Abstract
Purpose
This study attempted to determine whether auditory-only and auditory-visual speech perception could be trained in a group format.
Method
A randomized controlled trial with at least 16 participants per group was completed. A training-only group completed at least 5 hr of group speech perception training; a training plus psychosocial group completed at least 5 hr of group speech perception training and psychosocial exercises; and a control group did not receive training. Evaluations were conducted before and after training and included analytic and synthetic measures of speech perception, hearing loss–related and generic quality of life scales, and a class evaluation form.
Results
No significant group changes were measured on any of the analytic auditory-only or auditory-visual measures of speech perception, yet the majority of training participants (regardless of training group) reported improvement in auditory and auditory-visual speech perception. The training participants demonstrated a significant reduction on the emotional subscale of the hearing loss–related quality of life scale, while the control participants did not demonstrate a change on this subscale.
Conclusions
Benefits of group audiologic rehabilitation classes may not result from an actual improvement in auditory or visual speech perception abilities, but participants still perceive training in these areas as useful.
Keywords: audiologic rehabilitation, training, auditory-only speech perception, auditory-visual speech perception, hearing loss
Speech understanding is a perceptual ability in which training is expected to result in learning (Watson, 1980). There is evidence that individuals with normal hearing can be trained to discriminate novel speech contrasts (Logan, Lively, & Pisoni, 1993; Tremblay, Kraus, Carrell, & McGee, 1997), individuals with hearing loss can improve word or sentence perception after auditory-only training (Burk, Humes, Amos, & Strauser, 2006; Rubinstein & Boothroyd, 1987; Walden, Erdman, Montgomery, Schwartz, & Prosek, 1981), and individuals with hearing loss can improve word or sentence perception after visual-only speech training (Bernstein, Auer, & Tucker, 2001; Walden et al., 1981). Due to reimbursement issues, audiologists have little financial incentive to offer auditory or visual speech perception training on an individual basis in the clinical setting (Kander & White, 2006). Audiologists who do want to offer these services to their patients with hearing loss can offer them through home-based computer training (Sweetow & Sabes, 2006) or with in-office group training. There is, however, only limited evidence that auditory-only and auditory-visual speech perception can be trained at home via a computer or in a group setting.
Laboratory-Based Individual Training
Speech perceptual training is traditionally performed using analytic materials that focus on individual phonemes (or visemes) in syllables or in words and with synthetic materials that involve the use of sentence or paragraph materials. There is evidence that visual-only speech perception (speechreading) can be trained on an individual basis using either live instruction or computer-based instruction. Walden, Prosek, Montgomery, Scherr, and Jones (1977) demonstrated improved phoneme perception after just a few hours of training using live instruction. Individuals with hearing loss practiced visual-only speech perception with three different instructors during 14 training sessions, each an hour long, over a 2-week period. Participants in the training group demonstrated an increase in the number of visemes that were recognized and an increase in the percentage correct performance for each viseme. Walden et al. tracked the learning curves over the 14 training sessions and found that most learning occurred during the first few hours of training and performance plateaued after 5 or 6 hr of training. Other studies have demonstrated the benefit of visual-only speech training using computer-based instruction (Bernstein et al., 2001; Gagné, Dinon, & Parsons, 1991; Massaro, Cohen, & Gesi, 1993), and research has also demonstrated the benefit of live-voice auditory-visual training (Montgomery, Walden, Schwartz, & Prosek, 1984). There is, however, no optimal training paradigm. Improved visual-only speech perception abilities have been measured following synthetic training for analytic materials (but not for synthetic materials; Bernstein et al., 2001). Conversely, improved visual-only speech perception abilities have been measured following synthetic training for synthetic materials (but not for analytic materials) following analytic training (Gagné et al., 1991). It should be pointed out that in many studies, the measured improvements, whether analytic or synthetic, have been quite small. For example, Bernstein et al. (2001) measured a 2% increase in performance for speechreading phonemes in sentences after 9 training sessions.
A recent systematic review of the literature (Sweetow & Palmer, 2005) concluded that auditory-only speech perception training is efficacious, but there is no agreement on what constitutes the optimal training program. Walden et al. (1981) demonstrated that adults with sensorineural hearing loss who wear hearing aids could be trained to improve their recognition of syllables after a short-term analytic individual training program (7 hr over a 10-day period). Subsequent studies have demonstrated small but significant improvements in synthetic auditory-only speech recognition following synthetic training, with no added benefits from analytic training (Kricos & Holmes, 1996; Rubinstein & Boothroyd, 1987). Most recently, Burk et al. (2006) evaluated the effectiveness of analytic training in a group of adults over the age of 65 with hearing loss who did not wear hearing aids using laboratory-based computer training. Training was conducted in seven 60-min sessions over a 2-week period. The results indicated a clinically small but significant improvement in word recognition as a result of training. There were, however, no measured improvements for the trained words presented in sentences.
Home-Based Computer Training
Two recent studies have demonstrated the potential of home-based auditory-only training using computers (Stecker et al., 2006; Sweetow & Sabes, 2006). Stecker et al. (2006) trained 31 new and experienced hearing aid users using a computer-based program with syllable materials. All participant groups demonstrated significant improvements on a nonsense syllable test throughout the 8-week training period; this improvement was maintained 8 weeks after the training ended. A subgroup of participants was evaluated with sentence materials, but no improvement in performance was measured for these materials. Sweetow and Sabes (2006) measured the effectiveness of an auditory-only, synthetic, home-based computer training program conducted over 20 half-hour-long sessions. Participants demonstrated improved posttraining performance on two out of three clinical tests of sentence understanding in noise as compared with pretraining performance. Participants also demonstrated improved performance on a listening span test and a test of processing speed. These initial results are quite encouraging, and further research will demonstrate the clinical utility of these home-based programs.
Clinic-Based Group Training
Recently, Hawkins (2005) conducted a systematic review to examine the effectiveness of group audiologic rehabilitation programs. Twelve studies were identified that used either a randomized controlled trial, a quasi-experimental, or a nonintervention cohort design. Hawkins concluded that there are short-term psychosocial benefits from adult audiologic rehabilitation groups. A careful review of the methods of these 12 studies reveals that in the majority of studies (7 out of 12), between one quarter and one half of the group class time was devoted to auditory-only, visual-only, and/or auditory-visual speech perception training (Abrams, Chisolm, & McArdle, 2002; Abrams, Hnath-Chisolm, Guerreiro, & Ritterman, 1992; Beynon, Thornton, & Poole, 1997; Brewer, 2001; Chisolm, Abrams, & McArdle, 2004; Norman, George, Downie, & Milligan, 1995; Preminger, 2003; Smaldino & Smaldino, 1988). None of these studies attempted to measure whether training in speech understanding actually resulted in improvements in speech recognition abilities; instead, most of these studies used hearing loss–related or general health–related quality of life scales as outcome measures. For example, in the study conducted by Abrams et al. (1992), approximately one third of the class time was devoted to “speechreading and methods for improving basic communication” (p. 373). Following class participation, the majority of participants demonstrated significant improvements on the Hearing Handicap Inventory for the Elderly (HHIE), a hearing loss–related quality of life scale. Similarly, in the study conducted by Preminger (2003), approximately one third of the class time was devoted to auditory-only and auditory-visual speech perception training in adverse listening conditions. Following class participation, the majority of participants demonstrated significant improvements on the HHIE.
A review of the literature reveals only two studies that attempted to measure whether speech perception could be trained in a group format. Binnie (1977) reported the results of group visual-only speech perception training. A class of 12 listeners with hearing loss received 18 hr of training over a 12-week period; unfortunately, the procedures for training were not described. The results of pre- and postclass testing revealed no improvement in visual-only speech perception as a result of the training. Six participants reported, however, that they were better speechreaders as a result of the class (this was not supported by the testing). In addition, most of the participants reported a strong feeling of support from the group. Scott, Metz, Rohland, and Samar (1989) measured the benefit of visual-only speech perception training in a group of 30 college students with hearing loss enrolled in a speechreading and communication course. Students reported that their visual-only and communication skills improved, but actual visual speech perception abilities were not reported.
Can auditory-only and auditory-visual speech perception be trained in a group setting? There is theoretical evidence which suggests that speech perception can be trained in a group. The review of the literature demonstrates that individualized auditory-only, auditory-visual, and visual-only speech perception training often results in small but significant improvements in speech understanding. It is possible that these findings can generalize to a group setting. In their 2005 systematic review of the auditory training literature, Sweetow and Palmer proposed that successful home-based computer training programs should (a) include analytic and synthetic materials; (b) be easy, fun, and rewarding for patients; (c) be practical and verifiable; and (d) be able to provide feedback to patients. All of these characteristics can easily be applied in a group training model and were applied in the procedures used in the current study. Finally, due to scheduling issues, group training is typically conducted only once or twice per week. Recent research has shown no significant difference in auditory speech performance gains whether auditory training occurred once per week or five times per week (Nogaki, Fu, & Galvin, 2007). On the other hand, there is theoretical evidence that speech perception cannot be trained in group sessions. One of the most compelling arguments is given by Merzenich et al. (1996), who suggest that for perceptual learning to occur, training should occur on a series of successive days, with intense practice and under conditions where the participants are highly motivated (Merzenich et al., 1996). This is difficult to accomplish in a group setting.
Previous research has demonstrated that group audiologic rehabilitation, which frequently includes auditory and visual speech perception training, often results in improvements on hearing loss–related quality of life measures. It has not been demonstrated that group-based speech perceptual training results in improvements in speech recognition, and it has not been demonstrated that improvements on hearing loss–related quality of life scales were a result of training conducted during the group classes. Therefore, it is not clear whether group audiologic rehabilitation class time should be devoted to speech perception training, or if class time would be better spent on other activities. A randomized controlled trial was carried out to determine whether (a) auditory-only speech perception can be successfully trained in a group format, (b) auditory-visual speech perception can be successfully trained in a group format, (c) individuals who participate in auditory-only and auditory-visual speech perception training will report improvements in these abilities, and (d) speech perception training will improve self-perceived quality of life. Three groups of participants were evaluated. Two groups (experimental groups) received analytic and synthetic auditory-only and auditory-visual speech perception training in a group class, while the third group of participants (control group) did not participate in any classes. One experimental group only received training, while the other experimental group received the same training and participated in structured psychosocial exercises. All participants were evaluated with analytic and synthetic auditory-only and auditory-visual speech perception measures, quality of life questionnaires, and a class-specific questionnaire at baseline, at 6 weeks (postclass for experimental participants), and at 6 months.
Method
Participants
Participants were adults with hearing loss between the ages of 55 and 75 years recruited from the Louisville, KY, area. All participants had at least 3 months of hearing aid experience and a score of at least 20 on the HHIE or the Hearing Handicap Inventory for Adults (HHIA; Newman, Weinstein, Jacobson, & Hug, 1990; Ventry & Weinstein, 1982). See Table 1 for a description of the demographic characteristics across the three groups of participants.
Table 1.
Demographic characteristics of participants.
| Factor | Control group | Training and psychosocial group | Training-only group | Statistical difference |
|---|---|---|---|---|
| Number | 16 | 16 | 18 | |
| Age | 66.0 (5.2) | 65.3 (5.4) | 64.9 (6.3) | F(2, 47) = 0.149, p = .86 |
| 3-frequency PTA | 49.8 (9.6) | 54.7 (11.0) | 52.5 (14.3) | F(2, 47) = 0.665, p = .52 |
| Years aided | 9.2 (8.5) | 6.9 (7.6) | 10.2 (6.8) | F(2, 47) = 0.847, p = .44 |
| HHIE/A | 44.0 (15.8) | 49.1 (17.3) | 50.7 (20.9) | F(2, 47) = 0.605, p = .55 |
| Percentage male | 75.0 | 37.5 | 66.7 | χ2(2, N = 50) = 5.21, p = .074 |
Note. Mean values (with standard deviations in parentheses) are shown for age, three-frequency pure-tone average (PTA), years aided, and baseline Hearing Handicap Inventory for the Elderly or Adults (HHIE/A).
All participants were screened to ensure that they met the following criteria: (a) Participants had corrected binocular visual acuity of at least 20/40. This level of acuity is considered the minimum necessary for speechreading training (Hardick, Oyer, & Irion, 1970). (b) Participants had performance within the normal range for age and educational level on the Mini-Mental State Examination (Folstein, Folstein, & McHugh, 1975). (c) Participants passed a screening for auditory processing disorder (APD) using the Synthetic Sentence Identification-Ipsilateral Competing Message test (SSI-ICM) and the Northeastern University Auditory Test No. 6 (NU-6) word list. Participants were considered APD positive if the difference between the NU-6 word score and the SSI-ICM score was greater than 20% (Stach, Spretnjak, & Jerger, 1990) or if the SSI-ICM score was “disproportionately poor”—that is, less than the empirically derived lower boundary of SSI-ICM scores as a function of pure-tone average (Yellin, Jerger, & Fifer, 1989). The SSI-ICM was administered after two practice lists were completed, and then scores were averaged across two lists.
Hearing levels of all participants were monitored during their participation in the study. They were screened at each visit for active middle ear disease using acoustic immittance measures and otoscopy, and pure-tone thresholds. Individuals with fluctuating hearing levels were excluded from the study.
Outcome Measures
Analytic speech perception
Analytic auditory-only and auditory-visual speech perception abilities were measured with the City University of New York (CUNY) AB Isophonemic Word Lists (Boothroyd, 1984; Boothroyd, Hnath-Chisolm, Hanin, & Kishon-Rabin, 1988). The original video recordings had been stored on laser disc and then were converted to .avi (audio visual interleave) files with sampling rates of 44100 Hz for audio and a video resolution of 304 × 228 pixels. Percentage correct scores measured at each session were based on performance for 50 words (five word lists, 150 phonemes), presented in the auditory-only condition and for 50 new words in the auditory-visual condition. One hundred words were selected randomly for presentation at the initial session; because there were only 120 stored words available, the remaining 20 new words were presented at the second test session along with 80 words selected at random that had been presented at the first test session. This same procedure was used at the final test session.
Synthetic speech perception
Synthetic auditory-only and auditory-visual speech perception abilities were measured with the CUNY Topic Related Sentences (Boothroyd et al., 1988). The original video recordings had been stored on laser disc and then were converted to .avi files with sampling rates of 44100 Hz for audio and a video resolution of 304 × 228 pixels. Performance in percentage correct was measured for 48 sentences (four sentence lists, 408 words) presented in the auditory-only condition and for 48 new sentences in the auditory-visual condition at each test session. Eight lists were selected randomly for presentation at the first test session, eight new lists were selected randomly for presentation at the second test session, and the remaining two lists were presented at the final session along with six repeated lists selected randomly. Participants were not provided with the topic prior to the administration of each sentence.
Quality of life
Hearing loss–related quality of life was measured with the HHIE scale for individuals 65 and older and with the HHIA for those under 65 (Newman et al., 1990; Ventry & Weinstein, 1982). These are 25-item scales with two subscales: social function and emotional function (as it relates to hearing loss).
Generic quality of life was measured with the World Health Organization Disability Assessment Schedule II (WHODAS II). This is a comprehensive quality of life scale that is based on the WHO’s International Classification of Functioning, Disability and Health. It contains 36 items and six subscales: Communication, Mobility, Self-Care, Interpersonal, Life Activities, and Participation. The WHODAS II has been shown to have adequate psychometric characteristics for a group of individuals with adult onset hearing loss (Chisolm, Abrams, McArdle, Wilson, & Doyle, 2005). In addition, group scores on the WHODAS II demonstrated small but significant improvements in generic quality of life following hearing aid fitting (McArdle, Chisolm, Abrams, Wilson, & Doyle, 2005).
Class evaluation form
A subjective class evaluation form was completed by all participants who completed the classes. The purpose of this form was to measure the perceived benefit of the training and the psychosocial exercises received in the classes. A copy of the class evaluation is shown in the Appendix.
Audiologic Rehabilitation Classes
Because one purpose of this project was to determine whether speech perception could be trained in a group class in a typical audiology clinic setting, all classes were held in conference rooms located in three different audiology clinical practices throughout the Louisville area. As a result, listening and viewing conditions were controlled as much as these various room configurations would allow. Participants were seated around a conference table with the instructors at the head of the table. All training was initially presented in noise, which was presented from a CD player located near the instructor. Performance of each class member was constantly monitored. If necessary, participants were moved either closer to the instructor or closer to the noise, in order to achieve the desired level of performance.
Auditory-only and auditory-visual speech perception training
Speech perceptual abilities were taught in an auditory-visual and an auditory-only format using at least two instructors per class. Analytic materials were same/ different tasks and syllable drills adapted from Tye-Murray (1997). Each class focused on a new group of three phonemes. The first three classes focused on phoneme groups that were expected to be easier to discriminate (e.g., /b/, /d/, and /g/), while the last three classes focused on phoneme groups that were expected to be more difficult to discriminate (e.g., /d/, /t/ and /sh/). All exercises were conducted in noise: a multitalker (20-talker) babble. In the same/different task, the instructor presented two CV syllables (e.g., /ba/, /ba/), and all class participants had to mark same or different on an answer sheet. Immediate feedback was given after every stimulus presentation; syllables were presented with visual cues in quiet, and each participant marked his or her responses as correct or incorrect. Following the presentation of each stimulus set (10 syllable pairs), answer sheets were graded and individual placements (in relation to the instructors and the babble generated by the CD player) were adjusted in the classroom so that each participant attained scores of approximately 70% correct for auditory-only exercises. Presentation alternated between auditory-visual and auditory-only, 10 syllable pairs in each condition. In comparison with the auditory-only condition, noise levels were raised for the auditory-visual exercises in order to keep performance at approximately 70% correct. With this method, audibility of individual phonemes could not be ensured; however, visual cues could be made available when audibility was not achieved. In the phoneme identification task, the instructor presented a single CV from among a closed set of three possible CVs. Following each presentation in noise, syllables were presented in quiet, and individual performance was monitored using individual answer sheets in order to maintain performance of approximately 70% correct. Same/ different exercises and the identification exercises proceeded from easier vowels contexts (e.g., /a/) to more difficult vowel contexts (e.g., /u/; Erber, 1971) during each class session. All classes were led by at least two instructors who alternated leading the exercises. It was expected that the use of multiple talkers would aid in the generalization of training to novel talkers (Lively, Pisoni, Yamada, Tohkura, & Yamada, 1994).
Synthetic exercises were sentence length and paragraph materials adapted from Kaplan, Bally, and Garretson (1985). For the majority of exercises, the instructor introduced a topic and then presented sentences or a paragraph related to the topic. Participants took turns either answering questions about the paragraph or repeating the sentences. Immediate feedback was always presented; stimuli were presented repeatedly with decreased noise levels and/or with visual cues available until each participant could complete the task correctly. During these training sessions, individuals were encouraged to use contextual knowledge and active listening skills as described by Rubinstein and Boothroyd (1987). These exercises were conducted in the same noise levels used for the analytic exercises.
In order to keep participants motivated, class period instruction alternated between analytic exercises for 10 min and synthetic exercises for 10 min over a period of 1 hr. Instructors and activities changed frequently. The synthetic exercises included quizzes, jokes, and short stories to keep participants engaged.
Psychosocial exercises
Hogan (2001) developed psychosocial exercises for individuals with hearing loss based on the premise that individuals who acquire hearing loss need to recognize their problems before they will begin to try and fix these problems. Exercises were adapted from Hogan, and new exercises were developed in which participants were able to discuss (a) the problems, feelings, attitudes, and emotions associated with hearing loss; (b) other people’s reactions to their hearing loss; and (c) the impact of hearing loss on personal and professional relationships. For most exercises, students were given a written scenario, for example, a scenario in which a husband who has a hearing loss cannot understand his wife’s speech when he is washing the dishes and she is trying to have a discussion. The instructors used a list of predetermined questions and prompts in order to lead a structured discussion about this scenario.
Procedures
Participants were randomly assigned to one of three groups: (a) a control group, (b) a speech perception training (auditory-only and auditory-visual) group (Train Only), and (c) a speech perception training (auditory-only and auditory-visual) plus psychosocial exercise group (Train + PS). Most classes were led by the first author along with two students in the doctor of audiology program at the University of Louisville. Students only led classes on their own after completing a full-session of six classes with the first author. Even after students received extensive training, the first author was present for at least 50% of all classes. All audiologic rehabilitation classes met once per week over a 6-week period. At least 1 hr was spent each week on the auditory and visual speech perception exercises in both training groups; an additional 30 min was spent each week on the psychosocial exercises in the Train + PS group classes. All experimental participants completed at least five of the six classes. As a result, all experimental participants completed at least 5 hr of speech perception training, but the majority of participants (71%) completed 6 hr of training.
Prior to testing, hearing aids were evaluated in a test box and hearing aid gain was measured for a 60-dB SPL input. These results were recorded and stored to ensure that the hearing aid performed in a consistent manner for all future testing. The analytic and synthetic speech evaluations were conducted individually in the sound field in an audiometric test booth while each individual wore his or her hearing aid(s) at user gain. All testing was conducted in the presence of speech-shaped noise generated by an audiometer (Grason-Stadler GSI 61) presented at a 180° azimuth 1 m from the listener’s head. The word and sentence files were stored in a digital format, routed through a programmable attenuator (TDT PA5) to the audiometer, and then presented through a loudspeaker located 1 m from the listener’s head at 0° and a 10 in. × 13 in. monitor located 0.5 m from the listener’s head at 15° azimuth. When the .avi files were presented in the auditory-visual format, the talker’s face was contained in a 4 in. × 5 in. rectangle.
All testing began using two lists of the AB words in order to set the signal-to-noise ratio (SNR) for auditory-visual speech perception. The speech-shaped noise was fixed at 50 dBA located at the position of the participant’s head. With both the auditory and the visual signal available, the level of the speech signal was varied using a simple up-down technique (Levitt, 1971). After the initial four reversals, the step size was reduced to 2 dB and the 50% point was estimated based on the average of the final 16 reversals; this SNR was maintained for the next step. The visual signal was eliminated, and the participant completed five practice words in an auditory-only format. If necessary, the signal was raised using a 2-dB step size until performance exceeded 30% correct for all phonemes in the auditory-only format. This SNR was used for all subsequent AB word testing (both auditory-only and auditory-visual). By beginning near the 50% level for auditory-visual performance, ceiling and floor effects were avoided. Percentage correct performance was measured for 50 words in the auditory-only condition and then 50 new words in the auditory-visual condition.
The SNR had to be adjusted for the synthetic testing (CUNY sentences) in order to avoid ceiling effects. Using 5 or 10 practice sentences, the SNR that had been used for the AB words was adjusted until the participants could repeat approximately 50% of the words in the auditory-only condition. This SNR was used for all subsequent CUNY sentence testing (both auditory-only and auditory-visual). Percentage correct performance was measured for 48 sentences in the auditory-only condition and then 48 new sentences in the auditory-visual condition.
All questionnaires (HHIE/A, WHODAS II, and the class evaluation) were administered in a paper-and-pencil format. The examiner read over the instructions with the participant, and then the participant completed the scale. The examiner was available to answer any questions and ensured that all questions were answered.
Participants assigned to rehabilitation classes were evaluated within a 2-week time period prior to the first class. The evaluation included the quality of life scales and the speech perception measures. Participants were evaluated again over a 2-week time interval immediately after the completion of the course; this evaluation was the same as the preclass evaluation and included the class evaluation form (see Appendix). Finally the evaluation battery was completed a third time, 6 months after the classes were completed. The control participants also were evaluated three times with the entire test battery, except for the class evaluation form. The first two evaluations were separated by 6 weeks, and the final two evaluations were separated by 6 months.
Participants’ hearing aids were evaluated at each visit and adjusted as needed to ensure consistent root-mean-square gain. Participants’ air-conduction thresholds were measured at each evaluation. If the three-frequency pure-tone average in the better ear varied by more than 5 dB from the preclass visit to any of the subsequent visits, then the hearing aid gain was adjusted so that the speech and noise signals were perceived at the same sensation level as at the initial visit.
Data Analyses
In a randomized controlled trial, it is typical to measure the effectiveness of a new treatment in comparison with an existing treatment using an equivalence trial (Piantadosi, 1997).1 In equivalence trials, the null hypothesis is that the interventions are different, and the alternative hypothesis is that they are the same (Friedman, Furberg, & Demets, 1998). This is the converse of traditional hypothesis testing, where the null states no difference is found between interventions or therapies. In the present study, we evaluated a typically used treatment, group training of speech perception abilities, but there was no standard of care treatment available for comparison. Therefore, we compared performance for all participant groups to a clinically significant improvement in speech perception abilities. It was hypothesized that short-term training would not result in a clinical improvement in auditory-only or auditory-visual perceptual abilities as measured by tests of speech perception. A clinical improvement over the initial test score was considered to be greater than the 95% critical difference. For the word tests, the critical difference was based on the number of words evaluated (50) and the mean score at the initial visit using the binomial method described by Thornton and Raffin (1978). For the sentence test, the binomial method was modified as described by Boothroyd et al. (1988) so that critical differences were based on 192 words (48 phrases, each of 4 words), rather than 408 words.
The classic confidence interval paired t test for equivalence of means (Schuirmann, 1987) was used to test the null hypothesis that the correct change percentage going from the baseline to the 6-week retest would be equal to or greater than the clinically determined equivalence limit. The alternative hypothesis for this equivalence study is that any change going from the pretraining to posttraining measurement will be less than the clinically determined equivalence limit. Thus,
where μpre = preclass percentage correct, μpost = postclass percentage correct, and tn–1,1–αSE = the upper confidence limit. The analyses were conducted for the auditory-only results (three separate analyses: phonemes in AB words, AB words, words in CUNY sentences), and for auditory-visual results (three separate analyses: phonemes in AB words, AB words, words in CUNY sentences). A one-tailed test was used because only an improvement in performance would be expected if training was effective; it was not expected that scores would actually decrease as a result of training (or as a result of no training in the control participants). An a priori power analysis and sample size estimate were performed, and it was determined that a sample size of 16 per instructional group would give over the standard 80% power with a one-sided alpha of .05. This was based on a critical difference of 20% for 50 word lists and a pretraining score of 50% correct (Thornton & Raffin, 1978). While actual pretraining scores varied according to participant and according to test condition (auditory-only versus auditory-visual), a pretest score of 50% was targeted for the auditory-visual condition across all participants.
To assess whether group training enhanced hearing loss–related quality of life, a 3 × 3 mixed randomized/repeated measures analysis of variance (ANOVA) was used to analyze the effects of the three participant groups across the time of baseline (preclass), 6 weeks (postclass), and 6 months postclass periods. Separate ANOVAs were conducted for the hearing loss–related quality of life scale (three separate analyses from the HHIE/A: total, Emotional subscale, and Social subscale) and for the generic quality of life scale (five separate analyses from the WHODAS II: total, Understanding and Communicating subscale, Getting Along With People subscale, Life Activities subscale, and Performance in Society subscale). In each analysis, there was one between-group factor (participant type: control, Train + PS, Train Only), and there was one within-group factor (time: baseline, 6 weeks, 6 months). Accordingly, group, time, and Group × Time interaction effects were tested. SAS Proc Mixed was used to perform these analyses.
The Mann–Whitney U nonparametric test was performed on the class evaluation to test whether the response distributions of these Likert scaled items were comparable across the two treatment groups. Statements 1, 2, and 3 centered around self-perceived improvement in auditory and visual speech understanding (see Appendix). Since both treatment groups received training in these areas, two-tailed tests were performed. Statements 4, 5, and 6 were about the benefits of the structured psychosocial exercises. Since only one treatment group received treatment in this area, it was hypothesized that this group would agree with these statements more strongly than the other group; thus, a directional one-tailed test was used.
Results
Participant Characteristics
Fifty individuals with at least 3 months of hearing aid experience participated in the study. More than 16 participants were in the Train Only group because more than the minimum number of participants required were enrolled in each treatment group in case any participants did not complete the minimum number of required classes. Individual ANOVAs were performed to determine whether there were any differences in demographic characteristics across groups. Mean age, average hearing loss, number of years aided, baseline HHIE/A scores, and the results of the ANOVAs are shown in Table 1. The gender distribution across each group was evaluated with a chi-square analysis. There were no significant differences in these demographic characteristics across the three participant groups.
Three participants (not included in the 50 individuals shown in Table 1 or any of the statistical analyses) did drop out of the treatment groups. One individual completed a subsequent rehabilitation class in a different research study; the other two individuals did not complete the classes or the postclass evaluations. The two permanent dropouts were both female. One of these individuals was 70 years old, had a preclass HHIE score of 74 and a pure-tone average of 52 in the better ear, and had worn hearing aids for 2½ years. The other individual was 68 years old, had a preclass HHIE of 42 and a pure-tone average of 25 in her better ear, and had worn hearing aids for 4 years.
Two individuals completed both the baseline and the 6-week evaluation but did not complete the 6-month evaluation; one of these individuals was in the Train Only group, and the other was in the Train + PS group. One of these individuals passed away, and the other could not be reached for the final evaluation. SAS Proc Mixed is designed to handle missing data cases such as these. Proc Mixed uses full information maximum likelihood estimates to analyze all the data that are present. In effect, this technique does not delete missing data and is a more efficient and less biased technique than listwise deletion, pairwise deletion, and mean-imputation methods of handling missing data (Wothke, 1998).
Speech Perception Results
Auditory-only performance
At the baseline test (preclass), the average auditory-only performance for phonemes in words was approximately 40% correct across all participant groups. Table 2 shows the percentage correct scores for auditory-alone performance for phonemes in words, words in isolation, and words in sentences. These data demonstrate no apparent change in performance as a function of time for phonemes in words or for words in isolation.
Table 2.
Equivalency findings for auditory-alone performance.
| Baseline | 6-week | 6-month | Difference (SE ) | Upper confidence limit | Clinical critical difference | Clinical equivalence? | |
|---|---|---|---|---|---|---|---|
| Phonemes in AB words | |||||||
| Control | 40.75 | 39.44 | 38.38 | −1.31 (1.86) | 1.95 | 13.0 | Yes |
| Train + PS | 40.63 | 40.81 | 41.67 | 0.19 (3.11) | 5.63 | 13.0 | Yes |
| Train only | 38.72 | 41.00 | 36.93 | 2.28 (3.35) | 8.10 | 13.0 | Yes |
| AB words | |||||||
| Control | 18.13 | 16.63 | 14.25 | −1.5 (1.77) | 1.6 | 16.0 | Yes |
| Train + PS | 16.56 | 16.25 | 18.14 | −0.31 (3.36) | 5.58 | 16.0 | Yes |
| Train only | 16.78 | 16.78 | 14.20 | 0.00 (3.36) | 5.85 | 16.0 | Yes |
| Words in CUNY sentences | |||||||
| Control | 51.94 | 54.56 | 55.19 | 2.63 (3.84) | 9.35 | 9.6 | Yes |
| Train + PS | 52.19 | 53.75 | 54.93 | 1.56 (3.84) | 9.91 | 9.6 | No |
| Train only | 57.00 | 58.5 | 57.65 | 1.5 (5.86) | 11.69 | 9.6 | No |
Note. Columns display the mean baseline (preclass) performance, the mean 6-week evaluation (postclass) performance, the mean 6-month performance, the mean difference between the baseline and 6-week performance (with the standard error in parentheses), the upper level of the confidence interval measured around the difference score, and the upper level of the confidence interval that must be exceeded in order to demonstrate a true clinical improvement. If the measured upper level of the confidence limit was less than the required clinical critical difference, this indicates that there was no clinically significant change in performance, and this is indicated by a “yes” in the rightmost column. Control = control participants; Train + PS = participants who received training plus psychosocial exercises; Train only = participants who received only training; CUNY = City University of New York.
All speech perception performance was evaluated using an equivalence trial paradigm in which the difference scores between the baseline and the 6-week evaluations were compared with a predetermined critical difference level.2 If the difference score (see Table 2) was less than or equal to the critical difference level, there was no true clinical improvement in performance at the 6-week visit in comparison with the baseline visit. This suggests that the two scores are clinically equivalent (shown by a “yes” in the rightmost column of Table 2); in other words, the training did not improve performance. If performance at the 6-week evaluation was significantly better than the performance at the baseline, this would be indicated by a no; in other words, the training did improve performance.
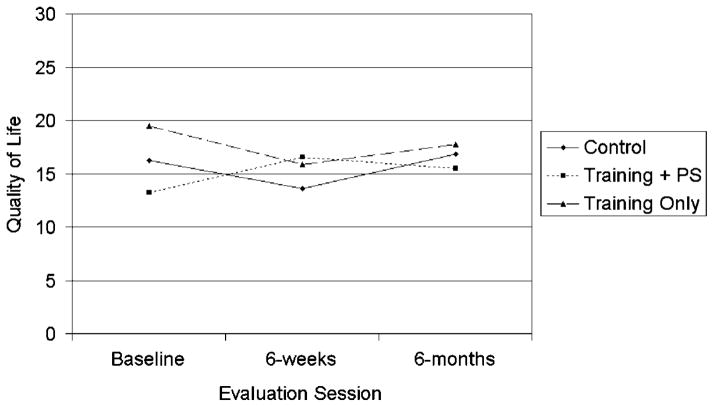
Examination of Table 2 reveals that the upper confidence limit of the difference scores for the auditory-only tasks did not exceed the clinically determined critical differences for phonemes in AB words or for AB words alone. Thus, the group training did not result in significantly improved auditory perceptual abilities for the analytic measure, and equivalence was established. For the auditory-alone synthetic test, words in CUNY sentences, equivalency was established for the control group but not for the two treatment groups. These results are shown in Figure 1. The results of the equivalence analysis suggest that there was a significant mean improvement in performance for the two training groups but not for the control group; this finding is not apparent in Figure 1. There are only slight improvements in performance between the baseline evaluation and the 6-week evaluation for the two training groups. Error bars are not shown in the figures to improve their visibility; however, the standard errors are reported in Table 2. The clinical inequivalence demonstrated by the two training groups may be due to variability in the test measure rather than to true clinical improvements.
Figure 1.
Average auditory-only performance for words in sentences, for each participant group, before training (baseline), after training (6 weeks), and 6 months after training. Performance for the control group is shown with the solid line, for the training plus psychosocial group with the dotted line, and for the training-only group with the dashed line.
Auditory-visual performance
Because auditory-visual performance is influenced by auditory-only ability, visual enhancement rather than actual auditory-visual performance was the metric used in all analyses. Visual enhancement was calculated using the following equation:
where VE = visual enhancement, AV is the auditory-visual performance, and A is the auditory-only performance. This formula takes into account the fact that better auditory-only performance results in less potential for auditory-visual benefit (Grant & Seitz, 1998; Grant, Walden, & Seitz, 1998; Sommers, Tye-Murray, & Spehar, 2005).
The equivalence findings shown in Table 3 demonstrate no improvement in visual enhancement as a function of time for any participant groups for the analytic measures. The null hypothesis of inequivalence could not be rejected for each of the two training groups for visual enhancement of words in sentences. Examination of the mean data across the three participant groups reveals a mean decline in performance from baseline to the 6-week visit for the control group and the Train + PS group. The Train Only group did show a small mean improvement at the 6-week visit, but this was not maintained at the 6-month visit. These findings suggest that the clinical inequivalence demonstrated by the two training groups may be due to variability in the sentence recognition task rather than to true clinical improvement.
Table 3.
Equivalency findings for visual enhancement performance.
| Baseline | 6-week | 6-month | Difference (SE) | Upper confidence limit | Clinical critical difference | Clinical equivalence? | |
|---|---|---|---|---|---|---|---|
| Phonemes in AB words | |||||||
| Control | 52.71 | 56.32 | 56.77 | 3.61 (2.52) | 8.03 | 13.0 | Yes |
| Train + PS | 57.09 | 56.93 | 58.48 | −0.16 (3.12) | 5.33 | 13.0 | Yes |
| Train only | 55.41 | 57.83 | 55.76 | 2.42 (4.26) | 9.83 | 13.0 | Yes |
| AB words | |||||||
| Control | 40.18 | 41.26 | 43.47 | 1.08 (3.02) | 6.37 | 18.0 | Yes |
| Train + PS | 43.65 | 42.81 | 44.86 | −0.84 (3.50) | 5.29 | 18.0 | Yes |
| Train only | 42.32 | 45.65 | 43.46 | 3.33 (3.98) | 10.24 | 18.0 | Yes |
| Words in CUNY sentences | |||||||
| Control | 35.64 | 29.69 | 41.39 | −5.95 (8.52) | 8.99 | 9.8 | Yes |
| Train + PS | 41.17 | 35.54 | 48.28 | −5.63 (9.42) | 10.88 | 9.6 | No |
| Train only | 48.67 | 52.20 | 45.05 | 3.59 (4.47) | 11.30 | 9.7 | No |
Note. Columns display the mean baseline (preclass) performance, the mean 6-week evaluation (postclass) performance, the mean 6-month performance, the mean difference between the baseline and 6-week performance (with the standard error in parentheses), the upper level of the confidence interval measured around the difference score, and the upper level of the confidence interval that must be exceeded in order to demonstrate a true clinical improvement. If the measured upper level of the confidence limit was less than the required clinical critical difference, this indicates that there was no clinically significant change in performance, and this is indicated by a “yes” in the rightmost column.
Perceived benefit
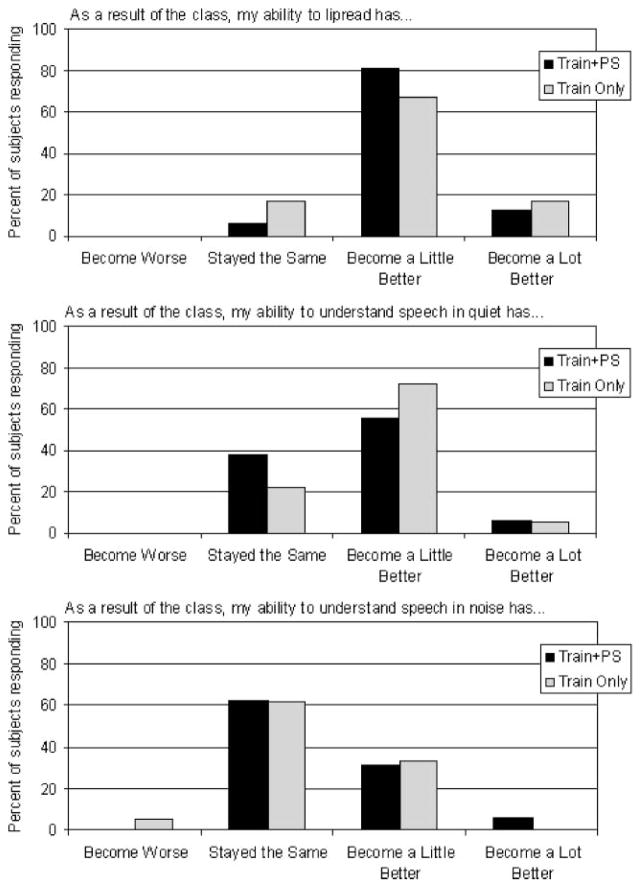
All participants in the Train Only group and the Train + PS group completed a questionnaire after the completion of the class. The first three statements determined whether participants noticed any improvement in “lipreading,” speech understanding in quiet, or speech understanding in noise as a result of class participation. (While we trained auditory-visual speech perception, the participants considered this skill to be lipreading.) The ratings for these statements across the two treatment groups are shown in Figure 2. As can be seen in the figure, the majority of participants in each group reported at least some improvement in lipreading as a result of class participation (Train + PS: 94%, Train Only: 83%). Fewer participants in each group reported an improvement in speech understanding in quiet (Train + PS: 63%, Train Only: 78%), and even fewer participants in each group reported an improvement in speech understanding in noise (Train + PS: 38%, Train Only: 33%). It is interesting to note that more than half of the participants in each group reported improvements in visual-only and in auditory-only speech perception, but these gains were not measured by objective tests of auditory-only performance and visual enhancement (see Tables 2 and 3). There did not appear to be a difference in self-perceived benefit as a result of class type; participants in the Train + PS group did not report greater lipreading or auditory speech perception improvements than participants in the Train Only group. This was confirmed with a Mann-Whitney U test in which the distribution of responses was compared between each of the training groups. Using a two-tailed test, the significance levels were p = .485 for the top graph in Figure 2, p = .461 for the middle graph, and p = .593 for the bottom graph.
Figure 2.
Percentage of participants responding to Statements 1–3 from the class evaluation form. The top panel shows responses to the statement “As a result of the class, my ability to lipread has…"; the middle panel shows responses to the statement “As a result of the class, my ability to understand speech in quiet has…”; and the bottom panel shows responses to the statement “As a result of the class, my ability to understand speech in noise has….” The solid bars show responses for the training plus psychosocial group, and the shaded bars show responses for the training-only group.
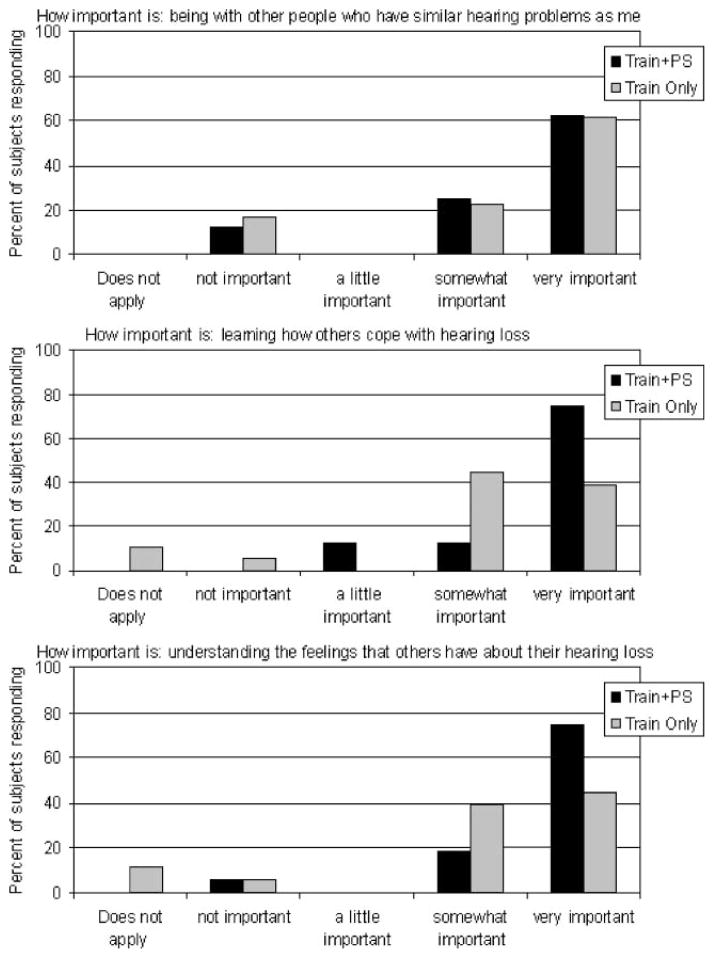
Additional questionnaire items were evaluated to determine whether participants in the Train + PS group reported greater feelings of support as compared with the Train Only group; results are shown in Figure 3. There appeared to be no difference across the two participant groups in the percentage responding to the statement regarding the importance of “being with other people who have similar hearing problems as me.” There was no significant difference in the response distributions across the two training groups (p = .493). There were differences, however, in how participants rated the remaining statements (the middle and bottom graphs in Figure 3). More participants in the Train + PS group (75%) rated the importance of learning how others cope with hearing loss as very important than did the participants in the Train Only group (39%; p = .026). In addition, more participants in the Train + PS group (75%) rated the importance of understanding the feelings that others have about their hearing loss as very important than did participants in the Train Only group (44%; p = .040).
Figure 3.
Percentage of participants responding to Statements 4– 6 from the class evaluation form. The top panel shows responses to the question regarding the importance of “being with other people who have similar hearing problems as me”; the middle panel shows responses to the question regarding the importance of “learning how others cope with hearing loss”; and the bottom panel shows responses to the question regarding the importance of “understanding the feelings that others have about their hearing loss.” The solid bars show responses for the training plus psychosocial group, and the shaded bars show responses for the training-only group.
There was concern that the differences in responses for the statements shown in Figure 3 were due to gender differences across the two training groups rather than to differences in class content. This gender difference was not significant (see Table 1), yet the Train + PS group was 62.5% female while the Train Only group was 33% female. The results for the middle and bottom statements shown in Figure 3 were analyzed separately for men and for women, and the results are shown in Figure 4. The top graphs in Figure 4 correspond to the middle graph in Figure 3. There was a significant difference in the responses of women to the question that rated the importance of “learning how others cope with hearing loss.” Most women in the Train + PS group rated this as very important (90%), in comparison with 17% in the Train Only group (p = .006). For men, 50% in the Train + PS group and 54% in the Train Only group rated this as being very important (p = .955). This finding suggests that women benefited from the psychosocial exercises in the Train + PS group while the men did not. It is important to remember that this finding is based on only 14 female participants and 18 male participants.
Figure 4.
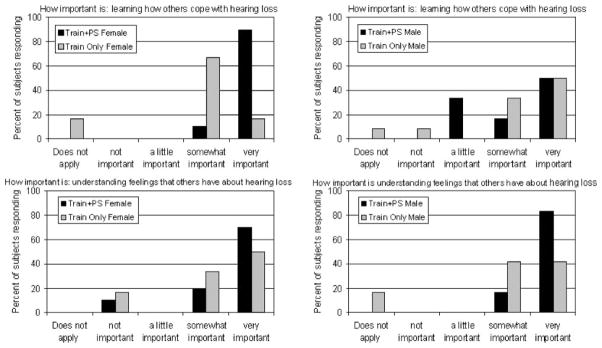
Percentage of participants responding to two class evaluation statements as a function of gender and class type. The top panel shows responses to the question regarding the importance of “learning how others cope with hearing loss,” and the bottom panel shows responses to the question regarding the importance of “understanding the feelings that others have about their hearing loss.” The solid bars show responses for the training plus psychosocial group, and the shaded bars show responses for the training-only group. Results for female participants are shown in the graphs on the left, and results for male respondents are shown in the graphs on the right.
The results for the statement rating the importance of “understanding the feelings that others have about their hearing loss” are shown in the bottom of Figure 4. Although statistical significance was not detected between training groups for each gender, 83% of males in the Train + PS group rated this as being very important, while only 42% of Train Only males rated it highly. Analogously, 70% of females in the Train + PS group rated this statement as being very important, while only 50% of those in the Train Only group rated it highly. This implies that gender is not confounding the difference detected among the two training groups for this statement, and the actual nonsignificant results may be an artifact of lower power due to reducing the sample size by splitting the analysis into two groups.
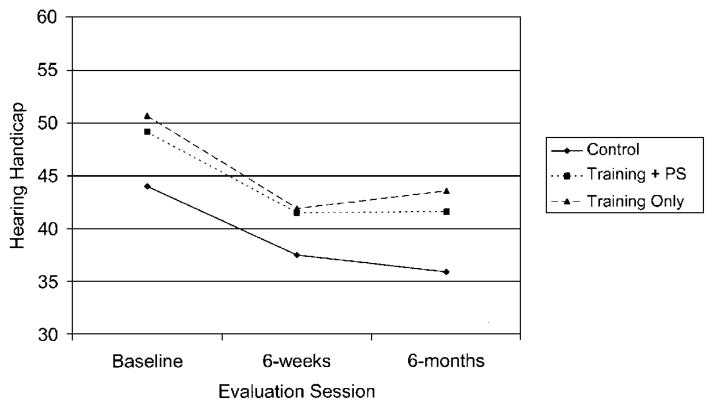
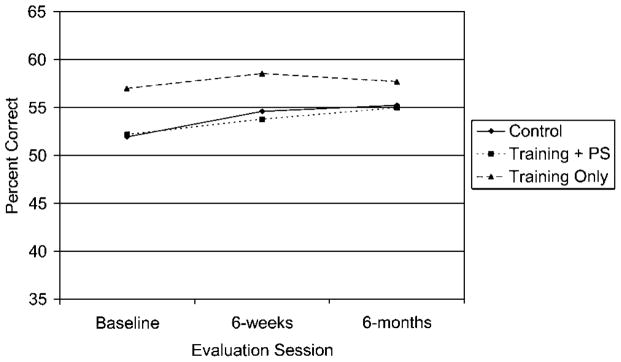
Quality of life
Disease-specific (hearing loss) quality of life was measured with the HHIE/A, which measures hearing loss–related participation restrictions and activity limitations, referred to here as “hearing handicap.” Figure 5 shows the average HHIE/A scores for each participant group at each test time. At the baseline evaluation, the average HHIE/A scores were approximately 48 across all participants. Figure 5 shows an improvement in hearing handicap at the postclass time interval that was maintained at the 6-month evaluation. This was confirmed by a repeated measures ANOVA (see Table 4). The results of the ANOVA showed an overall significant effect for time, F(2, 102) = 12.46, p = .0001. Follow-up testing showed a significant difference in HHIE/A scores between the baseline and 6-week testing times ( p < .0001) and between the baseline and the 6-month testing times ( p = .0005), but not between the 6-week and 6-month testing times ( p = .9284). There was no Time × Participant group interaction, indicating that all three groups showed a significant reduction in hearing handicap at the postclass evaluations, even the control group whose members did not participate in any classes or receive any training. Because the control group showed the significant reduction in hearing handicap along with the two treatment groups, the significant reduction in hearing handicap cannot be attributed to the training and/or the psychosocial support from the group classes.
Figure 5.
Average Hearing Handicap Inventory for the Elderly or Adults (HHIE/A) total score for each participant group before training (baseline), after training (6 weeks), and 6 months after training. Performance for the control group is shown with the solid line, for the training plus psychosocial group with the dotted line, and for the training-only group with the dashed line. A lower score indicates less hearing handicap.
Table 4.
Mean quality of life scores for each treatment group at each testing session.
| Scale and subscales | Control
|
Train + PS
|
Training-only
|
P values
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preclass | Postclass | 6-months | Preclass | Postclass | 6-months | Preclass | Postclass | 6-months | Group | Time | Group × Time | |
| HHIE/A | ||||||||||||
| Total | 44.00 | 37.50 | 35.88 | 49.13 | 41.50 | 41.59 | 50.67 | 41.89 | 43.54 | .594 | <.001** | .932 |
| Social | 23.13 | 19.00 | 18.50 | 24.50 | 21.25 | 21.49 | 26.44 | 22.11 | 22.73 | .511 | <.001** | .942 |
| Emotional | 20.63 | 18.50 | 17.38 | 24.63 | 20.25 | 20.12 | 24.22 | 19.78 | 20.89 | .660 | .012** | .875 |
| WHODAS II | ||||||||||||
| Total | 16.26 | 13.60 | 16.87 | 13.21 | 16.53 | 15.47 | 19.48 | 15.90 | 17.71 | .779 | .498 | .116 |
| UC | 16.87 | 16.25 | 19.30 | 15.63 | 20.00 | 17.73 | 22.22 | 24.72 | 20.45 | .439 | .394 | .301 |
| GAWP | 13.54 | 13.54 | 15.62 | 10.42 | 10.42 | 8.79 | 24.54 | 18.52 | 15.45 | .126 | .396 | .288 |
| LA | 22.50 | 16.38 | 16.79 | 22.50 | 26.88 | 27.07 | 23.33 | 16.11 | 26.27 | .622 | .163 | .040** |
| PIS | 21.87 | 14.06 | 21.35 | 15.10 | 18.23 | 14.49 | 22.69 | 15.97 | 20.82 | .684 | .111 | .075* |
Note. The rightmost columns show the significance levels from the repeated measures analysis of variance for group and time and the Group × Time interaction. WHODAS II = World Health Organization Disability Assessment Schedule II; UC = Understanding and Communicating; GAWP = Getting Along With People; LA = Life Activities; PIS = Performance in Society.
= significant at the .05 level.
= significant at the .1 level.
Because a significant time effect was measured for the total HHIE/A scores, the results for each of the subscales (Social and Emotional) were evaluated. The results for the Social subscale were the same as for the total score (see Table 4); all three groups (including the control group) demonstrated a significant reduction in handicap from the pre-class to the postclass testing evaluations. This reduction in hearing handicap was retained at the 6-month testing time. The results for the Emotional subscale are shown in Figure 6. While a significant overall time effect was measured (p = .003), the slope of the time effect is noticeably shallower for the control group as compared with the two treatment groups. Follow-up testing demonstrated a significant effect between baseline and 6-weeks results for the Train + PS group (p = .033) and for the Train Only group (p = .0042); this effect was not significant for the control group (p = .32). Participants in the control group had noticeably lower baseline scores on the Emotional subscale, but these baseline scores were not significantly different across participant groups (see Table 1). In addition, each had an initial HHIE/A score of at least 20; each individual had the potential to demonstrate a clinically significant decrease in hearing handicap.
Figure 6.
Average HHIE/A score for the Emotional subscale for each participant group before training (baseline), after training (6 weeks), and 6 months after training. Performance for the control group is shown with the solid line, for the training plus psychosocial group with the dotted line, and for the training-only group with the dashed line. A lower score indicates less hearing handicap.
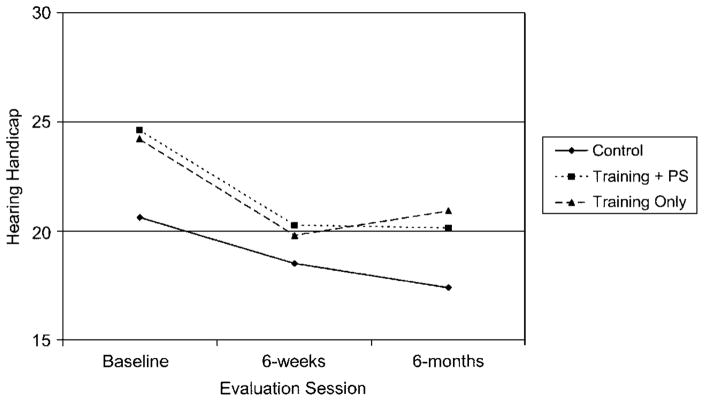
Generic quality of life was measured with the WHODAS II; the results for the total scale are shown in Figure 7. Unlike the HHIE/A, improved quality of life on the WHODAS II is indicated with a higher score. Relatively stable results are shown across all three groups over test time; this was confirmed with the ANOVA (see Table 4). There were no significant effects for group, for time, or for a Group × Time interaction. Previous research has shown that the WHODAS II Communication and Participation subscales were sensitive to hearing aid fittings (McArdle et al., 2005). Interestingly, both treatment groups demonstrate a slight improvement on the Understanding and Communicating subscale, from preclass to postclass, that was not shown by the control group (see Table 4). These changes were not significant, however, and they were not retained at the 6-month visit. There was only one significant finding for a WHODAS II subscale. The Group × Time interaction was significant for the Life Activities subscale, F(4, 91) = 2.62, p = .0401. Follow-up testing revealed a significant drop in quality of life for the Train Only group (p = .02) going from baseline to 6 weeks, and an improvement from 6 weeks to 6 months (p = .051). The control group also demonstrated a drop in quality of life for Life Activities that approached significance (p = .06), going from the baseline to the 6-week evaluation. These results are unexpected and may in fact be unrelated to the treatment (or lack of treatment) received in the current experiment.
Figure 7.
Average World Health Organization Disability Assessment Schedule II (WHODAS II) total score for each participant group before training (baseline), after training (6 weeks), and 6 months after training. Performance for the control group is shown with the solid line, for the training plus psychosocial group with the dotted line, and for the training-only group with the dashed line. A higher score indicates improved quality of life.
Discussion
Auditory-Only and Auditory-Visual Training
The results revealed that analytic speech perception skills could not be trained in a group format after at least 5 hr of training offered one time per week. This lack of improvement may be due to the frequency and intensity of the training and/or to the inability to personalize the training. Recent research by Nogaki et al. (2007) demonstrated improved auditory perception of spectrally shifted compressed speech in normal hearing participants trained one time per week, three times per week, and five times per week. While there was no statistical difference in overall improvement between the three treatment groups, the figures did suggest greatest improvement for the individuals trained five times per week. Most studies that have reported successful training of speech perception have included many training sessions over a short period of time (Bernstein et al., 2001; Logan et al., 1993; Massaro et al., 1993; Walden et al., 1977, 1981). Unfortunately, due to scheduling constraints, it is typically not possible to schedule a group of individuals for frequent training sessions. In addition, in a group environment, it is difficult to personalize training to specific needs. This will likely be better achieved with home-based computer training using analytic materials that can focus on specific consonant confusions (Miller, Watson, Kistler, Wightman, & Preminger, 2007) or synthetic training in which the SNR can be adjusted to ensure target levels of performance (Sweetow & Sabes, 2006).
The results demonstrated variable and inconclusive results for the synthetic materials despite the large number of items (408 words) presented at each evaluation session. Other studies have shown training effects for individual synthetic training but not for individual analytic training (Kricos & Holmes, 1996; Rubinstein & Boothroyd, 1987). It seems possible that these findings in other studies were due to improvements in the use of higher level processing abilities. In other words, participants may have learned how to take advantage of context, a skill that most adults already have but may not take advantage of. It is not clear that this was the case for the synthetic materials in the current study.
While auditory-only and auditory-visual speech perception did not appear to improve as a result of training, the majority of participants who received training reported that these skills improved. As a result of class participation, 88% of the participants reported improved lipreading skills, 71% reported an improved ability to understand speech in quiet, and 35% reported an improved ability to understand speech in noise. This is similar to the finding reported by Binnie (1977), who demonstrated that 50% of his 12 participants reported improved lipreading abilities after a group class, despite the fact that none of the participants actually demonstrated improvement on a lipreading test. Binnie hypothesized that this feeling of benefit was associated with a feeling of support from the group. An alternative explanation for Binnie’s findings and the findings reported in the current study is that speech perception abilities actually did improve in everyday communication but this improvement was not measured with the objective assessments. Class participants may have learned how to take advantage of context and/or may have learned to take advantage of visual speech perception skills. For example, many times during the group classes, the instructors had to remind certain participants to watch the talker’s face during the training exercises. These individuals may have actually learned to attend to the talker’s face during the training, and this could have carried over to everyday communication (Howell & Montgomery, 1997). On the other hand, the self-reported benefit in auditory-only and auditory-visual speech perception may have been due to the attention that the participants received in the group classes (i.e., the Hawthorne effect) rather than to a true improvement in perception.
The addition of structured psychosocial exercises appeared to have little impact on the feelings of support from the group. While the participants in the Train + PS group rated “learning how others cope with their hearing loss” and “understanding the feelings that others have about their hearing loss” as “very important” significantly more often than did the participants in the Train Only group, the participants in the Train Only group rated these two statements as being either “somewhat important” or “very important” 83% of the time. It seems that most of the participants, regardless of class type and gender, were able to get the support they needed. In all classes, students tried to initiate informal discussions about hearing loss, communication strategies, feelings, and family relationships. The instructors in the Train Only classes did not allow the classes to pursue these discussions by simply moving on to the next training exercise. Even without group discussion, the participants in the training-only group tried to gain psychosocial benefits. Participants frequently made jokes about the communication breakdowns that occurred during the training exercises. This humor and mutual understanding of a commonly shared experience led to a feeling of camaraderie among the class participants. While participants were not given the opportunity for group discussion during the class, many of the students in the Train Only classes came early or stayed late so that they could meet with the other class members in the waiting room. It appeared that the participants wanted the opportunity to discuss their hearing loss with others, and they created this opportunity even though it was not provided by the instructors.
Quality of Life
The results in the present study demonstrated a significant improvement in hearing loss–related quality of life as measured by the Emotional subscale of the HHIE/A for the training participants but not for the control participants. The Emotional subscale of the HHIE/A measures how the experience of hearing loss affects feelings (e.g., “Does your hearing problem cause you to feel embarrassed when meeting new people?”), while the Social subscale measures the impact of hearing loss on daily activities (e.g., “Does your hearing problem cause you to avoid groups of people?”). It is possible that there were no significant findings for the treatment groups on the Social subscale because the auditory-only and auditory-visual training did not actually improve performance in daily activities. On the other hand, the experience of being with a group of others with hearing loss may have resulted in an increased acceptance of the difficulties associated with hearing loss and thus resulted in improved scores on the Emotional subscale. It is possible that other class content, such as communication strategies training, may be more effective in ameliorating the impact of hearing loss on daily activities and would then result in significant effects for both the Social and Emotional subscales of the HHIE/A.
It was surprising that the participants in the control group demonstrated significantly lower total HHIE/A scores on the postclass evaluation and the 6-month evaluation as compared with the baseline evaluation. It is unlikely that this was due to poor test–retest reliability. The reliability of the HHIE/A has been demonstrated in many studies. For example, the initial test development studies reported test–retest correlation coefficients of .96 for the HHIE and .97 for the HHIA (Newman, Weinstein, Jacobson, & Hug, 1991; Weinstein, Spitzer, & Ventry, 1986), and mean total handicap scores differed by 1 point on the HHIE and by 2.6 points on the HHIA over a 6-week time interval (Newman et al., 1991; Weinstein et al., 1986). More recently, McArdle et al. (2005) demonstrated a mean change of 1.8 points in the HHIE scores of 186 veterans when the test was administered and readministered 10 weeks later after a period of no treatment.
It is possible that participation in the initial evaluation session is what resulted in the change in the HHIE/A scores for the control participants. All participants completed the initial HHIE/A form prior to the first evaluation session (this was required because all participants had to demonstrate an initial score of at least 20 in order to participate). At the initial evaluation, all participants completed the auditory-only word recognition task followed by the auditory-visual word recognition task. Then, each participant completed the auditory-only sentence task followed by the auditory-visual sentence task. After completing these tasks, several participants came out of the test booth and commented that they never realized how important speechreading was or how much they depended on it. It is possible that some participants changed their view of their hearing handicap after they were able to see how well they could speechread. Kricos, Holmes, and Doyle (1992) reported a similar finding for a group of 13 control participants. Their control participants were evaluated with a similar test battery as the one used in the present study, in that it included the HHIE and an auditory-only and an auditory-visual sentence recognition task. The control participants were evaluated with the test battery twice, separated by a period of 4 weeks. At the second evaluation, the 13 control participants in the Kricos et al. study showed a mean drop of 8 points on the HHIE. The control participants in the present study demonstrated a similar mean change of 6.5 points on the HHIE/A from the first session to the second test session.
The participants in the two treatment groups showed only modest improvements on the total HHIE/A scale following training. Using a change in HHIE scores greater than 14 to indicate a true change (McArdle et al., 2005), 3 out of 16 (19%) in the control group, 4 out of 16 in the Train + PS group (25%), and 7 out of 18 (39%) in the Train Only group demonstrated significant improvements on the HHIE/A between the baseline and the 6-week evaluations. There are a variety of factors that may have contributed to the small treatment effects in the present research. Most studies that have demonstrated significant benefits from group audiologic rehabilitation training have been studies in which the group program followed hearing aid dispensing in new hearing aid users (Abrams et al., 1992; Chisolm et al., 2004); in studies such as these, the group training supplements the new hearing aid fitting, and the effect on hearing loss–related quality of life is additive. Previous studies that have shown more modest effects of group training have typically studied experienced hearing aid users (Brewer, 2001; Preminger, 2003). It is possible that experienced hearing aid users have different rehabilitation needs than new hearing aid users and may require modifications in the class content. In the current study, class content was limited to auditory-only and auditory-visual speech perception training, as well as psychosocial exercises. Content in other studies that have demonstrated treatment effects (e.g., Abrams et al., 1992) frequently includes communication strategy exercises and informational lectures. A final factor to consider is the outcome measure used. Outcome measures other than the HHIE/A may have been more sensitive to the treatment effects in the group audiologic rehabilitation classes. It would be worthwhile to explore the impact of duration of hearing aid use and class content on the efficacy of group audiologic rehabilitation in future studies.
Hearing loss–related quality of life was measured with the HHIE/A in the current study, and overall quality of life was measured with the WHODAS II. The WHODAS II has only a few questions that relate directly to communication, such as “In the last 30 days how much difficulty did you have in generally understanding what people say?” The WHODAS II was included because it was shown to be sensitive to hearing aid fitting (McArdle et al., 2005), but the effect size was quite small. While both the training groups demonstrated small improvements on the Communication subscale, these were not maintained at the 6-month visit. It appears worthwhile to include the WHODAS II in future research where larger numbers of participants will be evaluated.
Summary and Conclusions
The purpose of the current study was to determine whether (a) auditory-only speech perception can be successfully trained in a group format; (b) auditory-visual speech perception can be successfully trained in a group format; (c) individuals who participate in auditory-only and auditory-visual speech perception training will report improvements in these abilities; and (d) speech perception training will improve self-perceived quality of life. The results did not reveal significant group changes on any of the analytic auditory-only or auditory-visual measures of speech perception between the baseline and the 6-week evaluation or between the baseline and the 6-month evaluation. Results for the synthetic measures were inconclusive. All participants, including the control participants, demonstrated a significant improvement in hearing loss–related quality of life at the 6-week evaluation. Both training groups demonstrated a significant improvement for the Emotional subscale of the HHIE/A, while the control participants did not. There were few meaningful group changes in performance measured for the generic quality of life scale. Based on these findings, the following conclusions can be drawn:
At least 5 hr of group auditory-only and auditory-visual speech perception training in a group format did not result in observable changes on analytic tests of speech perception. Participants who completed this training, however, reported subjective improvements in these skills. Further research is necessary to determine the nature of this subjective benefit. It is possible that participants may have learned to use contextual skills or to take advantage of their innate visual speech perception abilities as a result of class participation.
Audiologic rehabilitation groups in which class content is limited to auditory-only and auditory-visual training and psychosocial activities appear to have little effect on hearing handicap associated with communication in daily activities. This training may affect the emotional aspects of hearing loss. These results suggest that time in group audiologic rehabilitation classes should be spent on activities other than speech perception training.
There were no differences between the two training groups in the improvement measured for hearing loss–related quality of life and only minimal differences across the groups for the subjective class evaluation. Most class participants reported that it was important to be with others who had hearing loss, to learn how they coped and to learn the feelings that they had about their hearing loss. The addition of structured psychosocial exercises added only a minimal benefit to the class experience. It appeared that class members achieved psychosocial benefits without explicit psychosocial activities.
Acknowledgments
This research was supported by National Institutes of Health Grant 5R03DC004939-02, “The Efficacy of Group Aural Rehabilitation Programs.” Portions of this article were presented at the American Auditory Society, Scottsdale, AZ, March 2005, and at the Rehabilitative Audiology Annual Institute, Park City, UT, October 2005. The authors would like to thank the many students who have worked on this project: Scott Anderson, James Baer, Tara Blalock, Mitchell Campbell, Elizabeth Everett White, Miriam Harris-Shelton, Jennifer Leddy, Jodee Pride, Emily Schauwecker, Jeff Shannon, and Allison Young.
Appendix
Audiologic Rehabilitation Research Project, Rehabilitation Class Evaluation
| As a result of these classes… | Become worse | Stayed the same | Become a little better | Become a lot better | |
|---|---|---|---|---|---|
| 1. My ability to lipread has… | 1 | 2 | 3 | 4 | |
| 2. My ability to understand speech in quiet has… | 1 | 2 | 3 | 4 | |
| 3. My ability to understand speech in noise has… | 1 | 2 | 3 | 4 | |
|
| |||||
| Please rate how important each aspect of the course was to you: | Does not apply (did not occur) | Not important | A little important | Somewhat important | Very important |
|
| |||||
| 4. Being with other people who have similar hearing problems as me | 1 | 2 | 3 | 4 | 5 |
| 5. Learning how others cope with hearing loss | 1 | 2 | 3 | 4 | 5 |
| 6. Understanding the feelings that others have about their hearing loss | 1 | 2 | 3 | 4 | 5 |
Footnotes
In our study design, the hypothesis is one-directional, and the training is hypothesized not to improve outcomes. This type of study design can be classified as an equivalence trial or as a “non-superiority trial” (Chi, 2002).
Table 2 shows that the mean baseline auditory-alone performance, for the AB words across all participant groups, was approximately 17% correct. According to Thornton and Raffin, the upper limit of the 95% critical difference score for a score of 17% correct and a 50-word list is 33%. The difference between 33% and 17% is 16; this is the clinical critical difference shown for AB words for each participant group. In practical terms, for AB words, group performance had to improve by at least 16 percentage points in order for the improvement to be considered significant (in order to demonstrate a true improvement). In order to compare the mean difference score with the clinical critical difference score, we must consider that the mean difference score has error associated with it due to sample variability (as shown by the standard errors in parentheses) and may not be the true population mean difference score. While the training-only group showed no change in performance between baseline and 6 weeks for auditory-only AB words, the mean standard error for this 0% difference was 3.36. As a result, there is a confidence interval around the difference score, and the upper limit of this confidence interval is shown. The upper confidence limit was calculated using the measured standard error and a t-distribution table. For the training-only group, we can say with 95% confidence that the actual population mean difference between baseline and 6 weeks is not greater than the upper limit of 5.85. Since this value is less than the predetermined clinical critical difference of 16 percentage points, we can say that a true clinical change has not occurred. As a result, we must consider the scores at baseline and at 6 weeks to be clinically equivalent; this is shown by a “yes” in the rightmost column (for training-only AB words).
Contributor Information
Jill E. Preminger, University of Louisville School of Medicine, Louisville, KY
Craig H. Ziegler, University of Louisville School of Public Health
References
- Abrams HB, Chisolm TH, McArdle R. A cost-utility analysis of adult group audiologic rehabilitation: Are the benefits worth the cost? Journal of Rehabilitation Research and Development. 2002;39:549–558. [PubMed] [Google Scholar]
- Abrams HB, Hnath-Chisolm T, Guerreiro SM, Ritterman SI. The effects of intervention strategy on self-perception of hearing handicap. Ear and Hearing. 1992;13:371–377. doi: 10.1097/00003446-199210000-00013. [DOI] [PubMed] [Google Scholar]
- Bernstein LE, Auer ET, Tucker PE. Enhanced speechreading in deaf adults: Can short-term training/practice close the gap for hearing adults? Journal of Speech Language and Hearing Research. 2001;44:5–18. doi: 10.1044/1092-4388(2001/001). [DOI] [PubMed] [Google Scholar]
- Beynon GJ, Thornton FL, Poole C. A randomized, controlled trial of the efficacy of a communication course for first time hearing aid users. British Journal of Audiology. 1997;31:345–351. doi: 10.3109/03005364000000028. [DOI] [PubMed] [Google Scholar]
- Binnie CA. Attitude changes following speechreading training. Scandinavian Audiology. 1977;6:13–19. doi: 10.3109/01050397709044993. [DOI] [PubMed] [Google Scholar]
- Boothroyd A. Auditory perception of speech contrasts by subjects with sensorineural hearing loss. Journal of Speech and Hearing Research. 1984;27:134–144. doi: 10.1044/jshr.2701.134. [DOI] [PubMed] [Google Scholar]
- Boothroyd A, Hnath-Chisolm T, Hanin L, Kishon-Rabin L. Voice fundamental frequency as an auditory supplement to the speechreading of sentences. Ear and Hearing. 1988;9:306–312. doi: 10.1097/00003446-198812000-00006. [DOI] [PubMed] [Google Scholar]
- Brewer DM. Considerations in measuring effectiveness of group audiologic rehabilitation classes. Journal of the Academy of Rehabilitative Audiology. 2001;34:53–60. [Google Scholar]
- Burk MH, Humes LE, Amos NE, Strauser LE. Effect of training on word-recognition performance in noise for young normal-hearing and older hearing-impaired listeners. Ear and Hearing. 2006;27:263–278. doi: 10.1097/01.aud.0000215980.21158.a2. [DOI] [PubMed] [Google Scholar]
- Chi G. Active control non-superiority trial—what it is about. Paper presented at the 2002 ICSA Applied Statistics Symposium; Plymouth Meeting, PA. 2002. Jun, Retrieved February 21, 2008, from www.fda.gov/cder/offices/Biostatistics/chi_5/index.htm. [Google Scholar]
- Chisolm TH, Abrams HB, McArdle R. Short-and long-term outcomes of adult audiological rehabilitation. Ear and Hearing. 2004;25:464–477. doi: 10.1097/01.aud.0000145114.24651.4e. [DOI] [PubMed] [Google Scholar]
- Chisolm TH, Abrams HB, McArdle R, Wilson RH, Doyle PJ. The WHO-DAS II: Psychometric properties in the measurement of functional health status in adults with acquired hearing loss. Trends in Amplification. 2005;9:111–126. doi: 10.1177/108471380500900303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erber NP. Effects of distance on the visual reception of speech. Journal of Speech and Hearing Research. 1971;14:848–857. doi: 10.1044/jshr.1404.848. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Friedman LM, Furberg CD, Demets DD. Fundamentals of clinical trials. 3. New York: Springer-Verlag; 1998. [Google Scholar]
- Gagné JP, Dinon D, Parsons J. An evaluation of CAST: A computer-aided speechreading training program. Journal of Speech and Hearing Research. 1991;34:213–221. doi: 10.1044/jshr.3401.213. [DOI] [PubMed] [Google Scholar]
- Grant KW, Seitz PF. Measures of auditory-visual integration in nonsense syllables and sentences. Journal of the Acoustical Society of America. 1998;104:2438–2450. doi: 10.1121/1.423751. [DOI] [PubMed] [Google Scholar]
- Grant KW, Walden BE, Seitz PF. Auditory-visual speech recognition by hearing-impaired subjects: Consonant recognition, sentence recognition, and auditory-visual integration. Journal of the Acoustical Society of America. 1998;103:2677–2690. doi: 10.1121/1.422788. [DOI] [PubMed] [Google Scholar]
- Hardick EJ, Oyer HJ, Irion PE. Lipreading performance as related to measurements of vision. Journal of Speech and Hearing Research. 1970;13:92–100. doi: 10.1044/jshr.1301.92. [DOI] [PubMed] [Google Scholar]
- Hawkins DB. Effectiveness of counseling-based adult group aural rehabilitation programs: A systematic review of the evidence. Journal of the American Academy of Audiology. 2005;16:485–493. doi: 10.3766/jaaa.16.7.8. [DOI] [PubMed] [Google Scholar]
- Hogan A. Hearing rehabilitation for deafened adults: A psychosocial approach. London: Whurr; 2001. [DOI] [PubMed] [Google Scholar]
- Howell I, Montgomery AA. Auditory-visual integration: A practical approach. Seminars in Hearing. 1997;18:141–151. [Google Scholar]
- Kander M, White S. Coding auditory and aural rehabilitation procedures. The ASHA Leader, 11(4), pp. 2006 Mar 21;3:16–17. [Google Scholar]
- Kaplan H, Bally S, Garretson C. Speechreading: A way to improve understanding. Washington, DC: Gallaudet University Press; 1985. [Google Scholar]
- Kricos PB, Holmes AE. Efficacy of audiologic rehabilitation for older adults. Journal of the American Academy of Audiology. 1996;7:219–229. [PubMed] [Google Scholar]
- Kricos PB, Holmes AE, Doyle DA. Efficacy of a communication training program for hearing-impaired elderly adults. Journal of the Academy of Rehabilitative Audiology. 1992;25:69–80. [Google Scholar]
- Levitt H. Transformed up-down methods in psycho-acoustics. Journal of the Acoustical Society of America. 1971;49(Suppl 2):467. [PubMed] [Google Scholar]
- Lively SE, Pisoni DB, Yamada RA, Tohkura Y, Yamada T. Training Japanese listeners to identify English /r/ and /l/. III. Long-term retention of new phonetic categories. Journal of the Acoustical Society of America. 1994;96:2076–2087. doi: 10.1121/1.410149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan JS, Lively SE, Pisoni DB. Training listeners to perceive novel phonetic categories: How do we know what is learned? Journal of the Acoustical Society of America. 1993;94:1148–1151. doi: 10.1121/1.406963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massaro DW, Cohen MM, Gesi AT. Long-term training, transfer, and retention in learning to lipread. Perception and Psychophysics. 1993;53:549–562. doi: 10.3758/bf03205203. [DOI] [PubMed] [Google Scholar]
- McArdle R, Chisolm TH, Abrams HB, Wilson RH, Doyle PJ. The WHO-DAS II: Measuring outcomes of hearing aid intervention for adults. Trends in Amplification. 2005;9:127–143. doi: 10.1177/108471380500900304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merzenich MM, Jenkins WM, Johnston P, Schreiner C, Miller SL, Tallal P. Temporal processing deficits of language-learning impaired children ameliorated by training. Science. 1996;271:77–81. doi: 10.1126/science.271.5245.77. [DOI] [PubMed] [Google Scholar]
- Miller JD, Watson CS, Kistler DJ, Wightman FL, Preminger JE. Preliminary evaluation of the speech perception assessment and training system (SPATS) with hearing-aid and cochlear-implant users [Abstract] Journal of the Acoustical Society of America. 2007;122:3063. doi: 10.1121/1.2988004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery AA, Walden BE, Schwartz DM, Prosek RA. Training auditory-visual speech reception in adults with moderate sensorineural hearing loss. Ear and Hearing. 1984;5:30–36. doi: 10.1097/00003446-198401000-00007. [DOI] [PubMed] [Google Scholar]
- Newman CW, Weinstein BE, Jacobson GP, Hug GA. The Hearing Handicap Inventory for Adults: Psycho-metric adequacy and audiometric correlates. Ear and Hearing. 1990;11:430–433. doi: 10.1097/00003446-199012000-00004. [DOI] [PubMed] [Google Scholar]
- Newman CW, Weinstein BE, Jacobson GP, Hug GA. Test-retest reliability of the hearing handicap inventory for adults. Ear and Hearing. 1991;12:355–357. doi: 10.1097/00003446-199110000-00009. [DOI] [PubMed] [Google Scholar]
- Nogaki G, Fu QJ, Galvin JJ., III Effect of training rate on recognition of spectrally shifted speech. Ear and Hearing. 2007;28:132–140. doi: 10.1097/AUD.0b013e3180312669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman M, George CR, Downie A, Milligan J. Evaluation of a communication course for new hearing aid users. Scandinavian Audiology. 1995;24:63–69. doi: 10.3109/01050399509042212. [DOI] [PubMed] [Google Scholar]
- Piantadosi S. Clinical trials: A methodologic perspective. New York: Wiley; 1997. [Google Scholar]
- Preminger JE. Should significant others be encouraged to join adult group audiologic rehabilitation classes? Journal of the American Academy of Audiology. 2003;14:545–555. doi: 10.3766/jaaa.14.10.3. [DOI] [PubMed] [Google Scholar]
- Rubinstein A, Boothroyd A. Effect of two approaches to auditory training on speech recognition by hearing-impaired adults. Journal of Speech and Hearing Research. 1987;30:153–160. doi: 10.1044/jshr.3002.153. [DOI] [PubMed] [Google Scholar]
- Schuirmann DJ. A comparison of the two one-sided test procedure and the power approach for assessing the equivalence of average bioavailability. Journal of Phamacokinetics and Biopharmaceutics. 1987;15:657–680. doi: 10.1007/BF01068419. [DOI] [PubMed] [Google Scholar]
- Scott LC, Metz DE, Rohland P, Samar VJ. A cognitive/experiential approach to aural rehabilitation. American Annals of the Deaf. 1989;134:27–29. doi: 10.1353/aad.2012.0673. [DOI] [PubMed] [Google Scholar]
- Smaldino SE, Smaldino JJ. The influence of aural rehabilitation and cognitive style disclosure of the perception of hearing handicap. Journal of the Academy of Rehabilitative Audiology. 1988;21:49–56. [Google Scholar]
- Sommers MS, Tye-Murray N, Spehar B. Auditory-visual speech perception and auditory-visual enhancement in normal-hearing younger and older adults. Ear and Hearing. 2005;26:263–275. doi: 10.1097/00003446-200506000-00003. [DOI] [PubMed] [Google Scholar]
- Stach BA, Spretnjak ML, Jerger J. The prevalence of central presbyacusis in a clinical population. Journal of the American Academy of Audiology. 1990;1:109–115. [PubMed] [Google Scholar]
- Stecker GC, Bowman GA, Yund W, Herron TJ, Roup CM, Woods DL. Perceptual training improves syllable identification in new and experienced hearing aid users. Journal of Rehabilitation Research and Development. 2006;43:537–552. doi: 10.1682/jrrd.2005.11.0171. [DOI] [PubMed] [Google Scholar]
- Sweetow R, Palmer CV. Efficacy of individual auditory training in adults: A systematic review of the evidence. Journal of the American Academy of Audiology. 2005;16:494–504. doi: 10.3766/jaaa.16.7.9. [DOI] [PubMed] [Google Scholar]
- Sweetow RW, Sabes JH. The need for and development of an adaptive Listening and Communication Enhancement (LACE) Program. Journal of the American Academy of Audiology. 2006;17:538–558. doi: 10.3766/jaaa.17.8.2. [DOI] [PubMed] [Google Scholar]
- Thornton AR, Raffin MJ. Speech-discrimination scores modeled as a binomial variable. Journal of Speech and Hearing Research. 1978;21:507–518. doi: 10.1044/jshr.2103.507. [DOI] [PubMed] [Google Scholar]
- Tremblay K, Kraus N, Carrell TD, McGee T. Central auditory system plasticity: Generalization to novel stimuli following listening training. Journal of the Acoustical Society of America. 1997;102:3762–3773. doi: 10.1121/1.420139. [DOI] [PubMed] [Google Scholar]
- Tye-Murray N. Communication training for older teenagers and adults. Austin, TX: Pro-Ed; 1997. [Google Scholar]
- Ventry IM, Weinstein BE. The hearing handicap inventory for the elderly: A new tool. Ear and Hearing. 1982;3:128–134. doi: 10.1097/00003446-198205000-00006. [DOI] [PubMed] [Google Scholar]
- Walden BE, Erdman SA, Montgomery AA, Schwartz DM, Prosek RA. Some effects of training on speech recognition by hearing-impaired adults. Journal of Speech and Hearing Research. 1981;24:207–216. doi: 10.1044/jshr.2402.207. [DOI] [PubMed] [Google Scholar]
- Walden BE, Prosek RA, Montgomery AA, Scherr CK, Jones CJ. Effects of training on the visual recognition of consonants. Journal of Speech and Hearing Research. 1977;20:130–145. doi: 10.1044/jshr.2001.130. [DOI] [PubMed] [Google Scholar]
- Watson CS. Time course of auditory perceptual learning. The Annals of Otology Rhinology and Laryngology Supplement. 1980;89:96–102. [PubMed] [Google Scholar]
- Weinstein BE, Spitzer JB, Ventry IM. Test-retest reliability of the Hearing Handicap Inventory for the Elderly. Ear and Hearing. 1986;7:295–299. doi: 10.1097/00003446-198610000-00002. [DOI] [PubMed] [Google Scholar]
- Wothke W. Longitudinal and multi-group modeling with missing data. In: Little TD, Schnabel KU, Baumert J, editors. Modeling longitudinal and multiple group data: Practical issues, applied approaches and specific examples. Mahwah, NJ: Erlbaum; 1998. pp. 219–240. [Google Scholar]
- Yellin MW, Jerger J, Fifer RC. Norms for disproportionate loss in speech intelligibility. Ear and Hearing. 1989;10:231–234. doi: 10.1097/00003446-198908000-00003. [DOI] [PubMed] [Google Scholar]