Abstract
A 22-year-old male patient presented with a 3-day history of abdominal pain, diarrhoea, nausea and vomiting. He reported abdominal distention of a couple of weeks’ duration. He had been hospitalised 7 months earlier, owing to the same symptoms, however, the cause was never clarified. Initial examination showed abdominal distention and blood tests indicated eosinophilia. An abdominal CT scan showed mild ascites and a diffuse thickening of the small intestinal loops, and a cystic formation 3 cm in diameter on the liver. The differential diagnosis included parasite infection and eosinophilic gastroenteritis. Liver MRI revealed a simple biliary cyst. Microbiological tests, stool and blood cultures as well as stool examination for parasites were negative. The diagnostic paracentesis revealed eosinophilic ascites. An endoscopy was performed and histopathology revealed presence of moderate to marked lymphoplasmacytic infiltrate containing eosinophils, compatible with eosinophilic gastroenteritis. The patient responded well to the initiation of corticosteroids.
Background
This case illustrates a rare and heterogeneous condition with a varied presentation. It is characterised by eosinophilia, eosinophilic infiltration of the bowel wall and a wide variety of gastrointestinal symptoms. In fact, eosinophilic gastroenteritis (EG) should be suspected in any patient with gastrointestinal symptoms associated with peripheral eosinophilia. The diagnosis of EG is typically confirmed by endoscopic biopsies and/or eosinophilic ascites (EA). The symptoms are usually chronic and bothersome, with a relapsing course, but they can be successfully controlled with appropriate diagnosis and treatment. The aetiology of this disease remains unknown. It has been associated with food allergy, however, treatment with elimination diets gives poor results, while steroid therapy is effective in 90% of patients. A high index of suspicion is necessary as delays in diagnosis can result in unnecessary suffering.
Case presentation
A 22-year-old Bulgarian man presented with a 3-day history of abdominal pain, diarrhoea, nausea and vomiting. He also reported abdominal distention of a couple of weeks’ duration. He denied having choluria, acholia and haematemesis, as well as fever, night sweats, myalgia and weight loss. He had no history of atopy.
His medical history showed that he had been hospitalised in Bulgaria 7 months earlier, with the same symptoms, associated with ascites, however, the cause of the condition was never clarified despite considerable investigation.
On examination, the patient appeared dehydrated, but he was haemodynamically stable and afebrile. His abdomen was soft, but tender, with some guarding and rebound. No masses or organomegaly were palpated. On percussion, a shifting dullness was observed, which suggested ascites. Normal bowel sounds were present.
Initial investigations showed raised C reactive protein (1.13 mg/dL, reference range 0–0.5 mg/dL) and a white cell count of 13.7×109/L (reference range 4.0–10.0×109/L) at the expense of eosinophilia (3.4×109/L; reference range 0.02–0.5×109/L). An abdominal ultrasound scan showed diffuse thickening of the small intestinal loops, a large peritoneal effusion and a cystic formation of 3 cm in diameter on segment IV of the liver.
Investigations
The patient was hospitalised and laboratory testing showed maintained marked eosinophilia with normal blood count. Renal, hepatic and thyroid function as well as inflammatory markers were normal. Serology for hepatitis viruses and acquired immunodeficiency were negative. Research for parasites and their ova in stool, and coproculture were also negative. Tests for neoplastic markers were negative. An abdominal CT was carried out and the results revealed a cystic formation of 29 mm with a slight parietal enhancement in the IV segment, which was best characterised by liver MRI, which showed that it was a simple biliary cyst. Both imaging studies identified diffuse thickening of the small intestinal loops (figures 1 and 2) associated with multiple mesenteric lymph nodes, but with no criteria of adenopathy. An abdominal diagnostic paracentesis with ultrasound was performed and the patient's condition was found to be an EA with a serum-ascites albumin gradient (SAAG) of 0.8. Cytology identified reactive mesothelial cells and inflammatory cells with a predominance of polymorphonuclear cells with no neoplastic cells. Finally, the patient had an endoscopic study. Total colonoscopy showed no alterations, but the endoscopy identified erosive and erythaematous duodenal mucosa, so biopsies were performed. Histology from duodenal bulb and gastric antrum biopsies showed the presence in the lamina propria of moderate to marked lymphocytic infiltrates containing eosinophils, made evident by Congo Red, which in some areas had scores of 55–60/CGA: high magnification field high magnification field (figure 3).
Figure 1.
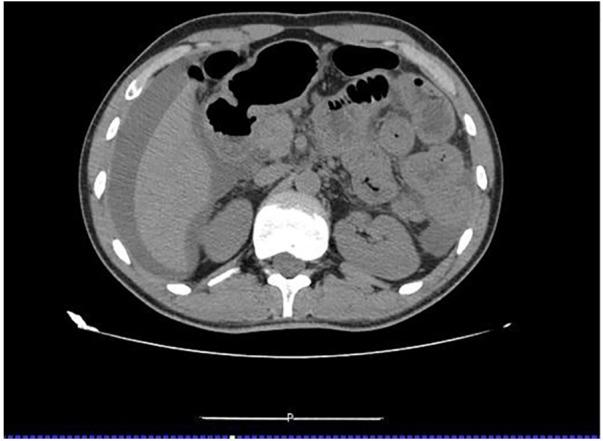
CT showing diffuse thickening of the small intestinal loops and considerable peritoneal effusion.
Figure 2.
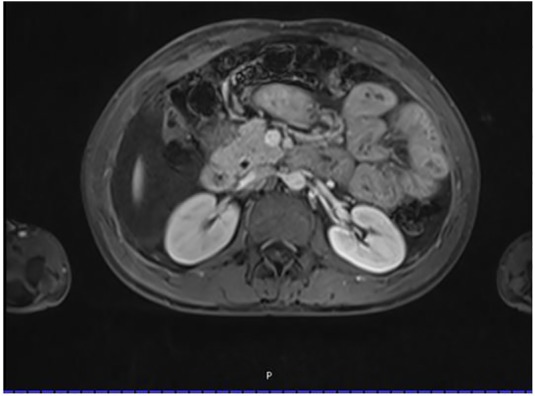
MRI showing diffuse thickening of the small intestinal loops.
Figure 3.
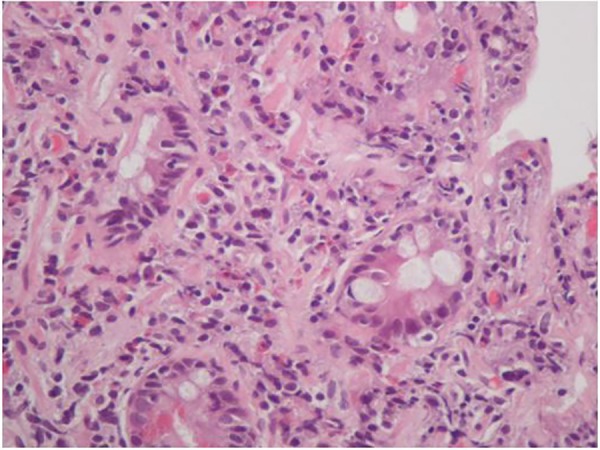
Duodenal biopsy with lamina propria containing inflammatory infiltrate with eosinophils (Congo Red). These pathological findings are consistent with erosive duodenal mucosa (H&E, ×400).
Differential diagnosis
In this particular case, it was extremely important to first exclude a parasite infection. Cystic lesions of the liver represent a heterogeneous group of disorders. The abdominal ultrasound scan showed a hepatic cyst of 3 cm, which in association with abdominal pain, diarrhoea, nausea, vomiting and eosinophilia, can be indicative of a parasite infection. The ultrasound also showed diffuse thickening of the small intestinal loops and a large peritoneal effusion, which could indicate a complication of a parasite infection. Nevertheless, due to the diversity in clinical presentation of EG differentiation from primary hypereosinophilic syndrome, ascites syndrome, Crohn's disease and malignancies had to be investigated.
Treatment
Systemic corticosteroids are the mainstay of therapy, and improve symptoms and endoscopic lesions dramatically in the vast majority of patients. So, prednisolone 40 mg/day was initiated.
Outcome and follow-up
Eight days after initiation of prednisolone, the patient had pain remission and normalisation of intestinal transit. He was discharged from hospital and was seen in medical consultation after a month. He remained asymptomatic with no ascites and blood tests showed clear improvement of eosinophilia. Therefore, corticosteroid weaning was started, without relapse to date.
Discussion
EG is an uncommon disorder, first reported by Kaijser in 1937 as a disease that selectively affects the gastrointestinal tract, and characterised as eosinophil-rich inflammation of the gastrointestinal tract in the absence of known causes for eosinophilia.1–4
Lesions can appear in the stomach and small intestine. A slight male preponderance has been reported. Although the disease can affect any age group, it mostly afflicts people between 30 and 50 years of age. Most affected individuals have a history of allergies, with some exhibiting eosinophilia and elevated serum IgE levels.5 In 1970, Klein et al classified the disease according to the anatomic location of eosinophilic infiltration: the mucosal, muscularis and subserosal layers, once they noticed that the EG symptoms often differ depending on the location of eosinophil infiltration.2 6 7 In fact, when the mucosa is in the primary inflammatory location, stomach ache, diarrhoea and/or weight loss are often noted. If the muscular layer is involved, nausea, vomiting and/or stomach ache may be the symptoms.1 EA is common when the serosa is involved, and is probably the most unusual and rare presentation of EG.4 7
In 80% of cases, EG is associated with increased eosinophils in the peripheral blood, and the biopsies of the area involved by the disease often reveal inflammatory cells composed primarily of eosinophils (>20–25/HPF) infiltrating mucous membranes. Several studies suggest a role of various cytokines, such as interleukin 3 and 4, granulocyte macrophage colony-stimulating factor and eotaxin, which are produced by eosinophils. Some studies also advocate that food allergens may play a role in local recruitment of eosinophils.1 4
Knowledge of the case history, physical examination and paracentesis are essential for the differential diagnosis of EG.
A SAAG value ≥1.1 g/dL suggests with 97% accuracy a diagnosis of ascites secondary to portal hypertension.8 However, our patient's paracentesis revealed a SAAG value of <1.1 g/dL, which indicates disease of the peritoneum, such as peritoneal carcinomatosis or peritoneal tuberculosis. The abdominal CT scan showed diffuse thickening of the small intestinal loops but without peritoneal implants, and the adenosine deaminase (ADA) level in the ascitic fluid was low, which excluded those diseases. The clinical history and physical examination were not suggestive of pancreatic ascites, intestinal obstruction or infarction, or biliary ascites. Renal function and serum albumin level were normal, so nephrotic syndrome or hypoalbuminaemia was not considered. Research for parasites and their ova in stool and coproculture were negative, rejecting intestinal parasites as the potential cause of the eosinophilia. Given that the paracentesis detected an EA, and a definitive diagnosis of EG requires histological evidence of eosinophilic infiltration, an endoscopic examination was performed. The biopsies of the duodenal bulb and gastric antrum noted moderate to marked lymphocytic infiltrates containing eosinophils. So, after careful investigation, the cause of abdominal pain, diarrhoea, nausea, vomiting and EA in our patient pointed to EG, which was supported further by the biopsy and a rapid clinical response to the steroid therapy.7 9 10
In summary, EA is a rare presentation of EG and should be considered when diagnosing a young patient with refractory gastrointestinal symptoms, eosinophilia and ascites in the absence of liver disease.
Learning points.
Eosinophilic gastroenteritis (EG) is an uncommon disorder and should be considered in a patient with refractory gastrointestinal symptoms, eosinophilia and ascites.
EG is a heterogeneous condition with several presentations, so a high index of suspicion is necessary.
A definitive diagnosis of EG requires histological evidence of eosinophilic infiltration.
It has been associated with food allergy, however, the treatment with elimination diets gives poor results, while steroid therapy is effective in 90% of patients.
Acknowledgments
The authors thank Dr Augusta Cipriano, anatomic pathologist in Centro Hospitalar e Universitário de Coimbra, EPE, who provided assistance, insight and expertise that greatly assisted the research.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Nakamura A, Iwaya Y, Iwaya M et al. Eosinophilic gastroenteritis complicated with Helicobacter pylori infection unresponsive to eradication therapy. Intern Med 2014;53:2061–5. 10.2169/internalmedicine.53.2111 [DOI] [PubMed] [Google Scholar]
- 2.Lyngbaek S, Adamsen S, Aru A et al. Recurrent acute pancreatitis due to eosinophilic gastroenteritis. Case report and literature review. JOP 2006;7: 211–17. [PubMed] [Google Scholar]
- 3.Leal R, Fayad L, Vieira D et al. Unusual presentations of eosinophilic gastroenteritis: two case reports. Turk J Gastroenterol 2014;25:323–9. 10.5152/tjg.2014.6735 [DOI] [PubMed] [Google Scholar]
- 4.Hepburn IS, Sridhar S, Schade RR. Eosinophilic ascites, an unusual presentation of eosinophilic gastroenteritis: a case report and review. World J Gastrointest Pathophysiol 2010;1:166–70. 10.4291/wjgp.v1.i5.166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baig MA, Qadir A, Rasheed J. A review of eosinophilic gastroenteritis. J Natl Med Assoc 2006;98:1616–19. [PMC free article] [PubMed] [Google Scholar]
- 6.Mori A, Enweluzo C, Grier D et al. Eosinophilic gastroenteritis: review of a rare and treatable disease of the gastrointestinal tract. Case Rep Gastroenterol 2013;7:293–8. 10.1159/000354147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maleki M, Kalantar Hormozi M, Bahtouee M et al. Eosinophilic ascites and duodenal obstruction in a patient with liver cirrhosis. Case Rep Gastrointest Med 2014;2014:928496 10.1155/2014/928496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhat KJ, Bhat S, Dutt K et al. Chronic diarrhea, eosinophilic ascites, acute pancreatitis and deep venous thrombosis: a case report. Caspian J Intern Med 2014;5:182–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Naik R, Joshipura VP, Patwari SI et al. A rare case of predominantly muscular infiltrative eosinophilic gastroenteritis with ascites: a case report and review of the literature. Trop Gastroenterol 2009;30:225–6. [PubMed] [Google Scholar]
- 10.Salgueiro P, Magalhães R, Lago P. Cramping pain and eosinophilic ascites: what is the diagnosis? Gastroenterology 2013;144:1353–6. 10.1053/j.gastro.2013.01.008 [DOI] [PubMed] [Google Scholar]


