Abstract
A 22-year-old man presented with a painful ‘clunking’ sensation in the right mid-clavicle, and pain and dysaesthesia along the medial aspect of his right arm and hand. Three months earlier, he had been involved in a vehicle accident and sustained a right clavicle fracture. He had a large step off of the right clavicle with a medialisation of the right shoulder. At 90° abduction in external rotation of both shoulders he developed pain, paraesthesia and disappearance of the right radial artery pulsation. CT of the right shoulder in the neutral position demonstrated the clavicle-to-first rib distance of 5.5 mm, MRI showed the clavicular bone callus had a mass effect with effacement of anterior fat adjacent to the brachial plexus cords. He was diagnosed with thoracic outlet syndrome and underwent a corrective right clavicle osteotomy with the use of an AcuMed superior clavicle plate.
Background
Thoracic outlet syndrome (TOS) is a rare complication of conservative treatment of a clavicle fracture. Its surgical management is challenging and includes a costoclavicular space decompression with an excision of excessive bone callus,1 resection of the first rib, an anterior and middle scalenectomy,2 partial or complete clavicle resection3 4 and claviculoplasty.5 We report a case of TOS secondary to mid-clavicle malunion treated with a corrective clavicle osteotomy and plate fixation, which allowed decompression of the costoclavicular space, restoring of the clavicle length and improvement in the patient's right shoulder function.
Case presentation
A 22-year-old man, a right hand dominant surveyor presented with a 3-month history of a painful ‘clunking’ sensation in the right clavicle, and a gradual onset of pain and dysaesthesia along the medial aspect of his right arm and hand and, on right shoulder abduction, of the little finger and the lateral aspect of the fourth finger. In October 2013, he was driving a car at high speed and inadvertently ploughed into a log and sustained multiple nasal bone fractures, a displaced Le Fort I maxillary fracture, inferior endplate C2 fracture, compound medial epicondyle of the left humerus fracture and a right diaphyseal clavicle (Edinburgh type 2B1) fracture with a 28 mm shortening of its length (figure 1). At the time, he underwent, in another hospital, a wound debridement and open reduction and internal fixation (ORIF) of his left elbow fracture, and an ORIF of the displaced Le Fort I maxillary fracture. The patient's cervical spine fracture was treated with an Aspen collar for 6 weeks. Treatment options for right clavicle fracture were discussed with the patient, who elected conservative management with an arm sling.
Figure 1.
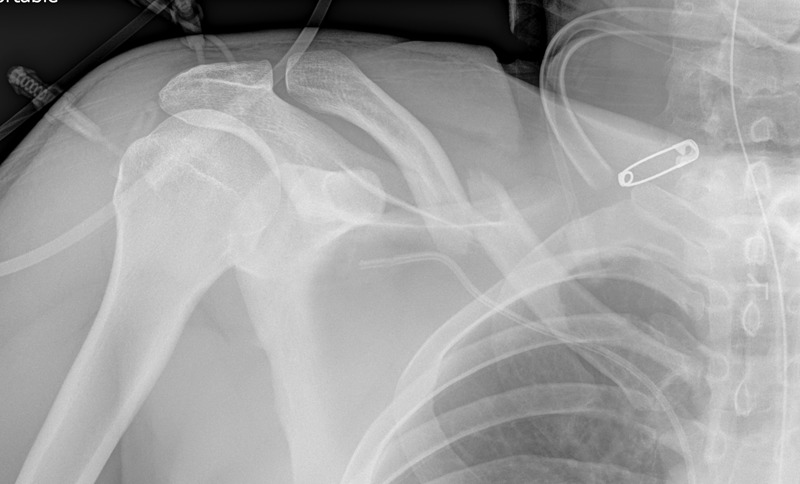
A right diaphyseal clavicle (Edinburgh type 2B1) fracture with a 28 mm shortening of its length.
On physical examination he had a large step off of the right clavicle with a medialisation of the right shoulder. At 90° abduction in external rotation (ABER) of both shoulders, he developed severe pain in the right arm and disappearance of the right radial artery pulsation. In addition, the patient had winging of his right scapula.
Investigations
A right clavicle X-ray showed that the distal clavicle fragment was 150% inferiorly displaced and overrode the proximal fragment by 30 mm, forming a malunion (figure 2). CT image of the right shoulder in the neutral position demonstrated a clavicle-to-first rib distance of 5.5 mm (normal range: 7.2–18 mm;6 figure 3). The patient was not able to tolerate the ABER position due to severe pain, therefore, imaging studies were performed in the neutral position.
Figure 2.

The right clavicle X-ray shows that the distal clavicle fragment was 150% inferiorly displaced and overrode the proximal fragment by 30 mm, forming a malunion.
Figure 3.
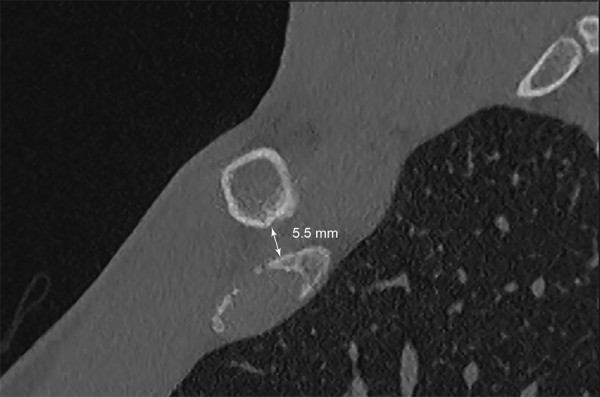
CT image of the right shoulder in the neutral position demonstrating a clavicle-to-first rib distance of 5.5 mm.
MRI of the right brachial plexus in the neutral position showed the bone callus had a mild mass effect with effacement of anterior fat adjacent to the brachial plexus cords (an arrow in figure 4). There was a subtle increased short τ inversion recovery signal within the serratus anterior muscle overlying the cranial margin of the right second rib posteriorly, which may be related to injury of the long thoracic nerve.
Figure 4.
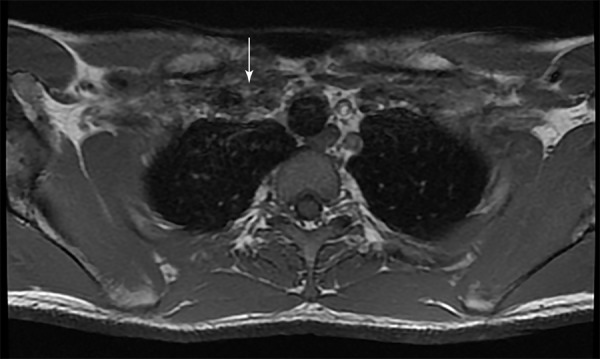
MRI of the right brachial plexus in the neutral position shows the bone callus had a mild mass effect with effacement of anterior fat adjacent to the brachial plexus cords (arrow).
MRI of the cervical spine demonstrated a united C2 anteroinferior endplate fracture, but no focal disc protrusion or neural compromise.
Treatment
The patient underwent a corrective right mid-clavicle osteotomy and internal fixation with the use of an AcuMed superior clavicle plate via a supraclavicular approach. An intraoperative assessment in the ABER position revealed good right radial artery pulsation.
Outcome and follow-up
The patient was reviewed in 3 months. He was asymptomatic. His right arm was neurovascularly intact. Winging of the right scapula had improved. The right clavicle fracture had united (figure 5) and the patient returned to full manual work.
Figure 5.
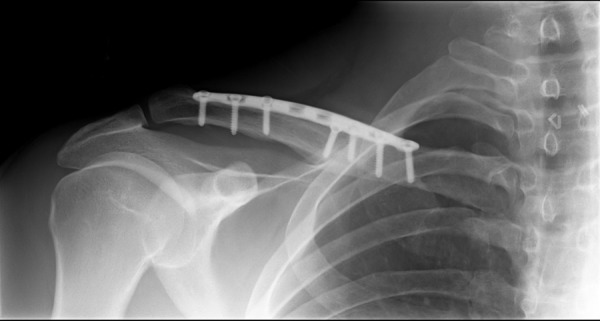
The right clavicle fracture is seen united.
Discussion
Clavicle fractures are common injuries. In the USA, an average annual incidence of clavicle fracture is 58 per 100 000 persons.7 Males 20–30 years of age have an incidence of clavicle fractures between 50 per 100 000 persons to 40 per 100 000 populationper year.8 Diaphyseal clavicle fractures account for 80% of all clavicle fractures; of these 50% are displaced.9 Initial shortening of the clavicle ≥20 mm is considered a risk factor for non-union.10 Patients with a middle third clavicle fracture can be treated conservatively and/or surgically. Conservative methods include an arm sling, strapping, figure-of-eight bandage and splints. Two of the most common surgical methods of shaft clavicle fracture treatment are plate fixation and intramedullary fixation. The most recent systematic review comparing surgical versus conservative interventions for acute shaft clavicle fractures showed that surgical interventions do not result in an improvement in shoulder function.11 Therefore, it was concluded that treatment options must be tailored to individual patients and take into account their health-related preferences.11 A cost minimisation analysis conducted by Walton et al12 demonstrated that initial conservative treatment of displaced diaphyseal clavicle fractures followed by delayed surgery as needed is less costly for the healthcare provider than operative management. On the other hand, a cost analysis of operative and conservative management of displaced mid-clavicle fractures performed from a societal perspective that considered all costs and benefits regardless who paid for or received them demonstrated a cost saving of $5000 per operative patient.13
Our patient with a right displaced mid-clavicle fracture elected to be treated conservatively. As a result, he developed TOS secondary to right clavicle malunion. Neither an excision of the bone callus nor the distal fragment of the clavicle would be effective in decompression of the costoclavicular space. A partial or complete clavicle resection would make the patient's shoulder girdle unstable and result in a permanent physical disability. An anterior and middle scalenectomy would be ineffective because it does not increase the costoclavicular space. A resection of the first rib would not restore the clavicle length to improve the patient's right shoulder function. A corrective clavicle osteotomy with plate fixation was performed with an intent to decompress the costoclavicular space, to achieve good stabilisation of the clavicle fragments, restore the clavicle length and improve the patient's right shoulder function.
Learning points.
Patients with a displaced mid-clavicular fracture who are managed conservatively should be regularly followed up in an outpatient clinic with a thorough clinical examination and shoulder X-ray.
If patients develop symptoms and signs of thoracic outlet syndrome they should undergo diagnostic imaging studies and an operative treatment.
A corrective clavicle osteotomy with plate fixation allows decompression of the costoclavicular space, good stabilisation of clavicle fragments, restoration of clavicle length and an improvement of shoulder functions.
Footnotes
Contributors: AMB and CF equally contributed in writing this paper.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res 1968;58:29–42. [PubMed] [Google Scholar]
- 2.Yoo MJ, Seo JB, Kim JP et al. Surgical treatment of thoracic outlet syndrome secondary to clavicular malunion. Clin Orthop Surg 2009;1:54–7. 10.4055/cios.2009.1.1.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mulder DS, Greenwood FA, Brooks CE. Posttraumatic thoracic outlet syndrome. J Trauma 1973;13:706–15. 10.1097/00005373-197308000-00006 [DOI] [PubMed] [Google Scholar]
- 4.Enker SH, Murthy KK. Brachial plexus compression by excessive callus formation secondary to a fractured clavicle. A case report. Mt Sinai J Med 1970;37:678–82. [PubMed] [Google Scholar]
- 5.Fujita K, Matsuda K, Sakai Y et al. Late thoracic outlet syndrome secondary to malunion of the fractured clavicle: case report and review of the literature. J Trauma 2001;50:332–5. 10.1097/00005373-200102000-00022 [DOI] [PubMed] [Google Scholar]
- 6.Matsumura JS, Rilling WS, Pearce WH et al. Helical computed tomography of the normal thoracic outlet. J Vasc Surg 1997;26:776–83. 10.1016/S0741-5214(97)70090-9 [DOI] [PubMed] [Google Scholar]
- 7.Karl JW, Olson PR, Rosenwasser MP. The Epidemiology of Upper Extremity Fractures in the United States, 2009. J Orthop Trauma 2015. [Epub ahead of print]. PMID:25714441 [DOI] [PubMed] [Google Scholar]
- 8.Khan LA, Bradnock TJ, Scott C et al. Fractures of the clavicle. J Bone Joint Surg Am 2009;91:447–60. 10.2106/JBJS.H.00034 [DOI] [PubMed] [Google Scholar]
- 9.Postacchini F, Gumina S, De Santis P et al. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002;11:452–6. 10.1067/mse.2002.126613 [DOI] [PubMed] [Google Scholar]
- 10.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997;79:537–9. 10.1302/0301-620X.79B4.7529 [DOI] [PubMed] [Google Scholar]
- 11.Lenza M, Buchbinder R, Johnston RV et al. Surgical versus conservative interventions for treating fractures of the middle third of the clavicle. Cochrane Database Syst Rev 2013;6:CD009363 10.1002/14651858.CD009363.pub2 [DOI] [PubMed] [Google Scholar]
- 12.Walton B, Meijer K, Melancon K et al. A cost analysis of internal fixation versus nonoperative treatment in adult midshaft clavicle fractures using multiple randomized controlled trials. J Orthop Trauma 2015;29:173–80. 10.1097/BOT.0000000000000225 [DOI] [PubMed] [Google Scholar]
- 13.Althausen PL, Shannon S, Lu M et al. Clinical and financial comparison of operative and nonoperative treatment of displaced clavicle fractures. J Shoulder Elbow Surg 2013;22:608–11. 10.1016/j.jse.2012.06.006 [DOI] [PubMed] [Google Scholar]


