Abstract
Platypnea orthodeoxia syndrome is associated with dyspnea and arterial oxygen desaturation accentuated by an upright posture. It can be secondary to an intracardiac shunt. We report a case of platypnea-orthodeoxia syndrome (POS) in a 58-year old male patient who had a pre-existing patent foramen ovale (PFO) and substantial pulmonary pathologies. He was successfully treated by percutaneous transcatheter closure of the PFO. Our case highlights the importance of recognition of this rare syndrome in patients who present with unexplained hypoxia for whom transcatheter closure of the interatrial shunt can be safely carried out.
Keywords: Intracardiac shunt, Platypnea-orthodeoxia syndrome, Patent foramen ovale, Transcatheter closure
1. Introduction
Platypnea-orthodeoxia syndrome is marked by dyspnea and arterial oxygen desaturation, which is accentuated by an upright posture and relieved by recumbency.[1] This rare condition develops in patients who have an existing interatrial communication via an atrial septal defect (ASD) such as patent foramen ovale (PFO) or fenestrated atrial septal aneurysm.[2] The syndrome is normally detected in patients who suffer from pulmonary diseases such as pneumonectomy, pulmonary embolism, other chronic lung diseases or aortic root disease.[3] Herein, we report the findings of a case of platypnea-orthodeoxia syndrome that was successfully treated by percutaneous transcatheter closure of a pre-existing PFO.
2. Case Report
A 58-year-old male was admitted to our department because of aggravated chest tightness and shortness of breath for one month. The patient suffered repeated episodes of shortness of breath and chest tightness for two years, which were accentuated by an upright position, but not by exertion. He complained of no chest pain and had no history of hypertension, diabetes or atrial fibrillation.
Physical examination was unremarkable except diminished breath sound of the right lower lung. No wet or dry rales were heard. PO2 was 46 mmHg and PCO2 was 40 mmHg. Transcutaneous oxygen saturation (SaO2) was 97%−98% in the supine position and 78%−85% in the upright position while the patient was on continuous oxygen therapy (6−8 L/min). No other obvious laboratory abnormalities were found.
Cerebral computed tomography (CT) scan showed multiple old lacunar infarcts and brain atrophy (Figure 1A). Chest CT scan revealed right middle lobe atelectasis, right upper lobe bullae, right lower lobe calcification, right diaphragm elevation and mediastinal lymph node calcification (Figure 1B). ECG was normal, and angiography revealed no significant coronary artery stenosis (Figure 1C), no pulmonary embolism and pulmonary arteriovenous fistula (Figure 1D). Bronchoscopy showed inflammatory changes in the bilateral bronchi and the posterior segment of the right lower lobe. Transcranial Doppler (TCD) foaming test revealed numerous raindrop beaded curtain-like micro-embolism signals lasting approximately 2 min (Figure 2A). Valsalva test was not performed because of obvious shortness of breath in the patient. Transthoracic echocardiography demonstrated left to right shunt at the atrial level due to a patent foramen ovale. Pulmonary artery pressure is normal, and right heart angiography showed a large number of micro-bubbles in the resting state (Figure 2B). Platypnea-orthodeoxia syndrome was contemplated.
Figure 1. Results of computed tomography and angiography.
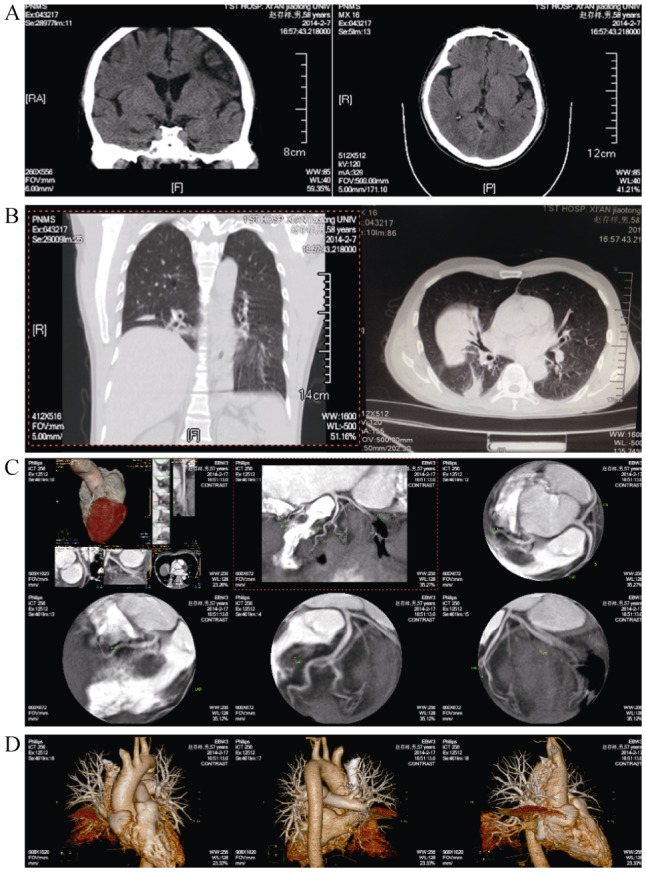
(A): Cerebral computed tomography scan showed multiple old lacunar infarcts and brain atrophy; (B): chest computed tomography scan reveals right middle lobe atelectasis, right upper lobe bullae, right lower lobe calcification, right diaphragm elevation and mediastinal lymph node calcification; (C): angiography revealed no significant coronary artery stenosis; (D): angiography revealed no pulmonary embolism and pulmonary arteriovenous fistula.
Figure 2. Diagnosis, treatment and subsequent visit of this PFO patient.
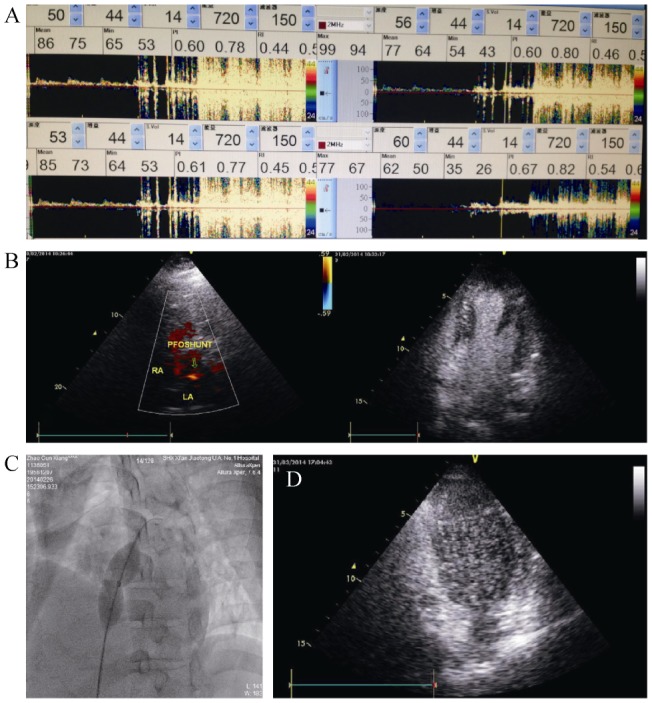
(A): TCD foaming test reveals raindrop beaded curtain-like micro-embolism signals lasting approximately 2 min; (B): transthoracic echocardiography and right heart angiography demonstrates left to right shunt in the atrial level and the presence of a patent foramen ovale and numerous micro-bubbles; (C): 24-mm balloon was advanced to determine the size of the PFO and the inflated balloon waist was 15 mm. A closure test was conducted simultaneously and the balloon was set right in the foramen ovale for 30 min under non-oxygen condition; (D): right heart angiography reveals substantial reduction in the amount of micro-bubbles one month after operation. PFO: patent foramen ovale; TCD: transcranial Doppler.
The patient underwent transcatheter PFO closure. Right heart catheterization showed normal pulmonary artery pressure and oval fossa angiography revealed a large PFO. A 24-mm balloon was advanced to determine the size of the PFO and the inflated balloon waist was 15 mm. A closure test was conducted simultaneously and the balloon was set right in the foramen ovale for 30 min under non-oxygen condition (Figure 2C). Transcutaneous oxygen saturation changed from 92% to 97% and shortness of breath and chest tightness of the patient were relieved. A 20 mm ASD occluder was then placed.
The symptoms in the patient were improved significantly after PFO closure, the femoral arterial SaO2 in the upright position increased from 85.7% to 95.8%, and PO2 increased from 46 mmHg to 76 mmHg. One month after the operation, pulse oximetry revealed a radial artery PO2 of 79.3 mmHg in the supine position and.83.6 mmHg in the upright position. SaO2 was 95.4% in the supine position and 96.5% in the upright position. The patient only had slight chest tightness and his daily lives were not affected. Right heart angiography showed that the micro-bubbles were reduced significantly (Figure 2D).
3. Discussion
We describe a case of platypnea-orthodeoxia syndrome (POS) in a patient with preexisting PFO who was successfully managed by transcatheter PFO closure. The causes and pathophysiology of POS remain unelucidated.[4] Intracardiac shunting, pulmonary vascular shunting, or ventilation/perfusion mismatch due to pulmonary parenchymal diseases or a combination of these mechanisms is likely contributory to POS. Intracardiac shunting is predominantly due to a PFO as in the current case and, less frequently, due to an ASD as a PFO/ASD is present in up to 30% of adults. What triggers POS remains unclear. Our patient had substantial pulmonary pathologies, which, together with a PFO, may cause the onset of POS.
For definitive diagnosis of POS, TCD and transthoracic echocardiography is important, allowing localization, visualization and semi-quantification of the shunt at the atrial level. In our patient, anatomic shunts were sought using microbubble injection during transesophageal echocardiography, which clearly demonstrated the presence of left to right shunt at the atrial level. In rare cases, the shunt is seen only on Valsalva maneuvers, which, however, was not performed in our patient because of his apparent shortness of breath. Oxygen supplementation may also aid the identification of POS as the right-to-left atrial shunt prevents systemic oxygen saturation reaching 100% in an upright posture. SaO2 was 97%–98% in our patient in the supine position but only 78%–85% in the upright position despite he was receiving continuous oxygen therapy. POS is typically treated by closure of the interatrial shunt and most patients improved almost thoroughly following transcatheter closure of the interatrial shunt. Our patient showed marked alleviation in symptoms and SaO2 and his quality of life rapidly improved following PFO closure.
The most revelatory experience that this rare case gives us is that when a patient has unexplained orthostatic hypoxemia, especially when pulmonary disease is present, a PFO should be suspected. The presence of a POS should be contemplated when accentuated oxygenation failure occurs when a patient assumes an upright posture. In addition, whether the patient with such condition should have occluder treatment requires a comprehensive assessment. Our case highlights the importance of recognition of this rare syndrome in patients who present with unexplained hypoxia for whom transcatheter closure of the interatrial shunt can be safely carried out.
Acknowledgments
This research was supported by Science and Technology Innovative Project Program of Shaanxi Province (Grant No.:2014KTCL03-11).
References
- 1.Velagapudi P, Turagam M, Agrawal H, et al. Cardiac platypnea-orthodeoxia syndrome secondary to patent formen ovale. J Am Coll Cardiol. 2014;63(Suppl 1):A628. [Google Scholar]
- 2.Ning M, Lo EH, Ning PC, et al. The brain's heart-therapeutic opportunities for patent foramen ovale (PFO) and neurovascular disease. Pharmacol Ther. 2013;139:111–123. doi: 10.1016/j.pharmthera.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zavalloni D, Lisignoli V, Barbaro C, et al. Platypnoea-orthodeoxia syndrome secondary to patent foramen ovale (PFO): a challenging subset for PFO percutaneous closure. Heart Lung Circ. 2013;22:642–646. doi: 10.1016/j.hlc.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 4.Chopard R, Meneveau N. Right-to-left atrial shunting associated with aortic root aneurysm: a case report of a rare cause of platypnea-orthodeoxia syndrome. Heart Lung Circ. 2013;22:71–75. doi: 10.1016/j.hlc.2012.08.007. [DOI] [PubMed] [Google Scholar]


