Abstract
Internet-based group contingencies have been shown to promote brief periods of abstinence from cigarette smoking. Under a group contingency, small teams of smokers must collectively meet abstinence goals to receive monetary consequences. The present study investigated two arrangements, one in which all team members had to meet group treatment goals to receive monetary consequences (Full Group), and one in which team members had to meet some group goals and some individual goals to receive these consequences (Mixed Group). Mōtiv8 Systems, an Internet-based remote monitoring platform, was used to collect video-recorded breath carbon monoxide (CO) samples. All team members could communicate with each other via an online discussion forum. During baseline conditions, only 3.3% of CO samples were negative for smoking, which suggests that self-monitoring and access to the online discussion forum were insufficient to initiate abstinence. When the group contingencies were instituted 41.3% of CO samples were negative. There were no statistically significant differences between the two arrangements in the percentage of negative CO samples or point prevalence at the end of treatment or at the 3-month follow-up. Participants posted an average of 25 comments on the discussion forum, most of which were rated as positive by independent observers. The mean cost of vouchers per participant was lower in the Full Group ($33) relative to the Mixed group ($190). The present results replicate and extend previous findings on group contingencies to promote abstinence and social support.
Keywords: Cigarette smoking, contingency management, mHealth, technology
Technology-based contingency management (CM) interventions have been evolving rapidly (Alessi & Petry, 2013; Barnett, Tidey, Murphy, Swift, & Colby, 2011; Dallery, Kurti, & Erb, 2014; Dougherty et al., 2014). Under technology-based CM interventions for smoking cessation, individuals transmit videos of themselves providing breath carbon monoxide (CO) samples into a handheld CO meter, and receive monetary consequences based on evidence of abstinence. Early versions of the intervention involved emailing videos to researchers (Dallery & Glenn, 2005), which entailed inevitable delays to reinforcement based on when emails were viewed by researchers and when feedback and reinforcers were provided. More recent iterations have involved a user-friendly website that enabled automated video capture and immediate reinforcement (Dallery, Raiff, & Grabinski, 2013), and access to smokers in wider geographical areas than in early versions (e.g., smokers in rural Appalachia, Stoops et al., 2009). In addition, Hertzberg et al. (2013) successfully used mobile-phone-based CM, as opposed to Internet-based CM, to promote smoking cessation in smokers diagnosed with post-traumatic stress disorder.
Across technology-based platforms and diverse populations, technology-based CM has been efficacious in initiating abstinence (for a review see Dallery et al., 2014). In a randomized clinical trial, Dallery et al. (2013) found that Internet-based CM promoted higher rates of abstinence (66.7% negative COs) than a control group (25% negative COs) during treatment. These results were consistent with the results of previous studies, regardless of whether comparisons were made within-subjects (Dallery, Glenn, & Raiff, 2007; Dallery & Glenn, 2005) or between-groups (Stoops et al., 2009). In addition to efficacy, Raiff, Jarvis, Turturici, and Dallery (2013) evaluated the social validity of Internet-based CM and found high levels of acceptability among smokers, non-smokers, and health-care professionals (Foster & Mash, 1999).
In some respects, the evolution of technology-based CM has been propelled by technology. For example, early applications of the intervention were developed before the advent of smartphones and social media platforms (Dallery & Glenn, 2005), and now video capture is possible via smartphones and wireless internet connectivity (Hertzberg et al., 2013). Technology will continue to inspire more accessible and cost-effective variations of CM, particularly as mobile-phone based methods are integrated with more affordable breath CO monitors (Meredith et al., 2014). In other respects, however, the progression of the intervention has been driven by novel applications of behavioral technology (Dallery et al., 2014). For instance, Dallery, Meredith, and Glenn (2008) evaluated whether a deposit contract procedure, in which individuals could recoup a deposit based on evidence of abstinence, could reduce costs associated with CM relative to standard, earnings only CM. The authors found that relative to an earnings-only CM group, the deposit group showed similar rates of abstinence, but the costs associated with monetary consequences were lower. In fact, a small surplus accrued in the deposit group. This investigation was a small, pilot study, and thus these results require replication in a larger and more diverse sample.
Another example of behavioral technology is a group contingency (Gresham & Gresham, 1982; Kirby, Kerwin, Carpenedo, Rosenwasser, & Gardner, 2008; Williamson, Williamson, Watkins, & Hughes, 1992). A group contingency is arranged when consequences (e.g., vouchers exchangeable for goods and services) are delivered to each member of a group only if all members of the group meet a specified criterion. Meredith, Grabinski, and Dallery (2011) used an Internet-based CM model and incorporated group contingencies, where small groups or “teams” (n≈3) of smokers were required to achieve cessation goals to receive desirable consequences. Participants provided and/or received encouragement, feedback, and support via a discussion forum integrated into the Mōtiv8 architecture. Using a multiple baseline design, Meredith et al. found that fewer than 1% of CO samples submitted during baseline were negative for smoking, compared to 57% submitted during the treatment phase. In addition, 65% of participants' comments on the online peer support forum were rated as positive by independent observers.
Meredith et al. (2011) used a so-called mixed contingency, in which some consequences depended only on individual performance, and some consequences depended on group performance. Another variation, called a full group contingency, requires all group members to achieve their goals to receive consequences. There are reasons to believe that either one of these arrangements could produce greater effectiveness and/or acceptability. For example, because of the greater stringency of the full group contingency, participants may rate it as less acceptable. However, this more stringent feature may also produce higher rates of cessation by virtue of more social encouragement and support.
The present study used an Internet-based monitoring system, called Mōtiv8, to verify smoking status, and group CM to promote smoking abstinence. Our primary goal was to evaluate rates of smoking abstinence between a mixed and a full group contingency, both during treatment and at 3-month follow up. Secondary goals included evaluating the frequency and nature of social interactions on the discussion forum, the cost of delivering group CM, and quantitative and qualitative measures of the acceptability of the interventions.
Method
Participants
Participants were 43 healthy smokers recruited from Gainesville, FL and surrounding communities through print media, radio announcements, television advertisements, and word of mouth. Interested applicants were screened over the phone for basic qualifying criteria. To qualify for an in-person intake, applicants had to be between 18 and 60 years of age, have Internet access from their home, smoke ≥ 10 cigarettes per day, report a minimum 2-year smoking history, and express a desire to quit smoking [i.e., answer affirmatively to the question, “Do you want to quit smoking?” (Perkins, Stitzer, & Lerman, 2006)].
During intake, applicants provided informed consent and completed several questionnaires, including a psychosocial history survey, which contained questions about demographics, smoking history, drug use, and physical and psychological health. Applicants were confirmed smokers if they presented with a breath CO ≥ 10 ppm. Urine samples were collected and analyzed for the presence of cocaine, benzodiazepines, and opiates. Applicants were excluded from study participation if they showed evidence of illicit drug use, smoked marijuana more than twice per month, resided with another smoker who smoked inside the residence, or reported a history of physical or psychological illness that, in our judgment, would interfere with study participation. In addition, women were disqualified if they were pregnant or breastfeeding. The University of Florida Institutional Review Board approved all study procedures.
Materials and Measures
Data collection and treatment delivery were enabled by Mōtiv8 Systems software (Dallery, Raiff, et al., 2013) and the Mōtiv8 Group Support Forum (Meredith & Dallery, 2013; Meredith et al., 2011). CO meters (Bedfont piCO+ Smokerlyzer®) were loaned to each participant. Researchers calibrated the CO meters every 6 months according to manufacturer recommendations. Web cameras (Creative Live!® Cam) and laptops (Asus® Eee PC) were loaned to those participants who needed them; however, most participants used their own webcams and computers. Copies of participants’ drivers licenses were obtained, and participants were asked to sign an off-campus property contract stating that they would return all equipment. Participants were also provided a study instruction manual that included a detailed description of study procedures. Participants were required to pass a quiz demonstrating that they read and understood all study procedures (Silverman, Chutuape, Bigelow, & Stitzer, 1999).
At intake, the Fagerström Test for Nicotine Dependence (FTND) was administered. The FTND is a 6-item questionnaire that assesses nicotine dependence with a scale ranging from 0–10 (higher scores representing greater dependence; (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1989). In addition, participants completed the Need to Belong (NTB) scale (Mellor, Stokes, Firth, Hayashi, & Cummins, 2008). This 10-item questionnaire with a 5-point Likert scale assessed participants’ need to belong to social groups. Last, participants completed three items on a visual analog scale (VAS; range 0–100, higher scores indicating greater motivation) to assess readiness to quit smoking, confidence in ability to quit, and importance of quitting (Miller & Rollnick, 2002).
At the end of treatment and at the 3-month follow-up, participants completed a behavior change inventory, which included questions about previous 7-day smoking and other behavior patterns (e.g., “Have you started taking any new medications?”). Participants also completed a treatment acceptability questionnaire which included responses on a VAS (range 0–100; higher scores indicating greater acceptability) and several open-ended questions (e.g., “What suggestions do you have for changes to the intervention?”).
Set-up
Researchers demonstrated how to use the Mōtiv8 Systems software, including how to submit a video breath CO sample and how to communicate with teammates through the Mōtiv8 Group Support Forum. Participants were then required to practice both of these tasks in the presence of the researchers.
Participants were divided into small groups or “teams.” They were assigned to their teams based on the order in which they qualified to participate in the study. Participants assigned to the same team were required to begin the study on the same day. Thus, relatively small team sizes – three or four participants - were used to minimize the delay between study qualification and the onset of experimental conditions.
Participants were asked if they knew anyone else who was participating in the study. A policy was in place to assign familiar participants to different teams. This policy was developed to minimize the potential confounding influence of external communications on experimental procedures.
Participants were instructed to avoid ambient sources of CO (e.g., second-hand smoke) and to avoid smoking other substances (e.g., marijuana) that could elevate breath CO. Participants were also instructed to notify researchers if they wished to make a purchase with their vouchers during the study; however, most participants did not make any purchases until after they completed the study.
Mōtiv8 Systems and CO Monitoring Procedure
Participants were instructed to submit video samples of breath CO measurements twice daily (minimum 8 h inter-sample interval) via the Mōtiv8 website. Participants logged into the secure website using usernames and passwords that were assigned to them at set-up. Each participant had a personalized homepage where they could view their voucher account history (a record of any vouchers earned or spent during the study) and their quantitative progress graph (a graphical representation of breath CO levels submitted over the course of the study). In addition, participants could click on a link that would direct them to their teammates’ quantitative progress graphs. This feature allowed participants to stay informed of their teammates’ smoking status, so that they could provide appropriate social consequences (e.g., praise or encouragement) via the Mōtiv8 Group Support Forum contingent upon their teammates’ performance.
A “Post Video” button was also available on participants’ homepages. The button was only active if participants had not yet submitted two videos that day and if 8 h had passed since their last video submission. When participants were ready to submit a sample, they clicked on the Post Video button and followed simple on-screen instructions on how to turn on their web camera, measure their breath CO with their CO meter, show the result to the camera, and enter the CO level into the website. Mōtiv8 Systems immediately notified participants whether they met their goals or earned any vouchers, and the website informed them how many vouchers would be available contingent upon their next negative sample submission (see Dallery et al., 2013 for a more detailed description of the video submission process). Participants were notified during set-up that attempts to falsify samples were easily detected and would lead to dismissal from the study. Researchers reviewed videos daily to ensure CO sampling fidelity. In the event of deviations from sampling fidelity (e.g., breath exhalation into the monitor was not visible), researchers provided additional instructions about ensuring that all elements of the CO sampling procedure were present in the video.
Online Peer Support Forum
Immediately following video submissions, the website directed participants to the Mōtiv8 Group Support Forum. Participants could also access the forum at any time by clicking on a link located on their Mōtiv8 Systems homepage. On the Mōtiv8 Group Support Forum, participants could post comments or read comments posted by their teammates or by a counselor who served as the forum moderator. Every member of the team and the forum moderator could view each post. However, participants only had access to their team’s discussion thread. Participants were instructed to use their usernames, not their real names, on the forum. Participants also received the following guidelines for communicating via the Mōtiv8 Group Support Forum: “Make sure your posts are supportive in nature. Posts that are discouraging or offensive will not be allowed. Keep in mind you want to help encourage other group members to quit smoking. You should congratulate them when they make progress toward this goal!”
The role of the forum moderator was to facilitate communication and provide praise for submitting breath CO samples indicative of smoking reduction or cessation (Meredith et al., 2011). Across teams, moderator posts were not identical, but they were similar in tone and content.
Experimental Design
Teams were randomly assigned to either a full group contingency group (i.e., “Full Group”) or a mixed group contingency group (i.e., “Mixed Group”). The effects of each contingency were evaluated within subjects using a non-concurrent multiple-baseline design (Barlow, Nock, & Hersen, 2008). The maximum potential earnings was $530 in both groups.
Full Group
Baseline
As required by a multiple-baseline design, the duration of this condition varied between 2 and 6 days across teams. Thus, some teams experienced a 2-day baseline, some experienced a 3-day baseline, and so on, up to 6 days. Baseline duration was randomly determined for each team so that each experimental group would contain teams with baseline durations of 2, 3, 4, 5, and 6 days. Participants submitted video breath CO samples twice daily. No vouchers were available during baseline. However, participants had access to all other features of the intervention (e.g., self-monitoring and feedback via the Mōtiv8 Systems website and Mōtiv8 Group Support Forum).
Tapering
Participants continued to submit video samples twice daily during this 4-day condition. Participants were instructed to gradually reduce their smoking to meet their tapering goals, which were breath CO goals displayed on their quantitative progress graphs. These goals were tailored to each participant, such that the first tapering goal was lower than the participant’s mean baseline breath CO, and each of the seven remaining tapering goals was progressively lower than the previous goal. The second tapering goal on the last day of tapering (i.e., the quit date) was ≤ 4 ppm (the abstinence threshold) for all participants. If every member of a team submitted a breath CO sample less than or equal to their respective tapering goals for a given sample, then they each received a $3.00 voucher. However, if one or more teammates failed to submit a sample or submitted a sample that exceeded his or her tapering goal, then none of the team members received a voucher for that sample.
Abstinence Induction
Participants continued to submit video samples twice daily during this 21-day condition. During abstinence induction, participants were informed that they would need to be abstinent to earn vouchers contingent upon breath CO levels ≤ 4 ppm (i.e., negative samples). For each of the 42 scheduled samples, if all members of a team submitted a negative sample, then they each earned a voucher. An escalating schedule of voucher delivery was used to promote continuous periods of abstinence, such that the first voucher awarded contingent upon team abstinence was $3.00, the second was $3.25, the third was $3.50, and so on (Roll, Higgins, & Badger, 1996). Participants also earned a $5.00 bonus voucher each time every member of the team submitted three consecutive negative samples. If one or more teammates missed a sample or submitted a positive sample, then no one on that team earned a voucher, and the value of the next available voucher was reset to the initial amount (i.e., $3.00; Roll & Higgins, 2000). If, following a reset, all members of a team submitted two consecutive negative samples, then the schedule of voucher earnings returned to the value of the voucher that preceded the reset.
Thinning
During this 21-day condition, participants submitted video samples only once per day. The escalating schedule of reinforcement that began during the abstinence induction phase continued into thinning. However, the frequency of voucher delivery was thinned to twice per week. Two days per week were randomly selected, and teammates were awarded vouchers on each of these days if every member of a team submitted a negative sample on that day (even if positive or missed samples occurred on intervening days).
Mixed Group
The Mixed Group intervention was similar to the Full Group intervention. The only difference was in how the vouchers were awarded during the tapering, abstinence induction, and thinning conditions.
Baseline
This condition was identical to the Full Group baseline condition. However, in the Mixed Group, two teams experienced 6-day baseline durations. Researchers extended the baseline from 4 days to 6 days for one team in the Mixed Group because the additional time was needed to set-up one of the team members.
Tapering
Vouchers were contingent upon individual performance, rather than team performance. Each time participants submitted breath CO samples less than or equal to their tapering goals, they received a $3.00 voucher.
Abstinence Induction
Vouchers were available on the same escalating schedule of reinforcement that was used in the Full Group. All vouchers, except the bonus vouchers, were contingent upon individual abstinence. The $5.00 bonus vouchers were awarded just as they were in the Full Group—they were contingent upon continuous group abstinence over three consecutive samples.
Thinning
The same thinning schedule that was used in the Full Group was used in the Mixed Group. However, in the Mixed Group, vouchers were available based on individual performance instead of group performance.
Counseling
At set-up, at the end of abstinence induction, and at the end of thinning, counselors trained by a Licensed Psychologist (JD) provided in-person behavioral counseling. The counseling protocol was based on Public Health Service recommendations (Fiore, 2000) and the National Cancer Institute’s guide to quitting smoking, Clearing the Air (http://smokefree.gov/sites/default/files/pdf/clearing-the-air-accessible.pdf). Participants were provided a copy of the Clearing the Air booklet. Counselors were supportive and non-judgmental. They discussed reasons why participants wanted to quit smoking, and they helped participants identify and strengthen tactics to promote smoking reduction and cessation. If a participant achieved abstinence, then strategies to maintain abstinence and avoid lapse were discussed. Counselors were not blind to study conditions. Each counselor served as the forum moderator on the Mōtiv8 Group Support Forum for the same teams that they counseled.
Follow-up
Three months after the thinning phase ended, researchers met with participants to obtain a breath CO measure and self-reports of smoking.
Results
Table 1 displays participant characteristics. Mann-Whitney U and Χ2 tests revealed no statistically significant differences on any characteristics between the Full and Mixed groups. Multi-level modeling (MLM) analyses were run in SAS 9.3, and all other tests were run in SPSS 21. Alpha was set at .05 for all statistical tests.
Table 1.
Participant Characteristics
| Full Contingency (n = 22) | Mixed Contingency (n = 21) | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Gender (% male) | 54.5 | --- | 66.7 | --- |
| Age | 45.1 | 11.0 | 41.4 | 11.1 |
| Race (% White) | 66.7 | --- | 73.7 | --- |
| Marital status (% single) | 54.5 | --- | 71.4 | --- |
| Live with smoker (%) | 28.6 | --- | 38.1 | --- |
| Education (median) | Some college | --- | Some college | --- |
| Weekly income (median, $) | 201–300 | --- | 201–300 | --- |
| Cigarettes per day | 19.8 | 7.4 | 18.0 | 5.4 |
| Years smoking | 22.8 | 11.2 | 20.0 | 11.6 |
| Intake CO (ppm) | 30.6 | 11.5 | 27.8 | 17.4 |
| NTB score | 2.9 | 0.6 | 3.0 | 0.8 |
| FTND score | 5.7 | 1.9 | 5.3 | 1.9 |
| Quit readiness | 86.2 | 16.9 | 88.1 | 15.5 |
| Quit confidence | 70.6 | 27.1 | 76.1 | 27.0 |
| Quit importance | 91.4 | 15.5 | 88.0 | 14.3 |
Note. CO = carbon monoxide; NTB = Need to Belong; FTND = Fagerström Test for Nicotine Dependence
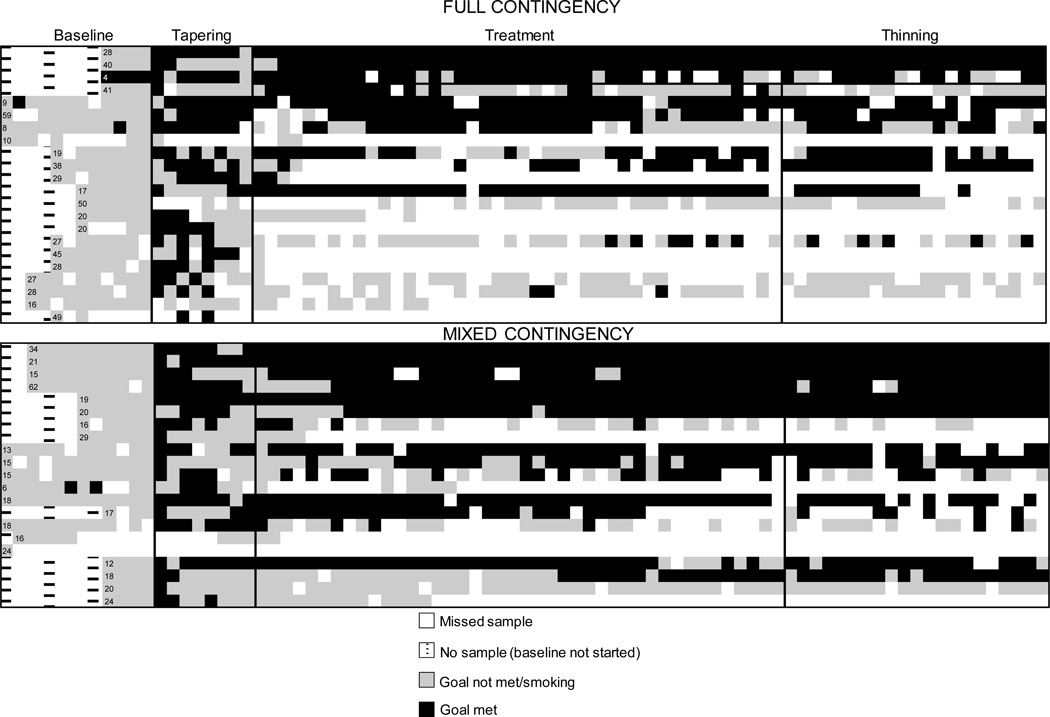
Figure 1 shows CO outcomes for each individual CO sample for all participants across all study phases. The logic of a multiple-baseline design requires that behavior should change only when the intervention is introduced (Kazdin, 2011). Figure 1 reveals that this requirement was met: despite the “staggered” start times of the intervention, breath CO decreased only when the intervention was introduced.
Figure 1.
Smoking status as assessed by breath carbon monoxide (CO) by group across all study phases. Each row represents a participant. Data are organized by team from most to least successful. Note that the durations of the baseline phase varied across groups, as required by a multiple baseline design. Numbers for each participant indicate the average CO during the Baseline condition.
Statistical analyses included team as a covariate, and analyses of CO data relied on an intention-to-treat approach. Thus, missing samples were counted as positive for smoking. The results of CO sample submissions that did not meet our CO sample fidelity standards were also considered positive. Two participants provided CO video samples that did not meet our CO fidelity standards. After researchers provided additional instructions about the CO sampling procedure, one of these participants withdrew from the study and the other modified their CO sampling behavior to achieve fidelity. Although the Mixed Group submitted more negative samples than the Full Group (49% vs. 32%), multi-level modeling (MLM) analyses indicated no statistically significant effect of group or a group-by-phase interaction on the percentage of negative samples. However, for both the Full and Mixed groups there was a significant effect of phase, F(3, 123) = 28.94, p < .0001. Tukey’s post-hoc tests revealed that relative to baseline (3.3%), the number of samples meeting the abstinence criterion was significantly higher during treatment (41.3%) and thinning (40.0%; ps < .05).
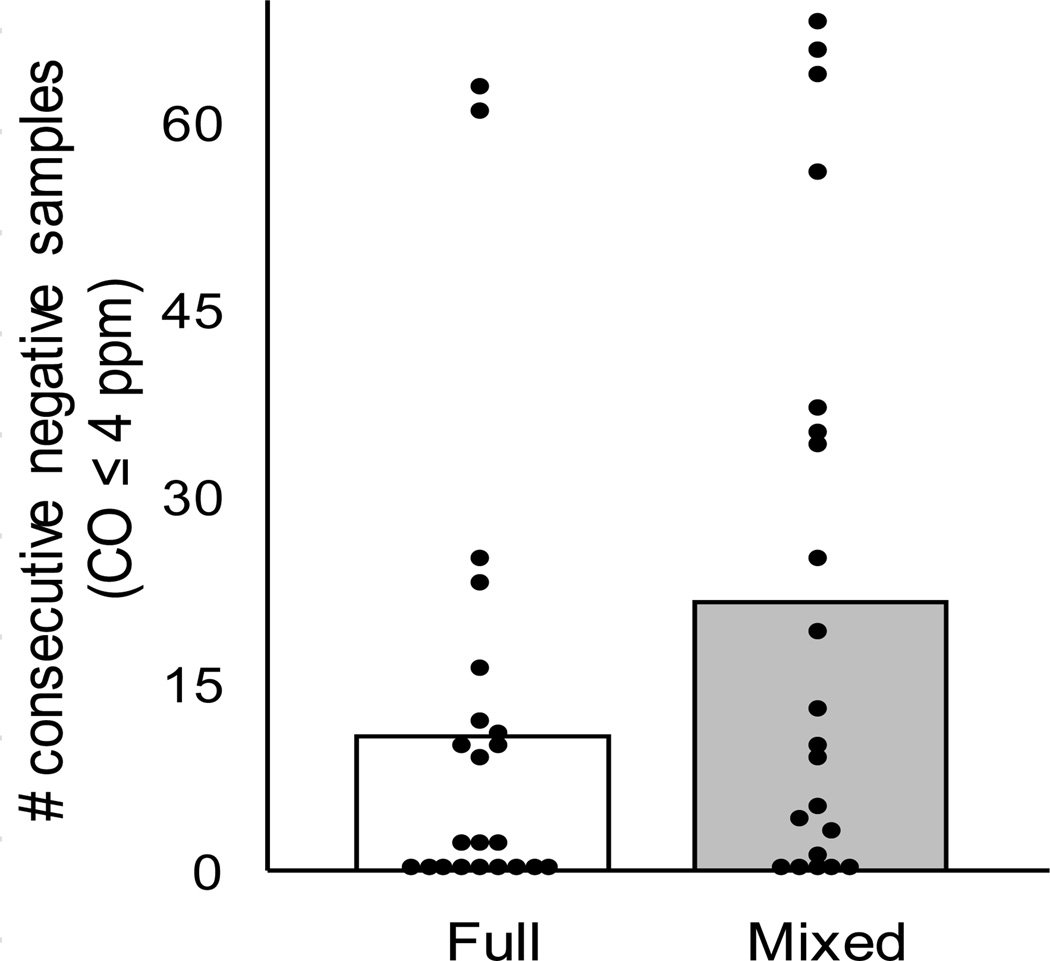
Figure 2 shows continuous abstinence in both groups, defined as the largest number of consecutive samples with breath CO ≤ 4 ppm during the entire intervention. Participants in the Mixed Group showed higher rates of continuous abstinence than those in the Full Group (21.4 vs. 11.2 consecutive negative samples), but this difference was not statistically significant.
Figure 2.
Longest consecutive abstinence achieved during the intervention by group. Each dot represents an individual participant and bars represent group averages. CO = carbon monoxide
Chi-square analyses did not indicate statistically significant differences between the groups on point prevalence abstinence at Week 7 (Full = 18.2% vs. Mixed = 28.6%) or at the 3-month follow-up period (Full = 9.1% vs. Mixed = 14.3%). Point prevalence was defined as breath CO ≤ 4ppm and a self-report of no cigarette smoking in the past 7 days.
Support forum posts were rated as positive, negative, or neutral based on a scale developed by Speltz, Shimamura, and McReynolds (1982; see Meredith & Dallery, 2013 for more details on the rating scale). Two independent observers rated all forum posts. Interobserver agreement (IOA) was calculated by subtracting the number of disagreements from the total number of posts, dividing this number by the total number of posts, and multiplying by 100. Interobserver agreement for the ratings was 92.8%. Among those who completed the study, the average number of posts made was 25.6 (SD = 24.8). The vast majority of posts were rated as positive (87.8%) or neutral (11.8%), and only 0.3% were rated as negative. Furthermore, most of (90.6%) the communication on the forum related to individuals’ quitting processes or teammates’ cessation progress. MLM analysis indicated that the Full and Mixed groups did not differ significantly on the number of forum posts per day at any time-point (analysis was conducted for study completers and moderator was included as a covariate). However, there were statistically significant decreases in posts from baseline to thinning, and there was a significant group-by-phase interaction, F(3, 84) = 3.72, p < .05. Reductions in posts per day for those in the Full Group occurred from tapering to treatment, and for the Mixed Group this decrease occurred from baseline to tapering. Participants did not report interacting with one another outside of the forum during the baseline through thinning phases. The forum remained accessible to participants through the 3-month follow-up period, however no participants regularly used it. Following thinning, one team reported meeting in person for lunch and two other participants exchanged telephone numbers.
The number of posts per day was associated with the percentage of abstinent samples submitted during treatment (r = .39, p = .03) and thinning (r = .41, p = .02), but not during the tapering phase. In addition, there was no statistically significant relationship between average NTB scores and number of posts during any phase.
There were no statistically significant differences in attrition between groups (36.4% in the Full Group and 23.8% in the Mixed Group). Participants who completed the study submitted 83.9% (SD = 14.8) of the required video samples. There were no statistically significant differences in CO submission rates between the Mixed and Full groups.
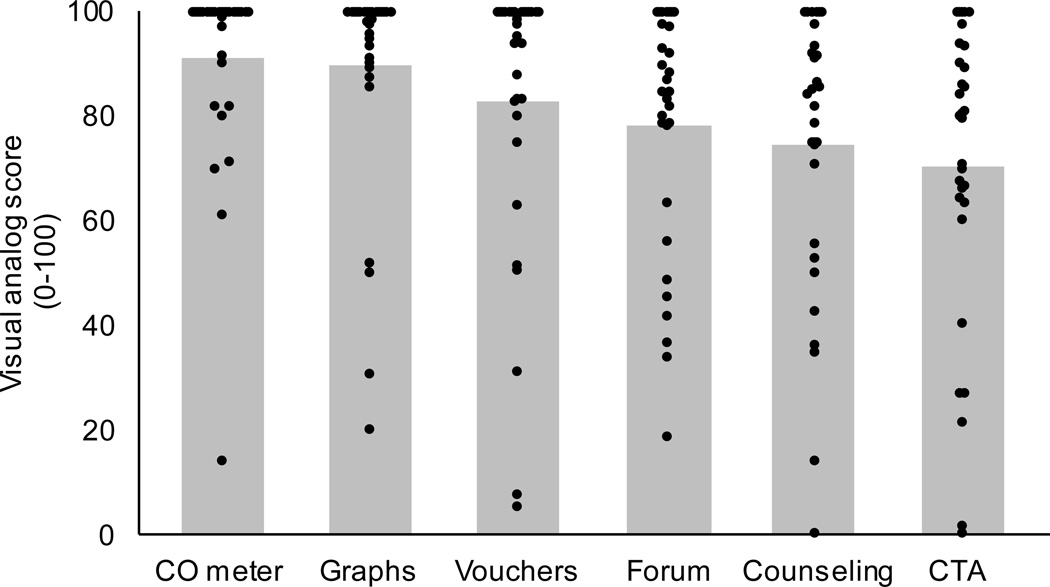
Figure 3 shows acceptability ratings for several aspects of the intervention. In general, participants who completed the study found the intervention easy, helpful, convenient, and fair. Median scores for each of these categories were 96 (IQRs = 18.8–19.8) or greater on a 100-point scale. There were no statistically significant differences between any acceptability ratings between the Full and Mixed groups. Ninety-six percent of participants indicated that if they were to attempt to quit again in the future that they would prefer to use the current treatment (40.0%) or the current treatment and an additional treatment (e.g., NRT, counseling; 56.7%). Participants also were highly likely to recommend the intervention to another smoker who wished to quit (Median = 100; IQR = 8.5). Responses to several open-ended questions about the intervention, the discussion forum, and suggestions for changes to the intervention are provided as online supplementary material to this article.
Figure 3.
Acceptability of Mōtiv8TM treatment components. Each dot represents an individual participant and bars represent combined group (Full and Mixed) averages. Higher scores represent great acceptability. CO = carbon monoxide, CTA = Clearing the Air (educational booklet)
Participants assigned to the Full Group earned $33.97 (SD = 42.05) in vouchers on average compared to $189.57 (SD = 183.85) for those in the Mixed Group (U = 120.0, p < .01).
Discussion
The present study replicates and extends previous research involving group contingencies to promote smoking cessation and social support. Consistent with previous work (Meredith & Dallery, 2013; Meredith et al., 2011), the results suggest that group contingencies can increase rates of CO-verified smoking abstinence relative to baseline control conditions. During baseline, nearly all samples submitted were positive for smoking, which suggests that self-monitoring and brief access to the online support forum alone did not promote abstinence. Smoking declined only after the group contingencies were instituted. The study also sheds new light on the effects of two arrangements of group contingencies: one in which all incentives were contingent on group behavior (the Full Group) and one in which only some incentives were contingent on group behavior (the Mixed Group). Statistical analysis indicated no significant differences in the percentage of negative COs, sustained abstinence, or point prevalence at the end of treatment and at the 3-month follow-up.
Participants who completed the study used the discussion forum to provide encouragement and information related to quitting. Participants posted an average of 25 posts in the forum, the vast majority of which were rated as positive. These results are consistent with previous Internet-based group CM interventions (Meredith & Dallery, 2013; Meredith et al., 2011). Although there were modest correlations between posts and abstinence in the current study, the direction of causality cannot be established. In a recent study, Meredith and Dallery investigated the influence of access to a discussion forum using brief, one-week CM intervention periods, and found that access did not promote higher rates of abstinence than no access. In the current study, many participants endorsed social support on the forum as a positive and potentially influential component of the intervention. In addition, participants suggested that the social component could have been enhanced in several respects. For example, several participants wondered if their teammates were in fact real people, and others suggested that more engagement from their group would have been beneficial. Disentangling the role of social support in the context of group contingencies will require experimental manipulation, possibly by using CM to promote different levels or types of social behavior (e.g., relatively immediate social consequences based on evidence of abstinence).
Negative social behavior occurred at a low rate (0.3% of posts; see also Meredith et al., 2011). It is possible that the presence of a moderator in the forum reduced the inclination to post negative comments. It is also possible that the nature of the groups – comprised of strangers – influenced group behavior. Although the use of groups comprised of strangers reduces threats to internal validity by minimizing interactions outside of the experimental procedures, the impact of social consequences may be diminished relative to consequences in the context of pre-existing relationships. Several responses to the open-ended questions about the forum support this possibility. For example, one participant noted, “It was a little difficult knowing how my thoughts we're actually being received since I had very little info about other group members.”
The costs in vouchers per participant were lower in the Full Group ($34) relative to the Mixed Group ($190). To some extent, this is not surprising because earnings in each group depended on smoking outcomes, which were generally superior in the Mixed relative to the Full Group. Relative to traditional individual-based CM, however, group CM might entail cost offsets. Meredith and Dallery (2013) found that CM based on individual performance produced four times the payout compared to a group CM arrangement, and both arrangements produced equivalent smoking outcomes. Further work is necessary to explore parameters of the magnitude of earnings in combination with group CM to optimize cost-effectiveness.
The present study had several limitations. First, the study may not have been powered sufficiently to detect differences in abstinence between the two group contingency arrangements. Future research should involve larger samples sizes to detect statistically significant differences between groups. Second, attrition was 36.4% and 23.8% in the Full and Mixed groups, respectively. Although treatment acceptability data were not collected from these participants, several of them communicated that the social, cooperative component of the intervention was a deterrent to participation, and that they feared letting their teammates down if they were not successful. Third, two participants submitted videos that were deemed unacceptable in terms of fidelity, which may have been attempts to falsify CO samples. It is unknown to what extent the monetary or social consequences, or their combination, contributed to this behavior. One of these participants withdrew from the study. Fourth, several participants rated various aspects of the study unfavorably (i.e., < 50 on the visual analog scale, see Figure 3). Based on the responses to the open-ended questions, these participants found the lack and/or quality of group participation was unacceptable. To improve this aspect of the intervention, one participant suggested an in-person meeting among group members prior to the intervention, and another suggested that a minimum amount of participation should be required as part of the intervention. Another participant suggested that the intervention should be tailored based on whether an individual would be “better in a group or alone.” Finally, at 7-weeks, the current intervention was relatively brief. Future work should explore the sustained implementation of technology-enabled group CM, and incorporate advances in mobile devices to increase access and potentially usability of this intervention (Hertzberg, et al., 2013).
The present study adds to the literature on technology-based methods to implement contingency management to promote smoking cessation (Dallery et al., 2014). The two group contingency arrangements produced comparable smoking outcomes, and the Full Group was less costly to implement than the Mixed Group in terms of voucher expenses. However, more research is needed on the acceptability of group contingency arrangements. Previous research indicates that some group contingency arrangements may be less preferred than individual contingencies (Meredith & Dallery, 2013). Future studies should collect treatment acceptability data from all participants, including those who are lost to attrition. Nevertheless, group contingencies can be arranged in a variety of ways, and some of these arrangements may promote greater efficacy and cost-effectiveness than others. For example, groups could compete against each other for social and monetary incentives, or group contingencies could be arranged in dynamic, adaptive ways to target less successful participants for brief periods (e.g., a so-called hero contingency; Coleman, 1970). Information and digital technology will continue to afford innovative methods to implement contingency management interventions to promote cessation.
Supplementary Material
Acknowledgments
Research was supported by R21DA029162 from the National Institute on Drug Abuse (PI: J. Dallery).
Footnotes
All authors made significant contributions to the article and read and approved the final article. The authors report no real or potential conflicts of interest with any organization that may inappropriately influence the research or the manuscript.
Contributor Information
Jesse Dallery, Department of Psychology, University of Florida.
Steven Meredith, Department of Psychology, University of Florida.
Brantley Jarvis, Department of Psychology, University of Florida.
Paul A. Nuzzo, Department of Psychiatry, University of Kentucky.
References
- Barlow D, Nock M, Hersen M. Single case research designs: Strategies for studying behavior change. New York: Allyn and Bacon; 2008. [Google Scholar]
- Alessi SM, Petry NM. A randomized study of cellphone technology to reinforce alcohol abstinence in the natural environment. Addiction. 2013;108(5):900–909. doi: 10.1111/add.12093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Tidey J, Murphy JG, Swift R, Colby SM. Contingency management for alcohol use reduction: A pilot study using a transdermal alcohol sensor. Drug and Alcohol Dependence. 2011;118(2):391–399. doi: 10.1016/j.drugalcdep.2011.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman R. A conditioning technique applicable to elementary school classrooms. Journal of Applied Behavior Analysis. 1970;3:293–297. doi: 10.1901/jaba.1970.3-293. doi: http://dx.doi.org/10.1901/jaba.1970.3-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Glenn IM. Effects of an Internet-based voucher reinforcement program for smoking abstinence: A feasibility study. Journal of Applied Behavior Analysis. 2005;38:349–357. doi: 10.1901/jaba.2005.150-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Glenn IM, Raiff BR. An Internet-baed abstinence reinforcement treatment for cigarette smoking. Drug and Alcohol Dependence. 2007;86:230–238. doi: 10.1016/j.drugalcdep.2006.06.013. [DOI] [PubMed] [Google Scholar]
- Dallery J, Kurti A, Erb P. A new frontier: Integrating behavioral and digital technology to promote health behavior. The Behavior Analyst. 2014;37:1–24. doi: 10.1007/s40614-014-0017-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Meredith S, Glenn IM. A deposit contract method to deliver abstinence reinforcement for cigarette smoking. Journal of Applied Behavior Analysis. 2008;41:609–615. doi: 10.1901/jaba.2008.41-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Raiff BR, Grabinski MJ. Internet-based contingency management to promote smoking cessation: A randomized controlled study. Journal of Applied Behavior Analysis. 2013;46:750–764. doi: 10.1002/jaba.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Hill-Kapturczak N, Liang Y, Karns TE, Cates SE, Lake SL, Roache JD. Use of continuous transdermal alcohol monitoring during a contingency management procedure to reduce excessive alcohol use. Drug and Alcohol Dependence. 2014;142:301–306. doi: 10.1016/j.drugalcdep.2014.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC. A clinical practice guideline for treating tobacco use and dependence: A US public health service report. Journal of the American Medical Association. 2000;283:3244–3254. [Google Scholar]
- Foster SL, Mash EJ. Assessing social validity in clinical treatment research: Issues and procedures. Journal of Consulting and Clinical Psychology. 1999;67:308. doi: 10.1037//0022-006x.67.3.308. [DOI] [PubMed] [Google Scholar]
- Gresham FM, Gresham GN. Interdependent, dependent, and independent group contingencies for controlling disruptive behavior. The Journal of Special Education. 1982;16:101–110. [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom K-O. The Fagerstrom Test for Nicotine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hertzberg JS, Carpenter VL, Kirby AC, Calhoun PS, Moore SD, Dennis MF, Beckham JC. Mobile contingency management as an adjunctive smoking cessation treatment for smokers with posttraumatic stress disorder. Nicotine & Tobacco Research. 2013;15:1934–1938. doi: 10.1093/ntr/ntt060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE. Single-case research designs: Methods for clinical and applied settings. New York: Oxford University Press; 2011. [Google Scholar]
- Kirby KC, Kerwin ME, Carpenedo CM, Rosenwasser BJ, Gardner RS. Interdependent group contingency management for cocaine-dependent methadone maintenance patients. Journal of Applied Behavior Analysis. 2008;41:579–595. doi: 10.1901/jaba.2008.41-579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellor D, Stokes M, Firth L, Hayashi Y, Cummins R. Need for belonging, relationship satisfaction, loneliness, and life satisfaction. Personality and Individual Differences. 2008;45:213–218. [Google Scholar]
- Meredith SE, Dallery J. Investigating group contingencies to promote brief abstinence from cigarette smoking. Experimental and Clinical Psychopharmacology. 2013;21:144–154. doi: 10.1037/a0031707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith SE, Grabinski MJ, Dallery J. Internet-based group contingency management to promote abstinence from cigarette smoking: A feasibility study. Drug and Alcohol Dependence. 2011;118:23–30. doi: 10.1016/j.drugalcdep.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith SE, Robinson A, Erb P, Spieler CA, Klugman N, Dutta P, Dallery J. A mobile-phone-based breath carbon monoxide meter to detect cigarette smoking. Nicotine & Tobacco Research. 2014;16:766–773. doi: 10.1093/ntr/ntt275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W, Rollnick S. Motivational Interviewing: Preparing people for change. New York: Guilford; 2002. [Google Scholar]
- Perkins KA, Stitzer M, Lerman C. Medication screening for smoking cessation: A proposal for new methodologies. Psychopharmacology. 2006;184:628–636. doi: 10.1007/s00213-005-0105-5. [DOI] [PubMed] [Google Scholar]
- Raiff BR, Jarvis BP, Turturici M, Dallery J. Acceptability of an Internet-based contingency management intervention for smoking cessation: Views of smokers, nonsmokers, and healthcare professionals. Experimental and Clinical Psychopharmacology. 2013;21:204–213. doi: 10.1037/a0032451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll JM, Higgins ST. A within-subject comparison of three different schedules of reinforcement of drug abstinence using cigarette smoking as an exemplar. Drug and Alcohol Dependence. 2000;58:103–109. doi: 10.1016/s0376-8716(99)00073-3. [DOI] [PubMed] [Google Scholar]
- Roll JM, Higgins ST, Badger GJ. An experimental comparison of three different schedules of reinforcement of drug abstinence using cigarette smoking as an exemplar. Journal of Applied Behavior Analysis. 1996;29:495–505. doi: 10.1901/jaba.1996.29-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Chutuape MA, Bigelow GE, Stitzer ML. Voucher-based reinforcement of cocaine abstinence in treatment-resistant methadone patients: Effects of reinforcement magnitude. Psychopharmacology. 1999;146:128–138. doi: 10.1007/s002130051098. [DOI] [PubMed] [Google Scholar]
- Speltz ML, Shimamura JW, McReynolds WT. Procedural variations in group contingencies: Effects on children's academic and social behaviors. Journal of Applied Behavior Analysis. 1982;15:533–544. doi: 10.1901/jaba.1982.15-533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoops WW, Dallery J, Fields NM, Nuzzo PA, Schoenberg NE, Martin CA, Wong CJ. An internet-based abstinence reinforcement smoking cessation intervention in rural smokers. Drug and Alcohol Dependence. 2009;105:56–62. doi: 10.1016/j.drugalcdep.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson DA, Williamson SH, Watkins PC, Hughes HH. Increasing cooperation among children using dependent group-oriented reinforcement contingencies. Behavior Modification. 1992;16:414–425. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.