Abstract
An ectopic opening of the common bile duct (CBD) into the duodenal bulb is a very rare congenital anomaly of the biliary system, which may cause recurrent duodenal ulcer or biliary diseases such as choledocholithiasis and cholangitis. Endoscopic retrograde cholangiopancreatography (ERCP) plays a major role in the diagnosis of this anomaly. We report two such cases: one in a 61-year-old man and the other in a 57-year-old man. In the first case, this anomaly caused acute cholangitis with multiple CBD stones, which were successfully treated by ERCP. In the second case, abdominal computed tomography showed pneumobilia, which was further evaluated using ERCP. Besides, this patient was diagnosed with an ectopic opening of the CBD associated with gallbladder cancer. We report these unusual cases and review the relevant medical literature.
Keywords: Ectopic opening, Common bile duct, Duodenal bulb, Acute cholangitis, Gallbladder neoplasms
INTRODUCTION
The major papilla of Vater is typically located in the posteromedial wall of the second portion of the duodenum, and is the main exit for the bile and pancreatic juices that flow down the common bile duct (CBD) and the main pancreatic duct (MPD). Sometimes, the opening of the CBD can be located in aberrant sites along the duodenum, mainly in the third or the fourth portion of the duodenum or rarely in the duodenal bulb.1,2,3,4,5 We present two cases in which the ectopic opening of the CBD is located in the duodenal bulb. Notably, our report includes a case associated with gallbladder cancer. To the best of our knowledge, such a case has never been previously described; therefore, we have discussed pathogenesis, diagnosis, and treatment in detail in this report.
CASE REPORTS
Case 1
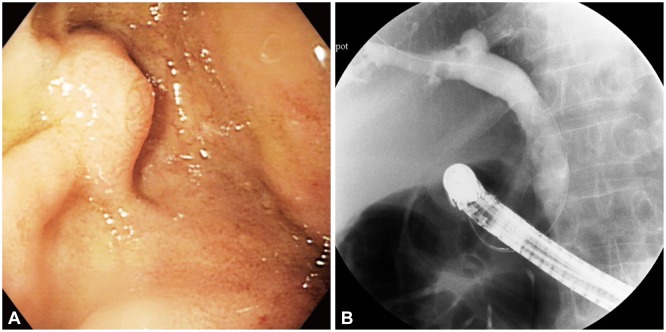
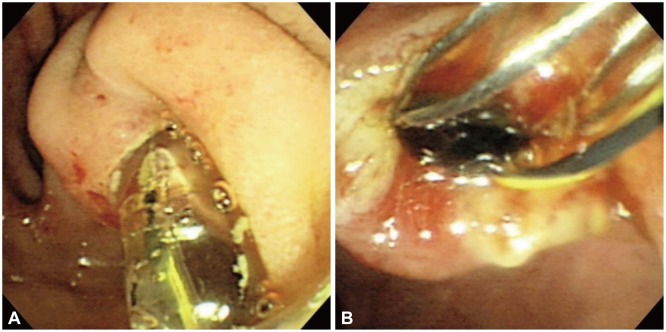
A 61-year-old man was admitted to our hospital because of abdominal discomfort since 3 days. He had been in good health without any previous medical history of note. About 23 years ago, he had undergone primary repair of bowel rupture. Physical examination did not show any abnormalities. Initial laboratory data showed elevated serum total bilirubin 1.48 mg/dL, serum aspartate aminotransferase 980 IU/L, serum alanine transaminase 274 IU/L, and serum C-reactive protein 10.8 mg/L. Serum amylase and lipase were within normal limits. Serum was negative for hepatitis B and C markers. Abdominal computed tomography (CT) scan showed multiple CBD stones with dilated bile duct and MPD. On esophagogastroduodenoscopy, the major papilla of Vater was not found in the second duodenal portion. It was finally located in the duodenal bulb (Fig. 1A). Endoscopic retrograde cholangiopancreatography (ERCP) was successfully performed via cannulation of the ectopic opening in the duodenal bulb. Dilated CBD with multiple stones was directly visualized radiographically (Fig. 1B) by injecting contrast media via the orifice. The patient underwent dilatation of the papilla with a balloon catheter (CRE wire-guided balloon dilator 12 to 15 mm; Boston Scientific, Marlborough, MA, USA), and a basket was used to remove the stones (Fig. 2). He was discharged without complications after the procedure.
Fig. 1. Endoscopic retrograde cholangiopancreatography showing the major papilla of Vater located in the duodenal bulb (A) and dilatation of the common bile duct with multiple floating filling defects (B).
Fig. 2. Endoscopic papillary balloon dilation was performed with a balloon catheter (A) and common bile duct stones were removed using a basket (B).
Case 2
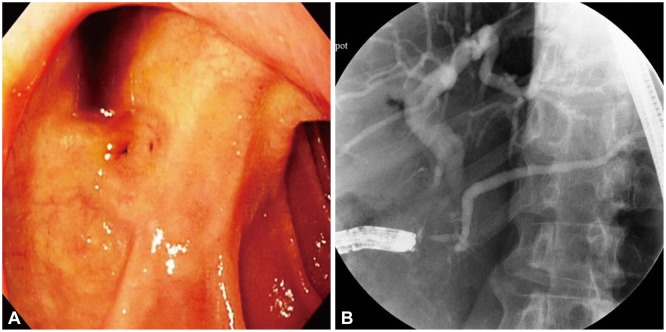
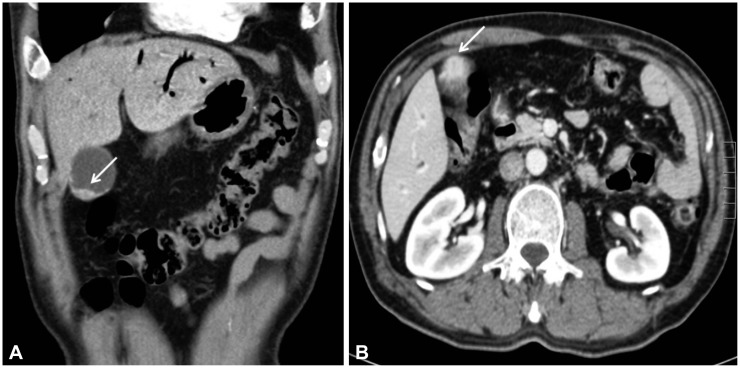
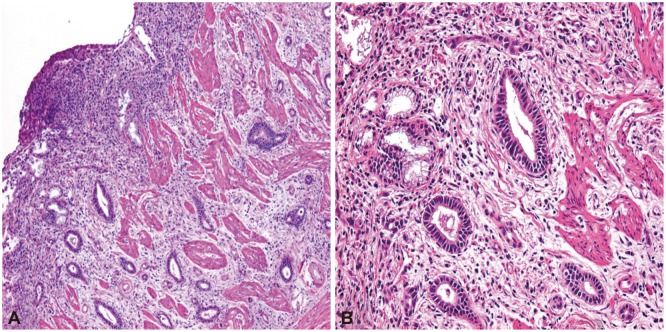
A 57-year-old man was referred to our hospital for further evaluation of pneumobilia. He was complaining of nausea for 1 month. He had no past medical history of note. On admission, physical examination was unremarkable. Initial laboratory findings were normal. On abdominal CT, diffuse pneumobilia was evident, and a communication was suspected between the duodenal bulb and the extrahepatic bile duct. For confirmation, ERCP was performed. ERCP showed an ectopic opening of the major papilla of Vater in the duodenal bulb (Fig. 3A). We cannulated the ectopic opening and injected contrast media via the orifice. We found that the CBD and MPD were communicating with the duodenal bulb (Fig. 3B). After 9 months, abdominal CT scan showed focal nodular wall thickening with enhancement of the gallbladder (Fig. 4). Consequently, the patient underwent radical cholecystectomy with hepaticojejunostomy as gallbladder cancer was suspected. Histopathological examination revealed a moderately differentiated adenocarcinoma arising from the gallbladder and extending into the perimuscular connective tissue (Fig. 5). After the operation, he was discharged without complications.
Fig. 3. Endoscopic retrograde cholangiopancreatography showing the major papilla of Vater located in the duodenal bulb (A) and mild dilatation of the common bile duct along with normal appearance of the main pancreatic duct (B).
Fig. 4. Contrast-enhanced computed tomography scan showing focal nodular wall thickening with enhancement (arrows) of the gallbladder in the coronal view (A) and in the axial view (B).
Fig. 5. Microscopic examination of the resected gallbladder showing a moderately differentiated adenocarcioma extending into the perimuscular connective tissue (A: H&E stain, ×40; B: H&E stain, ×100).
DISCUSSION
The etiology of ectopic opening of the CBD has been ascribed to unidentified errors in embryogenesis. The liver originates from the primitive hepatic furrow, which, during embryogenesis, is divided into the pars hepatica and the pars cystica. The pars hepatica develops into the liver and the hepatic ducts, while the pars cystica develops into the gallbladder and the cystic duct. The CBD originates from the hepatic antrum, which is the common area of the hepatic furrow. According to the hypothesis of Boyden, anomalous drainage of the CBD occurs due to a disproportional elongation and early subdivision of the primitive hepatic furrow.6,7
An ectopic opening of the CBD has a frequency of 5.6% to 23% and is most commonly located distal to the second duodenal portion, around the third and the fourth duodenal portions.8 In contrast, ectopic papillae in the duodenal bulb are extremely rare. Previous reports have shown diverse complications of ectopic papillae, including gallstone, choledocholithiasis, obstructive jaundice, cholangitis, pancreatitis, and peptic ulcer.1,5 In our patients, one had acute cholangitis with multiple CBD stones and the other had gallbladder cancer. Notably, gallbladder cancer has not been previously reported as a complication. There may be different possible explanations for these complications. First, the hook-shaped configuration of the distal CBD may be associated with bile stasis, which could lead to choledocholithiasis.7 Second, a poorly developed or absent sphincter of Oddi permits reflux of intestinal bacteria and duodenal contents into the biliary system, which could cause cholangitis in association with biliary obstruction.4,5,6 In addition, biliary stasis or reflux may play a central role in the process of carcinogenesis. The probable sequence of events may be pancreatobiliary reflux leading to inflammation which, in turn, may result in dysplasia with or without intestinal metaplasia, and finally resulting in an invasive carcinoma. However, further studies are needed to confirm the association between ectopic opening of the CBD and gallbladder cancer.
Although plain upper GI barium radiography,9 intraoperative cholangiography,10 CT,11 and endoscopic ultrasonography12 have been used, ERCP is the "gold standard" for diagnosing ectopic opening of the CBD. As described by Lee et al.,5 the diagnosis of an ectopic opening of the CBD into the duodenal bulb can be established on ERCP as follows: (1) an orifice is observed in the bulb by duodenoscopy or upper endoscopy, and the bile duct and/or the pancreatic duct are directly visualized radiographically when contrast is injected via this opening; (2) there is a direct drainage of the CBD into the duodenal bulb without evidence of any other drainage into the duodenum on cholangiography; and (3) there is no evidence of a papilla-like structure in the second or the third portion of the duodenum on duodenoscopy. We clearly observed these diagnostic requirements in both of our cases.
Fistula secondary to ulcer or choledocholithiasis, spontaneous or iatrogenic surgical fistula, and surgical choledochoenteric diversion should be included in the differential diagnosis.2 Nonvisualization of the major papilla in the second duodenal portion may be the key for ruling out these conditions. In addition, as the dilated CBD can terminate abruptly, it may sometimes be difficult to differentiate anomalous drainage of the CBD from periampullary cancer.8 In both of our cases, these differential diagnoses could be ruled out because the major papilla of Vater was not observed in the second duodenal portion. Although the location of the minor papilla in an ectopic opening of the CBD into the duodenal bulb has not been previously reported, we could not identify the minor papilla within the observable range in both of our cases. Therefore, further studies are needed to confirm the association between an ectopic opening of the CBD into the duodenal bulb and the location of the minor papilla.
An ectopic papilla of Vater in the duodenal bulb increases the difficulty in performing therapeutic interventions during ERCP. This anomaly has a high risk of perforation and bleeding during endoscopic sphincterotomy because the intramural portion of the duct is not fully developed.8 Therefore, balloon dilatation may be the preferred technique for removing the stones. However, if inserting the balloon catheter into the ectopic opening is difficult due to acute angulation of the distal CBD and deformity of the bulb, stent installation or surgery may be necessary. Surgical treatments include choledochoenterostomy, surgical stone extraction by choledochotomy, and rarely pancreatoduodenectomy.5 In our case, CBD stones were successfully removed without any complications by balloon dilatation of the major papilla.
In conclusion, although ectopic opening of the CBD into the duodenal bulb is an extremely rare anomaly, it can have important clinical implications. This anomaly should be considered particularly when the major papilla of Vater cannot be found in the second duodenal portion in patients with recurrent biliary pain, cholangitis, and/or recurrent duodenal ulcer. Although further studies are necessary, endoscopic treatment such as balloon dilatation of the orifice along with stone extraction should be preferred over surgical treatment in these patients. In addition, clinicians should keep in mind that this anomaly can be associated with biliary tract cancer.
Footnotes
Conflicts of Interest: The authors have no financial conflicts of interest.
References
- 1.Kanematsu M, Imaeda T, Seki M, Goto H, Doi H, Shimokawa K. Accessory bile duct draining into the stomach: case report and review. Gastrointest Radiol. 1992;17:27–30. doi: 10.1007/BF01888503. [DOI] [PubMed] [Google Scholar]
- 2.Pereira-Lima J, Pereira-Lima LM, Nestrowski M, Cuervo C. Anomalaous location of the papilla of vater. Am J Surg. 1974;128:71–74. doi: 10.1016/0002-9610(74)90237-2. [DOI] [PubMed] [Google Scholar]
- 3.Moosman DA. The surgical significance of six anomalies of the biliary duct system. Surg Gynecol Obstet. 1970;131:655–660. [PubMed] [Google Scholar]
- 4.Kubota T, Fujioka T, Honda S, et al. The papilla of Vater emptying into the duodenal bulb. Report of two cases. Jpn J Med. 1988;27:79–82. doi: 10.2169/internalmedicine1962.27.79. [DOI] [PubMed] [Google Scholar]
- 5.Lee SS, Kim MH, Lee SK, et al. Ectopic opening of the common bile duct in the duodenal bulb: clinical implications. Gastrointest Endosc. 2003;57:679–682. doi: 10.1067/mge.2003.210. [DOI] [PubMed] [Google Scholar]
- 6.Boyden EA. The problem of the double ductus choledochus (an interpretation of an accessory bile duct found attached to the pars superior of the duodenum) Anat Rec. 1932;55:71–93. [Google Scholar]
- 7.Boyden EA. Congenital variations of the extrahepatic biliary tract: a review. Minn Med. 1944;27:932–933. [Google Scholar]
- 8.Disibeyaz S, Parlak E, Cicek B, et al. Anomalous opening of the common bile duct into the duodenal bulb: endoscopic treatment. BMC Gastroenterol. 2007;7:26. doi: 10.1186/1471-230X-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hwang SS, Park SY. Ectopic opening of the common bile duct into the duodenal bulb: a case report. J Korean Soc Radiol. 2009;61:109–112. [Google Scholar]
- 10.Lindner HH, Peña VA, Ruggeri RA. A clinical and anatomical study of anomalous terminations of the common bile duct into the duodenum. Ann Surg. 1976;184:626–632. doi: 10.1097/00000658-197611000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee HJ, Ha HK, Kim MH, et al. ERCP and CT findings of ectopic drainage of the common bile duct into the duodenal bulb. AJR Am J Roentgenol. 1997;169:517–520. doi: 10.2214/ajr.169.2.9242767. [DOI] [PubMed] [Google Scholar]
- 12.Krstic M, Stimec B, Krstic R, Ugljesic M, Knezevic S, Jovanovic I. EUS diagnosis of ectopic opening of the common bile duct in the duodenal bulb: a case report. World J Gastroenterol. 2005;11:5068–5071. doi: 10.3748/wjg.v11.i32.5068. [DOI] [PMC free article] [PubMed] [Google Scholar]