Abstract
The host tolerance mechanisms to avian influenza virus (H5N1) infection that limit tissue injury remain unknown. Emerging evidence indicates that cystic fibrosis transmembrane conductance regulator (CFTR), a cAMP-dependent Cl− channel, modulates airway inflammation. Janus tyrosine kinase (JAK) 3, a JAK family member that plays a central role in inflammatory responses, prominently contributes to the dysregulated innate immune response upon H5N1 attachment; therefore, this study aims to elucidate whether JAK3 activation induced by H5N1 hemagglutinin (HA) inhibits cAMP-dependent CFTR channels. We performed short-circuit current, immunohistochemistry and molecular analyses of the airway epithelium in Jak3+/+ and Jak3+/− mice. We demonstrate that H5N1 HA attachment inhibits cAMP-dependent CFTR Cl− channels via JAK3-mediated adenylyl cyclase (AC) suppression, which reduces cAMP production. This inhibition leads to increased nuclear factor-kappa B (NF-κB) signaling and inflammatory responses. H5N1 HA is detected by TLR4 expressed on respiratory epithelial cells, facilitating JAK3 activation. This activation induces the interaction between TLR4 and Gαi protein, which blocks ACs. Our findings provide novel insight into the pathogenesis of acute lung injury via the inhibition of cAMP-dependent CFTR channels, indicating that the administration of cAMP-elevating agents and targeting JAK3 may activate host tolerance to infection for the management of influenza virus–induced fatal pneumonia.
INTRODUCTION
Increasing evidence indicates that superinflammation, a consequence of an exacerbated innate immune response, plays a critical role (1,2) in the rapid progression to adult respiratory distress syndrome (ARDS) following H5N1 infection; however, innate immune mechanisms protect the infected host by reducing the viral burden. Thus, an optimal immune response is characterized by a balance between efficient pathogen clearance and an acceptable level of immunopathology (3,4). Tolerance to infection has recently been found to constitute a distinct strategy of host defense that limits tissue damage, facilitating a higher magnitude and duration of the immune response (5). The elucidation of the inducible tolerance mechanism in response to H5N1 infection will provide new therapeutic strategies for severe lung damage mediated by viral attack by attaining an optimal immune response.
The mechanisms that typically maintain the homeostasis of various physiological systems are likely to contribute to host tolerance to infection (6,7). Cystic fibrosis transmembrane conductance regulator (CFTR) is a cyclic adenosine monophosphate (cAMP)-dependent Cl−channel expressed at the apical membrane of epithelial cells lining the tracheobronchial tree. CFTR channels secrete Cl− and mucus simultaneously with Ca2+ activated Cl− channels (CaCCs) (8) and regulate the amiloride-sensitive epithelial Na+ channel (ENaC), constituting the pathways that restrict Na+ and mucus absorption (9). Coordinating the regulation of the secretion and absorption of NaCl and fluids and airway surface liquid (ASL) homeostasis is crucial. Changing the salt and water composition of the periciliary fluid causes isotonic dehydration of the airway surface, leading to an impairment of mucociliary clearance. In the case of the ΔF508-CFTR mutation, constitutive nuclear factor-kappa B (NF-κB) activation results in IL-8-mediated chronic neutrophilic lung disease (10,11). Several investigators in the field believe that airway inflammation in CF is secondary to persistent bacterial infection, which results from impaired mucociliary clearance; however, recent evidence supports the hypothesis that the dysregulation of the inflammatory response is an intrinsic component of the CF phenotype and that airway inflammation may occur prior to or in the absence of bacterial infection. Moreover, numerous in vitro studies using human epithelial CF and control cell lines have confirmed that CFTR is an important inflammatory regulator and that CFTR mutations are associated with both the constitutive activation of proinflammatory signaling, especially NF-κB, in the absence of any apparent microbial stimulus and the exaggerated responses to bacterial products (12,13).
We previously demonstrated that exposure to hemagglutinin (HA), the surface glycoprotein of H5N1 that is indispensable for viral receptor binding, fusion, transmission, virulence and pathology (14–16), induced the activation of IFN-independent JAK/STAT and NF-κB in pulmonary epithelial cells. This activation was accompanied by the elevated secretion of chemokines/cytokines, including IP-10, IL-6, IL-8, MCP-1, MIP-1α, MIP-1β and RENTES. Furthermore, Janus tyrosine kinase (JAK) 3, a member of the JAK family of tyrosine kinases involved in cytokine receptor-mediated intracellular signal transduction, is a molecular determinant in the H5N1 HA-induced dysregulated innate immune response. The inhibition of JAK3 activation causes the negative regulation of NF-κB signaling (17); therefore, we speculated that H5N1 HA-stimulated NF-κB signaling may be, at least in part, attributed to the disturbance of epithelial CFTR inflammatory regulation, a host tolerance mechanism to infection, via a JAK3 activation-dependent response. The present study reveals for the first time that H5N1 HA attachment to the airway epithelia stimulates the JAK3 signaling cascade, leading to the suppression of CFTR inflammatory regulation and exaggerating innate immune responses.
MATERIALS AND METHODS
Preparation of the HA Protein
The recombinant HA protein from H5N1 (A/chicken/Guangdong/191/04, GenBank: AY737289) was generated as described previously (17).
Animal Models
B6129S4-Jak3tm1Lj (JAK3−/−) mice and wild-type B6129SF2/J (JAK3+/+) mice (6 to 8 wks of age) are all from the C57BL/6 mouse genetic background and were purchased from the Jackson Laboratory (Bar Harbor, ME, USA). JAK3 heterozygous knockout (JAK3+/−) mice were generated by crossing JAK3−/− mice with JAK3+/+ mice. Then, the genotypes were identified via PCR. All mice were housed at a constant temperature (20°C) with a 12-h light–dark photoperiod and allowed food and water ad libitum. All procedures were performed in compliance with the National Institutes of Health–adopted Guide for Care and Use of Laboratory Animals (18) and were approved by the Bioethics Committee of State Key Laboratory of Respiratory Disease, Guangzhou Medical University. JAK3+/+ mice were intratracheally administered saline; HA (1 mg/kg) with or without pretreatment with either forskolin (10 mg/kg, Sigma-Aldrich, St. Louis, MO, USA) or JAK3 inhibitor VI (0.15 mg/kg, Calbiochem, Darmstadt, Germany) by intraperitoneal (IP) injection; or HA (0.5 mg/kg) with or without pretreatment with glibenclamide IP injection (10 mg/kg, Sigma-Aldrich). JAK3+/− mice were administered HA at a dose of 1 mg/kg. Pulmonary histopathology and immunostaining were performed 12 h after the preceding treatment.
Cell Culture and Treatment
Cultured 16HBE and calu-3 cells were treated with saline, JAK3 inhibitor VI (760 nmol/L), TLR4 inhibitor (candesartan, 5 μmol/L, 3B Scientific Corporation, Wuhan, China), forskolin (10 μmol/L) or glibenclamide (500 μmol/L) for 30 min prior to HA stimulation and then subjected to different experiments. To test Gαi-mediated inhibition of AC, 16HBE cells were pretreated with IBMX (1 mmol/L, Sigma-Aldrich) and forskolin and either HA alone or HA in combination with IL-2 (100 UI/mL). In some experiments, cells were pretreated with pertussis toxin (100 ng/mL, Sigma-Aldrich) for 16 h or a TLR4 inhibitor or JAK3 inhibitor VI for 30 min.
CFTR-Dependent Short-Circuit Current Measurements
Tracheas of JAK3+/− or JAK3+/+ mice that had or had not received JAK3 inhibitor VI and TLR4 inhibitor (100 mg/kg) were pretreated with exposure of apical membranes to H5N1 HA, and then mounted in an Ussing chamber bathed in Krebs-Henseleit (K–H) solution to perform short-circuit current assay by using a VCC MC6 voltage-current clamp amplifier (VCC MC6, Physiologic Instrument, San Diego, CA, USA). The data were displayed on a signal collection and analysis system (Acquire & Analyze Rev II, San Diego, CA, USA) (19). Forskolin (10 μmol/L) was used to induce anion secretion via an increase in cAMP levels. Cl− free KH solution was employed to examine the effects on Cl− current. To inhibit electrically conductive Na+ transport, amiloride (100 μmol/L) was added in all studies.
Intracellular cAMP and Adenylyl Cyclase (AC) Assays
cAMP and AC levels were measured in cells using a cAMP assay kit (Assay Designs Inc., Ann Arbor, MI, USA) and an AC assay kit (Uscn Life Science Inc., Wuhan, China), respectively. The levels were corrected to the total protein levels, and the data were expressed as picomoles per milligram of protein.
Immunofluorescent Staining
Frozen lung tissue sections and cells cultured on glass coverslips were subjected to immunofluorescent staining for evaluation of CFTR expression or NF-κB/JAK3 activation using primary antibodies against CFTR (Abcam, Cambridge, MA, USA), phosphorylated NF-κBp65 (Cell Signaling Technology Inc., Beverly, MA, USA) and phosphorylated JAK3 (Santa Cruz Biotechnology, Santa Cruz, CA, USA), respectively. The slides were then incubated with species-matched fluorescent secondary antibodies and DAPI (for nuclear staining). Images were captured using a Nikon C1 Si confocal system (Nikon Corporation, Tokyo, Japan).
Lung Histology
Lung histology was performed as previously described (17).
Luminex Assay
Cytokine and chemokine production levels in supernatants were analyzed using a Luminex assay LiquidChip system (Panomics, Santa Clara, CA, USA) as previously described (17).
Western Blot
Western blotting for examination of JAK3 activity or CFTR expression was performed as previously described (17). The intensities of the relevant bands were quantified using ImageJ software (National Institutes of Health, Bethesda, MD, USA).
Quantitative Reverse-Transcription PCR (RT-PCR) Analysis
Cellular RNA was extracted and reverse transcribed to cDNA using the M-MLV first strand kit (Invitrogen, Life Technologies [Thermo Fisher Scientific Inc., Waltham, MA, USA]). Quantitative real-time PCR was performed to evaluate CFTR or TLR4 gene expression using SYBR Premix Ex Taq II (TaKaRa, Dalian, China). Fold changes of gene expression were normalized to β-actin and were quantified by the change-in-threshold method (ΔΔCt). Primer sequences for the genes of interest were designed using TAKARA Biotechnology. The primer sequences are listed below:
CFTR forward primer, 5′-TTAAAGCTGT CAAGCCGTGTTC-3′;
CFTR reverse primer, 5′-GCCAATGCAA GTCCTTCATCA-3′;
TLR4 forward primer, 5′-AGAAC CTGGACCTGAGCTTTAATC-3′;
TLR4 reverse primer, 5′-GAGGTGGCTT AGGCTCTGATATG-3′;
β-actin forward primer, 5′-CCTGGCACCCAGCACAAT-3′;
β-actin reverse primer, 5′-GCTGATCCACATCTGCTGGAA-3′.
Statistical Analysis
All of the experimental data shown are expressed as the means ± S.D. and were repeated at least three times, unless otherwise indicated. Statistical analysis was performed using one-way analysis of variance (ANOVA) followed by Student t test, and p < 0.05 was considered to be significant.
All supplementary materials are available online at www.molmed.org.
RESULTS
H5N1 HA-Induced Activation of JAK3 Inhibits cAMP-Dependent CFTR in the Airway Epithelium by Blocking AC
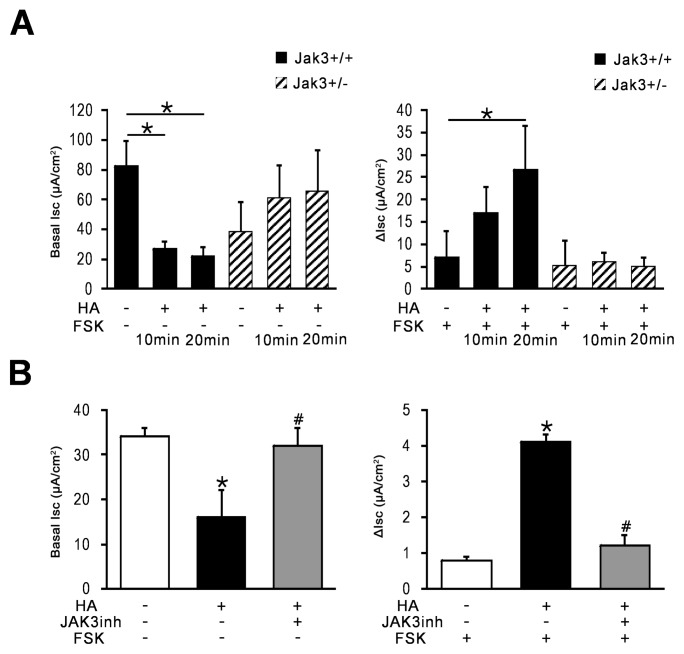
As predicted, treatment with HA (40 ug/mL) for 10 or 20 min resulted in a remarkable decline in the basal short-circuit current (Isc) of the apical membrane of the airway epithelium in the wild-type (JAK3+/+) mice but did not induce this change in the JAK3+/− mice. The addition of a single dose of the cAMP agonist forskolin to the micro-Ussing perfusion chamber caused an increase in the basal Isc (ΔIsc) of the murine tracheal tissues, as expected. However, with HA pretreatment, we detected an additional increase in Isc (ΔIsc) in the JAK3+/+ mice compared with JAK3+/− mice, in response to forskolin (Figure 1A), but did not find the change under the condition of Cl− free-KH perfusion (Supplementary Figure S1A). Exposure of tracheal tissues of JAK3+/+ mice that had received JAK3 inhibitor VI to HA reversed this HA-induced Isc decline, and ΔIsc returned to basal levels in response to forskolin (Figure 1B). We observed that H5N1 HA had no significant effect on amiloride-sensitive sodium current after exposure of the tracheal epithelium to HA for the indicated time (Supplementary Figure S1B).
Figure 1.
JAK3 activation by H5N1 HA results in the inhibition of cAMP-dependent CFTR Cl−channels. Tracheal tissues isolated from wild-type and JAK3 gene-deficient heterozygous (JAK3+/−) mice were pretreated with exposure of apical membranes to H5N1 HA (40 μg/mL) for 10 min or 20 min and then mounted into a perfused micro-Ussing chamber to perform short-circuit current assay. (A) Basal short-circuit current (Isc) and changes in the short-circuit current (ΔIsc) in response to forskolin (FSK, 10 μmol/L) addition (n = 5 per group, *p < 0.05 versus JAK3+/+ mice with saline). (B) Isc and ΔIsc measurement in wild-type mice treated with JAK3 inhibitor VI (JAK3inh, 0.15 mg/kg) or saline prior to exposure to HA (n = 5 per group, *p < 0.05 versus mice treated with saline; #p < 0.05 versus mice treated with HA).
The ELISA results indicate that HA stimulation in 16HBE cells inhibited AC activity, resulting in a significant reduction in intracellular cAMP levels. This inhibition was attenuated in cells pretreated with JAK3 inhibitor VI (Figures 2A, B).
Figure 2.
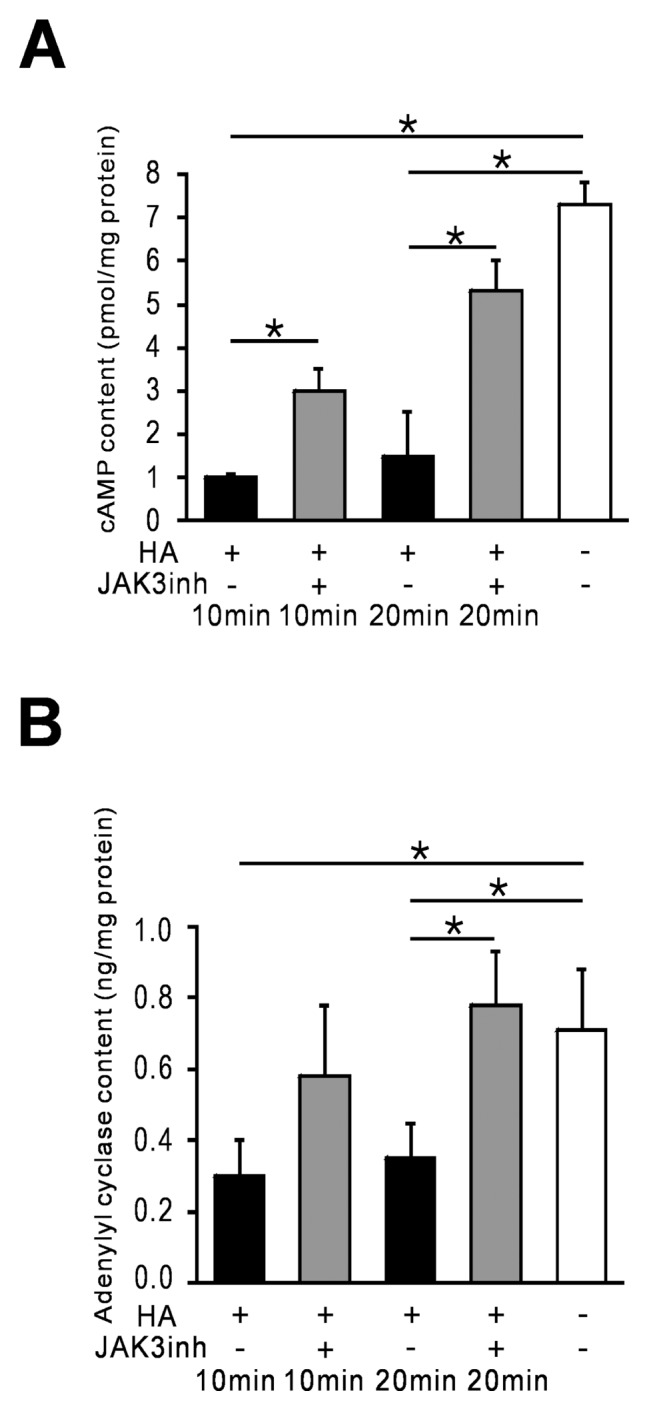
JAK3 activation by H5N1 HA inhibits AC activity and reduces the cAMP level. Cultured bronchial epithelial cells (16HBE) were pretreated with JAK3 inhibitor VI (JAK3inh, 760 nmol/L) or saline for 30 min prior to HA (40 μg/mL) treatment. Then, 10 min or 20 min after the HA challenge, (A) the intracellular cAMP levels and (B) the adenylyl cyclase activity in these cells were evaluated via ELISA. *p < 0.05 versus control cells treated with saline or cells treated with HA alone.
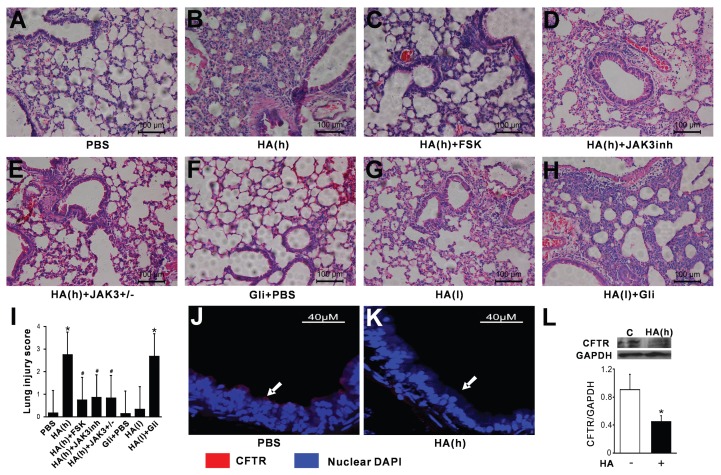
JAK3 Activation and the Suppression of cAMP-Dependent CFTR Expression Contribute to Acute Lung Injury Following H5N1 HA Challenge
Acute lung injury with severe interstitial edema and infiltration of inflammatory cells was observed (using pathologic examination) in wild-type mice 12 h following intratracheal challenge with HA (1 mg/kg) (Figures 3B, I). In contrast, wild-type mice pretreated with forskolin or JAK3 inhibitor VI and JAK3+/− mice were protected from this pulmonary inflammatory response (Figures 3C–E, I). However, pretreatment of JAK3+/+ mice with the CFTR inhibitor glibenclamide significantly accelerated the pulmonary inflammation triggered by a low dose of H5N1 HA (0.5 mg/kg) (Figures 3F–H, I). Corresponding to the pulmonary inflammation in the mice following intratracheal challenge with HA (1 mg/kg), the CFTR immunofluorescence signal in the airway epithelium was completely blocked (Figure 3K) compared with control mice treated with saline (Figure 3J). Furthermore, Western blot analysis showed a significant reduction of CFTR level in the lung of HA-challenged wild-type mice (Figure 3L).
Figure 3.
Blockade of cAMP-dependent CFTR channels via JAK3 activation exacerbates acute lung injury in response to H5N1 HA challenge. Histopathologic examination via hematoxylin and eosin (H&E) staining was performed on the lung sections of JAK3+/− and JAK3+/+ mice. (A) JAK3+/+ mice treated with saline; (B) with HA alone at 1 mg/kg or (G) 0.5 mg/kg; (C) HA (1 mg/kg) with either forskolin (FSK, 10 mg/kg) or (D) JAK3 inhibitor VI (JAK3inh, 0.15 mg/kg); (F) glibenclamide pretreatment (Gli, 10 mg/kg) alone or (H) HA (0.5 mg/kg) with glibenclamide pretreatment. (E) JAK3+/− mice treated with HA (1 mg/kg). Scale bars = 100 μm. h: high (1 mg/kg); L: low (0.5 mg/kg). (I) The lung injury score is assessed. The data are expressed as the mean ± SEM, with n = 5 per group. *p < 0.05, versus saline control; #p < 0.05 versus the HA(h)-challenged JAK3+/+ group. (J) Immunofluorescent staining was performed to examine CFTR expression in JAK3+/+mice treated with saline or (K) HA (1 mg/kg) for 4 h. Scale bars = 40 μm. The arrows indicate positively stained cells. (L) Western blot analysis was performed to determine the level of CFTR expression. *p < 0.05, versus saline control, c: control.
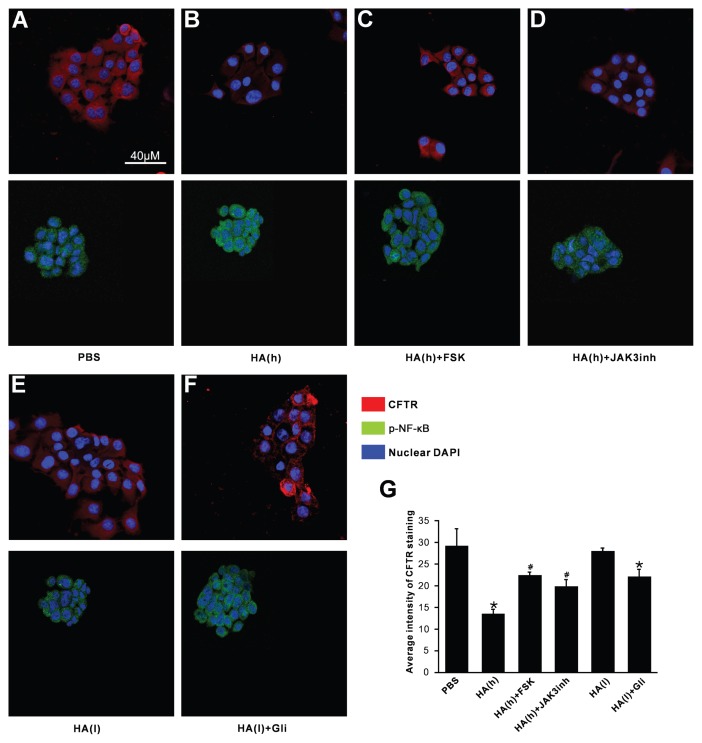
Inhibition of cAMP-Dependent CFTR Is Mediated by JAK3 Activation and Enhances NF-κB Signaling
Immunofluorescent staining and confocal microscopy examination revealed that CFTR was expressed and primarily localized to the plasma membrane in the calu-3 cells under basal conditions. In addition, Ser276-phosphorylated NF-κBp65, which indicates NF-κB activation (20), was dispersed throughout the cytoplasm (Figure 4A). After the exposure of these cells to 80 μg HA/mL for 12 h, the global CFTR immunofluorescence signal was sharply reduced (Figures 4B, G), and Ser276-phosphorylated NF-κBp65 was translocated from the cytoplasm to the nucleus (see Figure 4B). Pretreatment with either forskolin or JAK3 inhibitor VI for 30 min prior to HA (80 μg/mL) challenge ameliorated the reduction of the CFTR immunofluorescence signal (Figures 4C, D, G), concomitant with the absence of Ser276-phosphorylated NF-κBp65 nuclear accumulation (see Figures 4C, D). However, cells stimulated with a low dose of HA (20 μg/mL) displayed only a slight reduction in CFTR expression (Figures 4E, G) and exhibited no visible alteration in the nuclear translocation of Ser276-phosphorylated NF-κBp65 (see Figure 4E). However, a remarkable downregulation of CFTR expression (Figures 4F, G) concomitant with Ser276-phosphorylated NF-κBp65 activation was observed in HA (20 μg/mL)- challenged cells pretreated with the CFTR inhibitor glibenclamide (see Figure 4F).
Figure 4.
Inhibition of cAMP-dependent CFTR channels via JAK3 activation enhances phosphorylated NF-κBp65 nuclear translocation in bronchial cells after exposure to H5N1 HA. Immunofluorescent staining of cultured calu-3 cells was performed following HA addition at two doses for 12 h in the absence or presence of pretreatment with JAK3 inhibitor VI (JAK3inh, 760 nmol/L), forskolin (FSK, 10 μmol/L) or glibenclamide (Gli, 500 μmol/L). (A) The expression of CFTR and translocation of Ser276-phosphorylated NF-κBp65 (p-NF-κB) is shown in calu-3 cells treated with saline; (B) HA alone at 80 μg/mL or (E) 20 μg/mL; (C) HA (80 μg/mL) following pretreatment with either forskolin or (D) JAK3 inhibitor VI; or (F) glibenclamide pretreatment followed by treatment with HA at 20 μg/mL. Scale bars = 40 μm h: high (80 μg/mL), L: low (20 μg/mL). (G) Average fluorescence intensity of CFTR staining is represented. The data are expressed as the mean ± SEM, with n = 3 to 5 per group. *p < 0.05 versus saline control; #p < 0.05 versus the cells with HA (h) treatment alone.
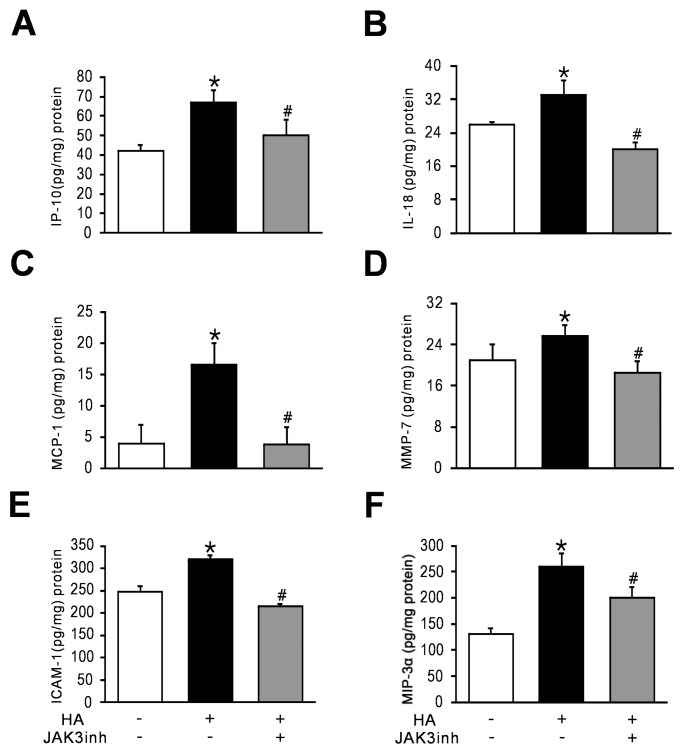
A bead array-based analysis was performed to examine the cytokine and chemokine levels in HA-treated 16HBE cells in the absence or presence of the JAK3 inhibitor VI. The results provide additional evidence that H5N1 HA induces the secretion of cytokines and chemokines, including ICAM-1, IL-18, IP-10, MCP-1, MIP-3α, MMP-7, which are related to the activation of JAK3 (Figure 5).
Figure 5.
Inhibiting JAK3 results in a reduction in cytokine/chemokine hyperproduction. Cultured 16HBE cells were incubated with HA (40 μg/mL) for 12 h with or without JAK3 inhibitor VI (JAK3inh, 760 nmol/L) pretreatment, and the culture supernatants were subjected to a LiquidChip assay. *p < 0.05 versus saline control cells; #p < 0.05 versus cells incubated with HA alone.
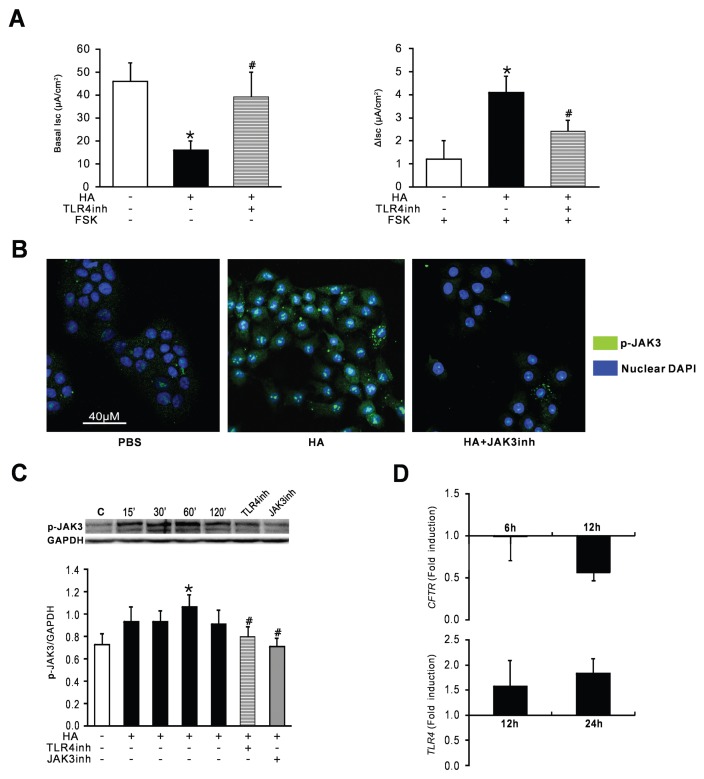
H5N1 HA Is Detected by TLR4 Expressed on Airway Epithelial Cells, which Facilitates JAK3 Activation
The cell-surface proteins Toll-like receptor (TLR)2 and TLR4, which belong to the family of pattern recognition receptors (PRRs), may interact with viral glycoprotein products (21). Therefore, we further examined the mechanism by which H5N1 HA, a pathogen-associated molecular pattern (PAMP), is sensed by TLR4 on the airway epithelial cell surface, leading to the activation of JAK3. We verified that the exposure of the apical surface of tracheal tissues isolated from wild-type mice to HA (40 μg/mL) in the presence of a TLR4 inhibitor did not induce a detectable decrease in the Isc in contrast to HA exposure in the absence of the TLR4 inhibitor. The response of the tracheal tissue to forskolin following pretreatment with HA and the TLR4 inhibitor displayed a reduced ΔIsc compared with tissue pretreated with HA alone (Figure 6A).
Figure 6.
H5N1 HA is detected by TLR4 expressed on respiratory epithelial cells, facilitating the activation of JAK3, which leads to the impairment of cAMP-dependent CFTR channels. (A) Isc and ΔIsc measurements in HA-challenged tracheal tissues of JAK3+/+ mice with or without TLR4 inhibitor treatment (n = 5 per group, *p < 0.05 versus mice administered saline; #p < 0.05 versus mice pretreated with HA alone); (B) Immunofluorescent staining for phosphorylated JAK3 (p-JAK3) expression in 16HBE cells. Scale bars = 40 μm (C) Western blot for p-JAK3 in 16HBE cells. The mean optical densities of the bands for each group are presented (C, bottom) (*p < 0.05 versus saline control cells; #p < 0.05 versus cells incubated with HA alone for 60 min); c: control. (D) Quantitative RT-PCR analysis of TLR4 and CFTR gene expression in HA-treated calu-3 cells for the indicated periods compared with control.
Immunofluorescence and Western blot analyses revealed that the HA-stimulated activation of JAK3 in bronchial epithelial cells was blocked by the addition of either a TLR4 or JAK3 inhibitor (Figures 6B, C). A 1.5-fold and 1.8-fold increase in TLR4 gene transcription was observed at 12 h and 24 h after HA exposure, respectively, and this increase was accompanied by a significant decrease in CFTR gene expression at 12 h (Figure 6D).
H5N1 HA Interaction with TLR4 Activates the Heterotrimeric Gαi/o Protein in Airway Epithelial Cells via JAK3 and Decreases cAMP Production
Activated heterotrimeric Gαi/o proteins inhibit the function of AC and reduce the intracellular cAMP levels (22); therefore, we determined whether Gαi/o proteins are activated by JAK3 following H5N1 HA stimulation in 16HBE cells. To confirm that the decrease in the cellular cAMP levels after H5N1 stimulation was due to the increased activation of Gαi/o proteins, these human airway epithelial cells were treated with a Gαi/o protein inhibitor (pertussis toxin, PTx), a JAK3 inhibitor (JAK3 inhibitor VI) or a TLR4 inhibitor prior to stimulation with H5N1 HA. Treatment with PTx or JAK3 inhibitor VI completely reversed the decrease in forskolin-induced cAMP production following challenge with H5N1 HA. The reduction in cAMP production was not observed in TLR4 inhibitor-pretreated cells. In addition, the simultaneous addition of IL-2, a JAK3 agonist, with H5N1 HA ameliorated the effects on cAMP production caused by pre-treatment with JAK3 inhibitor VI. These results demonstrate that Gαi/o proteins are activated by JAK3 following H5N1 HA stimulation in airway epithelial cells, contributing to the inhibition of the activity of AC, thereby reducing cellular cAMP production (Figure 7).
Figure 7.
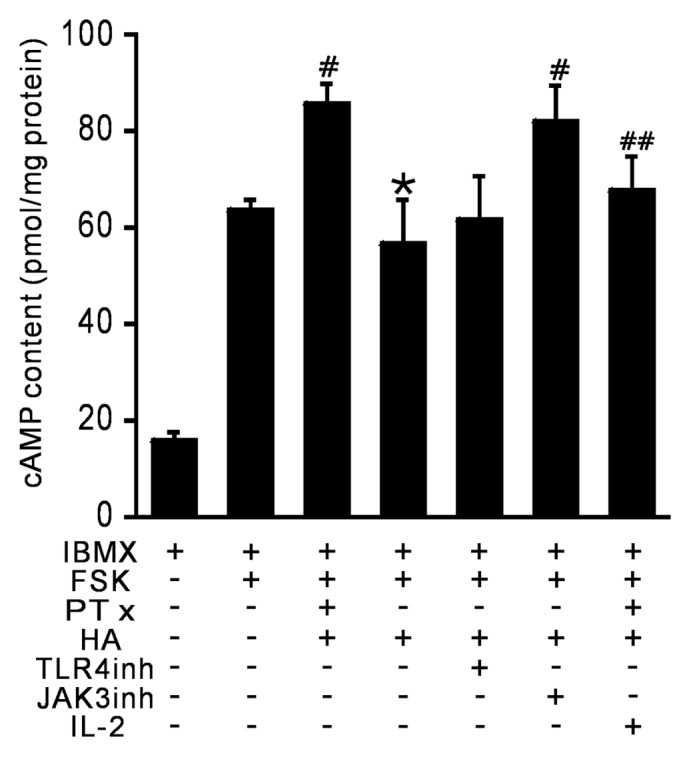
HA-induced JAK3 activation stimulates Gαimediated inhibition of AC, resulting in a decrease in the intracellular cAMP level 16HBE cells were pretreated with IBMX (1 mmol/L )for 15 min and then treated with forskolin (FSK, 10 μmol/L, 30 min) and either HA (40 μg/mL, 30 min) alone or HA (40 μg/mL, 30 min) in combination with IL-2 (100 UI/mL, 30 min) as indicated. In some instances, cells were pretreated with pertussis toxin (PTx, 100 ng/mL) for 16 h or a TLR4 inhibitor (TLR4inh, 5 μmol/L) or JAK3 inhibitor VI (JAK3inh, 760 nmol/L) for 30 min. The intracellular cAMP levels were examined in the cell lysates. *p < 0.05 versus forskolin-treated cells; #p < 0.05 versus HA-treated cells; and ##p < 0.05 versus PTx-treated cells.
DISCUSSION
Our findings provide novel insight into the pathogenesis of H5N1-induced acute lung injury via the inhibition of airway epithelium cAMP-dependent CFTR Cl− channels, which is associated with host tolerance to infection. We report that H5N1 HA-triggered JAK3 activation inhibits AC, the enzyme exclusively responsible for cAMP production (23). This inhibition induces a defect in cAMP production, thereby blocking cAMP-dependent CFTR channels.
A reduction in barrier function due to the impairment of CFTR-mediated trafficking caused by H5N1 HA exposure may facilitate the entry of viral or bacterial toxins into the submucosa, increasing the susceptibility of the host to pathogen infection (24–27).
Previous studies reported that an increase in cAMP due to the administration of forskolin or dibutyryl-cAMP reduced JAK3 expression, and this reduction resulted in impaired IL-2-dependent signal transduction and inhibition of T-cell activation (28). Consistently, targeting to JAK3 by the administration of JAK3 inhibitor VI alleviated acute lung injury (17). Current evidence provides strong support for the hypothesis that JAK3 activation via H5N1 HA attachment, which is associated with reduced cAMP production and suppression of cAMP-dependent CFTR Cl− channels in the airway epithelium, leads to an enhanced inflammatory reaction.
Recent observational data reported in an investigation of primary lower airway epithelial cells (AECs) in children with CF suggest a possible nexus between human rhinovirus (HRV) infection and AEC-initiated inflammatory cell recruitment and activation, thus leading to early airway inflammation (29). In the present study, we demonstrated an exaggerated inflammatory response in the lung tissue of HA-challenged wild-type mice following pretreatment with a CFTR channel inhibitor. These results are consistent with previous studies suggesting slower viral clearance, increased severity of infection and a prolonged inflammatory response to respiratory viral infection in CF (30,31).
Accumulating evidence has indicated that alterations in intracellular Cl− concentrations play an important role in a variety of physiological and pathological processes (32–34). Yang et al. recently reported that a decrease in the intracellular Cl− concentration promotes endothelial cell inflammation by activating the NF-κB pathway (35). Consistent with this result, our findings show that the attenuation of the CFTR Cl− channel by glibenclamide exacerbated H5N1 HA-induced acute lung injury, which was associated with enhanced NF-κB translocation. These data indicate that a reduction in CFTR channel-dependent Cl− transport underlies, at least in part, the HA-induced superinflammation. By contrast, in the presence of forskolin, which is commonly used to open CFTR channels by increasing cAMP levels, or a JAK3 inhibitor, bronchial epithelial calu-3 cells display reduced activation of NF-κB p65 induced by HA challenge. Therefore, the CFTR Cl− channel may play an essential role in the regulation of the innate immune inflammatory response by dynamically modulating Cl− movement across the plasma membrane.
NF-κB plays a crucial role in inducing the expression of a plethora of inflammatory and immune mediators; thus, NF-κB is one of the master regulators of the immune response and a key target for antiinflammatory drug design. A number of fundamental molecular mechanisms that contribute to the overall inhibitory action of cAMP on NF-κB function are well established (36). In the presence of forskolin and a JAK3 inhibitor, both wild-type mice and bronchial epithelial cells counteract NF-κB activation and inflammatory damage in response to HA challenge, indicating that interactions between cAMP and the NF-κB signaling cascade modulate the outcome of inflammation-associated NF-κB activation, which are modulated by JAK3 expression.
The activity of AC is modulated by G-protein subunits. Specifically, Gαs stimulates AC, inducing it to catalyze the formation of cAMP from ATP, whereas the Gαi protein exerts an inhibitory effect on AC. Recent studies have shown that TLR ligands activate Gαi proteins in endothelial cells (22,37). The authors speculated that TLR2, 3 and 4 also interact directly with Gαi via their intracellular domains due to a consensus motif for Gαi/o binding. Consistently, our results indicate that cytoplasmic JAK3 activation evokes the interaction between TLR4 and Gαi via their intracellular binding domains, leading to the inhibition of AC and reducing cAMP production. JAK3 activation, which is after activation of TLR4 by H5N1 HA, results in impaired cAMP-dependent CFTR regulation and CFTR gene expression, contributing to the exacerbation of immune inflammation. Therefore, we suggest that airway epithelial cAMP-dependent CFTR regulation represents an important host tolerance mechanism for limiting tissue damage to prevent severe immunopathology and that cAMP levels and CFTR function are closely modulated by JAK3 activity, which exerts an inhibitory effect on AC by activating Gαi G-protein subunits. Hence, cAMP-modulating therapeutic strategies potentially hold promise for treating ARDS induced by avian influenza virus infection; however, further investigation is required.
CONCLUSION
In conclusion, we suggest that the inhibition of cAMP-dependent CFTR channels by TLR4-stimulated JAK3 activation, which blocks AC-mediated cAMP production, disturbs the host tolerance to H5N1 infection, thereby enabling the exacerbation of innate immune inflammatory responses. Increasing the intracellular cAMP levels via the administration of cAMP- elevating agents and overcoming the attenuation of cAMP production by selective JAK3 inhibition (JAK3 inhibitor VI) may represent an effective therapeutic strategy for the management of influenza virus–induced severe pneumonia.
Supplemental Data
ACKNOWLEDGMENTS
The authors would like to thank Wenliang Zhou (School of Life Science, Sun Yatsen University, Guangzhou, China) for help with experiments. This work was supported by grants from the National Key Basic Research Program of China (973 Program; 2009CB522104), the National Natural Science Foundation of China (30900576), the China Postdoctoral Science Foundation (20100480734), the Yangcheng Scholars Research Program of Guangzhou Municipal Universities (10A024G) and the Program for Tackling Key Problems in Science and Technology of the Local Government in Guangzhou (2014), China.
Footnotes
Online address: http://www.molmed.org
DISCLOSURES
The authors declare that they have no competing interests as defined by Molecular Medicine or other interests that might be perceived to influence the results and discussion reported in this paper.
Cite this article as: Cao K, et al. (2015) H5N1 virus hemagglutinin inhibition of cAMP-dependent CFTR via TLR4-mediated Janus tyrosine kinase 3 activation exacerbates lung inflammation. Mol. Med. 21:134–42.
REFERENCES
- 1.Ramos I, Fernandez-Sesma A. Innate immunity to H5N1 influenza viruses in humans. Viruses. 2012;4:3363–88. doi: 10.3390/v4123363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peiris JSM, Cheung CY, Leung CYH, Nicholls JM. Innate immune responses to influenza A H5N1: friend or foe? Trends Immunol. 2009;30:574–84. doi: 10.1016/j.it.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmid-Hempel P. Evolutionary Parasitology: The Integrated Study of Infections, Immunology, Ecology, and Genetics. Oxford: Oxford University Press; 2011. p. 516. [Google Scholar]
- 4.Casadevall A, Pirofski L-a. Host-pathogen interactions: redefining the basic concepts of virulence and pathogenicity. Infect Immun. 1999;67:3703–13. doi: 10.1128/iai.67.8.3703-3713.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medzhitov R, Schneider DS, Soares MP. Disease tolerance as a defense strategy. Science. 2012;335:936–41. doi: 10.1126/science.1214935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Majno G, Joris I. Cells, Tissues, and Disease: Principles of General Pathology. 2nd edition. New York: Oxford University Press; 2004. p. 1005. [Google Scholar]
- 7.Nash AA, Dalziel RG, Fitzgerald JR. Mims’ Pathogenesis of Infectious Disease. Amsterdam: Academic Press; 2015. p. 356. [Google Scholar]
- 8.Caputo A, et al. TMEM16A, a membrane protein associated with calcium-dependent chloride channel activity. Science. 2008;322:590–4. doi: 10.1126/science.1163518. [DOI] [PubMed] [Google Scholar]
- 9.Stutts MJ, et al. CFTR as a cAMP-dependent regulator of sodium channels. Science. 1995;269:847–50. doi: 10.1126/science.7543698. [DOI] [PubMed] [Google Scholar]
- 10.Tarran R, Button B, Boucher RC. Regulation of normal and cystic fibrosis airway surface liquid volume by phasic shear stress. Annu Rev Physiol. 2006;68:543–61. doi: 10.1146/annurev.physiol.68.072304.112754. [DOI] [PubMed] [Google Scholar]
- 11.Venkatakrishnan A, et al. Exaggerated activation of nuclear factor-kappaB and altered IkappaBbeta processing in cystic fibrosis bronchial epithelial cells. Am J Respir Cell Mol Biol. 2000;23:396. doi: 10.1165/ajrcmb.23.3.3949. [DOI] [PubMed] [Google Scholar]
- 12.Cohen TS, Prince A. Cystic fibrosis: a mucosal immunodeficiency syndrome. Nat Med. 2012;18:509–19. doi: 10.1038/nm.2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen-Cymberknoh M, Kerem E, Ferkol T, Elizur A. Airway inflammation in cystic fibrosis: molecular mechanisms and clinical implications. Thorax. 2013;68:1157–62. doi: 10.1136/thoraxjnl-2013-203204. [DOI] [PubMed] [Google Scholar]
- 14.Rogers G, et al. Single amino acid substitutions in influenza haemagglutinin change receptor binding specificity. Nature. 1983;304:76–8. doi: 10.1038/304076a0. [DOI] [PubMed] [Google Scholar]
- 15.Salomon R, Webster RG. The influenza virus enigma. Cell. 2009;136:402–10. doi: 10.1016/j.cell.2009.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu W-C, Lin S-C, Yu Y-L, Chu C-L, Wu SC. Dendritic cell activation by recombinant hemagglutinin proteins of H1N1 and H5N1 influenza A viruses. J Virol. 2010;84:12011–7. doi: 10.1128/JVI.01316-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu W, Chen M, Ge N, Xu J. Hemagglutinin from the h5n1 virus activates Janus kinase 3 to dysregulate innate immunity. PloS One. 2012;7:e31721. doi: 10.1371/journal.pone.0031721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Committee for the Update of the Guide for the Care and Use of Laboratory Animals, Institute for Laboratory Animal Research, Division on Earth and Life Studies, National Research Council of the National Academies. Guide for the Care and Use of Laboratory Animals. 8th edition. Washington (DC): National Academies Press; 2011. [Google Scholar]
- 19.Goddard CA, Evans MJ, Colledge WH. Genistein activates CFTR-mediated Cl– secretion in the murine trachea and colon. Am J Physiol Cell Physiol. 2000;279:C383–92. doi: 10.1152/ajpcell.2000.279.2.C383. [DOI] [PubMed] [Google Scholar]
- 20.Vermeulen L, De Wilde G, Notebaert S, Haegeman G. Regulation of the transcriptional activity of the nuclear factor-kappaB p65 subunit. Biochem Pharmacol. 2002;64:963–70. doi: 10.1016/s0006-2952(02)01161-9. [DOI] [PubMed] [Google Scholar]
- 21.Bowie AG, Haga IR. The role of Toll-like receptors in the host response to viruses. Mol Immunol. 2005;42:859–67. doi: 10.1016/j.molimm.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 22.Dauphinee SM, Voelcker V, Tebaykina Z, Wong F, Karsan A. Heterotrimeric Gi/Go proteins modulate endothelial TLR signaling independent of the MyD88-dependent pathway. Am J Physiol Heart Circ Physiol. 2011;301:H2246–53. doi: 10.1152/ajpheart.01194.2010. [DOI] [PubMed] [Google Scholar]
- 23.Billington CK, Hall IP. Novel cAMP signalling paradigms: therapeutic implications for airway disease. Br J Pharmacol. 2012;166:401–10. doi: 10.1111/j.1476-5381.2011.01719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morimoto K, et al. Influence of absorption enhancers (bile salts) and the preservative (benzalkonium chloride) on mucociliary function and permeation barrier function in rabbit tracheas. Eur J Pharm Sci. 1998;6:225–30. doi: 10.1016/s0928-0987(97)10003-3. [DOI] [PubMed] [Google Scholar]
- 25.Boucher R. Evidence for airway surface dehydration as the initiating event in CF airway disease. J Int Med. 2007;261:5–16. doi: 10.1111/j.1365-2796.2006.01744.x. [DOI] [PubMed] [Google Scholar]
- 26.Humlicek AL, et al. Paracellular permeability restricts airway epithelial responses to selectively allow activation by mediators at the basolateral surface. J Immunol. 2007;178:6395–403. doi: 10.4049/jimmunol.178.10.6395. [DOI] [PubMed] [Google Scholar]
- 27.LeSimple P, Liao J, Robert R, Gruenert DC, Hanrahan JW. Cystic fibrosis transmembrane conductance regulator trafficking modulates the barrier function of airway epithelial cell monolayers. J Physiol. 2010;588:1195–209. doi: 10.1113/jphysiol.2009.182246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kolenko V, et al. Downregulation of JAK3 protein levels in T lymphocytes by prostaglandin E2 and other cyclic adenosine monophosphate-elevating agents: impact on interleukin-2 receptor signaling pathway. Blood. 1999;93:2308–18. [PubMed] [Google Scholar]
- 29.Sutanto EN, et al. Innate inflammatory responses of pediatric cystic fibrosis airway epithelial cells: effects of nonviral and viral stimulation. Am J Respir Cell Mol Biol. 2011;44:761–7. doi: 10.1165/rcmb.2010-0368OC. [DOI] [PubMed] [Google Scholar]
- 30.Wang EE, Prober CG, Manson B, Corey M, Levison H. Association of respiratory viral infections with pulmonary deterioration in patients with cystic fibrosis. N Eng J Med. 1984;311:1653–8. doi: 10.1056/NEJM198412273112602. [DOI] [PubMed] [Google Scholar]
- 31.Colasurdo GN, et al. Respiratory syncytial virus infection in a murine model of cystic fibrosis. J Med Virol. 2006;78:651–8. doi: 10.1002/jmv.20589. [DOI] [PubMed] [Google Scholar]
- 32.Wang XQ, et al. CLC-3 channels modulate excitatory synaptic transmission in hippocampal neurons. Neuron. 2006;52:321–33. doi: 10.1016/j.neuron.2006.08.035. [DOI] [PubMed] [Google Scholar]
- 33.Hong L, et al. Alteration of volume-regulated chloride channel during macrophage-derived foam cell formation in atherosclerosis. Atherosclerosis. 2011;216:59–66. doi: 10.1016/j.atherosclerosis.2011.01.035. [DOI] [PubMed] [Google Scholar]
- 34.Heimlich G, Cidlowski JA. Selective role of intracellular chloride in the regulation of the intrinsic but not extrinsic pathway of apoptosis in Jurkat T-cells. J Biol Chem. 2006;281:2232–41. doi: 10.1074/jbc.M507367200. [DOI] [PubMed] [Google Scholar]
- 35.Yang H, et al. Decrease of intracellular chloride concentration promotes endothelial cell inflammation by activating nuclear factor-κB pathway. Hypertension. 2012;60:1287–93. doi: 10.1161/HYPERTENSIONAHA.112.198648. [DOI] [PubMed] [Google Scholar]
- 36.Gerlo S, et al. Cyclic AMP: a selective modulator of NF-κB action. Cell Mol Life Sci. 2011;68:3823–41. doi: 10.1007/s00018-011-0757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hildebrand D, Sahr A, Wölfle SJ, Heeg K, Kubatzky KF. Regulation of Toll-like receptor 4-mediated immune responses through Pasteurella multocida toxin-induced G protein signalling. Cell Commun Signal. 2012;10:22. doi: 10.1186/1478-811X-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.