Abstract
Background
Pathological gambling (PG) is a prevalent and impairing public health problem. In this study we assessed age at onset in men and women with PG and compared the demographic and clinical picture of early- vs. later-onset individuals. We also compared age at onset in PG subjects and their first-degree relatives with PG.
Method
Subjects with DSM-IV PG were recruited during the conduct of two non-treatment clinical studies. Subjects were evaluated with structured interviews and validated questionnaires. Early-onset was defined as PG starting prior to age 33 years.
Results
Age at onset of PG in the 255 subjects ranged from 8 to 80 years with a mean (SD) of 34.0 (15.3) years. Men had an earlier onset than women. 84% of all subjects with PG had developed the disorder by age 50 years. Early-onset subjects were more likely to be male, to prefer action games, and to have substance use disorders, antisocial personality disorder, attention deficit/hyperactivity disorder, trait impulsiveness, and social anxiety disorder. Later-onset was more common in women and was associated with a preference for slots and a history of sexual abuse.
Conclusions
Age at onset of PG is bimodal and differs for men and women. Early- and later-onset PG have important demographic and clinical differences. The implications of the findings are discussed.
Keywords: pathological gambling, gambling disorder, family studies, longitudinal studies, age at onset
1. Introduction
Pathological gambling (PG) is characterized by the presence of persistent and recurrent maladaptive gambling behavior the person is unable to adequately control. 1 PG is common, affects people of all ages, and is associated with depression, substance misuse, domestic violence, bankruptcy, and suicide. 2 Renamed “Gambling Disorder” in DSM-5, the condition has been moved to the chapter on substance-related and addictive disorders to acknowledge its commonalities with alcohol and drug use disorders. 3
Age at onset is important to assess because it can give important clues to a disorder’s etiology and pathophysiology. There are often significant differences that influence course and outcome and in some instances treatment response. Age at onset is also fundamental to a disorder’s natural history. 4, 5 DSM-5 has acknowledged the importance of age at onset by arranging the chapters in a “neurodevelopmental” fashion, so that disorders with an earlier onset are placed before those with a later onset. 3
Fundamental differences can emerge when early- and later-onset cases are compared. For many disorders, early-onset cases are more severe, are concentrated in one gender, or are more difficult to treat. 5 For example, persons with childhood-onset schizophrenia or bipolar disorder have a poorer prognosis and worse treatment response than persons with a more typical later onset. 4, 6 This finding is also true for other conditions including major depression, anxiety disorders, and the addictions. 4, 7
Knowing a person’s age at onset is vital to gaining a better understanding of PG. Research has shown that the disorder tends to have an age at onset ranging from the mid-20s to the late 30’s, but can occur for the first time even during senescence. Importantly, men are reported to have an earlier onset than women. 8 The course for women is widely described as “telescoping,” meaning that the transition from problem gambling to PG occurs more rapidly in women than in men, 9 despite the later onset in women.
Complicating the discussion of age at onset is the fact that some researchers assess multiple ages at onset: first gambling exposure, first gambling symptoms, first treatment, and when a person meets DSM criteria for PG. 5, 10, 11 Furthermore, reported age at onset may in part reflect the gender distribution of the sample. Samples having a greater proportion of men tend to have an earlier mean age at onset. 11
The range for age at onset in clinical studies is fairly narrow, suggesting that the results are valid despite differences in assessment methods and populations. In our own work, we reported a mean age at onset of 36.4 years in 31 subjects enrolled in a pilot family study, 12 38.3 years for 19 persons enrolled in an escitalopram trial, 13 and 35.8 years for 39 subjects in a bupropion trial. 14 Grant and Kim 15 reported a mean age at onset among 131 treatment-seeking pathological gamblers of 36.8 years, while Grant et al. 16 reported that 207 PG subjects assigned to one of 4 treatment cells in a nalmefene trial had a mean age at onset ranging from 34.2 years to 36.9 years.
Epidemiological surveys have tended to report an earlier onset of PG. In a general population study in Edmonton, Bland et al. 17 reported a mean age at onset of 25 years for people with “heavy betting.” Blanco et al. 18 reported data from the National Epidemiologic Survey on Alcohol and Related Conditions and calculated an earlier mean age at onset for men (29.6 years) than women (34.9 years). Kessler et al. 19 reported data from the National Comorbidity Survey Replication; respondents with lifetime PG had an average of 9.4 years of gambling problems beginning at a mean age of 23 years.
We examined age at onset as part of the Iowa Family Study of PG, 20 and the ongoing Iowa Longitudinal Study of Addictions in Older Adults, both non-treatment seeking samples. The former is a family study of PG which demonstrated the familality of PG, while the latter is a follow up study of PG and co-occurring disorders in older adults with a younger comparison group. Based on the literature and our own work, we expected that PG would have a mean age at onset of less than 40 years, and that women would have a later onset than men. We also expected that when comparing early- and later-onset subjects, the former would be predominantly male, have more severe gambling symptoms, have higher trait impulsiveness, prefer action games (e.g., card games), and have more co-occurring externalizing disorders (e.g., substance use disorders, antisocial personality disorder). We expected that, compared with early-onset cases, subjects with later-onset PG would be predominantly female, have higher rates of depressive and anxiety disorders, have lower levels of trait impulsiveness, and prefer slots. Last, we expected that age at onset in PG subjects would be positively correlated with age at onset in their first-degree relatives with PG. With these expectations in mind, we first examine age at onset in men, women, and the total sample. We then examine the characteristics of early- vs. later-onset subjects with PG. Finally, we examine variables associated with age at onset using regression analysis.
2. Methods
2.1. Subjects
The study includes subjects who participated in the Iowa Family Study of Pathological Gambling 20 and the ongoing Iowa Longitudinal Study of Addictions. Persons with PG were recruited from the Iowa community. All had South Oaks Gambling Scores 21 and National Opinion Research Center (NORC) DSM Screen for Gambling Problems 2 scores ≥ 5; they also had to meet DSM-IV PG criteria. 22 All were 18 years or older, spoke English and lacked psychotic, cognitive, or chronic neurological disorders. Controls were required to have a SOGS score of ≤ 2 and a NODS score of 0. Written informed consent was obtained from all subjects according to procedures approved by the University of Iowa Institutional Review Board.
Subjects were interviewed between February 2005 and June 2010 in the family study and from March 2011 to September 2014 in the longitudinal study. All were interviewed in-person. In the family study, first-degree relatives were interviewed primarily by telephone. Informant interviews were conducted for those relatives who were deceased, chose not to participate, or could not be located. In most cases, multiple assessments were available. 20
For the subset participating in the Iowa Family Study of PG, a blind consensus procedure was used to assign diagnoses to first-degree relatives for major mental disorders and antisocial personality disorder. 23 They were also rated for the presence of PG, subclinical PG, recreational gambling, and no gambling. Only probable and definite cases of PG were included in the analyses. Details of the procedure are reported elsewhere. 20
2.2 Assessments
Diagnostic assessments included the Structured Clinical Interview for DSM-IV 24 and the Family History Research Diagnostic Criteria, adapted to include criteria for PG and used to collect information from relatives. 25, 26 The Minnesota Impulsive Disorders interview 27 was used to collect data on impulse control disorders including several non-DSM conditions (kleptomania, pyromania, intermittent explosive disorder, compulsive buying disorder, compulsive sexual behavior, Internet addiction, and trichotillomania). Attention deficit/hyperactivity disorder (ADHD) was assessed using a module from the Mini International Neuropsychiatric Interview. 28 The Structured Interview for DSM-IV Personality 29 was used to assess personality disorders. We used questions from the Temperament and Character Inventory (TCI) 30 to assess novelty seeking. The Barratt Impulsiveness Scale 31 was used to assess motor, cognitive, and non-planning impulsiveness. Age at onset was defined as when the individual first met full DSM-IV criteria for PG.
To determine “early-onset” versus “later-onset” PG, we examined frequency distributions of age at onset for men, women, and all subjects combined. Survival curves were also examined, showing the percentage of individuals with PG by age. If the distributions were unimodal, early-onset would be determined by the median. If the distributions were bimodal, early-onset would be determined by the age that best demarcates the two distributions. Based on this analysis, we defined the person with early-onset PG as being < 33 years.
2.3. Statistical Analysis
Individuals included in the analysis were drawn from three study groups: subjects with PG from the family study; first-degree relatives from the family study with definite or probable PG; and subjects with PG from the ongoing longitudinal study. Early and later-onset cases were compared on sociodemographic and clinical characteristics. For dichotomous variables (gender, race/ethnicity, being divorced, mental health hospitalization, treatment for gambling, childhood maltreatment, psychiatric comorbidity, and family history of psychiatric comorbidity), logistic regression was used to test for differences by early-onset category. For dimensional variables (age, PG severity, novelty seeking, and impulsiveness), multiple linear regression was used. Because the study groups varied on mean age at onset (the first-degree relatives from the family study had later age at onset), study group was used as a covariate in the regression analyses. For categorical variables (educational level and type of gambling preferred), Pearson’s Chi-Square test was used to compare early and late-onset cases. Some measures were only available for individuals from the family study, including novelty seeking and family history of psychiatric comorbidity. For these measures, the analyses are restricted to the Iowa Family Study data set.
Logistic regression was then used to examine predictors of early-onset. Sociodemographic and clinical variables were included in a stepwise selection model where significant variables were retained in the model. Study group was again used as a covariate (forced into the model). All statistical tests were 2-tailed with α = 0.05.
3. Results
The analysis included 255 subjects for whom age at onset was known, including PG subjects (n=94) and their first-degree relatives with PG (n=58) from the Iowa Family Study of PG and subjects with PG from the Iowa Longitudinal Study of Addictions (n=103). Nine individuals were not included because their age at onset was unknown, including PG subjects (n=1) and their first-degree relatives with PG (n=7) from the family study, and one individual from the longitudinal study. Within the family study sample, the correlation of age at onset for PG subjects and their first-degree relatives was 0.21 (P=.143).
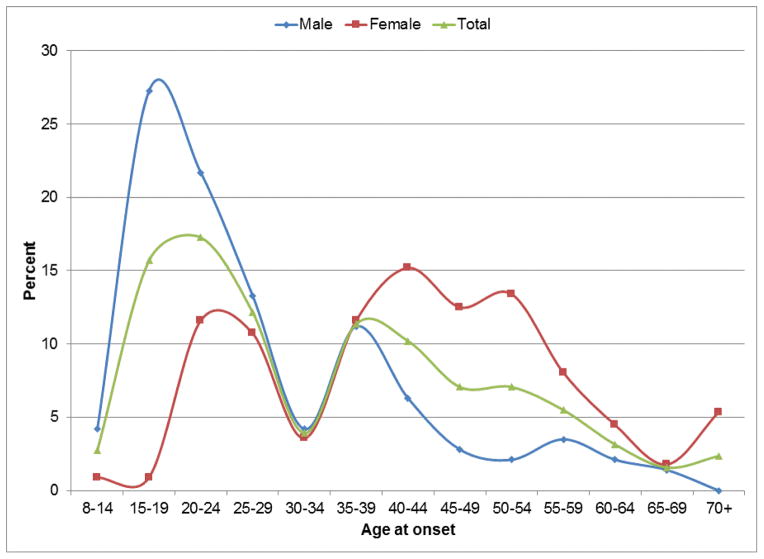
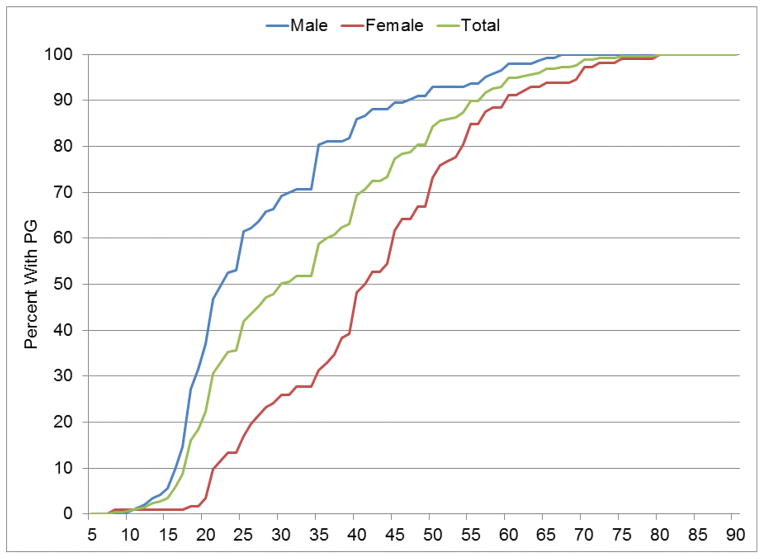
In the total sample, age at onset ranged from 8 to 80 years, with a mean (SD) of 34.0 (15.3) years (Table 1, Figure 1). Median age at onset was 30 years and the average duration of PG was 10.9 years (SD=11.4). As shown in Figure 2, 50% of the total sample had an onset by age 30 years, 69% by age 40, and 84% by age 50 years. Mean and median age at onset was earlier in men (mean=27.7, median=23) than women (mean=42.0, median=41) (Figure 1, p<.001). For women, age at onset was bimodal, with peaks appearing at the 20–24 and 40–44 year age ranges (Figure 1). For men, age at onset peaked for the 15–24 year age range and had a smaller spike for the 35–39 year age range. For both men and women, the 30–34 year age range appeared to separate relative peaks in the distributions. Therefore, the midpoint of this range (32) was chosen as the cutoff to define early-onset.
Table 1.
A comparison of subjects with early-versus later-onset PG
| Variables | Total (n=255) | Early-onset PG | Later-onset PG | X2 (F), df | P-value |
|---|---|---|---|---|---|
| (n =132) | (n =123) | ||||
| PG age at onset, years, mean (SD) | 34.0 (15.3) | 21.5 (4.8) | 47.4 (10.5) | ||
| Age, mean (SD) | 44.2 (17.1) | 33.7 (14.0) | 56.0 (11.9) | 155.8,1, 222 | <0.001 |
| Female, no. (%) | 143 (44%) | 101 (23%) | 42 (66%) | 38.3, 1 | <0.001 |
| European-Caucasian, no. (%) | 220 (86%) | 110 (83%) | 110 (89%) | 1.1, 1 | 0.293 |
| Ever divorced (%)* | 77 (58%) | 20 (43%) | 57 (66%) | 4.9, 1 | 0.026 |
| Education, years, mean (SD) | 14.2 (2.2) | 14.4 (2.3) | 13.9 (2.2) | 1.1, 1, 206 | 0.290 |
| Educational achievement | 3.1, 3 | 0.371 | |||
| Less than high school diploma, no. (%) | 23 (11%) | 14 (12%) | 9 (9%) | ||
| High school diploma, no. (%) | 92 (44%) | 54 (48%) | 38 (40%) | ||
| Associate’s degree/certificate, no. (%) | 41 (20%) | 18 (16%) | 23 (24%) | ||
| Bachelor’s degree or higher, no. (%) | 53 (25%) | 27 (24%) | 26 (27%) | ||
| Gambling preference | 56.8, 2 | <0.001 | |||
| Action games | 90 (41%) | 75 (64%) | 15 (15%) | ||
| Slots | 90 (41%) | 25 (21%) | 65 (65%) | ||
| Other | 38 (17%) | 18 (15%) | 20 (20%) | ||
| Psychiatric hospitalization, no. (%) | 55 (27%) | 28 (25%) | 27 (28%) | 0.3, 1 | 0.610 |
| Treatment of PG, no. (%) | 86 (43%) | 38 (36%) | 48 (51%) | 1.3, 1 | 0.252 |
| # of PG DSM-IV criteria, mean (SD) | 7.0 (2.8) | 7.2 (2.8) | 6.8 (2.9) | 0.4, 1, 251 | 0.543 |
| SOGS score, mean (SD) | 11.9 (4.2) | 11.9 (4.4) | 11.9 (4.1) | 0.8, 1, 206 | 0.386 |
| NODS score, mean (SD) | 13.1 (4.2) | 13.1 (4.2) | 13.1 (4.1) | 0.2, 1, 205 | 0.696 |
| BIS total score, mean (SD) | 68.6 (11.9) | 70.2 (12.9) | 67.0 (10.6) | 4.7, 1, 181 | 0.031 |
| Novelty seeking1, mean (SD) | 21.2 (7.1) | 21.9 (8.0) | 20.7 (6.3) | 1.1, 1, 97 | 0.303 |
| Childhood maltreatment | |||||
| Physical, no. (%) | 50 (26%) | 25 (25%) | 25 (27%) | 0.2, 1 | 0.696 |
| Verbal, no. (%) | 84 (43%) | 45 (44%) | 39 (42%) | 0.4, 1 | 0.529 |
| Sexual, no. (%) | 30 (15%) | 7 (7%) | 23 (25%) | 8.5, 1 | 0.004 |
| Any maltreatment, no. (%) | 103 (53%) | 50 (49%) | 53 (58%) | 0.4, 1 | 0.503 |
| Psychiatric comorbidity | |||||
| Any substance use disorder, no. (%) | 159 (62%) | 99 (75%) | 60 (49%) | 20.9, 1 | <0.001 |
| Alcohol use disorder, no. (%) | 140 (55%) | 85 (64%) | 55 (45%) | 11.8, 1 | 0.001 |
| Drug use disorder, no. (%) | 72 (28%) | 52 (39%) | 20 (16%) | 15.9, 1 | <0.001 |
| Any anxiety disorder, no. (%) | 95 (37%) | 55 (42%) | 40 (33%) | 2.1, 1 | 0.149 |
| GAD, no. (%) | 23 (9%) | 12 (9%) | 11 (9%) | 0.0, 1 | 0.852 |
| OCD, no. (%) | 18 (7%) | 13 (10%) | 5 (4%) | 2.2, 1 | 0.136 |
| Panic disorder, no. (%) | 47 (19%) | 28 (21%) | 19 (16%) | 0.3, 1 | 0.571 |
| Specific phobia, no. (%) | 20 (8%) | 12 (9%) | 8 (7%) | 0.0, 1 | 0.839 |
| Social anxiety disorder, no. (%) | 26 (10%) | 19 (14%) | 7 (6%) | 4.6, 1 | 0.032 |
| Any mood disorder, no. (%) | 138 (54%) | 68 (52%) | 70 (57%) | 0.3, 1 | 0.573 |
| Bipolar disorder, no. (%) | 19 (7%) | 10 (8%) | 9 (7%) | 0.0, 1 | 0.880 |
| Major depression disorder, no. (%) | 122 (48%) | 59 (45%) | 63 (52%) | 1.1, 1 | 0.288 |
| Any eating disorder, no. (%) | 21 (8%) | 9 (7%) | 12 (10%) | 0.6, 1 | 0.425 |
| Any impulse control disorder, no. (%) | 61 (24%) | 40 (30%) | 21 (17%) | 3.4, 1 | 0.065 |
| ADHD, no. (%) | 37 (15%) | 31 (23%) | 6 (5%) | 14.5, 1 | <0.001 |
| ASPD, no. (%) | 23 (12%) | 17 (16%) | 6 (6%) | 6.7, 1 | 0.009 |
| Past suicide attempt, no, (%) | 52 (20%) | 24 (18%) | 28 (23%) | 0.2, 1 | 0.637 |
| Family History | |||||
| Any mood disorder1, no. (%) | 129 (85%) | 52 (81%) | 77 (88%) | 1.2, 1 | 0.267 |
| Any substance use disorder1, no. (%) | 129 (85%) | 55 (86%) | 74 (84%) | 0.1, 1 | 0.768 |
| Any anxiety disorder1, no. (%) | 101 (66%) | 38 (59%) | 63 (72%) | 2.7, 1 | 0.099 |
| Any gambling disorder, no. (%) | 141 (56%) | 65 (50%) | 76 (64%) | 0.8, 1 | 0.367 |
| ASPD1, no. (%) | 18 (13%) | 7 (13%) | 11 (14%) | 0.0, 1 | 0.889 |
| Past suicide attempt1, no, (%) | 55 (36%) | 26 (41%) | 29 (33%) | 0.9, 1 | 0.339 |
Family study data only
ASPD=antisocial personality disorder; ADHD=attention deficit/hyperactivity disorder; GAD=generalized anxiety disorder; OCD=obsessive-compulsive disorder
Figure 1.
Age at onset in male and female subjects with PG
Figure 2.
Percentage with PG by age at onset, in 246 subjects with PG
Among subjects with early-onset PG, 23% were women, compared with 66% among later-onset subjects (Table 1, P<0.001). Early-onset PG was also associated with greater trait impulsiveness (P=0.031); and lifetime substance use disorders (P<0.001), ADHD (P<0.001), antisocial personality disorder (P=0.009), and social anxiety disorder (P=0.032). The relationship with impulse-control disorders approached significance (P=0.065). Early-onset cases were more likely to prefer action games (e.g., card games, pari-mutuel sports, roulette, table games) and less likely to prefer slots (P<0.001). Later-onset cases were more likely to report childhood sexual abuse (P=0.004).
We found that several variables were associated with early-onset PG (Table 1). Because, many of the associations could be due to inter-correlation of gender and the risk factor (e.g., male gender, substance use disorders), we modeled early-onset PG using multiple logistic regression to isolate unique effects. Significant predictors of early-onset PG include age, male gender (OR=4.46, P<0.001), a lifetime substance use disorder (OR=2.58, P=0.039), and lifetime ADHD (OR=5.13, P=0.006).
4. Discussion
PG has a clear bimodal distribution for age at onset with a peak in the late teens and early twenties, and a smaller secondary peak in the late 30s and early 40s. For women, the higher peak occurs in the 40s with the smaller secondary peak in the 20s. Mean age at onset is 34.0 years with men having an earlier onset than women, a finding consistent with a large body of work on PG and gender differences. 9, 18, 19 Women with PG have been observed to have a more rapid progression of their disorder through a process called “telescoping,” 9 a phenomenon also observed in women with alcohol use and cannabis use disorders. 6, 32 While our data on age at onset could be skewed by inaccurate retrospective self-reports regarding problematic gambling behavior, the findings are consistent with our own observations 12, 13 and those of other investigators. 15, 16
We had defined early- and later-onset cases based on sample characteristics and set the cut point at <33 years. Early-onset cases were more likely to be male, had higher levels of trait impulsiveness, preferred action games, and had higher rates of co-occurring mental health and addictive disorders. We found a higher frequency of social anxiety disorder, substance use disorders, impulse control disorders, antisocial personality disorder, and ADHD. Apart from anxiety disorders, the other disorders are widely considered externalizing disorders, that is, conditions in which symptoms are outwardly directed. 33 Other investigators have reported this pattern as well in early-onset samples. 10, 34 Our findings part company with Jimenez-Murcia et al.10 in that we did not find a difference between groups of early- and later-onset cases for overall PG severity or novelty seeking. Unlike Vizcaino et al., 34 in this study early-onset cases were not less likely to have a mood disorder.
The later-onset group, on the other hand, is characterized by a female preponderance; they prefer slots and are more likely to report a history of childhood sexual abuse. Contrary to expectation, we did not find an increase in internalizing disorders in the older group. Further, despite gender and age differences, familiality was unrelated to age at onset. We had expected that early-onset cases would be more likely to be familial by having more relatives with a gambling disorder, but that was not true. Unlike several mental disorders (e.g., schizophrenia, bipolar disorder) in which age at onset is related to familial transmission, we found no such association.
Several factors were associated with higher risk of early-onset PG, including male gender, higher trait impulsivity, and lifetime substance use disorders, social anxiety disorder, ADHD, and ASPD. Because many of these risk factors are inter-correlated (e.g., substance use disorder and trait impulsiveness) or frequently co-occur (e.g., ADHD and ASPD), it is not surprising that only a subset of these factors (male gender, lifetime substance use disorder, and ADHD) demonstrated independent effects on risk for early-onset PG.
Observed differences between early- and later-onset cases appear to partially validate the “escape-seeking” versus the “sensation-seeking” classification scheme for PG. 35 The former group includes persons – typically women – who are reported to gamble to relieve emotional tension, anxiety, or depression. For such people, gambling may provide an escape from unpleasant affects. In contrast, the latter group includes persons who seek stimulation and arousal to relieve boredom or hyperarousal. 36 The more comprehensive “pathways” model integrates biological, developmental, and cognitive variables to describe three types of persons with PG. 37, 38 In this model, early-onset PG appears consistent with the “antisocial, impulsive gambler” which begins early in life, escalates rapidly, and mainly involves men. These gamblers have features of antisocial personality disorder and trait impulsiveness that to some suggest neurological or neurochemical dysfunction. Later-onset cases partially fit the description of the “emotionally vulnerable gambler;” these persons are mostly female, suffer premorbid depression or anxiety, have difficulty coping, have frequent life events, and experience adverse developmental experiences (e.g., childhood abuse). For these individuals, gambling serves to modulate mood states or meet other psychological needs.
An important finding is that 84% of the subjects had developed PG by age 50 years, which indicates that it is unusual for a person to develop PG later in life. Thus, if a person has not developed PG by age 50 years, he or she is unlikely to do so. While the mean age at onset is in the 30s, the cumulative percent reaches 50% at age 30, and the mode is from age 20–24 years. Thus, like many other mental disorders, including psychotic, mood, and substance use disorders, PG develops for most at an early age possibly influenced by processes linked to brain maturation, which typically ends during the third decade of life. 4 PG is widely considered an externalizing disorder and appears to develop at a similar age to other disorders within that spectrum. 39
There are several methodologic limitations. First, PG probands recruited through an epidemiological sampling method would have been more desirable, but this was not feasible. Second, the low participation rate of minority subjects reduces the generalizability of our findings in these populations. Third, not all the interviews were direct and in person. Fourth, some relatives could not be interviewed due to death or other reasons, and while we aimed to include these relatives by conducting informant interviews, it is possible that information was missed because the PG or control subject was not sufficiently familiar with the individual in question. Because we recruited subjects 18 years and older, we may have missed early-onset cases. Last, the assessment of age at onset is somewhat arbitrary and relies on a person’s (or their relatives’) memory regarding symptom severity and that may be unreliable and flawed.
Table 2.
Predictors of early-onset PG
| Variables | Est. | SE | P-value | Odds Ratio (95% C.I.) |
|---|---|---|---|---|
| Age | −0.103 | 0.015 | <0.001 | 0.90 (0.88, 0.93) |
| Male gender | 1.496 | 0.420 | <0.001 | 4.46 (1.96, 10.16) |
| Any substance use disorder | 0.946 | 0.458 | 0.039 | 2.58 (1.05, 6.32) |
| ADHD | 1.636 | 0.596 | 0.006 | 5.13 (1.60, 16.52) |
| Study group* | ||||
| Family study probands | −1.100 | 0.468 | 0.019 | 0.33 (0.13, 0.83) |
| Family study relatives | −0.465 | 0.628 | 0.458 | 0.63 (0.18, 2.15) |
Results based on multiple logistic regression analyses with stepwise variable selection.
Subjects from the longitudinal study used as reference group.
ADHD=attention deficit/hyperactivity disorder
Acknowledgments
The research was supported in part through grants from the National Institute on Drug Abuse (RO1DA021361) and the National Institute on Aging (RO1AG037132), Bethesda, MD (to Dr. Black). Dr. Black also receives research support from AstraZeneca and royalties from American Psychiatric Publishing, Oxford University Press, and UpToDate. Drs. Crowe, Coryell, and Allen, and Ms. Shaw and Mr.McCormick report no conflicts.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. Washington, DC: American Psychiatric Press; 1980. [Google Scholar]
- 2.National Opinion Research Center at the University of Chicago (NORC) Gambling Impact and Behavior Study, Report to the National Gambling Impact Study Commission. Apr 1, 1999. [Google Scholar]
- 3.Black DW, Grant JE. DSM-5 Guidebook: The Essential Companion to the Diagnostic and Statistical Manual of Mental Disorders. 5. Washington DC: American Psychiatric Publishing; 2014. [Google Scholar]
- 4.Jones PB. Adult mental health disorders and their age at onset. Br J Psychiatry. 2013;202:s5–s10. doi: 10.1192/bjp.bp.112.119164. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorder: a review of the recent lilterature. Curr Opin Psychiatry. 2007;20:359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGorry PD, Purcell R, Goldstone S, Amminger GP. Age of onset and timing of treatment for mental and substance use disorders. Curr Opin Psychiatry. 2011;24:301–306. doi: 10.1097/YCO.0b013e3283477a09. [DOI] [PubMed] [Google Scholar]
- 7.Thyer BA, Parrish RT, Curtis GC, Nesse RM, Cameron OG. Ages of onset of DSM-III anxiety disorders. Compr Psychiatry. 1985;26:113–122. doi: 10.1016/0010-440x(85)90031-8. [DOI] [PubMed] [Google Scholar]
- 8.Argo T, Black DW. In: The characteristics of pathological gambling in Understanding and Treating Pathological Gambling. Grant J, Potenza M, editors. Washington DC: American Psychiatric Publishing Inc; 2004. pp. 39–53. [Google Scholar]
- 9.Tavares H, Martins SS, Lobo DSS, Silviera CM, Gentil V, Hodgins DC. Factors at play in faster progression for female pathological gamblers: an exploratory analysis. J Clin Psychiatry. 2003;64:433–438. doi: 10.4088/jcp.v64n0413. [DOI] [PubMed] [Google Scholar]
- 10.Jimenez-Murcia S, Alvarez-Moya EM, Stinchfield R, Fernandez-Arada F, Granero R, Aymami N, Gomez-Pena M, Juarrieta N, Bove F, Menchon JM. Age of onset of pathological gambling: clinical, therapeutic and personality correlates. J Gambl Stud. 2010;26:235–248. doi: 10.1007/s10899-009-9175-3. [DOI] [PubMed] [Google Scholar]
- 11.Teo P, Mythily S, Anantha S, Winslow M. Demographic and clinical features of 150 pathological gamblers referred to a community addictions programme. Ann Acad Med Singapore. 2007;36:165–168. [PubMed] [Google Scholar]
- 12.Black DW, Monahan P, Temkit M, Shaw M. A family study of pathological gambling. Psychiatry Res. 2006;141:295–303. doi: 10.1016/j.psychres.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Black DW, Shaw M, Forbush KT, Allen J. An open-label study of escitalopram in the treatment of pathological gambling. Clin Neuropharmacol. 2007;30:206–212. doi: 10.1097/wnf.0b013e31803d357f. [DOI] [PubMed] [Google Scholar]
- 14.Black DW, Arndt S, Coryell WH, Argo T, Forbush KT, Shaw M, Perry P, Allen J. Bupropion in the treatment of pathological gambling: a randomized, placebo-controlled, flexible-dose study. J Clin Psychopharmacol. 2007;27:143–150. doi: 10.1097/01.jcp.0000264985.25109.25. [DOI] [PubMed] [Google Scholar]
- 15.Grant J, Kim SW. Demographic and clinical features of 131 adult pathological gamblers. J Clin Psychiatry. 2001;62:957–962. doi: 10.4088/jcp.v62n1207. [DOI] [PubMed] [Google Scholar]
- 16.Grant JE, Potenza MN, Hollander E, Cunningham-Williams R, Nurminen T, Smits G, Kallio A. Multi-center investigation of the opioid antagonist nalmefene in the treatment of pathological gambling. Am J Psychiatry. 2006;163:303–312. doi: 10.1176/appi.ajp.163.2.303. [DOI] [PubMed] [Google Scholar]
- 17.Bland RC, Newman SC, Orn H, Stebelsky G. Epidemiology of pathological gambling in Edmonton. Can J Psychiatry. 1993;38:108–112. doi: 10.1177/070674379303800207. [DOI] [PubMed] [Google Scholar]
- 18.Blanco C, Hasin DS, Petry N, Stinson FS, Grant BF. Sex differences in subclinical and DSM-IV pathological gambling: results from the National Comorbidity Survey on Alcohol and Related Conditions. Psychol Med. 2006;36:943–953. doi: 10.1017/S0033291706007410. [DOI] [PubMed] [Google Scholar]
- 19.Kessler RC, Hwang I, LaBrie R, Petrukhova M, Sampson NA, Winters KC, Shaffer HJ. The prevalence and correlates of DSM-IV pathological gambling in the National Comorbidity Study Replication. Psychol Med. 2008;38:1351–1360. doi: 10.1017/S0033291708002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Black DW, Coryell WC, Crowe RR, McCormick B, Shaw M, Allen J. A direct, controlled, blind family study of pathological gambling. J Clin Psychiatry. 2014;75:215–221. doi: 10.4088/JCP.13m08566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lesieur HR, Blume SB. The South Oaks Gambling Screen (SOGS): A new instrument for identification of pathological gamblers. Am J Psychiatry. 1987;144:1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- 22.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 23.Leckman JF, Sholomska SD, Thompsen WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis - A methodologic study. Arch Gen Psychiatry. 1982;39:879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- 24.Spitzer RL, Williams JBW, Gibbons . Structured Clinical Interview for DSM-IV. New York: New York State Psychiatric Institute, Biometrics Research; 1994. [Google Scholar]
- 25.Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Arch Gen Psychiatry. 1977;34:1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- 26.Andreasen NC, Rice J, Endicott J, Reich T, Coryell W. The family history approach to diagnosis. Arch Gen Psychiatry. 1986;43:421–429. doi: 10.1001/archpsyc.1986.01800050019002. [DOI] [PubMed] [Google Scholar]
- 27.Christenson GA, Faber RJ, de Zwaan M, Raymond NC, Specker SM, Ekern MD, Mackenzie TB, Crosby RD, Crow SJ, Eckert ED. Compulsive buying: descriptive characteristics and psychiatric comorbidity. J Clin Psychiatry. 1994;55:5–11. [PubMed] [Google Scholar]
- 28.Sheehan D, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini International Neuropsychiatric Interview (MINI) J Clin Psychiatry. 1998;59 (suppl 20):22–33. [PubMed] [Google Scholar]
- 29.Pfohl B, Zimmerman M, Blum N. A Structured Interview for DSM-IV Personality Disorders (SIDP-IV) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 30.Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. The Temperament and Character Inventory (TCI) Center for the Psychobiology of Personality; St. Louis: 1994. [Google Scholar]
- 31.Barratt EE. Anxiety and impulsiveness related to psychomotor efficiency. Percept Motor Skills. 1959;9:191–198. [Google Scholar]
- 32.Khan SS, Secades-Villa R, Okuda M, Wang S, Pérez-Fuentes G, Kerridge BT, Blanco C. Gender differences in cannabis use disorders: results from the National Epidemiologic Survey of Alcohol and Related Conditions. Drug Alcohol Depend. 2013;130:101–108. doi: 10.1016/j.drugalcdep.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Markon KE, Krueger RF. Categorical and continuous models of liability to externalizing Disorders - a direct comparison in NESARC. Arch Gen Psychiatry. 2005;62:1352–1359. doi: 10.1001/archpsyc.62.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vizcaino EJV, Fernandez-Navarro P, Petry N, Rubio G, Blanco C. Differences between early-onset pathological gambling and later-onset gambling: data from the National Epidemiologic Survey on Alcohol and Related Disorders (NESARC) Addiction. 2013;109:807–813. doi: 10.1111/add.12461. [DOI] [PubMed] [Google Scholar]
- 35.Blaszczynski A, McConaghy N. Anxiety and/or depression in the pathogenesis of addictive gambling. Int J Addictions. 1989;24:337–350. doi: 10.3109/10826088909047292. [DOI] [PubMed] [Google Scholar]
- 36.Custer R. When Luck Runs Out. New York: Facts on File; 1985. [Google Scholar]
- 37.Blaszczynski A, Nower L. Pathways model of problem and pathological gambling. Addiction. 2002;97:487–499. doi: 10.1046/j.1360-0443.2002.00015.x. [DOI] [PubMed] [Google Scholar]
- 38.Ledgerwood DM, Petry NM. Subtyping pathological gamblers based on impulsivity, depression, and anxiety. Psychol Addict Behav. 2010;24:680–688. doi: 10.1037/a0019906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Slutske WS, Eisen S, Xian H, True WR, Lyons MJ, Goldberg J, Tsuang M. A twin study of the association between pathological gambling and antisocial personality disorder. J Abn Psychol. 2001;110:297–308. doi: 10.1037//0021-843x.110.2.297. [DOI] [PubMed] [Google Scholar]