Abstract
On the road to metastasis a cancer cell has to overcome two major obstacles: the physical escape from the primary tumor to a distant tissue and the adaptation to the new microenvironment via colonization and the formation of a secondary tumor. Accumulated scientific findings support the hypothesis that inflammation is a critical component of the tumor microenvironment and develops as a result of tumor-induced recruitment of inflammatory cells and their reciprocal interaction with other cells from the tumor network. These interactions modulate immune responses to suppress antitumor immunity and activate feedback amplification signaling loops that link nearly all the cells in the cancer inflammatory milieu. The coordinated regulation of cytokines/chemokines, receptors and other inflammatory mediators enables the different steps of the metastatic cascade. As a target organ for colonization, the bone is rich in inflammatory mediators that are critical for successful cancer growth. In this review, we focus on the inflammatory cells, molecules and mechanisms that facilitate the expansion of cancer cells from the primary tumor to their new ‘home' in the skeleton.
Introduction
Inflammation is a response of the organism to resolve infection, tissue injury or other cellular trauma, and it involves the repair mechanisms that restore the functionality of tissues.1 Experimental findings demonstrate that the tumor microenvironment is steeped with inflammation, including a high infiltration of immune cells and the expression of inflammatory cytokines/chemokines and their receptors.2,3 Cancer and wound healing share several molecular pathways, and tumors have been viewed as ‘wounds that do not heal', where continuous cell renewal and proliferation is induced by persistent inflammation.4 In the tumor microenvironment, immune cells interact with cancer cells leading to the progression, migration and invasion of tumors.5 The accumulated research evidence leaves no doubt to recognize inflammation as one of the hallmarks of cancer.6
About 15–20% of all human tumors originate as a result of chronic infections and lasting inflammatory conditions—for example, the association of Helicobacter pylori infection with gastric cancer, herpes virus with cervical cancer and obesity-mediated inflammation with liver cancer.7,8,9 Inflammation is capable of promoting malignancy through the release of chemicals that are deleterious for neighboring cells edging cancer toward the stage of higher malignancy. For example, reactive oxygen species (ROS), proteases, inflammatory cytokines and other detrimental factors released by macrophages and neutrophils at sites of inflammation have the potential to damage surrounding tissue by introducing genetic and epigenetic alterations in critical tumor suppressors or proto-oncogenes such as tumor protein p53 (TP53), phosphatase and tensin homolog (PTEN) and MYC.5,9,10,11,12,13 On the other hand, the activation of oncogenes and other cancer-promoting mutations or genetic rearrangements results in the induction of transcriptional programs that promote an inflammatory microenvironment.14,15,16 When the tumor is incipient, both antitumorigenic and protumorigenic inflammatory signaling concur, but tumor progression results in the predominance of protumorigenic molecules that shape the microenvironment and significantly contribute to the cancer hallmark potentials. This type of inflammation is the source of survival, growth and proangiogenic factors, as well as extracellular matrix (ECM)-modifying enzymes that facilitate vascularization, invasion and metastasis.9,17
In solid carcinomas, when the blood supply becomes insufficient (noticeably at the tumor core), oxygen and nutrient depletion occurs, which results in necrotic cell death. As a consequence, damage-associated molecular patterns (DAMPs) such as ATP, calreticulin, histones, heat-shock proteins and high-mobility group protein B1 (HMGB1) are exposed or released, and upon interaction with leukocyte receptors they stimulate the production of proinflammatory cytokines, such as interleukin (IL)-1, IL-6 and tumor necrosis factor-α (TNFα), or other mediators that modulate the immune responses causing tumor progression.18,19,20 Importantly, DAMPs can induce immunogenic cell death with the activation of antitumor immunity.21,22,23,24
Besides the immune cells, cancer-associated fibroblasts (CAFs) are an important component of tumor stroma. CAFs secrete stromal cell-derived factor 1 (SDF1, also known as chemokine C-X-C motif ligand 12 (CXCL12)), which stimulates tumor growth and angiogenesis by recruiting endothelial progenitor cells.25 CAFs are also involved in the homing of metastatic cells to the bone marrow through the expression of CXCL12 and insulin-like growth factor 1 (IGF-1), which are responsible for the selection of the metastatic cells directed to high CXCL12-expressing microenvironment.26 Fibroblasts isolated from mouse models of squamous-cell carcinoma, mammary and pancreatic cancers showed a proinflammatory gene signature including the tumor-promoting cytokines (such as IL-6, IL-1β), chemoattractants of macrophages and neutrophils (CXCL1, CXCL2 and CXCL5) and matrix-modifying proteases (such as matrix metalloproteinase 3 (MMP3) and MMP12). Inflammatory CAFs demonstrated the activation of nuclear factor-κB (NF-κB) signaling responsible for high macrophage infiltration, enhanced angiogenesis and tumor growth.27 Therefore, the persistent nonresolving inflammation that characterizes the tumor microenvironment originates tissue damage via increased cell necrosis. When tissue-resident phagocytes (predominantly macrophages and neutrophils) remove these cells they generate an inflammatory response,28 which develops into a vicious cycle that fuels tumor progression.
Inflammation and Metastasis
About 90% of cancer-related deaths are caused by metastasis. Metastasis is a multistep process that involves two major stages: the escape of the cancer cell from the primary tumor to a distant site and the adaptation of the disseminated cell to the new microenvironment with organ colonization.29 A critical step in the first phase is the activation of a regulatory program known as the epithelial to mesenchymal transition (EMT).30 EMT involves profound alterations in gene expression and morphology associated with the downregulation of cell adhesion proteins, such as E-cadherin (E-cad).31 When epithelial cancer cells undergo EMT, they acquire mesenchymal characteristics with an invasive ability to dissociate from the primary tumor and enter the circulation. These circulating cells are capable of disseminating, and they survive until they encounter a favorable niche where they can proliferate to form metastasis. Continuous inflammation is linked to the activation of the EMT program, which correlates with the expression of inflammatory mediators and myeloid cell infiltration. EMT occurs at the invasive front of tumors, where macrophage numbers are high.32,33 Macrophages are one of the major immune infiltrates in tumors,2 and the number of CD68+ tumor-associated macrophages has been convincingly associated with poor outcomes and treatment failures.34
Macrophages have been classified into M1 or M2 according to functional activation in response to environmental signals. M1s are activated by microbial signals or interferon-γ and are capable of killing tumor cells, whereas M2s are protumorigenic, promote angiogenesis, tissue repair, remodeling and have a role in the resolution of inflammation.35 M2s are activated by T helper (Th2) cytokines such as IL-4 and IL-13. In the tumor microenvironment, macrophages are generally polarized toward the M2-like phenotype,36 where they develop a prometastatic function, as illustrated in a model of mammary carcinogenesis.37 In this case, CD4+ T lymphocytes expressing IL-4 induced the M2-like characteristics of tumor macrophages with elevated epidermal growth factor expression that increased the metastatic potential of cancer cells.37 Furthermore, IL-4-activated M2-like macrophages express chemokine C-C motif ligand 18 (CCL18) and promote invasion and metastasis by enhancing the adherence of cancer cells to the ECM.38,39
Tumor cells can subvert the function of macrophages and take advantage of their signaling to escape from the primary tumor. For example, experimental findings showed that Snail (also known as zinc-finger protein SNAI1), a crucial EMT-inducer transcription factor that represses the expression of E-cad, was stabilized by the macrophage-derived inflammatory cytokine TNFα, which involved the activation of the NF-κB signaling pathway.40 Snail stabilization was demonstrated to be critical to promote cell migration and metastasis. In support of this relationship, lipopolysaccharide (LPS)-induced inflammation and TNFα expression by hematopoietic cells resulted in the activation of NF-κB in cancer cells and metastatic tumor progression in a mouse model of colon carcinoma.41 However, when NF-κB was inhibited in cancer cells, LPS reverted the growth response into tumor regression through the upregulation of TNF-related apoptosis-inducing ligand (TRAIL) and the activation of TRAIL receptor (TNF receptor superfamily member 10b). NF-κB has also been connected with the activation of EMT through regulation of crucial EMT inducers such as the zinc-finger E-box-binding homeobox (ZEB) family of transcription factors.42,43,44 Additional evidence linking inflammation and EMT was revealed recently, as M2-like (macrophage colony-stimulating factor (M-CSF; also known as colony-stimulating factor 1 (CSF1)) and IL-4-treated) macrophages were capable of inducing a stable-EMT program in prostate cancer cells, which involved the regulation of the transcription factor ZEB1.45 These EMT cells demonstrated an increased metastatic potential in vivo and were capable of proliferating and colonizing a distant site.45 Of note, a recent study in models of head and neck and breast cancer revealed how TNFα-mediated Snail acetylation regulated its transcriptional activity to control the expression of crucial EMT genes. Snail acetylation further activated the feedback expression of TNFα, CCL2 (also known as monocyte chemotactic protein-1 (MCP-1)) and CCL5 to promote macrophage infiltration, M2 polarization and increased metastasis.46
Inflammation in EMT is a critical step in metastasis. A breast cancer study found that activation-induced cytidine deaminase (AID/AICDA), an enzyme implicated in DNA demethylation and cell reprograming,47,48 was required for EMT, as it regulated the methylation of crucial genes involved in this transition.49 These findings suggest that AID may have a critical role in early stages of metastasis. As AID is induced by inflammatory cytokines such as TNFα and its expression has been correlated with chronic inflammation and tumor progression,11,50,51,52 these results implicate inflammation in EMT. Other findings in a mouse model of pancreatic cancer identified EMT as an early event in the dissemination of malignant cells, where it preceded tumor formation and was facilitated by inflammation. When the mice were treated with the anti-inflammatory drug dexamethasone, they demonstrated a radical suppression of cancer dissemination.53
The inflammatory cytokine IL-6 is elevated during several tumorigenic processes in correlation with tumor grade and poor survival.54,55 IL-6 induces EMT in breast cancer cells,56 which could be a consequence of continuous signal transducer and activator of transcription 3 (STAT3) activation that leads to the downregulation of crucial EMT-regulatory microRNAs.57 An interesting report illustrates how tumor-derived IL-6 and IL-8 (CXCL8) attract circulating tumor cells (CTCs) to the original tumors (termed as ‘tumor self-seeding') and influence tumor progression and metastasis through the selection of the most aggressive cancer cells.58 Furthermore, tumor self-seeding induced an increase in infiltrating myeloid cells, significantly macrophages and neutrophils, which promote an inflammatory microenvironment and stimulate the expression of IL-6, IL-8 and other tumor-promoting factors.8,58
The chemokine CCL2 has been correlated with poor prognosis in cancer patients.59 In a mouse model of breast cancer metastasis, it was determined that CCL2 facilitated metastasis by attracting inflammatory Gr1+/CCR2+ monocytes to the tumor microenvironment of lung metastases.60 In this model, which resembles human metastasis, the inflammatory monocytes promoted the extravasation of tumor cells, which was mediated by the vascular endothelial growth factor (VEGF). CCL2 produced by CAFs has been implicated in the mechanism of EMT by inducing the expression of fibroblast growth factor receptor 4 (FGFR4) in colorectal cancer.61 In addition, CCL2 activates endothelial cells through the chemokine receptor CCR2 to increase vascular permeability and promote cancer cell extravasation and metastatic dissemination in a model of colon cancer.62
In mouse models of lung metastasis, the inflammatory protein S100A8 induced serum amyloid A3 (SAA3) to activate NF-κB signaling via the toll-like receptor 4 (TLR4) in endothelial cells and macrophages. This resulted in high myeloid cell infiltration, and it accelerated the migration of primary tumor cells to lungs to form metastasis.63 The authors suggested that factors such as S100A8 produced by primary tumors induced the formation of a premetastatic niche.63,64 Recently, the same group discovered that CCL2-CRR2 signaling activated the formation of regions with high vascular permeability, which preceded the appearance of metastatic lesions.65 It was also determined that the expression of the inflammatory factors S100A8/A9 and SAA3 was induced by CCL2 and increased in the regions of vascular permeability through TLR4 lymphocyte antigen 96 (LY96/MD2) signaling activation in endothelial cells and CD45+ leucocytes. These results correlated with lung metastasis patient data for which colocalization of high permeability related to inflammation and CCR2 expression was observed.65 Overall, CCL2 and IL-6 are critical inflammation-induced factors that promote cancer progression and metastasis through multiple mechanisms. Notably, a feedback amplification loop between CCL2 and IL-6 has been revealed in human macrophages, which promote their survival and the M2-like phenotype.66
Accumulated experimental findings provide evidence that in the tumor microenvironment tumor cells and macrophages establish a symbiotic relationship, where macrophages generate an inflammatory microenvironment in favor of cancer growth. In return, macrophages are rewarded with factors that promote their survival, activation and proliferation such as tumor-derived M-CSF.67 A feedback loop has been suggested, which links the macrophage production of cytokines IL-1 and TNF with the induction of colony-stimulating factors (M-CSF, granulocyte–macrophage colony-stimulating factor (GM-CSF) and granulocyte colony-stimulating factor (G-CSF)) in the surrounding cells of the inflammatory microenvironment such as T cells, endothelial cells, fibroblasts and epithelial cells.68,69,70,71,72,73 The CSFs can further promote the proliferation/survival or activation of macrophages and neutrophils to enhance the production of factors that sustain a chronic inflammatory stage. The analysis of Lewis lung carcinoma (LLC) cell-secreted factors further revealed the complex interactions in the tumor milieu. The ECM protein versican (VCAN) produced by cancer cells was identified as a powerful inducer of the inflammatory cytokines IL-6 and TNFα in macrophages upon the activation of TLR2/TLR6 receptors.74 In LLC mouse models, the authors validated that both TNFα and TLR2 were essential for metastasis. The expression of VCAN also potentiated macrophage infiltration and lung metastasis in a mouse model of invasive bladder cancer.75 However, the blockage of the CCL2/CCR2 axis with neutralizing antibodies or by using CCL2−/− and CCR2−/− knockout mice reduced macrophage infiltration, which correlated with a significant decrease in the number of metastases. Similarly, direct macrophage ablation also decreased lung metastases and the expression levels of proinflammatory factors IL-6, CCL2 and cytochrome C oxidase 2 (COX2) in the tumor microenvironment.75 Altogether, these findings illustrate how cancer cells produce factors that build the ECM, such as VCAN, to generate an inflammatory microenvironment that promotes the metastatic growth.
By interacting with cancer cells, macrophages can facilitate their intravasation into the blood and lymphatic vessels and travel together in the circulation to promote dissemination and metastasis.76,77 For example, COX2-expressing macrophages infiltrate the LLC tumors expressing the inflammatory cytokine IL-1α, and they are required for angiogenesis and tumor progression mediated by this cytokine.78 These findings highlight the crucial role of macrophages in inflammation-mediated tumor vascularization and progression.
Myeloid-derived cells facilitate metastatic seeding at distant organs. Interesting findings suggest that VEGF receptor 1 (VEGFR1)+ bone marrow-derived hematopoietic progenitor cells create a premetastatic niche that promotes cancer adherence and growth.79 These cells are directed to specific sites via factors expressed in the primary tumor to condition the distant sites for metastasis. Furthermore, these cells expressed the cluster of differentiation molecule 11b (CD11b), which is found on the surface of myeloid cells including monocytes and macrophages.64,80,81
Tumor-infiltrated myeloid cells express MMPs (MMP2, MMP9 MMP12, MMP13 and MMP14) and other proteases such as cathepsins, which enhance angiogenesis, invasion and metastasis.81,82,83,84 By controlling the proteolytic cleavage of ECM components and chemokines, MMPs increase the infiltration of inflammatory cells providing a regulatory loop that enhances metastasis.15,85 Chemokines and their receptors such as the CXCL12/CXCR4 and CXCL5/CXCR2 axes have been implicated in the accumulation of CD11b+/Gr1+ myeloid cells in the tumor microenvironment.81 Myeloid cells also mediate the mechanistic interactions between different cells in the tumor milieu. For example, a signaling mechanism identified in breast carcinoma connected myeloid, endothelial and cancer cells to facilitate metastasis.86 In the study, CXCL1 and CXCL2 produced by cancer cells recruited myeloid (CD11b+/Gr1+) cells that expressed proinflammatory factors S100A8/9, which enhanced tumor survival, metastasis and resistance to chemotherapy. Feedback signaling originated when TNF-α produced by endothelial cells in response to chemotherapeutic drugs activated the expression of CXCL1/2 in cancer cells.86 Furthermore, in a melanoma model, myeloid cell-derived IL-1β induced paracrine VEGF expression in endothelial cells and the activation of an amplification loop that promoted angiogenesis, inflammation and tumor progression.87
In addition to their role in metastasis and chemoresistance, myeloid cells (CD11b+/Gr1+) suppress the antitumor response mediated by CD8+ T cells.88 In this model of pancreatic carcinoma, tumor cells produced GM-CSF driving the recruitment and development of suppressive CD11b+/Gr1+ cells. These myeloid-derived suppressor cells (MDSCs) comprise a heterogeneous group of myeloid progenitors and immature cells with different phenotypes and a potent immune-suppressor activity.89 Two main MDSC subgroups have been identified in mouse tumor models: the cells with granulocytic (polymorphonuclear) morphology characterized by the surface coexpression of CD11b+Ly6G+Ly6Clow and the monocytic phenotype with the markers CD11b+Ly6G-Ly6Chigh.90 The MDSC subgroups in these models also differ by mechanisms of T-cell suppression: the granulocytic MDSCs generate high levels of ROS and low nitric oxide (NO), whereas the monocytic MDSCs show nearly an opposite pattern (NOhigh/ROSlow). In the majority of murine tumor models the granulocytic MDSCs are the predominant subgroup. Another suppression mechanism common to both subgroups is the production of arginase 1, which induces T-cell suppression via depletion of L-arginine.89 Clinical findings in cancer patients correlate the number of MDSCs in the blood with poor prognosis and metastatic progression.91 Proinflammatory cytokines such as IL-1β and IL-6 have been implicated in the accumulation of MDSCs in the tumor milieu.92,93,94 Furthermore, CXCL1, CXCL2 and CXCL5 chemokines and the CXCR2 receptor have been associated with the infiltration of granulocytic MDSCs (CD11b+Ly6Ghigh) from the circulation into the inflammatory tumor microenvironment.95 These CXCR2+ MDSCs accelerated tumorigenesis induced by chronic inflammation by suppressing the cytotoxicity of CD8+ T cells.
Some reports connect MDSCs with the induction of forkhead box P3 (FOXP3+) regulatory T (Treg) cell differentiation and expansion.96,97 Tregs promote immunosuppression in the tumor microenvironment, and their accumulation in the tumor milieu promotes tumor progression and enables metastasis.98,99,100 Tregs express galectin-1, a mediator of the immunosuppressive activity of these cells.101,102 In normal tissues, Tregs function to maintain immune homeostasis limiting autoimmune responses; however, cancer cells highjack these cells to avoid the immune attack. In the tumor microenvironment inflammatory factors recruit Tregs by inducing the expression in myeloid cells of the chemokine CCL22, a potent chemoattractant of Treg cells.103 Furthermore, the induction of CCL22 by transforming growth factor beta (TGFβ) in certain tumor cells has been reported as a critical mechanism for tumor progression.100
An intriguing report illustrates how a common mutation in the TLR5 occurring in 7.5% of humans influences cancer growth via tumor-related inflammation.104 The use of a genetic mouse model of sarcoma tumorigenesis commensal bacteria promoted distal tumor progression through TLR5-mediated increase in systemic IL-6 levels. In turn, IL-6 stimulated the mobilization and expansion of MDSCs and the tumor infiltration of γδT cells that secreted galectin-1.105 Further analysis showed similar results in a murine model of ovarian cancer, whereas TLR5 loss of function accelerated tumor growth in a model of IL-6 unresponsive breast cancer cells via an increase in systemic IL-17 mediated also by the commensal microbiota.104 Therefore, TLR5 signaling regulates systemic inflammation and immune responses resulting in cancer suppression or progression.
Recent work in a transgenic mouse model of metastatic melanoma further highlights the link between inflammation and metastasis. The authors uncovered a mechanism of how ultraviolet (UV) radiation-induced inflammation and promoted metastasis without affecting the growth or number of primary tumors.106 HMGB1 released by damaged UV-treated cells attracted neutrophils to the tumor. In turn, infiltrated neutrophils secreted TNFα via HMGB1-TLR4 signaling107 to favor the formation of blood vessels, the dissemination of tumor cells through the circulation and lung metastases. Depletion of neutrophils or their chemoattractant HMGB1 significantly abolished metastasis.106 These results emphasize how qneutrophils mediate an inflammatory response facilitating the interactions between tumor cells and blood vessels to enable tumor dissemination and progression. Other studies in different cancer types implicate inflammation-mediated neutrophil infiltration and their interaction with cancer cells in angiogenesis, metastasis and tumor progression.108,109,110,111
Further experimental evidence suggests the role of inflammatory neutrophils in the stabilization of CTCs, cancer cell adhesion to distant organs, tumor-endothelial interactions and resulting metastasis.112,113 For instance, an intriguing report indicates that neutrophils protect CTCs by trapping them in an extracellular DNA net to promote cancer dissemination and metastasis.114 Altogether, these findings suggest that neutrophils are crucial mediators of metastasis-related inflammation.115 However, it is worth noting that there are instances in which these cells turn into an antimetastatic shield.116,117 Furthermore, similar to macrophages, neutrophil functional plasticity in response to environmental signals has been suggested118 by classifying them into N1 (antitumoral) and N2 (protumoral) phenotypes.119 Using mesothelioma and lung cancer models, it was discovered that blocking TGFβ increased cytotoxic neutrophil (CD11b+/Ly6G+) infiltration mediated by CXCL2 and CXCL5.119 These neutrophils (N1-type) activated CD8+ T lymphocytes with an overall antitumor response, and their depletion significantly reversed this effect supporting tumor growth. Therefore, it was proposed that TGFβ, expressed by many cancer cells, functioned as an immunosuppressive cytokine modulating the neutrophil polarization toward the protumorigenic N2-type.119
In summary, convincing findings suggest that sustained inflammation in the tumor microenvironment suppresses antitumor immune responses and triggers feedback amplification loops that enable EMT, dissemination and the distant seeding of the cancer cells (Figure 1).
Figure 1.
The inflammatory tumor microenvironment provides a metastatic route for cancer cells. Cancer cells (CC) produce chemokines and other inflammatory mediators such as IL-6, IL-1β, TNFα, CCL2 and CXCL1/5 that are strong chemoattractants and activators of myeloid-lineage immune cells including monocytes/macrophages (Mφ) and neutrophils (N). Activated immune cells trigger feedback amplification loops with further production of proinflammatory mediators, resulting in a chronic inflammatory state and increased tumor infiltration of myeloid cells. Upon interaction with cancer cells, tumor-infiltrated myeloid cells (CD11b+/Gr1+, Mφ, N) express cytokines/chemokines such as TNFα, IL-6 and CCL2 that induce epithelial to mesenchymal transition (EMT), survival, proliferation and stimulate angiogenesis in the tumor microenvironment. Myeloid-lineage cells also suppress the antitumor immune responses and the activation of cytotoxic CD8+-T lymphocytes (T). Inflammation in the microenvironment results in enhanced stress and necrotic/apoptotic cell death, which leads to HMGB1 release, and triggers the production of TNFα by infiltrated neutrophils through the interaction with TLR4 receptor. Dying cancer cells are phagocytized by macrophages (efferocytosis) to induce their polarization into M2-like macrophages that activate protumoral Th2 responses. Furthermore, myeloid cells facilitate the intravasation and extravasation of EMT-transformed cancer cells through the activation of zones of high vascular permeability in the endothelial barriers. CCL2, S100A8-SAA3 and TNFα induce vascular permeability via their receptors CCR2, TLR4 and TNFR in endothelial cells, neutrophils and macrophages. Once in the circulation, neutrophils protect tumor cells (CTCs) by trapping them in a DNA web and together with monocytes and other myeloid cells mediate their extravasation and seeding at the distant metastatic niche. The conditioning of premetastatic niches is promoted by the accumulation of myeloid (CD11b+) cells with activated integrin α4β1 and the receptors S1PR1 and VEGFR1, which facilitate the seeding of metastatic cells. Enhanced inflammation and the accumulation of myeloid cells results in the increased production of VEGF by endothelial and myeloid cells and a higher expression of MMPs that stimulate angiogenesis and tumor growth.
Molecular Pathways of Metastasis-promoting Inflammation
Identification of the molecular pathways that define cell–cell interactions leading to protumor or antitumor outcomes remains a challenge. Two transcription factors, NF-κB and STAT3, have emerged as crucial regulators of these responses in the inflammatory tumor microenvironment. These factors co-regulate several genes that are critical for cancer survival, proliferation and metastasis.120 NF-κB is activated downstream of the TLR-MyD88 pathway and other inflammatory signals and cytokines such as TNFα, IL1α, IL-1β and HMGB1.19,40,41,63,121 Furthermore, key activators of STAT3 or NF-κB such as the proinflammatory mediators IL-6, IL-8, IL-17, IL-21, IL-23, IL-1β, CCL2 and COX2 are also common targets of both STAT3 and NF-κB.120,122,123 Because these factors are abundant in the tumor microenvironment, both NF-κB and STAT3 are steadily activated in cancer, immune and other stromal cells where they further stimulate the production of inflammatory mediators that trigger amplification loops.120,124,125 Consequently, in the tumor microenvironment, activation of STAT3 can lead to increased NF-κB activity and vice versa. Interestingly, the NF-κB subunit RELA (p65) is constitutively activated in tumors and largely induces the expression of tumor-promoting inflammatory factors. Another NF-κB protein REL, rarely activated in tumors, primarily regulates the cytokines/chemokines associated with antitumoral responses.120 In addition, genetic mutations that lead to constitutive STAT3 activation have been identified in inflammatory human epithelial tumors.126
Subsequently, in the tumor microenvironment, the proinflammatory signals can be transmitted from one cell to another, which promotes a chronic inflammatory status.125 NF-κB can both orchestrate the tumor-promoting inflammation19,121,123,127 and antitumor immune responses.9,128 However, STAT3 has been found to mediate the protumoral/immunosuppressive activity of macrophages and MDSCs, yet opposes the production of antitumoral Th1 cytokines, such as IL-12 and INFγ, whose expression is regulated by NF-κB signaling.124,125,129,130 In addition, STAT3 was shown to directly regulate the expression of the protumorigenic cytokine IL-23 in tumor-associated macrophages.129 In turn, IL-23 activated a signaling in Tregs via its receptor (IL-23R) to enhance FOXP3 expression critical to maintain their immune-suppressor function in the tumor microenvironment.131 Furthermore, a mechanism elucidated in cancer- and tumor-associated myeloid cells shows that continuous STAT3 activation enhances p300-mediated RELA acetylation, which retains RELA in the nucleus to sustain NF-kB activity.132 Ablation of STAT3 in tumor-associated myeloid cells significantly reduced the RELA activity in the tumor milieu including the CD11b+ myeloid infiltrate.132,133 A hypothesis was suggested that when both STAT3 and NF-κB are activated in the same cell they induce the expression of protumorigenic inflammatory signals.120 Accordingly, continuous STAT3 activation in the tumor microenvironment (including the immune cells) selectively favored NF-κB binding to the promoters of genes containing STAT3 DNA-binding sites, which are also associated with immunosuppression and tumor-promoting inflammation.134 In contrast, genetic ablation of STAT3 in myeloid cells increased NF-κB activity associated with the expression of genes that mediate the antitumor immune responses such as INFγ, INFβ, IL-12 and CXCL10.134 Therefore, in the tumor microenvironment, STAT3 prevented the NF-κB-mediated expression of Th1 responsive genes, while enhancing the NF-κB binding and activity in favor of tumorigenesis. Altogether, these findings suggest that the cross talk between STAT3 and NF-κB signaling in the tumor microenvironment is a crucial determinant of inflammation-associated tumor progression.
A recent study in a mouse model of colorectal cancer showed that loss of the tumor suppressor p53 in intestinal epithelial cells enhanced the activation of the IκB kinase (IKK)-β-NF-κB pathway to generate an inflammatory microenvironment and the activation of the EMT program permitting cancer progression, invasion and metastasis.135 Loss of p53 induced the EMT-activating transcription factor Twist and the accumulation of myeloid cells, which in turn produced proinflammatory factors (such as CXCL1, CXCL2, CCL2 and COX2) capable of paracrine STAT3 activation in tumor cells.135 Inflammation-mediated NF-κB activation also induces EMT and metastasis in breast cancer.40,136 The activation of oncogenes leading to inflammation that triggers the NF-κB pathway has also been described. For example, in a genetic mouse model of hepatocellular carcinoma the oncogenic activation of β-catenin induced an NF-κB-mediated inflammatory response that determined the degree of tumor aggressiveness.137
Persistent STAT3 activation has been linked not only to inflammation-induced tumorigenesis but also to the formation of premetastatic niches conditioning the sites of future distant metastases.138,139,140,141 An amplification loop identified in tumors links the sphingosine 1-phosphate (S1P) signaling through the S1P receptor 1 (S1PR1) and the activation of STAT3, which in turn feeds back to upregulate S1PR1.133 This pathway results in the upregulation of S1PR1 in the tumor microenvironment leading to continuous STAT3 activation in cancer cells inducing the expression of factors that trigger the same pathway in myeloid cells.138 This signaling allows STAT3-activated myeloid cells to invade, survive and proliferate at the distant premetastatic sites to facilitate the colonization of cancer cells at the preselected site. Of note, the analysis of lymph nodes from prostate and melanoma cancer patients revealed the accumulation of CD68+ myeloid cells before detecting a metastatic growth.138 Other studies suggest that cancer cells preferentially metastasize at sites at which the expression of specific tumor-promoting factors mimics the primary tumor conditions.26 Accordingly, myeloid cells may function as the initial ‘task force' that selects and prepares the future metastatic site to resemble the primary site, a process that could be enhanced by tumor self-seeding.58
Recent findings suggest another mechanism that leads to STAT3 activation in bone marrow-derived macrophages.142 The study revealed that macrophage-mediated phagocytosis of apoptotic tumor cells (a process termed as efferocytosis) induced STAT3 phosphorylation in macrophages to facilitate protumor M2-like polarization. As phagocytosis is an essential function of macrophages, and significant cell death occurs in the inflammatory tumor microenvironment,142,143 this pathway may represent important signaling toward the tumor-promoting function of macrophages. Although this mechanism is awaiting in vivo validation, in a similar way it could activate other phagocytic cells such as neutrophils and contribute to protumoral N2 polarization.119 Future evaluation of this mechanism in the context of the bone microenvironment may provide novel targets for therapeutic intervention of skeletal metastasis.
Although most pathways of metastasis-promoting inflammation converge in the activation of NF-κB and/or STAT3, different mechanisms that induce the activation of IKKα have been identified.144,145,146 In prostate and breast cancer models, the activation of IKKα by the receptor activator of NF-κB ligand (RANKL) signaling through RANK promotes metastasis.145,146 Upon activation, IKKα translocates to the cancer cell nucleus and directly represses the transcription of the metastasis suppressor maspin (SERPINB5), a mechanism that appears to be independent of NF-κB. Interestingly, the accumulation of inflammatory macrophages and Treg (CD4+/CD25+/FOXP3+) cells was detected in tumors and further identified as major contributors for RANKL expression.145,146
Diverse mechanisms of inflammation-induced tumor progression and metastasis stimulate the infiltration and activation of myeloid cells, which mediate the different steps of the metastasis from EMT and dissemination through circulation to distant organ colonization. Myeloid cells induce immunosuppression, promote angiogenesis, survival of tumor cells and prepare distant sites to facilitate tumor growth.89,147,148,149,150 Different cytokines/chemokines and inflammatory mediators are responsible for the accumulation, survival and proliferation of these cells. Importantly, experimental findings suggest that the phosphatidylinositol 3-kinase-γ (PI3Kγ), also known as p110γ, is the main isoform activated in myeloid cells by various receptor-signaling pathways (GPCR, RTK and TLR/IL-1R) in response to different ligands (CXCL12, VEGF-A, M-CSF, IL-1β and IL-6).151 The report illustrates how this isoform, not usually activated in cancer cells, mediates CD11b+/Gr1+ myeloid cell infiltration into tumors through the activation of the α4β1 integrin. PI3Kγ inhibition significantly suppressed inflammation, vascularization, tumor growth and metastasis, consistent with the role of this myeloid cell population in cancer, and it illuminates the potential inhibition of this activation to target cancer-promoting inflammation.151
The Inflammatory Bone Microenvironment as a ‘home' for Metastatic Cells
The bone marrow microenvironment is a fertile land for the seeding and colonization of metastatic cells. Bone marrow-derived myeloid precursors and other differentiated immune cells have been heavily implicated in metastasis. Furthermore, the majority of the signaling mechanisms that promote inflammation-mediated metastasis are active in the bone microenvironment, which is a rich source of factors that promote the proliferation and differentiation of proinflammatory cells. Although the bone is a frequent target site for several types of cancer such as prostate and breast cancers,152 only recently are the signals that direct bone-specific metastasis beginning to be understood.26,153,154 Importantly, in a dormancy model of bone-metastatic breast cancer, activation of the NF-κB pathway in tumor cells induced the expression of the vascular cell adhesion molecule-1 (VCAM-1). VCAM-1 attracted the α4+β1+-monocytic myeloid (CD11b+) cells containing osteoclast progenitors to enhance osteoclast differentiation and activity and to promote bone-metastatic colonization.153 Therefore, cancer cell–VCAM-1–α4+β1+–myeloid interactions induced the formation and activation of osteoclasts to stimulate tumor growth. Interestingly, the expression of α4β1 integrin was shown to be required for hematopoietic cell homing to the bone marrow.155 VCAM-1 expression can be induced in cancer cells by proinflammatory cytokines such as IL-1.156 Furthermore, as outlined above, the activation of α4β1 integrin induced the recruitment of CD11b+/Gr1+ myeloid infiltrate into tumors, which enhanced inflammation and metastasis.95,151 In addition, activation of α4β1 integrin in myeloid cells can be induced by chemoattractants and proinflammatory cytokines that are rich in the bone microenvironment, including CXCL12, M-CSF, IL-1β, TNFα and IL-6.151 As the mobilization of this myeloid population to tumors has been shown to mediate tumor inflammation and metastasis, the VCAM-1-α4β1 axis may provide a rational link between inflammation and skeletal metastasis. A different study shows that α4β1-expressing macrophages foster a survival PI3K-Akt pathway in VCAM-1+ breast cancer cells, suggesting that VCAM-1-α4β1 interaction promotes both survival and colonization of tumor cells at sites of metastasis.157
One of the hallmarks of skeletal metastasis is the alteration of bone homeostasis, which is accompanied by the production of ECM-derived factors that enhance tumor growth, invasion and survival. When ECM is degraded, it releases factors that stimulate cancer colonization (invasion, survival, proliferation and immunosuppression) and facilitates the bone remodeling process. Examples include IGF-1, bone morphogenetic proteins (BMPs) and TGFβ.26,158,159
RANKL is a master regulator of bone resorption, as an essential factor for osteoclast formation and activation. RANKL is produced by osteoblasts, marrow stromal cells and T cells.160,161,162 Disruption of the balance between RANKL and the decoy receptor osteoprotegerin results in the deregulation of bone homeostasis. Most inflammatory cytokines including TNFα, IL-1 and IL-6 potentiate osteoclastogenesis by inducing RANKL expression in marrow stromal cells, osteoblasts or by stimulating RANK expression in myeloid-lineage cells (osteoclast precursors).163,164,165 Of note, TGFβ was found to induce the expression of the FOXP3 transcription factor and to stimulate the transition of naive T cells into Tregs,166 whereas tumor-infiltrating Tregs produced RANKL to stimulate metastasis in breast cancer.146 Similarly, findings in metastatic prostate cancer suggest that RANKL derived from inflammatory cells (macrophages and T cells) activates IKKα directly repressing maspin. In addition, maspin suppressed the progression of osteolytic lesions in a model of prostate cancer bone metastasis.167 RANKL stimulates osteoclastogenesis and bone resorption, causing the release of TGFβ and other growth factors from the bone matrix. TGFβ in turn induces the accumulation of suppressive myeloid and Treg cells that further produce RANKL to perpetuate a cycle that promotes tumor growth. Given the elevated expression of RANKL and TGFβ in the bone microenvironment, this mechanism is likely to enhance the bone-metastatic colonization by prostate and breast cancer, two carcinomas that frequently progress into skeletal metastasis.152 Furthermore, the activation of NF-κB in breast cancer cells induces the expression of GM-CSF, which promotes osteoclast formation and osteolytic bone metastasis.168 Other findings in bone-metastatic melanoma linked the activation of RANKL-RANK signaling with skeletal metastasis. However, the proposed mechanism was different, through the increased cell migration and invasion of RANK-expressing cancer cells.169
Metastatic cancer cells secrete factors that induce proinflammatory cytokines/chemokines in osteoblasts such as IL-6, IL-8, CCL2 and CXCL5.170,171,172 One of the factors expressed by cancer cells in response to different stimuli such as TGFβ is parathyroid hormone-related protein (PTHrP), which acts in a paracrine manner to induce CCL2, IL-6 and the soluble IL-6 receptor (sIL-6R) in osteoblasts.159,173,174,175 A recent study showed that PTHrP induces IL-6 and VEGF-A in osteoblasts to activate CD11b+/Gr1+ myeloid cells in the bone marrow and enhance angiogenesis, the expression of matrix remodeling proteases and prostate cancer growth in bone.176 Furthermore, cyclophosphamide was found to drive a temporal accumulation of myeloid cells in the bone marrow, elevated expression of CCL2 and increased incidence of prostate cancer skeletal metastasis in mice.177 These studies provide evidence that inflammation not only promotes the infiltration of myeloid cells in the bone microenvironment but also their activation to enable the formation of skeletal metastases.
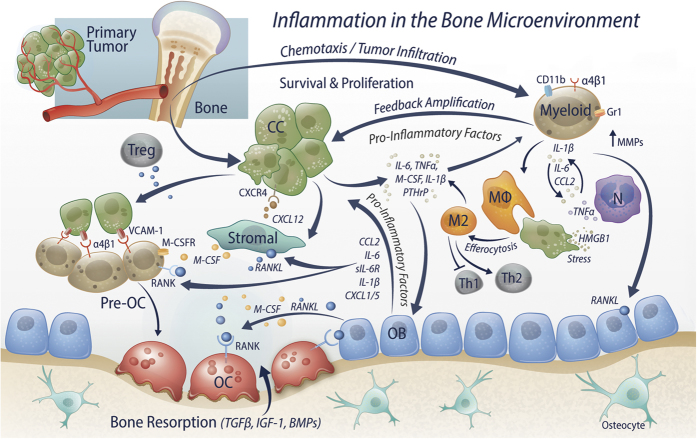
Inflammation generates feed-forward loops in the bone microenvironment that perpetuate the chronic inflammatory stage. For example, a report shows that inflammatory stimuli such as TNFα, IL1β and IL-6 induce the expression of WNT5A in bone marrow stromal cells (BMSCs), which in turn activates paracrine or autocrine NF-κB-mediated signaling in osteoblasts and BMSCs to trigger the expression of proinflammatory cytokines/chemokines including IL-1β, IL-6, CCL2, CCL5, CXCL1 and CXCL5.178 These factors are potent chemoattractants that promote tumor infiltration and activation of inflammatory cells, which foster chronic inflammation, immunosuppression, angiogenesis, matrix remodeling, survival and proliferation of tumor cells.46,66,94,140,179,180,181,182,183,184 A recent study revealed that expression of IL-1β promotes bone-metastatic growth in mouse models of prostate cancer, and its expression correlates with the highest Gleason scores (>7) in humans.185 Taken together, the inflammatory skeletal microenvironment promotes metastasis through multiple mechanisms that involve cycling interactions between tumor cells, inflammatory cells, osteoblasts, osteoclasts and other stromal cells to result in aberrant bone remodeling and tumor growth (Figure 2).
Figure 2.
Inflammation in the bone microenvironment facilitates the colonization of metastatic cancer cells. The bone marrow microenvironment as a source of leukocytes is a rich inflammatory soil for seeding and colonization of metastatic cells. CXCL12 chemokine produced by bone marrow stromal cells and activated myeloid (CD11b+/Gr1+) cells expressing the integrin α4β1 facilitate the homing of cancer cells (CC) through interactions with CXCR4 receptor and VCAM-1. Cancer cells and tumor-infiltrating myeloid cells, including monocytes/macrophages (Mφ) and neutrophils (N), produce proinflammatory stimuli such as IL-1β, IL-6, TNFα and CCL2, or hormones such as PTHrP, which induce an inflammatory response in osteoblasts (OB) and stromal cells. As a result, osteoblasts and stromal cells produce chemoattractants of myeloid cells such as CCL2, CXCL1, CXCL5 and the inflammatory cytokines IL-6, sIL-6R and IL-1β, which further perpetuate the inflammatory state. In addition, cancer cells favor the nucleation of myeloid cells through VCAM-1-α4β1 interactions, which form the osteoclast precursor cells (Pre-OC) that further differentiate into mature osteoclasts (OC) upon stimulation by M-CSF and the receptor activator of NF-κB ligand (RANKL). These factors, produced by osteoblasts, stromal and other immune cells (including Tregs), signal through by interacting with their receptors M-CSFR (CSF1R) and RANK expressed in myeloid-lineage cells, macrophages, osteoclasts and some cancer cells. Importantly, inflammatory cytokines including TNFα, IL-1 and IL-6 induce RANKL expression in marrow stromal cells and osteoblasts and stimulate RANK expression in pre-OC cells to enhance osteoclastogenesis. Activated osteoclasts initiate the degradation of the bone matrix, stimulated by matrix proteases such as MMPs produced by myeloid cells. In turn, bone resorption induces the release of factors that stimulate bone remodeling, osteoblast proliferation/differentiation and tumor progression such as BMPs, IGF-1 and TGFβ. Persistent inflammation also increases cell stress and tissue damage causing apoptotic/necrotic cell death, which releases the HMGB1 and induces TNFα in neutrophils. In addition, phagocytosis of dying cells (efferocytosis) stimulates the tumor-promoting M2-like macrophage polarization that supports further tumor growth and Th2 immune responses. Altogether, inflammation triggers an array of interconnected molecular mechanisms with the expression of factors that mediate the infiltration and activation of myeloid cells to enable the homing, survival and colonization of tumor cells.
Conclusion
Scientific evidence supports the view that chronic inflammation promotes tumor progression and metastasis through diverse mechanisms that converge in the recruitment of cells from the myeloid lineage, including macrophages and neutrophils. Cancer cells modify the function of immune cells to skip their attack and induce the expression of chemoattractants and proinflammatory mediators that perpetuate inflammation to enable metastasis. In particular, the skeleton as a target organ for colonization integrates a complex interaction between different cell types including cancer cells, osteoclasts, osteoblasts, endothelial, stromal and immune cells. Experimental reports suggest that populations of myeloid cells from the primary tumor are the first invaders that condition distant sites for the arrival of tumor cells. Once the tumor cells start proliferating in the bone, inflammatory signals induced by cancer cells and their interactions with neighboring cells trigger amplification cascades that involve virtually all the components of the microenvironment in which immune cells have a fundamental role permitting the tumor colonization. Anti-inflammatory therapies have been evaluated with success for targeting tumor progression and metastasis, and they are associated with reduced infiltration of bone marrow-derived myeloid cells and the prometastatic macrophages.17,186,187,188,189,190 A different approach to target metastasis involves the direct stimulation of antitumor immunity. For example, transformation of macrophages from M2 to M1 type has been demonstrated to recruit cytotoxic T cells and elicit antitumor responses.191,192 These approaches in combination with other therapies have the potential to inhibit tumor progression and metastasis; however, their success in human metastasis including bone remains to be a major challenge.
Acknowledgments
We acknowledge Stephanie O'Neal and Kenneth Rieger from Multimedia Design group of the School of Dentistry for their important contribution in the figure artwork. This work was supported by the National Cancer Institute Grant P01-CA093900 to LKM and HR.
Footnotes
The authors declare no conflict of interest.
References
- Medzhitov R. Origin and physiological roles of inflammation. Nature 2008; 454: 428–435. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Biswas SK, Galdiero MR, Sica A, Locati M. Macrophage plasticity and polarization in tissue repair and remodelling. J Pathol 2013; 229: 176–185. [DOI] [PubMed] [Google Scholar]
- Pages F, Galon J, Dieu-Nosjean MC, Tartour E, Sautes-Fridman C, Fridman WH. Immune infiltration in human tumors: a prognostic factor that should not be ignored. Oncogene 2010; 29: 1093–1102. [DOI] [PubMed] [Google Scholar]
- Dvorak HF. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med 1986; 315: 1650–1659. [DOI] [PubMed] [Google Scholar]
- Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell 2010; 140: 883–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell 2011; 144: 646–674. [DOI] [PubMed] [Google Scholar]
- Park EJ, Lee JH, Yu GY, He G, Ali SR, Holzer RG et al. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression. Cell 2010; 140: 197–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balkwill F, Charles KA, Mantovani A. Smoldering and polarized inflammation in the initiation and promotion of malignant disease. Cancer Cell 2005; 7: 211–217. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature 2008; 454: 436–444. [DOI] [PubMed] [Google Scholar]
- Campregher C, Luciani MG, Gasche C. Activated neutrophils induce an hMSH2-dependent G2/M checkpoint arrest and replication errors at a (CA)13-repeat in colon epithelial cells. Gut 2008; 57: 780–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endo Y, Marusawa H, Kou T, Nakase H, Fujii S, Fujimori T et al. Activation-induced cytidine deaminase links between inflammation and the development of colitis-associated colorectal cancers. Gastroenterology 2008; 135: 889–898. [DOI] [PubMed] [Google Scholar]
- Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 2009; 30: 1073–1081. [DOI] [PubMed] [Google Scholar]
- Iliopoulos D, Hirsch HA, Struhl K. An epigenetic switch involving NF-kappaB, Lin28, Let-7 MicroRNA, and IL6 links inflammation to cell transformation. Cell 2009; 139: 693–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrello MG, Alberti L, Fischer A, Degl'innocenti D, Ferrario C, Gariboldi M et al. Induction of a proinflammatory program in normal human thyrocytes by the RET/PTC1 oncogene. Proc Natl Acad Sci USA 2005; 102: 14825–14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuda A, Wang SC, JPth Morris, Folias AE, Liou A, Kim GE et al. Stat3 and MMP7 contribute to pancreatic ductal adenocarcinoma initiation and progression. Cancer Cell 2011; 19: 441–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shchors K, Shchors E, Rostker F, Lawlor ER, Brown-Swigart L, Evan GI. The Myc-dependent angiogenic switch in tumors is mediated by interleukin 1beta. Genes Dev 2006; 20: 2527–2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balkwill FR, Mantovani A. Cancer-related inflammation: common themes and therapeutic opportunities. Semin Cancer Biol 2012; 22: 33–40. [DOI] [PubMed] [Google Scholar]
- Kono H, Rock KL. How dying cells alert the immune system to danger. Nat Rev Immunol 2008; 8: 279–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakurai T, He G, Matsuzawa A, Yu GY, Maeda S, Hardiman G et al. Hepatocyte necrosis induced by oxidative stress and IL-1 alpha release mediate carcinogen-induced compensatory proliferation and liver tumorigenesis. Cancer Cell 2008; 14: 156–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scaffidi P, Misteli T, Bianchi ME. Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature 2002; 418: 191–195. [DOI] [PubMed] [Google Scholar]
- Guerriero JL, Ditsworth D, Catanzaro JM, Sabino G, Furie MB, Kew RR et al. DNA alkylating therapy induces tumor regression through an HMGB1-mediated activation of innate immunity. J Immunol 2011; 186: 3517–3526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaud M, Martins I, Sukkurwala AQ, Adjemian S, Ma Y, Pellegatti P et al. Autophagy-dependent anticancer immune responses induced by chemotherapeutic agents in mice. Science 2011; 334: 1573–1577. [DOI] [PubMed] [Google Scholar]
- Zitvogel L, Kepp O, Senovilla L, Menger L, Chaput N, Kroemer G. Immunogenic tumor cell death for optimal anticancer therapy: the calreticulin exposure pathway. Clin Cancer Res 2010; 16: 3100–3104. [DOI] [PubMed] [Google Scholar]
- Krysko DV, Garg AD, Kaczmarek A, Krysko O, Agostinis P, Vandenabeele P. Immunogenic cell death and DAMPs in cancer therapy. Nat Rev Cancer 2012; 12: 860–875. [DOI] [PubMed] [Google Scholar]
- Orimo A, Gupta PB, Sgroi DC, Arenzana-Seisdedos F, Delaunay T, Naeem R et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell 2005; 121: 335–348. [DOI] [PubMed] [Google Scholar]
- Zhang XH, Jin X, Malladi S, Zou Y, Wen YH, Brogi E et al. Selection of bone metastasis seeds by mesenchymal signals in the primary tumor stroma. Cell 2013; 154: 1060–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erez N, Truitt M, Olson P, Arron ST, Hanahan D. Cancer-associated fibroblasts are activated in incipient neoplasia to orchestrate tumor-promoting inflammation in an NF-kappaB-dependent manner. Cancer Cell 2010; 17: 135–147. [DOI] [PubMed] [Google Scholar]
- Rock KL, Kono H. The inflammatory response to cell death. Annu Rev Pathol 2008; 3: 99–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaffer CL, Weinberg RA. A perspective on cancer cell metastasis. Science 2011; 331: 1559–1564. [DOI] [PubMed] [Google Scholar]
- Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell 2009; 139: 871–890. [DOI] [PubMed] [Google Scholar]
- Yang J, Weinberg RA. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev Cell 2008; 14: 818–829. [DOI] [PubMed] [Google Scholar]
- Prall F. Tumour budding in colorectal carcinoma. Histopathology 2007; 50: 151–162. [DOI] [PubMed] [Google Scholar]
- Zhu XD, Zhang JB, Zhuang PY, Zhu HG, Zhang W, Xiong YQ et al. High expression of macrophage colony-stimulating factor in peritumoral liver tissue is associated with poor survival after curative resection of hepatocellular carcinoma. J Clin Oncol 2008; 26: 2707–2716. [DOI] [PubMed] [Google Scholar]
- Steidl C, Lee T, Shah SP, Farinha P, Han G, Nayar T et al. Tumor-associated macrophages and survival in classic Hodgkin's lymphoma. N Engl J Med 2010; 362: 875–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon S. Alternative activation of macrophages. Nat Rev Immunol 2003; 3: 23–35. [DOI] [PubMed] [Google Scholar]
- Biswas SK, Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol 2010; 11: 889–896. [DOI] [PubMed] [Google Scholar]
- DeNardo DG, Barreto JB, Andreu P, Vasquez L, Tawfik D, Kolhatkar N et al. CD4(+) T cells regulate pulmonary metastasis of mammary carcinomas by enhancing protumor properties of macrophages. Cancer Cell 2009; 16: 91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonecchi R, Locati M, Mantovani A. Chemokines and cancer: a fatal attraction. Cancer Cell 2011; 19: 434–435. [DOI] [PubMed] [Google Scholar]
- Chen J, Yao Y, Gong C, Yu F, Su S, Chen J et al. CCL18 from tumor-associated macrophages promotes breast cancer metastasis via PITPNM3. Cancer Cell 2011; 19: 541–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Deng J, Rychahou PG, Qiu S, Evers BM, Zhou BP. Stabilization of snail by NF-kappaB is required for inflammation-induced cell migration and invasion. Cancer Cell 2009; 15: 416–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo JL, Maeda S, Hsu LC, Yagita H, Karin M. Inhibition of NF-kappaB in cancer cells converts inflammation- induced tumor growth mediated by TNFalpha to TRAIL-mediated tumor regression. Cancer Cell 2004; 6: 297–305. [DOI] [PubMed] [Google Scholar]
- Chua HL, Bhat-Nakshatri P, Clare SE, Morimiya A, Badve S, Nakshatri H. NF-kappaB represses E-cadherin expression and enhances epithelial to mesenchymal transition of mammary epithelial cells: potential involvement of ZEB-1 and ZEB-2. Oncogene 2007; 26: 711–724. [DOI] [PubMed] [Google Scholar]
- Julien S, Puig I, Caretti E, Bonaventure J, Nelles L, van Roy F et al. Activation of NF-kappaB by Akt upregulates Snail expression and induces epithelium mesenchyme transition. Oncogene 2007; 26: 7445–7456. [DOI] [PubMed] [Google Scholar]
- Huber MA, Azoitei N, Baumann B, Grunert S, Sommer A, Pehamberger H et al. NF-kappaB is essential for epithelial-mesenchymal transition and metastasis in a model of breast cancer progression. J Clin Invest 2004; 114: 569–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roca H, Hernandez J, Weidner S, McEachin RC, Fuller D, Sud S et al. Transcription factors OVOL1 and OVOL2 induce the mesenchymal to epithelial transition in human cancer. PloS One 2013; 8: e76773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu DS, Wang HJ, Tai SK, Chou CH, Hsieh CH, Chiu PH et al. Acetylation of snail modulates the cytokinome of cancer cells to enhance the recruitment of macrophages. Cancer Cell 2014; 26: 534–548. [DOI] [PubMed] [Google Scholar]
- Bhutani N, Brady JJ, Damian M, Sacco A, Corbel SY, Blau HM. Reprogramming towards pluripotency requires AID-dependent DNA demethylation. Nature 2010; 463: 1042–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan HD, Dean W, Coker HA, Reik W, Petersen-Mahrt SK. Activation-induced cytidine deaminase deaminates 5-methylcytosine in DNA and is expressed in pluripotent tissues: implications for epigenetic reprogramming. J Biol Chem 2004; 279: 52353–52360. [DOI] [PubMed] [Google Scholar]
- Munoz DP, Lee EL, Takayama S, Coppe JP, Heo SJ, Boffelli D et al. Activation-induced cytidine deaminase (AID) is necessary for the epithelial-mesenchymal transition in mammary epithelial cells. Proc Natl Acad Sci USA 2013; 110: E2977–E2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endo Y, Marusawa H, Kinoshita K, Morisawa T, Sakurai T, Okazaki IM et al. Expression of activation-induced cytidine deaminase in human hepatocytes via NF-kappaB signaling. Oncogene 2007; 26: 5587–5595. [DOI] [PubMed] [Google Scholar]
- Matsumoto Y, Marusawa H, Kinoshita K, Endo Y, Kou T, Morisawa T et al. Helicobacter pylori infection triggers aberrant expression of activation-induced cytidine deaminase in gastric epithelium. Nat Med 2007; 13: 470–476. [DOI] [PubMed] [Google Scholar]
- Park SR, Zan H, Pal Z, Zhang J, Al-Qahtani A, Pone EJ et al. HoxC4 binds to the promoter of the cytidine deaminase AID gene to induce AID expression, class-switch DNA recombination and somatic hypermutation. Nat Immunol 2009; 10: 540–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhim AD, Mirek ET, Aiello NM, Maitra A, Bailey JM, McAllister F et al. EMT and dissemination precede pancreatic tumor formation. Cell 2012; 148: 349–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salgado R, Junius S, Benoy I, Van Dam P, Vermeulen P, Van Marck E et al. Circulating interleukin-6 predicts survival in patients with metastatic breast cancer. Int J Cancer 2003; 103: 642–646. [DOI] [PubMed] [Google Scholar]
- Schafer ZT, Brugge JS. IL-6 involvement in epithelial cancers. J Clin Invest 2007; 117: 3660–3663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan NJ, Sasser AK, Axel AE, Vesuna F, Raman V, Ramirez N et al. Interleukin-6 induces an epithelial-mesenchymal transition phenotype in human breast cancer cells. Oncogene 2009; 28: 2940–2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo L, Chen C, Shi M, Wang F, Chen X, Diao D et al. Stat3-coordinated Lin-28-let-7-HMGA2 and miR-200-ZEB1 circuits initiate and maintain oncostatin M-driven epithelial-mesenchymal transition. Oncogene 2013; 32: 5272–5282. [DOI] [PubMed] [Google Scholar]
- Kim MY, Oskarsson T, Acharyya S, Nguyen DX, Zhang XH, Norton L et al. Tumor self-seeding by circulating cancer cells. Cell 2009; 139: 1315–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueno T, Toi M, Saji H, Muta M, Bando H, Kuroi K et al. Significance of macrophage chemoattractant protein-1 in macrophage recruitment, angiogenesis, and survival in human breast cancer. Clin Cancer Res 2000; 6: 3282–3289. [PubMed] [Google Scholar]
- Qian BZ, Li J, Zhang H, Kitamura T, Zhang J, Campion LR et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature 2011; 475: 222–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R, Li J, Xie K, Zhang T, Lei Y, Chen Y et al. FGFR4 promotes stroma-induced epithelial-to-mesenchymal transition in colorectal cancer. Cancer Res 2013; 73: 5926–5935. [DOI] [PubMed] [Google Scholar]
- Wolf MJ, Hoos A, Bauer J, Boettcher S, Knust M, Weber A et al. Endothelial CCR2 signaling induced by colon carcinoma cells enables extravasation via the JAK2-Stat5 and p38MAPK pathway. Cancer Cell 2012; 22: 91–105. [DOI] [PubMed] [Google Scholar]
- Hiratsuka S, Watanabe A, Sakurai Y, Akashi-Takamura S, Ishibashi S, Miyake K et al. The S100A8-serum amyloid A3-TLR4 paracrine cascade establishes a pre-metastatic phase. Nat Cell Biol 2008; 10: 1349–1355. [DOI] [PubMed] [Google Scholar]
- Hiratsuka S, Watanabe A, Aburatani H, Maru Y. Tumour-mediated upregulation of chemoattractants and recruitment of myeloid cells predetermines lung metastasis. Nat Cell Biol 2006; 8: 1369–1375. [DOI] [PubMed] [Google Scholar]
- Hiratsuka S, Ishibashi S, Tomita T, Watanabe A, Akashi-Takamura S, Murakami M et al. Primary tumours modulate innate immune signalling to create pre-metastatic vascular hyperpermeability foci. Nat Commun 2013; 4: 1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roca H, Varsos ZS, Sud S, Craig MJ, Ying C, Pienta KJ. CCL2 and interleukin-6 promote survival of human CD11b+ peripheral blood mononuclear cells and induce M2-type macrophage polarization. J Biol Chem 2009; 284: 34342–34354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard JW. Tumour-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer 2004; 4: 71–78. [DOI] [PubMed] [Google Scholar]
- Cannistra SA, Rambaldi A, Spriggs DR, Herrmann F, Kufe D, Griffin JD. Human granulocyte-macrophage colony-stimulating factor induces expression of the tumor necrosis factor gene by the U937 cell line and by normal human monocytes. J Clin Invest 1987; 79: 1720–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cenci S, Weitzmann MN, Roggia C, Namba N, Novack D, Woodring J et al. Estrogen deficiency induces bone loss by enhancing T-cell production of TNF-alpha. J Clin Invest 2000; 106: 1229–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falkenburg JH, Harrington MA, de Paus RA, Walsh WK, Daub R, Landegent JE et al. Differential transcriptional and posttranscriptional regulation of gene expression of the colony-stimulating factors by interleukin-1 and fetal bovine serum in murine fibroblasts. Blood 1991; 78: 658–665. [PubMed] [Google Scholar]
- Groves RW, Rauschmayr T, Nakamura K, Sarkar S, Williams IR, Kupper TS. Inflammatory and hyperproliferative skin disease in mice that express elevated levels of the IL-1 receptor (type I) on epidermal keratinocytes. Evidence that IL-1-inducible secondary cytokines produced by keratinocytes in vivo can cause skin disease. J Clin Invest 1996; 98: 336–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindemann A, Riedel D, Oster W, Ziegler-Heitbrock HW, Mertelsmann R, Herrmann F. Granulocyte-macrophage colony-stimulating factor induces cytokine secretion by human polymorphonuclear leukocytes. J Clin Invest 1989; 83: 1308–1312. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Hamilton JA. Colony-stimulating factors in inflammation and autoimmunity. Nat Rev Immunol 2008; 8: 533–544. [DOI] [PubMed] [Google Scholar]
- Kim S, Takahashi H, Lin WW, Descargues P, Grivennikov S, Kim Y et al. Carcinoma-produced factors activate myeloid cells through TLR2 to stimulate metastasis. Nature 2009; 457: 102–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Said N, Sanchez-Carbayo M, Smith SC, Theodorescu D. RhoGDI2 suppresses lung metastasis in mice by reducing tumor versican expression and macrophage infiltration. J Clin Invest 2012; 122: 1503–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condeelis J, Pollard JW. Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell 2006; 124: 263–266. [DOI] [PubMed] [Google Scholar]
- Wyckoff JB, Wang Y, Lin EY, Li JF, Goswami S, Stanley ER et al. Direct visualization of macrophage-assisted tumor cell intravasation in mammary tumors. Cancer Res 2007; 67: 2649–2656. [DOI] [PubMed] [Google Scholar]
- Nakao S, Kuwano T, Tsutsumi-Miyahara C, Ueda S, Kimura YN, Hamano S et al. Infiltration of COX-2-expressing macrophages is a prerequisite for IL-1 beta-induced neovascularization and tumor growth. J Clin Invest 2005; 115: 2979–2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C et al. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature 2005; 438: 820–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erler JT, Bennewith KL, Cox TR, Lang G, Bird D, Koong A et al. Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the premetastatic niche. Cancer Cell 2009; 15: 35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Huang J, Ren X, Gorska AE, Chytil A, Aakre M et al. Abrogation of TGF beta signaling in mammary carcinomas recruits Gr1+CD11b+ myeloid cells that promote metastasis. Cancer Cell 2008; 13: 23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, DeBusk LM, Fukuda K, Fingleton B, Green-Jarvis B, Shyr Y et al. Expansion of myeloid immune suppressor Gr+CD11b+ cells in tumor-bearing host directly promotes tumor angiogenesis. Cancer Cell 2004; 6: 409–421. [DOI] [PubMed] [Google Scholar]
- Gocheva V, Wang HW, Gadea BB, Shree T, Hunter KE, Garfall AL et al. IL-4 induces cathepsin protease activity in tumor-associated macrophages to promote cancer growth and invasion. Genes Dev 2010; 24: 241–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitamura T, Kometani K, Hashida H, Matsunaga A, Miyoshi H, Hosogi H et al. SMAD4-deficient intestinal tumors recruit CCR1+ myeloid cells that promote invasion. Nat Genet 2007; 39: 467–475. [DOI] [PubMed] [Google Scholar]
- Kessenbrock K, Plaks V, Werb Z. Matrix metalloproteinases: regulators of the tumor microenvironment. Cell 2010; 141: 52–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acharyya S, Oskarsson T, Vanharanta S, Malladi S, Kim J, Morris PG et al. A CXCL1 paracrine network links cancer chemoresistance and metastasis. Cell 2012; 150: 165–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmi Y, Dotan S, Rider P, Kaplanov I, White MR, Baron R et al. The role of IL-1beta in the early tumor cell-induced angiogenic response. J Immunol 2013; 190: 3500–3509. [DOI] [PubMed] [Google Scholar]
- Bayne LJ, Beatty GL, Jhala N, Clark CE, Rhim AD, Stanger BZ et al. Tumor-derived granulocyte-macrophage colony-stimulating factor regulates myeloid inflammation and T cell immunity in pancreatic cancer. Cancer Cell 2012; 21: 822–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol 2009; 9: 162–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youn JI, Nagaraj S, Collazo M, Gabrilovich DI. Subsets of myeloid-derived suppressor cells in tumor-bearing mice. J Immunol 2008; 181: 5791–5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrilovich DI, Ostrand-Rosenberg S, Bronte V. Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol 2012; 12: 253–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunt SK, Yang L, Sinha P, Clements VK, Leips J, Ostrand-Rosenberg S. Reduced inflammation in the tumor microenvironment delays the accumulation of myeloid-derived suppressor cells and limits tumor progression. Cancer Res 2007; 67: 10019–10026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song X, Krelin Y, Dvorkin T, Bjorkdahl O, Segal S, Dinarello CA et al. CD11b+/Gr-1+ immature myeloid cells mediate suppression of T cells in mice bearing tumors of IL-1beta-secreting cells. J Immunol 2005; 175: 8200–8208. [DOI] [PubMed] [Google Scholar]
- Tu S, Bhagat G, Cui G, Takaishi S, Kurt-Jones EA, Rickman B et al. Overexpression of interleukin-1beta induces gastric inflammation and cancer and mobilizes myeloid-derived suppressor cells in mice. Cancer Cell 2008; 14: 408–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katoh H, Wang D, Daikoku T, Sun H, Dey SK, Dubois RN. CXCR2-expressing myeloid-derived suppressor cells are essential to promote colitis-associated tumorigenesis. Cancer Cell 2013; 24: 631–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang B, Pan PY, Li Q, Sato AI, Levy DE, Bromberg J et al. Gr-1+CD115+ immature myeloid suppressor cells mediate the development of tumor-induced T regulatory cells and T-cell anergy in tumor-bearing host. Cancer Res 2006; 66: 1123–1131. [DOI] [PubMed] [Google Scholar]
- Serafini P, Mgebroff S, Noonan K, Borrello I. Myeloid-derived suppressor cells promote cross-tolerance in B-cell lymphoma by expanding regulatory T cells. Cancer Res 2008; 68: 5439–5449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudo-Saito C, Shirako H, Takeuchi T, Kawakami Y. Cancer metastasis is accelerated through immunosuppression during Snail-induced EMT of cancer cells. Cancer Cell 2009; 15: 195–206. [DOI] [PubMed] [Google Scholar]
- Ozdemir BC, Pentcheva-Hoang T, Carstens JL, Zheng X, Wu CC, Simpson TR et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell 2014; 25: 719–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang P, Li QJ, Feng Y, Zhang Y, Markowitz GJ, Ning S et al. TGF-beta-miR-34a-CCL22 signaling-induced Treg cell recruitment promotes venous metastases of HBV-positive hepatocellular carcinoma. Cancer Cell 2012; 22: 291–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garin MI, Chu CC, Golshayan D, Cernuda-Morollon E, Wait R, Lechler RI. Galectin-1: a key effector of regulation mediated by CD4+CD25+ T cells. Blood 2007; 109: 2058–2065. [DOI] [PubMed] [Google Scholar]
- Toscano MA, Bianco GA, Ilarregui JM, Croci DO, Correale J, Hernandez JD et al. Differential glycosylation of TH1, TH2 and TH-17 effector cells selectively regulates susceptibility to cell death. Nat Immunol 2007; 8: 825–834. [DOI] [PubMed] [Google Scholar]
- Muthuswamy R, Urban J, Lee JJ, Reinhart TA, Bartlett D, Kalinski P. Ability of mature dendritic cells to interact with regulatory T cells is imprinted during maturation. Cancer Res 2008; 68: 5972–5978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutkowski MR, Stephen TL, Svoronos N, Allegrezza MJ, Tesone AJ, Perales-Puchalt A et al. Microbially driven TLR5-dependent signaling governs distal malignant progression through tumor-promoting inflammation. Cancer Cell 2015; 27: 27–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinstein N, Alvarez M, Zwirner NW, Toscano MA, Ilarregui JM, Bravo A et al. Targeted inhibition of galectin-1 gene expression in tumor cells results in heightened T cell-mediated rejection; a potential mechanism of tumor-immune privilege. Cancer Cell 2004; 5: 241–251. [DOI] [PubMed] [Google Scholar]
- Bald T, Quast T, Landsberg J, Rogava M, Glodde N, Lopez-Ramos D et al. Ultraviolet-radiation-induced inflammation promotes angiotropism and metastasis in melanoma. Nature 2014; 507: 109–113. [DOI] [PubMed] [Google Scholar]
- Lotze MT, Tracey KJ. High-mobility group box 1 protein (HMGB1): nuclear weapon in the immune arsenal. Nat Rev Immunol 2005; 5: 331–342. [DOI] [PubMed] [Google Scholar]
- Ardi VC, Kupriyanova TA, Deryugina EI, Quigley JP. Human neutrophils uniquely release TIMP-free MMP-9 to provide a potent catalytic stimulator of angiogenesis. Proc Natl Acad Sci USA 2007; 104: 20262–20267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nozawa H, Chiu C, Hanahan D. Infiltrating neutrophils mediate the initial angiogenic switch in a mouse model of multistage carcinogenesis. Proc Natl Acad Sci USA 2006; 103: 12493–12498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Q, Zhao YJ, Wang XY, Qiu SJ, Shi YH, Sun J et al. CXCR6 upregulation contributes to a proinflammatory tumor microenvironment that drives metastasis and poor patient outcomes in hepatocellular carcinoma. Cancer Res 2012; 72: 3546–3556. [DOI] [PubMed] [Google Scholar]
- Jablonska J, Leschner S, Westphal K, Lienenklaus S, Weiss S. Neutrophils responsive to endogenous IFN-beta regulate tumor angiogenesis and growth in a mouse tumor model. J Clin Invest 2010; 120: 1151–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spicer JD, McDonald B, Cools-Lartigue JJ, Chow SC, Giannias B, Kubes P et al. Neutrophils promote liver metastasis via Mac-1-mediated interactions with circulating tumor cells. Cancer Res 2012; 72: 3919–3927. [DOI] [PubMed] [Google Scholar]
- Huh SJ, Liang S, Sharma A, Dong C, Robertson GP. Transiently entrapped circulating tumor cells interact with neutrophils to facilitate lung metastasis development. Cancer Res 2010; 70: 6071–6082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cools-Lartigue J, Spicer J, McDonald B, Gowing S, Chow S, Giannias B et al. Neutrophil extracellular traps sequester circulating tumor cells and promote metastasis. J Clin Invest 2013; 123: 3446–3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol 2011; 11: 519–531. [DOI] [PubMed] [Google Scholar]
- Lopez-Lago MA, Posner S, Thodima VJ, Molina AM, Motzer RJ, Chaganti RS. Neutrophil chemokines secreted by tumor cells mount a lung antimetastatic response during renal cell carcinoma progression. Oncogene 2013; 32: 1752–1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granot Z, Henke E, Comen EA, King TA, Norton L, Benezra R. Tumor entrained neutrophils inhibit seeding in the premetastatic lung. Cancer Cell 2011; 20: 300–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantovani A, Sozzani S, Locati M, Allavena P, Sica A. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol 2002; 23: 549–555. [DOI] [PubMed] [Google Scholar]
- Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L et al. Polarization of tumor-associated neutrophil phenotype by TGF-beta: "N1" versus "N2" TAN. Cancer Cell 2009; 16: 183–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H, Pardoll D, Jove R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat Rev Cancer 2009; 9: 798–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pikarsky E, Porat RM, Stein I, Abramovitch R, Amit S, Kasem S et al. NF-kappaB functions as a tumour promoter in inflammation-associated cancer. Nature 2004; 431: 461–466. [DOI] [PubMed] [Google Scholar]
- Bollrath J, Phesse TJ, von Burstin VA, Putoczki T, Bennecke M, Bateman T et al. gp130-mediated Stat3 activation in enterocytes regulates cell survival and cell-cycle progression during colitis-associated tumorigenesis. Cancer Cell 2009; 15: 91–102. [DOI] [PubMed] [Google Scholar]
- Grivennikov S, Karin E, Terzic J, Mucida D, Yu GY, Vallabhapurapu S et al. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell 2009; 15: 103–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortylewski M, Kujawski M, Wang T, Wei S, Zhang S, Pilon-Thomas S et al. Inhibiting Stat3 signaling in the hematopoietic system elicits multicomponent antitumor immunity. Nat Med 2005; 11: 1314–1321. [DOI] [PubMed] [Google Scholar]
- Yu H, Kortylewski M, Pardoll D. Crosstalk between cancer and immune cells: role of STAT3 in the tumour microenvironment. Nat Rev Immunol 2007; 7: 41–51. [DOI] [PubMed] [Google Scholar]
- Rebouissou S, Amessou M, Couchy G, Poussin K, Imbeaud S, Pilati C et al. Frequent in-frame somatic deletions activate gp130 in inflammatory hepatocellular tumours. Nature 2009; 457: 200–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greten FR, Eckmann L, Greten TF, Park JM, Li ZW, Egan LJ et al. IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell 2004; 118: 285–296. [DOI] [PubMed] [Google Scholar]
- Tordella L, Koch S, Salter V, Pagotto A, Doondeea JB, Feller SM et al. ASPP2 suppresses squamous cell carcinoma via RelA/p65-mediated repression of p63. Proc Natl Acad Sci USA 2013; 110: 17969–17974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortylewski M, Xin H, Kujawski M, Lee H, Liu Y, Harris T et al. Regulation of the IL-23 and IL-12 balance by Stat3 signaling in the tumor microenvironment. Cancer Cell 2009; 15: 114–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kujawski M, Kortylewski M, Lee H, Herrmann A, Kay H, Yu H. Stat3 mediates myeloid cell-dependent tumor angiogenesis in mice. J Clin Invest 2008; 118: 3367–3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan YY, Flavell RA. Regulatory T-cell functions are subverted and converted owing to attenuated Foxp3 expression. Nature 2007; 445: 766–770. [DOI] [PubMed] [Google Scholar]
- Lee H, Herrmann A, Deng JH, Kujawski M, Niu G, Li Z et al. Persistently activated Stat3 maintains constitutive NF-kappaB activity in tumors. Cancer Cell 2009; 15: 283–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Deng J, Kujawski M, Yang C, Liu Y, Herrmann A et al. STAT3-induced S1PR1 expression is crucial for persistent STAT3 activation in tumors. Nat Med 2010; 16: 1421–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Deng J, Xin H, Liu Y, Pardoll D, Yu H. A requirement of STAT3 DNA binding precludes Th-1 immunostimulatory gene expression by NF-kappaB in tumors. Cancer Res 2011; 71: 3772–3780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwitalla S, Ziegler PK, Horst D, Becker V, Kerle I, Begus-Nahrmann Y et al. Loss of p53 in enterocytes generates an inflammatory microenvironment enabling invasion and lymph node metastasis of carcinogen-induced colorectal tumors. Cancer Cell 2013; 23: 93–106. [DOI] [PubMed] [Google Scholar]
- Li CW, Xia W, Huo L, Lim SO, Wu Y, Hsu JL et al. Epithelial-mesenchymal transition induced by TNF-alpha requires NF-kappaB-mediated transcriptional upregulation of Twist1. Cancer Res 2012; 72: 1290–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anson M, Crain-Denoyelle AM, Baud V, Chereau F, Gougelet A, Terris B et al. Oncogenic beta-catenin triggers an inflammatory response that determines the aggressiveness of hepatocellular carcinoma in mice. J Clin Invest 2012; 122: 586–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng J, Liu Y, Lee H, Herrmann A, Zhang W, Zhang C et al. S1PR1-STAT3 signaling is crucial for myeloid cell colonization at future metastatic sites. Cancer Cell 2012; 21: 642–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesina M, Kurkowski MU, Ludes K, Rose-John S, Treiber M, Kloppel G et al. Stat3/Socs3 activation by IL-6 transsignaling promotes progression of pancreatic intraepithelial neoplasia and development of pancreatic cancer. Cancer Cell 2011; 19: 456–469. [DOI] [PubMed] [Google Scholar]
- Liang J, Nagahashi M, Kim EY, Harikumar KB, Yamada A, Huang WC et al. Sphingosine-1-phosphate links persistent STAT3 activation, chronic intestinal inflammation, and development of colitis-associated cancer. Cancer Cell 2013; 23: 107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H, Lee H, Herrmann A, Buettner R, Jove R. Revisiting STAT3 signalling in cancer: new and unexpected biological functions. Nat Rev Cancer 2014; 14: 736–746. [DOI] [PubMed] [Google Scholar]
- Soki FN, Koh AJ, Jones JD, Kim YW, Dai J, Keller ET et al. Polarization of prostate cancer-associated macrophages is induced by milk fat globule-EGF factor 8 (MFG-E8)-mediated efferocytosis. J Biol Chem 2014; 289: 24560–24572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory CD, Pound JD. Cell death in the neighbourhood: direct microenvironmental effects of apoptosis in normal and neoplastic tissues. J Pathol 2011; 223: 177–194. [DOI] [PubMed] [Google Scholar]
- Ammirante M, Luo JL, Grivennikov S, Nedospasov S, Karin M. B-cell-derived lymphotoxin promotes castration-resistant prostate cancer. Nature 2010; 464: 302–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo JL, Tan W, Ricono JM, Korchynskyi O, Zhang M, Gonias SL et al. Nuclear cytokine-activated IKKalpha controls prostate cancer metastasis by repressing Maspin. Nature 2007; 446: 690–694. [DOI] [PubMed] [Google Scholar]
- Tan W, Zhang W, Strasner A, Grivennikov S, Cheng JQ, Hoffman RM et al. Tumour-infiltrating regulatory T cells stimulate mammary cancer metastasis through RANKL-RANK signalling. Nature 2011; 470: 548–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caronni N, Savino B, Bonecchi R. Myeloid cells in cancer-related inflammation. Immunobiology 2014; 220: 249–253. [DOI] [PubMed] [Google Scholar]
- Joyce JA, Pollard JW. Microenvironmental regulation of metastasis. Nat Rev Cancer 2009; 9: 239–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motz GT, Coukos G. The parallel lives of angiogenesis and immunosuppression: cancer and other tales. Nat Rev Immunol 2011; 11: 702–711. [DOI] [PubMed] [Google Scholar]
- Murdoch C, Muthana M, Coffelt SB, Lewis CE. The role of myeloid cells in the promotion of tumour angiogenesis. Nat Rev Cancer 2008; 8: 618–631. [DOI] [PubMed] [Google Scholar]
- Schmid MC, Avraamides CJ, Dippold HC, Franco I, Foubert P, Ellies LG et al. Receptor tyrosine kinases and TLR/IL1Rs unexpectedly activate myeloid cell PI3kgamma, a single convergent point promoting tumor inflammation and progression. Cancer Cell 2011; 19: 715–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roodman GD. Mechanisms of bone metastasis. N Engl J Med 2004; 350: 1655–1664. [DOI] [PubMed] [Google Scholar]
- Lu X, Mu E, Wei Y, Riethdorf S, Yang Q, Yuan M et al. VCAM-1 promotes osteolytic expansion of indolent bone micrometastasis of breast cancer by engaging alpha4beta1-positive osteoclast progenitors. Cancer Cell 2011; 20: 701–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen DX, Bos PD, Massague J. Metastasis: from dissemination to organ-specific colonization. Nat Rev Cancer 2009; 9: 274–284. [DOI] [PubMed] [Google Scholar]
- Papayannopoulou T, Priestley GV, Nakamoto B, Zafiropoulos V, Scott LM. Molecular pathways in bone marrow homing: dominant role of alpha(4)beta(1) over beta(2)-integrins and selectins. Blood 2001; 98: 2403–2411. [DOI] [PubMed] [Google Scholar]
- Dinarello CA. Why not treat human cancer with interleukin-1 blockade? Cancer Metastasis Rev 2010; 29: 317–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q, Zhang XH, Massague J. Macrophage binding to receptor VCAM-1 transmits survival signals in breast cancer cells that invade the lungs. Cancer Cell 2011; 20: 538–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang AC, Massague J. Molecular basis of metastasis. N Engl J Med 2008; 359: 2814–2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weilbaecher KN, Guise TA, McCauley LK. Cancer to bone: a fatal attraction. Nat Rev Cancer 2011; 11: 411–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier PG, Chirgwin JM, Guise TA. New insights into the role of T cells in the vicious cycle of bone metastases. Curr Opin Rheumatol 2006; 18: 396–404. [DOI] [PubMed] [Google Scholar]
- Kikuta J, Wada Y, Kowada T, Wang Z, Sun-Wada GH, Nishiyama I et al. Dynamic visualization of RANKL and Th17-mediated osteoclast function. J Clin Invest 2013; 123: 866–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature 2003; 423: 337–342. [DOI] [PubMed] [Google Scholar]
- Chen W, Foo SS, Rulli NE, Taylor A, Sheng KC, Herrero LJ et al. Arthritogenic alphaviral infection perturbs osteoblast function and triggers pathologic bone loss. Proc Natl Acad Sci USA 2014; 111: 6040–6045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam J, Takeshita S, Barker JE, Kanagawa O, Ross FP, Teitelbaum SL. TNF-alpha induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. J Clin Invest 2000; 106: 1481–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei S, Kitaura H, Zhou P, Ross FP, Teitelbaum SL. IL-1 mediates TNF-induced osteoclastogenesis. J Clin Invest 2005; 115: 282–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, Jin W, Hardegen N, Lei KJ, Li L, Marinos N et al. Conversion of peripheral CD4+CD25- naive T cells to CD4+CD25+ regulatory T cells by TGF-beta induction of transcription factor Foxp3. J Exp Med 2003; 198: 1875–1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cher ML, Biliran HR Jr, Bhagat S, Meng Y, Che M, Lockett J et al. Maspin expression inhibits osteolysis, tumor growth, and angiogenesis in a model of prostate cancer bone metastasis. Proc Natl Acad Sci USA 2003; 100: 7847–7852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park BK, Zhang H, Zeng Q, Dai J, Keller ET, Giordano T et al. NF-kappaB in breast cancer cells promotes osteolytic bone metastasis by inducing osteoclastogenesis via GM-CSF. Nat Med 2007; 13: 62–69. [DOI] [PubMed] [Google Scholar]
- Jones DH, Nakashima T, Sanchez OH, Kozieradzki I, Komarova SV, Sarosi I et al. Regulation of cancer cell migration and bone metastasis by RANKL. Nature 2006; 440: 692–696. [DOI] [PubMed] [Google Scholar]
- Hsu YL, Hou MF, Kuo PL, Huang YF, Tsai EM. Breast tumor-associated osteoblast-derived CXCL5 increases cancer progression by ERK/MSK1/Elk-1/snail signaling pathway. Oncogene 2013; 32: 4436–4447. [DOI] [PubMed] [Google Scholar]
- Sethi N, Dai X, Winter CG, Kang Y. Tumor-derived JAGGED1 promotes osteolytic bone metastasis of breast cancer by engaging notch signaling in bone cells. Cancer Cell 2011; 19: 192–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinder M, Chislock E, Bussard KM, Shuman L, Mastro AM. Metastatic breast cancer induces an osteoblast inflammatory response. Exp Cell Res 2008; 314: 173–183. [DOI] [PubMed] [Google Scholar]
- Cho SW, Pirih FQ, Koh AJ, Michalski M, Eber MR, Ritchie K et al. The soluble interleukin-6 receptor is a mediator of hematopoietic and skeletal actions of parathyroid hormone. J Biol Chem 2013; 288: 6814–6825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Loberg R, Liao J, Ying C, Snyder LA, Pienta KJ et al. A destructive cascade mediated by CCL2 facilitates prostate cancer growth in bone. Cancer Res 2009; 69: 1685–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EM, Horowitz MC, Lavish SA. Stimulation by parathyroid hormone of interleukin-6 and leukemia inhibitory factor expression in osteoblasts is an immediate-early gene response induced by cAMP signal transduction. J Biol Chem 1996; 271: 10984–10989. [DOI] [PubMed] [Google Scholar]
- Park SI, Lee C, Sadler WD, Koh AJ, Jones J, Seo JW et al. Parathyroid hormone-related protein drives a CD11b+Gr1+ cell-mediated positive feedback loop to support prostate cancer growth. Cancer Res 2013; 73: 6574–6583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park SI, Liao J, Berry JE, Li X, Koh AJ, Michalski ME et al. Cyclophosphamide creates a receptive microenvironment for prostate cancer skeletal metastasis. Cancer Res 2012; 72: 2522–2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauner M, Stein N, Winzer M, Goettsch C, Zwerina J, Schett G et al. WNT5A is induced by inflammatory mediators in bone marrow stromal cells and regulates cytokine and chemokine production. J Bone Miner Res 2012; 27: 575–585. [DOI] [PubMed] [Google Scholar]
- Ancrile B, Lim KH, Counter CM. Oncogenic Ras-induced secretion of IL6 is required for tumorigenesis. Genes Dev 2007; 21: 1714–1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dankbar B, Padro T, Leo R, Feldmann B, Kropff M, Mesters RM et al. Vascular endothelial growth factor and interleukin-6 in paracrine tumor-stromal cell interactions in multiple myeloma. Blood 2000; 95: 2630–2636. [PubMed] [Google Scholar]
- Lee HJ, Zhuang G, Cao Y, Du P, Kim HJ, Settleman J. Drug resistance via feedback activation of Stat3 in oncogene-addicted cancer cells. Cancer Cell 2014; 26: 207–221. [DOI] [PubMed] [Google Scholar]
- Roca H, Varsos Z, Pienta KJ. CCL2 protects prostate cancer PC3 cells from autophagic death via phosphatidylinositol 3-kinase/AKT-dependent survivin up-regulation. J Biol Chem 2008; 283: 25057–25073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valencia T, Kim JY, Abu-Baker S, Moscat-Pardos J, Ahn CS, Reina-Campos M et al. Metabolic reprogramming of stromal fibroblasts through p62-mTORC1 signaling promotes inflammation and tumorigenesis. Cancer Cell 2014; 26: 121–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voronov E, Shouval DS, Krelin Y, Cagnano E, Benharroch D, Iwakura Y et al. IL-1 is required for tumor invasiveness and angiogenesis. Proc Natl Acad Sci USA 2003; 100: 2645–2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, Russell MR, Shahriari K, Jernigan DL, Lioni MI, Garcia FU et al. Interleukin-1beta promotes skeletal colonization and progression of metastatic prostate cancer cells with neuroendocrine features. Cancer Res 2013; 73: 3297–3305. [DOI] [PubMed] [Google Scholar]
- Balkwill F, Mantovani A. Cancer and inflammation: implications for pharmacology and therapeutics. Clin Pharmacol Ther 2010; 87: 401–406. [DOI] [PubMed] [Google Scholar]
- Germano G, Frapolli R, Belgiovine C, Anselmo A, Pesce S, Liguori M et al. Role of macrophage targeting in the antitumor activity of trabectedin. Cancer Cell 2013; 23: 249–262. [DOI] [PubMed] [Google Scholar]
- Germano G, Mantovani A, Allavena P. Targeting of the innate immunity/inflammation as complementary anti-tumor therapies. Ann Med 2011; 43: 581–593. [DOI] [PubMed] [Google Scholar]
- Srivastava K, Hu J, Korn C, Savant S, Teichert M, Kapel SS et al. Postsurgical adjuvant tumor therapy by combining anti-angiopoietin-2 and metronomic chemotherapy limits metastatic growth. Cancer Cell 2014; 26: 880–895. [DOI] [PubMed] [Google Scholar]
- Zhang G, Panigrahy D, Hwang SH, Yang J, Mahakian LM, Wettersten HI et al. Dual inhibition of cyclooxygenase-2 and soluble epoxide hydrolase synergistically suppresses primary tumor growth and metastasis. Proc Natl Acad Sci USA 2014; 111: 11127–11132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klug F, Prakash H, Huber PE, Seibel T, Bender N, Halama N et al. Low-dose irradiation programs macrophage differentiation to an iNOS(+)/M1 phenotype that orchestrates effective T cell immunotherapy. Cancer Cell 2013; 24: 589–602. [DOI] [PubMed] [Google Scholar]
- Rolny C, Mazzone M, Tugues S, Laoui D, Johansson I, Coulon C et al. HRG inhibits tumor growth and metastasis by inducing macrophage polarization and vessel normalization through downregulation of PlGF. Cancer Cell 2011; 19: 31–44. [DOI] [PubMed] [Google Scholar]