Abstract
Background
Sedatives and analgesics are often administered to achieve conscious sedation for diagnostic and therapeutic procedures. Appropriate concerns have been raised regarding post procedure delirium related to peri-procedural medication in the elderly. The objective of this study was to investigate the effect of premedication on new onset delirium and procedural care in elderly patients.
Methods
Patients ≥ 70 years old and scheduled for elective cardiac catheterization were randomly assigned to receive either oral diphenhydramine and diazepam (25 mg/5 mg) or no premedication. All patients underwent a mini mental state exam and delirium assessment using confusion assessment method prior to the procedure and repeated at 4 h after the procedure and prior to discharge. Patients' cooperation during the procedure and ease of post-procedure were measured using Visual Analog Scale (VAS). The degree of alertness was assessed immediately on arrival to the floor, and twice hourly afterwards using Observer's Assessment of Alertness/Sedation Scale (OAA/S).
Results
A total of 93 patients were enrolled. The mean age was 77 years, and 47 patients received premedication prior to the procedure. None of the patients in either group developed delirium. Patients' cooperation and the ease of procedure was greater and pain medication requirement less both during and after the procedure in the pre-medicated group (P < 0.05 for both). Nurses reported an improvement with patient management in the pre-medicated group (P = 0.08).
Conclusions
In conclusion, premedication did not cause delirium in elderly patients undergoing cardiac catheterization. The reduced pain medication requirement, perceived procedural ease and post procedure management favors premedication in elderly patients undergoing cardiac catheterization.
Keywords: Cardiac catheterization, Diphenhydramine, Diazepam, Delirium, The elderly
1. Introduction
Delirium, defined as an acute confusional state, is characterized by disordered attention and cognition, usually resulting from an underlying medical condition or from medication or drug withdrawal. Delirium affects 10% to 30 % of hospitalized patients with medical illness and is more common among elderly patients.[1]–[5] It is estimated that up to 50% of elderly patients suffer postoperative delirium.[5]–[7] Medications especially sedatives, hypnotics and anticholinergics are considered to increase the risk of delirium in elderly patients.[2],[8]–[10] Delirium causes detrimental effects including increased mortality, prolonged hospitalization as well as delayed functional recovery.[11]–[13] With the aging US population there is a continuous increase in the proportion of elderly patients undergoing various medical and surgical procedures.[13]–[15] Conscious sedation is considered important for safe and successful completion of various procedures.[16],[17] Different medications including benzodiazepines, analgesics and antihistamines are used during conscious sedation.
Many cardiologists use conscious sedation during cardiac catheterization which often consists of oral diphenhydramine and diazepam prior to the procedure.[18] Additionally, during the procedure patients may receive intravenous midazolam for improved sedation and fentanyl citrate for pain control. Midazolam, a short acting benzodiazepine, has been shown to be a safe and effective means of sedation in elderly patients undergoing endoscopic procedures.[19] However, there are concerns regarding the development of delirium related to diazepam (long acting benzodiazepine) and diphenhydramine (antihistamine) especially in elderly patients. Various studies have reported inconsistent data regarding development of delirium as a result of periprocedure medications, and little data exist for elderly patients undergoing cardiac catheterization.[20],[21]
The objective of our study was to investigate whether oral premeditations (diphenhydramine and diazepam) would increase the risk of post-procedure delirium in elderly patients, while still providing adequate sedation when used with midazolam during the cardiac catheterization.
2. Methods
This was a randomized control study, with patients randomly assigned to receive oral premedications (diazepam 5 mg and diphenhydramine 25 mg) versus no premedications before the procedure. The catheterization laboratory staff and nursing staff that took care of patients after the procedure and majority of the operators were unaware of the randomization. A decrease of > 2 points in the mini-mental state examination (MMSE) from the baseline was considered significant for acute mental status change.[22] Delirium was diagnosed by confusion assessment method (CAM). A sample size of 80 patients was considered to provide 80% power to detect a meaningful difference in CAM and MMSE scores.
Primary outcomes included new onset of delirium and change in MMSE. The secondary outcomes included degree of ease of the procedure, level of alertness after the procedure, pain medication requirement during and after procedure, ease of post procedure patient management as assessed by nursing staff, and length of stay following the procedure.
The study protocol was reviewed and approved by the Institutional Review Board. Patients 70 years of age or older and scheduled for elective cardiac catheterization were screened for enrollment in study. All patients underwent baseline cognition assessment test using a 30-point questionnaire MMSE.[22]–[24] Presence or absence of delirium at baseline was evaluated by CAM.[25],[26] Patients with a MMSE score < 20, delirium prior to the procedure, history of allergic reaction to diphenhydramine, diazepam or midazolam were excluded from the study. Patients were randomly assigned to oral premeditations with diphenhydramine (25 mg) and diazepam (5 mg) versus no specific therapy prior to cardiac catheterization. At the start of procedure, all patients received intravenous midazolam (recommended dose 0.5 mg to 2.0 mg) at the discretion of cardiologist. Intravenous fentanyl (25–50 µL or in increments) was used during the procedure for pain if needed.
The ease of procedure and patients' collaboration during the procedure was assessed by operators or catheterization laboratory staff using visual analog scale (VAS).[27],[28] VAS is between 0 to 10, with 0 being no problem and 10 impossible. Following the procedure, we evaluated absence or presence of delirium using CAM and change in MMSE score at 4 h and next day for inpatients. Out-patients with a change in mini mental score underwent a repeat MMSE evaluation before discharge. VAS was also used to assess the ease of patient's post procedure management on the floor by nursing staff. The nursing staff also assessed patient's alertness immediately on arrival to the floor, at one and two hours using Observer's Assessment of Alertness/Sedation Scale (OAA/S).[29] The OAA/S is from 1 to 5 with 5 being fully alert and 1 deep sleep (5 = alert, 4 = lethargic, 3 = aroused by voice, 2 = aroused by shaking, 1 = deep sleep).
Baseline variables were expressed as mean ± SD or proportions. Change in MMSE was evaluated with repeated measures ANOVA. CAM score was evaluated with Chi-square test.
3. Results
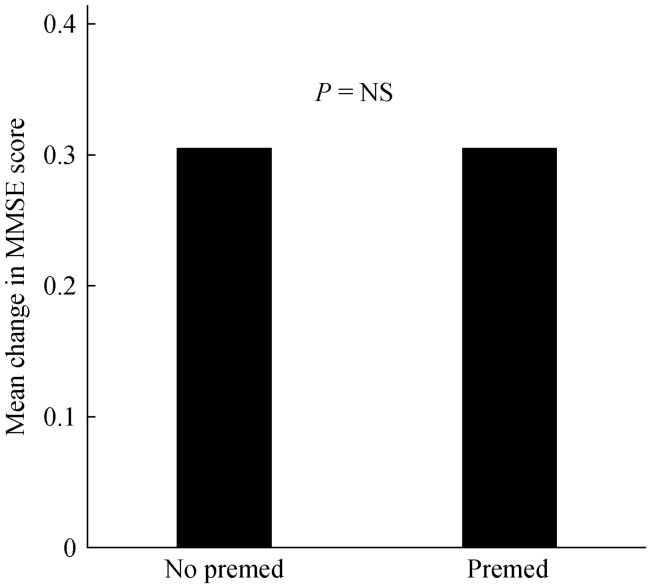
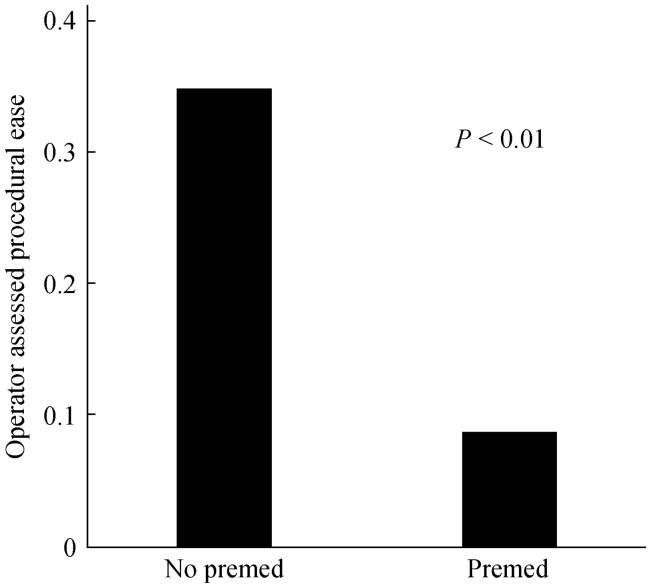
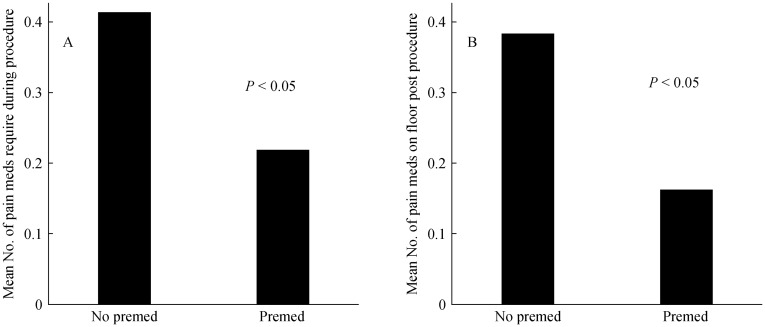
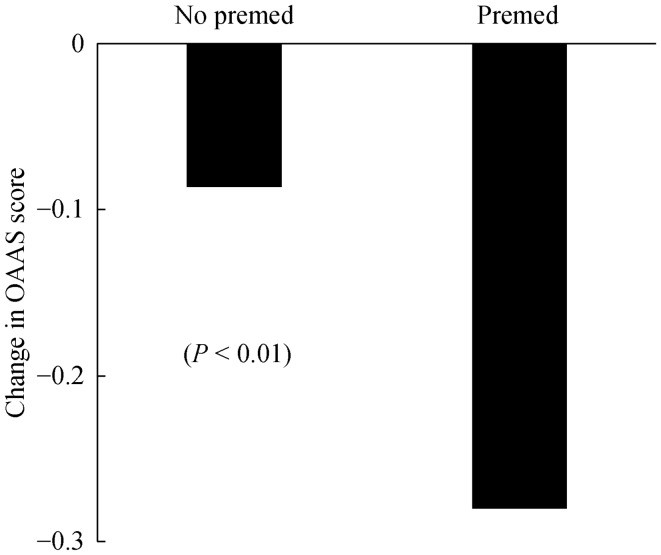
A total of 93 patients were enrolled in the study, of which 47 patients received premedication (diphenhydramine 25 mg and benzodiazepine 5 mg) prior to the procedure. Baseline characteristics are outlined in Table 1. The mean age was 77 ± 4.2 years, 56% were male and 53% were in-patients. The baselines mean MMSE was similar in each group (27.6 ± 1.4 in premedication group versus 28.17 ± 1.4 in patients without premedication). One patient had stroke during the procedure and therefore, post procedure observations were not made. None of the patients in either group developed delirium after the procedure as measured by CAM. The maximum decrease of MMSE score in either group was one point at any time post procedure which was not significant (Figure 1). There ease of procedure and patients' cooperation during the procedure was greater (P < 0.01) in the medicated group (Figure 2), and the pain medication requirement both during and after the procedure was higher (P < 0.05) in the group not premedicated (Figure 3). Premedicated patients were less alert (Figure 4) immediately and at 1 h after arrival on the floor (P ≤ 0.01). However, there was no difference of the level of alertness between the two groups at 2 h after arrival on the floor. There was a trend for nurses' assessment of the ease of patient management in the premedicated group (P = 0.08). Length of stay was similar for both groups. Two patients died during hospitalization, one after coronary artery bypass graft surgery and the second due to worsening heart failure. Neither of these two patients had delirium or change in MMSE score after the catheterization procedure.
Table 1. Baseline characteristics of the study patients.
| Premedication (n = 47) | No Premedication (n = 46) | |
| Age, yr | 78 ± 4.8 | 77 ± 3.5 |
| Male sex | 25 (53) | 28 (61) |
| Hypertension | 41 (87) | 39 (85) |
| Diabetes mellitus | 12 (26) | 13 (28) |
| Hyperlipidemia | 30 (64) | 35 (76) |
| Coronary artery disease | 16 (34) | 24 (52) |
| Anxiety | 15 (32) | 12 (26) |
| Depression | 6 (13) | 2 (4) |
| Delirium (past-history) | 2 (4) | 1 (2) |
| COPD | 3 (6) | 2 (4) |
| Atrial fibrillation | 6 (13) | 8 (17) |
| Employed | 2 (4) | 7 (15) |
| Medications | ||
| Aspirin | 35 (74) | 36 (78) |
| Beta blockers | 35 (74) | 33 (72) |
| ACEI/ARB | 29 (62) | 26 (57) |
| Statins | 27 (57) | 36 (78) |
| Diuretics | 16 (34) | 17 (37) |
| Sedatives | 6 (35) | 9 (20) |
| Antidepressants | 6 (13) | 2 (4) |
| Analgesics | 7 (15) | 9 (20) |
| Warfarin | 6 (13) | 9 (20) |
| Baseline MMSE | 27.7 ± 1.4 | 28.2 ±1.4 |
| In patients | 26 (55) | 23 (50) |
Data are presented as mean ± SD or n (%). ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; COPD: chronic obstructive pulmonary disease; MMSE: mini mental state exam.
Figure 1. Mini mental state exam changes in the premed and non-premed groups.
MMSE: mini-mental state examination; Premed: premedication.
Figure 2. Difference of ease of the procedure in the premed and non-premed groups.
Premed: premedication.
Figure 3. Pain medication requirements of premed and non-premed groups during (A) and after (B) procedure.
Premed: premedication.
Figure 4. Change of sedation level from baseline immediately on arrival to the floor after procedure.
OAAS: observer assessment of sedation; Premed: premedication.
4. Discussion
This is the first study to assess the effect of oral premedication with benzodiazepines and diphenhydramine on cognitive status of elderly patient during cardiac catheterization procedure. Although benzodiazepines and anticholinergics have been considered to cause delirium in elderly hospitalized patients, we did not observe any of these deleterious effects of premedication on the cognitive status of elderly patients undergoing cardiac catheterization procedure. The maximum decrease of MMSE score was also negligible.
Conscious sedation has been generally considered as an important component of a successful completion of invasive procedures as well as patient's satisfaction.[16],[30],[31] Many cardiologists use single oral dose of long acting benzodiazepine (diazepam) prior to a cardiac catheterization procedure to achieve better conscious sedation and alleviate anxiety. Diphenhydramine is also used along with diazepam for its antihistamine properties, and improved conscious sedation. Additionally, majority of the patients receive intravenous midazolam for improved sedation and fentanyl citrate for pain control during the procedure.
Most of the data regarding conscious sedation originate from endoscopic procedures.[30]–[32] The short acting benzodiazepine, midazolam, has been shown to be a safe and effective means of sedation in elderly patients undergoing endoscopic procedures. For cardiac procedures, the data of conscious sedation is mainly limited to electrophysiological studies.[33],[34] Conscious sedation with midazolam and fentanyl citrate has been found to be safe and efficacious for different electrophysiological procedures. Additionally, conscious sedation also provide better hemodynamic stability and patient cooperation without affecting the electrophysiological studies.[34] Premedication utilizing different combinations of diazepam, lorazepam, promethazine and diphenhydramine for cardiac catheterization did not cause over sedation or hypoxemia in one study.[35] Similarly in another study, conscious sedation using midazolam and fentanyl provided better hemodynamic stability during the procedure compared to placebo.[16]
In this study, we found higher pain medication (narcotics and non-narcotics) requirement among patients who did not receive oral premedication. This effect was likely due to a higher anxiety level as patients without premedication were more awake in the post procedure period. Although the pre-medicated patients were less alert immediately and at 1 h on arrival to the floor, the duration of this sedation was short and did not affect patients' cognitive status or planned discharge post procedure. We also found a trend of easier post procedure management (P = 0.08) of the pre-medicated group on the floor as reported by the nursing staff.
In the absence of randomized trials, the independent role of medication to cause delirium in elderly hospitalized patients is still not very clear. Most of the data is from retrospective reviews of elderly patients admitted with acute illness or post surgery. For example, Dasgupta, et al.[20] reported peri-operative medications as risk factor for development of delirium in patients underwent non-cardiac surgery. On the other hand, a large meta-analysis of twenty seven studies by Elie, et al.[21] revealed dementia, systemic illness, alcohol abuse and depression being the most common risk factors for development of delirium in elderly hospitalized patients while medications appeared to play only a contributory role.
More recently, a newer pharmaceutical agent, dexmedetomidine, an alpha 2 adrenergic receptor agonist with a relatively short half-life of two hours, is being increasingly used for various medical and surgical procedures.[36] Dexmedetomidine is well tolerated and has analgesic as well as sedative properties. In addition it has shown to reduce delirium and preserves respiratory function. The drug was initially approved and used only in the intubated patients especially patients in ICU. However, more recently dexmedetomidine is also being used in a number of clinical scenarios including non-intubated patients during endoscopic procedures. The anesthesiologists continue to administer and manage dexmedetomidine in non-intubated patients during the procedures. Considering well tolerated profile and reduced delirium side effects, we anticipate a wider future use of dexmedetomidine in the elderly non intubated patients including those undergoing cardiac catheterization.
Our study has several limitations. The study was done at a single institution and therefore our results may not be generalizable to other hospitals as the preprocedure protocols may not be similar to ours. Elderly patients with impaired cognitive status are at higher risk to develop delirium. This was not studied as baseline MMSE of our study subjects was not low (MMSE = 28), representing cognitively intact patients. Furthermore, the number of study subjects was also small. Although the study was non-blinded, the catheterization laboratory staff and nursing staff that took care of patients after the procedure and majority of the operators were unaware of the randomization.
In conclusion, oral premedication with single dose of diphenhydramine and diazepam did not cause delirium or confusion in elderly patients undergoing non-emergency cardiac catheterization. Premedication also did not affect the length of index hospitalization. In fact the lesser requirement of pain medication during and after procedure as well as improved procedural ease and post procedure management favors premedication in elderly patients undergoing cardiac catheterization.
Acknowledgments
We thank the nursing staff of cardiac telemetry floors, Day ward and cardiac catheterization laboratory of Baystate Medical Center, Springfield, MA, for their dedicated support to complete this study.
References
- 1.Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990;263:1097–1101. [PubMed] [Google Scholar]
- 2.Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275:852–857. [PubMed] [Google Scholar]
- 3.Iseli RK, Brand C, Telford M, et al. Delirium in elderly general medical inpatients: a prospective study. Intern Med J. 2007;37:806–811. doi: 10.1111/j.1445-5994.2007.01386.x. [DOI] [PubMed] [Google Scholar]
- 4.Edlund A, Lundström M, Karlsson S, et al. Delirium in older patients admitted to general internal medicine. J Geriatr Psychiatry Neurol. 2006;19:83–90. doi: 10.1177/0891988706286509. [DOI] [PubMed] [Google Scholar]
- 5.Bucht G, Gustafson Y, Sandberg O. Epidemiology of delirium. Dement Geriatr Cogn Disord. 1999;10:315–318. doi: 10.1159/000017161. [DOI] [PubMed] [Google Scholar]
- 6.Williams-Russo P, Urquhart BL, Sharrock NE, et al. Post-operative delirium: predictors and prognosis in elderly orthopedic patients. J Am Geriatr Soc. 1992;40:759–767. doi: 10.1111/j.1532-5415.1992.tb01846.x. [DOI] [PubMed] [Google Scholar]
- 7.Dasgupta M, Dumbrell AC. Preoperative risk assessment for delirium after noncardiac surgery: a systematic review. J Am Geriatr Soc. 2006;54:1578–1589. doi: 10.1111/j.1532-5415.2006.00893.x. [DOI] [PubMed] [Google Scholar]
- 8.Foy A, O'Connell D, Henry D, et al. Benzodiazepine use as a cause of cognitive impairment in elderly hospital inpatients. J Gerontol A Biol Sci Med Sci. 1995;50:99–106. doi: 10.1093/gerona/50a.2.m99. [DOI] [PubMed] [Google Scholar]
- 9.Gray SL, Lai KV, Larson EB. Drug-induced cognition disorders in the elderly: incidence, prevention and management. Drug Saf. 1999;21:101–122. doi: 10.2165/00002018-199921020-00004. [DOI] [PubMed] [Google Scholar]
- 10.Han L, McCusker J, Cole M, et al. Use of medications with anticholinergic effect predicts clinical severity of delirium symptoms in older medical inpatients. Arch Intern Med. 2001;161:1099–1105. doi: 10.1001/archinte.161.8.1099. [DOI] [PubMed] [Google Scholar]
- 11.McCusker J, Cole M, Dendukuri N, et al. Delirium in older medical inpatients and subsequent cognitive and functional status: a prospective study. CMAJ. 2001;165:575–583. [PMC free article] [PubMed] [Google Scholar]
- 12.McCusker J, Cole M, Abrahamowicz M, et al. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162:457–463. doi: 10.1001/archinte.162.4.457. [DOI] [PubMed] [Google Scholar]
- 13.Marcantonio ER, Flacker JM, Michaels M, et al. Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc. 2000;48:618–624. doi: 10.1111/j.1532-5415.2000.tb04718.x. [DOI] [PubMed] [Google Scholar]
- 14.Popovic J. 1999 National Hospital Discharge Survey: Annual Summary with Detailed Diagnosis and Procedure Data. Centers for Disease Control and Prevention web site. http://www.cdc.gov/nchs/about/major/hdasd/listpubs.htm (accessed on May 11, 2008) [DOI] [PubMed]
- 15.Etzioni DA, Liu JH, Maggard MA, et al. The aging population and its impact on the surgery workforce. Ann Surg. 2003;238:170–177. doi: 10.1097/01.SLA.0000081085.98792.3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baris S, Karakaya D, Aykent R, et al. Comparison of midazolam with or without fentanyl for conscious sedation and hemodynamics in coronary angiography. Can J Cardiol. 2001;17:277–281. [PubMed] [Google Scholar]
- 17.Pachulski RT, Adkins DC, Mirza H. Conscious sedation with intermittent midazolam and fentanyl in electrophysiology procedures. J Interv Cardiol. 2001;14:143–146. doi: 10.1111/j.1540-8183.2001.tb00725.x. [DOI] [PubMed] [Google Scholar]
- 18.Davidson CJ, Bonow RO. Cardiac Catheterization. In: Braunwald E, Libby P, Bonow RO, editors. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 7th Edition. Philadelphia, USA: Elsevier; 2005. pp. 395–422. [Google Scholar]
- 19.Christe C, Janssens JP, Armenian B, et al. Midazolam sedation for upper gastrointestinal endoscopy in older persons: a randomized, double, placebo-controlled study. J Am Geriatr Soc. 2000;48:1398–1403. doi: 10.1111/j.1532-5415.2000.tb02628.x. [DOI] [PubMed] [Google Scholar]
- 20.Dasgupta M, Dumbrell AC. Preoperative risk assessment for delirium after noncardiac surgery: a systematic review. J Am Geriatr Soc. 2006;54:1578–1589. doi: 10.1111/j.1532-5415.2006.00893.x. [DOI] [PubMed] [Google Scholar]
- 21.Elie M, Cole MG, Primeau FJ, et al. Delirium risk factors in elderly hospitalized patients. J Gen Intern Med. 1998;13:204–212. doi: 10.1046/j.1525-1497.1998.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O'Keeffe ST, Mulkerrin EC, Nayeem K, et al. Use of serial Mini-Mental State Examinations to diagnose and monitor delirium in elderly hospital patients. J Am Geriatr Soc. 2005;53:867–870. doi: 10.1111/j.1532-5415.2005.53266.x. [DOI] [PubMed] [Google Scholar]
- 23.Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 24.Kahle-Wrobleski K, Corrada MM, Li B, et al. Sensitivity and specificity of the Mini-Mental State Examination for identifying dementia in the oldest-old: the 90+ study. J Am Geriatr Soc. 2007;55:284–289. doi: 10.1111/j.1532-5415.2007.01049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Inouye SK, van Dyck C, Alessi CA, et al. Clarifying Confusion: The Confussion Asessment Method: a new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 26.Laurila JV, Pitkala KH, Strandberg TE, et al. Confusion assessment method in the diagnostics of delirium among aged hospital patients: would it serve better in screening than as a diagnostic instrument? Int J Geriatr Psychiatry. 2002;17:1112–1119. doi: 10.1002/gps.753. [DOI] [PubMed] [Google Scholar]
- 27.Lynch EP, Lazor MA, Gellis JE, et al. The impact of postoperative pain on the development of postoperative delirium. Anesth Analg. 1998;86:781–785. doi: 10.1097/00000539-199804000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Kuganeswaran E, Clarkston WK, Cuddy PG, et al. A double-blind placebo controlled trial of oral midazolam as premedication before flexible sigmoidoscopy. Am J Gastroenterol. 1999;94:3215–3219. doi: 10.1111/j.1572-0241.1999.01521.x. [DOI] [PubMed] [Google Scholar]
- 29.Chernik DA, Gillings D, Laine H, et al. Validity and reliability of the Observer's Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990;10:244–251. [PubMed] [Google Scholar]
- 30.Tu RH, Grewall P, Leung JW, et al. Diphenhydramine as an adjunct to sedation for colonoscopy: a double-blind randomized, placebo-controlled study. Gastrointest Endosc. 2006;63:87–94. doi: 10.1016/j.gie.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 31.Thompson DG, Lennard-Jones JE, Evans SJ, et al. Patients appreciate premedication for endoscopy. Lancet. 1980;2:469–470. doi: 10.1016/s0140-6736(80)91899-1. [DOI] [PubMed] [Google Scholar]
- 32.Morrow JB, Zuccaro G, Jr, Conwell DL, et al. Sedation for colonoscopy using a single bolus is safe, effective, and efficient: a prospective, randomized, double-blind trial. Am J Gastroenterol. 2000;95:2242–2247. doi: 10.1111/j.1572-0241.2000.02308.x. [DOI] [PubMed] [Google Scholar]
- 33.Pachulski RT, Adkins DC, Mirza H. Conscious sedation with intermittent midazolam and fentanyl in electrophysiology procedures. J Interv Cardiol. 2001;14:143–146. doi: 10.1111/j.1540-8183.2001.tb00725.x. [DOI] [PubMed] [Google Scholar]
- 34.Lau W, Kovoor P, Ross DL. Cardiac electrophysiologic effects of midazolam combined with fentanyl. Am J Cardiol. 1993;72:177–182. doi: 10.1016/0002-9149(93)90156-7. [DOI] [PubMed] [Google Scholar]
- 35.Bergeron P, Enns J, Delima L, et al. Effects of routine premedication for cardiac catheterization on sedation, level of anxiety and arterial oxygen saturation. Can J Cardiol. 1995;11:201–205. [PubMed] [Google Scholar]
- 36.Shagufta Naaz, Erum Ozair. Dexmedetomidine in current anaesthesia practice—a review. J Clin Diagn Res. 2014;8:GE1–GE4. doi: 10.7860/JCDR/2014/9624.4946. [DOI] [PMC free article] [PubMed] [Google Scholar]