Abstract
The juncturae tendinum and sagittal bands transmit precise forces through the dorsum of the hand. Both structures are integral in the mechanics of normal digital extension and in stabilization of the metacarpophalangeal (MCP) joints. Extensor tendon injury, or rupture/attenuation of sagittal bands and/or juncturae tendinum, may disrupt the kinematic chain and lead to a number of abnormal hand postures and motions. Early treatment of extensor tendon and/or sagittal band injury is dependent upon proper recognition of primary pathology. Proper evaluation and the use of special clinical tests should be implemented to rule out other pathologies. Once diagnosed, treatment may consist of relative motion splinting and standard pain/edema control measures to increase joint motion, tendon excursion, and functional use of the hand.
Keywords: Juncturae tendinum, Sagittal band, Extensor biomechanics, Cadaver dissection, Extensor quadriga, Swan neck deformity, Relative motion orthosis
Introduction
Extension of the digits is a complex process involving both extrinsic and intrinsic means, with assistance from several ligamentous structures. The three phalanges constitute an interdependent polyarticular chain, where lesions at one level of the chain may alter the balance of the entire digit and lead to characteristic deformities [1]. Normal balancing of this complex chain requires both linear and oblique forces to maintain digital extension. A disruption between any of the structures (i.e., bones, tendons, ligaments) may result in loss of chain equilibrium.
An intricate relationship is formed between the juncturae tendinum and sagittal bands. Both structures play a unique role in maintaining digital extension by stabilizing and mobilizing the extensor tendons at the MCP joints. In the case of rupture or attenuation of either structure, a set of severe consequences in joint motion and normal finger mechanics is observed. A cadaveric dissection was performed to illustrate how failure of either structure may alter hand kinematics during normal flexion and extension of the digits. Treatment guidelines are also discussed based on the complex relationship between these two structures.
MCP Anatomy
The extrinsic tendons at the MCP joint are formed by the extensor digitorum communis (EDC) tendon to each finger, the extensor indicis proprius (EIP) tendon to the index finger, and the extensor digiti minimi (EDM) tendon to the little finger. These tendons primarily extend the MCP joints, but are also weak extensors of the IP joints. At the level of the wrist, the EDC tendons are located in the fourth extensor compartment where they pass under the extensor retinaculum and diverge toward the fingers [1].
Just proximal to the MCP joints, the EDC tendons are interconnected by juncturae tendinum and intertendinous fascia (Fig. 1). The juncturae tendinum consist of bands of connective tissue that extend transversally and obliquely between the EDC tendons [2]. These bands have been described as ‘variable’ in anatomic studies, and have been shown to link motion between the extensor tendons [3]. Other functional roles of the juncturae tendinum include force redistribution, spacing of the EDC tendons, reducing an excessive load at the sagittal bands, and stabilization of the MCP joints [2].
Fig. 1.

Cadaver dissection showing the juncturae tendinum and sagittal bands
The sagittal bands, connective tissue structures on the dorsum of the MCP joints, help to maintain the EDC tendons over the midline of the joint (Fig. 2). These bands are dynamic structures that move with the extensor tendons during MCP joint motion [4]. The sagittal bands arise from the volar plate and deep transverse metacarpal ligaments, and extend dorsally to envelop the MCP joints. The sagittal bands also aid in digital extension, limit EDC slippage, prevent bowstringing of the tendons, and limit excessive extensor tendon excursion.
Fig. 2.

Cadaver dissection showing sagittal band anatomy
Other fibrous structures contributing to digital extension consist of the volar plate, the oblique retinacular ligament, the transverse retinacular ligament, and the triangular ligament. The volar plate attaches firmly to the volar aspect of the MCP joint and assists the sagittal bands in ‘pulling’ the EDC tendon over the metacarpal head with MCP extension. The oblique retinacular ligament links motion between the IP joints creating a tenodesis effect. The transverse retinacular ligament prevents excessive dorsal migration of the lateral bands, whereas the triangular ligament counterbalances this action by preventing excessive volar migration of the bands. Both ligaments play an important role in permitting adequate tendon motion and distributing precise forces across the joints.
The intrinsic muscles consist of the lumbrical and interosseous muscles. These muscles flex the MCP joints and extend the interphalangeal (IP) joints. By means of their distal insertions, the intrinsic muscles help to maintain MCP extension.
Mechanics of Normal Digital Extension
Digital extension from a fully flexed position is first initiated by the central slip from the EDC tendon at the proximal interphalangeal (PIP) joint. Extension at the PIP joint causes the lateral bands to migrate dorsally, increasing tension at the distal interphalangeal (DIP) joint. The intrinsic muscles continue to extend the IP joints through their insertions on the conjoined lateral bands. As the IP joints gain extension, the EDC tendon pulls on the sagittal bands, bringing them proximally over the metacarpal head. With assistance from the juncturae tendinum, the sagittal bands act as a ‘sling’ to bring the MCP joints into extension. Once the digits are in full extension, both the sagittal bands and juncturae tendinum help to maintain the extensor force by stabilizing the EDC tendons over the MCP joints. With help from the intrinsic muscles, MCP, PIP and DIP joint extension is maintained (Fig. 3) [1, 4].
Fig. 3.
Mechanics of digital extension. (1) Extension is first initiated by the central slip at the PIP joint. (2) Tension is created at the lateral bands causing them to migrate dorsally and extend the DIP joint. (3) The intrinsic muscles continue to extend the IP joints through their insertions on the lateral bands. (4) With proximal migration of the EDC tendon, the sagittal bands help to extend the MCP joints. Extension is maintained by means of the sagittal bands, juncturae tendinum, EDC tendon and intrinsic muscles. (Reproduced with permission; this information was originally published in Can J Plast Surg 2004;12(4):174–178)
Relationship Between the Sagittal Bands and Juncturae Tendinum
There is a direct relationship between the juncturae tendinum and the sagittal bands in the hand. During flexion and extension of the digits, the juncturae tendinum and sagittal bands help to link motion in the hand. Both structures help to reduce an excessive load placed onto the opposing structure, while contributing to MCP joint extension (Fig. 4). As demonstrated through a cadaveric dissection, and observed clinically in the hand, failure of either structure will lead to an imbalance of forces at the MCP joint due to a discrepancy in length and/or tension of nearby structures [4].
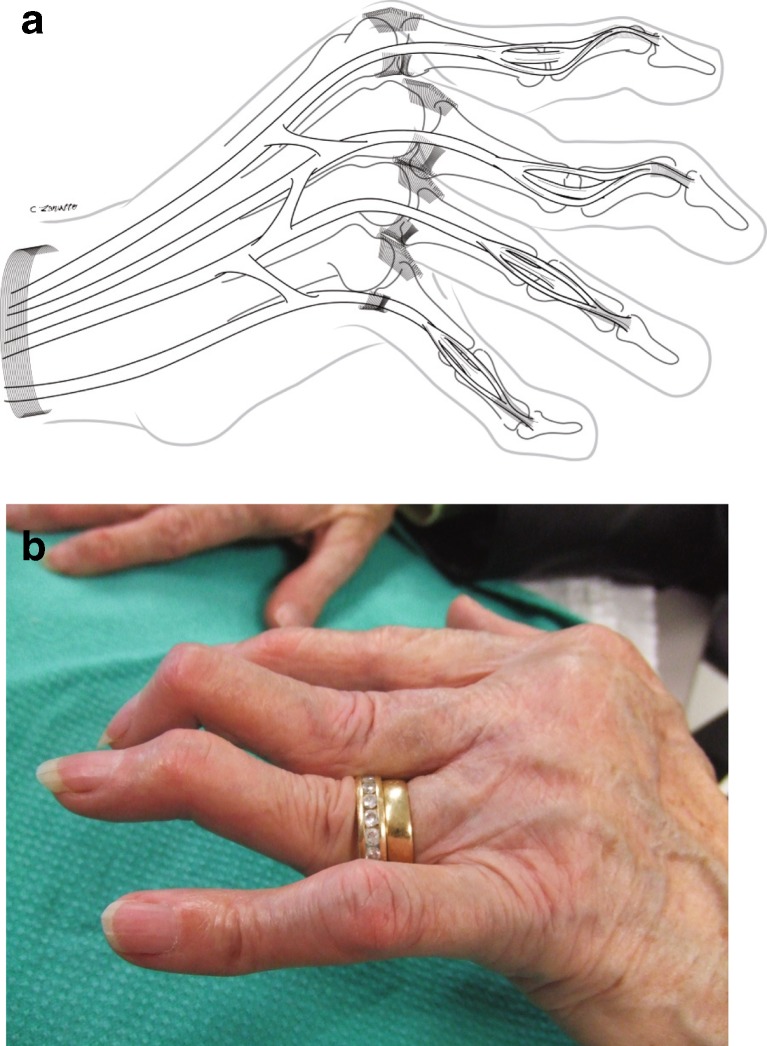
Fig. 4.
a Relationship between the sagittal bands and juncturae tendinum. b Sagittal band injury to the long finger resulting in ulnar subluxation of the long extensor tendon and increased tension placed on the transverse juncturae tendinum between the index and long finger
Complications
A sagittal band injury will typically result in ulnar subluxation of the EDC tendons. The extensor tendons are predisposed to falling ulnarly into the valleys between the MCP joints. This normal ulnar inclination at the MCP joints is due to asymmetry of the metacarpal heads and collateral ligaments, placement of extrinsic and intrinsic muscle insertions, and forward descent of the metacarpals with MCP flexion (due to height differential and interconnections with juncturae tendinum) [1]. As well, the radial sagittal bands are weaker than the ulnar sagittal bands [5–8]. In conditions such as rheumatoid arthritis, pathologic signs are often accentuated as the radial sagittal bands become ruptured or attenuated, and the extensor tendon falls into the ulnar valley of the MCP joints. As the EDC tendon falls ulnarly, a change in tension occurs at the level of the juncturae tendinum, whereby an increase or decrease in tension occurs. From a kinematic standpoint, increased tension on the juncturae tendinum will contribute to further ulnar subluxation of adjacent tendons, thereby altering normal motion of the hand (Fig. 5).
Fig. 5.
a Extensor quadriga resulting in loss of MCP joint extension in adjacent digits following a sagittal band injury (Reproduced with permission; this information was originally published in Can J Plast Surg 2004;12(4):174–178). b Note a sagittal band injury to the long finger resulting in ulnar subluxation of the EDC tendon with increased tension on the juncturae tendinum. c Ulnar subluxation of the EDC tendon to the long and ring finger
Less commonly, radial subluxation of the EDC tendon may result following a traumatic laceration to the ulnar sagittal band. In a study by Farrar and Kundra [9] it was observed that radial subluxation of the EDC tendon would not normally occur with complete division of the ulnar sagittal bands. In their study it was observed that only 1 out of 40 digits analyzed showed radial subluxation after complete division of the ulnar sagittal bands. However, when additional division of the corresponding juncturae tendinum was made, a further 5 tendons were noted to subluxate in the radial direction [9]. Finger position also played a key role in EDC tendon stabilization. In the same study it was shown that resisted flexion of adjacent digits increased tension on the radial juncturae tendinum of the affected digit, causing a destabilization force of the tendon toward the radial side (i.e., flicking motion of the long finger). During coordinated flexion however, the juncturae tendinum acted as stabilizers of the EDC tendons, where no subluxation was noted [9]. This study demonstrated the potential stabilizing role of the juncturae tendinum, dependent upon finger and wrist position, and sagittal band rupture.
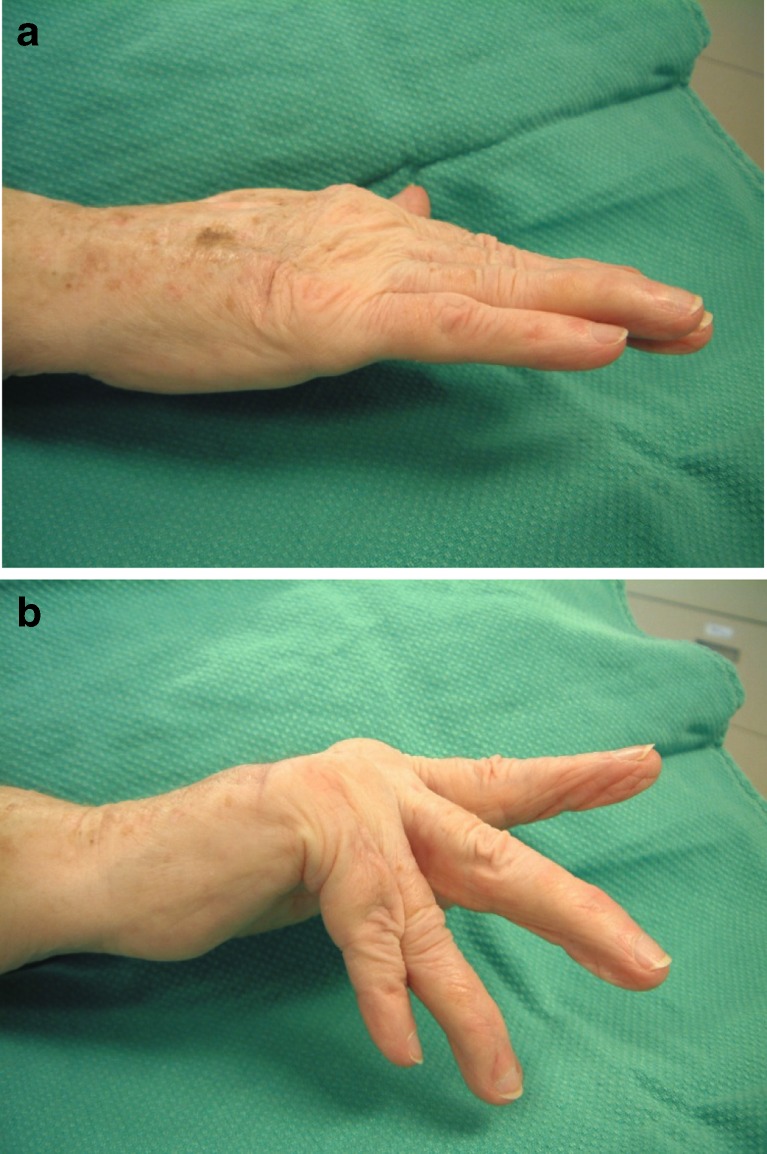
Specifically, the four extensor tendons in the hand are motored by the common EDC muscle belly. Effective motor function is dependent upon normal gliding amplitude of all four tendons. Lack of MCP extension in one finger will result in decreased excursion of the adjacent tendons through distal tension on the juncturae tendinum. When gliding amplitude is reduced in any of the extensor tendons, the extensor quadriga phenomenon will occur, resulting in decreased MCP extension (Fig. 5) [10]. Additional complications arising from extensor quadriga will result in interosseous muscle tightness and secondary swan neck deformity due to an increased load placed onto the extensor mechanism (Fig. 6) and possibly volar subluxation of the proximal phalanx in rheumatoid hands.
Fig. 6.
a and b Sagittal band injury to the long finger resulting in extensor quadriga and swan neck deformity. (Figure a - This information was originally published in Tech Hand Up Extrem Surg. 2006 Dec;10(4):206–11)
Isolated juncturae tendinum injuries are rare, and will typically result from a direct laceration to the hand. The juncturae tendinum assist with digital extension and help to reduce an extensor load across the sagittal bands [5].
With an extensor tendon injury proximal to zone IV, an increased load will be placed on the sagittal bands and juncturae tendinum with MCP joint motion. Careful examination is required to properly identify sagittal band, EDC and/or juncturae tendinum rupture/attenuation as an injury to one structure will lead to a predictable set of consequences in another.
Evaluation and Tests
A number of causes may lead to sagittal band and juncturae tendinum injury. Most commonly, these injuries result from trauma (i.e., forced MCP flexion, laceration, fracture) or from pathological conditions such as rheumatoid arthritis. A clear history may help to determine what structures are involved with loss of MCP joint motion.
To the inexperienced examiner, a sagittal band rupture may present itself like an extensor tendon injury or rupture of EDC. A classic test to reveal a sagittal band rupture is to passively place the digits into extension and actively hold them in place. If able to maintain full extension when passively placed, a long extensor injury or rupture is unlikely. A sagittal band rupture is evident if patients are unable to actively extend their digits from a flexed position (Fig. 7).
Fig. 7.
A test for sagittal band attenuation. a. When digits are passively placed into extension, patients are able to actively hold them in place b. However, a sagittal band rupture is evident if patients are unable to actively extend their digits from a flexed position. (This information was originally published in Tech Hand Up Extrem Surg. 2006 Dec;10(4):206–11)
Similarly, due to the anatomic arrangement of the juncturae tendinum, these structures have been found to mask an extensor tendon laceration. To rule out an extensor tendon laceration or rupture, patients are asked to maintain active extension of their digits. If patients are unable to maintain extension in this position, then an extensor tendon injury is likely. However, when coming from a flexed position, some extension of the digits will be possible due to ‘linkage’ of the juncturae tendinum. Further differential diagnosis may consist of a partial posterior interosseous nerve palsy, in which patients do not have active MCP extension due to loss of innervation to the EDC tendon. One method to distinguish between these types of injuries would be to assess the function of the EIP or extensor pollicis longus (EPL) tendon. Intact EPL and EIP function is suggestive of an EDC tendon laceration or rupture.
Treatment
Acute sagittal band injuries are treated by maintaining the MCP joints in relative extension and by limiting MCP flexion to a safe arc of motion (between 0 and 60° of flexion) [1]. This may be accomplished through an early controlled motion protocol using a static orthosis for both surgically and non-surgically repaired sagittal bands. A relative motion orthosis, or ‘yoke’ orthosis, places the affected MCP joint in relative extension while full IP motion is permitted within the orthosis for a 6 week period (Fig. 8). This orthosis helps to maintain the extensor tendons over the midline of the MCP joints, while reducing an excessive load on the sagittal bands and/or juncturae tendinum. Standard edema and pain control measures should also be implemented throughout the rehabilitation process to ensure optimal results and patient satisfaction.
Fig. 8.
A relative motion orthosis is made to place the affected long finger MCP joint in relative extension
In the case of an extensor tendon injury to one of the EDC tendons, a custom-moulded thermoplastic orthosis can also be fabricated to maintain the wrist in approximately 20–25° of extension. In an article by Minamikawa and colleagues [11], it was found that wrist positions of 21° or greater extension resulted in little to no tension in extensor tendon injuries in zones V and VI. Similarly, Howell and colleagues conducted cadaveric and intraoperative trials on zone V extensor tendon injuries of the long finger to assess tension on the repair [11]. Tendon gap was compared in cadaver trials ‘with’ and ‘without’ the yoke component in varying wrist positions. At 20° of wrist extension, no tendon gapping was noted with composite finger flexion when the yoke component was used, as compared to wrist neutral position, with and without the yoke component. Similar findings were observed with the intraoperative trial in which tendon gapping was found to be nonexistent with the yoke component and wrist in 20° of extension [12].
Discussion
A predictable set of consequences is observed following injury to the sagittal bands and/or juncturae tendinum injury. Loss of MCP extension will lead to an increased load placed on both the juncturae tendinum and sagittal bands. Volar subluxation of the MCP joints will occur with radial sagittal band weakness and ulnar inclination of the EDC tendons [13]. As well, extensor quadriga will develop and limit extension of the adjacent digits from the interconnections of the juncturae tendinum. Due to the intrinsic muscles being held in a shortened positioned, interosseous muscle tightness will occur and place an increased load on the extensor mechanism. Eventually, increased force placed on the extensor mechanism will result into a secondary swan-neck deformity and lead to subsequent joint contractures [4].
Treatment of these injuries is dependent upon proper recognition of primary pathology. Early identification of symptoms and clinical testing can help to recognize structures involved with loss of MCP joint motion. It is well known that extensor tendon injuries can be masked by the interconnections of the juncturae tendinum and sagittal bands. Proper evaluation and a battery of tests should be conducted to rule out certain pathologies. Once a firm diagnosis has been made, isolated sagittal band injuries may be treated with a custom made relative motion orthosis to allow for active-assisted MCP motion. A wrist component may be added in the case of an extensor tendon injury proximal to zone IV.
Conclusion
The juncturae tendinum and sagittal bands are integral in the mechanics of normal digital extension and at stabilizing the MCP joints. An extensor tendon and/or sagittal band injury may lead to a number of complications including volar subluxation of the MCP joints, extensor quadriga, swan neck deformity, and subsequent joint contractures. Direct attention should be placed on the intricate relationship between the sagittal bands and juncturae tendinum, and how failure of either structure may alter the normal kinematics of the hand during digital flexion and extension.
Acknowledgments
Conflict of Interest
Shrikant Chinchalkar, Chelsea Barker and Bobbi Owsley declare that they have no conflict of interest.
Contributor Information
Shrikant J. Chinchalkar, Phone: 519-646-6001, Email: schinchalkar@hotmail.com
Chelsea A. Barker, Email: barker_chelsea@hotmail.com
References
- 1.Tubiana R, Thomine JM, Mackin E. Examination of the hand and wrist. 2. New York: Informa Healthcare; 1998. [Google Scholar]
- 2.Von Schroeder H, Botte M, Gellman H. Anatomy of the juncturae tendinum of the hand. J Hand Surg [Am] 1990;15(4):595–602. doi: 10.1016/S0363-5023(09)90021-1. [DOI] [PubMed] [Google Scholar]
- 3.Agee JM, Guidera M. The functional significance of the juncturae tendinae in dynamic stabilization of the metacarpophalangeal joints of the fingers. J Hand Surg [Am] 1980;5:288–290. [Google Scholar]
- 4.Chinchalkar S, Pitts S. Dynamic assist splinting for attenuated sagittal bands in the rheumatoid hand. Technol Hand Up Extrem Surg. 2006;10(4):206–211. doi: 10.1097/01.bth.0000231581.70524.0c. [DOI] [PubMed] [Google Scholar]
- 5.von Schroeder H, Botte M. The functional significance of the long extensors and juncturae tendinum in finger extension. J Hand Surg [Am] 1993;18(4):641–647. doi: 10.1016/0363-5023(93)90309-Q. [DOI] [PubMed] [Google Scholar]
- 6.Young CM, Rayan GM. The sagittal band: anatomic and biomechanical study. J Hand Surg [Am] 2000;25(6):1107–1113. doi: 10.1053/jhsu.2000.18495. [DOI] [PubMed] [Google Scholar]
- 7.Rayan GM, Murray D, Chung KW, Kohrer M. The extensor retinacular system at the metacarpophalangeal joint. Anatomical and histological study. J Hand Surg (Br) 1997;22(5):585–590. doi: 10.1016/S0266-7681(97)80351-8. [DOI] [PubMed] [Google Scholar]
- 8.Andruss R, Herndon J. Ulnar subluxation of the extensor digitorum communis tendon: a case report and review of the literature. Iowa Orthop J. 1993;13(1):208–213. [PMC free article] [PubMed] [Google Scholar]
- 9.Farrar NG, Kundra A (2012) Role of the juncturae tendinorum in preventing radial subluxation of the extensor communis tendons after ulnar sagittal band rupture: a cadaveric study. ISRN Orthopaedics [DOI] [PMC free article] [PubMed]
- 10.Chinchalkar S, Gan BS, McFarlane RM, King GJ, Roth JH. Extensor quadriga: pathomechanics and treatment. Can J Plast Surg. 2004;12:174–178. doi: 10.1177/229255030401200405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Minamikawa Y, Yamaguchi T, Kambe K. Wrist position and extensor tendon amplitude following repair. J Hand Surg [Am] 1992;17(2):268–271. doi: 10.1016/0363-5023(92)90403-C. [DOI] [PubMed] [Google Scholar]
- 12.Howell J, Merritt W, Robinson S. Immediate controlled motion following zone 4–7 extensor tendon repair. J Hand Ther. 2005;18(2):182–190. doi: 10.1197/j.jht.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 13.von Schroeder HP, Botte MJ. Anatomy of the extensor tendons of the fingers: variations and multiplicity. J Hand Surg [Am] 1995;20(1):27–34. doi: 10.1016/S0363-5023(05)80053-X. [DOI] [PubMed] [Google Scholar]