Abstract
Background
The clinical significance of complete revascularization for ST segment elevation myocardial infarction (STEMI) patients during admission is still debatable.
Methods
A total of 1406 STEMI patients from the Korean Myocardial Infarction Registry with multivessel diseases without cardiogenic shock who underwent primary percutaneous coronary intervention (PPCI) were analyzed. We used propensity score matching (PSM) to control differences of baseline characteristics between culprit only intervention (CP) and multivessel percutaneous coronary interventions (MP), and between double vessel disease (DVD) and triple vessel disease (TVD). The major adverse cardiac event (MACE) was analyzed for one year after discharge.
Results
TVD patients showed higher incidence of MACE (14.2% vs. 8.6%, P = 0.01), any cause of revascularization (10.6% vs. 5.9%, P = 0.01), and repeated PCI (9.5% vs. 5.7%, P = 0.02), as compared to DVD patients during one year after discharge. MP reduced MACE effectively (7.3% vs. 13.8%, P = 0.03), as compared to CP for one year, but all cause of death (1.6% vs. 3.2%, P = 0.38), MI (0.4% vs. 0.8%, P = 1.00), and any cause of revascularization (5.3% vs. 9.7%, P = 0.09) were comparable in the two treatment groups.
Conclusions
STEMI patients with TVD showed higher rate of MACE, as compared to DVD. MP performed during PPCI or ad hoc during admission for STEMI patients without cardiogenic shock showed lower rate of MACE in this large scaled database. Therefore, MP could be considered as an effective treatment option for STEMI patients without cardiogenic shock.
Keywords: Culprit only intervention, Multivessel intervention, Multivessel coronary disease, Myocardial infarction, Primary percutaneous coronary intervention
1. Introduction
Multivessel disease (MVD) in coronary angiography is prevalent in 40%−50% of ST segment elevation myocardial infarction (STEMI) patients.[1],[2] MVD in STEMI patients is a significant risk factor to predict higher in-hospital and long-term mortality. These grave clinical results are due to higher co-morbid diseases including older age, diabetes mellitus (DM) and hypertension, lower left ventricular systolic function, and deterioration of renal function after the larger amounts of contrast agents used during coronary intervention.[3],[4] However, optimal treatment strategy for MVD in STEMI is still unclear. General principles in the ACC/AHA 2004 clinical guidelines and the ACC/AHA/SCAI 2005 guidelines do not recommend the simultaneous intervention for non-culprit lesion in STEMI patients during primary percutaneous coronary intervention (PPCI). However, PPCI can be considered in limited cases of continuous cardiogenic shock or hemodynamic instability even after adequate revascularization for culprit lesion under appropriate mechanical supports.[5],[6] Recent advancements of anti-platelet agents, ventricular assist devices, drug-eluting stents,[7] low nephrotoxic contrast agents,[8] and intensive hemodynamic monitoring induced on-site during PPCI or ad hoc coronary interventions during admission for non-culprit lesions in STEMI patients have unknown clinical benefits and risks. Hannan, et al.[9] showed that on-site multivessel percutaneous coronary interventions (MP) are related with worse long-term prognosis, but staged MP on 60 days after the index procedure reduced major adverse cardiac events (MACE) rates, as compared to culprit lesion only percutaneous coronary intervention (CP). In another study, patients who underwent CP showed a higher rate of long-term MACE, as compared to patients with MP.[10] Additionally, the death and repeat revascularization rates in the short-term were similar between patients with complete revascularization (CR) and patients with incomplete revascularization, whereas long-term MACE free survival was significantly higher in the incomplete revascularization group.[11] Cavender, et al.[12] suggested that performing MP during PPCI for STEMI does not improve short-term survival, even in patients with cardiogenic shock. However, most of these studies enrolled very limited numbers of patients,[10] and were retrospective analyses with differences in basal characteristics in MP and CP groups,[11] or invoked some statistical interrogations to overcome basal characteristic differences, e.g., propensity score matching (PSM) were not adopted.[10]–[12] Therefore, an intensive clinical study to investigate the clinical efficiency of MP for MVD in STEMI population is required. Our analysis of the large scale KAMIR (Korean Acute Myocardial Infarction Registry) database with PSM will corroborate basic data on the importance of MP in STEMI populations.
2. Methods
2.1. Patient population and study design
KAMIR was initiated to determine characteristics of Korean acute myocardial infarction (AMI) patients and define better modalities of control and treatment to improve the survival of AMI patients as a 50th anniversary memorial clinical project of the Korean Society of Cardiology from November, 2005.[13],[14] More than 50 cardiovascular centers with sufficient manpower and equipment for PPCI and venous thrombolysis for STEMI participated in this registry collected proper data on Korean AMI patients and established risk model and optimized therapeutic strategies for AMI. All participating cardiovascular centers achieved approval from the Institutional Review Board, and are under the regular monitoring processes.
This retrospective study included 1,406 STEMI patients in the KAMIR database who underwent PPCI and had MVD from Nov. 11, 2005 to Jan. 31, 2008. We included STEMI patients that underwent PPCI within 12 h after onset of chest pain with clear data on MACE for 1-year after discharge. Firstly, 7,818 selected patients had an initial diagnosis of STEMI. We eliminated a considerable number of patients via the following exclusion criteria: (1) patients with culprit lesion with left main area or significant stenosis with left main area (n = 195); (2) incomplete data of coronary angiography (n = 882); (3) Killip class IV (n = 376); (4) presenting to emergency room after 12 h of chest pain onset (n = 1,800); (4) more than two h delay from emergency room appearance to revascularization (n = 784); (5) no PPCI as the initial therapy (n = 720); (6) single vessel disease patients (n = 1,579); and (7) in-hospital death (n = 76). Survivors from the hospital after STEMI were included and analyzed to estimate MACE for one year after discharge.
2.2. Definition of terminology and primary endpoint
STEMI was defined as > 1 mm of ST segments elevation in at least two consecutive leads and reciprocal ST segment depression accompanied with at least 30 min of typical ischemic chest pain and typical form of myocardial enzyme elevation. MVD was defined as > 50% of diameter stenosis of ≥ 2 coronary vessels. We defined MP as multivessel coronary revascularization underwent during index PPCI or the 2nd time PCI during admission for STEMI treatment, whereas CP was defined as only culprit vessel revascularization. Double vessel disease group (DVD) was defined as significant stenosis in two major epicardial vessels including infarct related artery (IRA), and triple vessel disease group (TVD) was patient with significant coronary stenotic lesions in all three epicardial vessels. Primary end points of this study were defined as MACE for one year after discharge of STEMI patients who underwent PPCI. MACE was composed of all cause of death, MI, and any cause of revascularization including repeated PCI and coronary artery bypass graft (CABG).
2.3. Statistical analysis
Continuous variables were described as mean ± SD, and categorical variables were described as percentages (%). We used t-test based analysis for continuous variables and chi-square based approach for categorical variables. Our study was based on a large-scaled database that had significantly different baseline clinical characteristics between MP and CP groups. Therefore, we used the PSM to adjust baseline characteristics differences in both groups to obtain a significant meaning of the MACE rate. Kaplan-Meier analysis and the log-rank test were used in MACE free survival analysis. All analyses were performed using SPSS (SPSS Inc. Chicago, IL) version 21.0 and SAS (SAS Institute, Cary, NC) version 9.3.
3. Result
3.1. Baseline characteristics
We compared basic clinical characteristics in terms of patients groups (Table 1). TVD group was older (63.7 ± 12.0 years vs. 62.1 ± 12.1 years, P = 0.02), had higher prevalence of hypertension (52.3% vs. 46.4%, P = 0.03), diabetes mellitus (29.3% vs. 24.2%, P = 0.04), as compared to the DVD group. There was no significant difference of gender composition (female 26.4% vs. 24.2%, P = 0.38), body mass index (BMI) (24.2 ± 3.2 kg/m2 vs. 24.2 ± 3.1 kg/m2, P = 0.74), prevalence of dyslipidemia (8.5% vs. 7.9%, P = 0.77), history of ischemia heart disease (13.3% vs. 12.5%, P = 0.75), family history of cardiovascular disease (7.3% vs. 7.2%, P = 1.00), composition of Killip Class (P = 0.15) in the TVD and DVD groups. TVD showed a higher rate of discharge medication with calcium channel blocker (CCB, 10.3% vs. 5.5%, P = 0.00). There was similar prescription rates for aspirin (97.0% vs. 97.3%, P = 0.75), β-blocker (73.8% vs. 75.3%, P = 0.53), clopidogrel (94.3% vs. 95.7%, P = 0.25), angiotensin converting enzyme (ACE) inhibitor (68.6% vs. 67.2%, P = 0.60), angiotensin receptor blocker (ARB) (14.5% vs. 15.0%, P = 0.88), cilostazol (35.5% vs. 35.7%, P = 0.96), and statin (76.8% vs. 76.4%, P = 0.90) in TVD and DVD. There was different composition of Killip class (P = 0.04) with higher frequency of Killip class 1 in MP (81.4% vs. 78.4%) and Killip class 3 (8.1% vs. 5.5%), as compared to the CP group, whereas CP showed higher ratio of Killip class 2 (16.0% vs. 10.5%). However, age (63.0 ± 12.2 years vs. 61.9 ± 11.1 years, P = 0.22), gender composition (female: 25.7% vs. 22.3%, P = 0.22), BMI (24.2 ± 3.2 kg/m2 vs. 24.2 ± 2.9 kg/m2, P = 0.93), family history of cardiovascular disease (6.6% vs. 10.1%, P = 0.06), rate of smoking (60.7% vs. 65.6%, P = 0.15), hypertension (49.2% vs. 49.0%, P = 0.53), diabetes mellitus (26.2% vs. 26.3%, P = 1.00), dyslipidemia (8.5% vs. 6.9%, P = 0.52), and history of ischemia heart disease (13.5% vs. 10.1%, P = 0.17) were similar in both CP and MP groups. The discharge prescription rates of cilostazol (32.1% vs. 52.2%, P = 0.01) was significantly higher in the MP than CP group. Aspirin (97.2% vs. 97.2%, P = 1.00), clopidogrel (95.6% vs. 93.1%, P = 0.10), β-blocker (74.5% vs. 75.3%, P = 0.87), CCB (7.0% vs. 9.3%, P = 0.23), ACE inhibitor (70.0% vs. 71.7%, P = 0.16), ARB (15.4% vs. 12.1%, P = 0.24) and statin (76.6% vs. 76.1%, P = 0.87) were equally prescribed in both CP and MP groups at discharge.
Table 1. Baseline characteristics of study groups.
| Variable | DVD (n = 842) | TVD (n = 564) | P value | CP (n = 1159) | MP (n = 247) | P value |
| Demographic factor | ||||||
| Age, yrs | 62.1 ± 12.1 | 63.7 ± 12.0 | 0.02 | 63.0 ± 12.2 | 61.9 ± 11.1 | 0.22 |
| BMI, kg/m2 | 24.2 ± 3.1 | 24.2 ± 3.2 | 0.74 | 24.2 ± 3.2 | 24.2 ± 2.9 | 0.93 |
| Female sex | 204 (24.2) | 149 (26.4) | 0.38 | 298 (25.7) | 55 (22.3) | 0.29 |
| Clinical factor | ||||||
| Hypertension | 391 (46.4) | 295 (52.3) | 0.03 | 570 (49.2) | 116 (49.0) | 0.53 |
| Diabetes mellitus | 204 (24.2) | 165 (29.3) | 0.04 | 304 (26.2) | 65 (26.3) | 1.00 |
| Smoking | 526 (62.5) | 339 (60.1) | 0.37 | 703 (60.7) | 162 (65.6) | 0.15 |
| Dyslipidemia | 67 (7.9) | 48 (8.5) | 0.77 | 98 (8.5) | 17 (6.9) | 0.52 |
| Ischemic heart disease | 106 (12.5) | 75 (13.3) | 0.75 | 156 (13.5) | 25 (10.1) | 0.17 |
| Familial history of CVD | 61 (7.2) | 41 (7.3) | 1.00 | 77 (6.6) | 25 (10.1) | 0.06 |
| Killip class | ||||||
| Class I | 674 (80.0) | 436 (77.3) | 909 (78.4) | 201 (81.4) | ||
| Class II | 126 (15.0) | 86 (15.2) | 0.15 | 186 (16.0) | 26 (10.5) | 0.04 |
| Class III | 42 (5.0) | 42 (7.4) | 64 (5.5) | 20 (8.1) | ||
| Medication on discharge | ||||||
| Aspirin | 819 (97.3) | 547 (97.0 ) | 0.75 | 1126(97.2) | 240 (97.2) | 1.00 |
| Clopidogrel | 806 (95.7) | 532 (94.3) | 0.25 | 1108(95.6) | 230 (93.1) | 0.10 |
| Cilostazol | 301 (35.7) | 200 (35.5) | 0.96 | 372 (32.1) | 129 (52.2) | 0.00 |
| Beta blocker | 634 (75.3) | 416 (73.8) | 0.53 | 864 (74.5) | 186 (75.3) | 0.87 |
| Calcium channel blocker | 46 (5.5) | 58 (10.3) | 0.00 | 81 (7.0) | 23 (9.3) | 0.23 |
| ACEI | 566 (67.2) | 387 (68.6) | 0.60 | 776 (70.0) | 177 (71.7) | 0.16 |
| ARB | 126 (15.0) | 82 (14.5) | 0.88 | 178 (15.4) | 30 (12.1) | 0.24 |
| Statin | 643 (76.4) | 433 (76.8) | 0.90 | 888 (76.6) | 188 (76.1) | 0.87 |
Data are expressed as n (%) or mean ± SD. ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; BMI: body mass index; CP: only culprit vessel percutaneous coronary intervention; CVD: cardiovascular vessel disease; DVD: double vessel disease; MP: multivessel percutaneous coronary intervention; TVD: triple vessel disease.
3.2. Clinical outcomes using propensity score matching in DVD vs. TVD
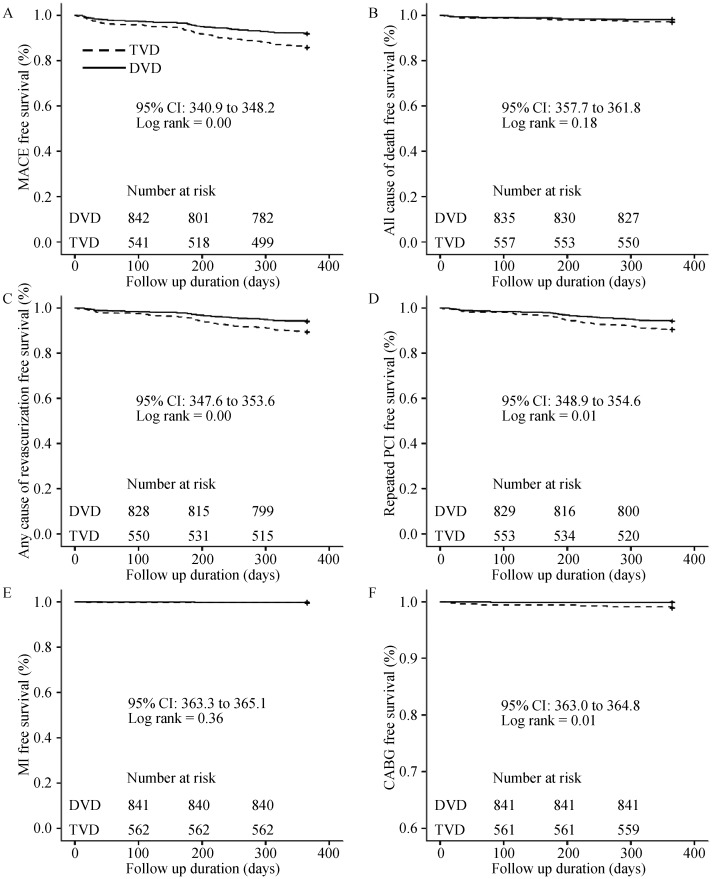
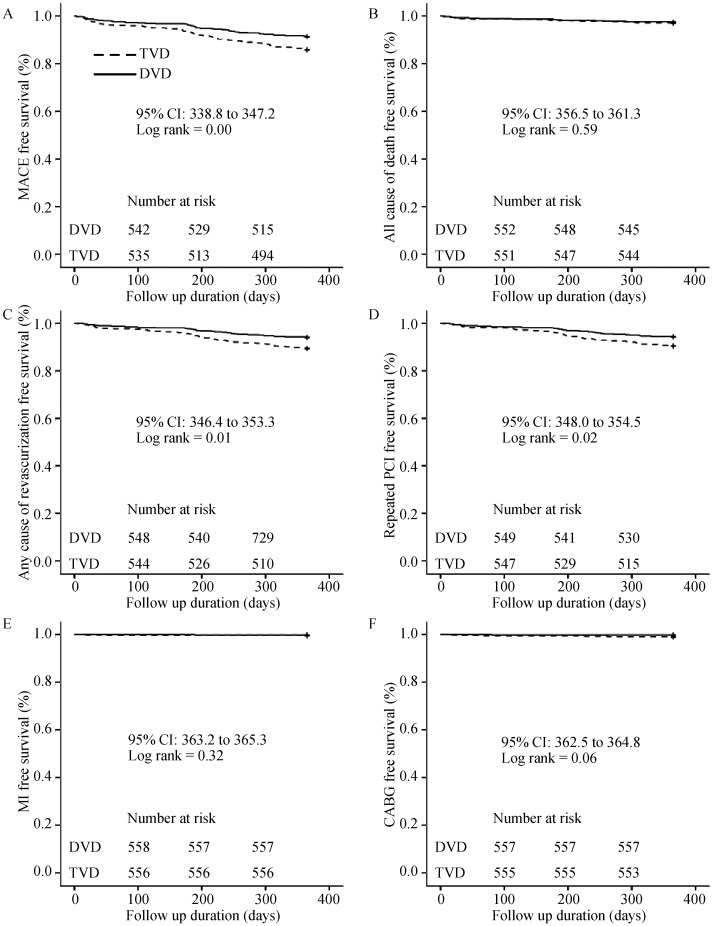
We used a PSM to adjust differences of the basic clinical characteristics and unbalanced number of patients in the DVD and TVD groups. Conditional variables were defined as age, female, hypertension, diabetes mellitus, smoking, dyslipidemia, family history of cardiovascular vessel disease (CVD), IHD, Killip Class, and discharge medications including asprin, clopidogrel, cilostazol, β-blocker, CCB, ACE Inhibitor, ARB, and statins. The confounding variables such as age, hypertension, diabetes mellitus and CCB were adjusted (Table 2). In the analysis of MACE without a PSM, the TVD group showed higher rate of MACE (14.2% vs. 8.1%, P = 0.00). There was no difference in all cause of death (3.0% vs. 1.9%, P = 0.21), MI (0.5% vs. 0.2%, P = 0.40), but any cause of revascularization was significantly high in TVD group (10.6% vs. 5.9%, P = 0.00) in both repeated PCI (9.6% vs. 5.8%, P = 0.01), and CABG (1.1% vs. 0.1%, P = 0.02) in the one year follow-up (Table 3). Survival analysis based on log rank test showed significant differences among the two groups in terms of one year MACE (log rank = 0.00; Figure 1A), any cause of revascularization (log rank = 0.00; Figure 1C), repeated PCI (log rank = 0.01; Figure 1D), and CABG (log rank = 0.01; Figure 1F). After the adjustment of confounding variables with a PSM, TVD group still showed significantly higher rate of MACE at one year after index PCI (14.2% vs. 8.6%, P = 0.01). In detail, TVD patients had a higher incidence of any cause of revascularization (10.6% vs. 5.9%, P = 0.01) and repeated PCI (9.5% vs. 5.7%, P = 0.02). There was no significant differences on all cause of death (3.0% vs. 2.5%, P = 0.72), MI (0.5% vs. 0.2%, P = 0.62), and CABG (1.1% vs. 0.2%, P = 0.12) (Table 3). Additionally, survival analysis based on log rank test showed significant differences among the two groups in terms of one year MACE (log rank = 0.00; Figure 2A), any cause of revascularization (log rank = 0.01; Figure 2C), and repeated PCI (log rank = 0.02; Figure 2D).
Table 2. Baseline characteristics of the propensity score matched study groups.
| Basic confound variable | DVD (n = 558) | TVD (n = 558) | P value | CP (n = 247) | MP (n = 247) | P value |
| Age, yrs | 63.3 ± 11.8 | 63.6 ± 12.0 | 0.67 | 63.0 ± 12.0 | 61.9 ± 11.1 | 0.29 |
| Female sex | 136 (24.4) | 148 (26.5) | 0.45 | 58 (23.5) | 55 (22.3) | 0.83 |
| Hypertension | 282 (50.5) | 290 (52.0) | 0.68 | 108 (43.7) | 116 (47) | 0.53 |
| Diabetes mellitus | 165 (29.6) | 160 (28.7) | 0.79 | 68 (27.5) | 65 (26.3) | 0.84 |
| Smoking | 345 (61.8) | 336 (60.2) | 0.62 | 147 (59.5) | 162 (65.6) | 0.19 |
| Dyslipidemia | 42 (7.5) | 47 (8.4) | 0.66 | 19 (7.7) | 17 (6.9) | 0.86 |
| Ischemic heart disease | 71 (12.7) | 73 (13.1) | 0.93 | 30 (12.1) | 25 (10.1) | 0.57 |
| Family history of CVD | 39 (7.0) | 41 (7.3) | 0.91 | 23 (9.3) | 25 (10.1) | 0.88 |
| Killip class | ||||||
| Class I | 446 (79.9) | 432 (77.4) | 207 (83.8) | 201 (81.4) | ||
| Class II | 75 (13.4) | 86 (15.4) | 0.58 | 18 (7.3) | 26 (10.5) | 0.44 |
| Class III | 37 (6.6) | 40 (7.2) | 22 (8.9) | 20 (8.1) | ||
| Aspirin | 543 (97.3) | 541 (97) | 0.86 | 241 (97.6) | 240 (97.1) | 1.00 |
| Clopidogrel | 530 (95) | 528 (94.6) | 0.89 | 232 (93.9) | 230 (93.1) | 0.86 |
| Cilostazol | 193 (34.6) | 198 (35.5) | 0.80 | 131 (53) | 129 (52.2) | 0.93 |
| Beta blocker | 419 (75.1) | 414 (74.2) | 0.78 | 193 (78.1) | 186 (75.3) | 0.52 |
| Calcium channel blocker | 44 (7.9) | 52 (9.3) | 0.46 | 27 (10.9) | 23 (9.3) | 0.66 |
| ACEI | 402 (72) | 382 (68.5) | 0.21 | 185 (74.9) | 177 (71.7) | 0.48 |
| ARB | 71 (12.7) | 82 (14.7) | 0.38 | 32 (30) | 30 (12.1) | 0.89 |
| Statins | 433 (77.6) | 429 (76.9) | 0.83 | 192 (77.7) | 188 (76.1) | 0.75 |
Data are expressed as n (%) or mean ± SD. ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; CP: only culprit vessel percutaneous coronary intervention; CVD: cardiovascular vessel disease; DVD: double vessel disease; MP: multivessel percutaneous coronary intervention; TVD: triple vessel disease.
Table 3. Clinical outcomes for one year in DVD, and TVD patients.
| Variable | Without PSM (n = 1406) |
With PSM (n = 1116) |
||||
| DVD (n = 842) | TVD (n = 564) | P value | DVD (n = 558) | TVD (n = 558) | P value | |
| MACE | 68 (8.1) | 80 (14.2) | 0.00 | 48 (8.6) | 79 (14.2) | 0.01 |
| All cause of death | 16 (1.9) | 17 (3.0) | 0.21 | 14 (2.5) | 17 (3.0) | 0.72 |
| MI (%) | 2 (0.2) | 3 (0.5) | 0.40 | 1 (0.2) | 3 (0.5) | 0.62 |
| Any cause of revascularization | 50 (5.9) | 60 (10.6) | 0.00 | 33 (5.9) | 59 (10.6) | 0.01 |
| Repeated PCI | 49 (5.8) | 54 (9.6) | 0.01 | 32 (5.7) | 53 (9.5) | 0.02 |
| CABG | 1 (0.1) | 6 (1.1) | 0.02 | 1 (0.2) | 6 (1.1) | 0.12 |
Data are expressed as n (%). CABG: coronary artery bypass graft; DVD: double vessel disease; MACE: major adverse cardiac events; MI: myocardial infarction; PCI: percutaneous coronary intervention; PSM: propensity score matching; TVD: triple vessel disease.
Figure 1. MACE analysis for one year in patients with DVD and TVD.
TVD patients showed higher MACE rate for one year. This result was due to higher incidence of all cause of revascularization including PCI and CABG. CABG: coronary artery bypass graft; DVD: double vessel disease; MACE: major adverse cardiac events; MI: myocardial infarction; PCI: percutaneous coronary intervention; TVD: triple vessel disease.
Figure 2. MACE analysis for one year in patients with DVD and TVD after controlling with propensity score matching.
After adjustment of clinical variable differences by propensity score matching, TVD patients showed higher MACE compared to DVD patients. Major difference existed in repeated revascularization. DVD: double vessel disease; MACE: major adverse cardiac event; MI: myocardial infarction; PCI: percutaneous coronary intervention; TVD: triple vessel disease.
3.3. Clinical outcomes using propensity score matching in CP, MP
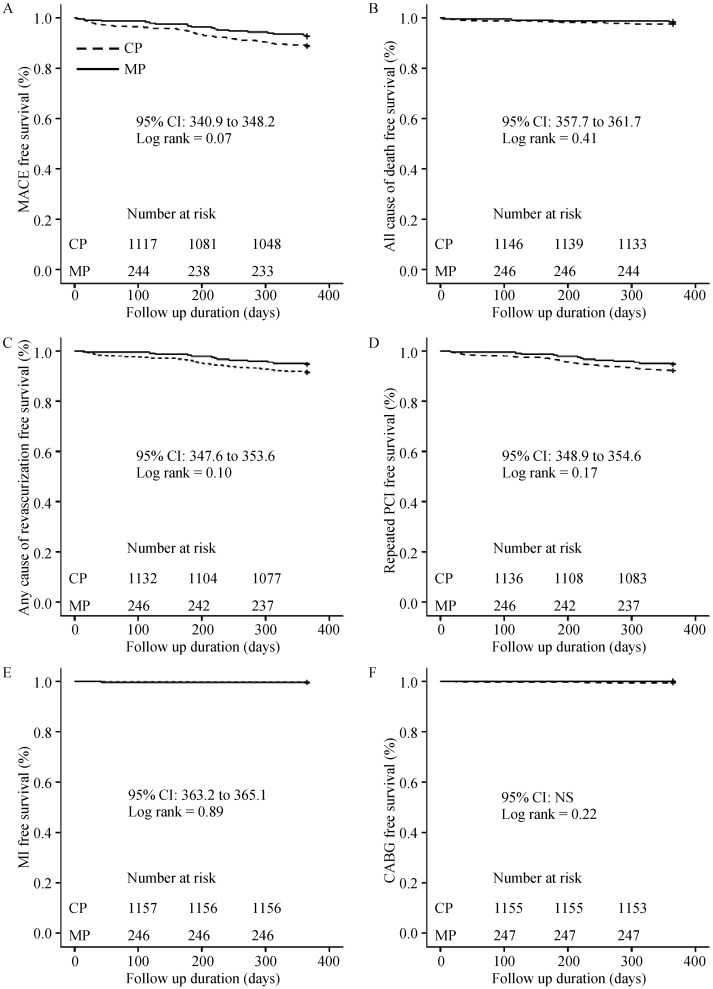
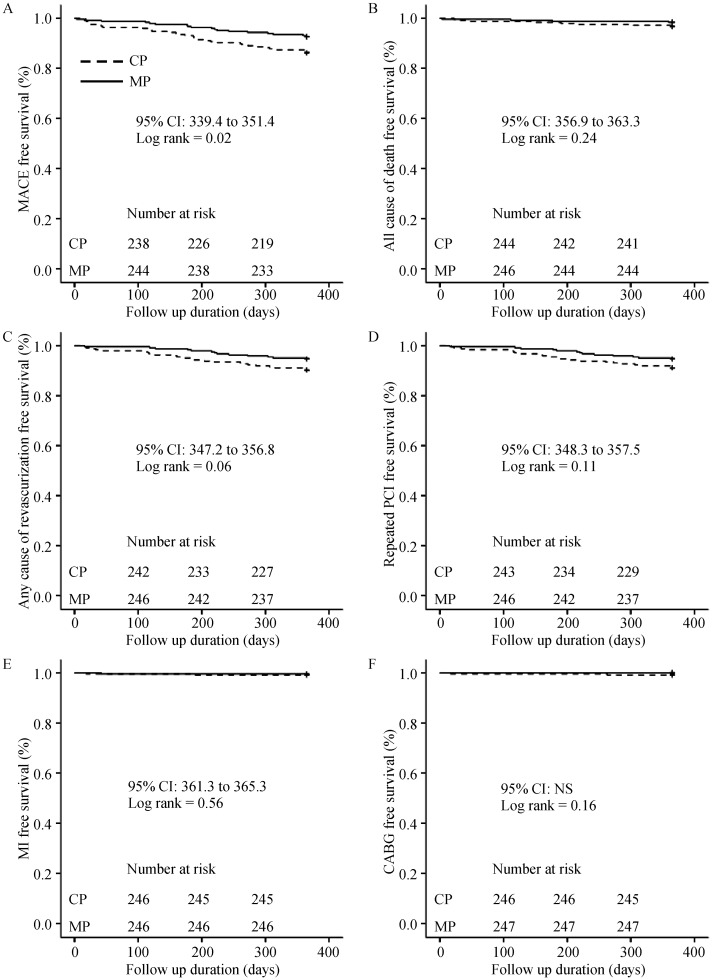
CP and MP group without PSM showed a similar rate of MACE (11.2% vs. 7.3%, P = 0.07), all cause of death (2.5% vs. 1.6%, P = 0.50), MI (0.3% vs. 0.4%, P = 1.00), any cause of revascularization (8.4% vs. 5.3%, P = 0.12) including repeated PCI (7.8% vs. 5.3%, P = 0.23), and CABG (0.6% vs. 0.0%, P = 0.61) (Table 4). Figure 3 showed survival analysis based on log rank test in CP and MP groups without PSM for one year. After the adjustment of confounding values i.e., Killip class and cliostazol using a PSM, CP group showed a significantly higher rate of MACE (13.8% vs. 7.3%, P = 0.03) in the one year follow-up. In detail, there were no significant differences on all cause of death (3.2% vs. 1.6%, P = 0.38), MI (0.8% vs. 0.4%, P = 1.00), any cause of revascularization (9.7% vs. 5.3%, P = 0.09) including repeated PCI (8.9% vs. 5.3%, P = 0.16), and CABG (0.8% vs. 0.0%, P = 0.25) (Table 4). Additionally, survival analysis based on log rank test showed a significant difference among the two groups in terms of one year MACE (log rank = 0.02) (Figure 4A).
Table 4. Clinical outcomes in one year in CP, and MP patients.
| Variable | Without PSM (n = 1406) |
With PSM (n = 594) |
||||
| CP (n = 1159) | MP (n = 247) | P value | CP (n = 247) | MP (n = 247) | P value | |
| MACE | 130 (11.2) | 18 (7.3) | 0.07 | 34 (13.8) | 18 (7.3) | 0.03 |
| All cause of death | 29 (2.5) | 4 (1.6) | 0.50 | 8 (3.2) | 4 (1.6) | 0.38 |
| MI | 4 (0.3) | 1 (0.4) | 1.00 | 2 (0.8) | 1 (0.4) | 1.00 |
| Any cause of revascularization | 97 (8.4) | 13 (5.3) | 0.12 | 24 (9.7) | 13 (5.3) | 0.09 |
| Repeated PCI | 90 (7.8) | 13 (5.3) | 0.23 | 22 (8.9) | 13 (5.3) | 0.16 |
| CABG | 7 (0.6) | 0 (0.0) | 0.61 | 2 (0.8) | 0 (0.0) | 0.25 |
Data are expressed as n (%). CABG: coronary artery bypass graft; CP: only culprit vessel percutaneous coronary intervention; DVD: double vessel disease; MACE: major adverse cardiac events; MI: myocardial infarction; MP: multivessel percutaneous coronary intervention; PCI: percutaneous coronary intervention; PSM: propensity score matching.
Figure 3. MACE analysis for one year in patients with CP and MP.
There was no significant difference in MACE between CP and MP group. CP: culprit vessel percutaneous coronary intervention; MACE: major adverse cardiac event; MP: multivessel percutaneous coronary intervention; MI: myocardial infarction; PCI: percutaneous coronary intervention.
Figure 4. MACE analysis for one year in patients with CP and MP after controlling with propensity score matching.
After use of propensity score matching, MP showed significant lower incidence of MACE compared to CP. Even though all subsets of MACE were comparable in both groups, composite MACE was significantly lower in MP. CP: culprit vessel percutaneous coronary intervention; MACE: major adverse cardiac event; MP: multivessel percutaneous coronary intervention; MI: myocardial infarction; PCI: percutaneous coronary intervention.
4. Discussion
We determined the clinical benefit of MP, as compared to CP during admission of STEMI. The KAMIR database was used in the retrospective study and a PSM was applied to adjust mismatched baseline characteristics of enrolled population between MP and CP in the KAMIR database. Conclusively, MP including on-site or ad hoc PCI after PPCI to open non-culprit lesions in STEMI with MVD significantly reduced MACE, as compared to CP for one year after PPCI. There are several debatable issues on MP for non-culprit lesions in STEMI patients. First is the possibility of higher in-stent restenosis and its related revascularization that occurred by higher number or longer stent usage in MP, as compared to CP in STEMI patients. However, this problem was significantly reduced with drug eluting stents.[7],[15],[16] Second is the higher amount of contrast agents, which it is directly related with renal dysfunction and closely related to higher MACE and overall mortality rate in AMI patients.[17] This problem can be prevented by adequate intravenous fluid resuscitation, reduced use of contrast agent with precise fluoroscopic image review during procedure, and low nephrotoxic contrast agents, e.g., non-ionic and iso-osmolar agents.[8] Despite the advances in PCI, the clinical benefit of MP in STEMI remains unclear. Cavender, et al.[12] analyzed the national cardiovascular data registry to determine the cardiac event in in-hospital outcomes of patients for STEMI with MVD. These data suggested that performing MP during primary PCI for STEMI does not improve short-term survival even in patients with cardiogenic shock. Although this study used the generalized estimation equation model to adjust the confounding values, their data on patients might be prejudiced by bias of patient characteristics among the groups, i.e., time of symptoms to bloom time or cardiogenic shock. Meliga, et al.[11] confirmed complete revascularization had a higher rate of periprocedural MI and MACE, as compared to culprit only PCI in short-term follow-up, but complete revascularization significantly reduced MACE at the two year follow-up post-PPCI; this long-term benefit was due to the reduction of revascularization, not from cardiovascular death or MI. This was a retrospective study with significant differences of baseline characteristics between the two groups. Hannan, et al.[9] showed that patients undergoing staged MP within 60 days after the index procedure had a significantly lower 12-month mortality rate that patients undergoing CP alone. The enrolled population of their study was older than our study patients possibly contributing to the intra-study differences in MACE free survival. Politi, et al[10] compared the clinical impact between CP and MP during PPCI and staged revascularization and simultaneous MP in STEMI patients. The CP showed a higher long-term MACE rate, as compared with MP and there was no significant MACE rate differences between the staged revascularization and simultaneous MP group.[10] The small study population, however, decreases the reliability of their result as compared with our study. More importantly, the previous studies included in-hospital events, whereas our study excluded in-hospital events in order to analyze the prognosis of discharged patients. Additionally, we considered the discharge medications, since the baseline characteristics in medication were significantly different. According to our data, TVD showed significantly higher MACE rate than DVD. MP during admission of STEMI patients likely reduces post-discharge MACE. We cannot generalize the current data to actual clinical practice, which was a study limitation. CP included simultaneous non-IRA lesion PCI during PPCI, and ad hoc PCI during admission for STEMI. So, MP does not mean complete revascularization in on-site PPCI. We could not estimate the incidence of puncture related complication and cerebrovascular events due to the basic structure of the KAMIR database.
Our data clearly showed that TVD patients showed significantly worse basal clinical characteristics. After the adjustment of baseline characteristics with a PSM, TVD group showed a higher MACE rate, as compared to DVD patients in one year after PPCI. The difference in MACE was due to the significant difference of any cause of revascularization and repeated PCI. A higher incidence of MACE was observed in the CP than MP group in one year follow-up. Hence, STEMI patients with TVD showed a higher rate of MACE, as compared to DVD. MP including those performed during index PPCI or admission for patients with STEMI and MVD in relatively stable vital status (Killip 1 to 3) can limit the MACE rate in the long-term period after discharge. A further decisive prospective, randomized, large scale clinical trial is clearly required.
Acknowledgments
This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (No. 2013R1A2A2A01068923) and (NO. 2013R1 A1A206518).
References
- 1.Waldecker B, Waas W, Haberbosch W, et al. Long-term follow-up after direct percutaenous transluminal coronary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 1988;32:1320–1325. doi: 10.1016/s0735-1097(98)00405-7. [DOI] [PubMed] [Google Scholar]
- 2.Grines CL, Cox DA, Stone GW, et al. Coronary angioplasty with or without stent implantation for acute myocardial infarction. N Engl J Med. 1993;341:1949–1956. doi: 10.1056/NEJM199912233412601. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein JA, Demetriou D, Grines CL, et al. Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med. 2000;343:915–922. doi: 10.1056/NEJM200009283431303. [DOI] [PubMed] [Google Scholar]
- 4.Parodi G, Memisha G, Valenti R, et al. Five year outcome after primary coronary intervention for acute ST elevation myocardial infarction: results from a single centre experience. Heart. 2005;91:1541–1544. doi: 10.1136/hrt.2004.054692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44:e1–e211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Smith SC, Jr, Feldman TE, Hirshfeld JW, Jr, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention) Circulation. 2006;113:e166–e286. doi: 10.1161/CIRCULATIONAHA.106.173220. [DOI] [PubMed] [Google Scholar]
- 7.Schwietz T, Ehrlich JR, De Rosa S, et al. Prognostic impact of using drug-eluting-stents on outcomes and strategy in multivessel PCI: data from the Frankfurt MV-PCI registry. J Cardiol. 2013;61:38–43. doi: 10.1016/j.jjcc.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Alexopoulos E, Spargias K, Kyrzopoulos S, et al. Contrast-induced acute kidney injury in patients with renal dysfunction undergoing a coronary procedure and receiving non-ionic low-osmolar versus iso-osmolar contrast media. Am J Med Sci. 2010;339:25–30. doi: 10.1097/MAJ.0b013e3181c06e70. [DOI] [PubMed] [Google Scholar]
- 9.Hannan EL, Samadashvili Z, Walford G, et al. Culprit vessel percutaneous coronary intervention versus multivessel and staged percutaneous coronary intervention for ST-segment elevation myocardial infarction patients with multivessel disease. JACC Cardiovasc Interv. 2010;3:22–31. doi: 10.1016/j.jcin.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 10.Politi L, Squra F, Rossi R, et al. A randomized trial of target-vessel versus multi-vessel revascularization in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart. 2010;96:662–667. doi: 10.1136/hrt.2009.177162. [DOI] [PubMed] [Google Scholar]
- 11.Meliga E, Fiorina C, Valqimigli M, et al. Early angio-guided complete revascularization versus culprit vessel PCI followed by ischemia-guided staged PCI in STEMI patients with multivessel Disease. J Interv Cardiol. 2011;24:535–541. doi: 10.1111/j.1540-8183.2011.00666.x. [DOI] [PubMed] [Google Scholar]
- 12.Cavender MA, Milford-Beland S, Roe MT, et al. Prevalence, predictors, and in hospital outcomes of non-infarct artery intervention during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (from the National Cardiovascular Data Registry) Am J Cardiol. 2009;104:507–513. doi: 10.1016/j.amjcard.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Chen KY, Rha SW, Wang L, et al. Unrestricted use of 2 new-generation drug-eluting stents in patients with acute myocardial infarction: a propensity score-matched analysis. JACC Cardiovasc interv. 2012;5:936–945. doi: 10.1016/j.jcin.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Cho Y, Tang HM, Park KW, et al. Paclitaxel-versus sirolimus-eluting stents for treatment of ST-segment elevation myocardial infarction: with analyses for diabetic and nondiabetic subpopulation. JACC: Cardiovasc Interv. 2010;3:498–506. doi: 10.1016/j.jcin.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 15.Kirtane AJ, Gupta A, Iyengar S, et al. Safety and efficacy of drug-eluting and bare metal stents: comprehensive meta-analysis of randomized trials and observational studies. Circulation. 2009;119:3198–3206. doi: 10.1161/CIRCULATIONAHA.108.826479. [DOI] [PubMed] [Google Scholar]
- 16.Lee SR, Jeong MH, Ahn YK, et al. Clinical safety of drug-eluting stents in the Korea acute myocardial infarction registry. Circ J. 2008;72:392–398. doi: 10.1253/circj.72.392. [DOI] [PubMed] [Google Scholar]
- 17.Bhatt DL, Topol EJ. Does creatinine kinase-MB elevation after percutaneous coronary intervention predict outcomes in 2005? Periprocedural cardiac enzyme elevation predicts adverse outcomes. Circulation. 2005;112:906–915. doi: 10.1161/CIRCULATIONAHA.104.483297. [DOI] [PubMed] [Google Scholar]