Abstract
Subchondral insufficiency fractures are non-traumatic fractures that occur immediately below the cartilage of a joint. Although low bone density may be present concurrently, it is not the underlying cause of subchondral insufficiency fractures in the majority of patients. Patients with subchondral insufficiency fracture characteristically have unremarkable plain radiographs, while MRI examination may reveal extensive bone marrow oedema and subchondral bone collapse. This article presents a 51-year-old postmenopausal woman, a physician, who had subchondral insufficiency fractures of the knee associated with prolonged standing during clinical work. She was treated with partial weight bearing on crutches until 14 months after the injury, viscosupplementation at 4 months to treat osteoarthritis and teriparatide treatment to improve bone healing at 7 months. By 26 months after the injury, she tolerated independent walking with a fabric knee support but still experienced mild posterolateral knee pain and numbness on prolonged standing.
Background
Subchondral insufficiency fractures are slowly healing fractures of the bone situated immediately below the cartilage of a joint.1 The prognosis may range from full recovery to rapidly escalating joint destruction.2 A case series of 32 patients (mean age 70 years, 5 patients osteoporotic) with knee insufficiency fractures concluded that osteoporosis is not the underlying cause of subchondral insufficiency fractures in the majority of patients.3 Instead, these fractures are typically precipitated by athletic or overuse injuries or trauma (including surgical interventions) to the knee, and they may occur on the non-weight bearing surface of the femur.4 5 The outcome of subchondral insufficiency fractures depends on several factors, including the initial fracture size, patient body mass index (BMI; positive association with obesity), degree of osteopenia, as well as early diagnosis and initial treatment.6 We present this case to encourage clinicians to consider subchondral fracture in the differential diagnosis when a patient with normal radiographic findings reports severe and worsening knee pain in the absence of overt traumatic injury.
Case presentation
A 51-year-old woman, a physician, was referred to our orthopaedic and endocrinology clinics owing to a 2-month history of worsening right posterolateral knee pain with abnormal MRI findings. Her pain began spontaneously after an 18 h hospital shift during which she had few opportunities to sit for longer than a few minutes. She consulted her primary care physician when her pain persisted on non-weight bearing. Her medical history included congenital bilateral pes planus, osteoporosis diagnosed in her late 30s after a cumulative 4½ years of amenorrhoea and a right metatarsal stress fracture in her early 20s. The patient had declined treatment of her osteoporosis because of low immediate fracture risk during the early postmenopausal period. She reported a marked increase in prolonged standing after her outpatient and hospital clinical schedules had been augmented 5 months before; however, she was asymptomatic and routinely walked four miles five times per week for exercise before the injury. Her family history was notable for a father who had bilateral knee replacements in his 80s owing to osteoarthritis (OA), a sister aged 53 and paternal grandfather both with OA, and a paternal grandmother with osteoporosis and hip fracture. Physical examination revealed a BMI of 19.5 kg/m2, antalgic gait favouring the right leg, and point tenderness to palpation on the most lateral aspect of the lateral joint line of the right knee and over the lateral femoral condyle. Ligamentous examination was stable, although the patient was jumpy and had guarding on examination due to pain.
Investigations
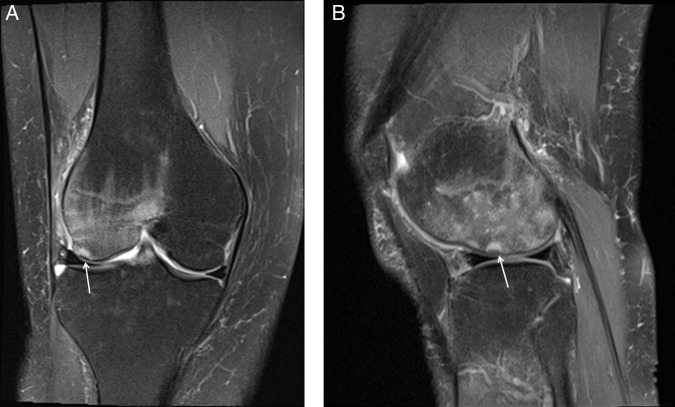
An MRI (figure 1A, B) of the right knee ordered by the patient's primary care physician 2 months postinjury revealed:
Two small subchondral insufficiency fractures involving the lateral femoral condyle with large amount of associated marrow oedema.
Complex, predominantly horizontal tear involving the posterior horn of the medial meniscus.
Possible small radial tear of the free edge of the posterior horn of the lateral meniscus.
Mild-to-moderate tricompartmental chondrosis.
Oedema and enlargement of the quadriceps fat pad, which can be seen in quadriceps impingement syndrome.
Figure 1.
Coronal (A) and sagittal (B) T2-weighted, fat-suppressed MRI of the right knee 58 days after injury. There is diffuse marrow oedema throughout the lateral femoral condyle and a minimal lateral femoral condylar depression (arrow) consistent with a subchondral insufficiency fracture.
Serial MRI over the subsequent 8 months showed progressive decrease of marrow oedema and subchondral fracture healing with some increase in the medial meniscal tear size.
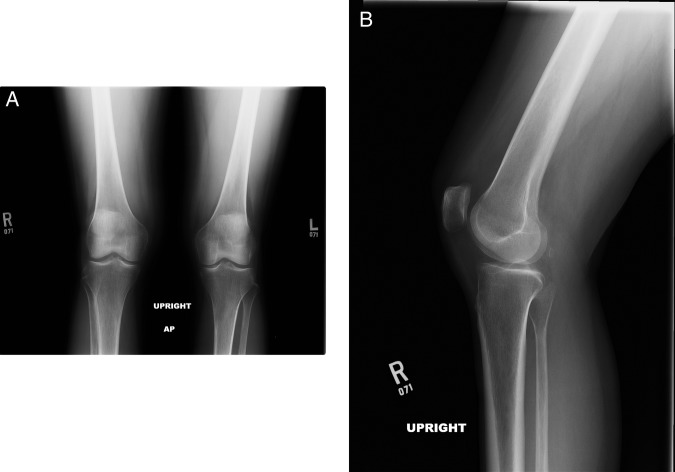
Serial radiographs (figure 2A, B) of the right knee showed an initial small right knee effusion with minimal osteophytosis along the lateral joint line, but no radiographic evidence of fracture and no narrowing of the medial or lateral compartment at baseline or on subsequent plain films.
Figure 2.
Anteroposterior radiograph of both knees (A) and a lateral radiograph of the right knee (B) show minimal osteophytosis, but are otherwise normal.
A dual-energy X-ray absorptiometry bone density test of the lumbar spine and right (ipsilateral to injury) hip 5 months after the injury showed T-scores −3.0 (spine), −2.0 (femoral neck) and −1.2 (total hip), respectively, which represented a stable spine density but a significant (−7.3%) decline in hip bone density compared with a previous study 8 years earlier.
Differential diagnosis
The characteristic radiographic lesion of subchondral insufficiency fractures is a band-like low signal intensity lesion surrounded by diffuse bone marrow oedema in T1-weighted MRI.1 The band-like lesion corresponds histopathologically to a fracture line with associated repair tissue.7
The differential diagnosis of subchondral insufficiency fractures includes spontaneous osteonecrosis. Osteonecrosis results from circulatory impairment of an area of bone, leading to the ischaemic death of the cellular constituents of the bone and marrow.8 Subchondral insufficiency fractures may be a potentially reversible precursor to osteonecrosis, but disease progression is unpredictable.1 2 The patient's MRI showed small subchondral bands of decreased signal intensity immediately deep to and parallel to the subchondral bone plate, which resolved without the features of necrosis. In contrast, the ischaemic lesions seen in osteonecrosis are often slightly deeper to the subchondral bone and may involve deformity of the subchondral bone plate in the weight bearing area of the involved condyle.9
Treatment
The initial orthopaedic recommendation included non-weight bearing, but due to work responsibilities, the patient was determined to use crutches to allow 50% weight bearing on the right lower extremity. A 12-week course of physical therapy comprising non-weight bearing exercises was prescribed. Four months after the injury, she received three intra-articular injections of hyaluronic acid at 2-week intervals to provide anti-inflammatory relief and because some pilot evidence in humans suggests hyaluronate may have a beneficial effect on the structural progression of OA.10 Seven months after the injury, the patient was begun on injections of teriparatide 20 µg daily for 4 months, instituted by her endocrinologist.
The patient self-administered magnesium salicylate and acetaminophen for pain, and she applied cold packs to the injury site intermittently every day. She reported rapid and effective pain relief with cold therapy than with medication. If she experienced pain at the injury site during the night or on waking in the morning, she stayed non-weight bearing as much as possible the following day.
Outcome and follow-up
The patient initially remained on crutches while working a reduced schedule of outpatient and inpatient work. Owing to failure to wean off crutches by 7 months, she elected to take medical leave for extended non-weight bearing to promote healing of the subchondral fractures. During the first 2½ weeks of medical leave, she reported continuous posterolateral knee pain, numbness, hamstring tightness and spasms, on weight bearing and non-weight bearing, as well as intolerance of keeping her knee dependent in a sitting position. Exacerbations of posterolateral knee pain occurred while she was lying on either side of her body, walking on hard floors, turning or placing her right heel on the ground.
After a final MRI 10 months after the injury, the patient was followed clinically. Fourteen months after the injury, she weaned off of daily crutch use with use of a fabric knee support, only using crutches for a few days at a time after minor reinjuries. She reported minimal pain on alternating weight bearing during walking, but worsening pain and numbness on continuous weight bearing during standing for more than a few seconds. By 18 months postinjury, she noted mild right rectus femoris muscle atrophy, which resolved as she increased walking distance. By 26 months after the injury, the patient was walking freely with intermittent use of the knee support. She has not resumed clinical work and is instead pursuing academic activities that can be accomplished while sitting.
Discussion
Subchondral insufficiency fractures of the knee are difficult to detect and may have an unpredictable course due to delayed diagnosis and lack of standard treatment approaches. When patients report joint pain in the absence of radiographic findings, MRI is usually not indicated, and observation and conservative measures often lead to spontaneous resolution. Clinical indications of a subchondral insufficiency fracture rather than a minor injury in this case were persistent localised pain on weight bearing and non-weight bearing after 2 months, and the history of increased periods of very prolonged standing. Healing may have occurred sooner if the patient had not resisted initial non-weight bearing activity recommendations; however, immediate initiation of partial weight bearing followed by a non-weight bearing period after 7 months still allowed progressive improvement. Since a recovery time of up to 3 years is documented for subchondral insufficiency fractures of the knee, the patient may have potential for further recovery.4
The patient's strong family history of OA was a predisposing factor to her subchondral insufficiency fractures. Her father's history of bilateral knee replacements suggested a genetic tendency towards defective joint cartilage, with OA expression exacerbated by obesity during three decades of adult life. The patient's sister, aged 53, had OA including a chronic knee effusion and cartilage damage after a fall injury, with subsequent arthroscopy and joint lavage. Concern over the sister's early and rapid OA progression was one reason the patient chose an extended non-weight bearing period in an effort to maximise her healing.
The patient's history of osteoporosis diagnosed in the premenopausal period seemed to be a plausible causal factor. However, review of the available literature suggested that an increase in duties requiring prolonged standing beginning 5 months before the injury was the key inciting factor, and that the subchondral fractures would probably have occurred in the absence of osteoporosis.3 4 The patient's significant decrease in hip bone density and quadriceps atrophy were probably due to decreased ipsilateral weight bearing in the 5 months since the injury, in addition to normal bone density loss during the menopausal transition. Her low normal body weight might have been a protective factor because subchondral fractures are more severe in patients with high BMI.6 Although not approved by the US Food and Drug Administration for treatment of subchondral fractures, teriparatide has been studied as a chondroregenerative agent in animal models.11 The endocrinologist initiated teriparatide based on data from a limited number of human trials supporting a potential role for teriparatide in promoting fracture healing in selected patients.12 13 Teriparatide also has demonstrated efficacy to increase bone density and to reduce fragility fractures in postmenopausal women with osteoporosis, so the patient was likely to receive benefit and was unlikely to experience harms from its use.14 Since it was initiated at the same time the patient assumed non-weight bearing, teriparatide’s role in the patient's recovery is uncertain but likely helpful.
Since there was an absence of loose bodies or other indications for arthroscopy, the orthopaedist did not encourage the patient to have a surgical procedure. Instrumentation may precipitate subchondral insufficiency fractures in some patients, and withholding of elective procedures during the acute period of injury is an important factor in healing.5 We could not find data regarding the value of physical therapy in this type of fracture. While appropriate physical therapy regimens are important to improve on aerobic capacity, quadriceps muscle strength, or lower extremity performance, weight bearing may exacerbate subchondral fracture pain and could potentially prolong healing.15 We recommend deferring physical therapy immediately after diagnosis of a subchondral insufficiency fracture, with subsequent consideration of short-term physical therapy comprised by non-weight bearing exercise to strengthen the quadriceps muscles, and prompt discontinuation if the patient reports exacerbation of pain.
Clinicians and patients find management of subchondral insufficiency fractures to be frustrating because the patient's reports of exquisite pain are discordant with normal radiographic findings, and because the recovery period is extremely prolonged. The key to maximising recovery is prompt diagnosis on MRI followed by immediate non-weight bearing and subsequent slow titration to full weight bearing directed by the patient's reports of pain. Diligent use of crutches, non-steroidal anti-inflammatory agents and cold therapy are the mainstays of conservative management. Efforts to ‘work through’ worsening pain are counteractive to recovery and must not be attempted.
Learning points.
Subchondral insufficiency fractures of the knee occur in association with prolonged weight bearing or repetitive impaction forces to the bone. The clinical hallmark is acute onset of severe and worsening knee pain in the absence of trauma.
Plain radiographs of the knee remain unremarkable throughout the period of subchondral fracture initiation; MRI is required for early diagnosis.
Recovery is slow; in one case series, 15 of 17 patients with subchondral insufficiency fractures became asymptomatic after conservative treatment, and none returned for clinical follow-up after an average of 3 years.
Prompt diagnosis and conservative management (immediate non-weight bearing followed by partial weight bearing as tolerated) are keys to successful treatment.
Teriparatide has been proposed as treatment for subchondral insufficiency fractures based on animal studies, but it remains an experimental treatment in humans.
Acknowledgments
The authors would like to acknowledge Julie Monaco, MD, and Donald Pathman, MD, for their diagnostic work and clinical recommendations for the patient.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Yamamoto T. Subchondral insufficiency fractures of the femoral head. Clin Orthop Surg 2012;4:173–80. 10.4055/cios.2012.4.3.173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yamamoto T, Bullough PG. Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. J Bone Joint Surg Am 2000;82:858–66. 10.1302/0301-620X.82B8.11194 [DOI] [PubMed] [Google Scholar]
- 3.Nelson FR, Craig J, Francois H et al. Subchondral insufficiency fractures and spontaneous osteonecrosis of the knee may not be related to osteoporosis. Arch Osteoporos 2014;9:194 10.1007/s11657-014-0194-z [DOI] [PubMed] [Google Scholar]
- 4.Depasquale R, Fotiadou A, Kumar DS et al. Subchondral impaction fractures of the non-weight-bearing portion of the lateral femoral condyle. Skeletal Radiol 2013;42:177–85. 10.1007/s00256-012-1492-4 [DOI] [PubMed] [Google Scholar]
- 5.MacDessi SJ, Brophy RH, Bullough PG et al. Subchondral fracture following arthroscopic knee surgery. A series of eight cases. J Bone Joint Surg Am 2008;90:1007–12. 10.2106/JBJS.G.00445 [DOI] [PubMed] [Google Scholar]
- 6.Jose J, Pasquotti G, Smith MK et al. Subchondral insufficiency fractures of the knee: review of imaging findings. Acta Radiol 2014;56:714–19. 10.1177/0284185114535132 [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto T, Schneider R, Bullough PG. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skeletal Radiol 2001;30:247–54. 10.1007/s002560100348 [DOI] [PubMed] [Google Scholar]
- 8.Narvaez J, Narvaez JA, Rodriguez-Moreno J et al. Osteonecrosis of the knee: differences among idiopathic and secondary types. Rheumatology (Oxford) 2000;39:982–9. 10.1093/rheumatology/39.9.982 [DOI] [PubMed] [Google Scholar]
- 9.Roemer FW, Frobell R, Hunter DJ et al. MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthritis Cartilage 2009;17:1115–31. 10.1016/j.joca.2009.03.012 [DOI] [PubMed] [Google Scholar]
- 10.Hunter DJ. Viscosupplementation for osteoarthritis of the knee. N Engl J Med 2015;372:1040–7. 10.1056/NEJMct1215534 [DOI] [PubMed] [Google Scholar]
- 11.Sampson ER, Hilton MJ, Tian Y et al. Teriparatide as a chondroregenerative therapy for injury-induced osteoarthritis. Sci Transl Med 2011;3:101ra93 10.1126/scitranslmed.3002214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aspenberg P, Genant HK, Johansson T et al. Teriparatide for acceleration of fracture repair in humans: a prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J Bone Miner Res 2010;25:404–14. 10.1359/jbmr.090731 [DOI] [PubMed] [Google Scholar]
- 13.Campbell EJ, Campbell GM, Hanley DA. The effect of parathyroid hormone and teriparatide on fracture healing. Expert Opin Biol Ther 2015;15:119–29. 10.1517/14712598.2015.977249 [DOI] [PubMed] [Google Scholar]
- 14.Neer RM, Arnaud CD, Zanchetta JR et al. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 2001;344:1434–41. 10.1056/NEJM200105103441904 [DOI] [PubMed] [Google Scholar]
- 15.Juhl C, Christensen R, Roos EM et al. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol 2014;66:622–36. 10.1002/art.38290 [DOI] [PubMed] [Google Scholar]