Abstract
Objective
The purpose of this study was to provide updated national estimates and correlates of service use, unmet need, and barriers to mental health treatment among adults with mental disorders.
Method
The sample included 36,647 adults aged 18–64 years (9723 with any mental illness and 2608 with serious mental illness) from the 2011 National Survey on Drug Use and Health. Logistic regression models were used to examine predictors of mental health treatment and perceived unmet need.
Results
Substantial numbers of adults with mental illness did not receive treatment (any mental illness: 62%; serious mental illness: 41%) and perceived an unmet need for treatment (any mental illness: 21%; serious mental illness: 41%). Having health insurance was a strong correlate of mental health treatment use (any mental illness: private insurance: AOR=1.63 (95% CI=1.29–2.06), Medicaid: AOR=2.66, (95% CI=2.04–3.46); serious mental illness: private insurance: AOR=1.65 (95% CI=1.12–2.45), Medicaid: AOR=3.37 (95% CI=2.02–5.61)) and of reduced perceived unmet need (any mental illness: private insurance: AOR=.78 (95% CI:.65–.95), Medicaid: AOR=.70 (95% CI=.54–.92)). Among adults with any mental illness and perceived unmet need, 72% reported at least one structural barrier and 47% reported at least one attitudinal barrier. Compared to respondents with insurance, uninsured individuals reported significantly more structural barriers and fewer attitudinal barriers.
Conclusions
Low rates of treatment and high unmet need persist among adults with mental illness. Strategies to reduce both structural barriers, such as cost and insurance coverage, and attitudinal barriers are needed.
A substantial number of adults with mental disorders do not receive treatment for their condition, despite overall increases in the rates of treatment in the past 20 years (1–4). In the National Comorbidity Survey Replication, for example, only 33% of adults with any mental illness and 41% of adults with serious mental illness reported receiving mental health treatment in the previous year (1). People who are less likely to receive treatment tend to be male (1, 5, 6), black or Hispanic (1, 6–8), younger (1, 6, 9), uninsured (2, 5, 10), and of low socioeconomic status (1, 4, 9, 11).
Although rates of mental health service use are increasing, perceived unmet need for mental health treatment has also been rising (12). Barriers to treatment reported by people who perceive an unmet need include structural barriers, such as cost, lack of insurance or insufficient coverage for services, and not knowing where to go for help or not being able to get an appointment, and attitudinal barriers, such as perceived stigma and perceiving treatments to be ineffective (13–15). From 1997 to 2002, there was a significant increase the proportion of adults with psychological distress who did not use mental health services and medication because of cost (16). The high uninsurance rate among people with mental disorders contributes to cost being a barrier to treatment (17). Around 20% of people with mental disorders are uninsured compared to 15% in the US population (2, 17, 18).
Given the current implementation of the Patient Protection and Affordable Care Act (ACA), it is important to have updated data on rates and correlates of mental health treatment However, most available information on the topic is based on surveys that are now more than a decade old. This study provides updated estimates of use, perceived unmet need, and barriers to mental health treatment among adults with mental disorders. We used data from the National Survey on Drug Use and Health (NSDUH) to examine following questions: What proportion of all adults and adults with mental illness receive mental health treatment and perceive an unmet need for treatment? What factors are associated with receiving mental health treatment and perceiving and unmet need? What barriers to treatment are encountered by adults with mental illness who report an unmet need for treatment? How do these patterns and barriers differ by insurance status?
Methods
Sample
NSDUH is an annual survey that provides nationally representative estimates of drug use and mental health for the civilian, noninstitutionalized population in the US (14). Respondents include residents of households, civilians living on military bases, and persons in noninstitutional group quarters. Individuals with no fixed address, active-duty military personnel, and residents of institutional facilities are excluded. A representative sample is achieved through a multi-stage area probability sampling process.
Data are collected through in-person interviews at the participant’s residence. Computer-assisted interviewing is utilized to increase participants’ willingness to provide sensitive information. The 2011 NSDUH was administered from January 2011 to December 2011 and had a weighted response rate of 74.4% for all ages (19).
This sample included 36,647 adults aged 18–64 years in the publically available 2011 NSDUH dataset. Adolescents (12–17 years) were excluded because they were asked different questions about mental health services use and symptoms (20). Adults 65 years and older were excluded because of relatively low numbers classified as having any mental illness or serious mental illness.
Mental illness
All NSDUH participants completed the Kessler-6 (K6) scale, measuring psychological distress, and the World Health Organization Disability Assessment Schedule (WHODAS), assessing functional impairment. The Substance Abuse and Mental Health Services Administration developed prediction models using the K6 and WHODAS to estimate any and serious mental illness. The resulting variables indicate whether or not a person has any or serious mental illness. The prediction models were shown to be valid in predicting any mental illness and serious mental illness among a subsample of participants (n=1506) who completed a Structured Clinical Interview for DSM-IV Axis I Disorders (21, 22).
Mental health treatment and perceived unmet need
Mental health outpatient and prescription treatment was ascertained from two questions asking if during the past 12 months respondents received any outpatient treatment or counseling for any problems with emotions, nerves, or mental health in the past 12 months, and took any prescription medication to treat a mental or emotional condition. To assess perceived unmet need for mental health treatment, respondents were asked if during the past 12 months there was a time when they needed mental health treatment or counseling but did not get it. Respondents who reported unmet need were prompted to select any reason(s) for not receiving treatment from a list that included six structural barriers (e.g. cost, not knowing where to go, insurance not paying enough for mental health treatment) and eight attitudinal barriers (e.g. could handle problem on own, did not think treatment would help, concerns about being committed to a psychiatric hospital or taking medication).
Health Insurance
Health insurance was categorized into four exclusive categories: no insurance, private insurance, Medicaid (no private insurance), and other (Medicare, coverage by Tricare, Champus, Veteran’s Administration or military health care, or other insurance).
Sociodemographic Correlates
Sociodemographic correlates included age (18–25, 26–34, 35–49, 50–64), gender, racial or ethnic group (Non-Hispanic white, Non-Hispanic black, Hispanic, other), marital status (married, previously married, never married), education level (less than high school, high school graduate, some college, college graduate), employment status (not working, working), family income (≤$20,000, $20,000-$49,000, $50,000-$74,000, ≥$75,000), and self-rated health (poor/fair, good/very good/excellent).
Analyses
Due to the complex survey design of the NSDUH, all analyses were adjusted for sampling weights, clustering, and stratification of the data. Data analysis was conducted in IBM SPSS Statistics 21, using the complex samples module.
First, summary statistics and Pearson chi-square tests were used to describe demographic characteristics and determine patterns of mental health treatment use and unmet need. For all chi-square tests we report p-values based on the design-based F statistic. Second, logistic regression models were run to assess the association between the sociodemographic correlates and mental health treatment use or unmet need for treatment. We first entered each correlate separately to obtain unadjusted odd ratios; we then ran adjusted models that included all correlates simultaneously. All logistic regression models were run separately for adults with any and serious mental illness. We also performed an exploratory moderation analysis to determine if there was an interaction effect between race/ethnicity and insurance on treatment use. Finally, we used summary statistics and chi-square tests to examine the percentages of participants with any mental illness who reported different barriers to receiving mental health treatment and any variations by insurance type.
Results
The respondents’ demographic and health characteristics are summarized in Table 1. Compared to respondents without mental illness, individuals with mental illness were more likely to be uninsured or on Medicaid, non-Hispanic white, younger, female, unmarried, have lower education, unemployed, have a lower family income, and have poor health.
Table 1.
Demographic characteristics of adult participants in 2011 NSDUH with and without mental illnessa
| Characteristic | No Mental Illness | Any Mental Illness | Serious Mental Illness |
|---|---|---|---|
| Total sample (unweighted n) | 26924 | 9723 | 2608 |
| Weighted % | Weighted % | Weighted % | |
| Insurance | |||
| None | 18.9 | 22.2 | 23.4 |
| Private | 67.9 | 54.9 | 47.1 |
| Medicaid, no private | 8.0 | 14.9 | 19.1 |
| Other | 5.1 | 8.0 | 10.3 |
| Race or Ethnic Group | |||
| Non-Hispanic white | 62.8 | 68.7 | 74.0 |
| Non-Hispanic black | 12.4 | 11.1 | 7.6 |
| Hispanic | 17.1 | 12.7 | 11.4 |
| Other | 7.7 | 7.5 | 7.0 |
| Age Group | |||
| 18–25 | 16.0 | 24.2 | 22.5 |
| 26–34 | 18.6 | 20.2 | 22.1 |
| 35–49 | 32.2 | 30.9 | 31.4 |
| 50–64 | 33.2 | 24.6 | 24.0 |
| Gender | |||
| Female | 48.3 | 60.6 | 66.4 |
| Male | 51.7 | 39.4 | 33.6 |
| Marital Status | |||
| Married | 55.2 | 40.1 | 36.0 |
| Previously married | 15.8 | 20.3 | 24.6 |
| Never married | 29.1 | 39.6 | 39.4 |
| Education | |||
| Less than high school | 12.5 | 15.3 | 16.1 |
| High school graduate | 29.3 | 28.8 | 28.6 |
| Some college | 28.1 | 29.2 | 32.5 |
| College graduate | 31.1 | 26.7 | 22.8 |
| Employment Status | |||
| Not working | 24.6 | 38.1 | 44.7 |
| Working | 75.4 | 61.9 | 55.3 |
| Family Income | |||
| Less than $20,000 | 16.5 | 27.8 | 33.8 |
| $20,000-$49,000 | 29.7 | 33.0 | 34.4 |
| $50,000-$74,000 | 18.1 | 14.5 | 12.6 |
| $75,000 or more | 35.6 | 24.7 | 19.1 |
| Self-rated Health | |||
| Fair/Poor | 8.9 | 22.3 | 32.0 |
| Excellent/Very good/Good | 91.1 | 77.7 | 68.0 |
Design-based F-test comparing any mental illness to no mental illness or serious mental illness to no serious mental illness; for all comparisons p<.001
In the previous 12 months, 38.1% of adults with any mental illness and 59.1% of people with serious mental illness received outpatient and/or prescription treatment (see Table 2). Additionally, 7.9% of adults without mental illness received mental health treatment.
Table 2.
Weighted percentage of 12-month mental health treatment use and perceived unmet need for treatment among adults ages 18–64 by severity of mental illness and insurance status
| Severity of mental illness/Insurance status |
Mental health treatmenta |
Perceived unmet need | ||
|---|---|---|---|---|
| Received mental health treatment (N=5046) |
All who perceived unmet need (N=2251) |
Did not receive treatmentb (N=1277) |
Received treatmentc (N=1267) |
|
| No mental illness | 7.9 | 1.3 | .8 | 6.8 |
| Uninsured | 4.5 | 1.5 | 1.1 | 8.0 |
| Private | 8.3 | 1.1 | .7 | 6.2 |
| Medicaid | 11.0 | 1.8 | .9 | 8.9 |
| Other | 11.0 | 1.3 | .5 | 8.2 |
| Any mental illness | 38.1 | 21.3 | 14.8 | 32.0 |
| Uninsured | 25.2 | 25.7 | 17. | 48.7 |
| Private | 38.5 | 19.2 | 14.3 | 26.9 |
| Medicaid | 48.3 | 22.6 | 11.4 | 34. |
| Other | 51.8 | 21.9 | 12.6 | 30.6 |
| Serious mental illness | 59.1 | 41.2 | 35.2 | 45.4 |
| Uninsured | 44.1 | 46.6 | 36.8 | 58.6 |
| Private | 57.2 | 38.0 | 34.3 | 40.8 |
| Medicaid | 73.0 | 41.6 | 28.7 | 46.3 |
| Other | 76.3 | 43.3 | 47.1 | 42.1 |
| Total | 14.5 | 5.7 | 3.0 | 21.3 |
Outpatient and/or prescription treatment
Percentage of adults who perceived an unmet need among all adults who did not receive mental health treatment
Percentage of adults who perceived an unmet need among all adults who received mental health treatment
Uninsured people with mental illness were significantly less likely to receive treatment compared to people with any type of health insurance (any mental illness: design-based F=28.85, df=3,159, p<.001; serious mental illness: designed-based F=13.73, df=3,165, p<.001). The majority of adults with any mental illness who had private insurance or Medicaid did not receive treatment (61.5% and 51.7%, respectively). In the previous 12 months, 21.3% of adults with any mental illness and 41.2% of adults with serious mental illness reported a perceived unmet need for treatment. Uninsured adults with any mental illness perceived more unmet need compared to insured adults (design-based F=4.78, df=3,162, p=.004). A similar trend was found for serious mental illness, though the differences were not significant.
Insurance status had the strongest association with mental health treatment in the past 12 months relative to the other covariates in the model (Table 3). In the multivariate models, adults with mental illness with any type of health insurance had significantly higher odds of receiving treatment compared to uninsured individuals. Adults with mental illness who had private insurance had over 1.5 times the odds (any mental illness: AOR=1.63; serious mental illness: AOR=1.65) and those with Medicaid had over 2 to 3 times the odds (any mental illness: AOR=2.66; serious mental illness: AOR=3.37) of receiving treatment compared to individuals who were uninsured. Among the other significant sociodemographic correlates, adults over 26 years of age for any mental illness, adults aged 35–45 for serious mental illness, and college graduates had significantly higher odds of receiving mental health treatment. Non-Hispanic blacks, Hispanics, individuals in the “other” race category (any mental illness only), males, working individuals, and those with good to excellent health (any mental illness only) had lower odds of receiving treatment. We tested the interaction effect between insurance status and race and ethnicity, but the results were not significant.
Table 3.
Correlates of outpatient and/or prescription treatment use in the past 12 months among adults with mental illness
| Any Mental Illness | Serious Mental Illness | |||||
|---|---|---|---|---|---|---|
| Characteristic | ORa | AORb | 95% CIb | ORa | AORb | 95% CIb |
| Insurance | ||||||
| None (reference) | ||||||
| Private | 1.86* | 1.63* | 1.29–2.06 | 1.69* | 1.65* | 1.12–2.45 |
| Medicaid, no private | 2.77* | 2.66* | 2.04–3.46 | 3.42* | 3.37* | 2.02–5.61 |
| Other | 3.20* | 2.85* | 1.93–3.98 | 4.08* | 4.10* | 2.42–6.97 |
| Race or Ethnic Group | ||||||
| Non-Hispanic white (reference) | ||||||
| Non-Hispanic black | .42* | .38* | .30–.49 | .51* | .42* | .27–.66 |
| Hispanic | .37* | .40* | .29–.56 | .40* | .42* | .26–.69 |
| Other | .45* | .41* | .28–.61 | .62 | .52 | .26–1.04 |
| Age Group | ||||||
| 18–25 (reference) | ||||||
| 26–34 | 1.54* | 1.43* | 1.18–1.73 | 1.41* | 1.13 | .80–1.61 |
| 35–49 | 2.04* | 1.78* | 1.42–2.23 | 2.46* | 1.73* | 1.15–2.60 |
| 50–64 | 2.63* | 1.88* | 1.43–2.47 | 2.91* | 1.62 | .83–3.17 |
| Gender | ||||||
| Female (reference) | ||||||
| Male | .58* | .58* | .49–.70 | .72* | .73* | .55–.98 |
| Marital Status | ||||||
| Married (reference) | ||||||
| Previously married | 1.23 | 1.05 | .83–1.33 | 1.10 | .93 | .62–1.41 |
| Never married | .63* | 1.02 | .81–1.29 | .52* | .73 | .48–1.12 |
| Education | ||||||
| Less than high school (reference) | ||||||
| High school graduate | .98 | 1.05 | .83–1.33 | 1.01 | 1.05 | .71–1.57 |
| Some college | 1.21 | 1.38 | 1.07–1.77 | 1.24 | 1.54 | .98–2.40 |
| College graduate | 1.48* | 1.72* | 1.28–2.33 | 1.48 | 1.99* | 1.16–3.40 |
| Employment Status | ||||||
| Not working (reference) | ||||||
| Working | .65* | .70* | .58–.84* | .53* | .57* | .42–.78 |
| Family Income | ||||||
| Less than $20,000 (reference) | ||||||
| $20,000-$49,000 | .90 | .96 | .79–1.18 | .79 | .93 | .66–1.30 |
| $50,000–$74,000 | .95 | .94 | .70–1.25 | 1.12 | 1.29 | .73–2.90 |
| $75,000 or more | .99 | .91 | .69–1.19 | .98 | 1.04 | .57–1.90 |
| Self-rated Health | ||||||
| Fair/Poor (reference) | ||||||
| Excellent/Very good/Good | .58* | .69* | .55–.86 | .60* | .84 | .61–1.16 |
Unadjusted odd ratio (OR): models include each correlate separately
Adjusted odds ratio (AOR): model includes all correlates
p<.05
Insurance status was significantly associated with perceived unmet need for adults with any mental illness (Table 4). In the multivariate models, individuals with private insurance (AOR=.78) or Medicaid (AOR=.70) had lower odds of reporting unmet need compared to respondents without insurance. Additionally, among people with any mental illness, adults aged 26–34 had significantly higher odds of reporting an unmet need for treatment, while non-Hispanic blacks, Hispanics, adults 50–64, males, working individuals, respondents with a family income of $75,000 or more, and people in good to excellent health had lower odds of perceiving an unmet need for treatment. Among people with serious mental illness, adults aged 26–34 had higher odds of reporting an unmet need, whereas Hispanics had lower odds of reporting an unmet need.
Table 4.
Correlates of perceived unmet need for mental health treatment in the past 12 months among adults with mental illness
| Any Mental Illness | Serious Mental Illness | |||||
|---|---|---|---|---|---|---|
| Characteristic | ORa | AORb | 95% CIb | ORa | AORb | 95% CIb |
| Insurance | ||||||
| None (reference) | ||||||
| Private | .69* | .78* | .65–.95 | .70* | .85 | .62–1.15 |
| Medicaid, no private | .84 | .70* | .54–.92 | .81 | .73 | .47–1.14 |
| Other | .83 | .88 | .61–1.28 | .90 | 1.08 | .63–1.85 |
| Race or Ethnic Group | ||||||
| Non-Hispanic white (reference) | ||||||
| Non-Hispanic black | .72* | .59* | .45–.76 | .92 | .82 | .52–1.31 |
| Hispanic | .68* | .61* | .47–.79 | .59* | .56* | .36–.87 |
| Other | .80 | .73 | .46–1.15 | 1.33 | 1.39 | .70–2.76 |
| Age Group | ||||||
| 18–25 (reference) | ||||||
| 26–34 | 1.28* | 1.34* | 1.13–1.59 | 1.31 | 1.51* | 1.05–2.17 |
| 35–49 | 1.09 | 1.15 | .90–1.47 | 1.00 | 1.18 | .76–1.82 |
| 50–64 | .74* | .70* | .52–.94 | .85 | .91 | .55–1.49 |
| Gender | ||||||
| Female (reference) | ||||||
| Male | .63* | .60* | .49–.75 | .78 | .73 | .51–1.04 |
| Marital Status | ||||||
| Married (reference) | ||||||
| Previously married | 1.40* | 1.19 | .90–1.59 | 1.25 | 1.10 | .74–1.65 |
| Never married | 1.33* | 1.32 | .97–1.79 | 1.38 | 1.35 | .90–2.04 |
| Education | ||||||
| Less than high school (reference) | ||||||
| High school graduate | .86 | .92 | .67–1.25 | .71 | .72 | .48–1.12 |
| Some college | 1.11 | 1.21 | .95–1.55 | .91 | .92 | .64–1.32 |
| College graduate | .88 | 1.11 | .80–1.55 | .70 | .78 | .48–1.29 |
| Employment Status | ||||||
| Not working (reference) | ||||||
| Working | .73* | .77* | .63–0.95 | .79 | .85 | .66–1.11 |
| Family Income | ||||||
| Less than $20,000 (reference) | ||||||
| $20,000-$49,000 | .83 | .88 | .70–1.10 | .80 | .83 | .64–1.08 |
| $50,000-$74,000 | .80 | .91 | .69–1.20 | .92 | .96 | .63–1.48 |
| $75,000 or more | .59* | .71* | .52–.97 | .59 | .69 | .42–1.13 |
| Self-rated Health | ||||||
| Fair/Poor (reference) | ||||||
| Excellent/Very good/Good | .72* | .69* | .58–.83 | .88 | .92 | .68–1.26 |
Unadjusted odd ratio (OR): models include each correlate separately
Adjusted odds ratio (AOR): model includes all correlates
p<.05
Among adults with any mental illness who perceived an unmet need for mental health treatment, 72.2% reported at least one structural barrier and 46.6% reported at least one attitudinal barrier to receiving treatment. The inability to afford the cost of treatment was the most commonly reported structural barrier to receiving treatment (50.9%), followed by not knowing where to go (16.2%), not having enough time (14.4%), and insurance not covering enough of the cost (12.2%). The most common attitudinal barrier was the respondent thinking that they could handle the problem without treatment (22.9%), followed by thinking that treatment would not help (9.1%), fear of a neighbors or community having a negative opinion of them (8.7%), and a fear of being committed to a psychiatric hospital or having to take medication (8.6%).
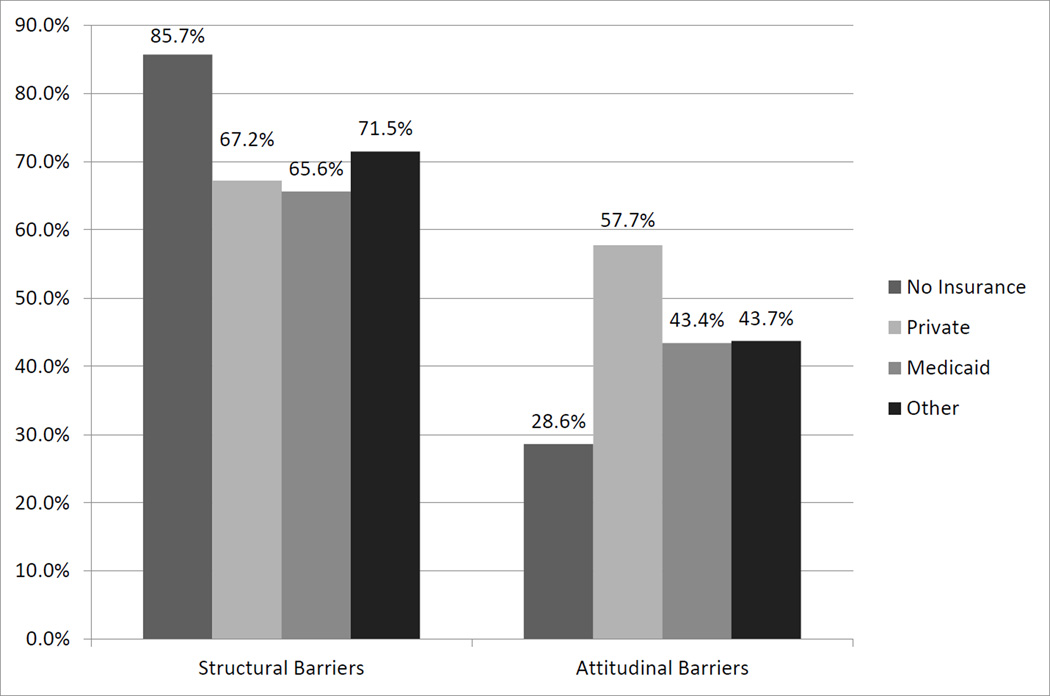
Figure 1 shows the differences in barriers to receiving treatment by type of health insurance. Significantly more uninsured adults who perceived an unmet need reported structural barriers (85.7%) compared to adults with private insurance (67.2%), Medicaid (65.6%), or other insurance (71.5%) (design-based F=7.8, df=3, 164, p<.001). Conversely, significantly fewer uninsured adults reported attitudinal barriers (28.6%) compared to adults with private insurance (57.7%), Medicaid (43.4%), or other insurance (43.7%) (design-based F=16.6, df=2.6, 156, p<.001).
Figure 1.
Structurala and attitudinalb barriers to receiving mental health treatment among adults with any mental illness who perceived an unmet need, by type of health insurance.
a Structural barriers included six options covering cost of treatment, extent of insurance coverage, not knowing where to go for treatment, and barriers to attending appointments.
b Attitudinal barriers included 8 options covering perceptions about need for treatment and treatment ineffectiveness, thinking the respondent could handle problems on their own, and stigma.
Discussion
Substantial numbers of adults with mental illness do not receive mental health treatment and perceive an unmet need for treatment. People with mental illness were more likely to be uninsured or on Medicaid, and less likely to have private insurance, compared to people without mental illness, which is consistent with earlier findings (17, 23). Insurance status was the strongest correlate for receiving treatment in the past year (any and serious mental illness) and perceived unmet need for treatment (any mental illness only). Over 70% of adults with any mental illness who perceived an unmet need for treatment cited structural barriers, particularly treatment cost, as a reason for not receiving treatment. Furthermore, uninsured adults with any mental illness were more likely to report structural barriers and less likely to report attitudinal barriers compared to individuals with insurance.
In the current study, 75% of uninsured adults with any mental illness and 56% of uninsured adults with serious mental illness in our sample did not receive treatment. The ACA, which requires qualified health plans in the exchanges to include coverage for mental health treatment, holds the promise of substantially reducing the numbers of uninsured individuals with mental disorders (24, 25). Furthermore, the Mental Health Parity and Addiction Equity Act of 2008 and the final parity regulations issued in 2013 require insurance plans that cover mental health services to provide coverage on par with general medical services (26). Results from the Oregon Experiment, a randomized Medicaid expansion, showed that Medicaid coverage was associated with a reduction in the probability of a positive depression screen, an increase in the probability of a diagnosis of depression, and a reduction of out-of-pocket expenses (27).
Even among those with insurance, rates of unmet need were quite high. A total of 40% of adults with any mental illness who perceived an unmet need reported attitudinal barriers to receiving treatment. Consistent with earlier findings (14, 28, 29), the most common attitudinal barrier among the NSDUH respondents was thinking they could handle the problem without treatment. Efforts at changing attitudes toward mental health care will need to target multiple sectors of the population and involve a variety of approaches, such as public education and awareness of mental disorders and effective treatments, addressing social norms and cultural factors, and empowering people with mental disorders to overcome barriers to treatment (28, 30). Additional research is needed to identify which programs can effectively reduce attitudinal barriers and improve treatment seeking (31)
Unmet need for treatment was substantial not only among those individuals who did not use mental health services, but also among those who received treatment. Among adults with any or serious mental illness who received mental health treatment, 32% and 45%, respectively, perceived an unmet need for services. Efforts to improve access to mental health services need to also be coupled with initiatives to ensure quality of care (8), and ability to obtain a full range of needed services (24, 25).
It is also important to consider subpopulations at risk for not receiving mental health treatment. In our results, black and Hispanic respondents were less likely than non-Hispanic whites to receive treatment. Although black and Hispanic individuals are more likely to be uninsured than whites (18), in the current study both insured and uninsured racial minorities had a similar likelihood of receiving treatment. Distrust of healthcare providers, low perceived efficacy of treatment, internalized stigma of mental disorders, and loss of income due to taking time off from work to go to appointments are key reasons among minorities for not seeking mental health treatment (32–35). Culturally tailored interventions may be helpful in overcoming barriers to mental health services use.
Several limitations must be considered. First, the NSDUH is a cross-sectional survey. As such we cannot rule out the possibility of selection into, or out of, insurance based on the presence of a mental illness, which would bias the estimated relationship. For instance, people who expect to use more services or more activated patients may be more likely to obtain insurance and to use services (36). Second, while any and serious mental illness are estimated by valid and robust prediction models (21), the survey did not include structured diagnostic interviews that would make it possible to identify individual disorders or to identify individuals with disorders whose symptoms are in remission. Third, mental health treatment use and unmet need were self-reported, and the NSDUH does not include provider-level information about the extent or quality of treatment. Finally, having a diagnosis of a mental illness does not necessarily mean that treatment is needed, and many common disorders may remit even in the absence of treatment (37).
Conclusions
Efforts to improve access to mental health care will need to address structural barriers, such as cost and uninsurance, as well as attitudinal barriers, such as mental health stigma and misconceptions about the effectiveness of treatments. Additional attention will also be needed to ensure quality of care among individuals once they enter the mental health treatment system.
Acknowledgments
Funding: This research was supported by a National Institutes of Health/National Institute of General Medical Sciences Institutional Research and Academic Career Development Award (K12 GM00680-05) and by National Institute of Mental Health Awards 5K24 MH07586703 and 5K01MH09582302.
Footnotes
Disclosures: None for any author.
Contributor Information
Elizabeth Reisinger Walker, Rollins School of Public Health, Emory University - Department of Health Policy and Management, 1518 Clifton Rd, 30322, Georgia, ereisin@emory.edu.
Janet R. Cummings, Emory University - Department of Health Policy and Management, Rollins School of Public Health, 1518 Clifton Road NE Suite 650, Atlanta, Georgia 30322
Jason M. Hockenberry, Emory University - Department of Health Policy and Management, Rollins School of Public Health, Atlanta, Georgia
Benjamin G. Druss, Emory University - Rosalynn Carter Chair in Mental Health, Rollins School of Public Health 1518 Clifton Rd, Atlanta, Georgia 30322.
References
- 1.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McAlpine DD, Mechanic D. Utilization of specialty mental health care among persons with severe mental illness: the roles of demographics, need, insurance, and risk. Health Services Research. 2000;35:277–292. [PMC free article] [PubMed] [Google Scholar]
- 3.Shim RS, Baltrus P, Ye J, et al. Prevalence, treatment, and control of depressive symptoms in the United States: Results from the National Health and Nutrition Examination Survey (NHANES), 2005–2008. Journal of the American Board of Family Medicine. 2011;24:33–38. doi: 10.3122/jabfm.2011.01.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang PS, Angermeyer M, Borges G, et al. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. 2007;6:177–185. [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper-Patrick L, Gallo JJ, Powe NR, et al. Mental health service utilization by African Americans and Whites: the Baltimore Epidemiologic Catchment Area Follow-Up. Medical Care. 1999;37:1034–1045. doi: 10.1097/00005650-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Narrow WE, Regier DA, Norquist G, et al. Mental health service use by Americans with severe mental illnesses. Social Psychiatry and Psychiatric Epidemiology. 2000;35:147–155. doi: 10.1007/s001270050197. [DOI] [PubMed] [Google Scholar]
- 7.Alegria M, Canino G, Rios R, et al. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatric Services. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- 8.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 9.Neighbors HW, Caldwell C, Williams DR, et al. Race, ethnicity, and the use of services for mental disorders: results from the National Survey of American Life. Archives of General Psychiatry. 2007;64:485–494. doi: 10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]
- 10.Druss BG, Hoff RA, Rosenheck RA. Underuse of antidepressants in major depression: prevalence and correlates in a national sample of young adults. Journal of Clinical Psychiatry. 2000;61:234–237. quiz 238–239. [PubMed] [Google Scholar]
- 11.Donisi V, Tedeschi F, Percudani M, et al. Prediction of community mental health service utilization by individual and ecological level socio-economic factors. Psychiatry Research. 2013;209:691–698. doi: 10.1016/j.psychres.2013.02.031. [DOI] [PubMed] [Google Scholar]
- 12.Roll JM, Kennedy J, Tran M, et al. Disparities in unmet need for mental health services in the United States, 1997–2010. Psychiatric Services. 2013;64:80–82. doi: 10.1176/appi.ps.201200071. [DOI] [PubMed] [Google Scholar]
- 13.Mojtabai R. Unmet need for treatment of major depression in the United States. Psychiatric Services. 2009;60:297–305. doi: 10.1176/ps.2009.60.3.297. [DOI] [PubMed] [Google Scholar]
- 14.Mojtabai R, Olfson M, Sampson NA, et al. Barriers to mental health treatment: results from the National Comorbidity Survey Replication. Psychological Medicine. 2011;41:1751–1761. doi: 10.1017/S0033291710002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sareen J, Jagdeo A, Cox BJ, et al. Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatric Services. 2007;58:357–364. doi: 10.1176/ps.2007.58.3.357. [DOI] [PubMed] [Google Scholar]
- 16.Mojtabai R. Trends in contacts with mental health professionals and cost barriers to mental health care among adults with significant psychological distress in the United States, 1997–2002. American Journal of Public Health. 2005;95:2009–2014. doi: 10.2105/AJPH.2003.037630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rowan K, McAlpine DD, Blewett LA. Access and cost barriers to mental health care, by insurance status, 1999–2010. Health Affairs (Millwood) 2013;32:1723–1730. doi: 10.1377/hlthaff.2013.0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeNavas-Walt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States, 2012. Washington, DC: U.S. Census Bureau; 2013. Contract No.: P60–245. [Google Scholar]
- 19.Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of national findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- 20.Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Mental Health Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- 21.Aldworth J, Colpe LJ, Gfroerer JC, et al. The National Survey on Drug Use and Health Mental Health Surveillance Study: calibration analysis. International Journal of Methods in Psychiatric Research. 2010;19(Suppl 1):61–87. doi: 10.1002/mpr.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liao D, Aldworth J, Yu F, et al. Prepared by RTI International for the United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. 2012. Mental Health Surveillance Study: Design and estimation report. [Google Scholar]
- 23.Garfield RL, Zuvekas SH, Lave JR, et al. The impact of national health care reform on adults with severe mental disorders. American Journal of Psychiatry. 2011;168:486–494. doi: 10.1176/appi.ajp.2010.10060792. [DOI] [PubMed] [Google Scholar]
- 24.Beronio K, Glied S, Frank R. How the Affordable Care Act and Mental Health Parity and Addiction Equity Act Greatly Expand Coverage of Behavioral Health Care. Journal of Behavioral Health Services Research. 2014;41:410–428. doi: 10.1007/s11414-014-9412-0. [DOI] [PubMed] [Google Scholar]
- 25.Garfield RL, Lave JR, Donohue JM. Health reform and the scope of benefits for mental health and substance use disorder services. Psychiatric Services. 2010;61:1081–1086. doi: 10.1176/ps.2010.61.11.1081. [DOI] [PubMed] [Google Scholar]
- 26.Department of the Treasury, Internal Revenue Service, Department of Health and Human Services Final rules under the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008; Technical amendment to external review for multi-state plan program. Washington, D.C.: Federal Register; 2013. pp. 68240–68296. [PubMed] [Google Scholar]
- 27.Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment--effects of Medicaid on clinical outcomes. New England Journal of Medicine. 2013;368:1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Andrade LH, Alonso J, Mneimneh Z, et al. Barriers to mental health treatment: results from the WHO World Mental Health surveys. Psychological Medicine. 2013:1–15. doi: 10.1017/S0033291713001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Beljouw I, Verhaak P, Prins M, et al. Reasons and determinants for not receiving treatment for common mental disorders. Psychiatric Services. 2010;61:250–257. doi: 10.1176/ps.2010.61.3.250. [DOI] [PubMed] [Google Scholar]
- 30.Mechanic D. Removing barriers to care among persons with psychiatric symptoms. Health Affairs (Millwood) 2002;21:137–147. doi: 10.1377/hlthaff.21.3.137. [DOI] [PubMed] [Google Scholar]
- 31.Clement S, Lassman F, Barley E, et al. Mass media interventions for reducing mental health-related stigma. Cochrane Database Systematic Reviews. 2013;7:CD009453. doi: 10.1002/14651858.CD009453.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Conner KO, Koeske G, Brown C. Racial differences in attitudes toward professional mental health treatment: the mediating effect of stigma. Journal of Gerontological Social Work. 2009;52:695–712. doi: 10.1080/01634370902914372. [DOI] [PubMed] [Google Scholar]
- 33.Gonzalez JM, Alegria M, Prihoda TJ, et al. How the relationship of attitudes toward mental health treatment and service use differs by age, gender, ethnicity/race and education. Social Psychiatry and Psychiatric Epidemiology. 2011;46:45–57. doi: 10.1007/s00127-009-0168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ojeda VD, McGuire TG. Gender and racial/ethnic differences in use of outpatient mental health and substance use services by depressed adults. Psychiatric Quarterly. 2006;77:211–222. doi: 10.1007/s11126-006-9008-9. [DOI] [PubMed] [Google Scholar]
- 35.Waite R, Killian P. Health beliefs about depression among African American women. Perspectives on Psychiatric Care. 2008;44:185–195. doi: 10.1111/j.1744-6163.2008.00173.x. [DOI] [PubMed] [Google Scholar]
- 36.Frank RG, McGuire TG, Bae JP, et al. Solutions for adverse selection in behavioral health care. Health Care Financing Review. 1997;18:109–122. [PMC free article] [PubMed] [Google Scholar]
- 37.Sareen J, Henriksen CA, Stein MB, et al. Common mental disorder diagnosis and need for treatment are not the same: findings from a population-based longitudinal survey. Psychological Medicine. 2013;43:1941–1951. doi: 10.1017/S003329171200284X. [DOI] [PubMed] [Google Scholar]