Abstract
Background
Tuberculosis (TB) requires at least six months of treatment. If treatment is incomplete, patients may not be cured and drug resistance may develop. Directly Observed Therapy (DOT) is a specific strategy, endorsed by the World Health Organization, to improve adherence by requiring health workers, community volunteers or family members to observe and record patients taking each dose.
Objectives
To evaluate DOT compared to self‐administered therapy in people on treatment for active TB or on prophylaxis to prevent active disease. We also compared the effects of different forms of DOT.
Search methods
We searched the following databases up to 13 January 2015: the Cochrane Infectious Diseases Group Specialized Register; the Cochrane Central Register of Controlled Trials (CENTRAL), published in the Cochrane Library; MEDLINE; EMBASE; LILACS and mRCT. We also checked article reference lists and contacted relevant researchers and organizations.
Selection criteria
Randomized controlled trials (RCTs) and quasi‐RCTs comparing DOT with routine self‐administration of treatment or prophylaxis at home.
Data collection and analysis
Two review authors independently assessed risk of bias of each included trial and extracted data. We compared interventions using risk ratios (RR) with 95% confidence intervals (CI). We used a random‐effects model if meta‐analysis was appropriate but heterogeneity present (I2 statistic > 50%). We assessed the quality of the evidence using the GRADE approach.
Main results
Eleven trials including 5662 participants met the inclusion criteria. DOT was performed by a range of people (nurses, community health workers, family members or former TB patients) in a variety of settings (clinic, the patient's home or the home of a community volunteer).
DOT versus self‐administered
Six trials from South Africa, Thailand, Taiwan, Pakistan and Australia compared DOT with self‐administered therapy for treatment. Trials included DOT at home by family members, community health workers (who were usually supervised); DOT at home by health staff; and DOT at health facilities. TB cure was low with self‐administration across all studies (range 41% to 67%), and direct observation did not substantially improve this (RR 1.08, 95% CI 0.91 to 1.27; five trials, 1645 participants, moderate quality evidence). In a subgroup analysis stratified by the frequency of contact between health services in the self‐treatment arm, daily DOT may improve TB cure when compared to self‐administered treatment where patients in the self‐administered group only visited the clinic every month (RR 1.15, 95% CI 1.06 to 1.25; two trials, 900 participants); but with contact in the control becoming more frequent, this small effect was not apparent (every two weeks: RR 0.96, 95% CI 0.83 to 1.12; one trial, 497 participants; every week: RR 0.90, 95% CI 0.68 to 1.21; two trials, 248 participants).
Treatment completion showed a similar pattern, ranging from 59% to 78% in the self‐treatment groups, and direct observation did not improve this (RR 1.07, 95% CI 0.96 to 1.19; six trials, 1839 participants, moderate quality evidence).
DOT at home versus DOT at health facility
In four trials that compared DOT at home by family members, or community health workers, with DOT by health workers at a health facility there was little or no difference in cure or treatment completion (cure: RR 1.02, 95% CI 0.88 to 1.18, four trials, 1556 participants, moderate quality evidence; treatment completion: RR 1.04, 95% CI 0.91 to 1.17, three trials, 1029 participants, moderate quality evidence).
DOT by family member versus DOT by community health worker
Two trials compared DOT at home by family members with DOT at home by community health workers. There was also little or no difference in cure or treatment completion (cure: RR 1.02, 95% CI 0.86 to 1.21; two trials, 1493 participants, moderate quality evidence; completion: RR 1.05, 95% CI 0.90 to 1.22; two trials, 1493 participants, low quality evidence).
Specific patient categories
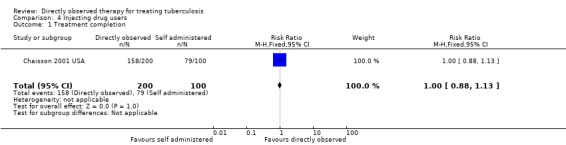
A trial of 300 intravenous drug users in the USA evaluated direct observation with no observation in TB prophylaxis to prevent active disease and showed little difference in treatment completion (RR 1.00, 95% CI 0.88 to 1.13; one trial, 300 participants, low quality evidence).
Authors' conclusions
From the existing trials, DOT did not provide a solution to poor adherence in TB treatment. Given the large resource and cost implications of DOT, policy makers might want to reconsider strategies that depend on direct observation. Other options might take into account financial and logistical barriers to care; approaches that motivate patients and staff; and defaulter follow‐up.
15 April 2019
Update pending
Studies awaiting assessment
The CIDG is currently examining a search conducted up to 5 Jul, 2018 for potentially relevant studies. These studies have not yet been incorporated into this Cochrane Review.
Plain language summary
Directly observing people with TB take their drugs to help them complete their treatment
This Cochrane Review summarises trials evaluating the effects of directly observed therapy (DOT) for treating people with tuberculosis (TB) or people on prophylaxis to prevent active disease compared to self‐administered treatment. After searching for relevant trials up to 13 January 2015, we included 11 randomized controlled trials, enrolling 5662 people with TB, and conducted between 1995 and 2008.
What is DOT and how might it improve treatment outcomes for people with TB
DOT is one strategy to ensure that patients with TB take all their medication. An 'observer' acceptable to the patient and the health system observes the patient taking every dose of their medication, and records this for the health system to monitor.
The World Health Organization currently recommends that people with TB are treated for at least six months to achieve cure. These long durations of treatment can be difficult for patients to complete, especially once they are well and need to return to work. Failure to complete treatment can lead to relapse and even death in individuals, and also has important public health consequences, such as increased TB transmission and the development of drug resistance.
What the research says
Overall, cure and treatment completion in both self‐treatment and DOT groups was low, and DOT did not substantially improve this. Small effects were seen in a subgroup of studies where the self‐treatment group were monitored less frequently than the DOT group.
There is probably no difference in TB cure or treatment completion when the direct observation was conducted at home or at the clinic (moderate quality evidence). There is probably little or no difference in TB cure direct observation is conducted by a community health worker or family member (moderate quality evidence) and there may be little or no difference in treatment completion either (low quality evidence).
Direct observation may have little or no effect on treatment completion in injection drug users (low quality evidence).
The authors conclude that DOT on its own may not offer the solution to poor adherence in people taking TB medication.
Summary of findings
Summary of findings for the main comparison. Directly observed therapy (DOT) versus self‐administered TB treatment.
| Directly observed therapy (DOT) versus self‐administered TB treatment | |||||
| Patient or population: Patients on TB treatment Settings: Low‐, middle‐ or high‐income countries Intervention: DOT Comparison: Self‐administered therapy | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (trials) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Self‐administered therapy | DOT | ||||
| Cure Follow‐up: up to 6 months | 617 per 1000 | 666 per 1000 (561 to 784) | RR 1.08 (0.91 to 1.27) | 1645 (5 trials) | ⊕⊕⊕⊝ moderate1,2,3,4 |
|
Treatment completion Follow‐up: 2 to 8 months5 |
709 per 1000 | 751 per 1000 (680 to 829) | RR 1.07 (0.96 to 1.19) | 1839 (6 trials) | ⊕⊕⊕⊝ moderate1,2,3,4 |
| The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; DOT: directly observed therapy; TB: tuberculosis. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1No serious risk of bias: three trials adequately described allocation concealment. Exclusion of trials at unclear or high risk of bias did not substantially change the result. 2Downgraded by 1 for inconsistency: trials include qualitative differences in effect size and direction. The benefit reached standard levels of statistical significance in the two trials where those receiving self‐administered therapy had less frequent contact with health services compared to the directly observed group, so any effect probably due to confounding. 3No serious indirectness: The trials were conducted in low‐, middle‐ and high‐income countries between 1995 and 2008. 4No serious imprecision: The analysis is adequately powered to detect clinically important differences between treatment arms. 5Some trials checked for completion of intensive phase treatment and others the completion of the whole therapy, hence the 2 to 8 months.
Summary of findings 2. Home DOT versus clinic DOT.
| Home DOT versus clinic DOT | |||||
| Patient or population: Patients with TB treatment Settings: Low‐, middle‐ or high‐income countries Intervention: Home observation Comparison: Clinic observation | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (trials) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Clinic observation | Home observation | ||||
| Cure Follow‐up: up to 6 months | 492 per 1000 | 502 per 1000 (433 to 580) | RR 1.02 (0.88 to 1.18) | 1556 (4 trials) | ⊕⊕⊕⊝ moderate1,2,3 |
| Treatment completion4 Follow‐up: 2 to 6 months | 751 per 1000 | 781 per 1000 (684 to 879) | RR 1.04 (0.91 to 1.17) | 1029 (3 trials) | ⊕⊕⊕⊝ moderate1,2,3 |
| The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; DOT: directly observed therapy; TB: tuberculosis. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1Downgraded by 1 for risk of bias: selection bias is probable in one trial, Wandwalo 2004 TZA, as there was no blinding and no allocation concealment. In Lwilla 2003 TZA, sequence generation and allocation concealment were unclear and there was no blinding. This could bias the measurement of treatment completion. 2No serious indirectness: The trials were conducted in low‐, middle‐ and high‐income countries between 1995 and 2008. 3No serious imprecision: The analysis is adequately powered to detect clinically important differences between treatment arms. 4Some trials checked for completion of intensive phase treatment and others the completion of the whole therapy, hence the 2 to 6 months.
Summary of findings 3. Summary of findings table 3.
| Community DOT versus family DOT | |||||
| Patient or population: Patients on TB treatment Settings: Low‐, middle‐ or high‐income countries Intervention: Community DOT Comparison: Family DOT | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (trials) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Family DOT | Community DOT | ||||
|
Cure Follow‐up: up to 6 months |
766 per 1000 | 781 per 1000 (659 to 927) | RR 1.02 (0.86 to 1.21) | 1493 (2 trials) |
⊕⊕⊕⊝ moderate1 |
|
Treatment completion Follow‐up: 2 to 6 months |
827 per 1000 | 869 per 1000 (744 to 1000) | RR 1.05 (0.90 to 1.22) | 1493 (2 trials) |
⊕⊕⊝⊝ low1,2 |
| *The basis for the assumed risk (eg the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; DOT: directly observed therapy; TB: tuberculosis. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1Downgraded by 1 for risk of bias. Both trials had unclear random sequence generation and recruitment bias could not be ruled out for Newell 2006 NPL. 2Downgraded by 1 for risk of bias for the outcome of treatment completion as there was no allocation concealment and selective reporting could not be ruled out in Wright 2004 SWZ.
Summary of findings 4. DOT versus self‐administered therapy for intravenous drug users.
| DOT versus self‐administered therapy for intravenous drug users | |||||
| Patient or population: Patients on TB treatment Settings: Low‐, middle‐ or high‐income countries Intervention: DOT Comparison: Self‐administered treatment | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (trials) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Self‐administered therapy | DOT | ||||
|
Treatment completion Follow‐up for 6 months |
79 per 100 | 79 per 1000 (70 to 89) | RR 1.00 (0.88 to 1.13) | 300 (1 trial) | ⊕⊕⊝⊝ low1,2,3 |
| *The basis for the assumed risk (eg the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; DOT: directly observed therapy; TB: tuberculosis. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1Downgraded by 1 for risk of bias. There was no blinding of outcome assessment and allocation concealment was unclear and treatment completion can be a bit subjective hence the results might be biased. The level of completeness to follow‐up was 88%. 2Downgraded by 1 for indirectness. The self‐administered group had a 10 dollar stipend which is may have enhanced adherence in this group. 3There may have been some imprecision. The study was had a small sample size and may have been underpowered to detect clinically important differences.
Background
Description of the condition
Tuberculosis (TB) remains a leading cause of death in low‐ and middle‐income countries despite the availability of effective treatments. In 2012, the World Health Organization (WHO) estimated that there were 8.6 million people infected with TB, of whom 1.3 million died (WHO 2013). Most people infected with Mycobacterium tuberculosis develop 'latent TB', where the bacteria are contained by the person's immune system and they do not develop symptoms. The risk of progression to active TB and development of symptoms is about 10% over the course of a lifetime (Frieden 2003), but co‐infection with human immune deficiency virus (HIV) increases this risk to about 10% per year (Sepkowitz 1995).
The WHO currently recommends at least six months of treatment for active disease, and 12 months for latent TB (Smieja 2010; WHO 2010). These long durations of treatment can be difficult for patients to adhere to, especially once they are well and need to return to work. Poor adherence can lead to relapse and even death in individuals, and also has important public health consequences, such as increased transmission and the development of drug resistance (Hirpa 2013; Moonan 2011).
Munro 2007 synthesized evidence from qualitative studies among patients and health workers and identified eight factors that influence adherence:
Organization of treatment and care for TB patients.
Interpretation of illness and wellness by the patient.
Financial cost.
Patient knowledge, attitudes and beliefs about treatment.
Law and immigration status.
Gender and substance abuse.
Drug side effects.
Influence of the family, community and peers.
We adapted an existing conceptual framework by van den Boogaard 2012 to develop a model for understanding approaches to improving adherence (Figure 1).There are health system level barriers (staff, inconvenient location, expensive and a poorly organized healthcare system) and personal level barriers (stigmatisation, poverty, competing demands and health beliefs) to adherence and the patient has to work through these barriers in order to be adherent. Healthcare workers have devised several strategies targeted at some of the key barriers to improve adherence, some of which are addressed by Cochrane Reviews:
1.
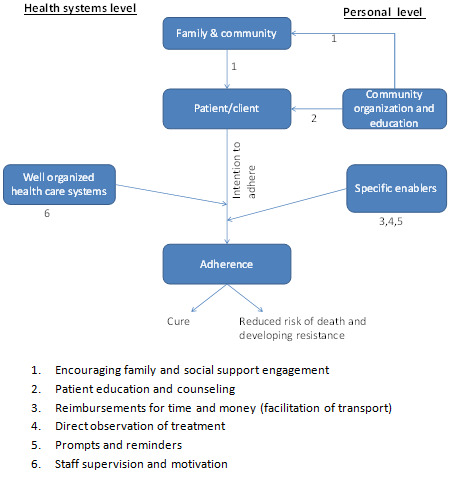
Factors influencing adherence and possible intervention points.
Reminder systems and late patient tracers in the diagnosis and management of TB (Liu 2008).
Patient education and counselling for promoting adherence to treatment for TB (M'Imunya 2012).
Material incentives and enablers in the management of TB (Lutge 2012).
Contracts: written or verbal agreements to return for an appointment or course of treatment (Bosch‐Capblanch 2007).
Description of the intervention
'Directly observed therapy' (DOT) is one component of a wider WHO strategy called 'Directly Observed Therapy Short course' (DOTS). This strategy incorporates wide ranging health system improvements, political commitment to improving TB programmes, improved TB laboratory services, free TB drugs for all TB patients, and accurate documentation and monitoring of TB diagnosis and treatment outcomes (WHO 2002). The DOT component is an attempt to improve adherence by active monitoring and recording of the consumption of each and every drug dose by an 'observer' acceptable to the patient and the health system (Hopewell 2006). This approach was first adopted in studies in Madras, India and Hong Kong as early as the 1960s (Bayer 1995), and is now considered a core component of TB programmes by the WHO to ensure cure and prevent the emergence of drug resistance (Chien 2013; Hirpa 2013). Proponents of DOT argue that the close monitoring has a social effect and acts as a peer pressure which leads to behavior change towards improved adherence (Macq 2003) and it has strong proponents (Chaulk 1998; Frieden 2007). However, to opponents it has been seen as a coercive model which leaves the patient as a passive recipient of therapy thereby eroding the gains made in involving patients in management of their own health (Zwarenstein 1998 ZAF).
The initial Cochrane Review (Volmink 1997) and subsequent updates (Volmink 2000a; Volmink 2001; Volmink 2003; Volmink 2006; Volmink 2007) challenged the dogma that DOT improved cure and thus helped prevent drug resistance developing. The debate has continued, with some even advocating for a shift of resources away from DOT programmes (Barbara 2013; Gross 2009; Moonan 2011; Pasipanodya 2013). There are also debates as to the best delivery of DOT, for example, should it be through healthcare workers or family members (Anuwatnonthakate 2008; Dick 2005).
Why it is important to do this review
Full implementation of DOT requires considerable resources. For example, in Pakistan it has been shown that direct observation at a health facility costs two times more than self‐supervision (USD310 versus USD164). Therefore, it is important to evaluate the effects in order to inform decisions about whether the benefits are worth investing in (Khan 2003). This Cochrane Review is an update of Volmink 2007.
Objectives
To evaluate DOT compared to self‐administered therapy in people on treatment for active TB or on prophylaxis to prevent active disease. We also compare the effects of different forms of DOT.
Methods
Criteria for considering studies for this review
Types of studies
Individually randomized controlled trials (RCTs) or cluster‐RCTs. We also included quasi‐RCTs.
Types of participants
People on treatment for active TB or receiving prophylaxis to prevent the development of active TB disease.
Types of interventions
Intervention
DOT where a health worker, community volunteer or family member, routinely observes participants taking their antituberculous drugs.
Control
Self‐administered therapy or an alternative form of DOT.
Types of outcome measures
Primary
Cure (having a negative sputum smear test in the last month of treatment having been smear‐positive initially).
Treatment completion.
Development of clinical TB (in trials of drug prophylaxis).
Secondary
Proportion of outpatient appointments attended.
Search methods for identification of studies
We attempted to identify all relevant trials regardless of language or publication status (published, unpublished, in press and in progress).
Databases
We searched the following databases using the search terms and strategy described in Appendix 1: Cochrane Infectious Diseases Group (CIDG) Specialized Register (13 January 2015); the Cochrane Central Register of Controlled Trials (CENTRAL), published in the Cochrane Library; MEDLINE (1966 to 13 January 2015); EMBASE (1974 to 13 January 2015); and LILACS (1982 to 13 January 2015). We also searched the metaRegister of Controlled Trials (mRCT) using 'tuberculosis AND DOT*' (13 January 2015).
Researchers and organizations
For unpublished and ongoing trials, we contacted individual researchers working in the field and the following organizations: WHO, the International Union Against Tuberculosis and Lung Disease, and the Centers for Disease Control and Prevention (CDC).
Reference lists
We also checked the reference lists of all studies identified by the above methods.
Data collection and analysis
Selection of studies
We independently applied the inclusion criteria to all identified trials. We used the titles and abstracts of the identified citations to exclude trials that clearly did not meet the inclusion criteria. If either review author judged that the trial might be eligible for inclusion, we obtained the full text article. We independently screened the full text articles of selected trials to confirm eligibility and resolved any disagreements by discussion.
Data extraction and management
We independently extracted the data and checked whether trial authors had conducted an intention‐to‐treat analysis. We contacted trial authors to obtain missing information and to clarify issues. We resolved discrepancies through discussion. For the outcomes, we extracted the number of participants experiencing the event.
Assessment of risk of bias in included studies
We independently evaluated the methodological quality of each trial, classifying the generation of allocation sequence and concealment of allocation as either adequate, inadequate or unclear, according to Jüni 2001. We classified blinding as adequate if the trial authors took steps to ensure the people recording the main outcome of the trial were blinded to the assigned interventions, and inadequate if this was not the case or if there was no mention of attempts to blind the observers. We assessed completeness of follow‐up as adequate if 90% or more of the enrolled participants had outcome data reported, inadequate if less than 90% of the participants had outcome data reported, or unclear if not mentioned in the trial.
Measures of treatment effect
For dichotomous outcomes, we calculated the results using the risk ratio (RR). We presented the effect estimates with 95% confidence intervals (CIs).
Assessment of heterogeneity
We looked for statistical heterogeneity by inspecting the forest plots for overlapping CIs, applying the Chi2 test (P value < 0.10 considered statistically significant) and the I2 statistic (I2 value of 50% used to denote moderate levels of heterogeneity). We assessed whether a difference in the intensity of supervision between the intervention and control group could explain heterogeneity.
Data synthesis
We used Review Manager 5 to analyse the data, using risk ratio (RR) with 95% CIs to assess estimates of effect. We used the fixed‐effect model when there was no statistically significant heterogeneity (Chi2 test, P > 0.1) and a random‐effects model when heterogeneity was present (I2 statistic > 50). We assessed the quality of the evidence using the GRADE approach.
Results
Description of studies
Eleven trials, enrolling 5662 participants, met the inclusion criteria (see 'Characteristics of included studies'), and we excluded 13 studies for the reasons listed in the 'Characteristics of excluded studies' table.
Nine included trials were individually RCTs, and two were cluster‐RCTs (Lwilla 2003 TZA; Newell 2006 NPL). One trial used a quasi‐random method of allocation (MacIntyre 2003 AUS).
Three trials were conducted in low‐income countries (Tanzania: Lwilla 2003 TZA; Wandwalo 2004 TZA; Nepal: Newell 2006 NPL); six in middle‐income countries (Taiwan: Hsieh 2008 TWN; Pakistan: Walley 2001 PAK; Thailand: Kamolratanakul 1999 THA; South Africa: Zwarenstein 1998 ZAF; Zwarenstein 2000 ZAF; and Swaziland: Wright 2004 SWZ); and two were from high‐income countries (Australia: MacIntyre 2003 AUS; USA: Chaisson 2001 USA).
Populations targeted
Ten trials evaluated DOT in people on treatment for active TB, and one evaluated directly observed prophylaxis in intravenous drug users (see Table 5; Table 6; Table 7).
1. Summary of interventions in trials of DOT versus self‐administered.
| Trial ID | DOT | Self administered therapy | |||||||
| Who observed? | Where? | How often? | Adherence recorded at each contact | Cure | Frequency of contact with health service | Adherence recorded at each contact | Cure | ||
| Intensive phase | Consolidation phase | ||||||||
| Zwarenstein 1998 ZAF | Nurses | Clinic | 5 times per week | 3 times per week | Yes | 38% (42/111) |
Weekly | Yes | 51% (31/61 |
| Zwarenstein 2000 ZAF | Nurse | Clinic | 5 times per week | 3 times per week | Yes | 57% (31/54) |
Weekly | Yes | 41% (9/22) |
| Lay health worker | Lay health workers home | ||||||||
| Kamolratanakul 1999 THA1 | Healthcare worker | Clinic | Daily | Daily | Yes | 76% (315/414) | Monthly | Unclear | 67% (283/422) |
| Community health worker | Home | Daily | Daily | ||||||
| Family member | Home | Daily | Daily | ||||||
| Walley 2001 PAK | Healthcare worker | Clinic | 6 times per week | 2 times per month | Yes | 59% (199/335) |
Every two weeks | Unclear | 62% (100/162) |
| Community health worker | Home | ||||||||
| Family member | Home | Daily | Daily | ||||||
| MacIntyre 2003 AUS2 | Family member | Home | Daily | Daily | Yes | Not reported | Monthly | Yes | Not reported |
| Hsieh 2008 TWN3 | Case manager or Hospital care |
Hospital | Daily | Once per week | Yes | 94% (30/32) |
Monthly unscheduled visit | Yes | 69% (22/32) |
1In Kamolratanakul 1999 THA patients could choose which observer they preferred and there a more intense supervision of observers in the intensive phase. 2In MacIntyre 2003 AUS nurses made weekly calls to the patients who were observed by a family member. 3In Hsieh 2008 TWN the case manager directly supervised medicine intake for first two months (Intensive phase), then self‐administration with weekly unscheduled visit.
2. Interventions comparing home versus clinic direct observation.
| Trial ID | DOT at patient's home | DOT at clinic | |||||||
| Who observed? | How often? | Supervision of observer | Cure | Who observed? | How often? | Cure | |||
| Intensive phase | Consolidation phase | Intensive phase | Consolidation phase | ||||||
| Walley 2001 PAK1 | Family member | Daily | Not described | Observers collected drugs from the clinic every 2 weeks | 55% (91/165) |
Health worker | 6 times per week | Self‐supervised | 64% (108/170) |
| Wandwalo 2004 TZA1 | Family member or former TB patient | Daily | Self‐supervised | Observers collected drugs from clinic weekly and spot checks were conducted by health worker | 43% (111/260) |
Health worker | Daily | Self‐supervised | 43% (141/327) |
| Zwarenstein 2000 ZAF | Lay health worker2 | 'Several times a week' | Not described | Observer collected drugs monthly | 57% (31/54) |
Health worker | 5 times a week | 3 times a week | 41% (24/58) |
| Lwilla 2003 TZA1 | Community volunteer | Daily | Self‐supervised | Observer was visited every two weeks by the health worker and every month by the district co‐ordinator3 | 53% (117/221) |
Health worker | Daily | Self‐supervised | 49% (148/301) |
1In Lwilla 2003 TZA, Walley 2001 PAK and Wandwalo 2004 TZA observation was during the intensive phase, while in the clinic observation arm of Zwarenstein 2000 ZAF it continued in the consolidated phase. 2In Zwarenstein 2000 ZAF the observation took place in the lay health worker's home, not the patient's home. 3In Lwilla 2003 TZA there was additional supervision by the district coordinator.
3. Interventions comparing family‐administered DOT versus community health worker DOT.
| Trial ID | Who observed? | Where? | How often? | Additional intervention | Who observed? | Where? | How often? | ||
| Intensive phase | Consolidation phase | Intensive phase | Consolidation phase | ||||||
| Newell 2006 NPL | Family member | Patient's home | Daily | Daily | Drugs supplied to supervisor every week | Community health worker | Patient's home1 | Daily | Daily |
| Wright 2004 SWZ | Family member | Patient's home | Daily | Daily | Patient reviewed at the diagnostic centre once per month Recorded in a patient adherence card |
Community health worker | Community health worker's home | Daily | Daily |
1In Newell 2006 NPL the community health worker mainly visited the patients at their homes but occasionally the patients came to the health worker's home.
Six trials compared DOT with self‐administered therapy:
Zwarenstein 1998 ZAF included two arms in two locations (Elsies River and Khayelitsha); Zwarenstein 2000 ZAF was the same trial containing data from one of these two locations, and had an additional arms (lay health worker administered DOT). The control arms (self‐administered treatment) were therefore the same for Elsies River in both trials, and so in the meta‐analysis we adjusted the data to ensure they were not counted twice.
Kamolratanakul 1999 THA allowed participants to choose between DOT by a health worker, community leader or family member; 85% chose the latter.
Walley 2001 PAK compared DOT by a health worker or community health worker with DOT by a family member and with self‐administration of treatment.
MacIntyre 2003 AUS evaluated DOT by a family member compared to self‐administration.
Hsieh 2008 TWN had DOT by case managers; there were three arms; weekly observation, monthly observation and the control group was patients admitted to hospital (Inpatient care).
Four trials compared different forms of DOT:
Newell 2006 NPL compared community health worker observation to family member observation.
Wandwalo 2004 TZA trials compared DOT by a family member with either DOT by a health worker at a health facility or DOT by a community health worker.
Wright 2004 SWZ compared community health worker observation to family member observation coupled with a once per week visit by a community health worker.
Lwilla 2003 TZA compared a community health worker DOT at home to DOT at a health facility.
One trial evaluated DOT in injecting (intravenous) drug users in the USA:
Chaisson 2001 USA involved intravenous drug users, and studied DOT by an outreach nurse with self‐administration either with monthly peer support or monthly clinic visits.
Intensity of supervision
Intensity of supervision varied in the included trials. For the six RCTs of DOT compared to self‐administered treatment, three trials appeared to be a direct comparison of healthcare worker administered DOT versus self‐administered. Another three trials appeared to have more intense supervision in the DOT arm only, with health workers visiting patients at home every two weeks. In Kamolratanakul 1999 THA, community health workers and family members received additional supervision by health centre staff once every two weeks. In MacIntyre 2003 AUS, nurses had weekly calls to the patients who were observed by family members. In Hsieh 2008 TWN the case manager visited the patients in the intervention arm and was supervised by weekly unscheduled supervision. In the control group of these trials no such intensive supervision was described.
Adjustment for clustering
Both cluster‐RCTs adjusted for clustering appropriately: standard error of the coefficients for clustering on units corrected using the Huber‐White‐Sandwich method (Lwilla 2003 TZA); and, in Newell 2006 NPL, using the coefficient of variation between clusters.
Risk of bias in included studies
We have summarized the 'Risk of bias' assessments Figure 2 and Figure 3, and have listed the reasons in the Characteristics of included studies section.
2.
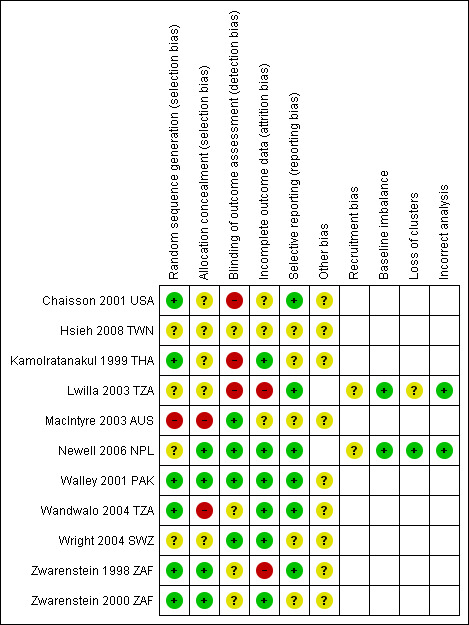
Risk of bias summary: review authors' judgements about each risk of bias item for each included trial.
3.
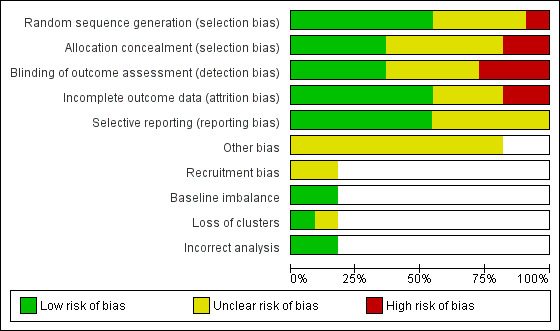
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials.
Allocation
Seven trials used adequate methods to generate a random sequence: computer‐generated random sequences (Chaisson 2001 USA; Walley 2001 PAK; Zwarenstein 1998 ZAF; Zwarenstein 2000 ZAF), a random‐number table (Kamolratanakul 1999 THA), coin tossing (Wandwalo 2004 TZA) or drawing of lots from a basket (Newell 2006 NPL). One trial used alternate allocation, which was an inadequate randomization method (MacIntyre 2003 AUS). The remaining trials reports did not provide information (Hsieh 2008 TWN; Lwilla 2003 TZA; Wright 2004 SWZ).
Four trials employed adequate methods for concealing allocation (Newell 2006 NPL; Walley 2001 PAK; Zwarenstein 1998 ZAF; Zwarenstein 2000 ZAF). Five trials had unclear allocation concealment (Chaisson 2001 USA; Hsieh 2008 TWN; Kamolratanakul 1999 THA; Lwilla 2003 TZA; Wright 2004 SWZ) and the remaining two trials did not use allocation concealment (MacIntyre 2003 AUS; Wandwalo 2004 TZA).
Blinding
Only four trials blinded outcome assessment (MacIntyre 2003 AUS; Newell 2006 NPL; Walley 2001 PAK; Wright 2004 SWZ). It was not used in three trials (Chaisson 2001 USA; Kamolratanakul 1999 THA; Lwilla 2003 TZA) and unclear in the remaining trials (Hsieh 2008 TWN; Wandwalo 2004 TZA; Zwarenstein 1998 ZAF; Zwarenstein 2000 ZAF).
Incomplete outcome data
Two trials excluded more than 10% of participants from the analyses (Lwilla 2003 TZA; Zwarenstein 1998 ZAF). A further three trials did not provide sufficient information to assess this aspect of trial quality (MacIntyre 2003 AUS; Newell 2006 NPL; Zwarenstein 2000 ZAF). The remaining trials had adequate follow‐up.
Selective reporting
We found no evidence of selective reporting.
Other potential sources of bias
Hsieh 2008 TWN had a control group which was inpatient based. We have not included this group in our analyses. Two trials had the same control groups (Zwarenstein 1998 ZAF; Zwarenstein 2000 ZAF; see Table 5).
Lwilla 2003 TZA had one cluster in the community observed arm lost to follow‐up and we therefore did not include it in the final analysis. Two cluster‐RCTs had cluster adjustment.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
1. DOT versus self‐administered therapy
The details of the interventions are described in Table 5; and see Table 1.
Six trials compared DOT and self‐administered therapy. The observers were described as either nurses (Zwarenstein 1998 ZAF; Zwarenstein 2000 ZAF), healthcare workers (Kamolratanakul 1999 THA; Walley 2001 PAK), community health workers (Kamolratanakul 1999 THA; Walley 2001 PAK), lay health workers (Zwarenstein 2000 ZAF), case managers (Hsieh 2008 TWN) or family members (Kamolratanakul 1999 THA; MacIntyre 2003 AUS; Walley 2001 PAK). In one trial participants were allowed to choose either a healthcare worker, a community health worker or a family member (Kamolratanakul 1999 THA).
Overall TB cure was low with self‐administered therapy, ranging from 41% to 69% across trials, but on average this did not substantially improve with DOT (RR 1.08, 95% CI 0.91 to 1.27; five trials, 1645 participants, moderate quality evidence; Analysis 1.1). However, there was moderate statistical heterogeneity between trials (I2 statistic = 68%; P = 0.01), with two trials finding benefits which reached standard levels of statistical significance (Kamolratanakul 1999 THA; Hsieh 2008 TWN). These differential effects may be explained by differences in the intensity of follow‐up between the intervention and control arms (Analysis 1.2). However it is important to note that these two trials were also at unclear or high risk of selection bias and detection bias.
1.1. Analysis.
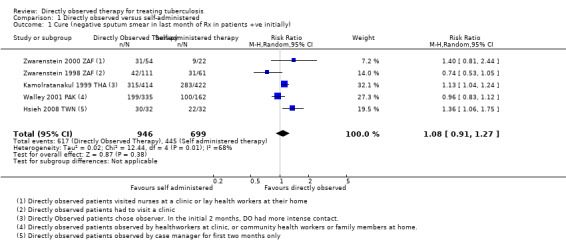
Comparison 1 Directly observed versus self‐administered, Outcome 1 Cure (negative sputum smear in last month of Rx in patients +ve initially).
1.2. Analysis.
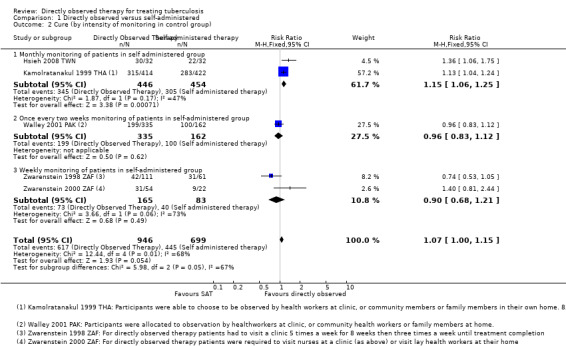
Comparison 1 Directly observed versus self‐administered, Outcome 2 Cure (by intensity of monitoring in control group).
Kamolratanakul 1999 THA is the largest trial of DOT to date and found a higher TB cure with the intervention (76% versus 67%; RR 1.13, 95% CI 1.04 to 1.24; one trial, 836 participants). This trial had the least supervised control group (patients picked up their medication monthly), and one of the most intensely supervised intervention groups (doses were directly observed daily by a choice of health worker, community health worker or family member, and a health worker visited the patient at home every two weeks to check on adherence). This difference in intensity was similar in the second trial showing a difference (94% versus 69%; RR 1.36, 95% CI 1.06 to 1.75; one trial, 64 participants), but this trial was small and underpowered to have full confidence in this effect (Hsieh 2008 TWN).
Similarly, TB treatment completion ranged from 59% to 78% in those allocated to self‐administration, and on average did not substantially improve with DOT (RR 1.07, 95% CI 0.96 to 1.19; six trials, 1839 participants, moderate quality evidence; Analysis 1.3). There was again moderate heterogeneity between trials (I2 = 57%; P = 0.04), with the same two trials finding statistically significant benefits (Hsieh 2008 TWN; Kamolratanakul 1999 THA).
1.3. Analysis.
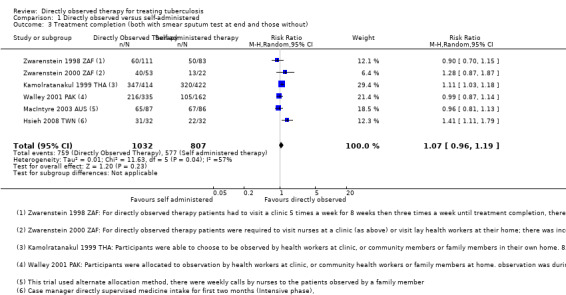
Comparison 1 Directly observed versus self‐administered, Outcome 3 Treatment completion (both with smear sputum test at end and those without).
Different levels of monitoring in the self‐administered groups did not yield substantially different levels of completion. (Self‐treatment group: monthly monitoring RR 1.12, 95% 0.95 to 1.31; three trials, 1073 participants; every two weeks: RR 0.99, 95% 0.87 to 1.14; one trial, 497 participants); weekly monitoring RR 1.04, 95% 0.74 to 1.46; two trials, 269 participants; Analysis 1.4).
1.4. Analysis.
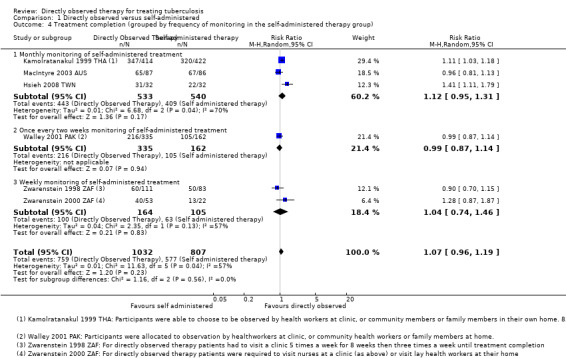
Comparison 1 Directly observed versus self‐administered, Outcome 4 Treatment completion (grouped by frequency of monitoring in the self‐administered therapy group).
2. Home observation versus clinic observation
The trials are described in Table 6; and see Table 2.
Four trials compared home with clinic observation. Two tested family member direct observation against direct observation at clinic (Walley 2001 PAK; Wandwalo 2004 TZA) while the other two tested community health worker home visits to direct observation at clinic (Lwilla 2003 TZA; Zwarenstein 2000 ZAF).
TB cure was generally low for both the home observation groups (ranging from 43% to 57%) and for clinic observation (ranging from 41% to 64%). On average there was little or no difference between the two strategies (RR 1.02, 95% CI 0.88 to 1.18; four trials, 1556 participants, moderate quality evidence; Analysis 2.1).
2.1. Analysis.
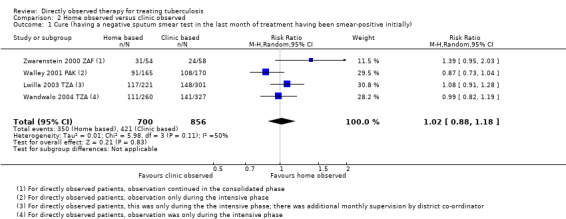
Comparison 2 Home observed versus clinic observed, Outcome 1 Cure (having a negative sputum smear test in the last month of treatment having been smear‐positive initially).
Treatment completion ranged from 62% to 85% in those being observed at home and between 57% and 83% in clinic observation. On average there was little or no difference between the two locations (RR 1.04, 95% CI 0.91 to 1.17; three trials, 1034 participants, moderate quality evidence; Analysis 2.2).
2.2. Analysis.
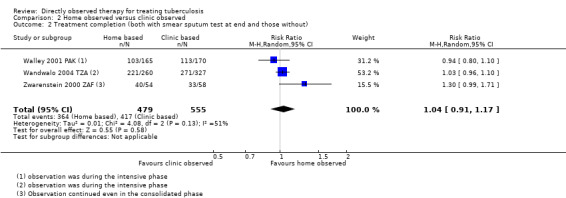
Comparison 2 Home observed versus clinic observed, Outcome 2 Treatment completion (both with smear sputum test at end and those without).
One trial, Lwilla 2003 TZA, had more intense supervision of the observer than the other three trials. This intense supervision however did not improve cure rates (53% for home observation and 49% for clinic observation; RR 1.01, 95% CI 0.91 to 1.11; four trials, 1556 participants, Analysis 2.3). This trial however did not report on completion of treatment.
2.3. Analysis.
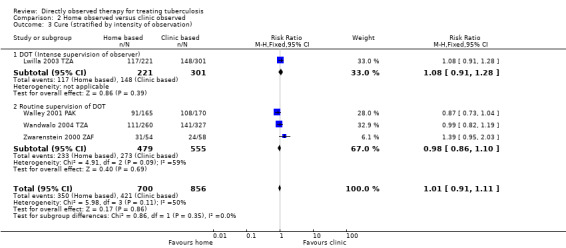
Comparison 2 Home observed versus clinic observed, Outcome 3 Cure (stratified by intensity of observation).
Wandwalo 2004 TZA had high completion rates (85% in home and 83% in clinic observation arm) but the cure rates were quite low in either arm (43% in both arms).
3. Community observed versus family observed
Two trials compared community health worker based observation with family based observation (Newell 2006 NPL; Wright 2004 SWZ). The trials are described in Table 7.
The Nepal trial, Newell 2006 NPL, had higher cure rates across the two arms (85% for community and 89% for family observed) compared with Wright 2004 SWZ (68% for community and 61% for family observed). There was little or no difference between community and family observation (RR 1.02, 95% CI 0.86 to 1.21; two trials, 1493 participants, moderate quality evidence; Analysis 3.1). However there was high statistical heterogeneity (I2 = 86%; P = 0.009).
3.1. Analysis.
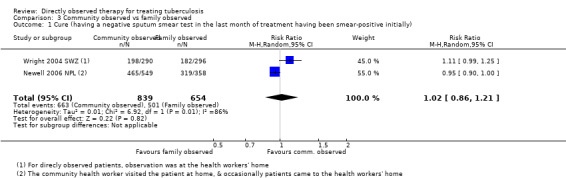
Comparison 3 Community observed vs family observed, Outcome 1 Cure (having a negative sputum smear test in the last month of treatment having been smear‐positive initially).
Similarly, for the completion of treatment outcome Newell 2006 NPL had higher rates across the two arms (96% in both arms) compared with Wright 2004 SWZ (74% for community and 67% for family observed). There was little or no difference between community and family observation (RR 1.05, 95% CI 0.90 to 1.22; two trials, 1493 participants, low quality evidence; Analysis 3.2). Again there was high statistical heterogeneity (I2 = 87%; P = 0.005).
3.2. Analysis.
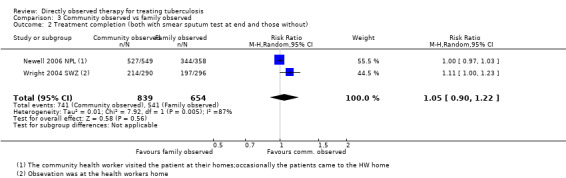
Comparison 3 Community observed vs family observed, Outcome 2 Treatment completion (both with smear sputum test at end and those without).
4. DOT versus self‐administered therapy for intravenous drug users
One trial, Chaisson 2001 USA, had three arms, supervision at a clinic, peer group supervision and self‐administered treatment. The level of treatment completion was similar in those self‐administering (79%) and those under peer or clinic supervision (79%) (RR 1.00, 95% CI 0.88 to 1.13; one trial, 300 participants, low quality evidence; Analysis 4.1).
4.1. Analysis.
Comparison 4 Injecting drug users, Outcome 1 Treatment completion.
Discussion
Summary of main results
TB cure and treatment completion were low with self‐administered therapy in these trials, and direct observation did not substantially improve this. Positive effects with direct observation were seen in two trials where patients in the control group were only seen in clinic once a month, but not in the three trials where the controls were seen more frequently (every one or two weeks).
Trials comparing home observation (community observer or family observer) to clinic or healthcare worker led observation did not show any difference in TB cure or treatment completion. Within home‐based direct observation, there were no differences between direct observation by a family member and direct observation by a community health worker.
Overall completeness and applicability of evidence
This Cochrane Review includes trials from both high‐ and low‐burden countries, conducted between 1994 and 2008. Direct observation was implemented in line with current recommendations, and the findings remain applicable to TB treatment programmes today.
Cure and treatment completion with self‐administered treatment were low in these trials, consistent with the outcomes seen in TB programmes at the time, and consequently it is remarkable that direct observation failed to substantially improve these.
One interpretation, offered by Frieden 2007, is that these trials failed to implement direct observation effectively. This interpretation seems unreasonable to us, as the authors of the included trials did what they could to implement direct observation, and it may even be harder to implement, and less successful, outside of a clinical trial . Alternative interpretations are that the health systems were struggling to deliver TB treatment, and direct observation on its own did not resolve these underlying issues, or that TB patients experience financial or logistical barriers to compliance with direct observation. For example, it may cost patients money if they have to visit a health facility as was the case in Walley 2001 PAK.
Direct observation as a strategy is still debated in TB and other chronic diseases. These debates and the findings of this review and others are important given the often huge resource implications of implementing a direct observation therapy programme. In two studies conducted in Brazil to evaluate the cost effectiveness of direct observation strategy; one reported a doubling of indirect costs to the patient compared to self‐administered therapy (Mohan 2007) while the other reported an incremental cost‐effectiveness ratio (ICER) of USD6616 per completed direct observed treatment compared to self‐administered therapy (Steffen 2010).
Agreements and disagreements with other studies or reviews
The findings of this Cochrane Review are similar to the findings of a meta‐analysis by Pasipanodya 2013, who reported no difference between DOT and self‐administered treatment in terms of reduction in microbiological failure, adverse drug reactions acquired resistance and relapses. The meta‐analysis included ten studies, five RCTs and five observational studies. However, it is worth noting that the included trials were quite heterogenous for a meta‐analysis, the quality scales used were quite unclear and their findings were probably influenced by one observational study.
In their clinical review, Chan 2002 reported that direct observation is essential and effective for treatment and, by extension, TB elimination. The review was not systematic and mainly looked at areas where DOT has been done in conjunction with other interventions. It is probable that the other interventions or inputs, rather than specifically observing a patient as they take their medication, were beneficial for benefit, as highlighted by Volmink 2000b. A review by Tian 2014 reported that direct observation at a clinic was not more effective than self‐treatment; but that community direct observation may be, with no difference detected between family and non‐family direct observation. The review did not assess the inputs and associated supervision to the extent that we did in this Cochrane Review.
Ford 2009, a review of direct observation in HIV therapy, also reported no effect on virological suppression. Though it might be argued that the therapy of these two diseases is different given that TB is for a finite duration whereas HIV is lifelong and thus adherence issues are different.
Authors' conclusions
Implications for practice.
The available evidence indicates that direct observation, even when supervised by health staff, does not resolve poor adherence in TB treatment. Given the huge cost implications of direct observation, policy makers therefore might want to rethink their strategies for improving adherence. It is probably worthwhile in considering financial and logistical barriers to care, motivating patients and staff, and enhancing defaulter tracing mechanisms.
Implications for research.
The lack of effects of direct observation in improving cure and completion rates is surprising but reflects the complexity of adherence. Further research in well functioning health systems is needed to assess alternative and complementary strategies to direct observation. Qualitative work focusing on defaulters, where defaulter mechanisms exists and how clinicians interact with patients would especially be important. Evaluation of the cost of DOT for patients and providers would also help in properly assessing these strategies.
What's new
| Date | Event | Description |
|---|---|---|
| 13 May 2015 | New search has been performed | We added a trial and a table documenting in detail the inputs to the intervention and control groups. Also, we constructed 'Summary of findings' tables and carried out additional analyses investigating possible effects of confounding by intense health worker contacts. We rewrote the review and conclusions. |
| 13 May 2015 | New citation required but conclusions have not changed | One trial was added and summary of findings tables were constructed. |
History
Protocol first published: Issue 4, 2001 Review first published: Issue 4, 2001
| Date | Event | Description |
|---|---|---|
| 11 August 2011 | New search has been performed | Categorised as Current question ‐ no update intended (results conclusive). See "Published notes" section for details |
| 10 August 2011 | Amended | Pilot classification system added; explanation provided in "published notes" section |
| 19 September 2008 | Amended | Converted to new review format with minor editing. |
| 13 August 2007 | New citation required and conclusions have changed | 2007, Issue 4: One new trial included (Newell 2006 NPL). Also added references to new tuberculosis adherence reviews in the 'Background' section and reworded objectives to clarify that the review encompasses comparisons between different types of directly observed therapy. |
| 15 February 2006 | Amended | 2006, Issue 2 (Volmink 2006): Four new trials included (Lwilla 2003 TZA; MacIntyre 2003 AUS; Wandwalo 2004 TZA; Wright 2004 SWZ). |
| 19 November 2003 | New citation required and conclusions have changed | 2003, Issue 1: Two trials added (Chaisson 2001 USA; Malotte 2001 USAa). |
| 8 August 2001 | New citation required and major changes | 2001, Issue 4 (Volmink 2001): first version of this review on directly observed therapy. 2000, Issue 4 (Volmink 2000a): original review split into a series of Cochrane Reviews, each focusing on particular intervention promotion strategies, such as directly observed therapy in this review. 1997, Issue 2: review first published as 'Interventions for promoting adherence to tuberculosis management'. |
Acknowledgements
We acknowledge the Aubrey Sheiham Public Health and Primary Care Scholarships for supporting Jamlick Karumbi in updating this Cochrane Review. The editorial base for the CIDG is funded by the UK Department for International Development (DFID) for the benefit of developing countries.
Appendices
Appendix 1. Search methods: detailed search strategies
| Search set | CIDG SRa | CENTRAL | MEDLINEb | EMBASEb | LILACSb |
| 1 | tuberculosis | tuberculosis | tuberculosis | tuberculosis | tuberculosis |
| 2 | DOT* | PATIENT COMPLIANCE | PATIENT COMPLIANCE | PATIENT COMPLIANCE | DOT* |
| 3 | directly observed therapy | PATIENT PARTICIPATION | PATIENT PARTICIPATION | PATIENT MONITORING | supervision |
| 4 | 2 or 3 | patient monitoring | MOTIVATION | DOT$ | 2 or 3 |
| 5 | 1 and 4 | MOTIVATION | DECISION SUPPORT TECHNIQUES | directly observed therapy | 1 and 4 |
| 6 | — | DECISION SUPPORT TECHNIQUES | DOT* | compliance | — |
| 7 | — | DOT* | directly observed therapy | motivation | — |
| 8 | — | directly observed therapy | compliance | patient$ | — |
| 9 | — | compliance | patient* | defaulter$ | — |
| 10 | — | defaulter* | defaulter* | adheren$ | — |
| 11 | — | adheren* | adheren* | supervis$ | — |
| 12 | — | supervision* | supervis* | 2‐11/or | — |
| 13 | — | 2‐12/or | 2‐12/or | 1 and 12 | — |
| 14 | — | 1 and 13 | 1 and 13 | Limit 13 to human | — |
| 15 | — | — | Limit 14 to human | — | — |
aCIDG Specialized Register. bSearch terms used in combination with the search strategy for retrieving trials developed by Cochrane (Higgins 2011); upper case: MeSH or EMTREE heading; lower case: free text term.
Data and analyses
Comparison 1. Directly observed versus self‐administered.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cure (negative sputum smear in last month of Rx in patients +ve initially) | 5 | 1645 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.27] |
| 2 Cure (by intensity of monitoring in control group) | 5 | 1645 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.00, 1.15] |
| 2.1 Monthly monitoring of patients in self administered group | 2 | 900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [1.06, 1.25] |
| 2.2 Once every two weeks monitoring of patients in self‐administered group | 1 | 497 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.83, 1.12] |
| 2.3 Weekly monitoring of patients in self‐administered group | 2 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.68, 1.21] |
| 3 Treatment completion (both with smear sputum test at end and those without) | 6 | 1839 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.96, 1.19] |
| 4 Treatment completion (grouped by frequency of monitoring in the self‐administered therapy group) | 6 | 1839 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.96, 1.19] |
| 4.1 Monthly monitoring of self‐administered treatment | 3 | 1073 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.95, 1.31] |
| 4.2 Once every two weeks monitoring of self‐administered treatment | 1 | 497 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.87, 1.14] |
| 4.3 Weekly monitoring of self‐administered treatment | 2 | 269 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.74, 1.46] |
Comparison 2. Home observed versus clinic observed.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cure (having a negative sputum smear test in the last month of treatment having been smear‐positive initially) | 4 | 1556 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.88, 1.18] |
| 2 Treatment completion (both with smear sputum test at end and those without) | 3 | 1034 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.91, 1.17] |
| 3 Cure (stratified by intensity of observation) | 4 | 1556 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.91, 1.11] |
| 3.1 DOT (Intense supervision of observer) | 1 | 522 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.91, 1.28] |
| 3.2 Routine supervision of DOT | 3 | 1034 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.86, 1.10] |
Comparison 3. Community observed vs family observed.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cure (having a negative sputum smear test in the last month of treatment having been smear‐positive initially) | 2 | 1493 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.86, 1.21] |
| 2 Treatment completion (both with smear sputum test at end and those without) | 2 | 1493 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.90, 1.22] |
Comparison 4. Injecting drug users.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Treatment completion | 1 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.88, 1.13] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chaisson 2001 USA.
| Methods | Generation of allocation sequence: randomized, with factorial overlay; computer‐generated random numbers. Allocation concealment: not stated. Blinding: none. Completeness of follow‐up: 88%. |
|
| Participants | Number: 300 randomized; 73% men; 85% unemployed; 27% with documented human immunodeficiency virus (HIV) infection. Included: adult, intravenous drug users with positive tuberculin skin test (at least 10 mm induration or 5 mm if HIV positive); given isoniazid preventive therapy for 6 months. Excluded: people with active TB. |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Location: Baltimore City Health Department TB Clinic, USA. Date: 1995 to 1997. Duration of DOT duration not stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "generated using computer algorithm". |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | None. "Blinding of the study was not possible." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | There were losses to follow‐up in each arm though not differential there are no reports on them. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methodology are reported. |
| Other bias | Unclear risk | Not applicable. |
Hsieh 2008 TWN.
| Methods | Generation of allocation sequence: not stated. Randomization: stratified. Allocation concealment: not stated. Blinding: not stated. Completeness of follow‐up: no losses (18/114) dropped to enable matching. |
|
| Participants | Number; 96 randomized into three groups; Matched by age and gender; confirmed TB diagnosis and over 18 yrs. | |
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Location: Taiwan. Trial period: May 2002 to July 2003. Duration of observation was 6 months. The patients were not given a choice of DOT observer. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "There were 114 subjects meeting the sampling criteria who were then matched by age and gender and randomized into one of three groups". |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 18/114 dropped to enable matching. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated in the methodology are reported. |
| Other bias | Unclear risk | Not applicable. |
Kamolratanakul 1999 THA.
| Methods | Generation of allocation sequence: central block random allocation scheme prepared for each of 15 trial sites; random‐number table used. Allocation concealment: none. Blinding: no blinding of assessors. Completeness of follow‐up: 100% (no losses). |
|
| Participants | Number: 837 randomized; 73% male. Included: new smear positive adults (aged 15+). |
|
| Interventions |
All participants received the same drug regimen: isoniazid‐rifampicin‐pyrazinamide‐ethambutol for 2 months and isoniazid‐rifampicin for 4 months. |
|
| Outcomes |
|
|
| Notes | Location: Thailand. Date: 1996 to 1997. Duration of DOT not stated. Informed consent not obtained as participants were not told that they were participating in a study. Choice of supervisor for DOT participants: 352 chose a family member; 34 chose a community member; and 24 chose health centre staff. One participant in daily supervision arm excluded due to protocol violation so not strictly intention‐to‐treat. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Generated using random number tables. |
| Allocation concealment (selection bias) | Unclear risk | Inadequate information. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Investigators not blinded though the patients were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no exclusions. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated in the methodology are reported. |
| Other bias | Unclear risk | Not applicable. |
Lwilla 2003 TZA.
| Methods | Cluster‐RCT: 9 pairs of centres matched by type and size. Generation of allocation sequence: unclear. Allocation concealment: unclear. Blinding: none. Completeness of follow‐up: 87% at 2 months and 69% at 7 months. |
|
| Participants | Number: 18 clusters randomized; 522 participants; mean age 35; 60% male. Included: new smear positive adults. |
|
| Interventions |
Continuation phase of 6 months: both groups managed the same and expected to self‐administer treatment daily. |
|
| Outcomes |
|
|
| Notes | Location: Tanzania. Date: 1999 to 2000. Duration of DOT not stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details reported. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | None. "This study was an unmasked cluster randomized trial". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 68% (311/437 participants) were evaluated at 7 months. (This could affect the cure outcome). |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methodology are reported. |
| Recruitment bias | Unclear risk | No details of any shifting, though the cluster sizes varied from as low as 2 persons to 232 persons. |
| Baseline imbalance | Low risk | Clusters were similar though the size varied and one cluster had possibly a more sicker patient profile due to its highly specialized nature. |
| Loss of clusters | Unclear risk | One cluster in the community based intervention did not have patients hence was dropped in the analysis. |
| Incorrect analysis | Low risk | Cluster adjusted hence comparable to other RCTs randomizing individuals. |
MacIntyre 2003 AUS.
| Methods | Quasi‐RCT Generation of allocation sequence: alternate allocation Concealment of allocation: none Blinding: assessment of urinary isoniazid blinded Completeness of follow‐up: not stated |
|
| Participants | Number: 173 recruited, mostly foreign nationals; male 51%; mean age 41 (range 14 to 83). Included: new TB participants. Excluded: multiple‐drug resistant TB; relapsed TB; human immunodeficiency virus (HIV)‐positive cases; and nontuberculous mycobacterial infections. |
|
| Interventions |
Both groups had monthly visits to health facilities and standardized recording charts. |
|
| Outcomes | Treatment completion measured by:
|
|
| Notes | Location: Australia. Date: 1998 to December 2000. Duration of DOT not stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomly. "Patients were systematically allocated to receive FDOT or ST". |
| Allocation concealment (selection bias) | High risk | Systematic allocation "The first patient was randomly allocated to the ST arm, every second patient was allocated to FDOT, and the remainder to ST". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information as to what happened to those who refused family DOT. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated in the methodology are reported. |
| Other bias | Unclear risk | Not applicable. |
Newell 2006 NPL.
| Methods | Cluster‐RCT. Generation of allocation sequence: 5 randomly selected districts allocated to each arm; the name of each district was written on an individual paper and randomly drawn from a basket. Allocation concealment: method not stated. Blinding: laboratory technicians assessing the primary outcomes were blinded. Completeness of follow‐up: 100% (no clusters or individuals lost). |
|
| Participants | Number: 10 districts with 907 people randomized; all smear positive; 67% male. Included: people with TB (aged 15+); new smear‐positive cases, diagnosed at health facilities in the trial area; human immunodeficiency virus (HIV) status not known. |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Location: hill and mountain districts of Nepal. Date: 2002 to 2003. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information on selection of 10 districts out of 17. |
| Allocation concealment (selection bias) | Low risk | Randomly picked papers from an opaque bag. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No cluster was lost to follow‐up or excluded. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methodology are reported. |
| Recruitment bias | Unclear risk | Not reported if there were patients who shifted to the different intervention arms, though they were separated by a mountainous region. |
| Baseline imbalance | Low risk | Characteristics similar. |
| Loss of clusters | Low risk | No loss reported. |
| Incorrect analysis | Low risk | Cluster adjustment done. |
Walley 2001 PAK.
| Methods | Generation of allocation sequence: computer‐generated random numbers. Allocation concealment: opaque, sealed envelopes. Blinding: assessors blinded. Completeness of follow‐up: not stated. |
|
| Participants | Number: 497 randomized; 51.3% male. Included: adults (aged 15+); new smear‐positive cases. |
|
| Interventions |
All participants received isoniazid‐rifampicin‐pyrazinamide‐ethambutol for 2 months and isoniazid‐ethambutol for 6 months. |
|
| Outcomes |
|
|
| Notes | Location: Pakistan Date: 1996 to 1998 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated random sequence. |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes were used and third party calls. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no exclusions after randomization. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methodology are reported. |
| Other bias | Unclear risk | Not applicable. |
Wandwalo 2004 TZA.
| Methods | Generation of allocation sequence: coin tossing in each of 5 clinics. Allocation concealment: none. Blinding: none. Completeness of follow‐up: 100% (no losses). |
|
| Participants | Number: 587 randomized; 322 smear positive, 182 smear negative, and 83 extrapulmonary TB; 57% male. Included: people with TB (aged 5+); new smear positive, smear negative, and extrapulmonary cases; human immunodeficiency virus (HIV) status not known. Excluded: previously treated for TB; severe illness; transferred from another clinic; previously enrolled in the study. |
|
| Interventions |
Apart from the observation option participants received the same standardized management including drug therapy. |
|
| Outcomes |
|
|
| Notes | Location: Dar es Salaam, Tanzania. Date: 2001 to 2003. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomly by coin toss". |
| Allocation concealment (selection bias) | High risk | None. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No exclusions. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methodology are reported. |
| Other bias | Unclear risk | Not applicable. |
Wright 2004 SWZ.
| Methods | Generation of allocation sequence: unclear; stratified into adults and children; then, within each group, randomized by type of TB (sputum positive, sputum negative, extrapulmonary, relapse). Allocation concealment: unclear; sealed, sequentially numbered envelopes not stated if opaque. Blinding: assessors of sputum results blinded. Completeness of follow‐up: 98%. |
|
| Participants | Number: 1353 randomized; 55% male; most 15+ years. Included: adults and children with smear positive or negative, extrapulmonary TB, or relapse of previously treated TB. Excluded: died before discharge; or too ill to receive outpatient treatment; lived in area without treatment supporter; or referred in after treatment commenced. |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Location: Swaziland. Date: 2000 to 2002. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. |
| Allocation concealment (selection bias) | Unclear risk | Use of sealed envelopes not clear whether opaque. " sealed, sequentially numbered, stratum specific envelopes containing treatment assignments". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Laboratory assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Non differential loss to follow‐up (4/664 and 5/662). |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated in the methodology are reported. |
| Other bias | Unclear risk | Not applicable. |
Zwarenstein 1998 ZAF.
| Methods | Generation of allocation sequence: computer‐generated random numbers. Allocation concealment: consecutively numbered, opaque, sealed envelopes in each of 5 clinics. Blinding: none. Completeness of follow‐up: 114/120 (95%) in 1 trial and 102/120 (85%) in other trial excluded from analysis. |
|
| Participants | Number: 216 included in analysis; 62% male; 57% < 35 years. Included: adults (aged 15+) with pulmonary TB; both new and re‐treatment cases. Excluded: severe disease or multiple drug resistance; treatment at a non‐study clinic for more than 2 weeks; need to be supervised at school or at the workplace; and leaving the area within a month. |
|
| Interventions |
New cases received Rifater (combined rifampicin‐isoniazid‐pyrazinamide) for 8 weeks followed by Rifinah 4 (combined rifampicin‐isoniazid) plus additional isoniazid for 18 weeks. Retreatment participants received Rifater plus ethambutol for 12 weeks and Rifinah plus rifampicin‐ethambutol for 22 weeks. |
|
| Outcomes |
|
|
| Notes | Location: 1 trial in each of 2 low‐income communities near Cape Town, South Africa. Date: 1994 to 1995. Results combined. 54 participants in 1 trial allocated to community supervision not reported in this paper. Exclusions from analysis: trial 1 (6 cases of multiple drug resistance) and trial 2 (12 cases of multiple drug resistance and 6 not TB). Number of exclusions per arm of the 2 trials not given. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random sequence generated by a computer algorithm". |
| Allocation concealment (selection bias) | Low risk | "Consecutively numbered opaque sealed envelops were used". |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information on whether there was any blinding or not. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There was differential exclusions between the intervention and control arms. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methodology are reported. |
| Other bias | Unclear risk | Not applicable. |
Zwarenstein 2000 ZAF.
| Methods | Generation of allocation sequence: computer‐generated random numbers. Allocation concealment: consecutively numbered, opaque, sealed envelopes. Blinding: none. Completeness of follow‐up: not stated. |
|
| Participants | Number: 174 randomized. Included: new or re‐treatment participants aged 15+ who were sputum or culture positive. |
|
| Interventions |
|
|
| Outcomes | As for Zwarenstein 1998 ZAF. | |
| Notes | Location: 4 clinics in a township near Cape Town, South Africa. Date: 1994 to 1995. 18 participants excluded from analysis: 12 with multiple‐drug resistant TB and 6 not TB. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence generated by a computer algorithm. |
| Allocation concealment (selection bias) | Low risk | Consecutively numbered opaque sealed envelopes. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information on whether there was any blinding or not. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were exclusions though not differentiated between intervention arms. "After exclusion of 12 MDR and six non‐TB patients". |
| Selective reporting (reporting bias) | Unclear risk | All outcomes stated in the methodology are reported. |
| Other bias | Unclear risk | Not applicable. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Batki 2002 | Compared direct observation plus with methadone treatment for injecting drug users with routine TB treatment without methadone. |
| Carroll 2004 | Before‐and‐after study; no control group. |
| Hwang 2004 | Not randomized. |
| Jasmer 2004 | Different criteria for allocation to self‐administration or direct observation. |
| Lewin 2004 | An educational intervention was evaluated. |
| Malotte 2001 | Evaluates incentives for IV drug users within the context of a direct observation programme. |
| Matthew 2002 | Cohort study. |
| Moulding 2002 | Trial evaluating devices that monitor treatment using uranium along a strip of photographic film. |
| Pungrassami 2002a | Not randomly allocated; A publication reporting same data as Pungrassami 2002b. |
| Pungrassami 2002b | Not randomly allocated; A publication reporting same data as Pungrassami 2002a. |
| Sorete‐Abore 2002 | Cohort study. |
| Tandon 2002 | Described as a RCT, but the randomization led to very different numbers in the 2 groups; subsequently over 50 participants (out of a total of 379) crossed over from self‐treatment to direct observation and were excluded from the analysis; little detail for the rest of the study provided. |
| Thiam 2007 | Multifaceted intervention including DOT. |
| Toyota 2003 | Patients in hospital. |
Contributions of authors
Jimmy Volmink and Paul Garner carried out the first edition of this Cochrane Review (Volmink 2001) and review updates (Volmink 2003; Volmink 2006; Volmink 2007). Jamlick Karumbi performed this review update, assisted by Paul Garner. All review authors reviewed and approved the final manuscript.
Sources of support
Internal sources
South African Medical Research Council, South Africa.
Liverpool School of Tropical Medicine, UK.
External sources
Department for International Development, UK.
Declarations of interest
As a result of the earlier editions of this review from the mid 1990s, PG has become recognised and associated with the continued debate about whether DOT should be central to national programmes in low‐ and middle‐income countries.
Unchanged
References
References to studies included in this review
Chaisson 2001 USA {published data only}
- Chaisson RE, Barnes GL, Hackman J, Watkinson L, Kimbrough L, Metha S, et al. A randomized, controlled trial of interventions to improve adherence to isoniazid therapy to prevent tuberculosis in injection drug users. American Journal of Medicine 2001;110(8):610‐5. [DOI] [PubMed] [Google Scholar]
Hsieh 2008 TWN {published data only}
- Hsieh CJ, Lin LC, Kuo BI, Chiang CH, Su WJ, Shih JF. Exploring the efficacy of a case management model using DOTS in the adherence of patients with pulmonary tuberculosis. Journal of Clinical Nursing 2008;17(7):869‐75. [DOI] [PubMed] [Google Scholar]
Kamolratanakul 1999 THA {published data only}
- Kamolratanakul P, Sawert H, Lertmaharit S, Kasetjaroen Y, Akksilp S, Tulaporn C, et al. Randomized controlled trial of directly observed treatment (DOT) for patients with pulmonary tuberculosis in Thailand. Transactions of the Royal Society of Tropical Medicine and Hygiene 1999;93(5):552‐7. [DOI] [PubMed] [Google Scholar]
Lwilla 2003 TZA {published data only}
- Lwilla F, Schellenberg D, Masanja H, Acosta C, Galindo C, Aponte J, et al. Evaluation of efficacy of community‐based vs. institutional‐based direct observed short‐course treatment for the control of tuberculosis in Kilombero district, Tanzania. Tropical Medicine and International Health 2003;8(3):204‐10. [DOI] [PubMed] [Google Scholar]
MacIntyre 2003 AUS {published data only}
- MacIntyre CR, Goebel K, Brown GV, Skull S, Starr M, Fullinfaw RO. A randomised controlled trial of the efficacy of family‐based direct observation of anti‐tuberculosis treatment in an urban, developed‐country setting. International Journal of Tuberculosis and Lung Disease 2003;7(9):848‐54. [PubMed] [Google Scholar]
Newell 2006 NPL {published data only}
- Newell JN, Baral SC, Pande SB, Bam DS, Malla P. Family‐member DOTS and community DOTS for tuberculosis control in Nepal: cluster‐randomised controlled trial. Lancet 2006;367(9514):903‐9. [DOI] [PubMed] [Google Scholar]
Walley 2001 PAK {published data only}
- Khan MA, Walley JD, Witter SN, Imran A, Safdar N. Costs and cost‐effectiveness of different DOT strategies for the treatment of tuberculosis in Pakistan. Directly Observed Treatment. Health Policy and Planning 2002;17(2):178‐86. [DOI] [PubMed] [Google Scholar]
- Walley JD, Khan MA, Newell JN, Khan MH. Effectiveness of direct observation component of DOTS for tuberculosis: a randomised controlled trial in Pakistan. Lancet 2001;357(9275):664‐9. [DOI] [PubMed] [Google Scholar]
Wandwalo 2004 TZA {published data only}
- Wandwalo E, Kapalata N, Egwaga S, Morkve O. Effectiveness of community‐based directly observed treatment for tuberculosis in an urban setting in Tanzania: a randomised controlled trial. International Journal of Tuberculosis and Lung Disease 2004;8(10):1248‐54. [PubMed] [Google Scholar]
Wright 2004 SWZ {published data only}
- Wright J, Walley J, Phillip A, Pushpananthan S, Dlamini E, Newell J, et al. Direct observation of treatment for tuberculosis: a randomized controlled trial of community health workers versus family members. Tropical Medicine and International Health 2004;9(5):559‐65. [DOI] [PubMed] [Google Scholar]
Zwarenstein 1998 ZAF {published data only}
- Zwarenstein M, Schoeman JH, Vundule C, Lombard CJ, Tatley M. Randomised controlled trial of self‐supervised and directly observed treatment of tuberculosis. Lancet 1998;352(9137):1340‐3. [DOI] [PubMed] [Google Scholar]
Zwarenstein 2000 ZAF {published data only}
- Zwarenstein M, Schoeman JH, Vundule C, Lombard CJ, Tatley M. A randomised trial of lay health workers as direct observers for treatment of tuberculosis. International Journal of Tuberculosis and Lung Disease 2000;4(6):550‐4. [PubMed] [Google Scholar]
References to studies excluded from this review
Batki 2002 {published data only}
- Batki SL, Gruber VA, Bradley JM, Bradley M, Delucchi K. A controlled trial of methadone treatment combined with directly observed isoniazid for tuberculosis prevention in injection drug users. Drug and Alcohol Dependence 2002;66(3):283‐93. [DOI] [PubMed] [Google Scholar]
Carroll 2004 {published data only}
- Carroll K, Malefoasi G. Comparison of outcomes from a district tuberculosis control programme in the Pacific: before and after the implementation of DOTS. Tropical Doctor 2004;34(1):11‐4. [DOI] [PubMed] [Google Scholar]
Hwang 2004 {published data only}
- Hwang TG, Kim SD, Yoo SH, Shin YC. Sputum smear conversion during mDOT. Tuberculosis and Respiratory Diseases 2004;56(5):485‐94. [Google Scholar]
Jasmer 2004 {published data only}
- Jasmer RM, Seaman CB, Gonzalez LC, Kawamura LM, Osmond DH, Daley CL. Tuberculosis treatment outcomes: directly observed therapy compared with self‐administered therapy. American Journal of Respiratory and Critical Care Medicine 2004;170(5):561‐6. [DOI] [PubMed] [Google Scholar]
Lewin 2004 {published data only}
- Lewin S, Dick J, Zwarenstein M, Lombard CJ. Staff training and ambulatory tuberculosis outcomes: a cluster randomized controlled trial in South Africa. Bulletin of the World Health Organization 2005;83(4):250‐9. [PMC free article] [PubMed] [Google Scholar]
Malotte 2001 {published data only}
- Malotte CK, Hollingshead JR, Larro M. Incentives vs outreach workers for latent tuberculosis treatment in drug users. American Journal of Preventive Medicine 2001;20(2):103‐7. [DOI] [PubMed] [Google Scholar]
Matthew 2002 {published data only}
- Matthew AJ, Eicher A, Davies PD. Comparison of hospital checked directly observed therapy with family supervised and unchecked tuberculosis treatment in a rural setting in North India. European Respiratory Journal 2002;20(Suppl 38):215. [Google Scholar]
Moulding 2002 {published data only}
- Moulding TS, Caymittes M. Managing medication compliance of tuberculosis patients in Haiti with medication monitors. International Journal of Tuberculosis and Lung Disease 2002;6(4):313‐9. [PubMed] [Google Scholar]
Pungrassami 2002a {published data only}
- Pungrassami P, Johnsen SP, Chongsuvivatwong V, Olsen J. Has directly observed treatment improved outcomes for patients with tuberculosis in southern Thailand?. Tropical Medicine and International Health 2002;7(3):271‐9. [DOI] [PubMed] [Google Scholar]
Pungrassami 2002b {published data only}
- Pungrassami P, Chongsuvivatwong V. Are health personnel the best choice for directly observed treatment in southern Thailand? A comparison of treatment outcomes among different types of observers. Transactions of the Royal Society of Tropical Medicine and Hygiene 2002;96(6):695‐9. [DOI] [PubMed] [Google Scholar]
Sorete‐Abore 2002 {published data only}
- Sorete‐Arbore A, Mihaescu T. Three years of DOTS strategy in Iasi county, Romania. European Respiratory Journal 2002;20(Suppl 38):217. [Google Scholar]
Tandon 2002 {published data only}
- Tandon M, Gupta M, Tandon S, Gupta KB. DOTS versus self administered therapy (SAT) for patients with pulmonary tuberculosis: a randomised trial at a tertiary care hospital. Indian Journal of Medical Science 2002;56(1):19‐21. [PubMed] [Google Scholar]
Thiam 2007 {published data only}
- Thiam S, LeFevre AM, Hane F, Ndiaye A, Ba F, Fielding KL, et al. Effectiveness of a strategy to improve adherence to tuberculosis treatment in a resource‐poor setting: a cluster randomized controlled trial. JAMA 2007;297(4):380‐6. [DOI] [PubMed] [Google Scholar]
Toyota 2003 {published data only}
- Toyota E, Kobayashi N, Houjou M, Yoshizawa A, Kawana A, Kudo K. Usefulness of directly observed therapy (DOT) during hospitalization as DOTS in Japanese style. Kekkaku 2003;78(9):581‐5. [PubMed] [Google Scholar]
Additional references
Anuwatnonthakate 2008
- Anuwatnonthakate A, Limsomboon P, Nateniyom S, Wattanaamornkiat W, Komsakorn S, Moolphate S, et al. Directly observed therapy and improved tuberculosis treatment outcomes in Thailand. PLoS One 2008;3(8):e3089. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barbara 2013
- Seaworth BJ, Armitige LY, Griffith DE. First do no harm—adverse events, drug intolerance, and hepatotoxicity: how can we not justify directly observed therapy for treating tuberculosis?. Clinical Infectious Diseases 2013;57(7):1063‐4. [DOI] [PubMed] [Google Scholar]
Bayer 1995
- Bayer R, Wilkinson D. Directly observed therapy for tuberculosis: history of an idea. Lancet 1995;345(8964):1545‐8. [DOI] [PubMed] [Google Scholar]
Bosch‐Capblanch 2007
- Bosch‐Capblanch X, Abba K, Prictor M, Garner P. Contracts between patients and healthcare practitioners for improving patients' adherence to treatment, prevention and health promotion activities. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD004808.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chan 2002
- Chan ED, Iseman MD. Current medical treatment for tuberculosis. BMJ 2002;325(7375):1282‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaulk 1998
- Chaulk CP, Kazandjian VA. Directly observed therapy for treatment completion of pulmonary tuberculosis: Consensus Statement of the Public Health Tuberculosis Guidelines Panel. JAMA 1998;279(12):943‐8. [DOI] [PubMed] [Google Scholar]
Chien 2013
- Chien JY, Lai CC, Tan CK, Chien ST, Yu CJ, Hsueh PR. Decline in rates of acquired multidrug‐resistant tuberculosis after implementation of the directly observed therapy, short course (DOTS) and DOTS‐Plus programmes in Taiwan. Journal of Antimicrobial Chemotherapy 2013;68(8):1910–6. [DOI] [PubMed] [Google Scholar]
Dick 2005
- Dick J, Murray E, Botha E. Operations Research Results. The effectiveness of TB DOTS supporters in South Africa. April 2005. https://www.usaidassist.org/sites/assist/files/pnadf972.pdf (accessed 23 January 2014).
Ford 2009
- Ford N, Nachega JB, Engel ME, Mills EJ. Directly observed antiretroviral therapy: a systematic review and meta‐analysis of randomised clinical trials. Lancet 2009;374(9707):2064‐71. [DOI] [PubMed] [Google Scholar]
Frieden 2003
- Frieden TR, Sterling TR, Munsiff SS, Watt CJ, Dye C. Tuberculosis. Lancet 2003;362(9387):887‐99. [DOI] [PubMed] [Google Scholar]
Frieden 2007
- Frieden TR, Sbarbaro JA. Promoting adherence to treatment for tuberculosis: the importance of direct observation. Bulletin of the World Health Organization 2007;85(5):407‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gross 2009
- Gross R, Tierney C, Andrade A, Lalama C, Rosenkranz S, Eshleman SH, et al. Modified directly observed antiretroviral therapy compared with self‐administered therapy in treatment‐naïve HIV‐1–infected patients: a randomized trial. Archives of Internal Medicine 2009;169(13):1224‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins J, Green S (editors). Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org (accessed 20 August 2013).
Hirpa 2013
- Hirpa S, Medhin G, Girma B, Melese M, Mekonen A, Suarez P, et al. Determinants of multidrug‐resistant tuberculosis in patients who underwent first‐line treatment inAddis Ababa: a case control study. BMC Public Health 2013;13:782. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hopewell 2006
- Hopewell PC, Pai M, Maher D, Uplekar M, Raviglione MC. International Standards for Tuberculosis Care. Lancet Infectious Diseases 2006;6(11):710‐25. [DOI] [PubMed] [Google Scholar]
Jüni 2001
- Jüni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ 2001;323(7303):42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khan 2003
- Khan MA, Walley JD, Witter SN, Imran A, Safdar N. Cost and cost effectiveness of different DOT strategies for the treatment of tuberculosis in Pakistan. Directly observed treatment. Health Policy and Planning 2003;17(2):178‐86. [DOI] [PubMed] [Google Scholar]
Liu 2008
- Liu Q, Abba K, Alejandria MM, Balanag VM, Berba RP, Lansang MAD. Reminder systems and late patient tracers in the diagnosis and management of tuberculosis (Review). Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD006594.pub2] [DOI] [PubMed] [Google Scholar]
Lutge 2012
- Lutge EE, Wiysonge CS, Knight SE, Volmink J. Material incentives and enablers in the management of tuberculosis. Cochrane Database of Systematic Reviews 2012, Issue 1. [DOI: 10.1002/14651858.CD007952.pub2] [DOI] [PubMed] [Google Scholar]
M'Imunya 2012
- M'Imunya JM, Kredo T, Volmink J. Patient education and counselling for promoting adherence to treatment for tuberculosis. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD006591.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Macq 2003
- Macq JC, Theobald S, Dick J, Dembele M. An exploration of the concept of directly observed treatment (DOT) for tuberculosis patients: from a uniform to a customised approach. International Journal of Tuberculosis and Lung Disease 2003;7(2):103‐9. [PubMed] [Google Scholar]
Mohan 2007
- Mohan CI, Bishai D, Cavalcante S, Chaisson RE. The cost‐effectiveness of DOTS in urban Brazil. International Journal of Tuberculosis and Lung Disease 2007;11(1):27‐32. [PubMed] [Google Scholar]
Moonan 2011
- Moonan PK, Quitugua TN, Pogoda JM, Woo G, Drewyer G, Sahbazian B, et al. Does directly observed therapy (DOT) reduce drug resistant tuberculosis?. BMC Public Health 2011;11:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Munro 2007
- Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Medicine 2007;4(7):e238. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pasipanodya 2013
- Pasipanodya JG, Gumbo T. A meta‐analysis of self‐administered vs directly observed therapy effect on microbiologic failure, relapse, and acquired drug resistance in tuberculosis patients. Clinical Infectious Diseases 2013;57(1):21‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 5 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Sepkowitz 1995
- Sepkowitz KA, Raffalli J, Riley L, Kiehn TE, Armstrong D. Tuberculosis in the AIDS era. Clinical Microbiology Reviews 1995;8(2):180‐99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smieja 2010
- Smieja M, Marchetti C, Cook D, Smaill FM. Isoniazid for preventing tuberculosis in non‐HIV infected persons. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD001363] [DOI] [PMC free article] [PubMed] [Google Scholar]
Steffen 2010
- Steffen R, Menzies D, Oxlade O, Pinto M, Castro AZ, Monteiro P, et al. Patients' costs and cost‐effectiveness of tuberculosis treatment in DOTS and non‐DOTS facilities in Rio de Janeiro, Brazil. PLoS One 2010;5(11):e14014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tian 2014
- Tian JH, Lu ZX, Bachmann MO, Song FJ. Effectiveness of directly observed treatment of tuberculosis: a systematic review of controlled studies. International Journal Tuberculosis and Lung Disease 2014 September;18(9):1092‐8. [DOI: 10.5588/ijtld.13.0867.] [DOI] [PubMed] [Google Scholar]
van den Boogaard 2012
- Boogaard J, Msoka E, Homfray M, Kibiki GS, Heldens JJ, Felling AJ, et al. An exploration of patients perceptions of adherence to tuberculosis treatment in Tanzania. Qualitative Health Research 2012;22(6):835‐45. [DOI] [PubMed] [Google Scholar]
Volmink 2000b
- Volmink J, Matchaba P, Garner P. Directly observed therapy and treatment adherence. Lancet 2000;355(9212):1345‐50. [DOI] [PubMed] [Google Scholar]
WHO 2002
- WHO Global Tuberculosis Programme. An Expanded DOTS Framework for Effective Tuberculosis Control. Stop TB Communicable Diseases. Geneva: World Health Organization, 2002. [Google Scholar]
WHO 2010
- World Health Organization. Treatment of tuberculosis guidelines: Fourth edition. 2010. http://apps.who.int/iris/bitstream/10665/44165/1/9789241547833_eng.pdf?ua=1&ua=1 (accessed 01 August 2014).
WHO 2013
- WHO Global TB Programme. Global Tuberculosis Report 2013. http://apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf (accessed 01 August 2014).
References to other published versions of this review
Volmink 1997
- Volmink J, Garner P. Systematic review of randomised controlled trials of strategies to promote adherence to tuberculosis treatment. BMJ 1997;315(7120):1403‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Volmink 2000a
- Volmink J, Garner P. Interventions for promoting adherence to tuberculosis management. Cochrane Database of Systematic Reviews 2000, Issue 4. [DOI: 10.1002/14651858.CD000010] [DOI] [PubMed] [Google Scholar]
Volmink 2001
- Volmink J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database of Systematic Reviews 2001, Issue 4. [DOI: 10.1002/14651858.CD003343] [DOI] [PubMed] [Google Scholar]
Volmink 2003
- Volmink J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD003343] [DOI] [PubMed] [Google Scholar]
Volmink 2006
- Volmink J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD003343.pub2] [DOI] [PubMed] [Google Scholar]
Volmink 2007
- Volmink J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD003343.pub3] [DOI] [PubMed] [Google Scholar]


