Abstract
The perforation size affects the success of tympanic membrane (TM) reconstruction, in addition to the surgical technique used. Large TM perforations present a surgical challenge. The perforation size has been reported to be a prognostic factor, and poorer results are obtained with large versus small perforations. We aimed to evaluate patients who had undergone tympanoplasty for large perforations at our clinic using either the underlay or over-underlay technique and to compare the results in terms of re-perforation, retraction, lateralization, and improvement of hearing. Of 302 patients with chronic otitis media, 114 who had a perforation that involved over 50 % of the pars tensa were enrolled in the study. The underlay technique was used in 61 patients, and the over-underlay technique in 53 patients. In the underlay group, the preoperative mean perforation size was 30.11 ± 5.35 mm2 (range 20.00–52.00 mm2) (n = 61). In the over-underlay group, the preoperative mean perforation size was 31.41 ± 8.65 mm2 (range 22.00–48.00 mm2) (n = 53). The graft success rate of tympanoplasty performed using the underlay technique was 89.1 % in 61 patients. Seven (10.9 %) patients had graft failure. The graft success rate with the over-underlay technique in 53 patients was 90.5 %. Five (9.5 %) patients had graft failure in this group. Three graft lateralizations (5.6 %) and two retractions (3.8 %) were observed at 12 months postoperatively in the over-underlay group. However, in the underlay group, no graft lateralization but five retractions (8.2 %) were observed at 12 months. The graft-take rates and hearing improvement results in both groups were successful and compatible with those in the literature.
Keywords: Underlay tympanoplasty, Over-underlay tympanoplasty, Large perforation
Introduction
Tympanic membrane (TM) perforation is usually a consequence of chronic ear disease, trauma, or iatrogenic effects following surgical treatment [1]. For surgical repair of TM perforation, myringoplasty is usually proposed. The myringoplasty procedure is now one of the most common performed method on the ear. In TM reconstruction, two aims should be fulfilled. The first aim is the closure of the perforation, and the second aim is to obtain a new TM with acoustic qualities similar to those of a normal TM [2].
Two classic methods for the reconstruction of a TM perforation have been used: the underlay or overlay graft techniques. Each of these approaches and techniques has its advantages and disadvantages [3, 4]. The underlay technique is perhaps more commonly used worldwide; this technique is easier to perform and less time consuming. In this technique, the graft is placed medial to the entire TM remnant and also to the malleus handle and is more suitable for posterior perforations [5]. This technique has disadvantages, including a decreased mesotympanic space, medial displacement of the graft and lower success rate in subtotal and anterior perforations. Additionally, the technique has a lower risk for lateralization, and a more acceptable success rate, even in the hands of less-experienced surgeons [6]. In the overlay technique, after the elevation of squamous tissue, the graft is positioned lateral to the annulus and fibrotic layer of the TM residue. The overlay technique avoids this pitfall, but there is a risk of graft lateralization, anterior blunting, delayed healing, stenosis of the external canal, epithelial pearls, and iatrogenic cholesteatoma. Despite its higher success in repairing anterior and subtotal perforations, there is a consensus concerning the overlay technique being more technically challenging [7].
Various other techniques of TM repair have been described. The term ‘sandwich technique’ was coined by Farrior in 1983 to describe a method in which sheets of temporalis fascia were placed medial and lateral to the drum, with the fibrous layer as the ‘meat’ in the ‘sandwich’ [8]. Raghavan et al. used the same term to describe a technique in which a pedicled skin flap is used to partially cover an overlay TM graft [9].
Tabb and Shea first innovated medial positioning of grafting tissue to the malleus and residue of TM [10, 11]. Kartush et al. used the over-underlay technique for the tympanoplasty procedure [12]. The perforation size is also a factor affecting the success of TM reconstruction besides the chosen surgical technique. Subtotal or total TM perforations present a surgical challenge. It has been reported that the perforation size is a prognostic factor, and poorer results are obtained with large versus small perforations [13]. These perforations are at a high risk of reperforation, retraction pockets and obligatory revision surgeries. These TM perforations are more difficult to treat because of less extensive TM margins to support graft survival and less tension to resist tympanic retraction postoperatively. Reasons for graft failure include graft displacement, improper placement, autolysis, infection, and Eustachian tube dysfunction [14].
In the present study, the tympanoplasty results of patients with chronic otitis media who have large central perforations and underwent the procedure at our clinic by the underlay or over-underlay technique were compared in terms of re-perforation, retraction, lateralization, and hearing improvement. The results were also compared with those reported previously.
Patients and Methods
Ethics Committee approval was obtained from our institute at 12.12.2014 with the file number of 12. This study was conducted at the mardin and kızıltepe State Hospitals otorhinolaryngology (ENT) clinics between February 2010 and June 2013, according to the principles of the Helsinki Declaration. No pharmaceutical companies funded the study or contributed to the study design, outcome evaluation or writing of this paper.
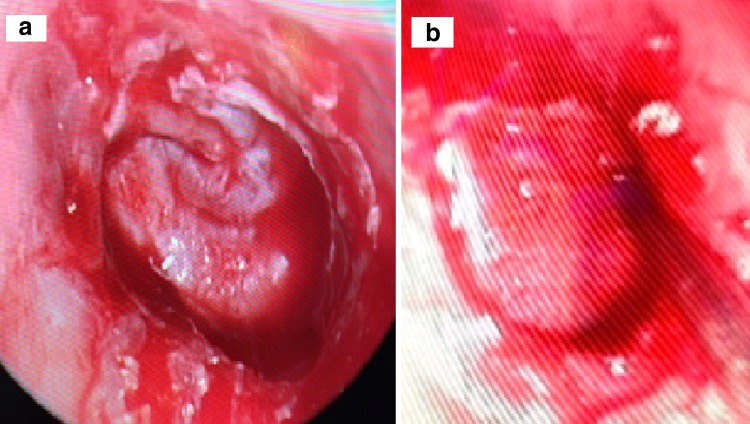
Of 302 patients with chronic otitis media, 114 who had a perforation that involved over 50 % of the TM were enrolled in the study. The measurement of perforation size was performed via otomicroscopic and endoscopic examination during the intraoperative period (Fig. 1a, b). Patients in whom cholesteatoma was identified during surgery and those with ossicular damage did not undergo follow up. Patients without any drainage from the ear were followed for at least 1 month before they underwent surgery. Chondroperichondrial cartilage grafts with a boomerang-shaped cartilage island at the anterior and inferior parts were used in all patients.
Fig. 1.
a Tympanic membrane with reference scale, b perforation zone shaded by the program
Surgical Technique
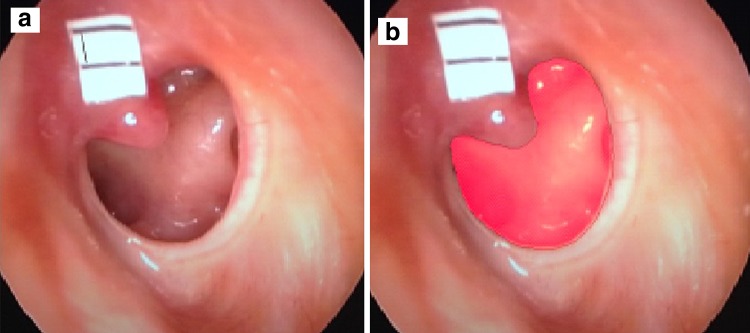
All patients were subjected to general anesthesia. A chondroperichondrial cartilage graft was removed from the tragal cartilage via a transcartilagenous incision. The lateral perichondrium was left in place. The graft was performed by endoscopic transcanal, endaural or postauricular incision. After slight incision of the perforation edges, the tympanomeatal flap was elevated. The ossicular system was found to be intact and mobile. A piece of gelfoam (Spongostan Standart; Ferrosan Inc., Copenhagen, Denmark) was placed in the posterior part of the middle ear and promontorium. The boomerang-shaped chondroperichondrial graft, including the cartilage support at the anterior and inferior part, was placed at the bottom of the manubrium mallei and annulus as an underlay graft (Fig. 2a). In patients who have undergone the over-underlay technique, we placed the graft under the annulus and over the manubrium mallei (Fig. 2b). The tympanomeatal flap was spread and then externally supported by gelfoam. The remaining cartilage was placed into the tragal area and sutured into place. Patients were examined via otomicroscopy at 1, 6 and 12 months postoperatively. Audiometric tests were performed. Patients were evaluated postoperatively in terms of perforation, graft lateralization, odiologic results (ABG, AC, BC) and graft retraction. The measurement of perforation size during surgery and postoperative audiometric data are presented according to the criteria of the American National Standards Institute (ANSI-1969) [15]. Pure-tone audiometry tests (0.25–8.0 kHz) of air and bone hearing levels (dB SPL) were performed. Pure-tone averages (PTAs) were calculated by averaging the hearing thresholds for 0.5, 1.0 and 2.0 kHz. Preoperative and postoperative ABGs were also calculated according to the PTAs of the patients.
Fig. 2.
a The view of the graft placed underlay, b the view of the graft placed over-underlay
Measurement of the Perforation Size
The TM of the patients were evaluated with 0 degree 4 mm endoscopic intraoperatively. Perforated TM were photographed with a scale located on it for reference length. These photographs were uploaded to universaldesktop ruler 3, 6 program which is created by AVPsoft. The perforation size were calculated in mm [2] by using this program. (Fig. 1a, b).
Statistical analysis
Medial, standard deviation, median, the lowest, the highest, frequency and rate values were used in descriptive statistics of datas. For qualitative data analysis, Chi square test and if it did not provide the condition fischer test was used. The distribution of the variables were measured with kolmogorov–smirnov test. Mann–whitney U test was used for analysis of quantitative datas while Wilcoxon test were used on repeating measurement analysis. SPSS 22.0 was used for statistical analysis.
Results
The underlay technique was used in 61 patients, and the over-underlay technique in 53 patients. The patients’ ages ranged from 14 to 61 years, with an average age of 29.40 ± 10.14 years. Sixty-seven patients (58 %) were female, and 47 (42 %) were male. The mean follow-up period was 19 months (range: 12–36 months).
The measurement of perforation size during surgery and the postoperative period was performed via otomicroscopic and endoscopic examination. The preoperative and postoperative (at month 12) perforation sizes are shown in Table 1. In the underlay group, the preoperative mean perforation size was 30.11 ± 5.35 mm2 (range: 20.00–52.00 mm2) (n = 61). In the over-underlay group, the mean preoperative perforation size was 31.41 ± 8.65 mm2 (range: 22.00–48.00 mm2) (n = 53).
Table 1.
Pre and postoperative perforation size
| Preoperative | Postoperative | |||
|---|---|---|---|---|
| Perforation size | Perforation size | |||
| n | Mean ± SD | n | Mean ± SD | |
| Underlay group | 61 | 30.11 ± 5.35 | 7 | 6.00 ± 3.13 |
| Over-underlay group | 53 | 31.41 ± 8.65 | 5 | 5.00 ± 5.15 |
At postoperative month 12 (Table 1), in the underlay group, the mean perforation size was 6.00 ± 3.13 mm2 (range: 3.00–9.00 mm2) (n = 8); in the over-underlay group, the postoperative mean perforation size was 5.00 ± 5.15 mm2 (range 2.00–9.00 mm2) (n = 6).
At the 12-month follow up, in the underlay group (n = 61), the graft success rate was 89.1 % (there were seven graft failures). There were five graft failures in the over-underlay group (n = 53) (the success rate was 90.5 %). Perforations were observed at the central (two patients), anterior (four patients) and posterosuperior (one patients) quadrants of the TM in the underlay group. In the over-underlay group, perforations were observed at the central (two patients) and anterior (three patients) quadrants of the TM. During the first year of use, the underlay tympanoplasty didn’t detect graft lateralization in any of the patients; however, lateralization was observed in three patients in the over-underlay group. In patients who still had hearing loss but an intact graft at 6 months postoperatively, revision surgery was performed, and the graft was placed using the underlay technique. At the same time, in two of these three patients, central-placed cholesteatoma was detected during revision surgery. Retraction was observed in five patients with the underlay technique and in two patients with the over-underlay technique. Retractions were localized to the posterosuperior quadrant (three patients) and central quadrant (two patients) of the TM in the underlay group. In the over-underlay group, two retractions were observed in the central (one patient) and anterior (one patient) quadrants of the TM. Retractions were of grade 1 according to the Sade classification [16].
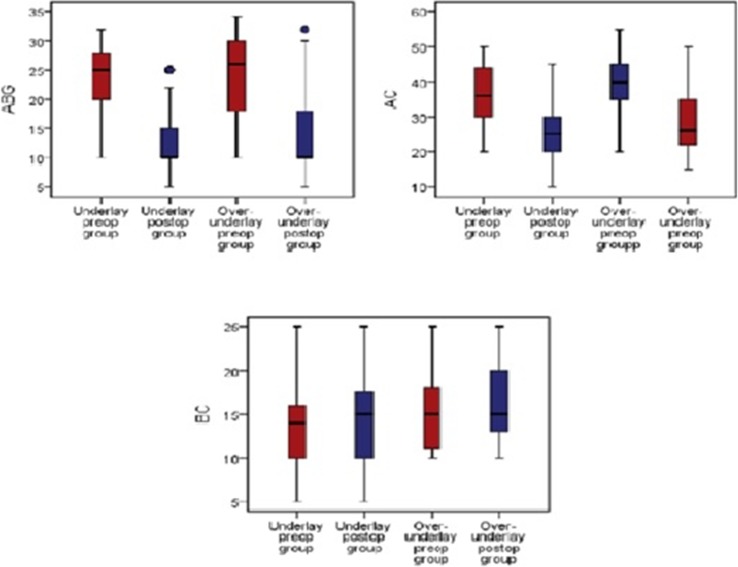
The mean preoperative average ABG was 23.8 ± 5.0 dB HL, the BC pure-tone average (PTA) was 13.5 ± 4.5 dB hearing level (HL), and air conduction (AC) PTA was 36.9 ± 7.2 dB HL in the underlay group. The postoperative 12-month bone conduction (BC) PTA was 13.9 ± 4.7 dB HL, the AC PTA was 26.8 ± 8.0 dB HL, and the ABG was 12.1 ± 5.5 dB HL. There was a statistically significant improvement in the mean ABG and PTA after surgery (p < 0.05).
In the over-underlay group, the mean preoperative average ABG was 24.3 ± 6.9 dB HL, the BC PTA was 14.7 ± 3.8 dB HL, and the mean AC PTA was 39.5 ± 7.8 dB HL. The postoperative 12-month average ABG was 13.3 ± 6.4 dB HL, the BC PTA was 15.8 ± 3.8 dB HL, and the AC PTA was 29.2 ± 8.3 dB HL. There was a statistically significant improvement in the mean ABG and PTA after surgery (p < 0.05). There were no cases of profound hearing loss.
No statistically significant difference was detected between the underlay and over-underlay groups with respect to re-perforation, graft success, lateralization and retractions (p > 0.05; Table 2). There was no statistically significant difference between the underlay and over-underlay groups regarding the ABG and PTA results (p > 0.05; Table 3).
Table 2.
Graft status of the groups
| Underlay group | Over-underlay group | p | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Graft | Intact | 54 | 89.1 | 48 | 90.5 | 0.656 |
| Perforated | 7 | 10.9 | 5 | 9.5 | ||
| Medialization | + | 5 | 8.2 | 2 | 3.8 | 0.624 |
| − | 56 | 91.8 | 60 | 97.2 | ||
| Lateralization | + | 0 | 0.0 | 3 | 5.6 | 0.051 |
| − | 61 | 100.0 | 50 | 94.4 | ||
Table 3.
Pre-post operative audiological results
| Underlay group | Over-underlay group | p | ||||
|---|---|---|---|---|---|---|
| Ort. ± s.s. | Med (Min−Mak) | Ort. ± s.s. | Med (Min−Mak) | |||
| ABG | Preop | 23.8 ± 5.0 | 25.0 (10.0−32.0) | 24.3 ± 6.9 | 26.0 (10.0−34.0) | 0.256 |
| Postop | 12.1 ± 5.5 | 10.0 (5.0−25.0) | 13.3 ± 6.4 | 10.0 (5.0−32.0) | 0.225 | |
| Preop/Postop change | −11.7 ± 4.6 | −12.0 (−21.0−0.0) | −11.1 ± 6.3 | −10.0 (−23.0−0.0) | 0.422 | |
| Change p | 0.000 | 0.000 | ||||
| BC | Preop | 13.5± 4.5 | 14.0 (5.0−25.0) | 14.7 ± 3.8 | 15.0 (10.0−25.0) | 0.099 |
| Postop | 13.9 ± 4.7 | 15.0 (5.0−25.0 | 15.8 ± 3.8 | 15.0 (10.0−25.0) | 0.013 | |
| Preop/Postop change | 0.4 ± 1.6 | 0.0 (−3.0−5.0) | 1.1 ± 2.0 | 0.0 (−3.0−6.0) | 0.045 | |
| Change p | 0.016 | 0.000 | ||||
| AC | Preop | 36.9 ± 7.2 | 36.0 (20.0−50.0) | 39.5 ± 7.8 | 40.0 (20.0−55.0) | 0.051 |
| Postop | 26.8 ± 8.0 | 25.0 (10.0−45.0) | 29.2 ± 8.3 | 26.0 (15.0−50.0) | 0.118 | |
| Preop/Postop change | −10.1 ± 5.4 | −10.0 (−25.0−2.0) | −10.3 ± 7.1 | −10.0 (−25.0−10.0) | 0.706 | |
| Change p | 0.000 | 0.000 | ||||
Mann–whitney U test/Wilcoxon test
Bold values indicate p < 0.05 accepted as significant
Discussion
Repair of TM defects aims to achieve anatomic and functional success and to maintain these properties over time. However, in the case of larger TM defects, healing has a much poorer prognosis and because of the increased technical difficulty and area that must be vascularized and epithelialized with larger perforations, surgical failures are not unexpected. The absence of an adequate residual TM in subtotal or total TM perforations remains a challenge to otolaryngologists [17]. Various techniques have been used to successfully repair TM perforations. The underlay and overlay procedures are presently the two most widely used techniques. Today, the underlay procedure is preferred over the overlay procedure because of the risk of blunting coupled with the greater time and complexity needed for the latter technique. The over-underlay tympanoplasty is a combination of the underlay and overlay techniques. This technique places the graft under the remaining drum and lateral to the malleus and has been developed to minimize the disadvantages inherent in the other two techniques. This may explain why the over-underlay procedure is becoming widespread as a means of TM repair [12].
For many years, myringoplasties have been performed using the over-underlay technique. However, after observing graft lateralization, we are currently performing mostly the underlay technique. Additionally, we have been performing techniques that have been reported in the literature, considering the size and location of the perforation. Several research articles concerning the two techniques mentioned above have been published [3, 7].
It is often reported that the repair of large perforations is less successful than that of smaller perforations because it is technically more difficult [13, 14]. Karela reported on a series of 211 patients who underwent underlay myringoplasty for perforations of any size and site, achieving a 91.5 % success rate and a 14.67-dB mean improvement in hearing function in 91.5 % of the patients. These authors stated that myringoplasty can improve hearing independent of the site and size of perforation, and suggest that the hearing improvement can be used as an indication for myringoplasty [18]. Angeli et al. reported that the lateral technique effectively addresses the largest possible eardrum defects, resulting in an intact neotympanum and an aerated middle ear in 91 % of cases [19]. Jung and Parks, using a mediolateral graft method to repair subtotal and anterior perforations, demonstrated 97 % ear drum closure and reported complications in 5 of 100 cases [20]. Blokmanis and Archibald reported a closure rate of 98 % for near-total perforations using a modified house tympanoplasty technique. However, in their study, 14 of 49 cases showed poor aeration of the middle ear space, often with retraction of the intact eardrum [21]. Fishman et al. found an overall success rate of 92 % (46/50) in a study evaluating the efficacy of total TM reconstruction using lateral onlay tecnique with either dermis allograft (84 % success rate) or temporalis fascia (97 % success rate) for the grafting material [22]. In the series reported by Kazikdas et al. the graft success rate was 95.7 % using Over-under technique with palisade cartilage tympanoplasty, and 75 % using temporalfascia in 51 cases with subtotal perforations [23].
In our study, the graft success rate of tympanoplasty performed using the underlay technique was 89.1 % in 61 patients. Seven (10.9 %) patients had graft failure. The graft success rate with the over-underlay technique in 53 patients was 90.5 %. Five (9.5 %) patients had graft failure in this group. Three graft lateralizations (5.6 %) and two retractions (3.8 %) at 12 months postoperatively in the over-underlay group were observed; however, in the underlay group, no graft lateralizations were identified, but five retractions (8.2 %) were observed at 12 months postoperatively. No statistical significance was observed between the underlay and over-under groups with respect to re-perforation,graft success, lateralization and retractions (p > 0.05, Table 2).
The audiometric tests performed at 12 months postoperatively revealed that the ABG was 12.1 ± 5.5 dB HL in underlay group and Mean ABG was 13.3 ± 6.4 dB HLin over-underlay group. The difference between these two groups was not statistically significant the ABG and PTA results (p > 0.05, Table 3; Fig. 3).
Fig. 3.
Preoperative and postoperative PTA changes in the groups
Conclusion
The graft-take rates in both groups were successful and compatible with those in the literature. This both methods has a high rate of success for the closure of large TM perforations with significant improvement in ABG.
Contributor Information
Erkan Kulduk, Email: erkankulduk@yahoo.com.
Rıza Dundar, Phone: +905304199225, Email: dundarkbb2@gmail.com.
Fatih Kemal Soy, Email: fatihkemalsoy@hotmail.com.
Osman Kadir Guler, Email: osman.guler@windowslive.com.
Ahmet Yukkaldiran, Email: ayukkaldiran@gmail.com.
Ismail Iynen, Email: iiynen@gmail.com.
Ferhat Bozkus, Email: drferhat65@hotmail.com.
References
- 1.Luetje CM. Reconstruction of the tympanic membrane and ossicular chain. In: Bailey B, Johnson J, Newlands S, editors. Head & neck surgery otolaryngology. 4. Lippincott: Williams & Wilkins; 2006. [Google Scholar]
- 2.Zahnert T, Huttenbrink KB, Murbe D, Bornitz M. Experimental investigation of the use of cartilage in tympanic membrane reconstruction. Am J Neurotol. 2000;21:322–328. doi: 10.1016/s0196-0709(00)80039-3. [DOI] [PubMed] [Google Scholar]
- 3.Rizer FM. Overlay versus underlay tympanoplasty. Part I: historical review of the literature. Laryngoscope. 1997;107:1–25. doi: 10.1097/00005537-199712001-00001. [DOI] [PubMed] [Google Scholar]
- 4.Wehrs RE. Grafting techniques. Otolaryngol Clin N Am. 1999;30(3):443–455. doi: 10.1016/S0030-6665(05)70144-4. [DOI] [PubMed] [Google Scholar]
- 5.Lee HY, Auo HJ, Kang JM. Loop overlay tympanoplasty for anterior or subtotal perforations. Auris Nasus Larynx. 2010;37:162–166. doi: 10.1016/j.anl.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Gerlinger I, Ráth G, Szanyi I, et al. Myringoplasty for anterior and subtotal perforations using KTP-532 laser. Eur Arch Otorhinolaryngol. 2006;263:816–819. doi: 10.1007/s00405-006-0077-z. [DOI] [PubMed] [Google Scholar]
- 7.Gersdorff M, Gerard J, Thill M. Overlay versus underlay tympanoplasty: comparative study of 122 cases. Rev Laryngol Otol Rhinol. 2003;24:15–22. [PubMed] [Google Scholar]
- 8.Raghavan U, Malik DSI, Mahmoud NA. Myringoplasty: update on onlay pedicle skin flap and temporalis fascia sandwich graft. J Laryngol Otol. 2000;114:174–177. doi: 10.1258/0022215001905274. [DOI] [PubMed] [Google Scholar]
- 9.Farrior JB. The anterior tympanomeatal angle in tympanoplasty: surgical techniques for the prevention of blunting. Laryngoscope. 1983;93:992–997. doi: 10.1288/00005537-198308000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Shea JJ., Jr Vein graft closure of eardrum perforations. J Laryngol Otol. 1960;74:358–362. doi: 10.1017/S002221510005670X. [DOI] [PubMed] [Google Scholar]
- 11.Tabb HG (1968) Experience with transcanal and postauricular myringoplasty. In: Transactions of the Pacific Coast Ophthalmological Society Annual Meeting, 52:121–125 [PubMed]
- 12.Kartush JM, Michaelides EM, Becvarovski Z, LaRouere MJ. Over-under tympanoplasty. Laryngoscope. 2002;112:802–807. doi: 10.1097/00005537-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Lee P, Kelly G, Mills RP. Myringoplasty: does size of the perforation matter? Clin Otolaryngol. 2002;27:331–334. doi: 10.1046/j.1365-2273.2002.00590.x. [DOI] [PubMed] [Google Scholar]
- 14.Indorewala S. Dimensional stability of free fascia grafts:clinical application. Laryngoscope. 2005;115:278–282. doi: 10.1097/01.mlg.0000154733.54152.54. [DOI] [PubMed] [Google Scholar]
- 15.Green DS. Pure tone air conduction testing. In: Katz J, editor. Handbook of clinical audiology. 2. Baltimore: Waverly Press; 1983. pp. 98–108. [Google Scholar]
- 16.Sade J. The atelectatic ear. In: Sade J, editor. Secretory otitis media and its sequelae. London: Churchill Livingstone; 1979. pp. 64–68. [Google Scholar]
- 17.Adkins WY, White B. Type I tympanoplasty: influencing factors. Laryngoscope. 1984;94:916–918. doi: 10.1288/00005537-198407000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Karela M, Sandeep B, Watkins A, et al. Myringoplasty: surgical outcomes and hearing improvement: is it worth performingto improve hearing? Eur Arch Otorhinolaryngol. 2008;265:1039–1042. doi: 10.1007/s00405-007-0570-z. [DOI] [PubMed] [Google Scholar]
- 19.Angeli SI, Kulak JL, Guzmán J. Lateral tympanoplasty for total or near-total perforation: prognostic factors. Laryngoscope. 2006;116:1594–1599. doi: 10.1097/01.mlg.0000232495.77308.46. [DOI] [PubMed] [Google Scholar]
- 20.Jung TTK, Park SK. Mediolateral graft tympanoplasty for anterior or subtotal tympanic membrane perforation. Otolaryngol Head Neck Surg. 2005;132:532–536. doi: 10.1016/j.otohns.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 21.Blokmanis A, Archibald JD. Modified house tympanoplasty for successful closure of near-total tympanoplasty membrane perforations. J Otolaryngol. 2004;33:370–376. doi: 10.2310/7070.2004.03091. [DOI] [PubMed] [Google Scholar]
- 22.Fishman A, Marrinan M, Huang T, Kanowitz S. Total tympanic membrane reconstruction: alloderm versus temporalis fascia. Otolaryngol Head Neck Surg. 2005;132:906–915. doi: 10.1016/j.otohns.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 23.Kazikdas CK, Onal K, Boyraz I, Karabulut E. Palisade cartilage tympanoplasty for management of subtotal perforations: a comparison with the temporalis fascia technique. Eur Arch Otorhinolaryngol. 2007;264:985–989. doi: 10.1007/s00405-007-0291-3. [DOI] [PubMed] [Google Scholar]