Abstract
Objective
There is growing interest in the role of emotion regulation in anorexia nervosa (AN). Although anxiety is also hypothesized to impact symptoms of AN, little is known about how emotion regulation, anxiety, and eating disorder symptoms interact in AN. In this study, we examined the associations between emotion regulation, anxiety, and eating disorder symptom severity in AN.
Methods
Questionnaires and interviews assessing emotion regulation difficulties, anxiety, eating disorder symptoms, and eating disorder-related clinical impairment were collected from group of underweight individuals with AN (n = 59) at admission to inpatient treatment. Hierarchical linear regressions were used to examine the associations of emotion regulation difficulties, anxiety, and the interaction of these constructs with eating disorder symptoms and eating disorder-related clinical impairment.
Results
Emotion regulation difficulties were significantly positively associated with eating disorder symptoms and related clinical impairment only when anxiety levels were low and anxiety was significantly positively associated with eating disorder symptoms and related clinical impairment only when emotion regulation problems were not elevated.
Conclusions
This study adds to a growing literature suggesting that emotion regulation deficits are associated with eating disorder symptoms in AN. Certain individuals with AN may especially benefit from a focus on developing emotion regulation skills in the acute stages of illness.
Keywords: anorexia nervosa, eating disorder, emotion regulation, anxiety
1. Introduction
Despite recent advancements, the psychological processes associated with Anorexia Nervosa (AN) remain poorly understood and, therefore, effective treatments for the disorder continue to be ellusive1,2. Treatments developed out of traditional cognitive behavioral models of eating disorders have been demonstrated to be of limited efficacy in treating individuals with AN1,3. As such, within recent years researchers have been attempting to develop novel models by which to understand the phenomenology of AN.
One such model is that proposed by Haynos and Fruzzetti4, which posits the central role of emotion regulation deficits in AN. According to this model, individuals with AN experience deficits in the ability to identify, understand, and modulate emotions, which results in an experience of emotions as overwhelming or unmanageable. Consequently, individuals with AN rely on disordered eating to regulate their affective state by reducing negative affect and/or increasing positive affect. Thus, the model proposes that disordered eating is maintained through reinforcement associated with momentary alterations in emotional states. In line with this hypothesis, studies have found that individuals with AN have more difficulties with emotion regulation than healthy controls and similar emotion regulation difficulties as individuals with and mood, anxiety, and personality disorders 5–10. Studies using ecological momentary assessment have found that changes in negative affect frequently precede restrictive eating and excessive exercise for individuals with AN11, suggesting that these behaviors may function to manage aversive emotional experiences. Finally, research suggests that emotion regulation abilities do not significantly improve with traditional inpatient treatment for AN12 and that emotion regulation deficits following treatment for AN are associated with long-term perpetuation of disordered eating13, potentially explaining the failure of traditional cognitive behavioral treatments for AN.
Although there is growing evidence supporting the idea that emotion regulation difficulties affect eating disorder symptoms in AN, few studies have examined the relationship between emotion regulation and other putative processes related to AN. There is concurrently increasing interest in the role that anxiety plays in influencing AN symptomology14,15. It has been suggested that individuals who develop AN have elevated levels of anxiety resulting from a dysfunctional serotonin system, and that restrictive eating serves to reduce baseline levels of anxiety to a more manageable level16. Though there is considerable overlap between anxiety and emotion regulation models, anxiety models differ from that outlined by Haynos and Fruzzetti4 in two main ways: 1) They place primacy on anxiety as the sole (or main) problematic emotional experience in AN, rather than identifying a wide array of problematic emotional experiences as relevant to AN; 2) They place emphasis on an elevated baseline level of anxiety as the primary problem associated with disordered eating, while emotion regulation theories suggest the inability to effectively regulate emotion, rather than the emotion itself, as the primary concern.
The relationship between emotion regulation problems and anxiety among individuals with AN has rarely been explored; therefore, it is unclear how much emotion regulation difficulties contribute uniquely to eating disorder symptoms and clinical impairment caused by these symptoms, independent of anxiety concerns. One study found that both anxiety and emotion lability uniquely predicted eating disorder symptoms in an AN sample, however only emotion lability specifically predicted restrictive eating, suggesting an independent contribution of emotion regulation difficulties to disordered eating17. However, more research is needed to determine the degree to which emotion regulation difficulties exert influence on eating disorder severity that is not solely attributable to the impact of elevated baseline anxiety. Additionally, the interaction between anxiety and emotion regulation on eating disorder severity in AN has not been explored. Thus, it remains unclear whether these processes independently contribute to eating disorder pathology or whether they interact in nuanced ways to affect eating disorder symptoms (e.g., individuals with AN who have higher anxiety are more vulnerable to consequences of emotional dysregulation).
In this study we examined the association between emotion regulation, anxiety, and the interaction of these variables, with two indictors of eating disorder severity (i.e., eating disorder symptom severity and eating disorder-related clinical impairment) among individuals with AN. These associations were examined at admission to inpatient eating disorder treatment, at which time patients were in the acute stage of illness and underweight. The main hypotheses were as follows:
Emotion regulation difficulties would be significantly positively associated with eating disorder symptoms and clinical impairment, even after controlling for anxiety and relevant covariates.
There would be an additive effect of emotion regulation difficulties and anxiety on eating disorder symptoms and clinical impairment. High levels of both emotion regulation difficulties and anxiety would be associated with the greatest problem severity, while low levels of both would be associated with the lowest problem severity.
Emotion regulation difficulties would moderate the relationship between anxiety and eating disorder symptoms and clinical impairment. Anxiety would have a significant positive association with eating disorder symptoms and impairment when emotion regulation difficulties were elevated, but not when emotion regulation concerns were lower. It was theorized that poor emotion regulation would make individuals with AN more vulnerable to the impact of anxiety on eating disorder severity4.
2. Methods
2.1 Participants
Participants were individuals with AN ≥ 18 years old (n = 63) consecutively admitted to an inpatient eating disorder treatment program over a three-year period. A power analysis conducted using G-Power software18 was conducted to determine whether this sample size was adequate, assuming an alpha level of 0.05 and sufficient power (80%) to detect a large effect size (f2 = 0.35) with seven predictor variables. Power analysis suggested that the sample size in this study (n = 64) exceeded the minimum suggested sample size (n = 49). Diagnosis of AN was established by the Structured Clinical Interview for DSM-IV (SCID-I)19. Participants completed questionnaires at inpatient admission. Procedures were approved by an institutional review board and participants provided informed consent for the use of assessment data for research purposes.
2.2 Measures
2.2.1 Independent variables
The Difficulties in Emotion Regulation Scale (DERS)20 was used to examine problems with emotion regulation. The DERS is a 36-item scale developed to assess multiple facets of emotion regulation, including abilities to identify, differentiate, and accept emotional experiences, engage in goal-directed behavior and inhibit impulsive behavior in the context of negative emotion, and use effective emotion modulation strategies. Total scores range from 36 to 180. There are no standardized clinical cutoffs for this measure, however prior research suggests that the clinical range on the DERS total score varies from averages of approximately 80 to 1278,21. The DERS has been shown to have high internal consistency and test-retest reliability, and good predictive and construct validity20.
The Beck Anxiety Inventory (BAI)22 was used to capture cognitive and somatic symptoms of anxiety. BAI total scores range from 0 to 63. The following clinical cutoffs have been established for the BAI: 0–7 (minimal anxiety), 8–15 (mild anxiety), 16–25 (moderate anxiety), 26+ (severe anxiety). The psychometrics of the BAI are well established22.
2.2.2 Dependent variables
The Eating Disorder Examination, Edition 16.0D (EDE)23 was used to measure eating disorder symptoms. This interview assesses eating disorder symptoms primarily over the past month, and includes the following subscales: 1) Restraint subscale (attempts to restrict eating); 2) Eating Concern subscale (eating preoccupations and concerns); 3) Shape Concern subscale (distress regarding body shape); 4) Weight Concern subscale (distress regarding body weight). The average of these subscales forms a Global EDE score, which we used as an outcome variable in this study. Higher scores represent greater eating disorder severity. The EDE is considered the gold-standard assessment for disordered eating and the psychometrics of this measure are well-established.23
The Clinical Impairment Assessment (CIA)24 was created to assess the severity of functional impairment due to eating disorder symptoms along domains of mood, self-perception, interpersonal relationships, and work functioning. The CIA is a 16-item questionnaire measure, with total scores ranging from 0 to 48, such that higher scores reflect greater impairment. A score of 16 is considered the clinical cutoff for eating disorder status. Though the CIA is a newer measure, a recent study suggests that the CIA is a reliable and valid measure of eating disorder related clinical impairment25.
2.2.3 Covariates
Covariates included patients’ self-reported age, BMI (calculated from measured height and weight at admission), diagnostic subtype (i.e., restricting or binge eating/purging subtype) obtained by the SCID-I 19 and the Beck Depression Inventory-II (BDI-II)26. The BDI-II is a 21-item measure, with higher scores indicating higher depression severity. The psychometrics of the BDI-II are well established 26.
2.3 Data analysis
Two hierarchical linear regressions were conducted. For both dependent variables (EDE global score and CIA score), the regression model building steps were as follows:
First step: DERS and BAI score as predictors
Second step: DERS, BAI scores, and DERS x BAI interaction as predictors
Third step: DERS, BAI scores, DERS x BAI interaction, and covariates (age, BMI, diagnostic subtype, and BDI-II scores) as predictors
Simple slope analyses were used to further understand the nature of the interaction effects between DERS x BAI on EDE and CIA scores. This was done by rerunning the regressions as described above with scores for the DERS and BAI that were calculated at one standard deviation above and below the mean scores, and examining the effects of high and low levels of one variable (e.g., DERS score) on the significance and effect size of the association between the other variable (e.g., BAI score) and the dependent variables. This allowed more thorough characterization of the relationship between the independent variables in their association with the dependent variables without altering the original regression equations. At admission, DERS high and low cutoffs were 87.69 and 138.03 respectively and BAI high and low cutoffs were 12.97 and 34.69.
Assumptions regarding linearity, independence of errors, and homoscedasticity were met for all linear regressions. All predictor variables were centered to reduce multicollinearity. Four multivariate outliers were identified based on the criteria of at least two of the following: standardized residual score > 3, Cook’s distance above critical cutoff according to standard calculations, and leverage values above the critical cutoff according to standard calculations. Outliers were removed listwise, resulting in a final sample of n = 59.
3. Results
3.1 Participants
The sample was 97% female with an average age of 25.88 (SD = 6.35) years, and an average BMI of 15.87 (SD = 1.47) kg/m2. Forty-one percent were diagnosed with AN-R. DERS and BAI scores were moderately positively correlated, r(59) = .534, p < .001.
3.2 Eating Disorder Symptoms
Regression results are summarized in Table 1. In the first model, including both emotion regulation and anxiety as predictors of eating disorder symptoms, the DERS was the only significant predictor, with greater emotion regulation problems associated with more eating disorder symptoms. However, in the final model that included covariates and the DERS x BAI interaction term, DERS scores were no longer significantly associated with eating disorder symptoms, but the DERS x BAI interaction was a significant predictor of eating disorder symptoms.
Table 1.
Results of regression analyses predicting Eating Disorder Examination (EDE) global scores and Clinical Impairment Assessment (CIA) scores among underweight individuals with anorexia nervosa at inpatient admission (n =59)
| Dependent variable | Step/independent variables | R2 adjusted | R2 change | F change | p | β | SE | |
|---|---|---|---|---|---|---|---|---|
| EDE global score | Step 1 | 0.173 | 0.201 | 7.064 | 0.002* | |||
| DERS | 0.014* | 0.345 | 0.007 | |||||
| BAI | 0.227 | 0.166 | 0.015 | |||||
|
| ||||||||
| Step 2 | 0.239 | 0.077 | 5.883 | 0.019* | ||||
| DERS | 0.008* | 0.359 | 0.006 | |||||
| BAI | 0.157 | 0.188 | 0.015 | |||||
| BAI x DERS interaction | 0.019* | −0.280 | 0.001 | |||||
|
| ||||||||
| Step 3 | 0.304 | 0.109 | 2.275 | 0.079 | ||||
| DERS | 0.158 | 0.201 | 0.007 | |||||
| BAI | 0.323 | 0.140 | 0.016 | |||||
| BAI x DERS interaction | 0.032* | −0.248 | 0.001 | |||||
| Age | 0.353 | −0.115 | 1.483 | |||||
| Body Mass Index | 0.148 | 0.167 | 0.094 | |||||
| Subtype | 0.026* | 0.290 | 0.310 | |||||
| BDI-II | 0.277 | 0.163 | 0.017 | |||||
|
| ||||||||
| CIA score | Step 1 | 0.258 | 0.284 | 11.091 | <0.001* | |||
| DERS | 0.001* | 0.433 | 0.035 | |||||
| BAI | 0.204 | 0.166 | 0.080 | |||||
|
| ||||||||
| Step 2 | 0.332 | 0.083 | 7.200 | 0.010* | ||||
| DERS | 0.001* | 0.448 | 0.033 | |||||
| BAI | 0.131 | 0.188 | 0.076 | |||||
| BAI x DERS interaction | 0.010* | −0.290 | 0.003 | |||||
|
| ||||||||
| Step 3 | 0.286 | 0.006 | 0.113 | 0.978 | ||||
| DERS | 0.002* | 0.454 | 0.038 | |||||
| BAI | 0.189 | 0.189 | 0.088 | |||||
| BAI x DERS interaction | 0.016* | −0.283 | 0.003 | |||||
| Age | 0.550 | 0.075 | 8.374 | |||||
| Body Mass Index | 0.828 | 0.025 | 0.529 | |||||
| Subtype | 0.637 | −0.061 | 1.749 | |||||
| BDI-II | 0.954 | 0.009 | 0.097 | |||||
denotes significance at p < .05
Note: DERS = Difficulties in Emotion Regulation Scale; BAI = Beck Anxiety Inventory; BDI-II = Beck Depression Inventory-Second Edition; Subtype reference group = AN restricting subtype
To understand the nature of this DERS x BAI interaction on eating disorder symptoms, simple slope analyses were conducted. As highlighted in Figure 1, DERS scores were significantly positively associated with EDE scores when anxiety levels were low (β = .453, SE = .009, p = .021), but not when anxiety was high (β = −.052, SE = .008, p = .764). Similarly, BAI scores were significantly positively related to EDE scores when emotion regulation problems were low (β = .392, SE = .021, p = .043), but not when emotion regulation concerns were high (β = −.112, SE = .019, p = .518).
Figure 1.
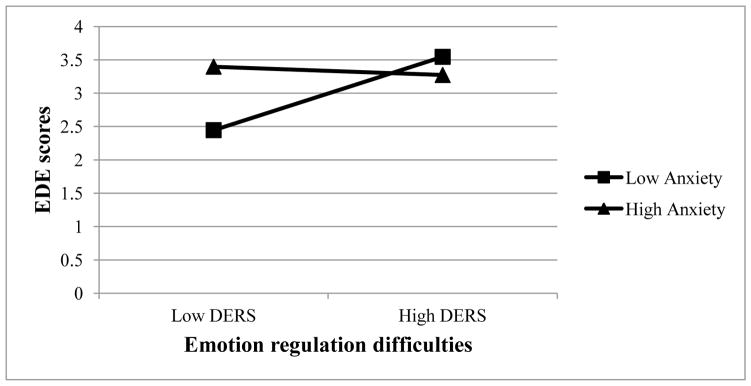
Interaction effect between Difficulty in Emotion Regulation Scale (DERS) and Beck Anxiety Inventory (BAI) scores on Eating Disorder Examination (EDE) global scores among individuals with anorexia nervosa (n = 59)
3.3 Eating Disorder-Related Clinical Impairment
In the first model including both emotion regulation and anxiety as predictors of clinical impairment, only the DERS was a significant predictor, such that greater emotion regulation problems were associated with more clinical impairment from eating disorder symptoms. However, after adding the DERS x BAI interaction term to the model, both the DERS and the interaction term were significantly associated with clinical impairment. This finding held after controlling for covariates.
To further characterize the nature of the DERS x BAI interaction on clinical impairment, simple slope analyses were conducted. As highlighted in Figure 2, we found the same pattern of findings with the CIA as with the EDE. At admission, DERS scores were significantly positively related to eating disorder-related clinical impairment when anxiety levels were low (β = .742, SE = .052, p < .001), but not when anxiety was high (β = .166, SE = .047, p = .342), and BAI scores were significantly positively related to CIA scores when emotion regulation problems were low (β = .476, SE = .119, p = .016), but not high, (β = −.099, SE = .109, p = .573).
Figure 2.
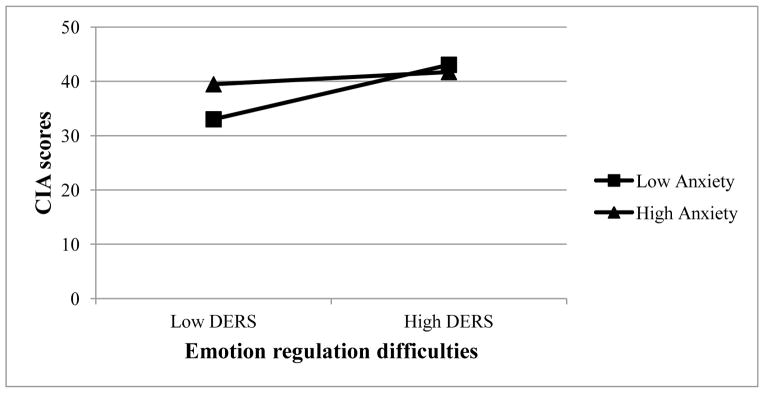
Interaction effect between Difficulty in Emotion Regulation Scale (DERS) and Beck Anxiety Inventory (BAI) scores on Clinical Impairment Assessment (CIA) scores among individuals with anorexia nervosa (n = 59)
In sum, the simple slope analyses suggest that emotion regulation difficulties were associated with eating disorder symptoms and related clinical impairment only when anxiety was low and anxiety symptoms were only associated with eating disorder symptoms and clinical impairment when emotion regulation difficulties were not elevated.
4. Discussion
In this study, we examined the relationship between emotion regulation difficulties, anxiety, and eating disorder symptom severity and eating disorder-related clinical impairment among underweight inpatients with AN. In line with hypotheses, emotion regulation concerns were significantly associated with eating disorder symptoms and clinical impairment, even after accounting for anxiety and other relevant covariates. However, the moderation effect of emotion regulation on the relationship between anxiety and eating disorder severity was different than anticipated. Greater difficulty regulating emotions was significantly associated with greater eating disorder symptoms and clinical impairment only when symptoms of anxiety were milder. Similarly, higher anxiety was only significantly associated with greater eating disorder symptoms and clinical impairment when emotion regulation problems were lesser. This suggests that anxiety and emotion regulation have independent associations with eating disorder symptoms and clinical impairment during the acute phase of the illness.
There are two important implications of these findings. First, these findings suggest that emotion regulation problems are not simply secondary to anxiety in AN and, therefore, emotion regulation difficulties are independently related to on eating disorder symptoms and impairment during acute stages of AN. In fact, in the regression models in this study, emotion regulation concerns were more strongly associated with eating disorder severity compared to anxiety, suggesting that emotion regulation difficulties may be particularly relevant to eating disorder symptoms and clinical impairment in acute stages of illness.
Second, these findings suggest that theories positing the importance of emotion regulation4, as well as those emphasizing anxiety14,15, during acute stages of AN are likely both valid, but may be identifying two different processes that may be associated with symptom expression among underweight individuals with AN. The data indicate that in the acute stages of AN, problems appropriately managing emotions may be more highly associated with eating disorder symptoms and impairment for some individuals, while high, but stable levels of anxiety may be more highly associated with eating disorder behavior for others. This suggests a potential benefit of assessing patients’ emotion regulation abilities and anxiety levels when presenting to treatment in order to tailor treatment to focus on either emotion regulation strategies or reducing/tolerating anxiety, depending on which seems more elevated for a particular patient.
This study has several strengths. The sample was entirely underweight and acutely ill, and therefore more likely to accurately capture the phenomenology of AN, as compared to less acute samples. Further, we investigated theory-based models using gold-standard assessment instruments, allowing for greater clarity regarding putative processes involved in AN. However, the study must also be considered in the context of its limitations. Though the assessments used in this study are well validated and widely used, they relied heavily on self-report, which can introduce biases. Further, because all measures were collected at the same time, we cannot assume directionality of associations detected in this study. Finally, because the sample consisted of acutely ill adult inpatients, it remains unclear whether these results would generalize to adolescent, outpatient, or less acute samples. Therefore, future studies ought to investigate the relationship between emotion regulation deficits, anxiety, and eating disorder and other clinical symptoms across multiple assessment points and patient groups, and using diverse assessment tools.
5. Conclusions
There is a growing interest in targeting emotion regulation difficulties in the treatment of AN27,28. The results of this study suggest that a treatment focus on enhancing emotion regulation abilities is likely be beneficial to at least some individuals with AN during illness. More research is needed to further understand the independent roles anxiety and emotion regulation play in the maintenance of eating disorder symptoms and to identify whether there are subtypes of individuals with AN who are most likely to benefit from an emotion regulation focus in treatment.
Acknowledgments
Research reported in this publication was partially supported by a pre-doctoral training fellowship awarded to Ann Haynos by the National Institute of Mental Health under Award Number F31MH097450. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Berkman ND, Bulik CM, Brownley KA, et al. Management of eating disorders. Evid Rep Technol Assess (Full Rep) 2006;(135):1–166. [PMC free article] [PubMed] [Google Scholar]
- 2.Walsh BT. The enigmatic persistence of anorexia nervosa. Am J Psychiatry. 2013;170(5):477–84. doi: 10.1176/appi.ajp.2012.12081074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Attia E. Anorexia nervosa: current status and future directions. Annu Rev Med. 2010;61:425–35. doi: 10.1146/annurev.med.050208.200745. [DOI] [PubMed] [Google Scholar]
- 4.Haynos AF, Fruzzetti AE. Anorexia nervosa as a disorder of emotion dysregulation: Theory, evidence, and treatment implications. Clinical Psychology Science and Practice. 2011;18:183–202. [Google Scholar]
- 5.Brockmeyer T, Bents H, Holtforth MG, Pfeiffer N, Herzog W, Friederich HC. Specific emotion regulation impairments in major depression and anorexia nervosa. Psychiatry Res. 2012;200(2–3):550–3. doi: 10.1016/j.psychres.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Brockmeyer T, Holtforth MG, Bents H, Kämmerer A, Herzog W, Friederich HC. Starvation and emotion regulation in anorexia nervosa. Compr Psychiatry. 2012;53(5):496–501. doi: 10.1016/j.comppsych.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Harrison A, Sullivan S, Tchanturia K, Treasure J. Emotion recognition and regulation in anorexia nervosa. Clin Psychol Psychother. 2009;16(4):348–56. doi: 10.1002/cpp.628. [DOI] [PubMed] [Google Scholar]
- 8.Harrison A, Sullivan S, Tchanturia K, Treasure J. Emotional functioning in eating disorders: attentional bias, emotion recognition and emotion regulation. Psychol Med. 2010;40(11):1887–97. doi: 10.1017/S0033291710000036. [DOI] [PubMed] [Google Scholar]
- 9.Harrison A, Tchanturia K, Treasure J. Attentional bias, emotion recognition, and emotion regulation in anorexia: state or trait? Biol Psychiatry. 2010;68(8):755–61. doi: 10.1016/j.biopsych.2010.04.037. [DOI] [PubMed] [Google Scholar]
- 10.Svaldi J, Griepenstroh J, Tuschen-Caffier B, Ehring T. Emotion regulation deficits in eating disorders: a marker of eating pathology or general psychopathology? Psychiatry Res. 2012;197(1–2):103–11. doi: 10.1016/j.psychres.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Engel SG, Wonderlich SA, Crosby RD, et al. The role of affect in the maintenance of anorexia nervosa: evidence from a naturalistic assessment of momentary behaviors and emotion. J Abnorm Psychol. 2013;122(3):709–19. doi: 10.1037/a0034010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haynos AF, Roberto CA, Martinez MA, Attia E, Fruzzetti AE. Emotion regulation difficulties in anorexia nervosa before and after inpatient weight restoration. Int J Eat Disord. 2014 doi: 10.1002/eat.22265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Racine SE, Wildes JE. Dynamic Longitudinal Relations Between Emotion Regulation Difficulties and Anorexia Nervosa Symptoms Over the Year Following Intensive Treatment. J Consult Clin Psychol. 2014 doi: 10.1037/ccp0000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the application of exposure and response prevention to the treatment of anorexia nervosa. Int J Eat Disord. 2011;44(2):134–41. doi: 10.1002/eat.20784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strober M. Pathologic fear conditioning and anorexia nervosa: on the search for novel paradigms. Int J Eat Disord. 2004;35(4):504–8. doi: 10.1002/eat.20029. [DOI] [PubMed] [Google Scholar]
- 16.Kaye WH, Barbarich NC, Putnam K, et al. Anxiolytic effects of acute tryptophan depletion in anorexia nervosa. Int J Eat Disord. 2003;33(3):257–67. doi: 10.1002/eat.10135. discussion 68–70. [DOI] [PubMed] [Google Scholar]
- 17.Lavender JM, De Young KP, Anestis MD, et al. Associations between retrospective versus ecological momentary assessment measures of emotion and eating disorder symptoms in anorexia nervosa. J Psychiatr Res. 2013;47(10):1514–20. doi: 10.1016/j.jpsychires.2013.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3. 1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–60. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 19.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis-1 Disorders, Research Version, Patient Edition with Psychotic Screen. New York, NY: Biometrics Research, New York State Psychiatric Institute; 1996. [Google Scholar]
- 20.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavior Assessment. 2006;26:41–54. [Google Scholar]
- 21.Staples AM, Mohlman J. Psychometric properties of the GAD-Q-IV and DERS in older, community-dwelling GAD patients and controls. J Anxiety Disord. 2012;26(3):385–92. doi: 10.1016/j.janxdis.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–7. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 23.Fairburn CG, Cooper Z, O’Connor M. The Eating Disorder Examination, 16th edition. In: Fairburn CG, editor. Cognitive Behavior Therapy and Eating Disorders. New York, NY: Guilford Press; 2008. [Google Scholar]
- 24.Bohn K, Doll HA, Cooper Z, O’Connor M, Palmer RL, Fairburn CG. The measurement of impairment due to eating disorder psychopathology. Behav Res Ther. 2008;46(10):1105–10. doi: 10.1016/j.brat.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jenkins PE. Psychometric validation of the Clinical Impairment Assessment in a UK eating disorder service. Eat Behav. 2013;14(2):241–3. doi: 10.1016/j.eatbeh.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 26.Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–97. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 27.Wildes JE, Marcus MD. Development of emotion acceptance behavior therapy for anorexia nervosa: a case series. Int J Eat Disord. 2011;44(5):421–7. doi: 10.1002/eat.20826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lynch TR, Gray KL, Hempel RJ, Titley M, Chen EY, O’Mahen HA. Radically open-dialectical behavior therapy for adult anorexia nervosa: feasibility and outcomes from an inpatient program. BMC Psychiatry. 2013;13:293. doi: 10.1186/1471-244X-13-293. [DOI] [PMC free article] [PubMed] [Google Scholar]


