Introduction
It is important for primary care providers (PCPs) to be able to identify “patient care complexity” when confronted with it in their practices in order for them to properly treat these patients and to obtain appropriate reimbursement for their care. In general these are patients who for various reasons do not participate effectively in their personal care and require extra time and resources to achieve even minimal therapeutic objectives (Peek, Baird, & Coleman, 2009). The patient, in turn, may experience frustration with the medical care system. Underlying these clinical dilemmas are contextual issues in patients’ lives that interfere with self-activation and proper self-care. The contextual issues can be intrinsic to the patient (e.g., literary or language incompetence, co-occurring mental illness) or extrinsic (e.g., lack of social support, spousal abuse) (Weiner, 2004).
Identifying patients who have complex care needs in the primary care setting is ever more important because the numbers of these patients are increasing (Turner & Cuttler, 2011; Weiss, 2007; Whittle & Bosworth, 2007), and many emerging health care reforms are aimed at improving services for these patients. The number of adults over 65 years of age is projected to reach 20% of the U.S. population by 2030, and these older adults have more health issues and almost four times the rate of hospitalization than their younger cohorts (CDC, 2007; He, Sengupta, Velkoff, & DeBarros, 2005). Despite increasing numbers of patients with complex care needs, a consensus definition for complexity is presently unavailable (Cohen et al., 2011; Peek et al., 2009; Turner & Cuttler, 2011; Whittle & Bosworth, 2007). In this paper “complexity” will be used to describe patient care complexity. Accurately defining complexity is essential in order to create interventions to improve patient care and to enable healthcare providers to be reimbursed properly for caring for these patients. Current definitions of complexity used in medical studies depend primarily on the simultaneous occurrence of multiple chronic medical conditions (Grembowski et al., 2014; Katon et al., 2010). However, experienced healthcare providers identify a spectrum of psycho-social-economic circumstances that impact a patient’s health (Peek et al., 2009; Shippee, Shah, May, Mair, & Montori, 2012; Weiner, 2004; Weiss, 2007). Customizing a patient’s care based on these circumstances has been described as “contextualization” (Weiner, 2004; Weiner et al., 2013). For the most part these psycho-social-economic contextual factors are not measured, codified in existing diagnoses, or accounted for in reimbursement for services (Weiner et al., 2013).
In the course of efforts to improve the care of patients with complex care needs in the practices of a large primary care network, we encountered a gap between the practitioners’ perceptions of complexity and the definitions of complexity reported in the medical literature where most authors attributed complexity to patients with multiple medical diagnoses (Grembowski et al., 2014; Katon et al., 2010; Loeb, Bayliss, Biswanger, Candrian, & deGruy, 2011; Newcomer, Steiner, & Bayliss, 2011). Although multiple medical diagnoses may contribute to complexity, PCPs described various other contextual issues that may complicate the care of patients (Weiner, 2004; Weiner et al., 2013). European physicians have developed tools to assist practitioners with screening and identifying factors that contribute to complexity, including the INTERMED (de Jonge, Huyse, Slaets, Sollner, & Stiefel, 2005; Huyse et al., 1999; Huyse et al., 2001; Stiefel et al., 1999; Stiefel et al., 2006) and the COMPRI (Huyse et al, 2001). Peek et al. (2009) adapted the INTERMED tool (de Jonge et al., 2005; Huyse et al., 1999; Huyse et al., 2000; Stiefel et al., 1999; Stiefel et al., 2006) to assess complexity in primary care practices and created the Minnesota Complexity Assessment Method (MCAM). Although the MCAM includes assessment for several contextual factors that contribute to complexity, the tool was trialed by PCPs in a local clinic and was found to be too cumbersome and time consuming to be useful in clinical practice.
Utilizing principles of action research (Svensson & Nielsen, 2006), we convened social scientists and PCPs with the aim of identifying and describing important dimensions of complexity. The purpose of this report is to describe the elucidation and validation of dimensions of complexity that were identified by PCPs and to assess the capacity of these items to discriminate between patients in their practices who did and did not require complex care.
Methods
Elucidation of Dimensions of Complexity
Action research emphasizes collaboration between researchers and community members “as co-producers in the creation of new knowledge” (Svensson & Nielsen, 2006, p. 4). Utilizing action research theory, researchers work with community members throughout the entire research process and “can only create knowledge in co-operation with [these] social actors based on trust and free agreement to participate” (Svensson & Nielsen, 2006, p. 4). The role of the researcher in action research is to manage the data, create new theories, and relate the findings to current research.
Utilizing action research principles to better understand complexity in primary care practices, we attempted to derive a construct for complexity from dialogue with practicing physicians. For the purposes of this paper, patients who require complex care will be designated as “complex patients” and those who do not require complex care will be described as “non-complex patients.” A group of three PCPs, a gerontologist, one social worker, and one nurse with prior experience as a primary care nurse practitioner were invited to participate in a structured discussion regarding complex patients. In addition to care providers, discussants included two self-identified complex patients and seven faculty members from a local university representing the disciplines of psychology, sociology, anthropology, and economics. The providers represented a convenience sample; however, they included family practitioners and internists who provide primary care in group practices that serve most of the population in a county of a Northwestern state. One physician served in the Indian Health Services and provided care for local tribes representing an important sub-population in the county.
Care providers were asked to develop a brief, anonymous case description that represented their perceptions of complexity and present the case to the group for discussion. Utilizing verbal factor analytical techniques, social science faculty were asked to listen to case reports and ask probing questions for the purpose of elucidating important dimensions of complexity. Following the initial combined discussion, the social science faculty convened independently to discuss observations and identify key relevant factors that contributed to complexity. From this analysis, a brief screening tool that incorporated the dimensions or classes of complexity into brief descriptive phrases was generated for validation and assessment in primary care practices.
Dimensions of Complexity
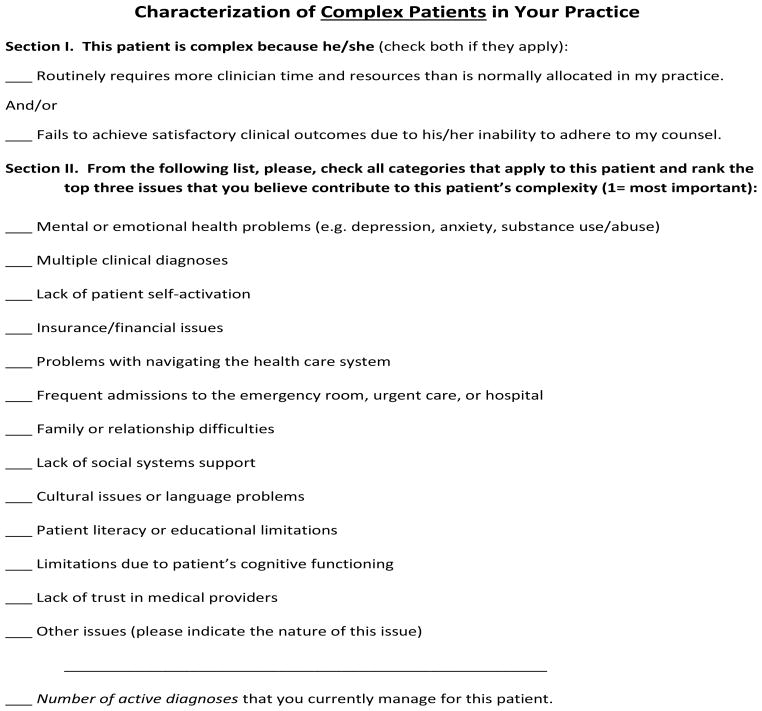
Figure 1 illustrates the complexity screening tool, listing the dimensions of complexity that were distilled from the initial structured discussions with physicians, patients, and social scientists. The tool was subdivided into two sections. Section 1 asked—from the physicians’ perspective—what adverse impact on their practice led them to consider the patient as having complex care needs. Section 2 included 13 brief phrases that described dimensions that contribute to complexity in this specific patient.
Figure 1.
Complex Patient Screening Tool
In the initial phase of the study that elucidated dimensions of complexity, the social scientists observed that while physicians did not use an explicit, operative definition for complexity, they concurred that patients were generally considered complex based on the adverse impact on their practice. In scenarios of complex patients, the patients either required more than the routine amount of time and resources and/or the patients failed to achieve satisfactory clinical outcomes due to not adhering to recommendations. The 13 dimensions of complexity identified under Section 2 were factors that contributed to complexity; however, independently these factors would not result in a patient being classified as complex as long as the patient could be managed within the typical time and resource constraints and satisfactorily followed treatment recommendations.
Assessment of the Discriminatory Capacity of the Complexity Tool
To validate and assess the discriminatory capacity of the classes of complexity identified by the social scientists, we designed a comparative study in the context of primary care practices in the county. A convenience sample of 13 primary care physicians was invited to trial the complexity tool in their respective practices. Participating physicians included the four practitioners that participated in the initial phase of the project elucidating the dimensions of complexity, as well as physicians trained in family medicine and internal medicine. Although the PCPs were not selected randomly from the community, they were representative of PCPs providing services in three large group practices. These group practices included a physician-owned primary care practice, a medical group affiliated with a medical center and a tribal health center, together these medical care organizations serve more than 90% of the county’s population.
During an eight-week period in the summer of 2013, the PCPs were asked to identify 12 patients that they encountered in practice with complex care needs and to complete the complexity tool for each patient. It should be noted that the PCPs were not provided criterion for complexity but rather were asked, based on their personal experience as to what constitutes complexity in their practice, to identify with the complexity tool those dimensions that were associated with that specific patient. PCPs could select one or more dimensions they perceived as important and were asked to rank the three most important contributing factors. In addition, PCPs were asked to note any additional factors or dimensions that contributed to complexity that were not included in the screening tool. Finally, the PCPs were asked to estimate the amount of time in minutes that were required to complete the tool to assess the feasibility of integrating the tool in practice.
For controls, the PCPs were asked to identify 12 patients seen in their respective practices during the same time period that were not perceived to have complex care needs. Using the same screening tool described in Figure 1, but with minor changes in syntax that were appropriate for non-complex patients,, PCPs were asked to complete the tool and to identify any dimension that might be relevant to the patient even though it did not contribute to complexity.
Several steps were taken to ensure confidentiality of both PCPs and patients. PCPs were assigned a random numeral identifier by one of the investigators and all data were submitted for analysis under the respective anonymous identifier. To further ensure the confidentiality of patients, the only demographic information collected for submission and analysis was gender and age range. The study was reviewed and approved by the Human Subjects Review Committee of Western Washington University.
Statistical Analysis
Twelve PCPs submitted a total of 267 screening tools, 135 from complex patients and 132 from non-complex patients. The coded, anonymous data were entered into a database by one of the authors for further analysis. The dimensions of complexity were analyzed as categorical, dichotomous variables where the frequency of occurrence among complex patients was compared with the frequency among control non-complex patients To examine the null hypothesis that the frequency of occurrence did not differ across patient groups, we utilized a simple t-test. Differences in the frequency of occurrence were considered significant when the p < 0.05. Next we submitted the data to a latent class analysis, which seeks to determine whether patients can be assigned to meaningful subgroups or classes (Collins & Lanza, 2010). A fitting routine was applied to a set of nominal-level variables to place individuals into latent classes. Models were built according to the number of classes assumed. Given that there were 13 variables used to describe patients, models with up to 13 classes are possible. Models were estimated starting with two classes, then three classes, and so on. In addition, models were estimated simultaneously across non-complex patients and complex patients, but allowing for different class structures across these two types of patients. The best-fitting model was ascertained using the Bayesian Information Criterion (BIC) (Collins & Lanza, 2010). Models with smaller values of BIC are preferred. In our analysis, a model with two classes fit the data best (BIC = 683.63). After two categories, models witnessed increasingly larger values of BIC (e.g., a model with three classes showed a BIC value of 707.39, with increases in BIC corresponding with increasing numbers of latent classes).
Results
Assessment of Discriminatory Capacity of the Dimensions of Complexity
Twelve PCPs submitted complexity screens for 267 patients, of which 135 required complex care and 132 required routine care. Descriptive statistics for the patients are reported in Table 2. There were more female patients than male patients; however, the difference in the gender distribution across the two groups was not significant. Patients considered complex were older than controls. It is noteworthy that the occurrence of multiple diagnoses was relatively frequent in both complex patient and non-complex patient care groups. However, the average number of diagnoses per patient was significantly greater in the complex patient group. Based on the physician’s perception of the adverse impact of care on their practice, non-complex patients were managed within the usual constraints of time and resources and were achieving satisfactory outcomes consistent with treatment plans. On the other hand, 92% of complex patients required more than the allotted encounter time, while 38% did not follow treatment recommendations. Thirty-two percent of complex patients did not follow treatment recommendations and required excessive amounts of clinical encounter time.
Table 2.
Comparing Complex Patients to Non-Complex Patients
| Dimension | Complex Patients a | Non-Complex Patients b | p c |
|---|---|---|---|
| Multiple diagnoses | .76 | .32 | .000 |
| Mental health issues | .66 | .30 | .000 |
| Lack of self-activation | .36 | .05 | .000 |
| Insurance/financial issues | .27 | .08 | .000 |
| Family/relationship difficulties | .26 | .08 | .000 |
| Lack of social support | .25 | .02 | .000 |
| Limitations due to cognitive functioning | .18 | .02 | .000 |
| Lack of trust in medical providers | .16 | .01 | .000 |
| Problems navigating healthcare system | .14 | .02 | .000 |
| Frequent admissions | .13 | .00 | .000 |
| Patient literacy or educational limitations | .10 | .03 | .017 |
| Other issues | .26 | .05 | .000 |
| Cultural issues | .05 | .02 | .097 |
Note. p values from t-test comparisons between complex and non-complex patients
Patients with complex care needs
Patients without complex care needs
p values: A t-test was used for the categorical (nominal data). A t-test works on nominal data when comparing two groups. This holds because with one degree of freedom the chi-square test is equal to the square of the t-test. Thus, identical results occur.
Table 3 summarizes the categorical analysis of the dimensions or classes of complexity. The complexity screening tool was able to discriminate complex patients on 12 of the 13 variables. Only the “cultural issues” class failed to discriminate between the two groups of patients. It is notable that a small proportion of non-complex patients were reported with each of the several dimensions of complexity, consistent with the earlier observation that classes of factors that contribute to complexity do not independently result in physicians classifying patients as complex patients..
Table 3.
Latent Class Analysis Results: Four Latent Classes and Related Loadings
| Complex Patients a | Non-Complex Patients b | |||
|---|---|---|---|---|
| Variable | Class 1 | Class 2 | Class 3 | Class 4 |
| Mental health issues | .459 | .800 | .227 | .809 |
| Multiple diagnoses | .759 | .763 | .303 | .459 |
| Lack of self-activation | .042 | .589 | .304 | .185 |
| Insurance/financial issues | .045 | .423 | .001 | .715 |
| Problems navigating health care system | .170 | .119 | .000 | .146 |
| Frequent admissions | .217 | .060 | .000 | .002 |
| Family/relationship difficulties | .055 | .403 | .043 | .364 |
| Lack of social support | .005 | .426 | .001 | .219 |
| Cultural issues or language problems | .070 | .038 | .017 | .001 |
| Patient literacy or educational limitations | .003 | .175 | .025 | .080 |
| Limitations due to cognitive functioning | .164 | .185 | .008 | .074 |
| Lack of trust in medical providers | .206 | .131 | .000 | .087 |
| Other issues | .310 | .022 | .041 | .109 |
| Probability of class placement | .415 | .585 | .898 | .102 |
Note. The values indicating the meaning of each construct are shown in boldface. For example, Class 1 consists of patients with primarily multiple diagnoses; Class 2 is composed of patients who have mental health issues, multiple diagnoses, and a lack of self-activation; Class 3 consists of patients with no discernable health issues; and Class 4 is composed of patients who have mental health and insurance/financial issues. The coefficients shown in each column correspond to factor loadings in a factor analysis, the difference being that latent class factor loadings are used for nominal outcomes, not interval outcomes.
Patients with complex care needs
Patients without complex care needs
Next we submitted the data to a latent class analysis to explore patterns of characteristics that are associated with complexity. The estimated class loadings for the latent class model with two categories are shown in Table 3. Among non-complex patients, 90% fell into class 1, in which patients reported no discernible issues that contribute to complexity. Ten percent of non-complex patients fell into class 2 and reported mental health issues and insurance issues. These patients were not regarded as complex because they did not require excessive encounter times and were able to effectively participate in their personal care. Finally, several patients designated as non-complex had multiple medical diagnoses; however, because they effectively participated in their personal care they were not considered complex. Among complex patients, 42% fell into class 3, consisting of patients with multiple diagnoses as the primary contributing factor for complexity. More than half (58%), however, fell into class 4 comprising patients who have mental health issues, multiple diagnoses, and did not participate effectively in recommended care plans. PCPs reported that 72% of patients in class 4 were classified as complex patients because they demanded excessive encounter times and were poorly activated in health behaviors.. The overall results demonstrate a substantial difference in contextual factors that contribute to complexity between complex patients and non-complex patients.
Participating physicians reported the average time to complete the screen was 1.4 (+/− 0.6) minutes. The screen was easy to complete given the physician’s general knowledge of the patient and their circumstances. Physicians reported it would be feasible to integrate the screen into their routine practices.
Discussion
The current report emerged from a more comprehensive effort among PCPs to improve services for complex patients and to improve the capacity and confidence of PCPs in managing their care. Published reports on complex patients in the new millennium have focused primarily on patients with multiple medical diagnoses (Grembowski et al., 2014; Katon et al., 2010). Practicing physicians, however, highlighted multiple contextual factors that contributed to the need for complex care, an observation that was described elsewhere among PCPs in the US and Europe (Peek et al., 2009; Weiner, 2004). Utilizing action research techniques (Svensson & Nielsen, 2006), we invited PCPs and patients to dialogue with social scientists representing several different disciplines for the purpose of distilling key dimensions or variables that contribute to complexity.. Among the several dimensions that PCPs identified, twelve of the thirteen dimensions contributed significantly to discriminating between patients requiring complex versus non-complex care. These variables did not, however, independently demand complex care. Furthermore, while multiple medical diagnoses contributed to complexity, it was considered an independent cause for complexity in less than half of the cases.
Contrary to many recent studies that identify complexity based on multiple medical diagnoses (Grembowski et al., 2014; Katon et al., 2010), in the present study less than half of the complex patients were considered complex because they had multiple medical conditions. Our findings are similar to Grant et al.’s study which compared PCPs’ subjective views of complex patients with three existing comorbidity models using the same set of patients and found poor agreement between the patients the PCPs identified as being complex patients and patients the comorbidity measures identified as being complex patients (2006). In this investigation, similar to Weiner et al. (2013) and Peek et al. (2009), we found that PCPs did not base their descriptions of complex patients solely on the numbers of patients’ medical diagnoses. In the current study PCPs based their identification of complex patients on whether the patient required more than usual encounter time and/or whether the patient participated in his or her personal care.
The identification of 12 contextual dimensions that were significantly associated with complexity by PCPs in the present study supports previous research that argues for a more comprehensive definition of complex patients that includes medical/biological, genetic, socioeconomic, environmental, cultural, and behavioral dimensions (Grant et al., 2006; Safford, Allison, & Kiefe, 2007; Weiner et al., 2013; Weiss, 2007).
Our study demonstrating significant differences in dimensions of patients’ lives between complex patients and non-complex patients illustrates the importance of contextualizing patient care. These observations are supported by Weiner (2004), who argues that when treating patients, PCPs must consider contextual factors in their patients’ lives and when patients’ contextual factors are addressed, they will experience better health outcomes (Weiner et al., 2013). Similarly, Peek et al. (2009) identified five domains—including illness, readiness, social, health system, and resources for care—that contributed to complex care. Complexity was defined as “interference with standard care caused by symptom severity/impairment or diagnostic uncertainty, behavioral unreadiness, lack of social safety or participation, and disorganization of care or difficult clinician-patient relationships” (p. 293). Similar to Weiner et al. (2013), Peek et al. (2009) emphasized that PCPs must identify complex patients and then create action steps to address the patient’s contextual factors that contribute to patient care complexity..
The current study was part of a local effort to improve the care of complex patients in primary care practices and to improve the confidence and capacity of PCPs to care for these patients. Therefore, generalizations from our observations are limited by the small geographic sample of physicians and patients and by the methods of sampling both providers and patients. It is noteworthy, however, that social scientists using action research techniques were able to identify a set of dimensions or variables that PCPs perceived as contributing to the need for complex care that are similar to those described by Weiner and colleagues (2013). These observations provide additional validation for an imperative to expand the definition of “complexity” beyond the simple notion of multiple medical diagnoses. Additionally, the study was limited by assessing only physicians’ perception of complexity. Future studies should expand the assessment to include other providers of primary care.
In conclusion, we found significant differences between complex patients and non-complex patients on 12 out of 13 contextual factors. Using latent class analysis, we identified subclasses of complex patients that included (1) a group with multiple medical diagnoses, and (2) a group with mental health issues, lack of activation, and multiple medical diagnoses. These results confirm earlier imperatives for expanding a definition for complexity beyond that of multiple medical diagnoses. The results support the need for PCPs to contextualize care for complex patients and to continue to ask themselves, “under the circumstances, what is the best next thing for this patient at this time” (Weiner, 2004, p. 281). It is important to better define patient complexity because it is only when we have a clear definition of it that we will be able to create interventions to improve the care of complex patients and reimburse providers appropriately for their care.
Table 1.
Demographic and Clinical Characteristics of Complex Patients and Non-Complex Patients
| N = 267 | |||
|---|---|---|---|
| Characteristic | Complex Patients a | Non-Complex Patientsb | p* |
| Male | 31% | 40% | .171 |
| Age: categories c | 4.86 | 3.09 | .000 |
| Number of categories d | 3.55 | 1.00 | .000 |
| Number of diagnoses e | 10.61 | 5.08 | .000 |
| More time f | 92% | -- | |
| Fail to adhere g | 38% | -- | |
| More time & failure to adhere h | 33% | -- | |
Patients with complex care needs
Patients without complex care needs
Age categories defined as category 1 = 18–29 years, category 2 = 30–39 years, category 3 = 40–49 years, category 4 = 50–59 years, category 5 = 60–69 years, category 6 = 70–79 years, category 7 = 79 years and beyond
Number of patient categories checked by the physician
Number of patient diagnoses currently managed by the physician
Patient required extra time for care
Patient failed to achieve satisfactory clinical outcome due to his/her inability to adhere to physician’s counsel
Patient required extra time for care and failed to achieve satisfactory outcome due to his/her inability to adhere to physician’s counsel
p values derived from simple t-test comparisons for comparing patients with complex care needs and patients without complex care needs p<.05
Acknowledgments
This research was supported by National Institutes of Health Conference Grant R13NR014046-02.
References
- Centers for Disease Control and Prevention and The Merck Foundation. The state of aging and health in America. Whitehouse Station, NJ: The Merck Company Foundation; 2007. [Google Scholar]
- Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SK, Simon TD, Srivastava R. Children with medical complexity: An emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538. doi: 10.1542/peds.2010-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins L, Lanza S. Latent class analysis and latent transition analysis: With applications in the social and health sciences. New York, NY: Wiley; 2010. [Google Scholar]
- de Jonge P, Huyse FJ, Slaets J, Sollner W, Stiefel FC. Operationalization of biopsychosocial case complexity in general health care: The INTERMED project. Australian and New Zealand Journal of Psychiatry. 2005;39:795–799. doi: 10.1080/j.1440-1614.2005.01684.x. [DOI] [PubMed] [Google Scholar]
- Grant RW, Ashburner JM, Hong CC, Chang Y, Barry MJ, Atlas SJ. Defining patient complexity from the primary care physician’s perspective. Annals of Internal Medicine. 2011;155:797–804. doi: 10.7326/0003-4819-155-12-201112200-00001. [DOI] [PubMed] [Google Scholar]
- Grembowski D, Schaefer J, Johnson KE, Fischer H, Moore SL, Tai-Seale M, LeRoy L. A conceptual model of the role of complexity in the care of patients with multiple chronic conditions. Medical Care. 2014;52(3):S7–S14. doi: 10.1097/MLR.0000000000000045. [DOI] [PubMed] [Google Scholar]
- He W, Sengupta M, Velkoff V, DeBarros K. Current population reports: 65+ in the United States. Washington, DC: US Census Bureau, Government Printing Office; 2005. [Google Scholar]
- Huyse FJ, de Jonge P, Slaets J, Herzog T, Lobo A, Lyons JS, Rigatelli M. COMPRI—An instrument to detect patients with complex care needs. Psychosomatics. 2001;42(3):222–228. doi: 10.1176/appi.psy.42.3.222. [DOI] [PubMed] [Google Scholar]
- Huyse FJ, Lyons JS, Stiefel FC, Slaets J, de Jonge P, Findk P, van Schijndel RS. “INTERMED”: A method to assess health service needs, Part I. Development and reliability. General Hospital Psychiatry. 1999;21:39–48. doi: 10.1016/s0163-8343(98)00057-7. [DOI] [PubMed] [Google Scholar]
- Huyse FJ, Lyons JS, Stiefel F, Slaets J, de Jonge P, Latour C. Operationalizing the biopsychosocial model: The INTERMED. Psychosomatics. 2001;42(1):5–13. doi: 10.1176/appi.psy.42.1.5. [DOI] [PubMed] [Google Scholar]
- Katon WJ, Lin EHB, Von Korff M, Ciechanowski P, Ludman EJ, Young B, McCulloch D. Collaborative care for patients with depression and chronic illnesses. The New England Journal of Medicine. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb DF, Bayliss EA, Binswanger IA, Candrian C, deGruy FV. Primary care physician perceptions on caring for complex patients with medical and mental illness. Journal of General Internal Medicine. 2012;27(8):945–952. doi: 10.1007/s11606-012-2005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomer SR, Steiner JF, Bayliss EA. Identifying subgroups of complex patients with cluster analysis. The American Journal of Managed Care. 2011;17(8):e324–e332. [PubMed] [Google Scholar]
- Nielsen KA, Svensson L. Introduction and background. In: Nielsen KA, Svensson L, editors. Action research and interactive research. Maastricht, The Netherlands: Shaker Publishing; 2006. pp. 1–12. [Google Scholar]
- Peek CJ, Baird MA, Coleman E. Primary care for patient complexity, not only disease. Families, Systems, & Health. 2009;27(4):287–302. doi: 10.1037/a0018048. [DOI] [PubMed] [Google Scholar]
- Safford MM, Allison JJ, Kiefe C. Patient complexity: More than comorbidity. The vector model of complexity. Journal of General Internal Medicine. 2007;22(3):382–390. doi: 10.1007/s11606-007-0307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shippee ND, Shah ND, May CR, Mair FS, Montori VM. Cumulative complexity: A functional, patient-centered model of patient complexity can improve research and practice. Journal of Clinical Epidemiology. 2012;65:1041–1051. doi: 10.1016/j.jclinepi.2012.05.005. [DOI] [PubMed] [Google Scholar]
- Stiefel FJ, Huyse FJ, Sollner W, Slaets J, Lyons JS, Latour C, de Jonge P. Operationalizing integrated care on a clinical level: The INTERMED project. The Medical Clinics of North America. 2006;90:713–758. doi: 10.1016/j.mcna.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Turner BJ, Cuttler L. The complexity of measuring clinical complexity. Annals of Internal Medicine. 2011;155(5):851–852. doi: 10.7326/0003-4819-155-12-201112200-00009. [DOI] [PubMed] [Google Scholar]
- Weiner SJ. Contextualizing medical decisions to individualize care. Journal of General Internal Medicine. 2004;19:281–285. doi: 10.1111/j.1525-1497.2004.30261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner SJ, Schwartz A, Sharma G, Binns-Calvey A, Ashley N, Kelly B, Harris I. Patient-centered decision making and health care outcomes. Annals of Internal Medicine. 2013;158(8):573–580. doi: 10.7326/0003-4819-158-8-201304160-00001. [DOI] [PubMed] [Google Scholar]
- Weiss KB. Managing complexity in chronic care: An overview of the VA State-of-the-Art (SOTA) conference. Journal of General Internal Medicine. 2007;22(3):374–378. doi: 10.1007/s11606-007-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle J, Bosworth H. Studying complexity is complex. Journal of General Internal Medicine. 2007;22(3):379–381. doi: 10.1007/s11606-007-0380-4. [DOI] [PMC free article] [PubMed] [Google Scholar]