Abstract
Purpose
The purpose of the current study is to examine the efficacy of Counselor-Assisted Problem Solving (CAPS) in improving caregiver adaptation following traumatic brain injury (TBI).
Research Method/Design
In a randomized clinical trial comparing CAPS (n = 65), an online problem-solving intervention with accompanying Web-based counseling sessions, with an information-based Internet Resource Comparison (IRC; n = 67) program, participants included families of 12- to17-year-olds who had sustained a TBI in the past 6 months. Linear regression analyses were used to identify main effects and to examine whether caregiver education, race, or prior computer use moderated treatment efficacy.
Results
Computer experience moderated postintervention improvements in caregiving self-efficacy following CAPS, Specifically, parents in CAPS with low levels of prior use reporting the greatest improvements. CAPS participants who completed 5 or more sessions reported greater reductions in depression than did the IRC; however, the groups did not differ on global distress.
Conclusions/Implications
Findings support the potential utility of counselor-supported Web-based interventions particularly for individuals with limited computer expertise following adolescent TBI.
Keywords: brain injury, caregiver outcomes, stress, trauma, adolescence
Introduction
Childhood traumatic brain injury (TBI) has been shown to contribute to parent/caregiver burden and psychological distress as well as family dysfunction (Wade, Taylor, Drotar, Stancin, & Yeates, 1998). Factors such as greater injury severity (Wade et al., 1998; 2004), high levels of chronic family stresses coupled with deficient resources (Wade et al., 2004), maladaptive preferred coping strategies (Wade et al., 2001; Yeates et al., 2002), and unmet health care needs (Aitken et al., 2009) appear to place caregivers at elevated risk for psychological distress.
Findings suggest that family burden, injury-related stress, and parental psychological symptoms often increase following TBI (Wade et al., 1998; Wade, Taylor, Drotar, Stancin, Yeates, & Minich, 2002). Given the negative effects of TBI on family and caregiver functioning, several teams of clinical researchers have adopted a caregiver or family problem-solving framework to address the complex array of issues that confront families following TBI (Kreutzer et al., 2009; Rivera, Elliott, Berry, & Grant, 2008). Problem-solving therapy provides a structured, yet flexible, approach for staying positive and addressing the varied difficulties and changing family dynamics that often accompany TBI (D’Zurilla & Nezu, 2006). Problem-solving therapy has been used with caregivers of adults with TBI (Kreutzer et al., 2009; Rivera et al., 2008) and has been used increasingly in family-centered treatments for children and youth with TBI (Gan, Gargaro, Kreutzer, Boschen, & Wright, 2010).
Three previous Randomized Control Trials (RCTs) provide conflicting evidence regarding the efficacy of family problem-solving therapy in reducing parent depression and distress following pediatric TBI. A study by Wade, Michaud, and Brown (2006) comparing the efficacy of family problem-solving therapy with standard psychosocial care in a cohort of 32 children with moderate to severe TBI failed to find differences in caregiver distress following treatment. However, they noted that relatively low levels of distress at baseline may have reduced the ability to detect treatment effects. A second study by the same investigative team (Wade, Carey, & Wolfe, 2006) examined the efficacy of an online-version of the family problem-solving treatment which integrated psychoeducational Web modules with synchronous videoconferencing to apply the problem-solving process to problems identified by the family. In a randomized clinical trial of 40 families of children ages 5 to 17 with moderate to severe TBI, the efficacy of online family problem solving was examined relative to an online information-based program in which participants received high-speed Internet and access to Internet resources about TBI. Results from this study indicated that online family problem-solving therapy was superior to access to Internet resources in reducing caregiver anxiety, depression, and global distress. However, further analyses suggested that the treatment was not effective for the 30% of parents who did not own a home computer prior to the study (Carey, Wade, & Wolfe, 2008). Greater nonadherence appeared to mediate the association between lack of computer ownership and poorer treatment response. A recent trial of the efficacy of problem-solving therapy versus access to Internet resources with families of adolescents with TBI provided evidence that treatment efficacy was moderated by socioeconomic status (SES), with families of lower SES benefiting more from problem-solving therapy whereas families of higher SES benefited more from access to Internet resources alone (Wade et al., 2012). Taken together, these studies provide support for the efficacy of family problem-solving therapy in reducing caregiver distress following TBI while underscoring the importance of considering potential moderators of treatment efficacy such as computer literacy and socioeconomic status.
Research has demonstrated that caregiver outcomes, including distress and depression, may be a particularly important influence on recovery following childhood TBI (Taylor et al., 2001; Taylor et al., 2002). For example, Taylor et al. (2001) reported that higher parent distress at 6 months post-TBI was associated with more child behavior problems at 12 months, suggesting that post-TBI recovery of the child is influenced by caregiver functioning. However, research with larger, more homogeneous samples with respect to the child’s age and time since injury is needed to allow for a more complete appreciation of the efficacy of family problem solving in reducing caregiver depression and distress and to identify who is most likely to benefit.
We examined the efficacy of online family problem solving supported by synchronous videoconference sessions with a licensed psychologist (Counselor-Assisted Problem Solving; CAPS) relative to access to Internet resources (Internet Resource Comparison; IRC) in reducing caregiver depression and distress following TBI in adolescence. This study expands upon previous studies (Wade, Carey, & Wolfe, 2006; Wade et al., 2009; 2012) by examining this question in a large, relatively homogeneous sample with respect to age and time since injury, thus allowing for conclusions to be made regarding the efficacy of the CAPS intervention within a specific population of interest (adolescents and their families within the initial 1–6 months postinjury). Consistent with previous studies, we hypothesized that CAPS would result in greater reductions in parent depression and distress and greater increases in caregiving efficacy than would access to Internet resources alone. Moreover, we extended consideration of potential moderators by evaluating the influences of race/ethnicity as well as factors considered in previous studies (computer usage, SES) on treatment response. SES, race, and computer literacy are likely to be correlated (Jackson et al., 2008; Lorence, Park, & Fox, 2006) and prior findings are contradictory with respect to who is most likely to benefit (i.e., both prior technology users and those of lower SES were more likely to benefit). As such, specific directional hypotheses for moderation were not offered.
Method
Recruitment
The trial was registered with www.clinicaltrials.gov, assigned identifier: NCT00409448. Participants were recruited via the Trauma Registries of five major trauma-centers in the Central and Western regions of the United States. The study was approved by the Institutional Review Board of each of the participating medical centers prior to inception. Children between the ages of 12–17 years who were hospitalized overnight for a complicated mild to severe TBI within the previous 1–6 months were considered for inclusion. Additional eligibility requirements included documented alteration of neurological functioning as measured by either a Glasgow Coma Scale (GCS) score less than 13 and/or evidence of neurological insult as seen on MRI or computerized tomography, English as the primary language spoken in the home, availability of the adolescent to participate in the intervention, and family residence within a 3 hr drive of the hospital. Exclusion criteria included: (a) insufficient child recovery by 6 months postinjury to participate in the intervention (e.g., persistent significant cognitive or verbal impairments that would prevent participation in the intervention, such as inadequate verbal and communication skills or insufficient attentional capabilities); (b) psychiatric hospitalization for either child or parent during the year prior to the injury; (c) family residence in an area without high-speed Internet access; (d) child residence outside the home (e.g., detention facility) or (e) diagnosis of intellectual disability (IQ < 65) prior to the injury. Seventeen percent (52/308) of those screened were ineligible for one or more of these reasons, with a primary language other than English constituting the most common reason for exclusion (see Figure 1).
Figure 1.
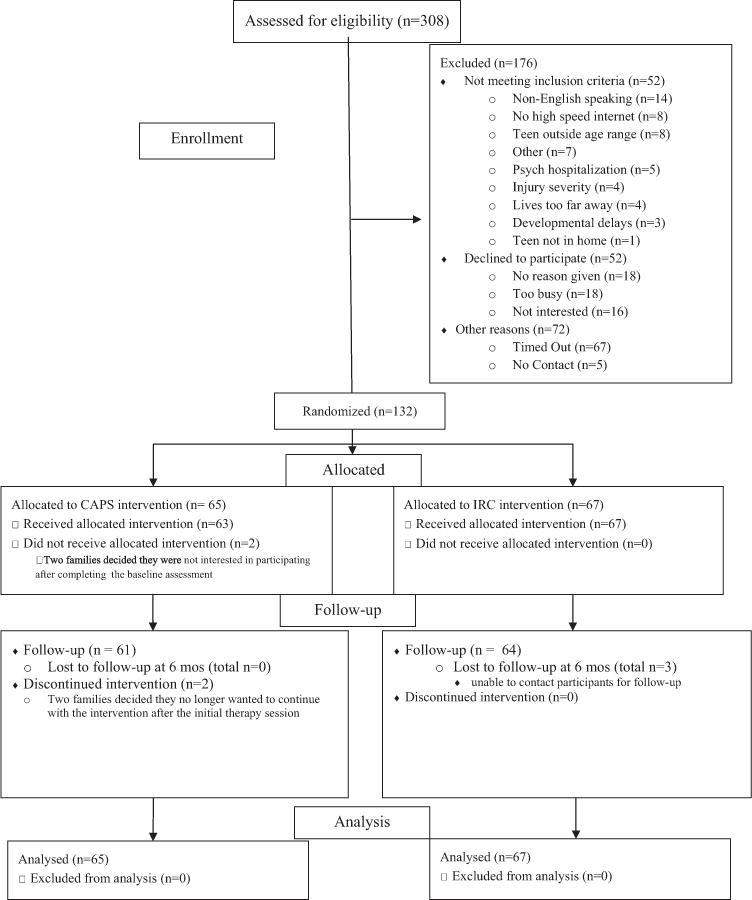
CONSORT diagram.
Baseline Assessment and Random Assignment
After obtaining informed consent from the parents and assent from the teen, study personnel completed the baseline/pretreatment assessment at the family’s home. During this assessment, the primary caregiver provided information regarding demographic characteristics and completed self-report measures of depression, distress, caregiving efficacy, and prior computer use. Participating families were given new computers and were provided with Web cameras and high-speed Internet access for the duration of the study. Families were also shown how to log onto the study Web site and access the links to TBI resources on the Web. Self-report measures of parent functioning were readministered at a follow-up assessment approximately 6 months later.
Adolescents and their families were randomly assigned to either of two 6-month long Internet-based interventions: CAPS, described in greater detail below, a family problem-solving intervention that provided training in communication skills, self-regulation and anger management; or an Internet resource comparison (IRC) group, a self-guided, information-based program. To ensure that group composition was balanced with respect to both gender and within each of the sites, randomization was stratified on these factors. A SAS program was created using permuted block sizes for each of the randomizations. A sealed envelope containing group assignment was handed to the participants at the end of the baseline visit allowing interviewers to remain naïve to group assignment at the baseline assessment. Thus, interviewers/research assistants were unaware of group assignment at both assessments, whereas parents were naïve to group assignment only at the baseline visit.
Treatment Groups
CAPS intervention
Four clinical psychologists, licensed an average of 3.25 years (range 0–7), delivered the CAPS treatment after completing an initial, 2-day training program. Session objectives were outlined in a detailed treatment manual (available from the first author upon request) and reviewed during weekly supervision calls to maintain treatment fidelity. To document adherence to and any deviations from specified content, both the psychologist and participating caregivers completed end of session checklists.
The initial CAPS session involved a face-to-face meeting in the family’s home to identify goals that each family member wanted to address and establish rapport. The teen with TBI and one parent or caregiver were required to attend each core session and both parents and school-age siblings, when present in the home, were encouraged to participate.
Each subsequent CAPS session consisted of a didactic online module that the family completed without the psychologist’s assistance. After completing the online module, the family subsequently had a Skype session with the psychologist. The intervention was designed to be completed over a 6-month period with weekly sessions for the first 2–3 weeks and then biweekly sessions until the family completed the initial seven core sessions. The core sessions primarily focused on problem solving and application to a goal or problem identified by the family. After generating a solution to the goal or problem that the family initially identified as problematic, the family’s homework was to implement the agreed-upon plan and evaluate its success. Subsequent core sessions focused on developing strategies to facilitate effective family problem solving, including basic communication skills and developing strategies to address common cognitive and behavioral consequences of TBI.
During Session 7, participating parents completed a measure of family burden and a self-assessment of family problem solving and communication skills. The psychologist used this self-assessment to identify the need for additional, supplemental sessions to address unresolved family concerns or skills deficits. Families received up to four supplemental sessions and a final wrap-session to review progress and develop a plan for addressing future problems. See Wade et al., in press for a list of core and supplemental sessions and additional details regarding session content.
IRC intervention
Families in the IRC group also received computers and Web cameras, the latter was provided to keep the interviewers unaware of group assignment. IRC families received access to a home page with links to online resources such as local, state, and national brain injury associations and sites focusing on pediatric brain injury, such as the Center on Brain Injury Research and Training, Brain Injury Partners, and the National Database of Educational Resources on Traumatic Brain Injury. Families were encouraged to spend at least 1 hr per week accessing information regarding pediatric brain injury on the Web throughout the 6-month intervention period and to track the sites that they visited. At follow-up, parents provided information about the TBI-related Web sites visited and the time spent at each site. By offering the IRC comparison group Web-based resources about TBI, we controlled for the nonspecific effects of having online access to the resources and information, including chat rooms, online support groups, and information-based resources on TBI, while also allowing for examination of the additive effects of problem-solving therapy sessions with a therapist and access to the didactic online modules that was offered by the CAPS intervention.
Follow-Up Assessment
The postintervention follow-up assessments were scheduled an average of 6 months after the baseline assessment and included an interview with the primary caregiver and completion of the self-report measures administered at the baseline assessment. To equate the time between baseline and follow-up assessments between groups and to maintain concealment of group assignment, follow-ups were scheduled without knowledge of whether the participant had completed the treatment protocol or not. As a consequence, a subset of families did not complete the core sessions until after the 6-month follow-up; this subset of families therefore did not receive the full course of treatment at the 6-month follow-up and may have therefore had lagged treatment effects.
Measures
Background questionnaire
Information regarding injury severity was extracted from relevant hospital records. Sociodemographic information, including median family income and primary caregiver educational attainment, was collected from the caregiver at the baseline assessment. Parents/primary caregivers completed a baseline interview regarding preinjury diagnoses and treatments, as well as current behavioral and medical treatments.
Caregiver depression and distress
Given prior research demonstrating that caregiver distress often impacts behavioral recovery following TBI (Taylor et al., 2001), the Global Severity Index (GSI) of the Symptom Checklist-90-R (SCL-90–R), a 90-item self-report inventory, provided a measure of global psychiatric symptoms and caregiver distress. The SCL-90–R has well-documented reliability and validity, including high levels of internal consistency, test–retest reliability, and convergent-discriminant validity. The GSI is reported as a T score with a mean of 50 and a standard deviation of 10. Scores greater or equal to 63 are considered to be indicative of clinically significant levels of distress (Derogatis & Lazarus, 1994). The Center for Epidemiologic Studies Depression Scale (CES-D) was used to assess specific symptoms of depression. It has well-established psychometric properties and is useful for screening individuals at risk for developing clinical depression. A raw score of 16 is typically used as a cutoff to indicate clinically significant depressive symptoms (Radloff, 1977).
Caregiving efficacy
Prior research has reported that caregiver burden and coping is of relevance when considering post-TBI outcomes (Wade et al., 2002; Wade et al., 2001). Therefore, we were interested in investigating the impact of the CAPS intervention on caregiver self-efficacy. The total from the Caregiver Self-Efficacy Scale (CSES), a 25-item parent report scale, provided a measure of parenting confidence and efficacy The CSES has documented high internal consistency for the assessment of caregiving efficacy (Boothroyd & Evans, 1997). For the CSES, higher scores indicate greater perceived caregiving self-efficacy.
Prior technology use
Given prior research suggesting that prior technology use influences response to post-TBI Web-based interventions (Carey et al., 2008), parents completed a 17-item self-report questionnaire pertaining to their prior computer use at home and at work. For each item, parents indicated whether they had performed that action (e.g., “sent an e-mail message,” “downloaded information from the Internet,” or “had a ‘real time’ conversation using Internet chat or instant messaging”) during the past week, past month, or more than a month/never and provided categorical responses about the frequency of computer use over the past week. For the current analyses, responses were dichotomized based on parents that reported the least number of hours of computer use per week on a categorical measure of technology use. Parents who indicated that they either did not use a computer or used a computer less than 5 hr in the last week were categorized as nonfrequent users and those that reported using a computer 5 hr or more in the last week were categorized as frequent users.
Analyses
Univariate statistics were run to examine the distribution of the data and to test for normality. T tests and Fisher’s exact tests were used to compare the groups (CAPS vs. IRC) on baseline demographic, injury, and behavioral characteristics. Similar analyses were conducted to examine baseline differences between those who completed the study and those who dropped out. Correlations (Pearson’s, point biserial, and tetrachoric) were used to test the bivariate relationships between predictors, moderators, and outcome variables. Linear regression analyses were used to examine the main effects of treatment group on caregiver depression, global distress, and caregiving self-efficacy after controlling for baseline scores on the dependent variable of interest. Based on prior research, the following moderators of treatment effects were considered: caregiver income and education, race/ethnicity, and prior computer usage. Each model tested controlled for the baseline score on the dependent variable of interest before entering the main effect for the hypothesized moderator, the effect for group, and the group × moderator interaction. Education, income, and race/ethnicity were dichotomized in these analyses to minimize the effects of outliers. The models were then trimmed until a best fitting model was achieved. To trim the models, an arbitrary criterion was established such that factors with alpha levels higher than .50 were first trimmed followed by nonsignificant factors until only statistically significant factors remained. R2 change provided an estimate of the amount of variance explained by the predictors in the regression models. Cohen’s d was used to examine the effect sizes for post hoc comparisons of means.
Using an intent-to-treat framework, all participants with valid data from the baseline and 6-month follow-up assessments were included regardless of the number of treatment sessions completed. We then reran the analyses after removing participants who received less than half of the CAPS intervention (<4 sessions; n = 8) by the follow-up assessment to examine group differences among those who received the treatment program as planned. The steps of problem solving were introduced in Session 3 and thus participants who completed three or fewer sessions would not have the opportunity to successfully implement the problem-solving process around their identified goals. All analyses were done in SPSS© Version15.
Results
Participants
As detailed in the CONSORT flowchart (see Figure 1), a total of 308 children were invited to participate and 256 met eligibility criteria (52 invited participants either declined to participate or were deemed ineligible upon further screening). Of these, 132 children (52%) completed the informed consent process and baseline assessment. Sixty-five were assigned to CAPS and 67 to IRC. As indicated in Table 1, the groups were well matched with respect to demographic and injury characteristics with no significant differences between groups noted (all ps > 0.05).
Table 1.
Baseline Demographic and Injury Characteristics and Caregiver Self-Report Measures
| IRC (n = 67)
|
CAPS (n = 65)
|
||
|---|---|---|---|
| Mean (SD) | Mean (SD) | t/chi square | |
| Child’s age at injury | 14.67 (1.77) | 14.40 (1.68) | .91 |
| Time since injury (years) | .29 (.14) | .30 (.16) | −.59 |
| Grade at return | 8.83 (1.78) | 8.45 (1.68) | 1.22 |
| N/% Non-White | 14 (19%) | 13 (20%) | .01 |
| Lowest GCS Score | 10.03 (4.33) | 10.08 (4.85) | −.06 |
| Caregiver age at baseline | 42.84 (6.45) | 41.91 (7.35) | .77 |
| Median income | $65,912 (22.84) | $71,325 (32.19) | −1.11 |
| Caregiver education(% high school diploma or less) | 33 (49.2%) | 26 (40.0%) | 1.14 |
| N/% Married | 40 (59.7%) | 42 (64.6%) | .34 |
| N/% regular computer user | 41 (65.0) | 35 (61.4) | .17 |
Note. GCS = Glasgow Coma Scale; CES-D = Centers for Epidemiological Studies Depression Scale; CSES = Caregiver Self-Efficacy Scale; GSI = Global Severity Index. All participants = based on entire sample; At least four sessions = based on only CAPS participants that completed at least four sessions by the 6-month follow-up.
Three participants completed consent but failed to complete either the SCL-90 or CESD at baseline and an additional 11 participants participated in the 6-month follow-up, but failed to complete either the SCL-90 or CESD at the 6-month follow-up assessment for an attrition rate of 10.6%. Follow-up assessments were conducted an average of 6.96 and 6.74 months post baseline in the CAPS and IRC groups respectively. Eighty-six percent of primary caregivers (104/121) were mothers, 10% were fathers (12/121), and 4% (5/121) were grandparents or other relations, and this did not differ by treatment group.
Baseline sample characteristics are reported in Table 1. IRC caregivers reported significantly greater baseline symptoms on the GSI than CAPS caregivers, t(120) = 2.96, p = .004, with no other group differences in baseline measures noted. Sixty-one percent (n = 35) of the CAPS group reported regular computer usage as defined by 5 or more hr per week compared with 65% (n = 41) of the IRC group. Proportions suggested that 73.8% of CAPS versus 83.6% of the IRC caregivers reported having a computer in the home prior to treatment; and 61.4% of the CAPS versus 68.3% of the IRC caregivers rated their computer skills as below average or poor. Chi-square analyses failed to identify significant (p < .05) group differences in factors related to baseline computer use.
Time spent engaged in the intervention did not differ by group. Forty-three percent of parents in the CAPS group versus 48% in the IRC group reported spending less than 30 min per week on the Web site (either the CAPS Web site or other links) and 50% of the CAPS group versus 47% of the IRC group reported spending between 30 min and 2 hr per week. Participants in the CAPS group completed an average of 7.23 sessions by the 6-month follow-up (range 0–13) with all but eight (12%) completing four or more sessions.
Bivariate Correlations
Contrary to expectations, the tetrachoric correlations among demographic characteristics such as race, caregiver education, and computer use were small in magnitude and not statistically significant, ranging from −.18 between race and caregiver education to .15 between computer use and caregiver education. Associations between demographic factors and self-report measures of distress and caregiving efficacy using point biserial correlations were also nonsignificant, with coefficients ranging from .01 between CES-D and race, to .10 between CSES and race. Significant moderate to large correlations were observed among measures of caregiver distress (−.37 between CSES and GSI, −.38 between CSES and CES-D, and .67 between GSI and CES-D).
Changes in Depression and Global Distress
For the trimmed intent to treat regression models for the CES-D, all individual factors (income, race/ethnicity, and computer use) were eliminated due to nonsignificance. Results revealed a trend for greater improvements in the CAPS versus IRC group (p = .055). Follow-up analyses removing participants who completed fewer than four sessions of CAPS revealed a significant effect for group, F(1, 110) = 4.79, p = .03. Although the R2 change was small (.03), mean differences at follow-up, CAPS = 9.90 (8.36) versus IRC = 15.46 (11.75) indicated medium sized effects (Cohen’s d = −.52). See Table 2.
Table 2.
Means and Standard Deviations for Caregiver Self-Report Measures
| IRC: baseline Mean (SD) |
IRC: 6 months Mean (SD) |
CAPS: baseline Mean (SD) |
CAPS: 6 months Mean (SD) |
CAPS = > 4 sessions: baseline Mean (SD) |
CAPS = > 4 sessions: 6 months Mean (SD) |
|
|---|---|---|---|---|---|---|
| CES-D | 11.46 (8.76) | 15.46 (11.72) | 13.87 (9.78) | 10.98 (9.48) | 10.52 (8.10) | 9.90 (8.36)* |
| CSES | 87.16 (10.86) | 87.24 (10.76) | 90.16 (7.43) | 91.92 (7.20)* | 90.92 (7.43) | 92.36 (6.93)* |
| GSI | 58.14 (9.80) | 53.83 (12.12) | 52.45 (11.34) | 47.80 (12.26) | 51.27 (10.80) | 47.52 (11.40)* |
indicates group difference at .05 alpha level (p < .05).
For the trimmed regression models for the SCL-90 GSI score, all individual factors were again eliminated due to nonsignificance. Results revealed no significant differences between groups at follow-up in either the intent-to-treat or more restricted analyses after controlling for baseline (preintervention) scores. Post hoc analyses indicated comparable, and statistically significant, reductions in global distress in both the CAPS and IRC group (M CAPS = 3.29; M IRC = 3.64; p = .007 for both analyses), suggesting that both treatment conditions were associated with reductions in caregiver distress.
Moderators of Treatment Response
When considering changes in caregiving self-efficacy, income and race/ethnicity were trimmed from the models due to nonsignificance. Results revealed a significant interaction between group and computer use, controlling for group and baseline (preintervention) CSES scores. Follow-up analyses revealed that, among non-frequent computer users, CAPS parents reported significantly higher levels of caregiver efficacy than did IRC parents at the 6-month follow-up, F(41) = 7.15, p = .01. See Figures 2a and 2b and Table 3. The corresponding effect size was moderate (Cohen’s d = .51). Conversely, among frequent computer users, there were no group differences in caregiver self-efficacy at follow-up, F(74) = .05, p = .82, and neither CAPS nor IRC evidenced changes in CSES scores from baseline to the 6-month follow-up.
Figure 2.
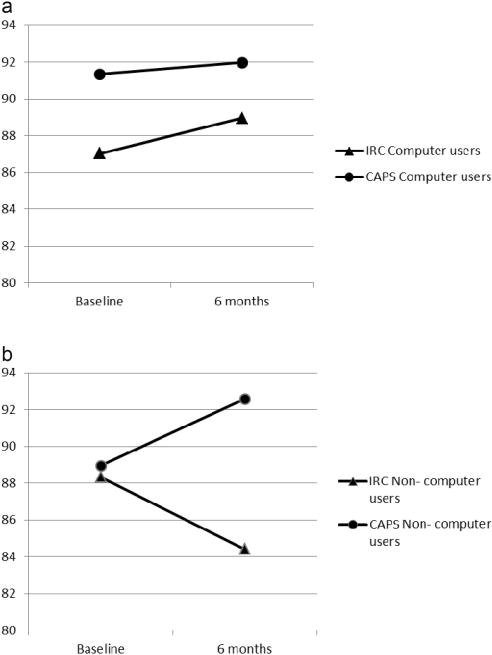
a. Mean baseline and 6-month Caregiver Self-Efficacy Scale (CSES) scores of frequent computer users. b. Mean baseline and 6-month Caregiver Self-Efficacy Scale (CSES) scores of nonfrequent computer users.
Table 3.
Linear Regression Examining Relationship of Individual Factors to Postintervention Caregiver Outcomes
| Variable | β | SE | Std β | T | p |
|---|---|---|---|---|---|
| CES-D as dependent variable | |||||
| Baseline symptoms | .66 | .08 | .56 | 7.48 | <.001 |
| Group individual factors | −3.19 | 1.65 | −.14 | −1.92 | .05 |
| None | — | — | — | — | — |
| R2 | .35 | ||||
|
| |||||
| GSI as dependent variable | |||||
| Baseline symptoms | .78 | .07 | .71 | 10.13 | <.001 |
| Group individual factors | −.30 | 1.72 | −.01 | −.17 | .86 |
| None | — | — | — | — | — |
| R2 | .51 | ||||
|
| |||||
| CSES as dependent variable | |||||
| Baseline symptoms | .58 | .07 | .59 | 8.04 | <.001 |
| Group individual factors | 6.79 | 2.25 | .36 | 3.01 | .003 |
| Computer use | 4.50 | 1.97 | .23 | 2.28 | .02 |
| Group × computer use | −6.32 | 2.82 | −.31 | −2.24 | .02 |
| R2 | .42 | ||||
Note. CES-D = Center for Epidemiologic Studies Depression Scale; GSI = Global Severity Index; CSES = Caregiver Self-Efficacy Scale. For group, IRC was the reference category. Income, race/ethnicity, and computer use considered as individual factors. Table 3 reports results of final models with nonsignificant factors eliminated.
Contrary to expectations and prior research, caregiver education and race/ethnicity did not moderate treatment response on any of the parent outcomes assessed. Additionally, prior computer use did not moderate the efficacy of CAPS in reducing caregiver depression and distress.
Regressions models were repeated using a more restricted analysis that excluded participants that completed <4 sessions. Similar to the findings in the intent to treat model, a significant interaction was found between group and computer use when considering CSES as the dependent measure, controlling for group and baseline CSES scores (β = 5.62, t = 1.96, p = .05). Parents who were nonfrequent computer users again evidenced higher self-efficacy than did those in the IRC. Also similar to the intent to treat analyses, caregiver education and race/ethnicity did not moderate treatment response on any of the parent outcomes assessed and prior computer use did not moderate the efficacy of CAPS in reducing caregiver depression and distress.
Discussion
We report findings from a large clinical trial regarding the efficacy of online family problem-solving therapy in reducing caregiver depression and distress and promoting caregiver efficacy during the initial 6–12 months following TBI in adolescents. The findings extend the results of previous smaller and less carefully controlled studies (e.g., Wade et al., 2006) while elucidating the evolving role of prior technology use as a moderator of treatment response. There was a trend such that the CAPS intervention was associated with borderline, but nonsignificant (p = .055) reductions in depressive symptoms compared with access to TBI Internet resources alone. When considering only those who completed at least half of the CAPS sessions, these group differences became significant. Both CAPS and IRC were associated with significant reductions in caregiver distress, however, CAPS was not more effective than IRC in this regard. Prior computer usage moderated treatment-related improvements in caregiver self-efficacy with parents who had limited prior computer usage reporting the greatest gains in caregiving efficacy following CAPS. As considered in greater detail below, these findings extend our understanding of the efficacy of Web-based problem solving for families of adolescents during the initial months postinjury.
Similar to previous studies with smaller and more heterogeneous samples, caregivers in the CAPS group reported greater reductions in depressive symptoms than did those in the IRC group (Wade et al., 2006). However, significant group differences were only found when analyses were limited to those who completed at least half of the CAPS intervention. The period immediately following childhood TBI is a time of elevated family burden and concomitant caregiver distress (Wade et al., 1998; Wade, Taylor, Drotar, Stancin, Yeates, & Minich, 2002). Participation in a supportive program, such as CAPS, may help to minimize post-TBI caregiver distress, including symptoms of depression, and may mitigate the development of problems within the family that may arise with greater time since injury. Contrary to previous studies with older children and adolescents (Wade et al., 2012), treatment efficacy was not moderated by socioeconomic status. Further, we failed to find differences between the CAPS and IRC groups in global distress as assessed by the SCL-90, although both groups reported significant improvements. The failure to find group differences on the SCL-90 may in part be attributable to a significant group difference in global distress at baseline. Although baseline distress was controlled in analysis, average distress in the CAPS group at baseline fell within the normal range making it less likely that the CAPS intervention would result in significant improvements.
Prior research, although limited (Carey et al., 2008), suggests that individuals with minimal prior computer experience would be less likely to benefit from Web-based problem-solving therapy. However, results from the current study indicate that adults who are infrequent technology-users may experience greater increases in caregiver efficacy if their experience with technology is scaffolded by therapist support and guidance. Interestingly, in the IRC group, without such support, parents who were not frequent computer users reported declines in caregiving efficacy despite the fact that they accessed information about brain injury. In explaining this finding, it may be that when noncomputer users are offered computer access without the support and scaffolding provided by the therapist to use the technology, general feelings of self-efficacy and confidence may decrease, including caregiving efficacy. Thus, the present results yield a more nuanced understanding of the potential role of prior technology experience in treatment efficacy. Contrary to earlier studies, the findings suggest that parents with limited prior computer experience may be equally or more likely to benefit from therapist-guided, Web-based interventions.
Caregiver burden and distress peak during the initial months following TBI. Within the CAPS problem-solving framework, parents were provided with strategies for stress management, self-care, and cognitive reframing. Problem-solving discussions could target managing emotions more effectively and coping with guilt and grief (emotion-focused coping) as well as more active strategies. Because parents and children identified the goals that were most salient for the family, the intervention was individualized to the family’s needs and context. Although problem-solving therapy has been effectively used to treat depression in numerous populations (D’Zurilla & Nezu, 2006), caregiver depression and burden were not the primary or sole targets of intervention in the current study. As such, greater effects may have been demonstrated if the therapy focused solely on caregiver issues and goals rather than teen and family concerns.
A lingering question may be whether the statistically significant changes in caregiver functioning here reported are clinically significant or meaningful. Interpretation of clinical significance is complicated as the current cohort was not experiencing clinically significant depression or distress at baseline, thus precluding examination of clinically significant changes in symptomatology. However, the chronic illness and quality of life literatures suggest that improvements or differences of 0.5 standard deviation can be considered to be minimally important (i.e., detectable by the patient; Norman, Sloan, & Wyrwich, 2003). Using this definition, both the CAPS and IRC groups reported minimally important change on the GSI and group differences between the CAPS and IRC groups on the CES-D would be deemed minimally important. Likewise, differences in caregiver self-efficacy in the low-computer usage group likely reflected clinically meaningful differences. However, it is worth noting that a sample with significant clinical elevations at baseline may have demonstrated more pronounced clinical improvements over time.
Several limitations of the current study should be noted. The groups were well-matched on most demographic, injury, and baseline characteristics; however, relatively low levels of distress on the SCL-90 GSI in CAPS group at baseline may have created floor effects Additionally, although the treatment conditions were equated for access to reliable information and resources regarding TBI, including Web sites regarding problem-solving strategies and stress management, the groups were not equated for therapist attention. Therefore, although we can tentatively conclude that CAPS is superior to access to Internet resources alone in reducing caregiver depressive symptomatology following TBI, we cannot conclude that it is superior to other forms of treatment affording therapist support. Reliance on self-report measures of parent outcomes is a further limitation. Additionally, as reported in Figure 1, a large proportion (57.1%) of potential participants that were assessed for eligibility were either deemed ineligible or declined to participate, potentially limiting generalizability of the current findings. The exclusionary criteria that the family residence must be in an area with high-speed Internet access may result in families living in rural areas being underrepresented and the criteria that English must be the primary language spoken in the home potentially results in exclusion of members of diverse populations. Specifically, potential participants that decline participation were more likely to be non-White and have sustained less severe injuries than participants. It is also notable that the median family income of the obtained sample is above the national median despite substantial variability in income levels. These limitations in recruitment and generalizability should be considered when interpreting the current results. Additionally, although the intent-to-treat model suggested that greater sessions completed was associated with greater improvements in caregiver depression, it is notable that the presence of a subset of participants that did not complete the entire course of treatment likely reduced the strength of the study’s design and limited our ability to detect improvements in caregiver outcomes that result following the CAPS intervention. Finally, the approach to assessing treatment fidelity to the CAPS intervention may be vulnerable to bias on the part of the therapist and untrained caregivers may be unable to make reliable evaluations about treatment fidelity. Future studies may wish to use other methods for assessing treatment fidelity, such as an expert independent rater.
This study provides limited support for the efficacy of CAPS, a Web-based family problem-solving program, in reducing parent depressive symptoms during the initial months following moderate to severe TBI in adolescents. The evidence also supports the potential utility of counselor-supported Web-based interventions for individuals with limited computer expertise for increasing caregiver self-efficacy. The current findings are consistent with limited research in other populations of caregivers of children with disabilities that have demonstrated that telehealth interventions correspond with positive changes in caregiver stress (Rivera, Shewchuk, & Elliott, 2003; Glueckauf & Noel, 2011) and self-efficacy (Glueckauf & Noel, 2011). In view of prior pediatric TBI research that has suggested that families with the greatest vulnerability for negative post-TBI sequelae, such as those with more severe TBI and/or greater socioeconomic disadvantage, often evidence the greatest benefit from post-TBI Web-based interventions (Wade et al., 2006; Wade et al., 2010), the current results indicate that families with limited prior computer use, who may be expected to be vulnerable to nonadherence to Web-based interventions (Carey et al., 2008), evidence the greatest benefit of the CAPS intervention. Families who may be candidates for Web-based interventions, such as those living in rural areas, may be expected to benefit from Web-based interventions that offer support for technology use. However, additional research is needed to determine the optimal timing and intensity of Web-based problem solving as well as the effectiveness of CAPS versus other forms of intervention involving therapist-directed support.
Impact.
Web-based interventions may have the ability to provide individualized and personally relevant mental health services to individuals who might otherwise be underserved, such as those living in rural communities. The current study adds to the literature on Web-based interventions by examining the efficacy of the family problem-solving therapy in a large, well-characterized cohort of youth with TBI.
Both Web-based problem-solving therapy and access to Web-based resources are associated with reductions in global caregiver distress following TBI. However, online problem-solving therapy may be superior for symptoms of depression and caregiver self-efficacy.
This study contributes to the current literature by examining moderators of treatment efficacy, thus allowing providers to tailor treatments based on individual characteristics. These findings indicate that familiarity with computer use moderated treatment outcomes with caregivers with less frequent preintervention computer use evidencing the greatest gains in pre- to postintervention caregiver self-efficacy.
Acknowledgments
This work was supported in part by (a) NIH Grant R01-MH073764 from the National Institute of Mental Health and (b) a grant from the Colorado Traumatic Brain Injury Trust Fund Research Program, Colorado Department of Human Services, Division of Vocational Rehabilitation, Traumatic Brain Injury Program. The authors wish to acknowledge the contributions of Kendra McMullen, Robert Blaha, Elizabeth Hagesfeld, Michelle Jacobs, Daniel Maier, Mary Ann Toth, and Nina Fox in data collection and entry, Jason Stock in data management, and John Stullenberger in Web site support. We would also like to acknowledge the contributions of the therapists JoAnne Carey, PsyD, Britt Nielsen, PsyD, and Brad Jackson, PhD.
Contributor Information
Shari L. Wade, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio and University of Cincinnati College of Medicine
Christine L. Karver, University of Cincinnati and Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio
H. Gerry Taylor, Case Western Reserve University, Rainbow Babies & Children’s Hospital, Cleveland, Ohio, and University Hospitals Case, Medical Center, Cleveland, Ohio.
Amy Cassedy, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio.
Terry Stancin, Case Western Reserve University and MetroHealth Medical Center, Cleveland, Ohio.
Michael W. Kirkwood, Children’s Hospital Colorado, Aurora, Colorado and University of Colorado School of Medicine
Tanya Maines Brown, Mayo Clinic, Rochester, Minnesota.
References
- Aitken ME, McCarthy ML, Slomine BS, Ding R, Durbin DR, Jaffe KM, CHAT Study Group Family burden after traumatic brain injury in children. Pediatrics. 2009;123:199–206. doi: 10.1542/peds.2008-0607. [DOI] [PubMed] [Google Scholar]
- Boothroyd RA, Evans ME. Preliminary manual for the caregiver self-efficacy scale. Tampa, FL: Department of Mental Health Law and Policy, University of South Florida; 1997. [Google Scholar]
- Carey JC, Wade SL, Wolfe CR. Lessons learned: The effect of prior technology use on web-based interventions. CyberPsychology & Behavior. 2008;11:188–195. doi: 10.1089/cpb.2007.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Lazarus L. SCL-90-R, brief symptom inventory, and matching clinical rating scales. In: Maruish M, editor. The use of psychological testing for treatment planning and outcome assessment. Hillsdale, NJ: Erlbaum; 1994. pp. 217–248. [Google Scholar]
- D’Zurilla TJ, Nezu AM. Problem-solving therapies. In: Dobson KS, editor. Handbook of cognitive– behavioral therapies. 3. New York, NY: Guilford Press; 2006. pp. 211–245. [Google Scholar]
- Gan C, Gargaro J, Kreutzer J, Boschen K, Wright V. Development and preliminary evaluation of a structured family system intervention for adolescents with brain injury and their families. Brain Injury. 2010;24:651–663. doi: 10.3109/02699051003692142. [DOI] [PubMed] [Google Scholar]
- Glueckauf RL, Noel LT. Telehealth and family caregiving: Developments in research, education, and health care policy. In: Toseland RW, Haigler DH, Monahan DJ, editors. Education and support programs for caregivers: Research, practice, policy. New York, NY: Springer; 2011. pp. 85–105. [Google Scholar]
- Jackson LA, Zhao Y, Kolenic A, Fitzgerald HF, Harold R, von Eye A. Race, gender, and information technology use: The new digital divide. CyberPsychology & Behavior. 2008;11:437–442. doi: 10.1089/cpb.2007.0157. [DOI] [PubMed] [Google Scholar]
- Kreutzer JS, Stejskal T, Ketchum J, Marwitz J, Taylor L, Menzel J. A preliminary investigation of the Brain Injury Family Intervention: Impact on family members. Brain Injury. 2009;23:535–547. doi: 10.1080/02699050902926291. [DOI] [PubMed] [Google Scholar]
- Lorence DP, Park H, Fox S. Racial disparities in health information access: Reliance of the digital divide. Journal of Medical Systems. 2006;30:241–249. doi: 10.1007/s10916-005-9003-y. [DOI] [PubMed] [Google Scholar]
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of change in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care. 2003;41:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Rivera PA, Elliott TR, Berry J, Grant J. Problem-solving training for family caregivers of persons with traumatic brain injuries: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2008;89:931–941. doi: 10.1016/j.apmr.2007.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera PA, Shewchuk R, Elliott TR. Project FOCUS: Using videophones to provide problem-solving training to family caregivers of persons with spinal cord injuries. Topics in Spinal Cord Injury Rehabilitation. 2003;9:53–62. doi: 10.1310/G82F-BR2R-T69L-3QX8. [DOI] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Burant C. Bidirectional child-family influences on outcomes of traumatic brain injury in children. Journal of the International Neuropsychological Society. 2001;7:755–767. doi: 10.1017/S1355617701766118. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037/0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Wade SL, Borawski EA, Taylor HG, Drotar D, Yeates KO, Stancin T. The relationship of caregiver coping to family outcomes during the initial year following pediatric traumatic brain injury. Journal of Consulting and Clinical Psychology. 2001;69:406–415. doi: 10.1037/0022-006X.69.3.406. [DOI] [PubMed] [Google Scholar]
- Wade SL, Carey J, Wolfe CR. An online family intervention to reduce parental distress following pediatric brain injury. Journal of Consulting and Clinical Psychology. 2006;74:445–454. doi: 10.1037/0022-006X.74.3.445. [DOI] [PubMed] [Google Scholar]
- Wade SL, Michaud L, Brown TM. Putting the pieces together: Preliminary efficacy of a family problem-solving intervention for children with traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2006;21:57–67. doi: 10.1097/00001199-200601000-00006. [DOI] [PubMed] [Google Scholar]
- Wade SL, Stancin T, Taylor HG, Drotar D, Yeates KO, Minich NM. Interpersonal stressors and resources as predictors of parental adaptation following pediatric traumatic injury. Journal of Consulting and Clinical Psychology. 2004;72:776–784. doi: 10.1037/0022-006X.72.5.776. [DOI] [PubMed] [Google Scholar]
- Wade SL, Taylor HG, Drotar D, Stancin T, Yeates KO. Family burden and adaptation during the initial year after traumatic brain injury in children. Pediatrics. 1998;102:110–116. doi: 10.1542/peds.102.1.110. [DOI] [PubMed] [Google Scholar]
- Wade SL, Taylor HG, Drotar D, Stancin T, Yeates KO, Minich MA. A prospective study of long-term caregiver and family adaptation following brain injury in children. Journal of Head Trauma Rehabilitation. 2002;17:96–111. doi: 10.1097/00001199-200204000-00003. [DOI] [PubMed] [Google Scholar]
- Wade SL, Walz NC, Carey J, McMullen KM, Cass J, Mark E, Yeates KO. A randomized trial of teen online problem-solving: Efficacy in improving caregiver outcomes after brain injury. Health Psychology. 2012;31:767–776. doi: 10.1037/a0028440. [DOI] [PubMed] [Google Scholar]
- Wade SL, Walz NC, Carey JC, Williams KM. Preliminary efficacy of a web-based family problem-solving treatment program for adolescents with traumatic brain injury. Journal of Head Trauma Rehabilitation. 2008;23(6):369–377. doi: 10.1097/01.HTR.0000341432.67251.48. [DOI] [PubMed] [Google Scholar]
- Wade SL, Walz NC, Carey J, Williams KM, Cass J, Herren L, Mark E, Yeates KO. A randomized trial of Teen Online Problem Solving for improving execution function deficits following pediatric traumatic brain injury. Journal of Head Trauma Rehabilitation. 2010;25(6):409–415. doi: 10.1097/HTR.0b013e3181fb900d. [DOI] [PubMed] [Google Scholar]
- Wade SL, Stancin T, Kirkwood MW, Brown TM, McMullen KM, Taylor HG. Counselor-assisted problem solving (CAPS) improves behavioral outcomes in older adolescents with complicated mild to severe TBI. Journal of Head Trauma Rehabilitation. :406–415. doi: 10.1097/HTR.0b013e31828f9fe8. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Woodrome SE, Wade SL, Stancin T, Drotar D. Race as a moderator of parent and family outcomes following pediatric traumatic brain injury. Journal of Pediatric Psychology. 2002;27:393–403. doi: 10.1093/jpepsy/27.4.393. [DOI] [PubMed] [Google Scholar]


