
| Baseline vs. 6-month | F(2, 49) = 4.20, p = .021* | F(2, 49) = 0.01, p = .990 | F(2, 49) = 0.22, p = .803 |
Note. Probability levels followed by a plus sign are significant at the .10 level; probability levels followed by an asterisk are significant at the .05 level.
Figure 1.
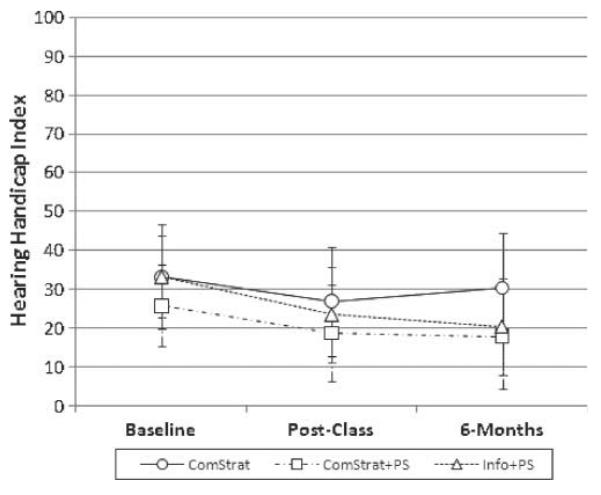
Average Hearing Handicap Index Emotional score for each subject group before class (Baseline), after class (Post-Class), and 6 months after class (6-Months). Performance for the communication strategies training (ComStrat) group is shown with the solid line and circle symbols, communication strategies training plus psychosocial (ComStrat + PS) group with a dashed and dotted line and square symbols, and informational lectures plus psychosocial (Info + PS) group with the dashed line and triangle symbols. Error bars indicate ±1 SD. A lower score indicates better hearing loss–related quality of life.
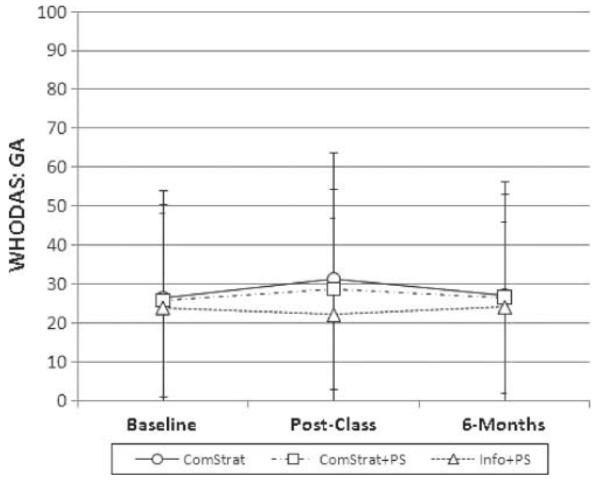
Figure 4.
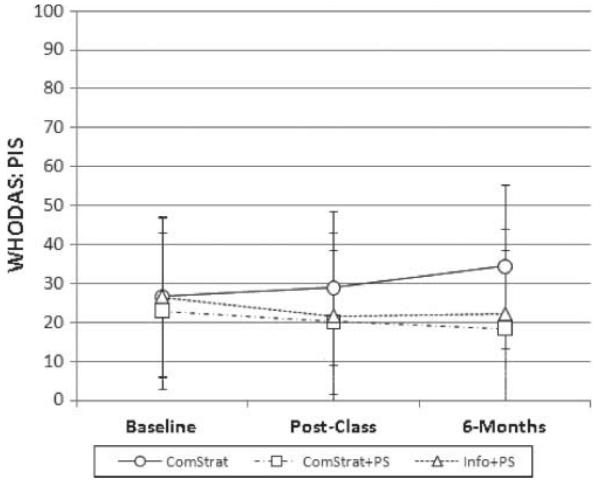
WHODAS II scores for the Performance in Society (PIS) subscale. Average scores are shown for each subject group before class (Baseline), after class (Post-Class), and 6 months after class (6-Months). Performance for the ComStrat group is shown with the solid line and circle symbols, ComStrat + PS group with a dashed and dotted line and square symbols, and Info + PS group with the dashed line and triangle symbols. Error bars indicate ±1 SD. A lower score indicates better quality of life.
There was one Visit × Treatment Group interaction that was significant at a .10 alpha level (but not at .05) for the HHI data; this was seen for the Emotional subscale. The RM-ANOVA results showed a significant effect for time, with no significant interaction for the baseline versus postclass visit. This can be seen in Figure 1; all three groups showed improved performance on the HHI scale from the initial visit to the postclass visit. The significant interaction was observed for the preclass versus 6-month visit. The results for the ComStrat group showed a slight improvement in hearing loss–related quality of life from the baseline to the 6-month visit (mean improvement = 2.8 points). The other two groups demonstrated greater improvements in hearing loss–related quality of life from the baseline to the 6-month visit (mean improvements = 7.9 points for ComStrat + PS and 12.9 points for Info + PS).
Three follow-up tests were performed on the baseline versus 6-month difference score comparisons. Using the Bonferroni correction, probability levels had to be less than .0167 (.05/3) to be considered significant. The results showed a significant difference for the ComStrat versus Info + PS difference scores (p = .008); however, no significant findings were observed when comparing the ComStrat and ComStrat + PS difference scores (p = .033) or the ComStrat + PS and the Info + PS difference scores (p = .262). Similar findings are seen by examining the long-term effects sizes (see Table 4), which were small for the ComStrat group, medium for the ComStrat + PS group, and large for the Info + PS group. In the two groups with psychosocial exercises, baseline to 6-month effect sizes for the HHI Total subscale as well as the HHI Total scale were greater than the 0.74 effect size reported by McArdle et al. (2005).
Generic Quality of Life
Results for the WHODAS II are shown in Table 4, and results of the RM-ANOVAs are shown in Table 5. Scores are reported in terms of health state, with a lower score indicating a better health state and a higher score indicating greater participation restrictions and activity limitations. The mean WHODAS II group scores at baseline ranged between 21 and 25. These are poorer than mean WHODAS II scores for 384 veterans with hearing loss reported by Chisolm et al. (2005), who reported a mean of 15.8 with a standard deviation of 16.10. The participants in the present study were all experienced hearing aid users who were motivated enough to attend AR classes, whereas the individuals in the Chisolm et al. study were hearing aid candidates with better average hearing levels and HHI scores, indicating better hearing loss–related quality of life than the participants in the current study.
In the current study, the mean total WHODAS II scores remained stable over time for all treatment groups. This was confirmed with the RM-ANOVA results. This is not surprising, as the majority of scale items do not directly or indirectly assess communication. Additional RM-ANOVAs were run for the three WHODAS II subscales that included questions directly or indirectly related to communication (U&C, GAWP, and PIS) and, for comparison purposes, two scales that did not include any communication-related items (GA and LA).
There were no significant findings for the U&C subscale (the scale with only three of the six items related to communication). There were significant RM-ANOVA interactions for the GAWP and PIS subscales (in which all items were related to communication). Figure 2 shows the results for the GAWP subscale. The RM-ANOVAs demonstrated a significant interaction between visit (preclass vs. 6-month) and treatment group. Health states improved slightly for the ComStrat + PS group and the Info + PS groups, and there was a small effect size for the ComStrat + PS data. Participation restrictions and activity limitations declined over the same time period for the ComStrat group (with a small negative effect size).
Figure 2.
World Health Organization Disability Assessment Schedule II (WHODAS II) scores for the Getting Along With People (GAWP) subscale. Average scores are shown for each subject group before class (Baseline), after class (Post-Class), and 6 months after class (6-Months). Performance for the ComStrat group is shown with the solid line and circle symbols, ComStrat + PS group with a dashed and dotted line and square symbols, and Info + PS group with the dashed line and triangle symbols. Error bars indicate ±1 SD. A lower score indicates better quality of life.
Three follow-up tests were performed on the baseline versus 6-month difference score comparisons. Using the Bonferroni correction, probability levels had to be less than .0167 (.05/3) to be considered significant. The results showed a significant difference for the ComStrat versus ComStrat + PS difference scores (p = .005) and between the ComStrat and Info + PS difference scores (p = .012). No significant finding was observed when comparing the ComStrat + PS and the Info + PS difference scores (p = .429). It is difficult to interpret these results, as it is unclear why the individuals in the ComStrat group showed a small decline in health state as measured by this scale. What is interesting is that the two groups who included psychosocial activities did not demonstrate this negative trend, and the individuals in the ComStrat + PS group did demonstrate a small positive improvement in health state.
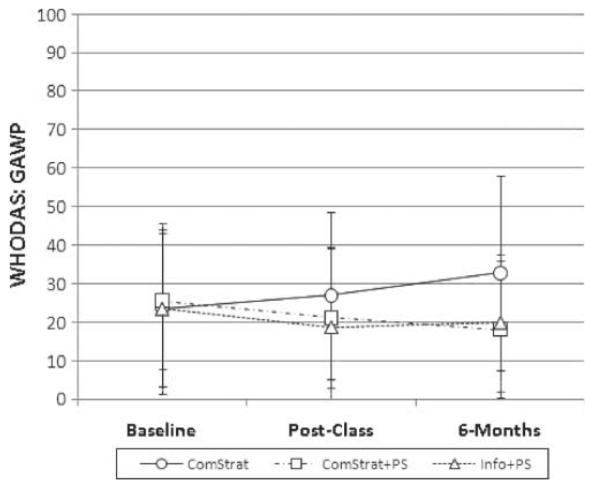
To aid in the interpretation of the results for the GAWP subscale, it is useful to consider the findings for the two subscales that did not contain any communication-related items: the GA and LA subscales. Across all three groups, the results remained very stable over time; this is shown by short-term and long-term effect sizes that were all less than 0.2 (see Table 4) and by the lack of any significant within-subjects contrasts in the RM-ANOVA findings (see Table 5). Figure 3 shows the findings for the GA subscale. Whereas Figure 2 shows a clear separation in long-term treatment effects for the ComStrat + PS and Info + PS groups versus the ComStrat group, Figure 3 shows a relatively stable health state with no evidence of long-term treatment effects and no evidence of between-group differences.
Figure 3.
WHODAS II scores for the Getting Around (GA) subscale. Average scores are shown for each subject group before class (Baseline), after class (Post-Class), and 6 months after class (6-Months). Performance for the ComStrat group is shown with the solid line and circle symbols, ComStrat + PS group with a dashed and dotted line and square symbols, and Info + PS group with the dashed line and triangle symbols. Error bars indicate ±1 SD. A lower score indicates better quality of life.
The findings for the PIS subscale are similar to findings for the GAWP subscale. The RM-ANOVAs demonstrated a significant interaction between visit (preclass vs. 6-month) and treatment group. Figure 4 appears almost identical to Figure 2; health status improved slightly for the ComStrat + PS group and the Info + PS groups (with small effect sizes for both groups), while participation restrictions and activity limitations declined over the same time period for the ComStrat group (with a small negative effect size). While the long-term effect sizes were small, they were all larger than the effect size of 0.13 reported by McArdle et al. (2005) for the PIS subscale. In the case of the RM-ANOVA, however, none of the difference score comparisons were significant after applying the Bonferroni correction (ComStrat vs. ComStrat + PS, p = .0169; ComStrat vs. Info + PS, p = .061; ComStrat + PS vs. Info + PS, p = .337).
Class Evaluation
Each individual who participated in an actual class completed a 10-item evaluation form at the postclass assessment. The response distributions are shown in Table 6. Participants, regardless of AR group, reported benefit from attending a class. The majority of participants reported that, as a result of attending the classes, their ability to lipread, understand speech in quiet, and communicate became either a little better or a lot better (Questions 1, 2, and 4). Between 40% and 50% of participants reported improved ability to understand speech in noise (Question 3). The majority of participants reported that they enjoyed the classes and learned new skills (Question 7). Despite the fact that they received no explicit training, 70% of the participants in the Info + PS group reported learning new skills. The majority of participants reported benefit from being with others who had hearing loss, from learning how others with hearing loss cope, and from understanding the feelings of others with hearing loss (Questions 8, 9, and 10). This was the case for those who did participate in psychosocial exercises (ComStrat + PS and Info + PS) and those who did not (ComStrat).
Table 6.
Percentage per treatment group responding to each statement in the class evaluation scale.
| As a result of these classes… | Become worse | Stayed the same | Become a little better | Become a lot better | |
|---|---|---|---|---|---|
| 1. My ability to lipread has | |||||
| ComStrat | 0% | 22% | 50% | 28% | |
| ComStrat + PS | 0% | 41% | 53% | 6% | |
| Info + PS | 0% | 35% | 41% | 24% | |
| χ2(2, N = 52) = 2.75, p = .253a | |||||
| 2. My ability to understand speech in quiet has | |||||
| ComStrat | 5% | 28% | 56% | 11% | |
| ComStrat + PS | 0% | 18% | 70% | 12% | |
| Info + PS | 0% | 53% | 29% | 17% | |
| χ2(2, N = 52) = 2.09, p = .352 | |||||
| 3. My ability to understand speech in noise has | |||||
| ComStrat | 11% | 45% | 44% | 0% | |
| ComStrat + PS | 6% | 53% | 35% | 6% | |
| Info + PS | 0% | 53% | 47% | 0% | |
| χ2(2, N = 52) = 0.25, p = .882 | |||||
| 4. My ability to communicate with others has | |||||
| ComStrat | 0% | 16% | 68% | 16% | |
| ComStrat + PS | 0% | 12% | 70% | 18% | |
| Info + PS | 0% | 18% | 70% | 12% | |
| χ2(2, N = 52) = 0.38, p = .829 | |||||
|
|
|||||
| 5. If you would have had to pay for these classes, think about how much money you believe these 5 classes were worth in relation to other services that you pay for: |
$0 | $25–$50 | $75–$100 | >$100 | |
|
|
|||||
| ComStrat | 0% | 39% | 33% | 28% | |
| ComStrat + PS | 0% | 23% | 53% | 24% | |
| Info + PS | 6% | 29% | 65% | 0% | |
| χ2(2, N = 52) = 2.96, p = .228 | |||||
|
|
|||||
| 6. If you had the opportunity to continue taking these classes, how much would you be willing to pay for a 5-week course? |
$0 | $25–$50 | $75–$100 | >$100 | Not interested |
|
|
|||||
| ComStrat | 5% | 39% | 39% | 11% | 6% |
| ComStrat + PS | 12% | 23% | 59% | 0% | 6% |
| Info + PS | 18% | 41% | 23% | 6% | 12% |
| χ2(2, N = 52) = 0.89, p = .642 | |||||
|
|
|||||
| 7. Which statement best describes your feelings about this course: |
Enjoy no/learn no | Enjoy no/learn yes | Enjoy yes/learn no | Enjoy yes/learn yes | |
|
|
|||||
| ComStrat | 0% | 0% | 11% | 89% | |
| ComStrat + PS | 0% | 0% | 6% | 94% | |
| Info + PS | 6% | 0% | 24% | 70% | |
| χ2(2, N = 52) = 4.09, p = .129 | |||||
|
|
|||||
| Please rate how important each aspect of the course was to you: |
Did not occur | Not important | A little important | Somewhat important |
Very important |
|
|
|||||
| 8. Being with other people who have similar hearing problems as me |
|||||
| ComStrat | 0% | 0% | 17% | 39% | 44% |
| ComStrat + PS | 0% | 6% | 18% | 29% | 47% |
| Info + PS | 0% | 0% | 12% | 29% | 59% |
| χ2(2, N = 52) = 0.96, p = .629 | |||||
| 9. Learning how others with hearing loss cope | |||||
| ComStrat | 0% | 0% | 0% | 67% | 44% |
| ComStrat + PS | 0% | 0% | 18% | 29% | 53% |
| Info + PS | 0% | 0% | 0% | 29% | 71% |
| χ2(2, N = 52) = 2.75, p = .268 | |||||
| 10. Understanding the feelings that others have about their hearing loss |
|||||
| ComStrat | 0% | 0% | 0% | 44% | 56% |
| ComStrat + PS | 0% | 0% | 12% | 41% | 47% |
| Info + PS | 0% | 0% | 0% | 35% | 65% |
| χ2(2, N = 52) = 1.64, p = .440 | |||||
Results of Kruskal–Wallis test for statement.
The results were compared across groups using the Kruskal–Wallis test, a nonparametric method for testing equality of medians among groups. The results for these analyses are shown in Table 6. There were no significant differences in response distributions across the three AR groups for any of the 10 questions. This was also the case for the questions that measured the worth of the classes (Questions 5 and 6). The majority of participants reported that the 5-week class was worth between $75 and over $100.
Discussion
The purpose of this study was to determine whether group AR content affected the measured outcomes. It was hypothesized that (a) individuals who participated in AR classes, which included both training and psychosocial activities (ComStrat + PS), would demonstrate the best outcomes and (b) individuals who participated in AR classes, which included training and no psychosocial activities (ComStrat), would show the poorest outcomes. Class benefit was measured in three ways: with a hearing loss–specific quality of life scale, with a generic quality of life scale, and with a class-specific questionnaire. The results showed very limited support for the hypotheses. Whereas all three groups demonstrated short-term and long-term improvements in hearing loss–related quality of life, there was a trend toward greater improvements for the two groups who included psychosocial exercises. The ComStrat + PS group and the Info + PS group demonstrated medium or large short-term and long-term effect sizes for the HHI scale and subscales, while the ComStrat group showed only small effect sizes. The Info + PS group demonstrated greater long-term benefits on the HHI Emotional subscale than the ComStrat group. Similar findings were observed for two of the three WHODAS II subscales that contained communication-related items. The two groups who included psychosocial activities demonstrated small long-term treatment effects for the GAWP and PIS subscales, while the ComStrat group showed small long-term declines in quality of life. Significant findings were observed for the GAWP subscale, where both groups who contained psychosocial exercises demonstrated significantly better long-term improvement in health state than the group without psychosocial exercises. The results for the class evaluation did not discriminate among the treatment groups. The majority of participants, regardless of group affiliation, reported improved communication following class participation. Additionally, the majority of participants valued sharing with and learning from their AR classmates.
Similar findings have recently been reported by Hickson et al. (2007); they compared outcomes for a training group who participated in a group-directed communication strategies program (the ACE program) with a placebo social group who participated in lectures/discussions about communication as it related to aging. Their ACE training group had similar content to the ComStrat groups in the current study, and their placebo social group had similar content to our Info + PS group. Hickson et al. did measure significant postclass versus preclass improvement on a variety of quality of life measures for the ACE training group; however, there were no significant differences between the ACE training group and the social placebo group in preclass versus post-class outcomes. In other words, class content did not influence benefit.
The results from the present study can also be compared to the findings from an earlier study in which we evaluated the influence of AR class content on quality of life outcomes using a similar study design (Preminger & Ziegler, 2008). In the previous study, three groups of participants were evaluated: a group who received auditory-only and auditory-visual speech perception training (SpeechTrain), a group who received speech perception training plus psychosocial exercises (SpeechTrain + PS), and a control group who received no attention but did participate in the extensive evaluation battery over three test intervals. The results demonstrated a significant improvement in hearing loss–related quality of life as measured by the Emotional subscale of the HHI for the training participants but not for the control participants. None of the participant groups demonstrated any short-term or long-term treatment effects on the WHODAS II or any of its subscales (Preminger & Ziegler, 2008).
Effect sizes can be compared across the present study and the Preminger and Ziegler (2008) study to determine whether there were consistent findings for different types of class content; these are shown in Table 7. The long-term (baseline vs. 6-months) results for the HHI Emotional subscale were examined, since that is where a significant finding was observed in the present study. The three groups who included psychosocial activities showed either medium or large effect sizes. Small effect sizes were seen for the two groups who had training but no psychosocial exercises and for the control group. (See Preminger & Ziegler, 2008, for a discussion that postulates why significant findings were measured in the control group; it is proposed that this finding was due to attention, specifically the speech perception testing.)
Table 7.
Effect sizes for the HHI Emotional subscale for participant groups in the current study and for participant groups in Preminger and Ziegler (2008).
| Participant group | Baseline vs. 6-month evaluation |
|---|---|
| ComStrat | 0.210* |
| ComStrat + PS | 0.752** |
| Info + PS | 1.217*** |
| SpeechTrain | 0.234* |
| SpeechTrain + PS | 0.515** |
| Control | 0.214* |
Note. The three groups from the Preminger and Ziegler (2008) study are in boldface.
= small effect size;
= medium effect size;
= large effect size.
Taken together, results in the present study and results in previous studies demonstrate two clinical findings. First, group AR classes result in improved hearing loss–related quality of life for the majority of individuals who participate. This is true for individuals with hearing loss who do not wear hearing aids (Hickson et al., 2007), for new hearing aid users (Hickson et al., 2007), and for experienced hearing aid users (current study; Preminger & Ziegler, 2008). Second, class content appears to have only a minimal influence on outcomes. There is limited evidence that the inclusion of psychosocial exercises will improve outcomes related to the emotional aspects of hearing loss–related quality of life. Outcomes were poorest for classes that included training only, either speech perception training or communication strategies training.
It is interesting to consider the theoretical basis for the small differences observed across studies. As discussed above, coping strategies can be classified into problem-focused coping that centers on problem management and emotion-focused coping that centers on management of one’s emotional response (Lazarus & Folkman, 1984). We can use this rubric to classify the class content shown in Table 7. Communication strategy training and speech perception training both encourage problem-focused coping, as the AR training includes the identification of problems and the practicing of possible solutions. Informational lectures thatwere included in the Info + PS group classes can also be considered problem-focused coping, as increasing one’s knowledge about hearing loss, communication, hearing aids, and assistive listening devices is also a way to identify problems and generate solutions. On the other hand, psychosocial exercises can be considered emotion-focused coping. Specific emotion-focused techniques were applied in these exercises, such as stress reduction exercises that aid individuals in minimizing negative emotions. Additionally, the group experience allowed for social comparison to occur. Group members engage in social comparison when they compare themselves with others who have the same condition (Suls, Matin, & Wheeler, 2002). Downward social comparison occurs when one feels that he or she is coping better than others with a similar condition (e.g., “My hearing loss and communication problems are not so bad compared to what the others in the group experience”), whereas upward social comparison occurs when one feels that he or she is coping as well as others who appear to manage their condition well (Suls et al., 2002).
Research in other fields has shown that habilitation/rehabilitation programs which include both problem-focused and emotion-focused activities result in the best outcomes (Auerbach, 1989; Duangdao & Roesch, 2008; Martelli, Auerbach, Alexander, & Mercuri, 1987). For example, Martelli et al. (1987) measured postsurgical outcomes in a group of individuals who had oral surgery; outcomes included measures of anxiety, pain, and satisfaction with surgery. Prior to surgery, one group of patients completed a problem-focused intervention (information and instruction), a second group completed an emotion-focused intervention (stress reduction exercises), and a third group completed both types of intervention. The highest satisfaction with surgery was measured in the mixed intervention group, and the emotion-focused intervention produced the poorest postsurgery attitudes (Martelli et al., 1987). More recently, Duangdao and Roesch (2008) published a meta-analysis of 21 studies that measured the effectiveness of emotion-focused and problem-focused programs for patients with diabetes. They measured better adjustment to disease in patients who completed problem-focused interventions, and they found that individuals who completed emotion-focused programs had better outcomes on indices of adjustment related to anxiety and depression.
These findings suggest that superior AR outcomes would result from classes that focus on a mix of coping strategies. Classes that include training (communication strategy and/or speech perception), informational lectures, and psychosocial exercises would likely result in the greatest improvement in hearing loss–related quality of life. There was a trend toward this finding in the current study. It must be stressed, however, that the difference in outcomes across class types was minimal.
Study Limitations
There are three limitations in the design of the present study that should be considered in the interpretation of the results. First, this randomized controlled study had three treatment arms but no control group. As a result, it is not possible to state with certainty that any of the treatments described here are more effective than no treatment at all. Second, the class evaluation questionnaire designed for use in this study has not received a psychometric evaluation. This questionnaire was included to determine whether participants believed that the course content (e.g., communication strategies training, informational lectures, and/or psychosocial exercises) influenced their ability to communicate (Questions 1–4), the value of the course (Questions 5–7), or the psychosocial content of the course (Questions 8–10). It is possible that differences were not observed across the treatment groups as a result of poor reliability or sensitivity in the class evaluation measure. Third, this study did not consider individual subject characteristics in determining treatment efficacy. It is possible that certain types of individuals may be more responsive to certain types of class content. For example, it has been shown that personality type is associated with self-reported hearing aid outcomes (Cox, Alexander, & Gray, 2007). Future research can determine whether personality type is associated with AR group outcomes by looking at individual results rather than group results.
Conclusions
The purpose of this study was to determine whether group AR content affected the outcomes. The results suggested that class content had only a minimal influence on treatment outcome, with poorer outcomes in classes that did not include psychosocial exercises. It is recommended that AR class content contain a mix of interventions including information, training, and psychosocial exercises.
Acknowledgments
This research was supported by National Institutes of Health Grant 5R03DC004939-02 (“The Efficacy of Group Aural Rehabilitation Programs”) and with resources at the Louisville VA Medical Center. Portions of this article were presented at the meeting of the American Auditory Society, Scottsdale, AZ, March 2006. We would like to thank the many students who have worked on this project: Scott Anderson, James Baer, Tara Blalock, Mitchell Campbell, Elizabeth Everett White, Miriam Harris-Shelton, Jennifer Leddy, Jodee Pride, Emily Schauwecker, Jeff Shannon, and Allison Young.
Appendix A. Audiologic Rehabilitation Research Project: Rehabilitation Class Evaluation
| As a result of these classes… | ||||
| Become worse |
Stayed the same |
Become a little better |
Become a lot better |
|
| 1. My ability to lipread has | 1 | 2 | 3 | 4 |
| 2. My ability to understand speech in quiet has | 1 | 2 | 3 | 4 |
| 3. My ability to understand speech in noise has | 1 | 2 | 3 | 4 |
| 4. My ability to communicate with others has | 1 | 2 | 3 | 4 |
| 5. If you would have had to pay for these classes, think about how much money you believe these 5 classes were worth in relation to other services that you pay for:
| ||||
6. If you had the opportunity to continue taking these classes, how much would you be willing to pay?
| ||||
7. Which statement best describes your feelings about this course?
| ||||
| Please rate how important each aspect of the course was to you: | |||||
| Did not occur |
Not important |
A little important |
Somewhat important |
Very important |
|
| 8. Being with other people who have similar hearing problems as me |
1 | 2 | 3 | 4 | 5 |
| 9. Learning how others with hearing loss cope | 1 | 2 | 3 | 4 | 5 |
| 10. Understanding the feelings that others have about their hearing loss |
1 | 2 | 3 | 4 | 5 |
Appendix B. Content in Each of the Three Audiologic Rehabilitation Class Types
| Group type | Info + PS | ComStrat | ComStrat + PS |
|---|---|---|---|
| Training activities | None | Communication strategiesa | Communication strategiesa |
| Psychosocial activitiesb | Yes | None | Yes |
| Informational lecturesc | Yes | None | None |
| Instructors | 2 or 3 | 2 or 3 | 2 or 3 |
| 1st author present | 1st author present | 1st author present | |
| 100% | 75% | 100% | |
| Total meeting time | 6 classes | 6 classes | 6 classes |
| 75 min each | 60 min each | 90 min each |
- Class 1: Communication Suggestions, Assertiveness Training, Repair Strategies (Repeat, Rephrase, Elaborate, Asking Specific Questions)
- Class 2: Problem Identification, Assertiveness Training, Keywords, Repair Strategies, Placement (Best Place to Sit in a Classroom)
- Class 3: Controlling the Situation, Keywords, Repair Strategies, Taking Advantage of Lipreading
- Class 4: Divided Attention, Assertiveness Training, Keywords, Repair Strategies, Placement (Best Place to Sit in a Restaurant)
- Class 5: Concentration, Keywords, Repair Strategies, Taking Advantage of Lipreading
- Class 6: Humor, Problem Identification, Problem Solving, Placement (Best Place to Sit in a Living Room)
- Class 1: What’s the Worst Thing About Having a Hearing Loss?
- Class 2: I’m at a House Party, and I Can’t Understand What Is Going On!
- Class 3: You Know I Can’t Hear You When the Water’s Running!
- Class 4: Stress Reduction and Relaxation Exercises
- Class 5: Discussion of Letters Written to Hearing Loss Magazine
- Class 6: Have You Ever Attended a Wedding and Missed Everything That Was Said?
- Class 1: How We Hear and Understanding Your Audiogram
- Class 2: A Model of Communication
- Class 3: Getting the Most Out of Your Hearing Aids: Features and Functions
- Class 4: Assistive Listening Devices: Demonstration and Explanations
- Class 5: Cochlear Implants: Who Is a Candidate, What Do They Do?
- Class 6: Tinnitus and Vestibular Problems
Contributor Information
Jill E. Preminger, University of Louisville School of Medicine, Louisville, KY
Jae K. Yoo, University of Louisville School of Public Health
References
- Abrams HB, Chisolm TH, McArdle R. A cost-utility analysis of adult group audiologic rehabilitation: Are the benefits worth the cost? Journal of Rehabilitation Research and Development. 2002;39:549–558. [PubMed] [Google Scholar]
- Abrams HB, Hnath-Chisolm T, Guerreiro SM, Ritterman SI. The effects of intervention strategy on self-perception of hearing handicap. Ear and Hearing. 1992;13:371–377. doi: 10.1097/00003446-199210000-00013. [DOI] [PubMed] [Google Scholar]
- Andersson G, Melin L, Lindberg P, Scott B. Development of a short scale for self-assessment of experiences of hearing loss. The hearing coping assessment. Scandinavian Audiology. 1995;24:147–154. doi: 10.3109/01050399509047528. [DOI] [PubMed] [Google Scholar]
- Andersson G, Melin L, Scott B, Lindberg P. An evaluation of a behavioural treatment approach to hearing impairment. Behaviour Research and Therapy. 1995;33:283–292. doi: 10.1016/0005-7967(94)00040-q. [DOI] [PubMed] [Google Scholar]
- Auerbach SM. Stress management and coping research in the health care setting: An overview and methodological commentary. Journal of Consulting and Clinical Psychology. 1989;57:388–395. doi: 10.1037//0022-006x.57.3.388. [DOI] [PubMed] [Google Scholar]
- Beynon GJ, Thornton FL, Poole C. A randomized, controlled trial of the efficacy of a communication course for first time hearing aid users. British Journal of Audiology. 1997;31:345–351. doi: 10.3109/03005364000000028. [DOI] [PubMed] [Google Scholar]
- Chisolm TH, Abrams HB, McArdle R. Short- and long-term outcomes of adult audiological rehabilitation. Ear and Hearing. 2004;25:464–477. doi: 10.1097/01.aud.0000145114.24651.4e. [DOI] [PubMed] [Google Scholar]
- Chisolm TH, Abrams HB, McArdle R, Wilson RH, Doyle PJ. The WHO-DAS II: Psychometric properties in the measurement of functional health status in adults with acquired hearing loss. Trends in Amplification. 2005;9:111–126. doi: 10.1177/108471380500900303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed Erlbaum; Hillsdale, NJ: 1998. [Google Scholar]
- Cox RM, Alexander GC, Gray GA. Personality, hearing problems, and amplification characteristics: Contributions to self-report hearing aid outcomes. Ear and Hearing. 2007;28:141–162. doi: 10.1097/AUD.0b013e31803126a4. [DOI] [PubMed] [Google Scholar]
- Demorest ME, Erdman SA. Development of the Communication Profile for the Hearing Impaired. Journal of Speech and Hearing Disorders. 1987;52:129–143. doi: 10.1044/jshd.5202.129. [DOI] [PubMed] [Google Scholar]
- Duangdao KM, Roesch SC. Coping with diabetes in adulthood: A meta-analysis. Journal of Behavioral Medicine. 2008;31:291–300. doi: 10.1007/s10865-008-9155-6. [DOI] [PubMed] [Google Scholar]
- Dunlop WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gagné JP. The ICF: A classification system and conceptual framework ideal for audiological rehabilitation. Perspectives on Aural Rehabilitation and Its Instrumentation. 2009;16:8–14. [Google Scholar]
- Giolas T, Owens E, Lamb S, Schubert E. Hearing Performance Inventory. Journal of Speech and Hearing Disorders. 1979;44:169–195. doi: 10.1044/jshd.4402.169. [DOI] [PubMed] [Google Scholar]
- Hallberg LRM, Barrenas ML. Group rehabilitation of middle-aged males with noise-induced hearing loss and their spouses: Evaluation of short- and long-term effects. British Journal of Audiology. 1994;28:71–79. doi: 10.3109/03005369409077917. [DOI] [PubMed] [Google Scholar]
- Hardick EJ, Oyer HJ, Irion PE. Lipreading performance as related to measurements of vision. Journal of Speech and Hearing Research. 1970;13:92–100. doi: 10.1044/jshr.1301.92. [DOI] [PubMed] [Google Scholar]
- Hawkins DB. Effectiveness of counseling-based adult group aural rehabilitation programs: A systematic review of the evidence. Journal of the American Academy of Audiology. 2005;16:485–493. doi: 10.3766/jaaa.16.7.8. [DOI] [PubMed] [Google Scholar]
- Hickson L, Worrall L. Beyond hearing aid fitting: Improving communication for older adults. International Journal of Audiology. 2003;42:S84–S91. [PubMed] [Google Scholar]
- Hickson L, Worrall L, Scarinci N. A randomized controlled trial evaluating the active communication education program for older people with hearing impairment. Ear and Hearing. 2007;28:212–230. doi: 10.1097/AUD.0b013e31803126c8. [DOI] [PubMed] [Google Scholar]
- Hogan A. Hearing rehabilitation for deafened adults: A psychosocial approach. Whurr; London, England: 2001. [DOI] [PubMed] [Google Scholar]
- Kaplan H, Bally S, Brandt F, Busacco D, Pray J. Communication Scale for Older Adults (CSOA) Journal of the American Academy of Audiology. 1997;8:203–217. [PubMed] [Google Scholar]
- Kaplan H, Bally S, Garretson C. Speechreading: A way to improve understanding. Gallaudet University Press; Washington, DC: 1985. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; New York, NY: 1984. [Google Scholar]
- Martelli M, Auerbach S, Alexander J, Mercuri L. Stress management in the health care setting: Matching interventions with patient coping styles. Journal of Consulting and Clinical Psychology. 1987;55:201–207. doi: 10.1037//0022-006x.55.2.201. [DOI] [PubMed] [Google Scholar]
- McArdle R, Chisolm TH, Abrams HB, Wilson RH, Doyle PJ. The WHO-DAS II: Measuring outcomes of hearing aid intervention for adults. Trends in Amplification. 2005;9:127–143. doi: 10.1177/108471380500900304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meline T, Schmitt JF. Case studies for evaluating statistical significance in group designs. American Journal of Speech-Language Pathology. 1997;6(1):33–41. [Google Scholar]
- Newman CW, Weinstein BE, Jacobson GP, Hug GA. The Hearing Handicap Inventory for Adults: Psychometric adequacy and audiometric correlates. Ear and Hearing. 1990;11:430–433. doi: 10.1097/00003446-199012000-00004. [DOI] [PubMed] [Google Scholar]
- Newman CW, Weinstein BE, Jacobson GP, Hug GA. Test-retest reliability of the Hearing Handicap Inventory for Adults. Ear and Hearing. 1991;12:355–357. doi: 10.1097/00003446-199110000-00009. [DOI] [PubMed] [Google Scholar]
- Noble W. What is a psychosocial approach to hearing loss? Scandinavian Audiology Supplement. 1996;43:6–11. [PubMed] [Google Scholar]
- Norman M, George CR, Downie A, Milligan J. Evaluation of a communication course for new hearing aid users. Scandinavian Audiology. 1995;24:63–69. doi: 10.3109/01050399509042212. [DOI] [PubMed] [Google Scholar]
- Preminger JE. Should significant others be encouraged to join adult group audiologic rehabilitation classes? Journal of the American Academy of Audiology. 2003;14:545–555. doi: 10.3766/jaaa.14.10.3. [DOI] [PubMed] [Google Scholar]
- Preminger JE. Issues associated with the measurement of psychosocial benefits of group audiologic rehabilitation programs. Trends in Amplification. 2007;11:113–124. doi: 10.1177/1084713807301084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preminger JE, Ziegler CH. Can auditory and visual speech perception be trained within a group setting? American Journal of Audiology. 2008;17:80–97. doi: 10.1044/1059-0889(2008/009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryden A, Karlsson J, Sullivan M, Torgerson JS. What happens after intervention? A 2-year follow-up from the Swedish Obese Subjects (SOS) study. Psychosomatic Medicine. 2003;65:435–442. doi: 10.1097/01.psy.0000041621.25388.1a. [DOI] [PubMed] [Google Scholar]
- Schow RL, Nerbonne MA. Hearing handicap and Denver Scales: Applications, categories and interpretation. Journal of the Academy of Rehabilitative Audiology. 1980;13:66–77. [Google Scholar]
- Smaldino SE, Smaldino JJ. The influence of aural rehabilitation and cognitive style disclosure of the perception of hearing handicap. Journal of the Academy of Rehabilitative Audiology. 1988;21:49–56. [Google Scholar]
- Stach BA, Spretnjak ML, Jerger J. The prevalence of central presbyacusis in a clinical population. Journal of the American Academy of Audiology. 1990;1:109–115. [PubMed] [Google Scholar]
- Stewart M, Davidson K, Meade D, Hirth A, Weld-Viscount P. Group support for couples coping with a cardiac condition. Journal of Advanced Nursing. 2001;33:190–199. doi: 10.1046/j.1365-2648.2001.01652.x. [DOI] [PubMed] [Google Scholar]
- Suls J, Matin R, Wheeler L. Social comparison: Why, with whom and with what effect? Current Directions in Psychological Science. 2002;11:159–163. [Google Scholar]
- Tye-Murray N. Communication training for older teenagers and adults. Pro-Ed; Austin, TX: 1997. [Google Scholar]
- Ventry IM, Weinstein BE. The Hearing Handicap Inventory for the Elderly: A new tool. Ear and Hearing. 1982;3:128–134. doi: 10.1097/00003446-198205000-00006. [DOI] [PubMed] [Google Scholar]
- Weber BA, Roberts BL, McDougall GJ., Jr. Exploring the efficacy of support groups for men with prostate cancer. Geriatric Nursing. 2000;21:250–253. doi: 10.1067/mgn.2000.110836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein BE, Spitzer JB, Ventry IM. Test-retest reliability of the Hearing Handicap Inventory for the Elderly. Ear and Hearing. 1986;7:295–299. doi: 10.1097/00003446-198610000-00002. [DOI] [PubMed] [Google Scholar]
- Yellin MW, Jerger J, Fifer RC. Norms for disproportionate loss in speech intelligibility. Ear and Hearing. 1989;10:231–234. doi: 10.1097/00003446-198908000-00003. [DOI] [PubMed] [Google Scholar]


