Abstract
Trigger finger (TF) is a condition that affects quality of life and one of the most common causes of hand pain and disability. TF is characterized by catching, snapping or locking of the involved finger flexor tendon, associated with pain. TF in the children occurs rarely than in adults and partial tendon laceration is an uncommon cause of TF in the children. Thus, our aim in this study to define TF due to partial flexor tendon laceration in a child.
Electronic supplementary material
The online version of this article (doi:10.1007/s12593-015-0180-8) contains supplementary material, which is available to authorized users.
Keywords: Trigger finger, Flexor tendon, Laceration, Child, Partial
Trigger finger (TF) is a clinical feature used to describe painful popping or snapping during flexion and extension of the involved finger. TF is also known as stenosing tenosynovitis and first described by Notta in 1850 [1]. TF in the children occurs more rarely than in adults and develops almost exclusively in the thumb which is called Congenital Trigger Thumb [2]. Compared to pediatric trigger thumb, pediatric TF is 10 times less frequent [3]. Although described as congenital by some authors, there are no clear records of this condition being present at birth [2, 4]. In the literature, TF is reported to occur between the ages of 3 weeks and 11 years [3]. The etiology of TF is not fully known but recurrent anatomic anomalies [3, 5, 6], inflammatory synovitis of rheumatoid arthritis [3, 6], post traumatic calcific tendonitis [7] or deposition of mucopolysaccharide in Hurler’s syndrome [8] are causes that reported. Many options have been described for TF treatment, from conservative splinting [9] to operative exploration and correction of the offending structures [3, 5]. In our case we described an uncommon cause of TF in a child, partial flexor tendon laceration.
Case
An 8 year-old boy who presented with triggering of the right third finger 5 years after sustaining sharp laceration to the volar aspect of his right hand that had been sutured in the emergency department. Time between onset triggering and referral to our clinic was 5 years. The time interval between the initial trauma and the development of triggering was 1 month. There were scar formation due to previous laceration on the third proximal digital crease (Fig. 1.) and triggering of the third finger in active movements. Triggering was reducible actively by applying external force with thumb or passively (Video 1.).
Fig. 1.

Scar formation due to previous laceration on the third proximal digital crease
Surgery was initiated under sedation and local anesthesia to assess the movement of the tendon immediately after repair . Scar formation on the third proximal digital crease was excised. The incision extended in Bruner fashion and dissected gently. A1 pulley was released and fibrotic tissue due to partial flexor digitorum superficialis (FDS) tendon laceration was observed (Fig. 2.). Fibrotic tissue was excised and laceration was less than 10 % of the FDS tendon cross-sectional area (Fig. 3.). The incision was sutured seperately with 5.0 Prolene. Fibrotic changes were observed on pathological samplings which were obtained from resected tissue. There were no complications and no recurrence of triggering after 12 months.
Fig. 2.
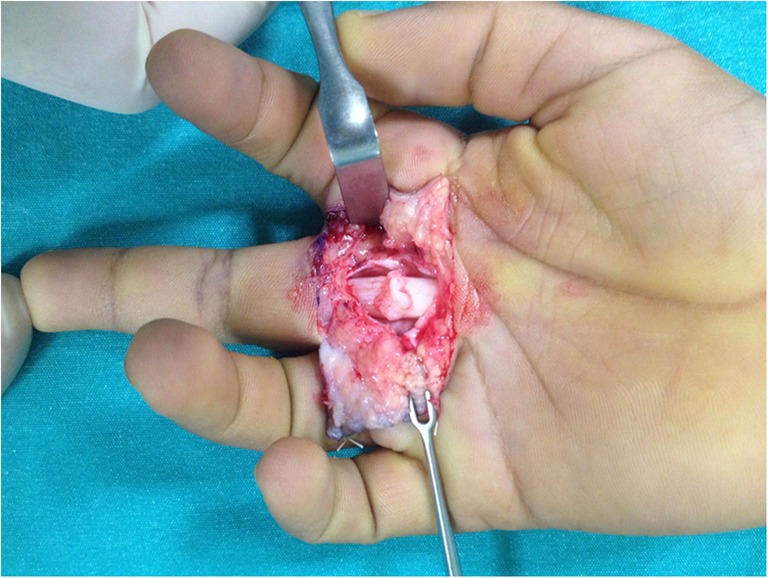
Released A1 pulley and fibrotic tissue due to partial flexor digitorum superficialis (FDS) tendon laceration
Fig. 3.
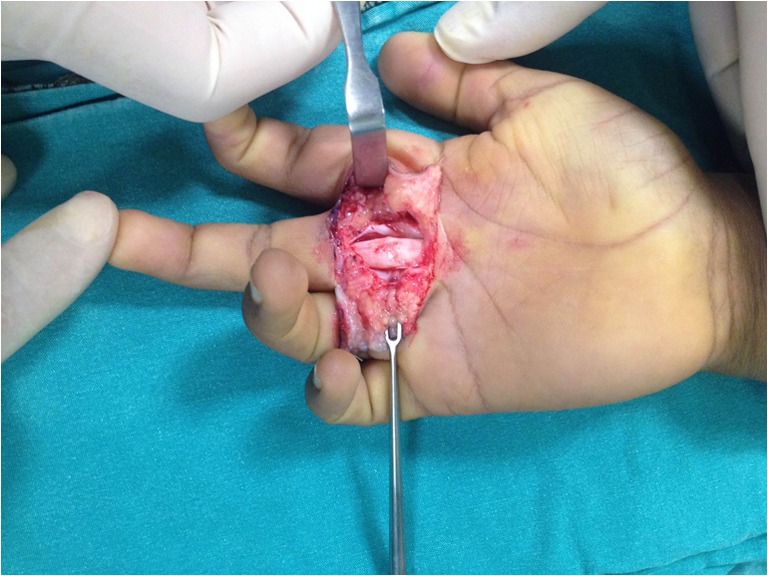
View after excision of fibrotic tissue
In conclusion, partial tendon laceration is an uncommon cause of TF in children, and few cases have been reported in the literature [10]. Partial tendon lacerations can be very difficult to diagnose unlike full-thickness lacerations and must be taken into account when dealing with trigger finger in after a penetrating injury.
Electronic Supplementary Material
Triggering of the third finger. There is no triggering by passive movements. The finger is brought to extension by applying an external force (By exerting force on the finger with thumb). (MP4 46002 kb)
Acknowledgments
Conflict of Interest
None
Funding
None
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Notta A. Recherches sur une affection particuliere des gaines tendineuses de la main. Arch Gen Med. 1850;24:142. [Google Scholar]
- 2.Rodgers WB, Waters PM. Incidence of trigger digits in newborns. J Hand Surg [Am] 1994;19(3):364–368. doi: 10.1016/0363-5023(94)90046-9. [DOI] [PubMed] [Google Scholar]
- 3.Cardon LJ, Ezaki M, Carter PR. Trigger finger in children. J Hand Surg [Am] 1999;24(6):1156–1161. doi: 10.1053/jhsu.1999.1156. [DOI] [PubMed] [Google Scholar]
- 4.Moon WN, Suh SW, Kim IC. Trigger digits in children. J Hand Surg (Br) 2001;26(1):11–12. doi: 10.1054/jhsb.2000.0417. [DOI] [PubMed] [Google Scholar]
- 5.Tordai P, Engkvist O. Trigger fingers in children. J Hand Surg [Am] 1999;24(6):1162–1165. doi: 10.1053/jhsu.1999.1162. [DOI] [PubMed] [Google Scholar]
- 6.Bae DS, Sodha S, Waters PM. Surgical treatment of the pediatric trigger finger. J Hand Surg [Am] 2007;32(7):1043–1047. doi: 10.1016/j.jhsa.2007.05.031. [DOI] [PubMed] [Google Scholar]
- 7.Seiler JG, 3rd, Kerwin GA. Adolescent trigger finger secondary to post-traumatic chronic calcific tendinitis. J Hand Surg [Am] 1995;20(3):425–427. doi: 10.1016/S0363-5023(05)80100-5. [DOI] [PubMed] [Google Scholar]
- 8.Van Heest AE, House J, Krivit W, Walker K. Surgical treatment of carpal tunnel syndrome and trigger digits in children with mucopolysaccharide storage disorders. J Hand Surg [Am] 1998;23(2):236–243. doi: 10.1016/S0363-5023(98)80120-2. [DOI] [PubMed] [Google Scholar]
- 9.Tsuyuguchi Y, Tada K, Kawaii H. Splint therapy for trigger finger in children. Arch Phys Med Rehabil. 1983;64(2):75–76. [PubMed] [Google Scholar]
- 10.Fujiwara M. A case of trigger finger following partial laceration of flexor digitorum superficialis and review of the literature. Arch Orthop Trauma Surg. 2005;125(6):430–432. doi: 10.1007/s00402-005-0823-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Triggering of the third finger. There is no triggering by passive movements. The finger is brought to extension by applying an external force (By exerting force on the finger with thumb). (MP4 46002 kb)


