Abstract
Objectives:
No study has described low back pain (LBP) treatment choices among physical therapists (PTs) in the United States (US) in the new millennium. Intervention for LBP in the new millennium is largely based on evidence-based practice (EBP) recommendations. The purpose of this study was twofold: (a) to describe PTs' preferences for treating acute and subacute non-specific LBP in Florida and to compare these preferences to EBP guideline recommendations and (b) to compare outpatient musculoskeletal therapist (MSPT) choices for management of acute and subacute LBP to non-outpatient musculoskeletal therapist (NMSPT) choices.
Methods:
The data were collected with an electronic survey. Study participants selected treatment choices for acute and subacute LBP clinical vignettes.
Results:
A total of 327 PTs participated in the study, of which 128 worked in outpatient musculoskeletal settings. The most common treatment choices for acute and subacute LBP were home exercise program, exercise in the clinic, back care education, joint mobilization, ice/heat, and interferential current. The EBP adherence rate for acute LBP was 30% for MSPTs and 15% for NMSPTs. Thirty-seven percent (37%) of MSPTs and 30% of NMSPTs adhered to EBP guidelines for subacute LBP.
Discussion:
The EBP adherence rate for management of acute and subacute LBP was low. Spinal manipulation was underutilized for management of acute LBP, and passive therapeutic procedures were overutilized for subacute LBP. Physical Therapy schools and professional associations should reemphasize the benefits of spinal manipulation to manage non-specific acute LBP and active interventional procedures to manage subacute LBP.
Keywords: Low back pain, Practice description, Evidence-based practice, Clinical guidelines, Physical therapy
Introduction
Low back pain (LBP) is the most common musculoskeletal condition seen by physical therapists (PTs) in the United States (US). The lifetime incidence of an acute episode of LBP ranges from 60 to 90%, and 30% of those with LBP may develop a chronic condition.1,2 In the early 2000s, LBP healthcare costs varied from $20 to $50 billion a year in the US.3,4 Because of the socioeconomic consequences of LBP, it is important that PTs engage in the most efficient management practices available for LBP.
Evidence-based practice (EBP) is the gold standard clinical practice method for PTs and other healthcare professionals, as it allows clinicians to reach the best possible patient outcomes with the lowest healthcare costs.5–7 Evidence-based practice is the process of making clinical decisions based on an integration of the best available evidence with the practitioner’s clinical expertise and the patient’s values.5,6 Because of the high incidence, prevalence, and recurrence rates of LBP, at least 1000 randomized clinical trials on the management of LBP have been conducted.8,9 To facilitate the use of EBP, researchers have summarized these randomized clinical trials into clinical practice guidelines to help clinicians make decisions about the best healthcare for LBP. Clinical practice guidelines are systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances. Their purpose is to make explicit recommendations with a definite intent to influence what clinicians do.10,11 Clinical practice guidelines function to influence clinical decision making by presenting the clinician with clear recommendations about what to do in particular situations.10 Low back pain management in the new millennium should be based on EBP recommendations.12
To date, only four studies describe the physical therapy management of LBP in the US.13–16 These latter studies were conducted in the 1990s when EBP was not widely discussed for clinical choices. It is easy to note that contemporary EBP recommendations for management of LBP were not commonly practiced in the 1990s. Passive modalities like heat and ultrasound were popular, even for patients with chronic LBP. Also, high velocity low amplitude (HVLA) spinal manipulation was not popular for LBP at the time, even for patients with non-specific LBP without radiculopathy.13–16 The present authors believe that therapists’ preferences for LBP management changed in the 2000s, particularly because of the development of the American Physical Therapy (APTA) Manipulation Task Force that was created to foster the teaching of manipulation in physical therapy curriculum and also because of the APTA 2020 Vision Statement, which states that patient treatment should be based on evidence.12,17 Therefore, the current authors decided to explore therapists’ preferences for treating acute and subacute LBP in the 2000s to determine whether therapists adhered to EBP recommendations to manage patients with LBP.
No study has described LBP management choices among PTs in the US in the new millennium. The purpose of this study was to describe therapists’ choices for managing acute and subacute LBP in Florida. The specific objective of this study was threefold. First, the present investigators wanted to describe physical therapy choices for management of acute and subacute LBP in Florida. Second, the investigators examined whether PTs in Florida adhered to EBP guideline recommendations for treating non-specific acute and subacute LBP. Third, the investigators compared outpatient musculoskeletal therapist (MSPT) choices for management of acute and subacute LBP to non-outpatient musculoskeletal therapist (NMSPT) choices. Adherence to EBP guidelines for treatment of LBP is associated with better patient outcome and reduced treatment costs.18,19
Methods
Sample
The sample was selected from the population of licensed PTs in the state of Florida. Information regarding the licensed PTs in Florida was collected from the Florida Department of Health, Division of Medical Quality Assurance. Of the 22 000 PTs licensed to work in Florida in 2006, 15% (2804 PTs) had an e-mail address listed with the Florida Department of Health. Study participants were divided into two groups: (a) therapists working primarily in outpatient musculoskeletal settings (MSPTs) and (b) NMSPTs working in multiple settings, home health, neurological or musculoskeletal inpatient settings, school systems, academia, etc. All Florida-licensed PTs with listed e-mail addresses were invited to participate in the study. All participants read a consent form approved by the Internal Review Board at Nova Southeastern University and electronically agreed to participate in the study. Data collection occurred in the second semester of 2007.
Research design
This was a descriptive study; the data for the study were collected with an electronic survey. Participants were asked to make their treatment selection choices based on hypothetical patient scenarios as has been done in prior studies.20,21 Clinical vignettes are valid and acceptable tools to measure clinical decision making and observance to EBP guidelines.21–23 Study participants were presented with an acute and a subacute LBP vignette (Appendix 1). In the acute vignette, the patient had LBP for 1 week prior to physical therapy intervention, whereas in the subacute vignette, the patient had LBP for 6 weeks prior to physical therapy intervention. Both scenarios had a patient with non-specific LBP (no radiculopathy or red flags) and impaired mobility. The therapist participants were instructed to select a minimum of two and a maximum of five preferred treatment procedures that they would use to manage the patient in each of the two clinical scenarios (Appendix 2). Adherence to EBP guidelines was based on this treatment selection. Three expert PTs validated the specific treatment techniques selected for the survey. All three experts hold a PhD and multiple peer-reviewed publications in musculoskeletal physical therapy. Two hold the title of full professor and one of an associate professor in physical therapy programs in the US or Canada. One is a fellow of the American Academy of Orthopedic Manual Therapy with 7 years of clinical experience. Another has over 30 years of clinical experience and has published a world-renowned textbook in orthopedic physical assessment.
Definitions regarding treatment adherence to both acute and subacute vignettes were based on EBP guideline recommendations published during the 6-year period (2002–2007) prior to data collection. The six-year timeline was intentionally used to prevent outdated practice guidelines from affecting the results of the current investigation. There were 12 guidelines published between 2002 and 2007.1,2,24–33 The definitions were based on the recommendations from the majority of the guidelines (75% of the guidelines or at least 9 guidelines out of 12).1,2,24–26,28,29,31,32 The present authors used guideline recommendations that were based on at least one higher quality randomized clinical trial.
For the acute LBP scenario, therapists adhered to EBP guideline recommendations for the management of LBP if their treatment choices included manual therapy (spinal mobilization or manipulation) and patient education. Therapists whose preferred management did not include both or only included manual therapy or education were not deemed adherent to EBP guidelines for acute LBP.
For the subacute LBP scenario, therapists adhered to EBP guideline recommendations for the management of LBP if their treatments of choice included exercises in the clinic and patient education (with or without home exercise program). Therapists whose preferred management did not include both or only included exercises in the clinic or education were not deemed adherent to EBP guidelines for subacute LBP. All therapists who included passive treatment approaches such as bed rest, laser, ultrasound, transcutaneous electrical nerve stimulation (TENS), interferential therapy, or magnetic therapy were not deemed adherent to EBP management of subacute LBP.
The PTs answering the electronic survey were not trained in the criteria for guideline adherence used in this study. This is similar to previous studies that investigated therapist adherence to LBP guidelines in the US18 and the United Kingdom.23 The intent of the study was not to investigate whether therapists were aware of or trained in the utilization of EBP guidelines, instead, the purpose of the study was to study whether therapists made treatment recommendations consistent with EBP.
Instrument
The self-report survey used in this questionnaire was adapted from Li and Bombardier's20 survey investigating the physical therapy management of acute and subacute LBP. A committee of three expert PTs (described previously in this paper) validated the survey used in the present investigation. The committee collectively considered the survey to have face validity and considered the questions of the survey suitable for the purpose of this study. Inter-item reliability was not assessed statistically because the survey did not include multiple items addressing the same content areas. The scenarios in the survey scored 100% in the Flesch reading easy test and 1.2 in the Flesch–Kincaid grade level test;34 these readability scores indicated that the English used in the survey was extremely easy to comprehend.35,36
Data analysis
Descriptive statistics was used in this study to describe the demographic characteristics of the sample (age, gender, clinical experience, patient caseload, LBP patient caseload, and continuing education courses attended in manual therapy). The investigators described the treatment choices for the therapists by rate (percentage). The therapists were given 25 treatment options to choose from Appendix 2. The present authors used the chi-square to compare MSPTs versus NMPTS adherence to EBP guideline recommendations for acute and for subacute LBP.
Results
Participant demographics
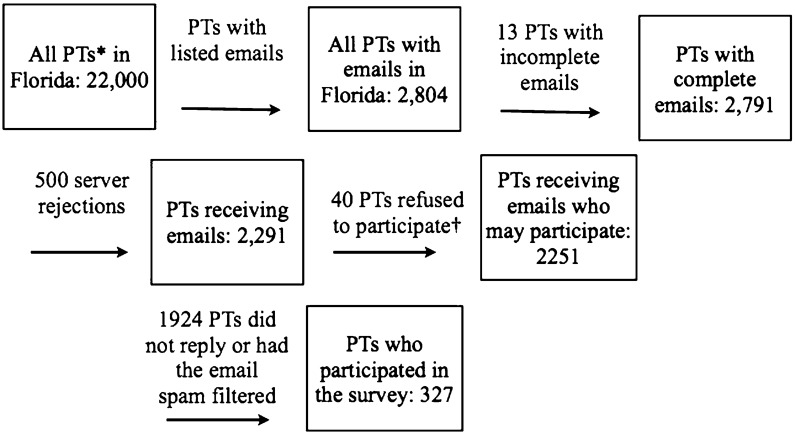
A total of 327 out of 2804 emailed PTs participated in the study (Fig. 1). The response rate was 14.5%. The demographics of the participants is in Table 1. In all, 61% of the therapists (n = 199) were NMSPTs. From these latter 199 therapists, 140 (70.4%) had a 10% caseload or more of patients with LBP. Thirty-nine percent of the therapists (n = 128) were MSPTs; 95% of these had a 10% caseload or more of patients with LBP. Musculoskeletal therapists attended more continuing education courses in manual therapy than NMSPTs (chi2 [1, n = 310] = 20.289, P = 0.001).
Figure 1.
Flowchart outlining participant recruitment and participation. *PTs: physical therapists; †PTs refused because they did not work with low back pain (LBP) or with orthopedics, or they no longer practiced in the state of Florida.
Table 1. Participant demographics.
| Participants | N = 327 |
| Age |
 =38, sigma = 9, range = 24–65 =38, sigma = 9, range = 24–65 |
| Gender | ♀ = 61.2%, ♂ = 38.8% |
| Clinical experience |
 =15.8, sigma = 8.2, range = 5–25 =15.8, sigma = 8.2, range = 5–25 |
| Post-professional training in musculoskeletal medicine (%) | |
| MTC | 5.5 |
| OCS | 4 |
| MDT | 1.8 |
| Multiple | 9.2 |
| Other | 3 |
| None | 76.5 |
| Work facility (%) | |
| Outpatient musculoskeletal | 39.1 |
| Outpatient multiple setting | 14.4 |
| Inpatient | 13.0 |
| All others | 33.5 |
| MSPTs (%) | NMSPTs (%) | |
| Number of continuing education courses in manual therapy* | ||
| ⩽1 | 37.2 | 57.7 |
| 2 | 13.2 | 13.2 |
| 3 | 09.9 | 10.0 |
| ⩾4 | 39.7 | 17.5 |
| Patient caseload | ||
| <5 | 7.0 | 14.6 |
| 5–10 | 24.2 | 55.3 |
| 11–15 | 51.6 | 26.2 |
| >15 | 17.2 | 4.0 |
| LBP patient caseload | ||
| <10% | 4.7 | 31.7 |
| 10–25% | 14.0 | 28.2 |
| 26–40% | 42.2 | 25.1 |
| >40% | 39.1 | 15.1 |
LBP: low back pain; MSPTs: therapists working in musculoskeletal outpatient settings; NMSPTs: therapists working in non-musculoskeletal outpatients settings; MTC: manual therapist certification; OCS: orthopedic clinical specialist; MDT: mechanical diagnosis and treatment.
*Significant statistical difference between MSPTs versus NMSPTs (comparison between number of manual therapy courses ≤1 vs ≧4).
Management of acute LBP
The treatment choices for acute LBP are displayed in Table 2. The five most common treatment choices for acute LBP for all participants were home exercise program (82.6%, n = 270), exercise in the clinic (77.1%, n = 252), patient education (70%, n = 229), ice/heat (58.3%, n = 191), and spinal mobilization (34.9%, n = 114). The five most common treatment choices for acute LBP for MSPTs were home exercise program (82.8%, n = 106), exercise in the clinic (81.3%, n = 104), patient education (69.5%, n = 89), interferential current (67.2%, n = 86), and spinal mobilization (54.7%, n = 70). The five most common treatment choices for acute LBP for NMSPTs were home exercise program (82.4%, n = 164), exercise in the clinic (75.4%, n = 150), patient education (70.4%, n = 140), ice/heat (66.8%, n = 133), and back school (35.2%, n = 70).
Table 2. Treatment choices for non-specific acute low back pain (LBP).
| Participants | PTs†† | (%) | MSPTs† | (%) | NMSPTs‡ | (%) |
| EBP§ recommends | ||||||
| Education on back care | 229 | 70.0 | 89 | 69.5 | 140 | 70.4 |
| Spinal manipulation* | 21 | 6.3 | 18 | 14.1 | 3 | 1.5 |
| Spinal mobilization* | 114 | 34.9 | 70 | 54.7 | 44 | 22.1 |
| Lacking or conflicting EBP§ to recommend | ||||||
| Acupuncture | 7 | 2.1 | 2 | 1.6 | 5 | 2.5 |
| Back school | 98 | 30.0 | 28 | 21.9 | 70 | 35.2 |
| Biofeedback | 1 | 0.3 | 0 | 0.0 | 1 | 0.5 |
| Ice or heat | 194 | 59.3 | 061 | 47.7 | 133 | 66.8 |
| Electrical stimulation | 60 | 18.3 | 20 | 15.6 | 40 | 20.1 |
| Exercise in the clinic | 254 | 77.1 | 104 | 81.3 | 150 | 75.4 |
| Interferential current | 86 | 26.3 | 86 | 67.2 | 0 | 0.0 |
| Laser | 3 | 0.9 | 1 | 0.8 | 2 | 1.0 |
| Lumbar corset | 5 | 1.5 | 1 | 0.8 | 4 | 2.0 |
| Ultrasound | 49 | 14.7 | 14 | 10.9 | 35 | 17.6 |
| EBP§ does not recommend | ||||||
| Bed rest | 1 | 0.3 | 0 | 0.0 | 1 | 0.5 |
| Mechanical traction | 4 | 1.2 | 2 | 01.6 | 2 | 1.0 |
| Refer to physician specialist | 3 | 0.9 | 0 | 0.0 | 3 | 1.5 |
| Refer to psychologist | 1 | 0.3 | 0 | 0.0 | 1 | 0.5 |
| TENSδ | 28 | 8.4 | 9 | 7.0 | 19 | 9.6 |
| EBP§ does not discussλ | ||||||
| McKenzie exercise | 58 | 17.7 | 23 | 17.9 | 35 | 17.6 |
| Refer to group exercise | 3 | 0.9 | 1 | 0.8 | 2 | 1.0 |
| Work conditioning | 3 | 0.9 | 0 | 0.0 | 3 | 1.5 |
| Work hardening | 37 | 11.1 | 11 | 8.6 | 26 | 13.1 |
| Work modification | 27 | 8.1 | 8 | 6.3 | 19 | 9.6 |
| Total participants | 327 | 100 | 128 | 100 | 199 | 100 |
§ EBP: evidence-based practice.
†† PTs: physical therapists.
† MSPTs: physical therapists in outpatient musculoskeletal setting.
‡ NMSPTs: physical therapists not working in outpatient musculoskeletal setting.
λ Evidence not discussed in the majority of guidelines for non-specific acute LBP.
*Significant statistical difference between MSPTs versus NMSPTs.
δ TENS: transcutaneous electrical nerve stimulation.
In terms of EBP guideline adherence for the acute LBP scenario, MSPTs performed at a statistically significant higher rate than NMSPTs (chi2 [1, n = 327] = 20.269, P = 0.001). This difference was related to the choice of manual therapy rather than patient education. There was no statistically significant difference for the choice of patient education between MSPTs and NMSPTs (chi2 [1, n = 327] = 0.025, P = 0.874). However, there was a statistically significant difference between MSPTs and NMSPTs for spinal mobilization (chi2 [1, n = 327] = 36.404, P = 0.001) and manipulation (chi2 [1, n = 327] = 12.929, P = 0.001).
Management of subacute LBP
The treatment choices for subacute LBP are displayed in Table 3. The five most common treatment choices for subacute LBP for all participants were home exercise program (77.7%, n = 254), exercise in the clinic (74.9%, n = 245), education (57.2%, n = 187), spinal mobilization (49.5%, n = 162), and ice/heat (46.2%, n = 151). The five most common treatment choices for subacute LBP for MSPTs were home exercise program (85.5%, n = 109), exercise in the clinic (79.7%, n = 102), spinal mobilization (64.1%, n = 82), education (57.8%, n = 74), and ice/heat (33.6%, n = 43). The five most common treatment choices for subacute LBP for NMSPTs were home exercise program (72.4%, n = 144), exercise in the clinic (71.9%, n = 143), education (56.8%, n = 113), ice/heat (54.3%, n = 108), and spinal mobilization (40.2%, n = 80).
Table 3. Treatment choices for subacute low back pain (LBP).
| Participants | PTs†† | (%) | MSPTs† | (%) | NMSPTs‡ | (%) |
| EBP§ recommends | ||||||
| Exercise in the clinic | 245 | 74.9 | 102 | 79.7 | 143 | 71.9 |
| Education on back care | 187 | 57.2 | 74 | 57.8 | 113 | 56.8 |
| Lacking or conflicting EBP to recommend | ||||||
| Acupuncture | 6 | 1.8 | 1 | 0.8 | 5 | 2.5 |
| Back school | 85 | 26.0 | 26 | 20.3 | 59 | 29.7 |
| Lumbar corset | 6 | 1.8 | 1 | 0.8 | 5 | 2.5 |
| McKenzie exercise | 80 | 24.5 | 26 | 20.3 | 54 | 27.1 |
| Spine manipulation | 19 | 5.8 | 14 | 10.9 | 5 | 2.5 |
| Spine mobilization | 162 | 49.5 | 82 | 64.1 | 80 | 40.2 |
| EBP§ does not recommend | ||||||
| Bed rest | 1 | 0.3 | 0 | 0.0 | 1 | 0.5 |
| Ice or heat* | 151 | 46.2 | 43 | 33.6 | 108 | 54.3 |
| Interferential current | 60 | 18.3 | 27 | 21.1 | 33 | 16.6 |
| Laser | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Magnetic therapy | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Mechanical traction | 12 | 3.7 | 5 | 3.9 | 7 | 3.5 |
| Refer to physician specialist | 15 | 04.6 | 3 | 2.3 | 12 | 6.0 |
| Refer to psychologist | 1 | 0.3 | 0 | 0.0 | 1 | 0.5 |
| TENSδ | 29 | 08.9 | 9 | 7.0 | 20 | 10.0 |
| Ultrasound* | 33 | 10.1 | 7 | 5.5 | 26 | 13.0 |
| EBP§ does not discussλ | ||||||
| Biofeedback | 5 | 01.8 | 2 | 1.6 | 3 | 1.5 |
| Electrical stimulation | 56 | 17.1 | 18 | 14.1 | 38 | 19.1 |
| Exercise at home* | 254 | 77.7 | 110 | 85.9 | 144 | 72.4 |
| Refer to group exercise | 2 | 0.6 | 1 | 0.8 | 1 | 0.5 |
| Work conditioning | 19 | 05.8 | 2 | 1.6 | 17 | 8.5 |
| Work hardening | 47 | 14.4 | 16 | 12.5 | 31 | 15.6 |
| Work modification | 28 | 8.6 | 6 | 4.7 | 22 | 11.1 |
| Total participants | 327 | 100 | 128 | 100 | 199 | 100 |
§ EBP: evidence-based practice.
†† PTs: physical therapists.
† MSPTs: physical therapists in outpatient musculoskeletal setting.
‡ NMSPTs: physical therapists not working in outpatient musculoskeletal setting.
λ Evidence not discussed in the majority of guidelines for non-specific subacute LBP.
*Significant statistical difference between MSPTs versus NMSPTs.
δ TENS: transcutaneous electrical nerve stimulation.
There was not a statistically significant difference for adherence to EBP guidelines for subacute LBP between MSPTs and NMSPTs (chi2 [1, n = 327] = 1.902, P = 0.168). However, the choice for management of subacute LBP with home exercise program was higher among MSPTs when compared to NMSPTs (chi2 [1, n = 327] = 8.279, P = 0.004). In addition, the management of subacute LBP with passive intervention modalities was lower for MSPTs than NMSPTs: ice/heat (chi2 [1, n = 327] = 13.401, P = 0.001) and ultrasound (chi2 [1, n = 327] = 4.954, P = 0.026).
Discussion
Acute LBP management
The rate of therapists adhering to EBP recommendations for acute LBP was low. This rate was significantly lower for NMSPTs (15%) when compared to MSPTs (36%). This difference was related to the higher rate of utilization of manual therapy among MSPTs and not the utilization of LBP education. Musculoskeletal therapists chose manual therapy more often than NMSPTs to manage acute LBP. Musculoskeletal therapists had taken more continuing education courses in manual therapy than NMSPTs and were probably more comfortable utilizing mobilization and manipulation techniques than NMSPTs.
Li and Bombardier studied how 274 Ontarian PTs manage patients with LBP.20 Their study methodology was similar to the one in the present investigation (clinical vignette with non-specific acute LBP; treatment choice options were the same). Based on the EBP definition in the present investigation, Ontarian PTs followed EBP guidelines more strictly (education 99%, mobilization 44%, and manipulation 5%) than the PTs in the current study (education 70%, mobilization 35%, and manipulation 6%). This difference may be explained by two factors. First, while both Canada and the US strive to promote healthcare coverage based on EBP,37 the Medicare system in the US has struggled to implement healthcare coverage based on EBP.38 In addition, while the Canadian Medicare system covers its entire population, the US Medicare system covers mostly the elderly. The rest of the US population is covered by private insurance that may not utilize EBP to make healthcare policy. This may partially explain why healthcare outcomes in Canada are better and cost less than in the US.39–41 This may also explain why Ontarian PTs followed EBP more strictly than Floridian PTs in the current study. Second, the Ontarian therapists had a larger patient caseload of patients with LBP and might be better informed on how to manage LBP than the PTs in the present study. In all, 95% of the Ontarian PTs saw at least five patients per day and had a 20% caseload of patients with LBP, whereas 88% of the PTs in the current study saw at least five patients per day and had a 10% caseload of patients with LBP.
Strand et al. investigated LBP management in Norway.42 They used graduate students to observe 34 nationally certified manual therapists evaluate 43 patients with acute LBP. According to the EBP definition in the current study, the Norwegian PTs had better adherence to EBP guidelines (education [clinical findings 90%, 50% stay active, 43% avoid pain provoking movements, 43% fear avoidance], 65% mobilization, and 14% manipulation), than the PTs in the present investigation (education 70%, mobilization 35%, and manipulation 6%). The main reason for this difference is that these Norwegian PTs were practitioners specialized in musculoskeletal medicine presumed to be familiar with LBP management recommendations from clinical research and clinical practice guidelines.42
Hendrick et al. studied the treatment choices of 170 New Zealand PTs specialized in manual therapy or sports therapy to manage non-specific acute LBP.43 Similar to the current study, they also used an electronic survey and a clinical vignette to assess treatment preferences. Based on the EBP definition of the present investigation, New Zealanders adhered better to LBP treatment guidelines (mobilization [92.9%], education [posture 92%, ergonomics 82.9%, and return to work 82%], and manipulation [33%]) than the PTs in the current study. The main reason for this discrepancy is that Hendrick et al. studied PTs specialized in sports medicine and manual therapy familiar with management of LBP,43 while the current authors investigated mostly generalist PTs (76%) without post-professional training in musculoskeletal care (Table 1).
High velocity low amplitude manipulation was underutilized in the present study. In the current investigation, 3% of NMSPTs and 14.1% of MSPTs chose HVLA to manage acute non-specific LBP. This rate is low considering that there is strong evidence to recommend HVLA to manage non-specific acute LBP.1,2,9 However, the current findings for MSPTs suggest that the use of HVLA in 2007 rose compared to the 1990s in the US13,15 (0–1.8%) and may be rising compared to the early 2000s in Canada20 and Britain44 (2.8–5%). The observed rise in utilization of HVLA manipulation in the US among MSPTs is consistent with an increase in utilization of HVLA manipulation among PTs internationally. In Norway (2005), 14% of the PTs specialized in manual therapy also utilized manipulation to manage non-specific acute LBP.42 In New Zealand (2013), this rate was even higher for PTs specialized in manual therapy or sports medicine; 33% of New Zealanders employed manipulation to manage acute non-specific LBP.43 This utilization rate of manipulation in the present study, even though low, might indicate that APTA’s17 efforts to promote HVLA manipulation to manage non-specific LBP might have made an impact in Florida in 2007.
Management of subacute LBP
Only 37.5% (n = 48) of MSPTs and 30% (n = 60) of NMSPTs adhered to EBP guidelines for subacute LBP. In all, 46% of all PTs prioritized the use of ice/heat and 18% the use of interferential therapy to manage patients with subacute LBP, despite recommendations from EBP guidelines to avoid passive modalities to manage patients with subacute LBP.1,2,9,27 This finding is a bit concerning because management of subacute LBP with passive intervention could contribute to patients developing chronic LBP.27 Chronic LBP is responsible for high utilization of healthcare intervention and increased costs (surgery, medication, workman compensation, and disability).4
Ontarian PTs20 observed EBP guidelines recommendations more often for subacute LBP (exercise in the clinic [93.4%] and education on back care [81.7%]) than the PTs in the current study (exercise in the clinic 74.9% and education on back care 57.2%). As explained above, the study design of this Canadian study was similar to the one in the current study. Overall, the PTs in the current investigation were more likely to select passive methods of intervention (ice/heat 46%) than the Canadian PTs (ice/heat 30%) to manage subacute LBP. The fact that Canadian therapists followed EBP more strictly was discussed above for management of acute LBP.
Gracey, McDonough, and Baxter studied how 157 PTs managed LBP in Northern Ireland.44 They collected data from 1062 patient records; 70% of these patients had subacute or chronic LBP. Based on the EBP definition for subacute LBP in the current study, there was not an adherence difference between these Irish PTs and the PTs in the present study. The Irish PTs used education (89%) more often, exercises (McKenzie 70%, general 26%) similarly, and interferential current (30%) more often than the current PTs (education 57.2%, exercise 74.9%, and interferential 18.3%). Even though they followed EBP better in terms of patient education than the PTs in the current study, they disregarded EBP advice about not using passive modalities to manage patients with subacute or chronic LBP. The difference in treatment choices between the Irish PTs and the PTs in the current study may be related to differences in study methodology or may be cultural and/or educational.
The current study would suggest that the APTA should also make an effort to encourage PTs not to overutilize passive interventional methods to manage LBP. The use of ice/heat (46%) and interferential therapy (18%) among the PTs in the current study was high for the management of subacute LBP. Devoting time to treat patients with subacute LBP with passive procedures may reduce active patient participation in their own rehabilitation process. It may also hinder positive patient outcome and contribute to chronic LBP.18,22,27,43
Limitations and delimitations of the study
The present study had a low response rate (14.5%). This was similar to Hendrick et al.’s study43 (17%) who also used an electronic survey. Electronic survey response rate is often lower than traditional postal response rate because of server rejection, automated out of office replies, and organizational, as well as personal, spam filters.45,46 In the current investigation, 500 surveys were server rejected (Fig. 1). Based on studies that investigate electronic survey response rate, at least 500 more participants were lost because of organizational and personal email spam filter.45 There is also a possibility that this low response introduced non-response and self-selection bias. The participants of the present surveys were probably working in the field of musculoskeletal medicine and were more knowledgeable in LBP management than non-respondents. In all, 40 potential participants emailed the present authors to explain that they would not participate in the study because they did not work in musculoskeletal medicine or did not treat patients with LBP (Fig. 1). This was a limitation of the study.
The data in the present study may be a bit dated (2008), and the definition of EBP guideline adherence was delimited to multidisciplinary guidelines published between 2002 and 2007. However, it is important to note that the definitions in the present study are still consistent with multidisciplinary EBP guideline recommendations published between 2008 and 2011.47 The recommendations for LBP management in the majority of these multidisciplinary guidelines focused on patient triage for surgical consult, imaging tests, medication, exercise, manual therapy, and/or behavioral therapy.47,48 The multidisciplinary guidelines recommended that primary care professionals refer patients with non-specific LBP to PTs for exercise and education; however, those guidelines did not detail to PTs what type of education and exercises to use in order to manage patients with non-specific LBP. This was also a limitation of the present investigation. Nonetheless, the definitions in the present research for adherence to acute and subacute LBP management were similar to the guidelines of the Orthopedic Section of the APTA published in 2012.9 The APTA guidelines recommended education that encourages the patients with acute and subacute LBP to pursue or maintain an active lifestyle; the current authors recommended education for both acute and subacute LBP, but they were not specific about the educational advice for LBP. The APTA Orthopedic Section recommended the use of HVLA manipulation and accepted the use of mobilization for acute LBP;9 the present investigators recommended the use of both HVLA manipulation and mobilization for acute LBP. The APTA recommended the use of specific exercises (coordination, strengthening, and endurance) for subacute LBP;9 the current researchers recommended general exercises in the clinic for subacute LBP.
Recommendation for future studies
Upcoming investigations should study therapist choices for management of LBP in the 2010s. In particular, future studies should investigate the therapeutic choices for patients with specific clinical scenarios (patients with lumbar radiculopathy, instability, hypomobility, or needing medical referral) based on recent monodisciplinary EBP guideline recommendations for PTs. The results of these future studies would help physical therapy associations and educational institutions plan the training of therapists managing LBP patients in the US and abroad. In addition, forthcoming studies could also attempt to implement the use of the APTA guidelines to manage LBP, which would probably benefit patient outcome and treatment cost in the US.43,49,50
Conclusion
The adherence to EBP guideline recommendations for LBP was low for all participating PTs in Florida. This was worse for NMSPTs, as compared to MSPTs. High velocity low amplitude manipulation was underutilized for the management of acute LBP, and passive interventional modalities were overutilized in the management of subacute LBP.
Disclosure
The authors have no conflict of interest to report.
Disclaimer statements
Contributors Carlos Ladeira: study design, literature review, methods, data collection, manuscript write up. Samuel Cheng: study design, methods, manuscript write up. Cheryl Hill: methods, manuscript write up.
Funding None.
Conflicts of interest None.
Ethics approval The ethics committee of the Nova Southeastern University approved the research project.
Appendix 1
Clinical scenario I
A 28-year-old woman has suffered from low back pain after lifting a 20-lb box at work a week ago. She has been unable to do her job managing a cafeteria since then. While anxious to return to work, she feels immobilized by the pain. In terms of activities, she can sit about 10 minutes and walk one block before she has to stop due to pain. She is able to sleep through the night; however, her back is stiff in the morning and the stiffness lasts about 10 minutes. There is no history of trauma. The pain is limited to the low back area, without radiation. She does not have red flags indicating cancer, infection, or any other visceral disease that could refer pain to the low back. She comes to you with a referral from a physician.
Clinical scenario II
A 30-year-old man has suffered from low back pain after lifting a 30-lb box at work 6 weeks ago. He was unloading a truck when he got hurt. He has been unable to do his job as a supermarket manager since then. He is motivated to return to work, but he feels immobilized by the pain. In terms of activities, he can stand about 10 minutes and walk about one block before he has to stop due to pain. He is able to sleep through the night; however, his back is stiff in the morning and the stiffness lasts about 10 minutes. There is no history of trauma. The pain is limited to the low back area, without radiation. He does not have red flags indicating cancer, infection, or any other visceral disease that could refer pain to the low back. During his physical exam, he continues to have pain with movement. He still has some limitation in the anterior flexion of the spine with a normal neurological examination. He comes to you with a referral from a physician.
Appendix 2
Preferred treatment procedures available for selection for each clinical scenario*
| Acupuncture | Exercise at clinic | Laser | Refer to specialist physician | TENSδ |
| Back school | Exercise at home | Lumbar corset | Refer for psychological screening | Ultrasound |
| Bed rest | Ice or heat | Magnetic therapy | Referral to group exercise programs | Work hardening |
| Biofeedback | Patient education on back care | McKenzie exercise | Spine manipulation (thrust) | Work conditioning |
| Electrical muscle stimulation | Interferential current | Mechanical traction | Spine mobilization (non-thrust) | Work modification |
*There were 25 low back pain management options in total. Each physical therapist (PT) selected a minimum of two and a maximum of five choices.
δTENS: transcutaneous electrical nerve stimulation.
References
- 1.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 2.van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006;15((Suppl 2)):S169–91. doi: 10.1007/s00586-006-1071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pai S, Sundaram LJ. Low back pain: an economic assessment in the United States. Orthop Clin North Am. 2004;35:1–5. doi: 10.1016/S0030-5898(03)00101-9. [DOI] [PubMed] [Google Scholar]
- 4.Mehra M, Hill K, Nicholl D, Schadrack J. The burden of chronic low back pain with and without a neuropathic component: a healthcare resource use and cost analysis. J Med Econ. 2012;15:245–52. doi: 10.3111/13696998.2011.642090. [DOI] [PubMed] [Google Scholar]
- 5.Ritter B. Considering evidence based practice. Nurse Pract. 2001;26:63–5. doi: 10.1097/00006205-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Sackett DL. Evidence based medicine: what it is and what it isn’t. Br Med J. 1996;312:71–2. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Philadelphia Panel. Philadelphia panel evidence-based clinical practice guidelines on selected rehabilitation interventions for low back pain. Phys Ther. 2001;81:1641–74. [PubMed] [Google Scholar]
- 8.Bouwmeester W, van Enst A, van Tulder M. Quality of low back pain guidelines improved. Spine (Phila Pa 1976). 2009;34:2562–7. doi: 10.1097/BRS.0b013e3181b4d50d. [DOI] [PubMed] [Google Scholar]
- 9.Delitto A, George SZ, Van Dillen LR, Whitman JM, Sowa G, Shekelle P, et al. Low back pain. J Orthop Sports Phys Ther. 2012;42:A1–57. doi: 10.2519/jospt.2012.42.4.A1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Appraisal of Guidelines for Research & Evaluation (AGREE) Instrument II. The agree collaboration. Appraisal of guidelines for research & evaluation (agree) instrument. 2009 [cited 2013 July 25]. Available from: http://www.agreetrust.org. [Google Scholar]
- 11.Arnau JM, Vallano A, Lopez A, Pellise F, Delgado MJ, Prat N. A critical review of guidelines for low back pain treatment. Eur Spine J. 2006;15:543–53. doi: 10.1007/s00586-005-1027-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.APTA. Vision sentence and vision statement for physical therapy. 2020 [cited 2013 Nov 8]. Available from http://www.apta.org/vision2020. [Google Scholar]
- 13.Jette AM, Delitto A. Physical therapy treatment choices for musculoskeletal impairments. Phys Ther. 1997;77:145–54. doi: 10.1093/ptj/77.2.145. [DOI] [PubMed] [Google Scholar]
- 14.Jette AM, Smith K, Haley SM, Davis KD. Physical therapy episodes of care for patients with low back pain. Phys Ther. 1994;74:101–10. doi: 10.1093/ptj/74.2.101. [DOI] [PubMed] [Google Scholar]
- 15.Battie MC, Cherkin DC, Dunn R, Ciol MA, Wheeler KJ. Managing low back pain: attitudes and treatment preferences of physical therapists. Phys Ther. 1994;74:219–26. doi: 10.1093/ptj/74.3.219. [DOI] [PubMed] [Google Scholar]
- 16.Mielenz TJ, Carey TS, Dyrek DA, Harris BA, Garrett JM, Darter JD. Physical therapy utilization by patients with acute low back pain. Phys Ther. 1997;77:1040–51. doi: 10.1093/ptj/77.10.1040. [DOI] [PubMed] [Google Scholar]
- 17.Manipulation Education Committee Task Force. Manipulation education manual: for physical therapist professional degree programs. American Physical Therapy Association. 2004 [cited 2013 Nov 8]. Available from http://www.apta.org/uploadedFiles/APTAorg/Educators/Curriculum_Resources/APTA/Manipulation/ManipulationEducationManual.pdf. [Google Scholar]
- 18.Fritz JM, Cleland JA, Brennan GP. Does adherence to the guideline recommendation for active treatments improve the quality of care for patients with acute low back pain delivered by physical therapists? Med Care. 2007;45:973–80. doi: 10.1097/MLR.0b013e318070c6cd. [DOI] [PubMed] [Google Scholar]
- 19.Rutten GM, Degen S, Hendriks EJ, Braspenning JC, Harting J, Oostendorp RA. Adherence to clinical practice guidelines for low back pain in physical therapy: do patients benefit? Phys Ther. 2010;90:1111–22. doi: 10.2522/ptj.20090173. [DOI] [PubMed] [Google Scholar]
- 20.Li LC, Bombardier C. Physical therapy management of low back pain: an exploratory survey of therapist approaches. Phys Ther. 2001;81:1018–28. [PubMed] [Google Scholar]
- 21.Jette DU, Ardleigh K, Chandler K, McShea L. Decision-making ability of physical therapists: physical therapy intervention or medical referral. Phys Ther. 2006;86:1619–29. doi: 10.2522/ptj.20050393. [DOI] [PubMed] [Google Scholar]
- 22.Rutten GM, Harting J, Rutten ST, Bekkering GE, Kremers SP. Measuring physiotherapists’ guideline adherence by means of clinical vignettes: a validation study. J Eval Clin Pract. 2006;12:491–500. doi: 10.1111/j.1365-2753.2006.00699.x. [DOI] [PubMed] [Google Scholar]
- 23.Bishop A, Foster NE, Thomas E, Hay EM. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health care practitioners? A survey of UK general practitioners and physiotherapists. Pain. 2008;135:187–95. doi: 10.1016/j.pain.2007.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rossignol M, Poitras S, Dionne C, Tousignant M, Truchon M, Arsenault B, et al. An interdisciplinary guideline development process: the clinic on low-back pain in interdisciplinary practice (clip) low-back pain guidelines. Implement Sci. 2007;2:36. doi: 10.1186/1748-5908-2-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hagmann KT, Talmage J, Belcourt R, Galper J, Genovese E, Goertz M., Low back disorders. In Glass LS (editor). Occupational medicine practice guidelines: evaluation and management of common health problems and functional recovery in workers. Elk Grove Village, IL: American College of Occupational and Environmental Medicine (ACOEM); 2007 [updated 2011, p. 333–796, cited 2014 Jan 3]. Available from http://www.guideline.gov/content.aspx?id = 38438. [Google Scholar]
- 26.Negrini S, Giovannoni S, Minozzi S, Barneschi G, Bonaiuti D, Bussotti A, et al. Diagnostic therapeutic flow-charts for low back pain patients: the Italian clinical guidelines. Eura Medicophys. 2006;42:151–70. [PubMed] [Google Scholar]
- 27.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15((Suppl 2)):S192–300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Institute for Clinical Systems Improvement (ICSI) Adult low back pain. Clinical practice guidelines. Bloomington, MN; 2005 [updated 2012; cited 2013 Nov 8]. Available from: https://www.icsi.org/_asset/bjvqrj/LBP.pdf. [Google Scholar]
- 29.Heijmans WFGJ, Hendriks HJM, van der Esch M, Pool-Goudzwaard A, Scholten-Peeters GGM, van Tulder MW, et al. Kngf-guideline manual therapy on low back pain. 2003 [updated 2006; cited 2013 Nov 8]. Available from http: //www.physio-europe.org/download.php?document = 110&downloadarea = 20. [Google Scholar]
- 30.Bekkering GE, Hendriks HJM, Koes BW, Oostendorp RAB, Ostelo RWJG, Thomassen JM, et al. Dutch physiotherapy guidelines for low back pain. Physiotherapy. 2003;89:82–96. [Google Scholar]
- 31.The Norwegian Back Pain Network -The communication unit. Acute low back pain. Interdisciplinary clinical guidelines Oslo; 2002 [cited 2013 Nov 8]. Available from: http://www.sohs.com.sg/pdf/Norway_Acute_Low_Back.pdf. [Google Scholar]
- 32.New Zealand Guidelines Group. New Zealand low back pain guide. 2004 [cited 2013 Nov 8]. Available from http://www.acc.co.nz/PRD_EXT_CSMP/groups/external_ip/documents/internet/wcm002131.pdf. [Google Scholar]
- 33.Australian Acute Musculoskeletal Pain Guidelines Group. Evidence based management of acute pain. Acute low back pain. 2004 [cited 2013 Nov 8]. Available from: http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/cp94.pdf. [Google Scholar]
- 34.Flesch R. A new readability yardstick. J Appl Psychol. 1948;32:221–33. doi: 10.1037/h0057532. [DOI] [PubMed] [Google Scholar]
- 35.Hall JC. The readability of original articles in surgical journals. ANZ J Surg. 2006;76:68–70. doi: 10.1111/j.1445-2197.2006.03651.x. [DOI] [PubMed] [Google Scholar]
- 36.Williamson JM, Martin AG. Assessing the readability statistics of national consent forms in the UK. Int J Clin Pract. 2010;64:322–9. doi: 10.1111/j.1742-1241.2009.02245.x. [DOI] [PubMed] [Google Scholar]
- 37.Garber AM. Evidence-based coverage policy. Health Affair. 2001;20:62–82. doi: 10.1377/hlthaff.20.5.62. [DOI] [PubMed] [Google Scholar]
- 38.Mendelson D, Carino TV. Evidence-based medicine in the United States – de rigueur or dream deferred? Health Affair. 2005;24:133–6. doi: 10.1377/hlthaff.24.1.133. [DOI] [PubMed] [Google Scholar]
- 39.Lasser KE, Himmelstein DU, Woolhandler S. Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. Am J Public Health. 2006;96:1300–7. doi: 10.2105/AJPH.2004.059402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Woolhandler S, Campbell T, Himmelstein DU. Costs of health care administration in the United States and Canada. N Engl J Med. 2003;349:768–75. doi: 10.1056/NEJMsa022033. [DOI] [PubMed] [Google Scholar]
- 41.LaPierre TA. Comparing the Canadian and US systems of health care in an era of health care reform. J Health Care Finance. 2012;38:1–18. [PubMed] [Google Scholar]
- 42.Strand LI, Kvale A, Raheim M, Ljunggren AE. Do Norwegian manual therapists provide management for patients with acute low back pain in accordance with clinical guidelines? Man Ther. 2005;10:38–43. doi: 10.1016/j.math.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 43.Hendrick P, Mani R, Bishop A, Milosavljevic S, Schneiders AG. Therapist knowledge, adherence and use of low back pain guidelines to inform clinical decisions – a national survey of manipulative and sports physiotherapists in New Zealand. Man Ther. 2013;18:136–42. doi: 10.1016/j.math.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 44.Gracey JH, McDonough SM, Baxter GD. Physiotherapy management of low back pain: a survey of current practice in northern Ireland. Spine (Phila Pa 1976). 2002;27:406–11. doi: 10.1097/00007632-200202150-00017. [DOI] [PubMed] [Google Scholar]
- 45.Dobrow MJ, Orchard MC, Golden B, Holowaty E, Paszat L, Brown AD, et al. Response audit of an internet survey of health care providers and administrators: implications for determination of response rates. J Med Internet Res. 2008;10:e30. doi: 10.2196/jmir.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dykema J, Stevenson J, Klein L, Kim Y, Day B. Effects of e-mailed versus mailed invitations and incentives on response rates, data quality, and costs in a web survey of university faculty. Soc Sci Comput Rev. 2013;31:359–70. [Google Scholar]
- 47.Ladeira CE. Evidence based practice guidelines for management of low back pain: physical therapy implications. Rev Bras Fisioter. 2011;15:190–9. doi: 10.1590/s1413-35552011000300004. [DOI] [PubMed] [Google Scholar]
- 48.Breen AC, van Tulder MW, Koes BW, Jensen I, Reardon R, Bronfort G. Mono-disciplinary or multidisciplinary back pain guidelines? How can we achieve a common message in primary care? Eur Spine J. 2006;15:641–7. doi: 10.1007/s00586-005-0883-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hoeijenbos M, Bekkering T, Lamers L, Hendriks E, van Tulder M, Koopmanschap M. Cost-effectiveness of an active implementation strategy for the Dutch physiotherapy guideline for low back pain. Health Policy. 2005;75:85–98. doi: 10.1016/j.healthpol.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 50.Dahan R, Borkan J, Brown JB, Reis S, Hermoni D, Harris S. The challenge of using the low back pain guidelines: a qualitative research. J Eval Clin Pract. 2007;13:616–20. doi: 10.1111/j.1365-2753.2007.00855.x. [DOI] [PubMed] [Google Scholar]