Abstract
Project HeartBeat! was a longitudinal “growth” study of cardiovascular disease (CVD) risk factors and body composition in childhood and adolescence. Its findings demonstrate patterns of change from ages 8 to 18 years in anthropometric indicators of adiposity, blood lipid components, and blood pressure measurements, as well as the varying inter-relations among these patterns. Especially noteworthy are differences among associations between the two components of BMI (kg/m2)—the lean or fat-free mass index, and the fat mass index—and each of several CVD risk factors. Policy development and public health recommendations for CVD prevention beginning in childhood have evolved over 30 years or more. A new impetus to action is the recognized increase in the prevalence of childhood overweight and obesity. Intervention to prevent obesity can have a major impact in preventing CVD risk factors more broadly. Opportunities to strengthen interventions for CVD prevention in childhood and adolescence include updated algorithms for monitoring body composition, blood lipids, and blood pressure throughout childhood and adolescence through use of the Project HeartBeat! study results.
Introduction
Project HeartBeat! was a longitudinal “growth” study of cardiovascular disease (CVD) risk factors and body composition in childhood and adolescence involving 678 participants aged 8, 11, or 14 years at entry to a program that included follow-up examinations at 4-month intervals. Follow-up examinations extended on average for eight occasions.1 Participants were enrolled in the Conroe Independent School District in The Woodlands or Conroe TX, two communities located near Houston, and included 50.9% boys and 20.1% blacks. Multilevel analysis provided models for change with age in each measure for the entire synthetic cohort from ages 8 to 18 years.2
Several articles in this supplement to the American Journal of Preventive Medicine from Project HeartBeat! present findings on the growth curves, or trajectories of change with age, in blood lipids (four components)3 and blood pressure (three components),4 as well as several indices of body composition, including BMI and its components, fat free–mass index (FFMI) and fat mass index (FMI).5,6 Where appropriate, measures of diet, physical activity, and sexual maturation were included in the models.
This article places these findings in the context of prior policy development and recommendations addressing CVD prevention, including obesity prevention, blood pressure monitoring, and blood lipid control, beginning in childhood.7 Project HeartBeat! can now contribute to further development and implementation of such recommendations and stimulate further research on prevention of CVD risk factors in youth. Especially in view of the recent impetus to prevent overweight and obesity in childhood and adolescence, these findings have broader relevance than to CVD risk factors alone; they add to further appreciation of differences among common measures of body composition as they develop through childhood and adolescence and thus to considerations in the design and evaluation of interventions to prevent childhood obesity.
Background of Policy and Practice Recommendations for Prevention of CVD Beginning in Childhood
Cardiovascular Risk, Including Overweight and Obesity
Strasser and “primordial prevention,” 1978/1980
The concept of preventing CVD beginning in childhood originated at least 30 years ago. In 1978, Strasser8 introduced the term “primordial prevention” to describe a strategy for preventing epidemics of the onset of risk factors in whole societies. Implicitly, this would require protecting children and young adults from influences that, unopposed, would result in high blood pressure, high cholesterol levels, and smoking. The focus on childhood became explicit in a subsequent essay9:
It will be shown that the prevention of a great proportion of the major cardiovascular diseases is far from being a utopian expectation, provided—and this is the point—it is started early in life.
He noted that the increase in blood pressure in childhood can continue throughout the adult years, although he did not distinguish the component of the increase that appears to universally accompany growth and maturation during childhood and adolescence.
Environmental contributions, such as salt intake, familial resemblance of blood pressure levels, and tracking of blood pressure ranks over time were raised in support of the concept of early intervention.9 Atherosclerosis and its outcomes—ischemic heart disease and stroke—appeared to be preventable by establishing and maintaining adequate behavioral patterns—avoidance of overeating—from early in life. Preventive measures should be applied to children in the community as a whole with more intensive efforts for children of high-risk parents. Children at the upper extreme of blood pressure levels should receive the expected benefits of interventions to reduce salt intake and control obesity, with periodic monitoring throughout their teens and into early adulthood. Strasser thus drew the broad outlines of the preventive recommendations being made today, as well as anticipating the complementary population-wide and individual or high-risk strategies later identified with Rose.10
WHO Expert Committee, 1990
The influence of Strasser’s thinking among his colleagues with the WHO Cardiovascular Disease Unit in Geneva was evident in the commission to a WHO Expert Committee meeting in 1988, under the title “Prevention in Childhood and Youth of Adult Cardiovascular Diseases.” The committee, after completing its deliberations and draft report, extended the title, adding for emphasis: “Time for Action.”11 This report provided details of the scientific basis for action, including evidence concerning early development of blood pressure, blood lipids, left ventricular mass, and BMI.
Recommended actions included specific quantitative goals for improved nutrition (including reduced salt intake), increased physical activity, and elimination of smoking. Overweight and obesity were included among the conditions to be averted by these means. Health promotion approaches were seen as fundamental to this effort. Roles for schools and community organizations were described, and it was recommended that “…countries develop and pursue a comprehensive population strategy for the primary prevention of these [cardiovascular] diseases as part of their long-term national development plan.”11
American Heart Association, 1992–2007
Over a period of at least 16 years, the American Heart Association (AHA) has published successive reports that address cardiovascular health in childhood.12–21 The focus of these statements has been on several topics: obesity and overweight, diet, physical activity, the role of schools in prevention, and more general cardiovascular health. The AHA Scientific Council on Cardiovascular Disease in the Young and its various writing committees were represented especially prominently among the authors of the reports.
In 1992, the AHA proposed12 a concept of integrated cardiovascular health promotion in childhood. The premise was that routine pediatric care should incorporate attention to cigarette smoking, physical activity, obesity, hypertension, and levels of cholesterol. The AHA noted that, in relation to a 1966–1970 baseline, the prevalence of obesity had increased 39% among those aged 12–17 years and 54% among those aged 6–11 years. A combination of weight and selected skinfold measurements was recommended for assessment of obesity: “It is important to discriminate between overweight and obesity. Overweight is defined as exceeding the population norm or average weight considering that person’s gender, height, and frame. Obesity is defined as an excessive amount of body fat.”12 Guidelines from the National Heart, Lung, and Blood Institute (NHLBI) for addressing blood pressure and blood lipids were referenced (see National Heart, Lung, and Blood Institute, 1977–2005, and 1991, below). In 1994, the still-increasing frequency of obesity was noted, and blood pressure screening of children was recommended for detection of treatable cases.13
The first report to focus specifically on obesity appeared in 1996.14 Referring to publications from the mid-1970s to the mid-1990s, a strong link was noted between obesity and both CVD and diabetes, through effects on insulin resistance, dyslipidemia, elevated blood pressure, and increased left ventricular mass, as well as development of atherosclerosis. It was recognized that
…clinical standards for defining obesity in children are not well established. In general, any child with weight for height above the 75th percentile and who suffers from a morbidity that would be worsened by obesity (e.g., dyslipidemia, diabetes mellitus, or hypertension) should be considered obese. For diagnostic and therapeutic purposes, obese people must be distinguished from those who are overweight because of increased lean body mass.14
As in 1992, incorporation of skinfold measurements into clinical practice was again recommended in preference to height-adjusted measures, such as BMI, that do not differentiate between fat and lean body mass. Body fat distribution in abdominal rather than gluteal areas was described as more predictive of morbidity than absolute body fatness. In addition to efforts to reverse obesity in individual patients, primary prevention through public health approaches to improve diet and increase physical activity was also advocated.
In 2002, the theme of cardiovascular health promotion was amplified in a new report.15 A “cardiovascular health schedule” expanded from the 1992 report was to be adopted in clinical primary care. Regarding obesity, it was judged that “…the evidence base is insufficient to provide specific generalizable guidelines for assessment and treatment of child and adolescent obesity.” However, “The BMI is a reliable and valid measure of relative weight in children and is recommended for clinical use.” It was recommended that BMI be calculated especially for children and adolescents at the 75th percentile and above for height and weight. Further, “Children who are crossing BMI percentiles in an upward direction also may be at risk of overweight.” The intent of these recommendations was to assist in preventing obesity as well as to treat it once present.
The concept of monitoring change in BMI over time as a screening approach extended also to blood pressure, blood lipids, and fasting plasma glucose. However, the desirable frequency of such observations was not addressed. Regarding the blood lipid profile, it was suggested15 that screening be done in the late teen years on the basis that the “turmoil of the teenage years” would be largely past and values obtained would be more predictive of adult levels than those recorded at earlier ages.
In 2003, a further report16 presented more explicit health promotion goals and recommendations for three categories of children and adolescents: “all,” those “at high risk of CVD,” and those “with identified risk.” With additional data from trials now available, the authors sought to complement the 2002 report, declaring that “with evidence for the extent and importance of identified risk factors in the young, the time for primary prevention beginning in childhood has come.”
By 2004, the next report17 characterized as “compelling” the engagement of schools in cardiovascular health education. This argument was supported by an overview of ten publications from eight studies of school-based research judged collectively to have shown that school involvement produced “a modest change in physiologic indicators including serum cholesterol, blood pressure, and measures of adiposity.” Recognizing the variability in outcomes among studies, the committee noted that:
Across well-controlled and well-conducted studies, differential results in physiologic outcome indicators point to the need for researchers to pay more attention to developmental age, gender, culture, and sociodemographic factors.
The need to implement school-based interventions in the context of their surrounding communities, in keeping with another AHA report,18 “Guide for Improving Cardiovascular Health at the Community Level,” was emphasized.
In 2005, the most recent report19 focusing on obesity in the context of CVD prevention appeared. The concept of “vulnerable periods for weight gain” within childhood and adolescence was emphasized as offering particular opportunities for prevention. The concept of preventing “abnormal weight gain” in the first place was also addressed. This committee continued to characterize definition of childhood obesity as “problematic”:
Almost all definitions use some variant of BMI. BMI is useful for depicting overweight in the population but is an imperfect approximation of excess adiposity. BMI in children varies with age. This in itself makes BMI definitions of overweight for children more complex than definitions for adults.19
The recommendations of 2005 took on greater urgency than previous reports:
Immediate action must be initiated to prevent excess weight gain and to treat those children and adolescents who are already overweight. Children and adolescents at risk of developing obesity and its complications must be identified and interventions begun. Strategies must be developed that involve families, the healthcare system, healthcare insurers, government agencies, the school system, the food and entertainment industries, and pubic health professionals. Support for research on the development and testing of interventions to prevent and treat overweight in young members of our population is needed to provide a strong evidence base for programs and policies.19
Subsequent AHA Scientific Statements in the area of cardiovascular health promotion in childhood and adolescence update earlier dietary recommendations,20 call on the nation’s schools to take leadership in promoting physical activity,21 and emphasize the role of “advanced practice nurses” in implementing both population-based and individual/high-risk approaches to CVD prevention in children and youth.22 The latest report, like that of 2005, concludes with a call for further research:
Additional research is needed, however, to inform, guide, and evaluate optimal life course strategies for CVD prevention, including multidisciplinary models and integrated systems of healthcare that link individual/high risk and population-based/public health strategies.22
Blood Pressure
National Heart, Lung, and Blood Institute, 1977–2005
In 1977, the NHLBI, addressing measurement procedures and guidelines for detection and evaluation of elevated blood pressure, made its first recommendations concerning blood pressure control in children that were intended for the whole population.23 Reference percentile values of systolic (SBP) and diastolic blood pressure (DBP) were provided for boys and girls by year of age for those aged 2–18 years, based on cross-sectional survey data from three NHLBI-funded pediatric Specialized Centers for Research in Atherosclerosis (SCOR-A) in Miami FL, Muscatine IA, and Rochester MN. A relationship between blood pressure and obesity, fatness, or increased relative weight (none of which was specifically defined) was noted. In defining hypertension, the fourth-phase diastolic blood pressure (DBP4) was used.
Three subsequent reports24–26 on blood pressure in childhood and adolescence have been presented from NHLBI’s National High Blood Pressure Education Program, in 1987, 1996, and 2005. The original report has been refined in several respects. In 1987, data were incorporated from two SCOR-A sites and seven additional data sources, among them the Second National Health and Nutrition Examination Survey (NHANES II).24 Hypertension was defined as blood pressure levels at or above the 95th and 99th percentiles, respectively, of SBP and DBP, separately for newborns, infants, and successive 3-year age groups to age 18 years, for boys and girls combined. Allowance was to be made for exceptional weight or height in applying the blood pressure criteria on the basis that blood pressure above the 90th percentile could be a result of being tall or heavy for age. Both DBP4 and DBP5 were to be recorded when distinguished, with use of DBP4 to classify infants and children aged ≤12 years, and DBP5 for adolescents aged 13–18 years.
The 1996 revision25 further updated the reference data, formally incorporated height percentiles into the scheme for identifying children and adolescents with blood pressure levels not attributable to linear growth, and adopted DBP5 as the standard for DBP levels at all ages. The 2005 report26 further expanded the reference data to include the 1999–2000 NHANES examinations. The category of readings between the 90th and 95th percentiles of blood pressure for age, gender, and height was designated “prehypertensive,” in parallel with the new practice in adult blood pressure evaluation. The DBP5 reading remained the standard for DBP at every age level. Therapeutic lifestyle changes are recommended for every category of blood pressure, including healthy diet, more sleep, and greater physical activity for those classified as “normal,” that is, lower than the 90th percentile.
Cholesterol
National Heart, Lung, and Blood Institute, 1991
Cholesterol levels in children and adolescents have been addressed only once by an NHLBI Expert Panel, in 1991.27 A population-wide approach to improving cholesterol levels in childhood and adolescence is addressed through recommended dietary patterns targeting all Americans. Regarding a high-risk approach, this report defines Acceptable, Borderline, and High categories of total and low-density lipoprotein cholesterol (LDL-C) concentrations. Selective screening is proposed for children and adolescents with a positive family history of high cholesterol or premature CVD, according to specific criteria. Critical values for each category of total cholesterol and LDL-C are fixed from ages 2 to 19 years and are the same for boys and girls. Dietary recommendations are included for lowering cholesterol in those found to have borderline or high values.
American Academy of Pediatrics, 2008
A new report28 on behalf of the American Academy of Pediatrics focuses on blood lipid screening in childhood. Screening is recommended not only for those with a positive family history but also for those—with a full lipid profile—with an unknown family history or the presence of other risk factors (overweight or obesity, hypertension, smoking, or diabetes). Noting variation in cholesterol concentration by age and gender in childhood, the authors propose age-and gender-specific percentile values in screening for total cholesterol and other blood lipid components. However, they rely on the crude age categories of the Lipid Research Clinic Pediatric Prevalence Survey, based on 4-year age bands, which do not take demonstrated variation by year of age into account. However, the basic principle of age- and gender-specific criteria is consistent with the proposal made previously in publications from Project HeartBeat!29,30
Emergent Themes
These examples of policy recommendations and guidelines for addressing CVD risk factors in childhood and adolescence present some common themes. The first is that childhood and adolescence are critical periods for risk factor development and progression of atherosclerosis, from a beginning status of low risk and no more than the ubiquitous minimal atherosclerotic lesions. The second is that personal habits regarding diet, physical activity, and tobacco use are shaped by experience during growth and have immediate and lasting adverse effects on chronic disease risk factors. Third, interventions to prevent and, when necessary, detect and manage the risk factors are well developed for application within a framework of regular health care, and strategies for risk factor prevention at the population level are readily available. Fourth is the mounting concern about child and adolescent obesity that adds new urgency to the recommendations for addressing CVD risk factors that were developed prior to recognition of the obesity epidemic.
Remaining Issues
Obesity
Definition and measurement of obesity present a dilemma between two competing practical concerns, ease of measurement and reliable assessment of true adiposity; the first favors BMI alone, the second suggests skinfold measurements. Monitoring change in BMI or other indicators of adiposity throughout childhood and adolescence is advocated, but guidance is lacking as to frequency, targeting of specific “vulnerable periods for weight gain,” relationship to developmental stages, and differences in targets or schedule by gender.
Blood Pressure and Blood Lipids
Blood pressure and blood lipids need to be monitored, but guidance is lacking on appropriate methods, as noted above for BMI and adiposity. Also lacking is a stated biological rationale for choosing either total cholesterol versus LDL-C or lipid profile along with DBP4 and DBP5, or both, as the focus of monitoring. Since 1991, selective screening has been the standard for cholesterol, with fixed criteria for classification by total cholesterol or LDL-C for all children and adolescents, of both genders, aged 2–19 years. Although the original argument for selective screening was clear, this approach fails to detect a large proportion of those with elevated cholesterol, and variation in total cholesterol and LDL-C by age and gender is overlooked. These limitations are partially overcome by the recent recommendations from the American Academy of Pediatrics, cited above.
Screening and Treatment Practices
Screening, monitoring, and management of obesity, high cholesterol, and high blood pressure are advocated as an integral part of “routine” pediatric or primary care practice, yet no provision is made for the large numbers of children and adolescents for whom no such routine care exists and, consequently, have no opportunity for risk factors to be detected or prevented. Dietary intake and physical activity are behavioral risk factors resulting from both individual- and family-level behaviors, as well as societal conditions. Obese children must be treated in the context of both the family and the broader environment to achieve behavior change. Effective interventions need to be implemented and evaluated through use of appropriate outcome measures that can be tracked and accurately measured.
Main Findings from Project HeartBeat!
Project HeartBeat! provides data closely related to the themes and issues that have been traced through this series of recommendations over the past 30 years, as a review of the main findings presented in this supplement to the American Journal of Preventive Medicine will indicate.
Anthropometry
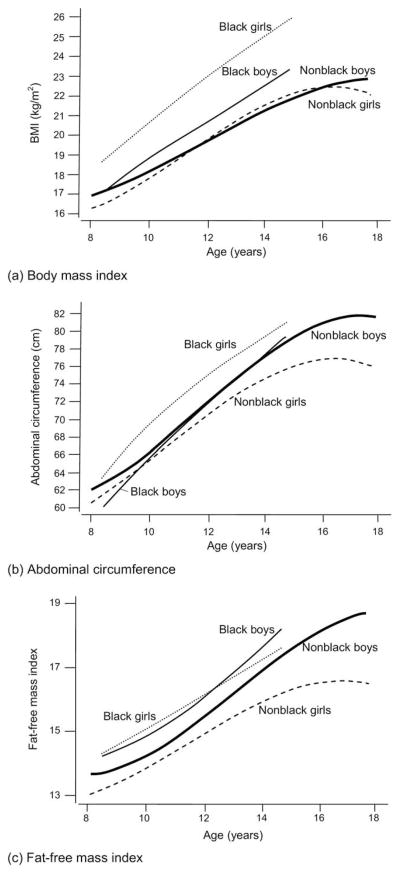
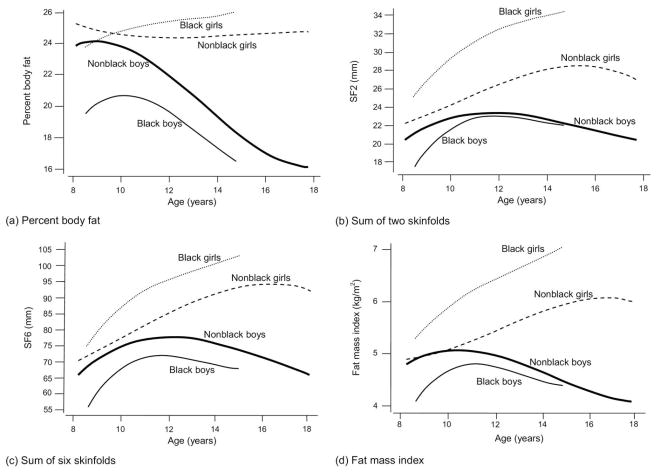
The anthropometric characteristics of primary interest are the measures of body composition addressed in previous publications as well as in this supplement to the American Journal of Preventive Medicine.5,6 These commonly used indices of adiposity are BMI, abdominal circumference, summed skinfold measurements (sum of two skinfolds [SSF2] and sum of six skinfolds [SSF6]), and percent body fat (PBF). These measures are readily differentiated into two groups by inspection of their plotted trajectories by age (Figures 1 and 2). One of the measures is usefully partitioned into two components, each of which conforms closely with one or the other of the two groups: FFMI (Figure 1a) and FMI (Figure 2d).
Figure 1.
Gender- and race-specific trajectories of (a) BMI (kg/m2); (b) abdominal circumference (cm); and (c) fat free–mass index (kg/m2), Project HeartBeat!, 1991–1995
Figure 2.
Gender- and race-specific trajectories of (a) percent body fat (PBF); (b) sum of two skinfolds (SSF2); (c) sum of six skinfolds (SSF6), and (d) fat mass index (kg/m2), Project HeartBeat!, 1991–1995
Abdominal circumference and BMI
Abdominal circumference and BMI (Figure 1a,b) both increase continuously with age from 8 to 18 years, with the exceptions that the increase slows in nonblacks (whites) aged >15 years, and it appears to decrease slightly from age 17 to 18 years in girls. Until this age, average BMI is equal at every age for white boys and girls, but for blacks in this sample, BMI is higher at each age level than it is for whites, especially for girls. Abdominal circumference exhibits the same general pattern of change with age as does BMI but has higher mean values for boys than for girls at each age. This difference widens with increasing age. For boys, abdominal circumference appears to be very similar among blacks and whites, especially for those aged 11–15 years.
Percent body fat, SSF2, and SSF6
The second group of measures consists of PBF, SSF2, and SSF6 (Figures 2a–c). In contrast with BMI and abdominal circumference, values for this second group of measures are higher for girls than for boys of both races at every age. Values decrease for boys from age 9 to 10 years for PBF and from 11 years for SSF2 and SSF6. For girls, PBF remains between 24% and 26% across the age range, whereas for boys it decreases from a peak of ~25% in whites aged 9 years and 21% in blacks aged 10 years to <16% in both blacks and whites for those aged 15–18 years.
Partitioning of BMI: FFMI and FMI
BMI can be partitioned into its two components, FFMI and FMI (Figures 1c and 2d), based on the estimated PBF applied to the total BMI.6 For FFMI, the gender- and race-specific trajectories closely resemble those for BMI (Figure 1a). By contrast, for FMI, the trajectories more closely resemble those for PBF, SSF2, and SSF6, with higher and increasing values with age for girls and lower and decreasing values for boys. For boys, change in BMI with age in adolescence reflects the predominant increase in FFMI, obscuring the fact that FMI is decreasing over the same range of ages, as are PBF, SSF2, and SSF6. This effect is especially strong at older ages for which the trajectories for FFMI and FMI are opposite in direction. For girls, the overall pattern of change with age is similar for FFMI, FMI, and BMI. How BMI is interpreted as a measure of adiposity or obesity for those aged 8–18 years is strongly dependent on both gender and age.
Anthropometry and covariates
Few direct relationships were found between behavioral and familial characteristics and these anthropometric variables.30 Moderate-to-vigorous physical activity (MVPA) was inversely related to FMI, but energy intake was not related. Time spent watching TV was directly related to BMI, but parental obesity was more strongly related. BMI at baseline did not differ by category of total fat intake or MVPA for either gender.31
Blood Lipids
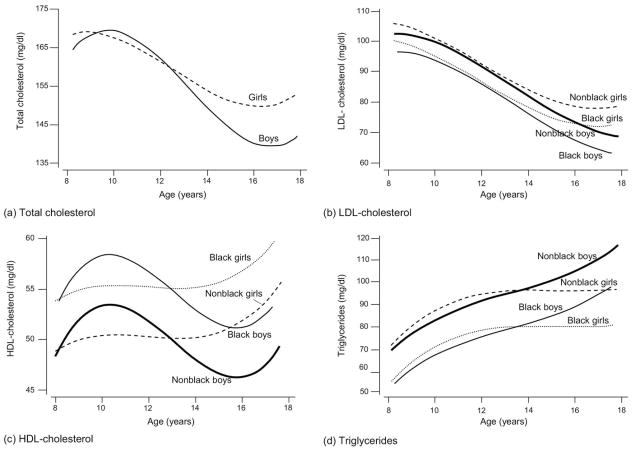
Each of the blood lipid components (total cholesterol, LDL-C, HDL-C, and triglycerides; Figure 3a–d;) exhibits a distinctive trajectory with age.3 Total cholesterol decreases in girls aged 8–16 years, and in boys aged 10–17 years. It then increases in the late teenage years to reach higher values in girls than in boys. This pattern is closely parallel to that for LDL-C in girls, but not in boys. For boys, LDL-C declines continuously from age 8 years, most steeply for those aged ~11–15 years.
Figure 3.
Trajectories of (a) total cholesterol (mg/dL); (b) low-density lipoprotein cholesterol (LDL-cholesterol, mg/dL); (c) high-density lipoprotein cholesterol (HDL-cholesterol, mg/dL); and (d) triglycerides (mg/dL) Project HeartBeat!, 1991–1995
The decline in total cholesterol is delayed in boys relative to girls. This difference is a result of still-increasing HDL-C in boys, before its sharp decline in those aged ~11–16 years. In girls, HDL-C increases to age 10 years, remains constant to age 15 years, then sharply increases. The upturn that appears in total cholesterol level in the late teens is a result of increasing HDL-C in both boys and girls. Triglycerides, by contrast, increase continually to age 18 years for boys. For girls, the increase in triglycerides continues to only age 13 years, and values are constant thereafter. Differences in trajectories by race are observed for LDL-C (blacks having lower values than nonblacks in the late teens), HDL-C (blacks having higher values than non-blacks at all ages), and triglycerides (blacks having lower values than nonblacks at all ages). Reflecting these varied changes in specific lipid components by age, gender, and race, lipid profiles would differ by these same characteristics. Determinants of the lipid profile, in turn, evidently differ among these subgroups within childhood and adolescence.
Blood Lipids, with Anthropometry and Covariates
In general, each index of fatness was associated with increases in total cholesterol, LDL-C, and triglycerides, and with decreases in HDL-C.3 In general, these associations were stronger for boys than for girls but were not influenced by sexual maturation. They were little altered by adjustment for energy intake or time spent in sedentary behavior or in MVPA. Increasing FMI was more strongly related to changes in blood lipids than was increasing FFMI (SD, unpublished observations, 2007). Diet was related to blood lipids only in that dietary cholesterol and monounsaturated fats, but not total energy, affected total cholesterol concentration.32 Apolipoprotein E genotype, studied in girls only, was associated with lower total cholesterol and LDL-C values at every age in the presence of the ε2 allele, a relationship not modified by the other measured factors.33
Blood Pressure, Anthropometry, and Covariates
Blood pressure
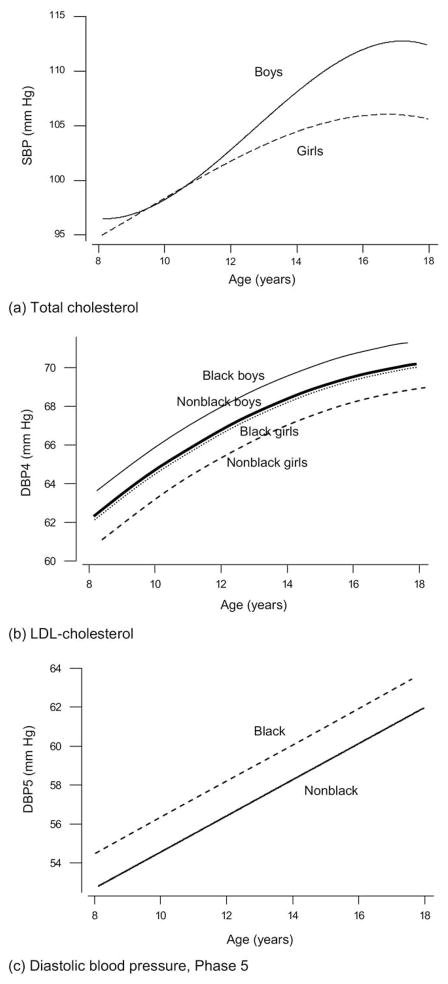
The three blood pressure components (Figure 4a–c) are also distinct from one another.4 SBP increases to age 17 years and appears to decrease slightly thereafter to age 18 years. The rise in SBP is steeper for boys than for girls aged >11 years, and SBP remains higher in boys in their late teens. The model for these two trajectories includes a significant term in age, specifically age 3. Trajectories for DBP4 differ from those for SBP in several respects: The rise in DBP4 with age is continuous, and the levels of the trajectories differ by gender (higher for boys) and by race (higher for blacks, both female and male). The models for DBP4 include a significant term in age, age2, but not age3. A further contrast with the picture for SBP is shown for DBP5. As with DBP4, the rise with age in DBP5 is continuous and the levels are higher for blacks than for nonblacks; but there is no difference by gender, and neither age3 nor age2 is significant—the trajectories for DBP5 by age are linear. The factors that determine the levels of these three measures of blood pressure are evidently distinct, as are their trajectories over the same age range of 8–18 years.
Figure 4.
Trajectories of (a) systolic blood pressure (SBP, mmHg); (b) fourth-phase diastolic blood pressure (DBP4, mmHg); and (c) fifth-phase diastolic blood pressure (DBP5, mmHg), Project Heartbeat!, 1991–1995
Increase in both fatness and FFMI was significantly associated with increasing SBP, and in models adjusted for age, gender, and race, successively less strongly with both DBP4 and DBP5.4 After adjustment for energy intake, MVPA, and sexual maturation, these associations remained significant for SBP, were weakened notably for DBP4, and were no longer significant for DBP5.
Summary
Findings from Project HeartBeat! presented in this supplement to the American Journal of Preventive Medicine include the following key points: Indicators of lean mass (BMI, abdominal circumference, FFMI) and fat mass (PBF, SSF2, SSF6, FMI) tend to cluster into two groups, each with its own close parallels in trajectories of change with age during childhood and adolescence. These multiple anthropometric indicators vary in their relationships to trajectories of change with age among the four components of the blood lipid profile and three measures of blood pressure, during childhood and adolescence.
Significant nonlinearity in patterns of change with age characterizes most of the anthropometric indicators, each component of the blood lipid profile, and two of the three measures of blood pressure. For blood lipids, associations with fatness and the ε2 allele of apolipoprotein E (in girls) were not appreciably altered by adjustment for energy intake, MVPA, and sexual maturation. For DBP4 and DBP5, but not SBP, modest associations with anthropometric indicators became nonsignificant after adjustment for energy intake, MVPA, and sexual maturation, suggesting that SBP may be more strongly determined by intrinsic growth-related factors, and DBP may potentially be more responsive than SBP to the direct influence of behavioral changes and sexual maturation.
Conclusion
Findings from Project HeartBeat! contribute in several ways to potential strengthening and implementation of policies and guidelines for risk factor monitoring, detection, and management, as well as prevention of obesity in children and adolescents. The importance of distinguishing between BMI and true adiposity, emphasized in scientific statements from the AHA, is underscored. Practical means of including skinfold measurements for this purpose could be devised by use of SSF2 (triceps and subscapular) alone, perhaps selectively among those with BMI above a specified threshold level. However, difficulties with skinfold measurement, especially among people with high BMI, may limit the utility of such an approach. High total cholesterol levels may reflect blood lipid profiles that differ widely by age and gender within childhood and adolescence.
General adoption of the most recently recommended age- and gender-specific criteria for screening, broadened to population-wide coverage at appropriate ages and developmental stages and narrowed to single year-of-age percentile values would increase the utility of blood lipid screening in childhood and adolescence. Selective screening among those with high LDL-C to determine apolipoprotein E genotype could also be of value in motivating greater than usual adoption of favorable behavioral patterns among those with the ε3/3 or 3/4 genotype. Blood pressure in childhood and adolescence exhibits differences in patterns of change with age and in relationships with adiposity and other factors when SBP and DBP (whether DBP4 or DBP5) are considered separately. There may be important advantages to assessing these measures separately, rather than defining prehypertension or hypertension based on an either/or consideration of SBP and DBP.
The question of appropriate reference values also warrants attention. Use of data from a recent phase of the NHANES as the reference distribution for blood pressure levels25 contrasts with the adoption of earlier reference values for BMI. If blood pressure distributions, like those for BMI, have shifted upward in recent years, a misleading baseline for evaluating current blood pressure levels may obscure important population changes in blood pressure. Monitoring of BMI, blood lipids, and blood pressure, recommended as standard pediatric care, can be informative if conducted on an appropriate schedule, considering age, gender, developmental stage, and previous trajectory of change. Further consideration of these factors in proposing a monitoring algorithm, adaptive to the observed course of change in individuals with unfavorable patterns of change, could enhance the utility and effectiveness of this aspect of care. There remains the need to address the gap in access to monitoring for those lacking a regular source of care.
Apart from these practical implications of the Project HeartBeat! findings, several points are relevant to further research in this area. Longitudinal observations in childhood and adolescence with sufficient frequency of follow-up assessments to monitor change in CVD risk factors and related characteristics at the individual level are scarce. The study design for Project HeartBeat! was based on observation of overlapping age groups to generate synthetic cohort patterns through multilevel analysis. Appreciation of variation with age in these characteristics and the interdependence of their development in childhood and adolescence is greatly enhanced by observation at frequent intervals, every 4 months in Project HeartBeat!.
This design could readily be expanded to include a wider range of age cohorts, with extended follow-up assessment for each cohort, to address important remaining questions. Enhancements of the design would provide longer-term individual trajectories (e.g., over a 10-year period) to detect points of inflection (or “vulnerable periods”) in the course of change, allow extension into early adult years, incorporate more frequent and more detailed assessment of nutrition and physical activity, and ensure adequate representation of multiple racial/ethnic groups. Among other characteristics to be included for the whole cohort or subsamples of the cohorts are glucose and insulin-related measures, and more precise measures of body composition. A study of this kind could incorporate newer instruments and technologies developed since the start of Project HeartBeat!, whereas measurement protocols supporting the original design largely remain current and are readily accessible via the corresponding author.
Acknowledgments
The authors acknowledge with gratitude the contribution of time and dedication of each Project HeartBeat! participant and family. Cooperation of the Conroe Independent School District and generous support of The Woodlands Corporation are deeply appreciated. The Woodlands and Conroe Advisory Committees have assisted greatly in the planning and conduct of the project. Cooperative Agreement U01-HL-41166, National Heart, Lung, and Blood Institute, provided major funding for the project. Support of the CDC, through the Southwest Center for Prevention Research (U48/CCU609653), and that of Compaq Computer Corporation is also gratefully acknowledged, as is that of the University of Texas Health Science Center at Houston, School of Public Health. We thank Prof. James M. Tanner for helpful advice on the design of the study while he was Visiting Professor at the School of Public Health, University of Texas. The authors also acknowledge the essential contributions of the Project HeartBeat! co-investigators to the design and implementation of this study, including Drs. Nancy Ayers, J. Timothy Bricker, John Kirkland, Claudia Kozinetz, Daniel Oshman, Alexander Roche, and William J. Schull. Senior staff of the data management and field center management were Tony Arrey and Marilyn Morrissey, and Candace Ayars and Pamela Folsom, respectively.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC.
No financial disclosures were reported by the authors of this paper.
References
- 1.Dai S, Labarthe DR, Day RS, et al. Project HeartBeat!: concept, development, and design. Am J Prev Med. 2009;37(1S):S9–S16. doi: 10.1016/j.amepre.2009.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harrist RB, Dai S. Analytic methods in Project HeartBeat! Am J Prev Med. 2009;37(1S):S17–S24. doi: 10.1016/j.amepre.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dai S, Fulton JE, Harrist RB, Grunbaum JA, Steffen LM, Labarthe DR. Blood lipids in children: age-related patterns and association with body-fat indices: Project HeartBeat! Am J Prev Med. 2009;37(1S):S56–S64. doi: 10.1016/j.amepre.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Dai S, Labarthe DR, Fulton JE, Harrist RB, Shah SM, Eissa MA. Systolic and fourth- and fifth-phase diastolic blood pressure from ages 8 to 18 years: Project HeartBeat! Am J Prev Med. 2009;37(1S):S86–S96. doi: 10.1016/j.amepre.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 5.Dai S, Labarthe DR, Grunbaum JA, Harrist RB, Mueller WH. Longitudinal analysis of changes in indices of obesity from age 8 to 18 years: Project HeartBeat! Am J Epidemiol. 2002;156:720–9. doi: 10.1093/aje/kwf109. [DOI] [PubMed] [Google Scholar]
- 6.Eissa MA, Dai S, Mihalopoulos NL, Day RS, Harrist RB, Labarthe DR. Trajectories of fat mass index, fat free–mass index, and waist circumference in children: Project HeartBeat! Am J Prev Med. 2009;37(1S):S34–S39. doi: 10.1016/j.amepre.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Labarthe DR, Dai S, Harrist RB. Blood lipids, blood pressure, and BMI in childhood and adolescence: background to Project HeartBeat! Am J Prev Med. 2009;37(1S):S3–S8. doi: 10.1016/j.amepre.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Strasser T. Reflections on cardiovascular diseases. Interdiscip Sci Rev. 1978;3:225–30. [Google Scholar]
- 9.Strasser T. Prevention in childhood of major cardiovascular diseases of adults. In: Falkner F, editor. Prevention in childhood of health problems in adult life. Geneva: WHO; 1980. [Google Scholar]
- 10.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14:32–8. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 11.WHO Expert Committee. Technical Report Series 792. Geneva: WHO; 1990. Prevention in childhood and youth of adult cardiovascular diseases: time for action. [PubMed] [Google Scholar]
- 12.Strong WB, Deckelbaum RJ, Gidding SS, et al. Special report: integrated cardiovascular health promotion in childhood: a statement for health professionals from the Subcommittee on Atherosclerosis and Hypertension in Childhood of the Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 1992;5:1638–44. doi: 10.1161/01.cir.85.4.1638. [DOI] [PubMed] [Google Scholar]
- 13.Moller JH, Taubert KA, Allen HD, Clark EB, Lauer RM. A Special Writing Group from the Task Force on Children and Youth, American Heart Association. Cardiovascular health and disease in children: current status. Circulation. 1994;9:923–30. doi: 10.1161/01.cir.89.2.923. [DOI] [PubMed] [Google Scholar]
- 14.Gidding SS, Leibel RL, Daniels S, Rosenbaum M, Van Horn L, Marx GR. Understanding obesity in youth. A Statement for healthcare professionals from the Committee on Atherosclerosis and Hypertension in the Young of the Council on Cardiovascular Disease in the Young and the Nutrition Committee, American Heart Association. Circulation. 1996;4:3383–7. doi: 10.1161/01.cir.94.12.3383. [DOI] [PubMed] [Google Scholar]
- 15.Williams CL, Hayman LL, Daniels SR, et al. Cardiovascular health in childhood. A Statement for Health Professionals from the Committee on Atherosclerosis, Hypertension, and Obesity in the Young (AHOY) of the Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2002;106:143–60. doi: 10.1161/01.cir.0000019555.61092.9e. [DOI] [PubMed] [Google Scholar]
- 16.Kavey R-EW, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003;107:1562–6. doi: 10.1161/01.cir.0000061521.15730.6e. [DOI] [PubMed] [Google Scholar]
- 17.Hayman LL, Williams CL, Daniels, et al. Cardiovascular health promotion in the schools. A Statement for health and education professionals and child health advocates from the Committee on Atherosclerosis, Hypertension, and Obesity in Youth (AHOY) of the Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004;110:2266–75. doi: 10.1161/01.CIR.0000141117.85384.64. [DOI] [PubMed] [Google Scholar]
- 18.Pearson TA, Bazzarre TL, Daniels SR, et al. American Heart Association guide for proving cardiovascular health at the community level. A statement for public health practitioners, healthcare providers, and health policy makers from the American Heart Association Expert Panel on Population and Prevention Science. Circulation. 2003;107:645–51. doi: 10.1161/01.cir.0000054482.38437.13. [DOI] [PubMed] [Google Scholar]
- 19.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents. Pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 20.Gidding SS, Dennison BA, Birch LL, et al. Dietary recommendations for children and adolescents. A guide for practitioners. Consensus statement from the American Heart Association. Endorsed by the American Academy of Pediatrics. Circulation. 2005;112:2061–75. doi: 10.1161/CIRCULATIONAHA.105.169251. [DOI] [PubMed] [Google Scholar]
- 21.Pate RR, Davis MG, Robinson TN, Stone EJ, McKenzie TL, Young JC. Promoting physical activity in children and youth. A leadership role for schools. A scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Physical Activity Committee) in collaboration with the Councils on Cardiovascular Disease in the Young and Cardiovascular Nursing. Circulation. 2006;114:1214–24. doi: 10.1161/CIRCULATIONAHA.106.177052. [DOI] [PubMed] [Google Scholar]
- 22.Hayman LL, Meininger JC, Daniels SR, et al. Primary prevention of cardiovascular disease in nursing practice: focus on children and youth. A Scientific Statement from the American Heart Association Committee on Atherosclerosis, Hypertension, and Obesity in Youth of the Council on Cardiovascular Disease in the Young, Council on Cardiovascular Nursing, Council on Epidemiology and Prevention, and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116:344–57. doi: 10.1161/CIRCULATIONAHA.107.184595. [DOI] [PubMed] [Google Scholar]
- 23.Task Force on Blood Pressure Control in Children. Report of the Task Force on Blood Pressure Control in Children. Pediatrics. 1977;2S:I–II. 797–820. [PubMed] [Google Scholar]
- 24.Task Force on Blood Pressure Control in Children. Report of the Second Task Force on Blood Pressure Control in Children–1987. Pediatrics. 1987;79:1–25. [PubMed] [Google Scholar]
- 25.National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Update on the 1987 task force report on high blood pressure in children and adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics. 1996;98:649–58. [PubMed] [Google Scholar]
- 26.USDHHS. Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. USDHHS, NIH, National Heart, Lung, and Blood Institute; May, 2005. NIH Publication No. 05-5267. [Google Scholar]
- 27.National Cholesterol Education Program Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Bethesda Maryland: USDHHS, Public Health Service, NIH, National Heart, Lung, and Blood Institute, National Cholesterol Education Program; 1991. NIH Publication No. 91-2732. [Google Scholar]
- 28.Daniels SR, Greer FR Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122:198–208. doi: 10.1542/peds.2008-1349. [DOI] [PubMed] [Google Scholar]
- 29.Labarthe DR, Nichaman MZ, Harrist RB, Grunbaum JA, Dai S. Development of cardiovascular risk factors from ages 8 to 18 in Project HeartBeat! Study design and patterns of change in plasma total cholesterol concentration. Circulation. 1997;95:2636–42. doi: 10.1161/01.cir.95.12.2636. [DOI] [PubMed] [Google Scholar]
- 30.Labarthe DR, Dai S, Fulton JE. Cholesterol screening in children: insights from Project HeartBeat! and NHANES III. Prog Ped Cardiol. 2003;17:169–78. [Google Scholar]
- 31.Fulton JE, Dai S, Steffen LM, Grunbaum JA, Shah SM, Labarthe DR. Physical activity, energy intake, sedentary behavior, and adiposity in youth. Am J Prev Med. 2009;37(1S):S40–S49. doi: 10.1016/j.amepre.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Altwaijri YA, Day RS, Harrist RB, Dwyer JT, Ausman LM, Labarthe DR. Sexual maturation affects diet–blood total cholesterol association in children: Project HeartBeat! Am J Prev Med. 2009;37(1S):S65–S70. doi: 10.1016/j.amepre.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 33.Fulton JE, Dai S, Grunbaum JA, Boerwinkle E, Labarthe DR. Effects of apolipoprotein E genotype on blood cholesterol in adolescent girls. Am J Prev Med. 2009;37(1S):S78–S85. doi: 10.1016/j.amepre.2009.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]