Abstract
IMPORTANCE
Despite the potential importance of understanding excess mortality among people with mental disorders, no comprehensive meta-analyses have been conducted quantifying mortality across mental disorders.
OBJECTIVE
To conduct a systematic review and meta-analysis of mortality among people with mental disorders and examine differences in mortality risks by type of death, diagnosis, and study characteristics.
DATA SOURCES
We searched EMBASE, MEDLINE, PsychINFO, and Web of Science from inception through May 7, 2014, including references of eligible articles. Our search strategy included terms for mental disorders (eg, mental disorders, serious mental illness, and severe mental illness), specific diagnoses (eg, schizophrenia, depression, anxiety, and bipolar disorder), and mortality. We also used Google Scholar to identify articles that cited eligible articles.
STUDY SELECTION
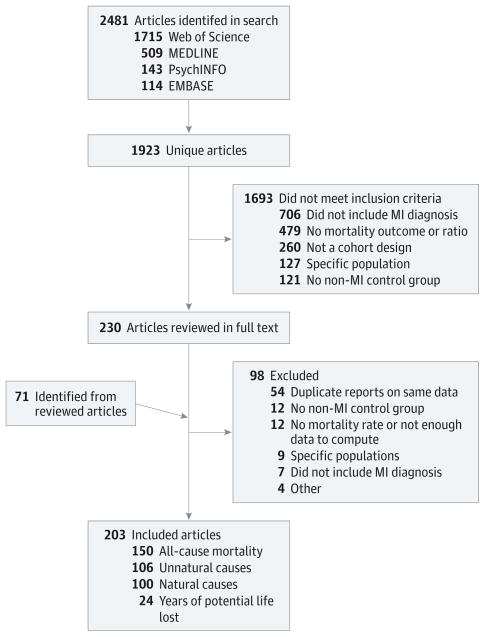
English-language cohort studies that reported a mortality estimate of mental disorders compared with a general population or controls from the same study setting without mental illness were included. Two reviewers independently reviewed the titles, abstracts, and articles. Of 2481 studies identified, 203 articles met the eligibility criteria and represented 29 countries in 6 continents.
DATA EXTRACTION AND SYNTHESIS
One reviewer conducted a full abstraction of all data, and 2 reviewers verified accuracy.
MAIN OUTCOMES AND MEASURES
Mortality estimates (eg, standardized mortality ratios, relative risks, hazard ratios, odds ratios, and years of potential life lost) comparing people with mental disorders and the general population or people without mental disorders. We used random-effects meta-analysis models to pool mortality ratios for all, natural, and unnatural causes of death. We also examined years of potential life lost and estimated the population attributable risk of mortality due to mental disorders.
RESULTS
For all-cause mortality, the pooled relative risk of mortality among those with mental disorders (from 148 studies) was 2.22 (95% CI, 2.12–2.33). Of these, 135 studies revealed that mortality was significantly higher among people with mental disorders than among the comparison population. A total of 67.3% of deaths among people with mental disorders were due to natural causes, 17.5% to unnatural causes, and the remainder to other or unknown causes. The median years of potential life lost was 10 years (n = 24 studies). We estimate that 14.3% of deaths worldwide, or approximately 8 million deaths each year, are attributable to mental disorders.
CONCLUSIONS AND RELEVANCE
These estimates suggest that mental disorders rank among the most substantial causes of death worldwide. Efforts to quantify and address the global burden of illness need to better consider the role of mental disorders in preventable mortality.
Researchers have consistently reported that people with mental disorders have elevated mortality compared with the general population. In 1937, Malzberg1 reported that psychiatric inpatients had a mortality rate that was 6 times greater than the rate in the general population of New York. Since then, numerous studies and reviews have been conducted on the mortality risks of people with a variety of mental disorders2–6 and specific diagnoses (eg, schizophrenia,7 depression,8,9 and bipolar disorder10).
The studies11,12 on the global burden of disease illustrate the growing burden of mental disorders, although this burden has largely been reflected in disability rather than mortality. The link between mental disorders and mortality is complicated because most people with mental disorders do not die of their condition; rather, they die of heart disease and other chronic diseases, infections, suicide, and other causes.11,12 Another complicating factor is that mental disorders are associated with risk factors for mortality. People with mental disorders have high rates of adverse health behaviors, including tobacco smoking, substance use, physical inactivity, and poor diet. In turn, these behaviors contribute to the high rates of chronic medical conditions among people with mental disorders.13,14
Quantifying and understanding the excess mortality among people with mental disorders can inform approaches for addressing this persistent issue and widen discussion of the effect of mental disorders on mortality. The purpose of this study was to systematically review the literature to examine the excess mortality rate of people with mental disorders, extending existing reviews of individual disorders. We sought to provide comprehensive estimates of individual- and population-level mortality rates related to mental disorders.
Methods
Data Sources and Searches
We followed the Meta-analysis of Observational Studies in Epidemiological guidelines for this meta-analysis.15 We searched EMBASE, MEDLINE, PsychINFO, and Web of Science from inception through May 7, 2014. Searching was conducted by the investigators after consulting with a librarian about the search strategy. Our search strategy included terms for mental disorders (eg, mental disorders, serious mental illness, and severe mental illness), specific diagnoses (eg, schizophrenia, depression, anxiety, and bipolar disorder), and mortality. We also limited the search or included terms to identify English-language cohort (eg, cohort or follow-up) studies depending on the database (eTable 1 in the Supplement includes the full search strings). We also searched references of eligible articles and used Google Scholar to identify articles that cited eligible articles.
Study Selection
Studies were included if they (1) were original research papers that used a cohort study design; (2) included diagnosed mental disorders (eg, not symptoms); (3) reported mortality as an outcome by comparing people with mental disorders with a general population or controls from the same study setting without mental illness; and (4) were written in the English language. Studies were excluded if the study population was restricted to people with specific medical conditions (eg, heart disease) or subgroups of the population (eg, homeless) or the study reported duplicate data. Titles, abstracts, and articles were reviewed by 2 independent reviewers (E.R.W. and R.E.M.), and disagreements were settled by consensus.
Data Extraction
From all eligible articles, we abstracted the first author’s name, year of publication, country, setting, year of baseline, years of follow-up, sample source, sample size, mental disorders included, population of people with mental disorders (eg, inpatient, outpatient, and community), method of diagnosing mental disorders, diagnostic system, control or comparison group, and assessment of mortality. We also abstracted the observed number of deaths and/or rate of death among people with mental disorders (when possible, we did not include substance use or dementia), expected number of deaths and/or rate of death among people with mental disorders, risk of mortality (eg, standardized mortality ratio [SMR], relative risk [RR], odds ratio, hazard ratio, and years of potential life lost [YPLL]), and adjustment variables. All-cause mortality and mortality due to natural causes (eg, acute and chronic illnesses) and unnatural causes (eg, suicide and unintentional injury) were abstracted separately. One reviewer conducted a full abstraction of all data, and 2 reviewers (E.R.W. and R.E.M.) verified accuracy. We addressed study quality in 2 ways: by incorporating quality components, such as study design, into the study selection criteria and by including quality criteria as independent variables in the meta-regression. The authors of 7 studies were contacted for information that was not included in their articles. Two emails were undeliverable. Of the remaining 5 researchers, 4 were able to provide information about numbers of deaths or YPLL.
Statistical Analysis
We compared information on study time frame, data source, and geographic location to identify potential sample overlap. In the case of overlap, we chose the article with the longest follow-up period. As a result, 54 of the studies were excluded from our analyses. An estimate from one study16 was excluded from the overall all-cause analyses because of overlap with another study,17 but it was included in the diagnosis-specific analyses. We included the following measures of risk: SMR, RR, odds ratio, and hazard ratio.18,19 We aimed to use comparably adjusted estimates across the different ratio types. The SMRs are typically adjusted for age and sex; therefore, if several estimates were reported, we chose the most basic adjusted model. For articles that reported multiple estimates by subgroup, we combined the ratios using the methods described by van Dooren and colleagues20 to derive one estimate per study for each analysis. For studies that reported multiple estimates by mental disorder diagnoses whose diagnoses were not mutually exclusive, we chose the estimate of the largest diagnostic group. For one study,21 2 ratios were included in the analyses because the researchers examined mortality in 2 nonoverlapping populations. One study22 was excluded from the analyses because the SMR was an outlier.
For the meta-analysis, mortality ratios were pooled using DerSimonian-Laird random-effects models to allow for heterogeneity across studies.23,24 Heterogeneity was assessed with the Cochran Q and theI2 tests.25,26 We ran random-effects meta-regression models to determine which study characteristics could explain heterogeneity.26,27 We first ran each variable in a separate model and then ran a model with all the variables together. We also conducted sensitivity analyses by study quality criteria and significant variables in the meta-regression. Potential bias was examined using the funnel plot and Egger test.28,29 We conducted all meta-analytic analyses on the natural log scale using STATA statistical software, version 12.1 (Stata Corp).
For YPLL analyses, when studies reported estimates by subgroups, we calculated a mean. When numbers of deaths by subgroup were available, we calculated weighted estimates of YPLL for people with mental disorders. Median and range of YPLL by mortality due to all causes, natural causes, and unnatural causes were determined.
We identified studies that included a measure of population attributable risk (PAR). We also calculated the number and percentage of deaths worldwide associated with mental disorders based on the pooled RRs and global prevalence of mental disorders. For the percentage of deaths attributable to mental disorders, we used the PAR formula b[(r − 1)/r], where b is the worldwide prevalence of mental disorders and r is the pooled RR.30 For the prevalence of all mental disorders and specific diagnoses, we used estimates from the World Health Organization World Mental Health Surveys.31,32 We calculated the approximate number of deaths attributable to mental disorders by multiplying the PAR by the number of deaths worldwide in 2012.33 The PAR and number of deaths were estimated for all-cause mortality and for all mental disorders and specific diagnoses (eg, mood disorders, anxiety disorders, and psychoses).
Results
We identified 2481 articles through the literature search (Figure). Of the 1923 unique articles, the full text of 230 articles was reviewed, along with an additional 71 articles identified through hand searching and Google Scholar. Most excluded studies did not include a sample of people with a diagnosed mental disorder or did not report mortality ratios of people with mental disorders compared with an appropriate comparison group. Fifty-four studies were excluded because they included data that overlapped with other studies. A total of 203 studies met the criteria for this systematic review and were included in the meta-analysis.
Figure. Flowchart of Study Selection.
MI indicates myocardial infarction.
The 203 studies were heterogeneous in terms of sample source, type of sample included, and comparison group. Overall descriptive data of the included studies are presented in Table 1, and descriptive information for each study is included in eTable 2 in the Supplement. The articles represented 29 countries on 6 continents. Most studies were conducted in Europe (n = 125), primarily Sweden (n = 30) and the United Kingdom (n = 18). The remaining studies were conducted in North America (United States [n = 42] and Canada [n = 9]), Asia (n = 16), Australia (n = 8), Africa (n = 2), and South America (n = 1). Included studies mainly used linked registers (42.9%) to identify samples, although community-or population-based samples were used in 21.2% of studies. Most studies included samples of inpatients (37.4%) or inpatients and outpatients (26.1%). For most studies (66.5%), mental disorder diagnoses were identified from medical records, registers, or administrative data; diagnostic interviews were conducted in 24.6% of studies. Follow-up time ranged from 1 to 52 years, with a median of 10 years. The studies used in the following analyses are cited in eTable 3 in the Supplement.
Table 1.
Summary of Characteristics of the 203 Eligible Studies
| Characteristic | No. (%) of Studies | |||
|---|---|---|---|---|
| All Studies (N = 203) | Causes | |||
| All (n = 150) | Natural (n = 100) | Unnatural (n = 106) | ||
| Source of sample | ||||
| National or community survey | 43 (21.2) | 32 (21.3) | 11 (11.0) | 10 (9.4) |
| Case or linked register | 87 (42.9) | 60 (40.0) | 57 (57.0) | 60 (56.6) |
| Insurance or health service system database | 19 (9.4) | 12 (8.0) | 6 (6.0) | 6 (5.7) |
| Hospital or clinic sample | 21 (10.3) | 16 (10.7) | 5 (5.0) | 8 (7.5) |
| Hospital or clinic records | 26 (12.8) | 24 (16.0) | 16 (16.0) | 18 (17.0) |
| Other | 7 (3.4) | 6 (4.0) | 5 (5.0) | 4 (3.8) |
| Years of follow-up | ||||
| ≤10 | 104 (51.2) | 79 (52.7) | 40 (40.0) | 51 (48.1) |
| >10 | 99 (48.8) | 71 (47.3) | 60 (60.0) | 55 (51.9) |
| Population of people with mental disorders | ||||
| Inpatient | 76 (37.4) | 60 (40.0) | 46 (46.0) | 50 (47.2) |
| Outpatient | 5 (2.5) | 3 (2.0) | 3 (3.0) | 4 (3.8) |
| Inpatient and outpatient | 53 (26.1) | 35 (23.3) | 26 (26.0) | 31 (29.2) |
| Community | 34 (16.7) | 29 (19.3) | 9 (9.0) | 8 (7.5) |
| Public sector | 8 (3.9) | 5 (3.3) | 4 (4.0) | 4 (3.8) |
| Other | 26 (12.8) | 17 (11.3) | 12 (12.0) | 9 (8.5) |
| Not specified | 1 (0.5) | 1 (0.7) | 0 (0.0) | 0 (0.0) |
| Method used to assess mental disorders | ||||
| Diagnostic interview | 50 (24.6) | 42 (28.0) | 14 (14.0) | 13 (12.3) |
| Diagnosis in medical record, register, or administrative data | 135 (66.5) | 93 (62.0) | 81 (81.0) | 87 (82.1) |
| Received services | 4 (2.0) | 3 (2.0) | 1 (1.0) | 2 (1.9) |
| Self-report | 3 (1.5) | 3 (2.0) | 0 (0.0) | 1 (0.9) |
| Other | 11 (5.4) | 9 (6.0) | 4 (4.0) | 3 (2.8) |
| Diagnostic system | ||||
| Any diagnostic system (eg, ICD or DSM) | 159 (78.3) | 119 (79.3) | 76 (76.0) | 80 (75.5) |
| Own system | 12 (5.9) | 7 (4.7) | 6 (6.0) | 6 (5.7) |
| No system or not specified | 32 (15.8) | 24 (16.0) | 18 (18.0) | 20 (18.9) |
| Comparison group | ||||
| General population, country | 73 (36.0) | 55 (36.7) | 40 (40.0) | 46 (43.4) |
| General population, other (eg, state, county) | 56 (27.6) | 42 (28.0) | 32 (32.0) | 33 (31.1) |
| Individuals with no mental disorders | 62 (30.5) | 41 (27.3) | 22 (22.0) | 22 (20.8) |
| Individuals with no psychiatric services use | 3 (1.5) | 3 (2.0) | 3 (3.0) | 2 (1.9) |
| Other | 6 (3.0) | 6 (4.0) | 2 (2.0) | 3 (2.8) |
| Not specified | 3 (1.5) | 3 (2.0) | 1 (1.0) | 0 (0.0) |
| Assessment of mortality | ||||
| Death register or death certificates | 169 (83.3) | 120 (80.0) | 89 (89.0) | 93 (87.7) |
| Medical or administrative records | 5 (2.5) | 5 (3.3) | 2 (2.0) | 2 (1.9) |
| Interviews (eg, family) | 7 (3.4) | 7 (4.7) | 0 (0.0) | 0 (0.0) |
| Multiple sources | 11 (5.4) | 10 (6.7) | 6 (6.0) | 7 (6.6) |
| Other | 3 (1.5) | 1 (0.7) | 1 (1.0) | 3 (2.8) |
| Not specified | 8 (3.9) | 7 (4.7) | 2 (2.0) | 1 (0.9) |
Abbreviations: DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD, International Classification of Diseases.
Mortality
For all-cause mortality, 148 studies provided 149 RRs on the mortality of people with mental disorders (Table 2). Of these studies, 135 revealed that mortality among people with mental disorders was significantly higher than the comparison population. Fourteen studies (9.4%) reported no significant difference in mortality risks between the 2 groups, and no studies reported lower mortality risks for people with mental disorders. No patterns were identifiable among these 14 studies that distinguished them from the rest of the studies.
Table 2.
Meta-analysis of Mental Disorders and Mortality
| Study Population | No. of Studies/No. of RRs | RR (95% CI)a | I2 Statistic, % |
|---|---|---|---|
| All-cause mortality | 148/149 | 2.22 (2.12–2.33) | 99.6 |
| Population of people with mental disorders | |||
| Inpatient | 60/61 | 2.42 (2.24–2.61) | 99.6 |
| Outpatient or inpatient and outpatient | 38/38 | 2.08 (1.91–2.27) | 99.6 |
| Community | 28/28 | 1.90 (1.61–2.25) | 94.6 |
| First year of baseline | |||
| Before 1970 | 26/26 | 1.79 (1.49–2.15) | 99.4 |
| 1970–1979 | 23/23 | 2.07 (1.86–2.31) | 99.4 |
| 1980–1989 | 28/28 | 2.28 (2.07–2.50) | 99.3 |
| 1990–1999 | 50/50 | 2.43 (2.24–2.63) | 99.6 |
| 2000 and later | 19/19 | 2.47 (2.17–2.79) | 99.2 |
| Method used to assess mental disorder | |||
| Diagnostic interview | 42/42 | 1.88 (1.69–2.11) | 92.2 |
| Diagnosis in records | 90/91 | 2.36 (2.23–2.51) | 99.8 |
| Years of follow-up | |||
| ≤10 | 78/78 | 2.43 (2.25–2.64) | 99.5 |
| >10 | 70/71 | 2.03 (1.89–2.18) | 99.7 |
| All-cause mortality by specific diagnosis | |||
| Psychoses | 65/66 | 2.54 (2.35–2.75) | 99.0 |
| Mood disordersb | 16/16 | 2.08 (1.89–2.30) | 97.3 |
| Depressionb | 43/43 | 1.71 (1.54–1.90) | 99.4 |
| Bipolar disorderb | 19/19 | 2.00 (1.70–2.34) | 99.1 |
| Anxiety | 29/29 | 1.43 (1.24–1.64) | 98.8 |
| Cause-specific mortality | |||
| Natural | 100/100 | 1.80 (1.71–1.88) | 99.3 |
| Unnatural | 106/106 | 7.22 (6.43–8.12) | 99.5 |
Abbreviation: RR, relative risk.
The Cochran Q tests indicated a high level of heterogeneity, with P < .001 for all studies.
These 3 groups are mutually exclusive.
The total number of deaths, reported in 133 studies, was 338 381. The overall pooled RR for mortality among people with mental disorders was 2.22 (95% CI, 2.12–2.33). eFigure 1 in the Supplement displays the forest plot of estimates of all-cause mortality. The Cochran Q and I2 tests indicated a high level of heterogeneity across studies (P < .001). No significant bias was observed based on the funnel plot and Egger test (P = .23) (eFigure 2 in the Supplement). For specific diagnoses, all-cause mortality was significantly elevated for psychoses, mood disorders, and anxiety (Table 2). The mortality risk for psychoses was significantly higher than those for depression (P < .001), bipolar disorder (P = .01), and anxiety (P < .001).
Results from the meta-regression models with each variable entered separately provided evidence of differential mortality risks by population of people with mental disorders, method of identifying mental disorders, decade of first year of baseline, and length of follow-up. No differences were found in mortality risk based on sample source, diagnostic system, or geographic location (Asia, Europe, North America, and Africa, Australia, and South America grouped together). In the full meta-regression model, populations of people with mental disorders, length of follow-up, and first year of baseline remained significant. Compared with studies that included inpatients, studies that included outpatients (P = .03) and studies that included community- or population-based samples (P = .04) were associated with smaller effects. Studies with a follow-up of more than 10 years were associated with lower mortality risks compared with studies with shorter follow-up lengths (P = .02). Studies with a first year of baseline during the 1990s were associated with stronger effects compared with studies with a first year of baseline before 1970 (P = .009). Table 2 lists the pooled RRs from the stratified analyses for each of these variables separately.
The analysis of natural causes of death included 100 studies and resulted in a pooled RR of 1.80 (95% CI, 1.71–1.88). For unnatural causes, the pooled RR from 106 studies was 7.22 (95% CI, 6.43–8.12). Across the 86 studies that reported number of deaths, 213 773 deaths occurred from natural causes. A total of 46 051 deaths occurred from unnatural causes across the 91 studies that reported number of deaths by unnatural causes. Fifty-seven studies reported the number of deaths for all, natural, and unnatural causes. From these studies, we estimate that 67.3% of deaths were due to natural causes and 17.5% were due to unnatural causes, with the remainder being unknown or unidentified.
Years of Potential Life Lost
Twenty-four studies included estimates of life expectancy or YPLL for people with mental disorders (eTable 4 in the Supplement). Results from all these studies indicated that people with mental disorders had more YPLL compared with people in the general population. For all-cause mortality, the reduction in life expectancy ranged from 1.4 to 32 years, with a median of 10.1 years (n = 22 studies). The YPLL ranged from 3 to 26.3 years for natural causes (n = 8 studies; median, 9.6 years) and 8.4 to 41.2 years for unnatural causes (n = 4 studies; median, 21.6 years).
Population Attributable Risk
Four studies34–37 in the systematic review included a PAR estimate. For all-cause deaths, the PAR was estimated at 1.3% for schizophrenia34 and 12.7% for depression.37 Among suicides, reported PAR estimates were 8.9% for schizophrenia,34 11.2% for depression,35 4.8% for manic-depressive disorders,35 and 7.7% for severe mental illness.36
The overall PAR estimate and number of deaths by diagnosis based on the meta-analysis results are given in Table 3. According to the World Health Organization World Mental Health Surveys, the median lifetime prevalence of any mental disorder across 17 countries is 26.1%. On the basis of this prevalence and the pooled RR from the meta-analysis, approximately 8 million deaths worldwide are attributable to mental disorders each year. Mood disorders and anxiety disorders have similar PARs, which are much higher than the PARs for psychoses.
Table 3.
All-Cause Deaths Attributable to Mental Disorders by Diagnosis
| Cause | Pooled RR (95% CI) | Prevalence, % | PAR, % | No. of Deaths Attributable to Mental Disorders, in Millionsa |
|---|---|---|---|---|
| Disorders | ||||
| All mental | 2.22 (2.12–2.33) | 26.1b | 14.34 | 8.00 |
| Mood | 1.86 (1.73–2.00) | 10.6b | 4.90 | 2.74 |
| Anxiety | 1.43 (1.24–1.64) | 14.3b | 4.30 | 2.41 |
| Psychoses | 2.54 (2.35–2.75) | 1.04c | 0.63 | 0.35 |
Abbreviations: PAR, population attributable risk; RR, relative risk.
On the basis of the World Health Organization estimate of 56 deaths worldwide in 2012.33
Median lifetime prevalence of estimates from the World Health Organization World Mental Health Surveys in 17 countries.31
Prevalence of self-reported lifetime diagnosis from the World Health Organization World Mental Health Surveys in 52 countries.32
Discussion
We conducted a meta-analysis to examine mortality among people with mental disorders across a range of diagnoses. People with mental disorders have a mortality rate that is 2.22 times higher than the general population or people without mental disorders, with a decade of YPLL. Our results align with other reviews, including a meta-review by Chesney and colleagues6 and a meta-analysis of depression by Cuijpers and Smit.8 In contrast to earlier work, our study provides individual- and population-based estimates of mortality due to mental disorders. The PAR due to mental disorders is estimated at 14.3%, which indicates that annually 8 million deaths worldwide can be attributable to mental disorders.
This is the most comprehensive meta-analysis of mortality related to mental disorders of which we are aware. Results included 203 studies that were conducted in 29 countries. A wide range of samples, diagnoses, and populations of people with mental disorders were examined, which contributed to the substantial heterogeneity across studies. The full meta-regression model included several factors that shed light on variability across study characteristics and subpopulations.
Length of follow-up was associated with differential risks of mortality; studies with longer follow-up tended to report lower mortality ratios compared with studies with a follow-up of 10 or fewer years. One explanation may be that people with mental illness die earlier and that, during a long follow-up, the background rate of mortality among people without mental illness starts to catch up with people with mental illness as the whole sample ages. The other study characteristics—sample source, methods of assessing mental disorders, and diagnostic system—were not significantly associated with mortality. However, we also found differential mortality rates by setting and first year of baseline.
Inpatients had significantly higher mortality rates compared with samples with outpatients and with community-based samples. The elevated mortality in inpatients is not surprising because inpatients tend to have more advanced psychiatric and general medical conditions than outpatients.38 Although inpatient samples may be most useful when looking to target the population with the greatest mortality burden, community-based samples are essential for examining the overall burden of mental disorders. Examining both types of studies in conjunction can help provide these perspectives on the mortality burden associated with mental disorders.
Higher mortality rates were found among more recent studies (Table 2), particularly those with a first year of baseline in the 1990s compared with before 1970. These results extend the findings by Saha and colleagues,7 who found that the mortality gap between people with schizophrenia and the general population has been increasing over time. Our results indicate that the mortality gap may apply to people with a variety of mental disorders and not only schizophrenia. It appears that people with mental disorders are not experiencing the increased life expectancy of the general population.
Examining individual-level measures, such as RR, and population-based measures, such as YPLL and estimated PAR, provides important and distinct perspectives on the excess mortality associated with mental disorders. The PAR reveals the high global burden of mortality associated with mental disorders, thus pointing to the importance of addressing mental illness along with more proximal causes of death. For specific diagnoses, whereas pooled RRs of mortality due to psychoses are significantly higher compared with depression and anxiety, depression and anxiety contribute to more deaths overall compared with psychoses because of their high base prevalence. Successfully reducing the mortality burden of mental disorders will require attention to less common but more severe illnesses and more prevalent but milder conditions.
Similarly, although RRs for unnatural causes of death were higher compared with those of natural causes of death, natural causes accounted for more than two-thirds of deaths among people with mental disorders. These findings suggest that a variety of approaches are necessary to address different causes of death among people with mental disorders. Efforts to reduce unnatural causes of death, such as suicide, need to focus on high-risk populations with mental disorders. However, efforts to reduce the excess burden of mortality among people with mental disorders need to also address the problem of natural causes, including cardiovascular disease, particularly as populations age. Differential mortality in people with mental disorders most likely stems from a number of causes, including behavioral and lifestyle factors, access to and quality of health care, and social determinants of health, such as poverty and social connectedness.13,14
Milstein and colleagues39 laid out a 3-pronged strategy for reducing avoidable deaths in the general population that involves expanding access to care, providing better preventive and chronic care, and enabling healthier behaviors and safer environments. These approaches are also applicable for people with mental disorders. Prevention aimed at reducing mental disorders and chronic medical conditions is crucial.40 In addition, evidence-based strategies for suicide prevention for people with mental disorders include physician education for diagnosing mental disorders and provision of quality mental health treatment.41,42 Prevention and care of chronic medical conditions among people with mental disorders require promotion of healthy behaviors, early diagnosis and coordinated management, and integrated care between the mental health and medical systems. People with mental disorders often do not receive preventive services, such as immunizations, cancer screenings, and tobacco counseling,43 and often receive a lower quality of care for medical conditions.14,44
Our results must be considered in light of several limitations. First, we searched for published English-language studies; therefore, some studies may have been missed. However, given the number of studies included in our analysis, it is unlikely that the results would be substantially affected. Second, the broad range of included studies resulted in a large amount of heterogeneity that could not be fully explained by the variables we assessed. Third, we were unable to specifically examine excess mortality due to substance use disorders; future work should examine the excess mortality associated with primary or comorbid substance use conditions. Fourth, the PAR and number of deaths attributable to mental disorders are estimates based on the best epidemiologic studies available on global mental health. The use of lifetime prevalence of mental disorders in the PAR estimate may be susceptible to recall bias but provides a comprehensive estimate.
Conclusions
People with mental disorders experience a high burden of mortality at the individual and population levels. Reduction of this burden will require a focus on less prevalent but more severe diagnoses and more common mental disorders. Likewise, efforts must be made to prevent and manage comorbid medical conditions and reduce the occurrence of unnatural deaths in this vulnerable population.
Supplementary Material
Acknowledgments
Funding/Support: This study was supported by National Institutes of Health/National Institute of General Medical Sciences Institutional Research and Academic Career Development Award K12GM00680-05 (Dr Walker) and National Institute of Mental Health Award 5K24MH07586703 (Dr Druss).
Footnotes
Supplemental content at jamapsychiatry.com
Conflict of Interest Disclosures: None reported.
Author Contributions: Dr Walker had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Walker, Druss.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Walker, Druss.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Walker.
Obtained funding: Druss.
Administrative, technical, or material support: McGee.
Study supervision: Walker, Druss.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: Jennie Kwon, BS, assisted with data abstraction. Cathy Lally, MSPH, provided statistical support. Neither individual received compensation for her contributions.
References
- 1.Malzberg B. Mortality in involution meloncholia. Am J Psychiatry. 1937;93:1231–1238. [Google Scholar]
- 2.Eaton WW, Martins SS, Nestadt G, Bienvenu OJ, Clarke D, Alexandre P. The burden of mental disorders. Epidemiol Rev. 2008;30:1–14. doi: 10.1093/epirev/mxn011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry. 1998;173:11–53. doi: 10.1192/bjp.173.1.11. [DOI] [PubMed] [Google Scholar]
- 4.Lawrence D, Kisely S, Pais J. The epidemiology of excess mortality in people with mental illness. Can J Psychiatry. 2010;55(12):752–760. doi: 10.1177/070674371005501202. [DOI] [PubMed] [Google Scholar]
- 5.Felker B, Yazel JJ, Short D. Mortality and medical comorbidity among psychiatric patients: a review. Psychiatr Serv. 1996;47(12):1356–1363. doi: 10.1176/ps.47.12.1356. [DOI] [PubMed] [Google Scholar]
- 6.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153–160. doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–1131. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- 8.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72(3):227–236. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- 9.Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, Penninx BW. Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. Am J Psychiatry. 2014;171(4):453–462. doi: 10.1176/appi.ajp.2013.13030325. [DOI] [PubMed] [Google Scholar]
- 10.Roshanaei-Moghaddam B, Katon W. Premature mortality from general medical illnesses among persons with bipolar disorder: a review. Psychiatr Serv. 2009;60(2):147–156. doi: 10.1176/ps.2009.60.2.147. [DOI] [PubMed] [Google Scholar]
- 11.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42. [PMC free article] [PubMed] [Google Scholar]
- 12.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382 (9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 13.Druss BG, Walker ER. Mental disorders and medical comorbidity. Synth Proj Res Synth Rep. 2011;(21):1–26. [PubMed] [Google Scholar]
- 14.Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425–448. doi: 10.1146/annurev-clinpsy-032813-153657. [DOI] [PubMed] [Google Scholar]
- 15.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 16.Zheng D, Macera CA, Croft JB, Giles WH, Davis D, Scott WK. Major depression and all-cause mortality among white adults in the United States. Ann Epidemiol. 1997;7(3):213–218. doi: 10.1016/s1047-2797(97)00014-8. [DOI] [PubMed] [Google Scholar]
- 17.Druss BG, Zhao L, Von Esenwein S, Morrato EH, Marcus SC. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative US survey. Med Care. 2011;49(6):599–604. doi: 10.1097/MLR.0b013e31820bf86e. [DOI] [PubMed] [Google Scholar]
- 18.Roerecke M, Rehm J. Alcohol use disorders and mortality: a systematic review and meta-analysis. Addiction. 2013;108(9):1562–1578. doi: 10.1111/add.12231. [DOI] [PubMed] [Google Scholar]
- 19.Zhang J, Yu KF. What’s the relative risk? a method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280 (19):1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 20.van Dooren FE, Nefs G, Schram MT, Verhey FR, Denollet J, Pouwer F. Depression and risk of mortality in people with diabetes mellitus: a systematic review and meta-analysis. PLoS One. 2013;8(3):e57058. doi: 10.1371/journal.pone.0057058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Healy D, Le Noury J, Harris M, et al. Mortality in schizophrenia and related psychoses: data from two cohorts, 1875–1924 and 1994–2010. BMJ Open. 2012;2(5):e001810. doi: 10.1136/bmjopen-2012-001810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ponnudurai R, Jayakar J, Sathiya Sekaran BW. Assessment of mortality and marital status of schizophrenic patients over a period of 13 years. Indian J Psychiatry. 2006;48(2):84–87. doi: 10.4103/0019-5545.31595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 24.Harris RJ, Bradburn MJ, Deeks JJ, Harbord RM, Altman DG, Sterne JAC. Metan: fixed- and random-effects meta-analysis. Stata J. 2008;8(1):3–28. [Google Scholar]
- 25.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lipsey MW, Wilson DB. Practical meta-analysis. Vol. 49. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- 27.Harbord RM, Higgins JP. Meta-regression in Stata. Stata J. 2008;8(4):493–519. [Google Scholar]
- 28.Harbord RM, Harris RJ, Sterne JAC. Updated tests for small-study effects in meta-analyses. Stata J. 2009;9(2):197–210. [Google Scholar]
- 29.Sterne JAC, Harbord RM. Funnel plots in meta-analysis. Stata J. 2004;4(2):127–141. [Google Scholar]
- 30.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88(1):15–19. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18(1):23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nuevo R, Chatterji S, Verdes E, Naidoo N, Arango C, Ayuso-Mateos JL. The continuum of psychotic symptoms in the general population: a cross-national study. Schizophr Bull. 2012;38(3):475–485. doi: 10.1093/schbul/sbq099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. [Accessed June 12, 2014];The top 10 causes of death. 2014 http://www.who.int/mediacentre/factsheets/fs310/en/index2.html.
- 34.Heilä H, Haukka J, Suvisaari J, Lönnqvist J. Mortality among patients with schizophrenia and reduced psychiatric hospital care. Psychol Med. 2005;35(5):725–732. doi: 10.1017/s0033291704004118. [DOI] [PubMed] [Google Scholar]
- 35.LeardMann CA, Powell TM, Smith TC, et al. Risk factors associated with suicide in current and former US military personnel. JAMA. 2013;310(5):496–506. doi: 10.1001/jama.2013.65164. [DOI] [PubMed] [Google Scholar]
- 36.Osborn D, Levy G, Nazareth I, King M. Suicide and severe mental illnesses: cohort study within the UK general practice research database. Schizophr Res. 2008;99(1–3):134–138. doi: 10.1016/j.schres.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 37.Gallo JJ, Bogner HR, Morales KH, Post EP, Ten Have T, Bruce ML. Depression, cardiovascular disease, diabetes, and two-year mortality among older, primary-care patients. Am J Geriatr Psychiatry. 2005;13(9):748–755. doi: 10.1176/appi.ajgp.13.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crump C, Ioannidis JP, Sundquist K, Winkleby MA, Sundquist J. Mortality in persons with mental disorders is substantially overestimated using inpatient psychiatric diagnoses. J Psychiatr Res. 2013;47(10):1298–1303. doi: 10.1016/j.jpsychires.2013.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Milstein B, Homer J, Briss P, Burton D, Pechacek T. Why behavioral and environmental interventions are needed to improve health at lower cost. Health Aff (Millwood) 2011;30(5):823–832. doi: 10.1377/hlthaff.2010.1116. [DOI] [PubMed] [Google Scholar]
- 40.Patel V, Araya R, Chatterjee S, et al. Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet. 2007;370 (9591):991–1005. doi: 10.1016/S0140-6736(07)61240-9. [DOI] [PubMed] [Google Scholar]
- 41.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 42.Scott A, Guo B. For Which Strategies of Suicide Prevention Is There Evidence of Effectiveness? Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2012. [Google Scholar]
- 43.Druss BG, Rosenheck RA, Desai MM, Perlin JB. Quality of preventive medical care for patients with mental disorders. Med Care. 2002;40(2):129–136. doi: 10.1097/00005650-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Björkenstam E, Ljung R, Burström B, Mittendorfer-Rutz E, Hallqvist J, Weitoft GR. Quality of medical care and excess mortality in psychiatric patients: a nationwide register-based study in Sweden. BMJ Open. 2012;2:e000778. doi: 10.1136/bmjopen-2011-000778. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.