Abstract
Individuals diagnosed with lung and head and neck (HN) cancers and their spouses are at increased risk for distress. This study assessed whether the way couples communicate about cancer and their perceptions of relationship intimacy influenced both partners' adjustment. One-hundred thirty-nine patients and their spouses [For purposes of clarity, we refer to the patients' intimate partner as the spouse, regardless of actual marital status and we reserve the term partner to refer to the other person in the couple (i.e., the patient's partner is the spouse and the spouse's partner is the patient)] completed measures of spousal communication, intimacy, and distress at three time points over 6 months. Using multilevel modeling, an over-time actor-partner interdependence model was specified that examined whether intimacy mediated associations between one's own and one's partner's reports of communication at baseline and later distress. Patients and spouses who reported greater baseline distress reported more negative baseline communication as well as lower levels of intimacy and greater distress over time. Mediation analyses showed patients' and spouses' reports of positive spousal communication were associated with less subsequent distress largely through their effects on intimacy. Clinicians working with head and neck or lung cancer patients should assess communication and intimacy because both impact couples' distress.
Keywords: Couple communication, Interpersonal processes, Relationship intimacy, Psychological adaptation, Cancer
Introduction
The diagnosis of lung or head and neck cancer can be very stressful for both patients and their spouses. Rates of distress among lung cancer (LC) patients have been reported to be as high as 43% for clinical depression (Hopwood & Stephens, 2000; Uchitomi et al., 2000), 17% for clinical anxiety (Montazeri et al., 2005; Rolke et al., 2009), and 60% for overall emotional distress (Graves et al., 2007; Steinberg et al., 2009). Between 15% (Sehlen et al., 2003) and 42% of patients diagnosed with head and neck cancers (HNC; Bergquist et al., 2007) report significant depressive symptoms, and similar elevations in anxiety have been reported (Jones et al., 1992; Kugaya et al., 2000). Reduced quality of life (Baile et al., 1992; Schliephake & Jamil, 2002) has also been reported for HNC patients. Taken together, the rates of distress reported among LC and HNC patients are higher than those reported for patients with many other types of cancer (Zabora et al., 2001). Spouses are also at risk. Over one-third of spouses of LC patients exhibit significant distress (Carmack Taylor et al., 2008; Kim et al., 2005) and lower levels of quality of life than the general population (Sarna et al., 2006). Few studies have examined distress among the spouses of HNC patients; however, the prevalence of clinically significant levels of anxiety among spouses may be as high as 40% (Vickery et al., 2003). Given the high rates of psychological distress reported among patients with LC and HNC and their spouses, it may be useful to identify factors in the marital environment that may either contribute to or alleviate this distress.
The marital relationship plays an important role in the psychological adaptation of both partners to cancer such that a higher quality marriage is associated with lower distress for both patients and partners (Banthia et al., 2003; Fang et al., 2001; Jenewien et al., 2008; Nijboer et al., 1999). Among couples not dealing with cancer, communication is an important way that couples maintain the quality of their relationship (Ayres, 1983; Canary & Stafford, 1992). Indeed, studies have suggested that communication problems are associated with declines in marital quality and ultimately with divorce (Cleek & Pearson, 1985). Relationship communication may play a particularly important role in how well couples manage stressful life events such as the diagnosis of a life threatening illness like cancer. Couples typically adopt a number of communication strategies to manage their own and their partner's cancer-related concerns (Manne et al., 2005). Communication strategies have been characterized as either positive (e.g., their use by one partner is associated with less distress for the other partner and/or the relationship) or negative (e.g., their use by one partner is associated with more distress for the other partner and/or the relationship). Positive communication includes the disclosure of feelings and concerns to one's partner (Pistrang & Barker, 1998; Porter et al., 2005) as well as a response from one's partner that conveys empathy, understanding, and helpfulness (Manne et al., 2005; Pistrang & Barker, 1998). Negative communication involves criticizing one's partner, avoiding discussion of cancer-related concerns, and/or pressuring one's partner to discuss concerns (Manne et al., 1997, 2005). Whereas positive communication strategies have been associated with lower distress among cancer patients and their spouses, negative communication strategies have been associated with greater distress for both partners (Kayser & Sormanti, 2002; Manne et al., 2005, 2006; Porter et al., 2005).
Few studies have examined the impact of LC and HNC on couples' relationships, and the results of existing studies have been mixed. For example, qualitative research has suggested a detrimental impact of LC on the marital relationship (Lindau et al., 2010), whereas quantitative studies have shown that only a subset of patients (7.7–16.4%) and spouses (14–16.4%) experience distressed relationships (Badr & Taylor, 2008; Carmack Taylor et al., 2008). Likewise, very little is known about the marital impact of HNC. Jenewein et al. (2008) reported that couples' marital satisfaction scores were no different than the normative mean; however, there is currently no other data on this topic.
Despite these mixed findings, the literature is clear with regard to the fact that couples coping with both LC and HNC experience serious difficulty with regard to communicating openly and often avoid discussing cancer-related concerns (Haman, 2008; Zhang & Siminoff, 2003). Indeed, LC and HNC may pose unique barriers to open spousal communication. Patients may blame themselves for causing their cancer, feel ashamed, and/or perceive that their spouses blame them for unhealthy behaviors (i.e., smoking, drinking alcohol) that may have caused their cancer (Chapple et al., 2004; Lobchuk et al., 2008). Likewise, practical issues such as problems with speaking, conveying emotions, and eating/drinking due to extensive facial disfigurement can interfere with communication as well as the quality of couples' relationships (Vickery et al., 2003).
One way that spousal communication may impact distress is by altering individuals' perceptions of their relationship. The relationship intimacy model (RIM) of couples' psychosocial adaptation to cancer (Manne & Badr, 2009) proposes that communication affects close relationships by affecting intimacy. According to the RIM, positive communication influences both partners' psychological adaptation by enhancing intimacy, and negative communication influences both partners' psychological adaptation by reducing relationship intimacy. Although the RIM is specific to cancer, it is based on the interpersonal process model of intimacy (Reis & Patrick, 1996; Reis & Shaver, 1988) which proposes that intimacy develops from the ongoing disclosures and responses to disclosures between partners.
Several cross-sectional studies provide support for the RIM. Manne et al. (2004) evaluated associations between self-disclosure, perceived partner disclosure, and relationship intimacy among couples dealing with early stage breast cancer. They found that greater self-disclosure and perceived partner disclosure was associated with greater intimacy for both patients and spouses. Porter et al. (2005) reported similar findings in a sample of gastrointestinal cancer patients and spouses. Finally, our analysis of the baseline data from the current sample of LC and HNC couples showed that positive communication strategies were associated with higher levels of relationship intimacy and that greater intimacy was associated with lower distress, particularly for spouses (Manne & Badr, 2009). Longitudinal studies would elucidate the mediational role of intimacy more clearly for both partners. In addition, although couples simultaneously adopt a number of communication strategies to cope with cancer, previous studies have evaluated the effects of each communication strategy separately. Assessing the effects of different positive and negative communication strategies together might provide a more accurate reflection of the role of relationship processes in couples' psychosocial adaptation to cancer.
Study aims
The study had two aims. The first was to prospectively assess the association between relationship communication and psychological distress. We hypothesized that more positive communication at baseline would be associated with lower distress for both patients and spouses over time, and that more negative communication at baseline would be associated with greater distress for both patients and spouses over time. The second aim was to evaluate whether relationship intimacy mediated the association between communication and distress. We hypothesized that higher levels of positive communication would be associated with greater intimacy and less distress over time for both patients and their spouses and that higher levels of negative communication would be associated with less intimacy and greater distress over time for both patients and their partners. While we proposed that communication and intimacy would play a significant role for both partners, we evaluated whether there were differences in these associations by including social role (i.e., whether the person being evaluated is the patient or the spouse) in our model.
Methods
Procedures
HNC and LC patients undergoing active treatment at a comprehensive cancer center in northeast Pennsylvania were eligible if they were: age 18 years or older; married or living with a significant other of either gender; had an Eastern Cooperative Oncology Group (ECOG) score of 0 or 1 (Oken et al., 1982), and were English speaking. Participants were identified and approached by the research assistant either after an outpatient visit or by telephone. If a couple was interested, they were provided the written informed consent and the baseline study questionnaire to complete and return by mail. Patients and spouses were instructed to complete the surveys on their own. Follow-up questionnaires were mailed out 3 and 6 months later.
Participants
Four-hundred twenty-five couples were approached, and 139 consented (33.1% acceptance). The most common reasons for refusal were that the patient felt the study would take “too much time” (10.4%) or felt too ill (10.4%). Comparisons were made between patients who agreed and declined to participate in the study based on available data (i.e., age, ethnicity, cancer stage, cancer type, and time since diagnosis). No significant differences were found.
One-hundred eight patients (77.6%) and 90 spouses (65%) completed the 3 month follow-up and 91 patients (65.5%) and 77 spouses (54%) completed the 6 month follow-up. The most frequently cited reasons for drop-outs were: the patient died, felt too ill to continue, or felt the survey was too upsetting. Comparisons were made between those who completed and dropped out of the study at each time point on demographic, medical, and psychological variables (e.g., baseline levels of communication and distress). Patients who dropped out reported a significantly lower income (M = $44,750, SD = $22,716) than those who completed the study (t(109) = 4.9, p < .001).
Measures
Positive communication
Self-disclosure and perceived partner disclosure
Using two 3-item measures adapted from Laurenceau et al. (1998) that we have used in our previous research (Manne et al., 2004; Manne & Badr, 2009), participants rated how much they (i.e., self-disclosure) and their partners (i.e., perceived partner disclosure) disclosed thoughts and concerns about cancer in the past week on a scale from 1 to 7. For both scales, answers were summed and higher scores indicated greater disclosure. For self-disclosure, Cronbach's alphas across assessments for patients ranged from .91 to .97 and from .89 to .92 for spouses. Across assessments, Cronbach's alphas for perceived partner disclosure for patients ranged from .93 to .96 and .91 to .97 for spouses.
Sharing concerns
A 10-item scale adapted from Pistrang and Barker (1995) was used. Participants rated the degree to which they talked to their partners about cancer-related concerns on a 5-point Likert scale (0 = did not talk at all about what I felt, 5 = talked about all that I felt). Answers were summed, and higher scores indicated greater sharing. Across assessments, Cronbach's alphas for patients ranged from .88 to .92 and from .85 to .87 for spouses.
Negative communication
Mutual avoidance
An adapted version of the 3-item mutual avoidance subscale of the Communication Patterns Questionnaire (CPQ) (Christensen, 1988; A. Christensen and M. Sullaway (1984) Communication Patterns Questionnaire (Unpublished manuscript)) was used. Items were rated on a 9-point Likert scale (1 = unlikely to 9 = likely) (Manne et al., 2006). Answers were summed and higher scores indicated greater avoidance. Across assessments, Cronbach's alphas for patients ranged from .61 to .72 and from .61 to .71 for spouses. While relatively low, these reliability coefficients are similar to those reported for mutual avoidance in other studies of couples coping with either prostate cancer (Badr and Taylor 2009; Manne et al., 2010) or early stage breast cancer (Manne et al., 2006).
Demand-withdraw communication (DW)
An adapted version of the Demand-Withdraw subscale of the CPQ (Christensen, 1988; A. Christensen and M. Sullaway (1984) Communication Patterns Questionnaire (Unpublished manuscript)) was used. Items assessed the frequency of one person pressuring the other to talk about a cancer-related issue and the other partner withdrawing from or avoiding the discussion (Manne et al., 2006). Items were rated on a 9-point Likert scale (1 = unlikely to 9 = likely). Three items assessed patient demand-spouse withdraw, and three items assessed spouse demand-patient withdraw. Answers were summed and higher scores indicated greater demand-withdraw. Across assessments, Cronbach's alphas ranged from .59 to .82 for patients and from .50 to .64 for spouses. These reliability coefficients are slightly lower than those reported in previous studies using this instrument (Badr and Taylor 2009; Manne et al., 2006, 2010).
Spouse unsupportive behavior
A 13-item scale adapted from the Cancer Support Inventory (Manne et al., 1999) was used. Items assessed critical responses such as, “Seemed impatient with you,” and avoidant responses such as, “Changed the subject when you tried to discuss your illness,” and were rated on a 4-point Likert-type scale (1 = never, 4 = often). Patients rated their spouse's behavior and spouses rated their own behavior. Answers were summed and higher scores indicated greater unsupportive behavior. Across assessments, Cronbach's alphas ranged from .83 to .88 for patients and from .74 to .88 for spouses.
Relationship intimacy
Cancer-specific relationship intimacy
This two item measure was adapted from Laurenceau et al., (1998) and has been used in our previous research (Manne et al., 2004). Participants rated the degree to which they felt close and emotionally intimate with their partner when talking about cancer on a scale from 1 to 7 (1 = not at all, 7 = very much). Answers were summed and higher scores indicated greater intimacy. Across assessments, Cronbach's alphas ranged from .93 to .96 for patients and from .88 to .94 for spouses.
Global relationship intimacy
The 6-item Personal Assessment of Intimacy in Relationships- Intimacy subscale (PAIR) (Schaefer & Olson, 1981) was used. Participants rated agreement on a 5-point Likert-type scale (1 = strongly disagree, 5 = strongly agree). Answers were summed (range = 5–30) with higher scores indicating greater intimacy. This scale has been used in a number of studies of relationship intimacy among healthy married couples (Greeff & Malherbe, 2001; Laurenceau et al., 2005; Talmadge & Dabbs, 1990). The scale has demonstrated good internal consistency in previous work focusing on couples coping with early stage breast cancer (Cronbach's alpha was .90 for patients and .88 for partners) (Manne & Badr, 2008) and couples coping with prostate cancer (Cronbach's alpha was .88 for patients and .83 for partners) (Manne et al., 2010). In the current study, across assessments, Cronbach's alphas ranged from .85 to .88 for patients and from .87 to .90 for spouses.
Global relationship affection
The 4-item affection subscale of the Dyadic Adjustment Scale (Spanier, 1976) was used. Two items assessed level of agreement about demonstration of affection and sex on a five point scale (1 = always disagree, 5 = always agree) and two items assessed whether the couple disagreed about demonstration of love and not showing love (yes, score = 1, and no = 1). Answers were summed, higher scores indicated greater affection. Across assessments, Cronbach's alphas ranged from .85 to .88 for patients and from .87 to .90 for spouses.
Cancer-related distress
Psychological distress
Two measures were used to assess psychological distress. The short, 18-item version of the Brief Symptom Inventory (BSI-18) was used to assess depression and anxiety symptoms. Items are ranked on a 5-point Likert-type scale (0 = not at all to 4 = extremely) The BSI-18 has been used extensively in cancer populations and yields a global rating of psychological distress called the Global Severity Index (GSI) and a normalized T-score that can be used in analyses. The cutoff for clinically-significant levels of distress is a T-score of >63. Across assessments, Cronbach's alphas ranged from .86 to .88 for patients and from .78 to .92 for spouses.
The Psychological Distress scale of the Mental Health Inventory (Veit & Ware, 1983) consksts of 24 items that assess depressive and anxiety symptoms. Items are ranked on a 6-point Likert-type scale with anchors relevant to each item. Participants rated their feelings over the past month, with higher scores indicating greater distress. Across assessments, Cronbach's alphas ranged from .86 to .93 for patients and from .89 to .94 for spouses.
Psychological well-being
The psychological well-being scale of the Mental Health Inventory (Veit & Ware, 1983) consists of 14 items assessing satisfaction with life, hopefulness about the future, and feelings of relaxation and calmness. Items are ranked on a 6-point Likert-type scale with anchors relevant to each item. Participants rated their feelings over the past month, with higher scores indicating greater well-being. Across assessments, Cronbach's alphas for patients and spouses ranged from .93 to .94.
Medical and demographic factors
Medical and demographic factors
Time since diagnosis, stage, type of treatment received, and cancer type were abstracted from patients' medical records. Demographic information (age, race, length of relationship, income) was collected from all participants.
Physical impairment
The 26-item functional status subscale of the Cancer Rehabilitation Evaluation System (CARES) (Schag et al., 1991) assessed patients' physical disability caused by cancer and its treatment during the past month at baseline. Answers were summed and items were rated on a 4-point Likert-type scale (1 = not at all, 4 = very much). Higher scores indicate greater functional impairment. Cronbach's alpha was .92.
Analytic strategy
Because this study included several measures of each construct, we examined whether the different measures could be combined into overall scores for each factor. Measures of cancer-related distress included psychological distress (BSI and MHI distress) and well-being (MHI well-being). These measures were highly correlated, so we first standardized them with respect to their grandmeans and standard deviations (computed across patients and spouses and across time), and then averaged the three standardized scores into a single index (α = .84) that measured the individual's cancer-related distress at each of the three assessments. Single indices of positive communication (α = .72), negative communication (α = .78), and intimacy (α = .74) were constructed in a similar fashion.
Using multilevel modgling, a lagged actor-partner model (Kenny et al., 2006) was used to predict each person's current distress as a function of his or her own past communication strategies (known as the actor effect) and his or her partner's past communication strategies (known as the partner effect), controlling for the individual's past distress. This approach allows for a correlation between the two partner's distress at any given time point and accounts for non-independence across time. This direct effects model is depicted in Fig. 1. Note that one of the strengths of a taking a multilevel approach is that all of the data at hand are used (i.e., couples with some missing data are not dropped). Moreover, with 3 waves of data, the over-time analyses have two replications for most couples, and as a result, the study has a reasonable level of power.
Fig. 1.
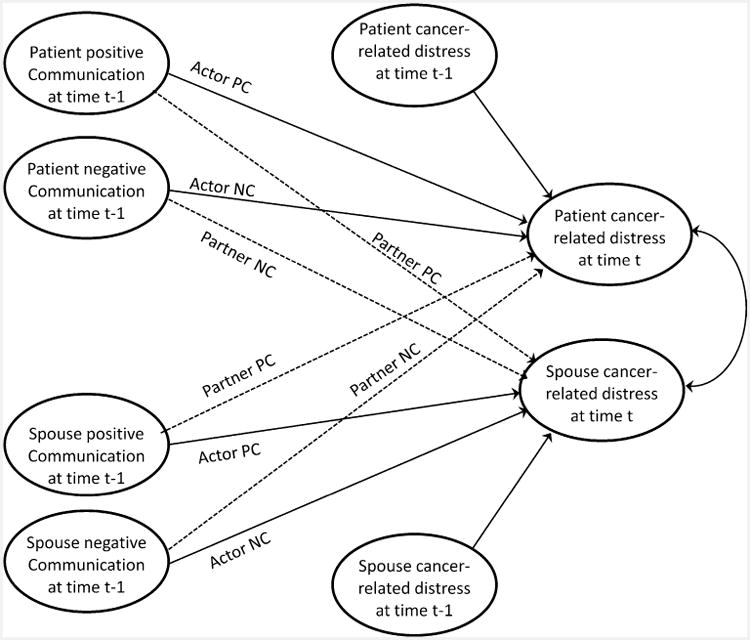
Actor-Partner Model depicting the direct effects of positive and negative communication measured in the previous wave (i.e., time t – 1, where t = 1, 2) on cancer-related distress at the current wave (i.e., time t, where t = 2, 3) controlling for cancer-rated distress at the previous wave (i.e., time = t – 1 where t = 1, 2). Actor PC represents the actor effect of the person's positive communication on his/her own distress, Partner PC represents the partner effect of the person's positive communication on his/her distress (likewise for negative communication or NC)
Given our study aims, we examined whether gender and role (patient vs. spouse) moderated the effects of past positive and negative communication on current distress. These analyses included both actor and partner effects for past positive and negative communication and controlled for the person's own past distress. This model was contrasted with one that only included the person's own previous distress and the four previous communication variables (i.e., role, gender, and interactions between these variables and communication were dropped). A deviance test based on estimation of these two models using maximum likelihood resulted in a χ2 (15) = 19.22, p = .204, suggesting that the simpler model that excluded gender and role did not significantly worsen model fit. A similar approach was used to examine whether gender and role moderated the effects of the person's current intimacy and the partner's current intimacy on current distress (controlling for past distress). This was contrasted with a simplified model that excluded gender and role. The deviance test resulted in a non-significant chi-square, χ2 (10) = 9.21, p = .512, again suggesting that the simpler model was adequate. Based on this, our analyses examined models that averaged over gender and role. In effect this is equivalent to estimating the model in Fig. 1 with equality constraints for parallel parameters across patients and spouses.
A key prediction of the RIM is that the effects of communication on distress are mediated by intimacy. In the context of the actor-partner model, this suggests that individuals who use more positive and less negative communication, and individuals whose partners use more positive and less negative communication should have higher subsequent intimacy. To this end, we estimated the lagged actor-partner model shown in Fig. 2. Each model was first estimated controlling for the patient's baseline physical impairment, time since diagnosis, and age; however, inclusion of these variables did not change the results and the variables were not significant predictors of distress. Thus, results are reported excluding these control variables. Finally, formal tests of mediation were conducted using Sobel tests (Baron & Kenny, 1986) and replicated using bootstrapping (Preacher & Hayes, 2008).
Fig. 2.
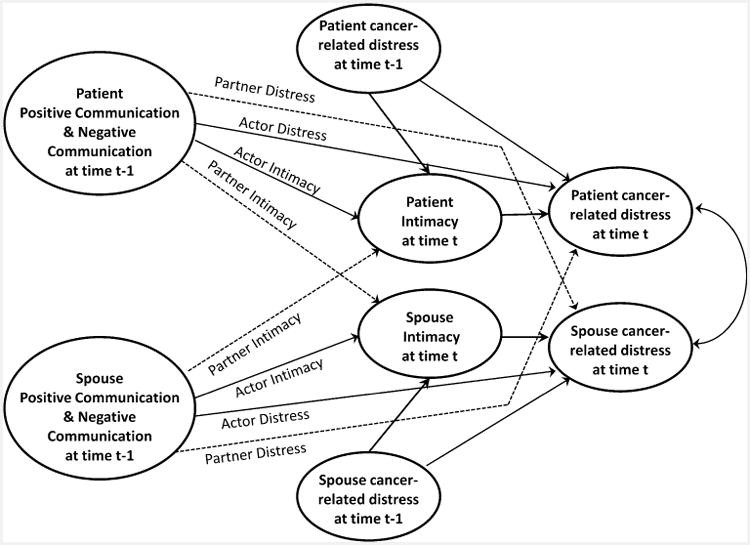
Actor-Partner Model mediational model depicting both the direct and indirect effects of previous positive and negative communication on current cancer-related distress in which the effects of communication are mediated by current intimacy. Note: For simplification purposes, in the figure, positive and negative communication are depicted together, but in the actual analysis each of the two types of communication were treated as separate predictors, each with its own actor and partner effects (as depicted in Fig. 1). Actor distress indicates the actor effect for communication on distress and Actor intimacy indicates the actor effect for communication on distress (likewise for the two partner effects)
Results
Descriptive analyses
Table 1 details the sample characteristics. With regard to disease site, the sample was relatively evenly divided between patients with LC and HNC. Baseline differences between the two disease site samples were evaluated with regard to demographic and medical variables as well as the major study variables. The only significant difference was that LC patients were significantly older (M = 63.0, SD = 12.5) than HNC patients (M = 58.3, SD = 10.6; t(137) = 2.4, p < .01).
Table 1. Descriptive information on study sample patients partners.
| Variable | N | % | M | SD | N | % | M | SD |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male | 86 | 61.9 | 49 | 35.3 | ||||
| Female | 53 | 38.1 | 90 | 64.7 | ||||
| Age (years) | 60.4 | 11.7 | 58.7 | 10.7 | ||||
| Ethnicity | ||||||||
| White | 129 | 92.8 | 116 | 92.1 | ||||
| Non-white | 10 | 7.2 | 7 | 5.0 | ||||
| Years of education | ||||||||
| <College | 82 | 59.4 | 74 | 59.2 | ||||
| ≥College | 55 | 39.9 | 51 | 40.8 | ||||
| Family income ($) | 72,362 | 49,078 | 72,304 | 52,921 | ||||
| Relationship length (years) | 30.4 | 15.1 | 31.4 | 15.1 | ||||
| Type of cancer | ||||||||
| Head & neck | 77 | 55.4 | ||||||
| Lung | 62 | 44.6 | ||||||
| Stage of disease | ||||||||
| 0 | 1 | 0.7 | ||||||
| 1 | 25 | 17.9 | ||||||
| 2 | 22 | 15.8 | ||||||
| 3 | 43 | 30.9 | ||||||
| 4 | 48 | 34.5 | ||||||
| Baseline ECOG | ||||||||
| 0 | 77 | 55.8 | ||||||
| 1 | 54 | 39.1 | ||||||
| 2 | 4 | 2.9 | ||||||
| 3 | 0 | 0 | ||||||
| 4 | 1 | 1 | ||||||
| Time since diagnosis (years) | 1.2 | 2.5 | ||||||
| Treatment administered | ||||||||
| Surgery (yes) | 93 | 67 | ||||||
| Chemotherapy (yes) | 82 | 59 | ||||||
| Radiation (yes) | 79 | 57 | ||||||
Table 2 presents the means and standard deviations for the study variables by social role and assessment time as well as the results of a multilevel analysis that examined mean differences as a function of role (patient/spouse), time, and a role by time interaction. Results showed that patients reported higher levels of positive communication and intimacy and lower levels of negative communication than spouses and that positive communication and distress decreased over time.
Table 2. Descriptive information on variables included in the analyses.
| Patient | Spouse | Role effect | Time effect | Role 9 × time interaction | |||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Time 1 (n = 139) M (SD) | Time 2 (n = 108) M (SD) | Time 3 (n = 91) M (SD) | Time 1 (n = 139) M (SD) | Time 2 (n = 90) M (SD) | Time 3 (n = 71) M (SD) | F(1,310) | F(2,186) | F(2,316) | |
| Functional impairment | 26.5 (18.2) | 23.0 (18.99) | 23.1 (16.6) | – | – | – | – | 4.26* | – |
| Positive communication | 0.23 (0.84) | −0.06 (0.85) | −0.05 (0.96) | −0.02 (0.80) | −0.03 (0.78) | −0.24 (0.84) | 8.57** | 9.13** | 1.93 |
| Sharing concerns | 3.0 (0.1) | 2.6 (1.2) | 2.5 (1.3) | 2.8 (1.0) | 2.6 (1.1) | 2.5 (1.3) | |||
| Self-disclosure | 15.3 (5.1) | 13.9 (5.4) | 14.0 (5.8) | 13.5 (5.5) | 13.6 (5.6) | 14.0 (5.8) | |||
| Perceived partner disclosure | 14.8 (5.4) | 13.2 (5.7) | 14.2 (5.9) | 13.8 (5.5) | 14.2 (5.4) | 14.1 (5.9) | |||
| Negative communication | −0.03 (0.82) | −0.04 (0.75) | −0.14 (0.73) | 0.10 (0.77) | −0.01 (0.77) | 0.08 (0.80) | 9.38** | 0.06 | 1.41 |
| Mutual avoidance | 7.4 (4.8) | 7.3 (4.6) | 6.9 (4.4) | 7.0 (4.2) | 7.0 (4.4) | 6.9 (4.1) | |||
| Patient demand-spouse withdraw | 7.1 (4.6) | 6.9 (4.2) | 6.1 (3.6) | 7.7 (4.9) | 7.1 (4.70) | 7.4 (5.2) | |||
| Spouse demand-patient withdraw | 6.8 (4.6) | 7.0 (4.9) | 6.5 (3.9) | 7.7 (4.9) | 7.2 (4.7) | 7.5 (4.8) | |||
| Spouse unsupportive behavior | 17.5 (5.7) | 17.4 (5.4) | 7.1 (5.0) | 17.4 (5.7) | 18.0 (4.6) | 18.7 (4.1) | |||
| Relationship intimacy | 0.11 (0.81) | 0.08 (0.84) | 0.12 (0.79) | −0.12 (0.93) | −0.09 (0.93) | −0.15 (0.93) | 29.07** | 0.32 | 0.53 |
| Cancer-specific intimacy | 6.1 (1.3) | 6.0 (1.4) | 6.0 (1.3) | 5.6 (1.8) | 5.6 (1.8) | 5.4 (1.7) | |||
| Global intimacy | 4.1 (0.8) | 4.1 (0.9) | 4.1 (0.8) | 3.8 (0.9) | 3.9 (0.9) | 3.7 (0.9) | |||
| Global relationship affection | 9.1 (2.3) | 9.0 (2.4) | 9.3 (2.1) | 9.0 (2.4) | 8.9 (2.9) | 8.8 (2.8) | |||
| Psychological adjustment | 0.14 (−0.01) | −0.01 (0.96) | −0.12 (0.93) | 0.07 (0.97) | −0.11 (.90) | −0.08 (0.91) | 0.23 | 5.89** | 0.52 |
| Brief symptom inventory | 10.3 (8.5) | 9.3 (8.2) | 8.5 (7.2) | 9.3 (8.2) | 6.3 (7.9) | 6.3 (7.2) | |||
| MHI Psychological distress | 57.1 (9.7) | 57.7 (12.0) | 55.3 (10.1) | 57.7 (12.0) | 57.6 (13.9) | 57.6 (13.9) | |||
| MHI Psychological well-being | 58.1 (9.9) | 58.6 (10.3 | 57.9 (9.4) | 58.6 (10.3) | 57.9 (13.1) | ||||
MHI mental health inventory. Standardized scores for the composite measures are in bold and means and standard deviations for the individual scale scores are under each composite score
For descriptive purposes comparisons were conducted between the current study sample and previously published studies with regard to scores on distress, intimacy, and communication. Because the BSI has a clinical cut-off, we compared patients and partners BSI distress levels in the present study with available data on similar populations from previous studies. In the current study, 16.7% of patients and 11.3% of partners met the clinical cutoff for psychological distress on the BSI. Although the rate for patients is lower than those reported in some studies (e.g., Bergquist et al., 2007; Graves et al., 2007; Hopwood & Stephens, 2000; Montazeri et al., 2005; Uchitomi et al., 2000) it is comparable to the rates reported in other studies (Kugaya et al., 2000; Sehlen et al., 2003). Patient ratings of global intimacy (PAIR) were significantly higher (t(212) = 5.9, p < .05) in a previously published study in prostate cancer patients (M = 4.29, SD = .68; Manne et al., 2010), compared to patients in the current study;, however spouse rated intimacy did not differ significantly between the two studies (t(212) = .07; p >.05; M = 3.89, SD = .82).
With regard to positive and negative communication, patients in the current study disclosed and shared concerns less, perceived greater partner disclosure, and rated mutual avoidance as being higher than previous studies of cancer patients (Manne et al., 2004, 2006, 2010), whereas their ratings of unsupportive spouse behaviors did not differ significantly from previous studies (Manne et al., 1999). In contrast, partner-rated patient demand-partner withdraw communication was higher than in previous studies of couples coping with cancer (Manne et al., 2010), but their levels of sharing (Manne et al., 2010)and mutual avoidance were similar to previous research (Manne et al., 2006, 2010).
Does communication predict distress?
The regression coefficients (and standard errors) assessing the direct effects of past communication on current distress (controlling for past distress) are presented in Table 3.1 As expected, there was a strong degree of continuity in distress such that individuals who were high at baseline were distressed at the subsequent assessments. Significant coefficients were also found for the actor effect of positive communication and the partner effect of negative communication. The actor effect indicates that individuals who used more positive communication strategies in the past reported lower subsequent distress. The partner effect indicates that if the person's partner used more negative communication in the past, the person reported higher subsequent distress.
Table 3. Multilevel regression coefficients predicting current distress and current intimacy.
| Predicting current distress without intimacy | Predicting current distress with current intimacy | Predicting current intimacy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Predictor variable | b | SE | b | SE | B | SE |
|
| ||||||
| Past distress | .705** | .041 | .650** | .041 | −.209** | .047 |
| Past own positive communication (Actor PC) | −.088* | .041 | −.042 | .041 | .188** | .047 |
| Past partner positive communication (Partner PC) | .030 | .040 | .041 | .038 | .046 | .046 |
| Past own negative communication (Actor NC) | −.002 | .051 | −.098 | .052 | −.389** | .057 |
| Past partner negative communication (Partner NC) | .100* | .047 | .050 | .046 | −.219** | .053 |
PC positive communication, NC negative communication;
p < .05;
p ≤ .01
Does intimacy mediate the effects of past communication on distress?
When the person's current report of intimacy was added to the model along with positive and negative communication, the effect of the person's intimacy on current distress was b = −.246, SE = .047, p < .01. As Table 3 shows, the effects of both a person's own past positive communication and his or her partner's past negative communication on distress decreased by approximately 50% after controlling for the person's current level of intimacy. This finding is consistent with mediation.
For the purposes of testing mediation, a final analysis was conducted in which intimacy was predicted by the four communication variables, controlling again for past distress (see the last two columns of Table 3). As Fig. 3 illustrates, individuals' past distress, as well as their own and their partner's use of negative communication were negatively related to current intimacy. Those who used more positive communication in the past reported higher levels of current intimacy; however, there was no evidence that the partner's past positive communication had an effect on the individual's reports of current intimacy.2 Sobel tests were conducted to test whether current intimacy mediated the relationship between past communication and current distress, controlling for past distress.3 The test for the partner's past negative communication was z = 3.264, p = .001 and the test for the person's own past positive communication z = 3.175, p = .002. Both are consistent with mediation.
Fig. 3.
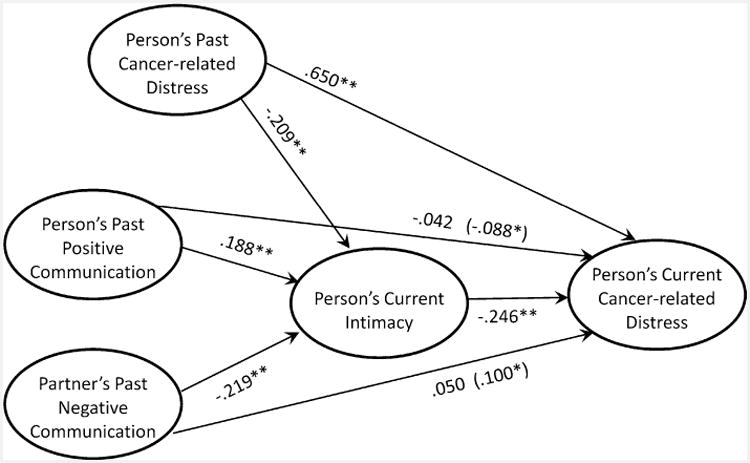
Summary of results from the mediational model in which the effects of the person's own past positive communication and his or her partner's past negative communication on current distress are mediated by the person's current intimacy. Coefficients in parentheses indicate direct effects when current intimacy is not included in the model. *p < .05; **p < .01
Discussion
Given the unique challenges to communication encountered by couples dealing with LC and HNC, it is surprising that there have been so few studies examining relationship communication processes and their association with distress in this population. Our findings showed that individuals who engaged in more positive spousal communication experienced less distress and that the partners of individuals who engaged in more negative communication experienced greater distress. Our findings also lend partial support for the RIM using longitudinal data and suggest that intimacy is a key mediator of the relationship between spousal communication and distress, regardless of social role.
It is not surprising that one's own perception of positive relationship communication was associated with greater intimacy and less distress whereas partner perceptions of positive relationship communication were not associated with either intimacy or distress. Although social support that is not perceived by the recipient (“invisible support”) may play a stronger role in predicting reductions in psychological distress than support that is perceived as being provided (Bolger et al., 2000), studies evaluating relationship communication have typically found that one's own perceptions of relationship communication have a stronger association with one's own distress than a partner's perceptions (Manne et al., 2006).
It is surprising that a partner's perceptions of negative communication predicted one's own intimacy, but one's own perception of negative communication did not. One possibility is that in this particular population of patients with more advanced disease; partner perceptions of negative communication had a detrimental effect on subsequent partner behavior. That is, if the partner perceives that communication is poor, they may be more likely to adopt negative communication, which could influence the other partner's perceptions of intimacy and distress. Future studies may benefit from evaluating the influence of partner perceptions of negative communication as well as the partner's own subsequent communication to determine whether this explanation is viable. Regardless, this finding underscores the importance of including both partners in assessments of communication processes as well as in clinical interventions.
The finding that relationship intimacy was compromised by earlier psychological distress is noteworthy and consistent with the general marital literature suggesting that distress adversely affects relationship quality (Karney, 2001; Whisman & Uebelacker, 2009) and may erode support provision (Bolger et al., 1996). Distressed partners may be less able to effectively communicate and provide support that is adequately matched to the patient's needs. They may also be more likely to devaluate their relationships and be less likely to recognize the support that is provided by their partners. Thus, individuals who are in couples where one or both partners are experiencing heightened distress levels may be at increased risk for future distress because of the adverse effects of individual-level distress on their relationship perceptions and interaction patterns. The possibility that there may be profiles of ‘at-risk’ couples should be examined in future research.
Strengths of this study include its prospective design, the fact that it is one of very few studies to have examined the role of relationship processes in the adjustment of both partners to LC and HNC, and the use of actor-partner statistical modeling that controlled for the non-independence of patient and spouse responses and allowed us to simultaneously model trajectories of distress for both partners over time.
This study also had some limitations. First, we had a low rate of study acceptance and a significant number of dropouts. Study refusers may have been more distressed which may have biased the results towards less distressed individuals and/or couples. Likewise, patients who completed the study had a higher income and their partners were more open with regard to sharing concerns. Second, the sample was comprised of predominantly Caucasian couples and there were more male than female patients. Although there are more male than female LC and HNC patients in the general population, a more diverse sample in terms of ethnicity and gender might have revealed different findings. For example, previous studies have suggested that there are ethnic/cultural differences with regard to the level of comfort that individuals have with depending on their partners for emotional support; suggesting that, intimacy may play a less pivotal role in predicting couples' distress when such cross-cultural differences are considered (Kagawa-Singer & Wellisch, 2003). Because so little is known about differences with regard to couples communication and intimacy across different ethnic groups, future studies would benefit from evaluating cultural differences. Third, we used self-report measures of spousal communication and these may not reflect actual spousal behaviors. Finally, the reliability coefficients for some of the individual communication measures were lower than those reported in previous studies of cancer patients and their partners, and future studies should consider other communication measures developed for the specific needs of this population.
Clinicians working with LC and HNC patients should assess both patient and partner perceptions of relationship communication and intimacy, because both impact couples' distress. A couple-based approach to psychosocial care which addresses couples' distress by enhancing relationship closeness by facilitating positive communication and reducing negative communication may prove beneficial for LC and HNC couples.
Acknowledgments
This research was supported by an Established Investigator in Cancer Prevention and Control Award to Sharon Manne by the NCI (K05 CA109008) and by a Cancer Prevention and Control Career Development Award by the NCI (K07 CA124668) to Hoda Badr.
Footnotes
Given the difference in age for the LC and HNC groups, we conducted a set of analyses examining whether age was a significant predictor in our models. Age was not a significant predictor of distress, and inclusion of age did not affect the results presented in Table 3. Although age did predict intimacy, its presence in the models did not change the pattern of results.
It should be noted that, because there were no significant role differences, Fig. 3 depicts the results using the more generic terms “person” and “partner.”
Mediational analyses were also conducted using the bootstrapping method described by Preacher and Hayes (2008) and conclusions were identical to those from the Sobel test.
Contributor Information
Sharon Manne, Email: mannesl@umdnj.edu, Cancer Institute of New Jersey, New Brunswick, NJ, USA.
Hoda Badr, Email: hoda.badr@mssm.edu, Mount Sinai School of Medicine, New York, NY, USA.
Deborah A. Kashy, Email: kashyd@msu.edu, Michigan State University, East Lansing, MI, USA.
References
- Ayres J. Strategies to maintain relationships: Their identification and perceived usage. Communication Quarterly. 1983;31:62–67. [Google Scholar]
- Badr H, Taylor CL. Effects of relationship maintenance on psychological distress and dyadic adjustment among couples coping with lung cancer. Health Psychology. 2008;27:616–627. doi: 10.1037/0278-6133.27.5.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badr H, Taylor CL. Sexual dysfunction and spousal communication in couples coping with prostate cancer. Psychooncology. 2009;18:735–746. doi: 10.1002/pon.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baile WF, Gibertini M, Scott LL, Endicotte J. Depression and tumor stage in cancer of the head and neck. Psychooncology. 1992;1:15–24. doi: 10.1002/pon.2960010104. [DOI] [Google Scholar]
- Banthia R, Malcarne VL, Varni JW, Ko CM, Sadler GR, Greenbergs HL. The effects of dyadic strength and coping styles on psychological distress in couples faced with prostate cancer. Journal of Behavioral Medicine. 2003;26:31–52. doi: 10.1023/a:1021743005541. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bergquist H, Ruth M, Hammerlid E. Psychiatric morbidity among patients with cancer of the esophagus or the gastro-esophageal junction: A prospective, longitudinal evaluation. Diseases of the Esophagus. 2007;20:523–529. doi: 10.1111/j.1442-2050.2007.00741.x. [DOI] [PubMed] [Google Scholar]
- Bolger N, Foster M, Vinokur AD, Ng R. Close relationships and adjustment to a life crisis: The case of breast cancer. Journal of Personality and Social Psychology. 1996;70:283–294. doi: 10.1037/0022-3514.70.2.283. [DOI] [PubMed] [Google Scholar]
- Bolger N, Zuckerman A, Kessler R. Invisible support and adjustment to stress. Journal of Personality and Social Psychology. 2000;79:953–961. doi: 10.1037//0022-3514.79.6.953OI:10.103//0022-3514.79.6.953. [DOI] [PubMed] [Google Scholar]
- Canary D, Stafford L. Relational maintenance strategies and equity in marriage. Communication Monographs. 1992;59:239–267. [Google Scholar]
- Carmack Taylor CL, Badr H, Lee JH, Fossella F, Pisters K, Gritz ER, et al. Lung cancer patients and their spouses: Psychological and relationship functioning within 1 month of treatment initiation. Annals of Behavioral Medicine. 2008;36:129–140. doi: 10.1007/s12160-008-9062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapple A, Ziebland S, McPerson A. Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. British Medical Journal. 2004;328:1470. doi: 10.1136/bmj.38111.639734.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen A. Perspectives on marital interaction. Multilingual Matters; Clevedon, England: 1988. Dysfunctional interaction patterns in couples; pp. 30–52. [Google Scholar]
- Cleek MG, Pearson TA. Perceived causes of divorce: An analysis of interrelationships. Journal of Marriage and the Family. 1985;47:179–183. [Google Scholar]
- Fang CY, Manne SL, Pape SJ. Functional impairment, marital quality, and patient psychological distress as predictors of psychological distress among cancer patients' spouses. Health Psychology. 2001;20:452–457. [PubMed] [Google Scholar]
- Graves KD, Arnold SM, Love CL, Kirsh KL, Moore PG, Passik SD. Distress screening in a multidisciplinary lung cancer clinic: Prevalence and predictors of clinically significant distress. Lung Cancer. 2007;55:215–224. doi: 10.1016/j.lungcan.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeff AP, Malherbe HL. Intimacy and marital satisfaction in spouses. Journal of Sex and Marital Therapy. 2001;27:247–257. doi: 10.1080/009262301750257100. [DOI] [PubMed] [Google Scholar]
- Haman KL. Psychologic distress and head and neck cancer: Part 1–review of the literature. Journal of Supportive Oncology. 2008;6:155–163. [PubMed] [Google Scholar]
- Hopwood P, Stephens R. Depression in patients with lung cancer: Prevalence and risk factors derived from quality-of-life data. Journal of Clinical Oncology. 2000;18:893–903. doi: 10.1200/JCO.2000.18.4.893. [DOI] [PubMed] [Google Scholar]
- Jenewien J, Zwahlen R, Zwahlen D, Drabe N, Moergeli H, Buchi S. Quality of life and dyadic adjustment in oral cancer patients and their female partners. European Journal of Cancer Care. 2008;17:127–135. doi: 10.1111/ecc.2007.17.issue-2. [DOI] [PubMed] [Google Scholar]
- Jones E, Lund VJ, Howard DJ, Greenberg MP, McCarthy M. Quality of life of patients treated surgically for head and neck cancer. Journal of Laryngology and Otology. 1992;106:238–242. doi: 10.1017/S0022215100119152. [DOI] [PubMed] [Google Scholar]
- Kagawa-Singer M, Wellisch DK. Breast cancer patients' perceptions of their husbands' support in a cross-cultural context. Psychooncology. 2003;12:24–37. doi: 10.1002/pon.619. [DOI] [PubMed] [Google Scholar]
- Karney BR. Depressive symptoms and marital satisfaction in the early years of marriage: Narrowing the gap between theory and research. In: Beach SRH, editor. Marital and family processes in depression. Washington, DC: American Psychological Association; 2001. pp. 45–68. [Google Scholar]
- Kayser K, Sormanti M. A follow-up study of women with cancer: Their psychosocial well-being and close relationships. Social Work in Health Care. 2002;35:391–406. doi: 10.1300/J010v35n01_04. [DOI] [PubMed] [Google Scholar]
- Kenny D, Kashy D, Cook D. Dyadic data analysis. New York: Guilford; 2006. [Google Scholar]
- Kim Y, Duberstein P, Sorensen S, Larson M. Levels of depressive symptoms in spouses of people with lung cancer: Effects of personality, social support, and caregiving burden. Psychosomatics. 2005;46:123–130. doi: 10.1176/appi.psy.46.2.123. [DOI] [PubMed] [Google Scholar]
- Kugaya A, Akechi T, Okuyama T, Nakano T, Mikami I, Okamura H, et al. Prevalence, predictive factors, and screening for psychologic distress in patients with newly diagnosed head and neck cancer. Cancer. 2000;88:2817–2823. doi: 10.1002/1097-0142(20000615)88:12<2817:AID-CNCR22>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- Laurenceau JP, Barrett LF, Pietromonaco PR. Intimacy as an interpersonal process: The importance of self-disclosure, partner disclosure and perceived partner responsiveness in interpersonal exchanges. Journal of Personality and Social Psychology. 1998;74:1238–1251. doi: 10.1037/0022-3514.74.5.1238. [DOI] [PubMed] [Google Scholar]
- Laurenceau JP, Barrett LF, Rovine MJ. The interpersonal process model of intimacy in marriage: A daily-diary and multilevel modeling approach. Journal of Family Psychology. 2005;19:314–323. doi: 10.1037/0893-3200.19.2.314. [DOI] [PubMed] [Google Scholar]
- Lindau ST, Surawska H, Paice J, Baron SR. Communication about sexuality and intimacy in couples affected by lung cancer and their clinical-care providers. Psychooncology. 2010 doi: 10.1002/pon.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobchuk MM, Murdoch T, McClment SE, McPherson C. A dyadic affair: Who is to blame for causing and controlling the patient's lung cancer? Cancer Nursing. 2008;31:435–443. doi: 10.1097/01.NCC.0000339253.68324.19. [DOI] [PubMed] [Google Scholar]
- Manne S, Badr H. Intimacy and relationship processes in couples' psychosocial adaptation to cancer. Cancer. 2008;112:2541–2555. doi: 10.1002/cncr.23450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Badr H. Psychooncology. 2009. Intimacy processes and psychological distress among couples coping with head and neck or lung cancers: A test of the relationship intimacy model of couples' psychosocial adaptation. Advance online publication. [DOI] [Google Scholar]
- Manne S, Badr H, Zaider T, Nelson C, Kissane D. Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. Journal of Cancer Survivorship. 2010;4:74–85. doi: 10.1007/s11764-009-0109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Ostroff J, Norton T, Fox K, Goldstein L, Grana G. Cancer-related relationship communication in couples coping with early stage breast cancer. Psychooncology. 2006;15:234–247. doi: 10.1002/pon.941. [DOI] [PubMed] [Google Scholar]
- Manne SL, Ostroff J, Rini C, Fox K, Goldstein L, Grana G. The interpersonal process model of intimacy: The role of self-disclosure, partner disclosure and partner responsiveness in interactions between breast cancer patients and their partners. Journal of Family Psychology. 2004;18:589–599. doi: 10.1037/0893-3200.18.4.589. [DOI] [PubMed] [Google Scholar]
- Manne SL, Ostroff J, Winkel G, Grana G, Fox K. Partner unsupportive responses, avoidant coping, and distress among women with early stage breast cancer: Patient and partner perspectives. Health Psychology. 2005;24:635–641. doi: 10.1037/0278-6133.24.6.635. [DOI] [PubMed] [Google Scholar]
- Manne SL, Pape S, Taylor K, Dougherty J. Spouse support, coping and mood among individuals with cancer. Annals of Behavioral Medicine. 1999;21:111–121. doi: 10.1007/BF02908291. [DOI] [PubMed] [Google Scholar]
- Manne SL, Taylor K, Dougherty J, Kemeny N. Social support and negative responses in the marital relationship: Their association with psychological adjustment among individuals with cancer. Journal of Behavioral Medicine. 1997;20:101–125. doi: 10.1023/a:1025574626454. [DOI] [PubMed] [Google Scholar]
- Montazeri A, Sajadian A, Ebrahimi M, Akbari ME. Depression and the use of complementary medicine among breast cancer patients. Supportive Care in Cancer. 2005;13:339–342. doi: 10.1007/s00520-004-0709-z. [DOI] [PubMed] [Google Scholar]
- Nijboer C, Triemstra M, Tempelaar R, Sanderman R, van den Bos GA. Determinants of caregiving experiences and mental health of partners of cancer patients. Cancer. 1999;86:577–588. doi: 10.1002/(sici)1097-0142(19990815)86:4<577::aid-cncr6>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Oken M, Creech R, Tormey D, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. American Journal of Clinical Oncology. 1982;5:649–655. doi: 10.1097/00000421-198212000-00014. [DOI] [PubMed] [Google Scholar]
- Pistrang N, Barker C. The partner relationship in psychological response to breast cancer. Social Science and Medicine. 1995;40:789–797. doi: 10.1016/0277-9536(94)00136-H. [DOI] [PubMed] [Google Scholar]
- Pistrang N, Barker C. Partners and fellow patients: Two sources of emotional support for women with breast cancer. American Journal of Community Psychology. 1998;26:439–456. doi: 10.1023/A:1022163205450. [DOI] [PubMed] [Google Scholar]
- Porter L, Keefe F, Hurwitz H, Faber M. Disclosure between patients with gastrointestinal cancer and their spouses. Psychooncology. 2005;14:1030–1042. doi: 10.1002/pon.915. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Reis R, Patrick B. Attachment and intimacy: Component processes. In: Higgins E, Kruglanski A, editors. Social psychology: Handbook of basic principles England. New York: Wiley; 1996. pp. 523–563. [Google Scholar]
- Reis H, Shaver PR. Intimacy as an interpersonal process. In: Duck S, editor. Handbook of personal relationships: Theory, research and interventions. New York: Wiley; 1988. pp. 367–389. [Google Scholar]
- Rolke HB, Bakke PS, Gallefoss F. Relationships between hand-rolled cigarettes and primary lung cancer: A Norwegian experience. Clinical Respiratory Journal. 2009;3:152–160. doi: 10.1111/j.1752-699X.2008.00125.x. [DOI] [PubMed] [Google Scholar]
- Sarna L, Cooley ME, Brown JK, Williams RD, Chernecky C, Padilla G, et al. Quality of life and health status of dyads of women with lung cancer and family members. Oncology Nursing Forum. 2006;33:1109–1116. doi: 10.1188/06.ONF.1109-1116. [DOI] [PubMed] [Google Scholar]
- Schaefer MT, Olson DH. Assessing intimacy: The pair inventory. Journal of Marital and Family Therapy. 1981;7:47–60. doi: 10.1111/j.1752-0606.1981.tb01351.x. [DOI] [Google Scholar]
- Schag CA, Ganz PA, Heinrich RL. Cancer rehabilitation evaluation system-short form (CARES-SF): A cancer specific rehabilitation and quality of life instrument. Cancer. 1991;68:1406–1413. doi: 10.1002/1097-0142(19910915)68:6<1406:AID-CNCR2820680638>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Schliephake H, Jamil MU. Prospective evaluation of quality of life after oncologic surgery for oral cancer. International Journal of Oral and Maxillofacial Surgery. 2002;31:427–433. doi: 10.1054/ijom.2001.0194. [DOI] [PubMed] [Google Scholar]
- Sehlen S, Lenk M, Hollenhorst H, Schymura B, Aydemir U, Herschbach P, et al. Quality of life (QoL) as predictive mediator variable for survival in patients with intracerebral neoplasma during radiotherapy. Onkologie. 2003;26:38–43. doi: 10.1159/000069862. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and Family. 1976;38:15–28. [Google Scholar]
- Steinberg T, Roseman M, Kasymjanova G, Dobson S, Lajeunesse L, Dajczman E, et al. Prevalence of emotional distress in newly diagnosed lung cancer patients. Supportive Care in Cancer. 2009;17:1493–1497. doi: 10.1007/s00520-009-0614-6. [DOI] [PubMed] [Google Scholar]
- Talmadge L, Dabbs JM. Intimacy, conversational patterns, and concomitant cognitive/emotional processes in couples. Journal of Social and Clinical Psychology. 1990;9:473–488. [Google Scholar]
- Uchitomi Y, Mikami I, Kugaya A, Akizuki N, Nagai K, Nishiwaki Y, et al. Depression after successful treatment for nonsmall cell lung carcinoma. Cancer. 2000;89:1172–1179. doi: 10.1002/1097-0142(20000901)89:5<1172:AID-CNCR27>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- Veit CT, Ware JE., Jr The structure of psychological distress and well-being in general populations. Journal of Consulting and Clinical Psychology. 1983;51:730–742. doi: 10.1037/0022-006X.51.5.730. [DOI] [PubMed] [Google Scholar]
- Vickery L, Latchford G, Hewison J, Bellew M, Feber T. The impact of head and neck cancer and facial disfigurement on the quality of life of patients and their partners. Head and Neck. 2003;25:289–296. doi: 10.1002/hed.10206. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA. Prospective associations between marital discord and depressive symptoms in middle-aged and older adults. Psychology and Aging. 2009;24:184–189. doi: 10.1037/a0014759. [DOI] [PubMed] [Google Scholar]
- Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantodosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19:AID-PON501>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- Zhang A, Siminoff L. Silence and cancer: Why do families and patients fail to communicate? Health Communication. 2003;15:415–429. doi: 10.1207/S15327027HC1504_03. [DOI] [PubMed] [Google Scholar]


