Abstract
Ischemia of the basilar artery is one of the most devastating types of arterial occlusive disease. Despite treatment of basilar artery occlusions (BAO) with intravenous tissue plasminogen activator, antiplatelet agents, intra-arterial therapy or a combination, fatality rates remain high. Aggressive recanalization with mechanical thrombectomy is therefore often necessary to preserve life. When direct access to the basilar trunk is not possible, exploration of chronically occluded vessels through collaterals with angioplasty and stenting creates access for manual aspiration. We describe the first report of retrograde vertebral artery (VA) revascularization using thyrocervical collaterals for anterograde mechanical aspiration of a BAO followed by stenting of the chronically occluded VA origin. Our novel retrograde–anterograde approach resulted in resolution of the patient's clinical stroke syndrome.
Keywords: Stroke, Thrombectomy, Technique, Stent, Intervention
Background
The first detailed description of basilar artery occlusion (BAO) was documented by Kubik and Adams1 in 1946. Approximately 60% of patients have prodromal transient ischemic attacks consisting of vertigo, nausea, and headaches. More serious sequelae range from seizures to tetraplegia and a locked-in-state.2
Despite advances in antithrombotic and antiplatelet medications, mortality remains high. In 2009 the Basilar Artery International Cooperation Study (BASICS), the largest BAO data registry, showed 54% mortality among conventionally treated patients, with only 3% having a good outcome.3 Outcomes data from this and several other studies are shown in table 1.
Table 1.
Outcomes data of non-surgical and surgical treatment of basilar artery occlusion
| Oral antithrombotics |
Intravenous thrombolysis |
Intra-arterial thrombolysis |
|||||
|---|---|---|---|---|---|---|---|
| BASICS4* Severe Deficit† | Broussalis et al5 | Schonewille et al6 | BASICS4* Severe Deficit† | SAMURAI 7‡ | BASICS4* Severe Deficit† | Jung et al8 | |
| Patients (n) | 79 | 22 | 82 | 72 | 23 | 196 | 106 |
| Recanalization rate (%) | – | 9 | – | 66 | 78 | 69 | 70 |
| Good outcome (mRS 0–2) (%) | 3 | 0 | 21 (mRS 0–3) | 21 | 44 | 11 | 33 |
| Poor outcome (mRS 4–5) (%) | 38 | 50 | 39 | 28 | 48 | 34 | 13 |
| Death (mRS 6) (%) | 54 | 41 | 40 | 46 | 4 | 49 | 41 |
| Combination of intra-arterial thrombolysis and abciximab |
Endovascular mechanical recanalization |
|||||||
|---|---|---|---|---|---|---|---|---|
| Barlinn et al9 | Chiti et al10 | Nagel et al11 | Broussalis12 et al | Baek et al13 | Jankowitz et al14 | Mohlenbruch et al15 | Mordasini et al16 | |
| Patients (n) | 20 | 10 | 43 | 77 | 25 | 6 | 24 | 14 |
| Recanalization rate (%) | 85 | 100 | 84 | 36 | 96 | 100 | 88 | 79 |
| Good outcome (mRS 0–2) (%) | 15 (mRS 0–3) | 80 | 19 | 45 | 48 | 83 | 33 | 29 |
| Poor outcome (mRS 4–5) (%) | 40 | 10 | 23 | 29 | – | 17 | 21 | 36 (mRS 3–5) |
| Death (mRS 6) (%) | 45 | 10 | 42 | 10 | 12 | 0 | 29 | 36 |
*The BASICS group defined the intra-arterial thrombolysis group as those receiving pharmacological, mechanical thrombolysis, or a combination of both.
†The severe deficit group is defined as patients who presented tetraplegic, comatose, or in a locked-in-state.
‡The Stroke Acute Management with Urgent Risk Factor Assessment and Improvement (SAMURAI): recombinant tissue plasminogen activator registry.
BASICS, Basilar Artery International Cooperation Study; mRS, modified Rankin Scale.
More sophisticated treatment modalities include intravenous thrombolysis (IVT), intra-arterial thrombolysis (IAT), and mechanical thrombectomy (MT). The BASICS registry reported no significant difference in good outcomes despite the more frequent use of IAT, including MT. However, patients who presented with severe deficits (defined as tetraplegia, coma, or locked-in-state) and underwent IVT or IAT showed a 19% and 10% lower absolute risk of death or dependency, respectively, compared with the IAT group. No significant differences were seen between the IVT and IAT groups.3 Mattle et al17 published a review of BAO case series from 1990 to 2011, which found no significant difference between the various treatment modalities.
Given the high mortality and poor recanalization rates of medical interventions, MT is often necessary. MT of BAO is commonly approached via transfemoral, direct VA access, and transcirculation routes through a patent posterior communicating artery (PCoA). When these approaches are not possible, exploration of chronically occluded vessels through collaterals with angioplasty and stenting remains a feasible though technically challenging option. Here we describe mechanical aspiration of a BAO via a transfemoral route after opening a chronically occluded VA through a retrograde–anterograde approach followed by stent placement across the previously occluded VA origin.
Case presentation
An elderly patient with a right femoral artery occlusion requiring thrombectomy and anticoagulation became acutely unresponsive. A CT scan demonstrated a subacute right cerebellar hypodensity in the superior cerebellar artery distribution. A CT angiogram of the brain showed a BAO, bilateral VA occlusions, and reconstitution of the left V3 segment via collaterals from the thyrocervical trunk. Tissue plasminogen activator (t-PA) was contraindicated due to the heparin infusion and recent surgery. The right femoral artery was not used because of the recent surgical thrombectomy. The left common femoral artery was accessed using a 10 cm/6 Fr sheath and diagnostic runs were performed using a 100 cm Simmons-2 catheter. The left subclavian artery demonstrated an occluded left VA with no evidence of an ostium, and a hypoplastic right VA (figure 1). The left proximal subclavian was explored with a Synchro (Stryker) and V-18 control wire (Boston-Scientific) but the left VA origin could not be traversed. The left thyrocervical trunk demonstrated a distal circuitous collateral that reconstituted the V3 segment of the VA. The PCoAs were diminutive bilaterally and no opacification of the basilar trunk was seen (figure 1).
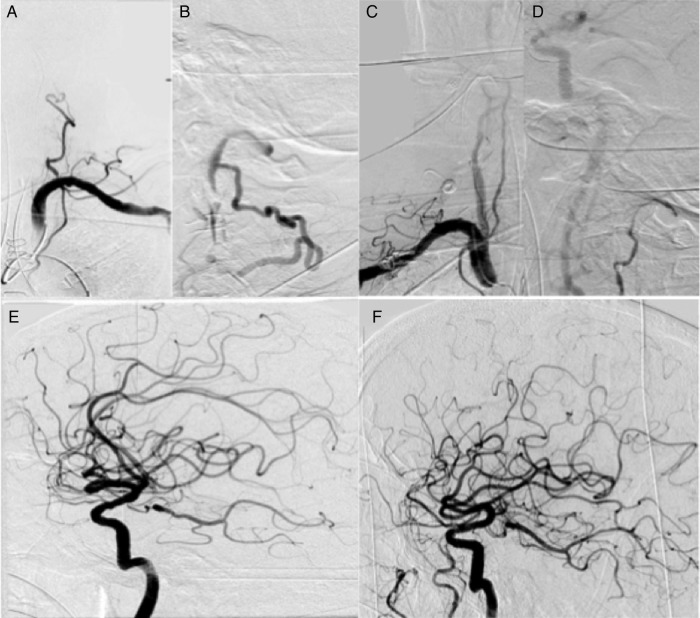
Figure 1.
Left subclavian anteroposterior (A) and lateral (B) injection demonstrating a completely occluded left vertebral artery (VA) with distal reconstitution of the V3 segment via tortuous muscular collaterals from the thyrocervical trunk. Right subclavian anteroposterior (C) and lateral (D) injection showing a hypoplastic VA with no intracranial opacification of the posterior circulation. Right (E) and left (F) internal carotid artery lateral injection demonstrating diminutive posterior communicating arteries bilaterally with no retrograde flow down the basilar.
The plan was to revascularize the left VA in a two-stage approach. The first step involved a retrograde route up the thyrocervical collateral to the V3 segment and down through the occluded VA origin. The second stage involved an antegrade approach, advancing the base catheter through the revascularized VA with MT of the BAO using distal access catheters for aspiration followed by stenting of the VA origin. Selective catheterization of the left VA via the large thyrocervical trunk collateral was performed. Using two 300 cm V-18 control wires, the Simmons-2 catheter was exchanged for a 90 cm/6 Fr Neuron Max (Penumbra) and advanced proximal to the thyrocervical trunk origin. The V-18 control wires were maintained in the distal axillary artery for stability. A triaxial system consisting of a 4.3 Fr/136 cm distal access catheter (Concentric Medical), an 18 L Merci microcatheter (Concentric Medical), and a 300 cm/0.014 inch Synchro was advanced to the distal ascending cervical anastomosis with the V3 segment. The system was then advanced retrograde down the left VA through the origin occlusion into the left subclavian artery. The distal access catheter and 18 L microcatheter were removed and a 3.00 mm×8 mm Trek balloon was advanced across the origin and angioplasty was performed. Subsequent control runs revealed filling of the left VA (figure 2). A 6 Fr Neuron Max was advanced into the now patent distal V2 segment. A control run confirmed occlusion of the mid-basilar segment. A triaxial system consisting of 058–115 cm distal access catheter, 18 L microcatheter, and Synchro was advanced across the basilar occlusion followed by manual aspiration of a large 7 mm×0.5 mm thrombus on a single pass and control runs demonstrated Thrombolysis in Myocardial Infarction/Thrombolysis in Cerebral Infarction grade 3 flow (figures 3 and 4) 2.5 h after groin puncture. After revascularization, the left VA origin was stented using a Mini Trek 2.0 mm×8 mm balloon mounted stent with good persistent patency. The femoral artery was closed using a 6 Fr Angio-Seal. The following morning the patient was awake, alert, and following commands with 4/5 muscle tone in all four extremities, but remained intubated for congestive heart failure. MRI demonstrated minimal strokes and no hemorrhagic conversion (figure 5).
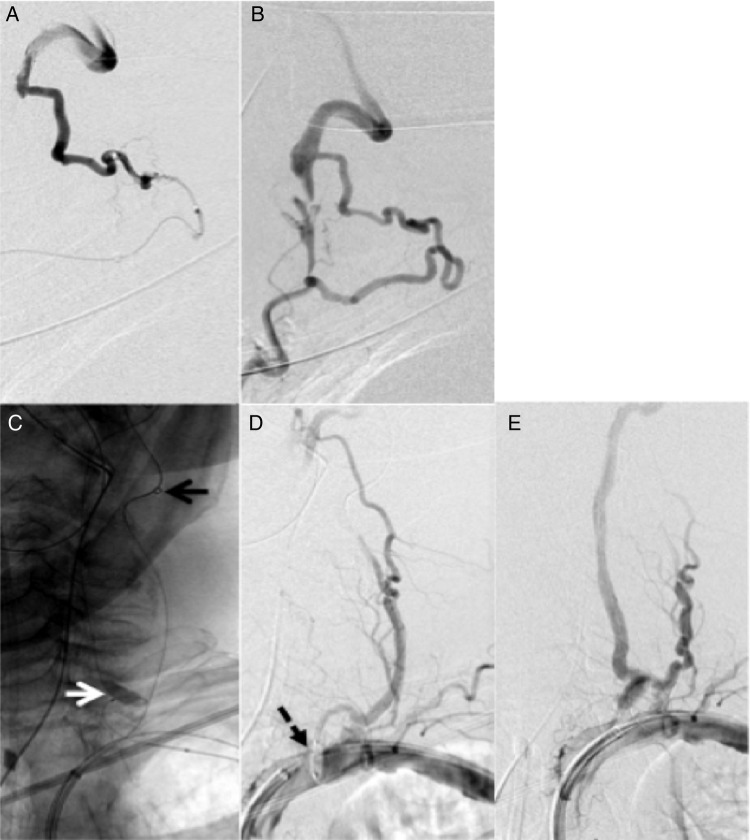
Figure 2.
Selected left thyrocervical anteroposterior (A) and lateral (B) injection demonstrating circuitous collaterals to the left V3 segment. The triaxial system was placed anterograde up the left thyrocervical trunk (C) using a 4.3 Fr distal access catheter (black arrow) and retrograde access down the left vertebral artery (VA) through the occlusion at the origin into the left subclavian using an 18 L and synchro (white arrow). A 3.00 mm×8 mm balloon (dashed black arrow) was advanced across the lesion (D). Post-angioplasty runs demonstrate anterograde flow through the left VA (E).
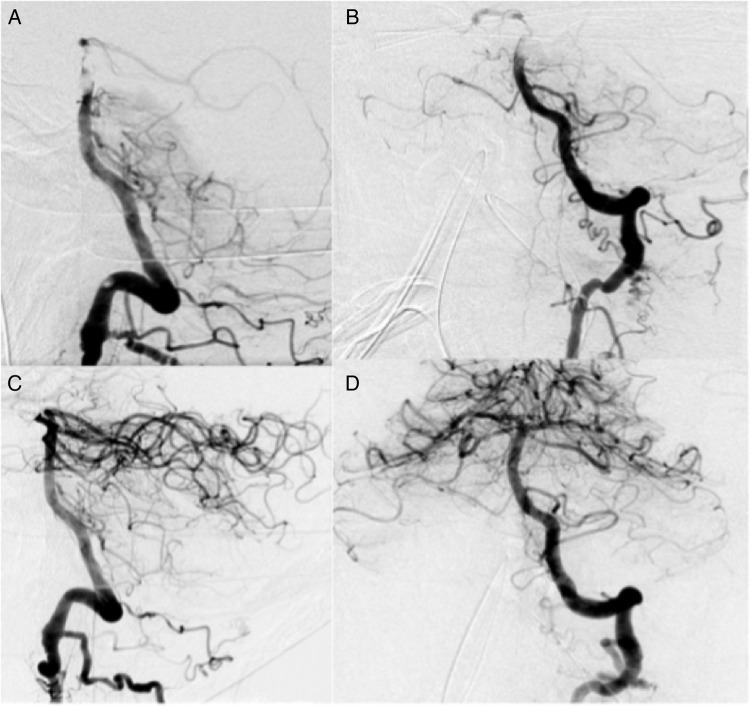
Figure 3.
Lateral (A) and anteroposterior (B) projections of left vertebral artery (VA) runs after initial revascularization of the left VA demonstrating a thrombus in the distal basilar artery. Lateral (C) and anteroposterior (D) projections of the left VA after thrombectomy of basilar artery thrombus.
Figure 4.
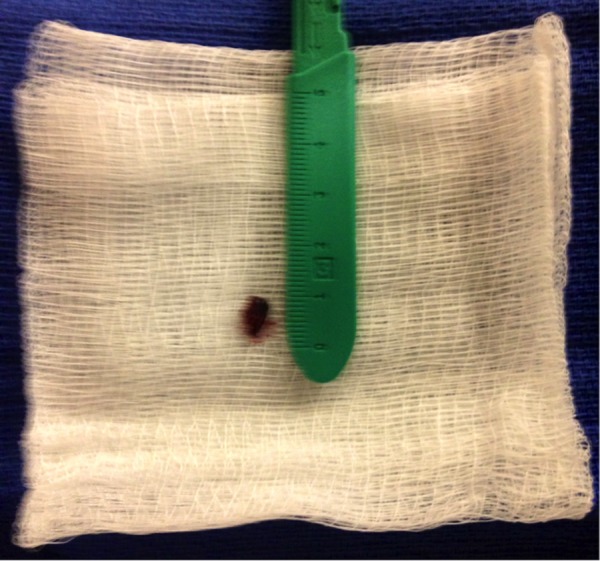
8×2 mm thrombus evacuated from the mid-basilar trunk.
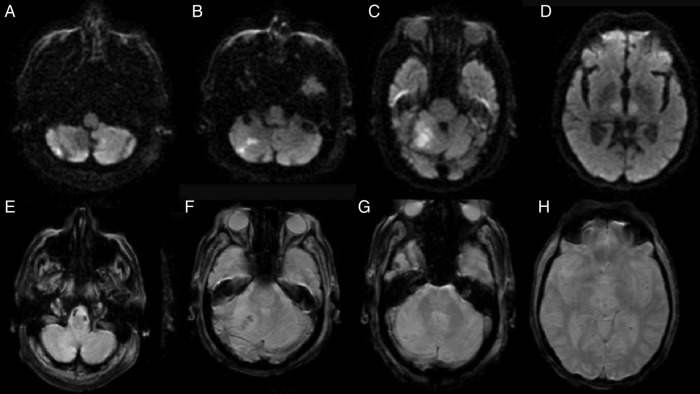
Figure 5.
(A–D) Axial diffusion-weighted MRI sequences after the procedure demonstrating small focal infarcts. (E–H) Axial MRI selective weighted angiography demonstrating no hemorrhagic conversion of the stroke.
Despite neurological recovery, the patient was ultimately palliated for inoperable recurrent bacterial endocarditis found after emergency thrombectomy.
Discussion
Advances in endovascular technology permit novel approaches for thrombolysis and thrombectomy of BAO when standard approaches are not possible. Liu et al4 described the anterior–posterior revascularization method for MT of BAO through a patent PCoA in a patient with a left VA occlusion and unfavorable right VA with a prior stent across the origin. Additionally, Hui et al18 reported successful revascularization of a middle cerebral artery (MCA) occlusion via a posterior circulation approach using a patent PCoA and MT. Although MT was not used, Kole et al19 and Ozdemir et al12 have demonstrated that MCA occlusions may be recanalized with IA-tPA using a patent PCoA with excellent clinical outcomes.
Here we describe the first report of retrograde VA revascularization using thyrocervical collaterals for anterograde mechanical aspiration of a BAO followed by stenting of the chronically occluded VA origin. Recanalization of a BAO through chronically occluded vessels or cervical collaterals may be necessary when direct access to the basilar trunk is not practical. Given the morbidity and mortality associated with BAO, we recommend aggressive recanalization of the vertebrobasilar system through both direct and indirect routes.
Learning points.
The literature on basilar artery occlusion (BAO) outcomes is conflicting and there is currently no gold standard of treatment.
Aggressive mechanical recanalization is often necessary when medical interventions fail as patients with BAO have a poor prognosis.
When direct access is not feasible, attempts should be made to explore chronically occluded vessels or cervical collaterals.
Footnotes
Contributors: AM contributed to the design of the work, performed the literature search, drafted the manuscript, revised it critically for intellectual content, and approved the final version for publication. PVP managed the case, had the idea for the article, drafted the manuscript, revised it critically for intellectual content, and approved the final version for publication. AJ guided the article towards its final draft, revised it critically for intellectual content, and approved the final version for publication. TJ managed the case, had the idea for the article, is the guarantor, and approved the final version for publication.
Competing interests: None declared.
Patient consent: Not obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kubik CS, Adams RD. Occlusion of the basilar artery; a clinical and pathological study. Brain 1946;69:73–121. 10.1093/brain/69.2.73 [DOI] [PubMed] [Google Scholar]
- 2.Ferbert A, Bruckmann H, Drummen R. Clinical features of proven basilar artery occlusion. Stroke 1990;21:1135–42. 10.1161/01.STR.21.8.1135 [DOI] [PubMed] [Google Scholar]
- 3.Schonewille WJ, Wijman CA, Michel P et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol 2009;8:724–30. 10.1016/S1474-4422(09)70173-5 [DOI] [PubMed] [Google Scholar]
- 4.Liu W, Kung DK, Mahaney KB et al. Anterior-to-posterior circulation approach for mechanical thrombectomy of an acutely occluded basilar artery using the penumbra aspiration system. World Neurosurg 2012;77:398.E17–20. 10.1016/j.wneu.2011.04.025 [DOI] [PubMed] [Google Scholar]
- 5.Broussalis E, Hitzl W, McCoy M et al. Comparison of endovascular treatment versus conservative medical treatment in patients with acute basilar artery occlusion. Vasc Endovasc Surg 2013;47:429–37. 10.1177/1538574413488458 [DOI] [PubMed] [Google Scholar]
- 6.Schonewille WJ, Algra A, Serena J et al. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry 2005;76:1238–41. 10.1136/jnnp.2004.049924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miyagi T, Koga M, Shiokawa Y et al. Intravenous alteplase at 0.6 mg/kg for acute stroke patients with basilar artery occlusion: the Stroke Acute Management with Urgent Risk factor Assessment and Improvement (SAMURAI) recombinant tissue plasminogen activator registry. J Stroke Cerebrovasc Dis 2013;22:1098–106. 10.1016/j.jstrokecerebrovasdis.2012.08.013 [DOI] [PubMed] [Google Scholar]
- 8.Jung S, Mono ML, Fischer U et al. Three-month and long-term outcomes and their predictors in acute basilar artery occlusion treated with intra-arterial thrombolysis. Stroke 2011;42:1946–51. 10.1161/STROKEAHA.110.606038 [DOI] [PubMed] [Google Scholar]
- 9.Barlinn K, Becker U, Puetz V et al. Combined treatment with intravenous abciximab and intraarterial tPA yields high recanalization rate in patients with acute basilar artery occlusion. J Neuroimag 2012;22:167–71. 10.1111/j.1552-6569.2011.00584.x [DOI] [PubMed] [Google Scholar]
- 10.Chiti A, Gialdini G, Terni E et al. Intra-arterial tissue plasminogen activator and abciximab in patients with acute basilar artery occlusion. Neurol Sci 2013;34:1871–3. 10.1007/s10072-013-1465-y [DOI] [PubMed] [Google Scholar]
- 11.Nagel S, Schellinger PD, Hartmann M et al. Therapy of acute basilar artery occlusion: intraarterial thrombolysis alone vs bridging therapy. Stroke 2009;40:140–6. 10.1161/STROKEAHA.108.526566 [DOI] [PubMed] [Google Scholar]
- 12.Ozdemir O, Bussiere M, Leung A et al. Intra-arterial thrombolysis of occluded middle cerebral artery by use of collateral pathways in patients with tandem cervical carotid artery/middle cerebral artery occlusion. AJNR Am J Neuroradiol 2008;29:1596–600. 10.3174/ajnr.A1163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baek JM, Yoon W, Kim SK et al. Acute basilar artery occlusion: outcome of mechanical thrombectomy with Solitaire stent within 8 hours of stroke onset. AJNR Am J Neuroradiol 2014;35:989–93. 10.3174/ajnr.A3813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jankowitz BT, Aleu A, Lin R et al. Endovascular treatment of basilar artery occlusion by manual aspiration thrombectomy. J Neurointerv Surg 2010;2:110–14. 10.1136/jnis.2009.001420 [DOI] [PubMed] [Google Scholar]
- 15.Mohlenbruch M, Stampfl S, Behrens L et al. Mechanical thrombectomy with stent retrievers in acute basilar artery occlusion. AJNR Am J Neuroradiol 2014;35:959–64. 10.3174/ajnr.A3796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mordasini P, Brekenfeld C, Byrne JV et al. Technical feasibility and application of mechanical thrombectomy with the Solitaire FR revascularization device in acute basilar artery occlusion. AJNR Am J Neuroradiol 2013;34:159–63. 10.3174/ajnr.A3168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mattle HP, Arnold M, Lindsberg PJ et al. Basilar artery occlusion. Lancet Neurol 2011;10:1002–14. 10.1016/S1474-4422(11)70229-0 [DOI] [PubMed] [Google Scholar]
- 18.Hui FK, Narayanan S, Cawley CM. Posterior-to-anterior circulation access using the Penumbra Stroke System for mechanical thrombectomy of a right middle cerebral artery thrombus. World Neurosurg 2010;73:17–21. 10.1016/j.surneu.2009.05.020 [DOI] [PubMed] [Google Scholar]
- 19.Kole MK, Pelz DM, Lee DH et al. Intra-arterial thrombolysis of embolic middle cerebral artery using collateral pathways. Can J Neurol Sci 2005;32:257–60. 10.1017/S031716710000408X [DOI] [PubMed] [Google Scholar]