Abstract
Background:
Eating disorder is one of the most common health problems with clinical and psychological consequences, which can affect body image in cancer patients. Similar studies in this area for checking the status of this disorder and its relevance with body image in patients with cancer are limited. Therefore, this study was designed with the aim of determination of eating disorders in patients with cancer and their relevance with body image.
Materials and Methods:
The research was a cross-correlation study. It was carried out in Sayed-Al-Shohada Hospital affiliated to the Isfahan University of Medical Sciences in 2013. Two hundred and ten patients with cancer were selected and were asked tocomplete the demographic and disease characteristics questionnaire, the Multidimensional Body-Self Relations Questionnaire (MBSRQ), and eating disorders questionnaire. SPSS statistical software, version 14 was used for statistical analysis’-Test, analysis of variance (ANOVA), and Pearson correlation coefficient were used for analyzing the obtained data.
Results:
The mean values of age, body mass index (BMI), and duration of illness were 48.2 ± 13.20 years, 24.6 ± 4.6kg/m2, and 25.64 ± 21.24months, respectively. Most patients were married (87%), without university education (96%), unemployed (67%), and with incomes below their requirement (52%). Most patients were diagnosed with breast cancer (36.5%). They received chemotherapy as the main treatment (56.2%). In addition, mean ± SD of eating disorders and body image were 12.84 ± 4.7 and184.40 ± 43.68, respectively. Also, 49.7% of patients with cancer had an eating disorder. Among these, 29% had experiences of anorexia and 20.7% had bulimia. There was a significant negative correlation between the score of body image and eating disorders (r = −0.47, P = 0.01).
Conclusions:
Findings of this study showed that most patients with cancer had experienced symptoms of eating disorders. This may lead to a negative impact on the body image in these patients and may be the cause of further psychological and physical changes in these patients. The findings of this study can assist the healthcare team to pay more attention to eating disorders and body image in patients with cancer and also in considering the relationship of these issues in their evaluations.
Keywords: Body image, cancer, eating disorder, Iran, nursing
INTRODUCTION
Cancer influences all dimensions of a patient's life including physical, emotional, and psychological aspects.[1] Among the most common these impacts, changes in weight, appetite, and eating disorders (EDs) are caused in these patients due to various reasons, with significant negative physical and emotional consequences for patients and their families.[2] People with EDspay too much attention to the food and even the shape and weight of their body. Among the most important types of these disorders, anorexia and bulimia belong to the fourth category of mental disorders.[3] EDs are serious public health problems; however, patient with chronic diseases are more likely to exhibit two or more disturbed eating behaviors than their peers without chronic diseases. In other words, people with chronic diseases are 2.4 times more at the risk of EDs and 1.9 times more at the risk of ED subgroups compared with those without the disease.[4]
Statistics show that more than 50% of those individuals with cancer experience some degree of change in their eating behaviors during the disease period.[5] These statistics indicate a frequent occurrence of EDs in patients with cancer at different stages of the disease.[6] In these patients, the occurrence of some specific situations such as overemphasis on food, special dietary patterns, periods of increasing and decreasing weight and the subsequent consequences, usage of restrictive diets, and existence of some of restrictions can create the context for the onset and progression of EDs.[4]
On the other hand, it should be noted that in many cases, EDs’ symptoms are associated with psychological problems including the patient's own body image.[7] Meanwhile, most physicians and healthcare teams carry out inappropriate assessments and interventions including using various drugs, in order to improve the eating habits and weight of patients. They are unaware that in most cases, changes in appetite and eating status of patients have psychological basis.[8] In fact, people with EDs demonstrate behaviors caused due to misunderstanding of the shape and weight of their body.[9] Therefore, many people who suffer from these disorders may have low self-esteem and preoccupation about their appearance.[10] Some studies have shown that people with EDs suffer more from feelings like depression, loneliness, isolation, low self-esteem, and obsession about weight loss.[7]
Nevertheless, no study could be found that focused on the type and intensity of the relationship between EDsandbody image in cancer patients in Iran. A review of the studies in this regard showed that these studies have only been conducted in healthy people with conflicting results. Among these studies, the study results of Asgari and colleagues on women in Ahwaz can be mentioned. In this study, there was a significant negative relationship between the body image and EDs (r= −0.2, P = 0.008). In other words, improving body image will reduce EDs.[11] The results of Shamsedin Saeid (2010) on girls of Kerman were also consistent in this regard. Comparison of body image scores and EDs in samples demonstrated that people with EDs had a lower score of body image compared with those without EDs. In addition, on comparing the body image scores, the difference was significant based on the subgroups of EDs, and those with anorexia (47.04 ± 11.07 vs 64.3 ± 16.4) had lower scores of body image compared to those without EDs.[12] In the study of Brannan, which was performed in USA on 847 academic women with a mean age of 20 years, there was a significant correlation between the dissatisfaction of body image and bulimia.[13] However, in the study of Safavi and colleagues on Tehran girls, even with a high sample size (400 subjects), there was no such a relationship found between the body image and EDs.[7]
Therefore, there were a few studies in the field of ED as a mental–social–biological illness in cancer patients and, on the other hand, inconsistency regarding the relationship of this disorder with body image in non-patients. Cancer can possibly influence the type and severity of communication, EDs, and body image ina different way, compared to non-patients. Therefore, the researchers decided to conduct a study with the purpose of considering ED and its relationship with body image in patients with cancer who were admitted to the selected hospital that was affiliated to the Isfahan University of Medical Sciences in 2013.
MATERIALS AND METHODS
This research was a cross-sectional correlation study performed on 210 patients with cancer in 2013. Convenience sampling was performed on the patients with cancer admitted to Sayed-Al-Shohada Hospital affiliated to Isfahan University of Medical Sciences and Clinic of Imam Reza (AS). After obtaining approval for the research from the ethics committee of Isfahan University of Medical Sciences, initially, the researcher chose the eligible patients based on inclusion criteria. The purpose of conducting the research was explained for them. Subsequently, written informed consents were obtained from the participants.
The inclusion criteria were as follows: Age 18–65 years (age less than 18 years is the period of adolescence and it can be effective on the body image, and age above 65 years can change the body image due to reduction of physical and mental abilities), definitive diagnosis of cancer by the physician, not being at the end-stage of life based on physician's diagnosis and the documents available in their clinical files, having mental and physical ability to participate in the study, ability to read and write in Persian language, extending a minimum of 2 months from cancer diagnosis (due to mental stability and body image), ability to eat and drink, absence of any disability (amputation, deformity, paralyzed extremities, mastectomy), lack of any clinical situation effective on food intake and body image in the patient such as nausea and vomiting, followed by chemotherapy, diabetes, kidney disease, thyroid, Cushing's syndrome, lupus, etc. based on the history taken from the patient.
The tools used in this study included: A questionnaire of demographic and disease characteristics with 12 items [age, gender, weight, height, body mass index (BMI), level of education, marriage, occupation, income, type of cancer, type of treatment, and duration of illness] and Multidimensional Body-Self Relations Questionnaire (MBSRQ) in patients with cancer. These tools were completed by interviewing patients.
MBSRQ with 64 items was used as a specific tool for evaluation of body image in patients with cancer, with nine dimensions of appearance orientation, fitness orientation, health orientation, illness orientation, appearance evaluation, fitness evaluation, health evaluation, body areas satisfaction, and overweight preoccupation. Orientation subgroups are related to the importance of one's appearance, health, and fitness. However, subgroups of evaluation examine the individual feelings toward physical attractiveness, health, and fitness. Overweight preoccupation subgroup also assesses the person's anxiety about obesity, dieting, and dietary restrictions.
Each question was given options from one to five (1 = strongly agree and 5 = strongly disagree). The minimum score was 64 and the maximum score was 320 in this regard. Higher scores represented more satisfaction of body image. Mean scores were calculated in general and also separately for each of these areas of body image for better description. According to a similar study,[7] the scores of 250–320, 193–256, 129–192, and 64–128 from left to right for the body image were considered as without problem, with a little problem, moderate problem, and so much troubled, respectively.
Another tool used in the study was the ED symptoms questionnaire in patients with cancer, which was obtained through adopting the analysis of eating habitual questionnaire,[14] and Ahwaz EDs scale.[15] This questionnaire consisted of 31 items with true and false options. There were 22 items for assessment of anorexia symptoms and 9 items to assess the symptoms of bulimia. The minimum score was zero and the maximum score was 31. Higher scores indicated more associated symptoms in each dimension. The mean score of EDs was calculated in general and the scores of anorexia and bulimia separately.
The validity of the questionnaire of demographic and disease characteristics was determined using content validity. This tool was developed by studying recent books and articles in the field of research topic. Then, they were given to some experts and professors for evaluation. Validity of the MBSRQ was determined by content validity method in 2009 by Safavi and colleagues[7] and also in 2005 by Conboy Croff[16] in cancer patients. Validity of the questionnaire of EDs in patients with cancer was determined by content validity. In order to determine the validity, the mentioned questionnaire was provided to 10 faculty members of the Isfahan University of Medical Sciences (from different faculties of nutrition, nursing, and biostatistics). After considering the necessary suggestions and improvements, the final tool was confirmed for use in the field of ED in cancer patients.
The reliability of MBSRQ questionnaire was determined in 2005 by Conboy Croff in USA in patients with cancer by calculating Cronbach's alpha coefficient which was 0.96. The reliability of ED questionnaire was calculated in this study by test–retest method. Thus, initially, the researcher performed the test twice for 20 patients with cancer in 2 weeks interval. The reliability was obtained by calculating Pearson correlation coefficient which was 0.86.
Data were analyzed by using SPSS statistical software, version 14. For statistical analysis, descriptive statistics (absolute and relative frequency, mean and standard deviation) and inferential statistics [independent t-test, analysis of variance (ANOVA), and Pearson correlation coefficient] were used to investigate the relationship between gender, marital status, type of treatment, type of cancer, income, level of education, BMI, age, and duration of cancer with ED and body image score. P ≤ 0.05 was considered as statistically significant level.
RESULTS
The results showed that the mean and standard deviation of age, BMI, and disease duration were 48.2 (± 13.20) years, 24/.6(± 4.6) kg/m2, and 25.64 (± 21.24) months, respectively. Majority of the patients were married (87%), without university education (96%), unemployed (67%), and with income below requirement(52%). The highest percentage of patients (56.2%) had undergone chemotherapy and had been diagnosed with breast (36.5%) and gastrointestinal (28.1%) cancer.
In this study, the mean ± SD of overall score of ED and the anorexia and bulimia scores separately in patients with cancer were 12.87 ± 2.7, 3.62 ± 1.3, and 9.25 ± 1.4, respectively. The results showed that in total, 49.7% of patients suffered from ED. Out of this, 29% were suffering from the symptoms of anorexia and 20.7% from bulimia symptoms [Table 1].
Table 1.
Frequency distribution of subjects in terms of incidence of eating disorders and body image status
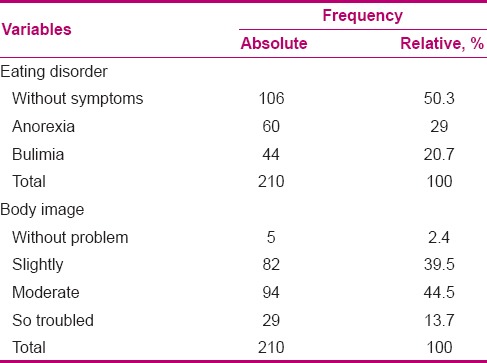
The mean and SD of body image score in cancer patients was 184.4 ± 43.68. 58.2% of the patients had from moderate to disproportionate number of problems in their body image [Table 1].
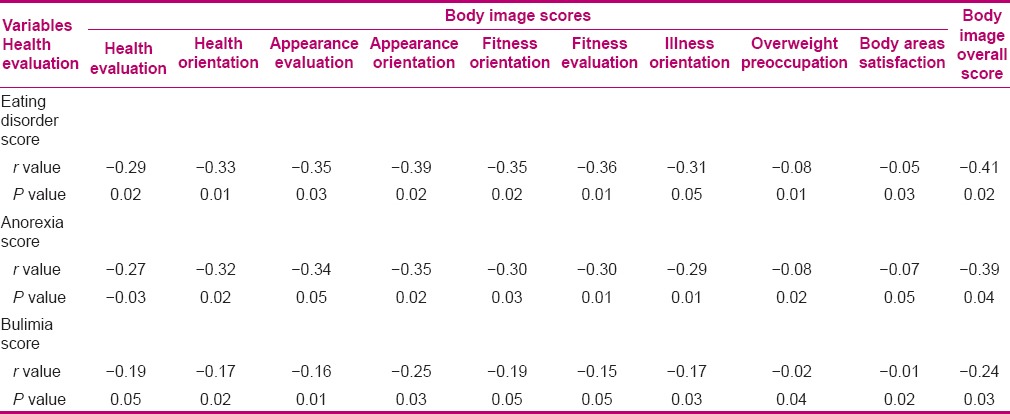
Pearson correlation coefficients between the mean overall score of body image and each of its dimensions are reported in Table 2, separately for ED, anorexia, and bulimia. The results showed that there was a statistically significant negative relationship between the overall score of body image and each dimension separately with ED (P ≤ 0.05). Among the dimensions of body image, the dimensions of appearance orientation (r= −0.39, −0.35, −0.25) and body areas satisfaction (r= −0.05, −0.07, −0.01) had the highest and lowest correlation, respectively, with the three variables of ED, anorexia, and bulimia [Table 2].
Table 2.
Relationship between overall mean score of body image and mean score of each dimension with the scores of eating disorder, anorexia, and bulimia in the cancer patients
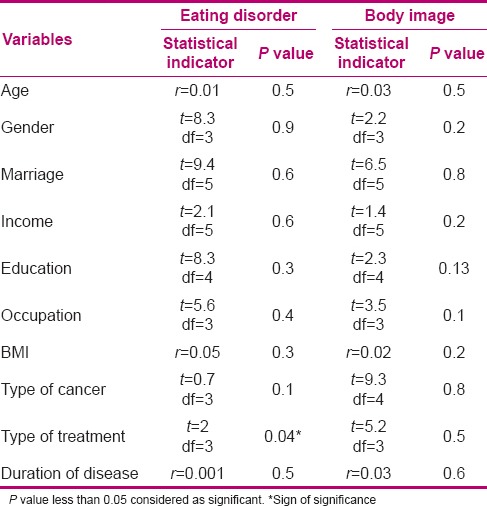
The results of the relationship between the mean score of ED and body image with demographic and disease variables are reported in Table 3. ANOVA test results showed that only the type of treatment had a significant relationship with ED. Thus, this disorder was lower in patients undergoing radiotherapy compared to patients on other treatments (P ≤ 0.05) [Table 3].
Table 3.
The relationship of eating disorder and body image with demographic and disease variables in the cancer patients
DISCUSSION
The present study is among the first researches which have been carried out in Iran for investigating ED in cancer patients and its relation to body image. In this study, 49.7% of the cancer patients had ED symptoms. Among these, 29.0% had experienced symptoms of anorexia and 20.7% had bulimia symptoms.
As previously mentioned, so far, no studies have been carried out investigating these disorders in patients with cancer in Iran. However, the results of studies in patients with other chronic diseases showed that the majority of these patients suffered from EDs. Thus, the incidence of EDs in people with type I diabetes determined by using ED questionnaires including questionnaire of Diagnostic Survey of Eating Disorder (DSED), Eating Disorder Inventory (EDI), and Eating Attitudes Test-26 (EAT-26) in John's study[17] and based on the 32-item Eating Disorder Examination Questionnaire (EDE-Q) in Markowitz's study[18] was 10% and 27.5%, respectively.
The causes of ED are multiple. In order to have a closer examination in this study, some of the possible reasons for ED were excluded from the study, including presence of any clinical conditions affecting eating such as nausea and vomiting after treatment, or gastrointestinal patients having undergone removal of stomach and intestines. Nevertheless, it should be noted that other reasons such as paying too much attention and caregivers of the patients insisting them to eat, and also, the impact of cultural and social factors are among the factors involved in the etiology of ED.[8] In addition, chronicity of the disease process, its diagnosis, and in some cases, the constraints faced by patients changed dietary habits in cancer patients. These causes provided the context for developing EDs in them.[19]
In the present study, among the demographic and disease characteristics, there was a significant relationship only between the types of treatment and ED. Mean score of ED in patients undergoing radiotherapy was lower compared to that in patients on other treatments. The possible reason of this issue could be less common complications of radiotherapy compared to other treatments. Considering that in this study, there was no possibility of locating the radiotherapy field. There is a need for further investigation in this areato find the relationship of radiation therapy field with ED.
Another finding of this study was that despite the fact that patients with any type of disability, such as amputation, deformity, paralyzed limbs, and mastectomy, were not allowed to enter the study, a high percentage of patients with cancer had body image from moderate to so much troubled (58.2%). In Peeters’ study,[20] 17% of patients with prostate cancer suffered from this disorder. In the study of Rhondali and colleagues,[21] it was reported that more than 50% of the patients with cancer had body image disorder.
In the present study, body image was assessed by a questionnaire that contained items such as fear of becoming dependent on others, loss of physical and mental strength, unknown future of disease, and also suffering from uncontrollable pain. Possible reasons for changing body image may be associated with these or ED. Body image disorder can be effective on treatment decisions. Therefore, according to the body image threatening changes in these individuals, healthcare workers should increase their understanding on factors relevant to body image in these patients.
In this study, demographic and disease factors associated with body image were examined. Finally, and contrary to our assumption, body image had no relationship with any of the demographic and disease characteristics in cancer patients. Harrington and Badger's study in patients with prostate cancer[22] and Erol et al.'s study[23] on women with breast cancer were also inline with the present study. Body image score had no relationship with age, level of education, occupation, income, and duration of treatment. However, in Holly et al.s[24] and Iradel's[25] studies on women with breast cancer, there was a significant negative correlation between demographic variables including age, gender, and marital status with body image. The reason of this difference in the results is due to this fact that in most of these studies, the samples were related to gender-related cancers. Gender-related cancer means more effectiveness of spouse on the body image.[22] However, this issue could be related to the limitation of samples in the present study. Therefore, it is necessary to perform further investigations on the relationship of these variables with body image in a study with a larger sample size.
Lack of relationship between clinical variables including duration of illness, type of treatment, and type of cancer with body image can be related to inclusion criteria Eligible patients for entry into the study should have had at least 2months passed from their illness. Therefore, it is likely that after this period, the patients had reached a minimum level of stability in body image and changes occurring after this period would be much less, or they had achieved compliance with the changes caused subsequent to disease and treatment. In this study, unlike the previous studies, patients with any disability (amputation, deformity, paralyzed limbs, limb amputation following illness and treatment) were not allowed to enter the study. Nevertheless, in this context, it is necessary to conduct further investigations.
This research evaluated the relationship of ED, anorexia, and bulimia with body image in cancer patients. Finally, it was found that body image had a significant negative correlation with all three conditions. Therefore, ED was decreased by improving body image. In this regard, the most significant relationshi p between the dimensions of body image were appearance orientation dimension, which is indicative of the imp ortance of appearance in these patients. In Christian's[26] and Peeters’[20] studies, it was reported that at the time of being threatened of body image, it is likely that people start using inappropriate ways of coping and are subsequently diagnosed with ED.
Finding the relationship of body image with EDs in patients with cancer is among the distinguishing characteristics of the present study from other studies. Because it is often believed that eating changes in these patients are entirely due to the disease process or treatment complications such as chemotherapy and radiotherapy.
Therefore, the findings of this study can help the healthcare providers and especially the nurses in the process of examining and caring of patients with a holistic perspective. During their assessments, they should ensure that on the one hand, they identify disorders of body image and ED symptoms in these patients, and on the other hand, reduce the levels of these two disorders to mitigate the consequences of physical and psychological damages in the patients and improve their quality of life.[21]
The results of this study should be considered along with its limitations. In this study, changes in body weight during illness have not been investigated due to administrative problems. This study only reviewed the symptoms of EDs in patients and it was not possible to check the status of ED based on patient weight throughout the study. Another limitation of this study was the attitude of family and friends toward nutrient intake and the history of their suffering to one of the types of EDs. In this study, due to the large number of questions, time constraints, and fatigue in patients, it was not possible to assess these variables. Therefore, it is recommended that the researchers, if possible, carry out research studies with the purpose of investigating other psychological factors associated with EDs in cancer patients.
Another limitation of this study was that different types of cancers have been treated by using different regimens. This may subsequently affect the status of eating, as due to the limited number of patients with cancer, it was not possible to examine this disorder only in one type of cancer, although the researcher tried as much as possible to control them with respect to some of the inclusion criteria (including any clinical condition affecting eating like vomiting after treatment and the ability to eat and drink). Despite the fact that the present study had a relatively acceptable sample size, it is suggested to repeat this research, particularly to find the relationship between demographic and disease variables with body image and disorders, with a larger sample size.
CONCLUSION
In general, according to the limited available knowledge associated with ED in cancer patients, the results of this study provide evidences about the status of this disorder symptoms and their relation to body image. By using the results of this study, the healthcare team will be able to gain a better understanding and more comprehensive knowledge of the status of ED and also the type and intensity of its relationship with body image disorder in these patients. They can consider these two disorders in their assessments.
In addition, identification and early interventions on EDs and related factors such as body image can prevent the progress of unsatisfactory and often severe symptoms of this disorder, in order to avoid creating situations with negative impact on the patient and even threatening the improvement of cancer. Meanwhile, nurses who spend most of their time with patients have been placed in an ideal position to manage the challenges ahead in cancer patients with changes in body image and ED. Nurses can improve their comprehension and understanding of these changes and the consequences that arise from them with effective and efficient treatment and care programs to take a step toward improving the body image and reducing the risk factors of ED in cancer patients. By considering different physio-psycho-social aspects of cancer patients, their quality of life might be improved.[27]
ACKNOWLEDGMENTS
This article was derived from a master thesis of Shahla Mohamadirizi with project number 392188 Isfahan University of Medical Sciences, Isfahan, Iran. We greatly appreciate the support and collaboration of University Research Deputy and also the sincere cooperation of patients in clinics and hospitals.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Bahrami M, Balouchestani E, Amini H, Eghbali M. Assessing the effect of two praying methods on the life quality of patients suffering from cancer hospitalized at Sayed-Al-Shohada Medical Center of Isfahan University of medical sciences. Iran J Nurs Midwifery Res. 2010;15(Suppl 1):296–301. [PMC free article] [PubMed] [Google Scholar]
- 2.Mc Clement S. Manitoba, Canada: University of Manitoba; 2001. Nutrition care in advanced cancer: The experience of patient families and health care providers. [Google Scholar]
- 3.Golden NH. Eating disorders in adolescence and their squeal. Best Pract Res Clin ObstetrGynaecol. 2003;17:57–73. doi: 10.1053/ybeog.2003.0344. [DOI] [PubMed] [Google Scholar]
- 4.Goebel-Fabbri AE. Disturbed eating behaviors and eating disorders in Type 1 Diabetes: Clinical signifycance and treatment recommendations. Curr Diab Rep. 2009;9:133–9. doi: 10.1007/s11892-009-0023-8. [DOI] [PubMed] [Google Scholar]
- 5.Neary NM, Small CJ, Wren AM, Lee JL, Druce MR, Palieri IC, et al. Increasing energy intake in cancer patients with impaired appetite: Acute, randomized, placebo-controlled trial. J Clin Endocrinol Metab. 2004;89:2832–6. doi: 10.1210/jc.2003-031768. [DOI] [PubMed] [Google Scholar]
- 6.Beagan BL, Chapman GE. Eating after breast cancer: Influences on women's actions. J Nutr Educ Behav. 2004;36:181–8. doi: 10.1016/s1499-4046(06)60232-7. [DOI] [PubMed] [Google Scholar]
- 7.Safavi M, Mahamoodi M, Roshandel A. Assessment of body image and its relationship with eating disorders among female students of Islamic Azad University Tehran center branch. Med Sci J Islamic Azad UnivTehran Med Branch. 2009;19:129–34. [Google Scholar]
- 8.Bernhardson B, Olson K, Baracos V, Wismer W. Reframing eating during chemotherapy in cancer patients with chemosensory alterations. Eur J Oncol Nurs. 2012;16:483–90. doi: 10.1016/j.ejon.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 9.Dalle Grave R. Eating disorders: Progress and challenges. Eur JInternMed. 2011;22:153–60. doi: 10.1016/j.ejim.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Túry F, Güleç H, Kohls E. Assessment methods for eating disorders and body image disorders. J Psychosom Res. 2010;69:601–61. doi: 10.1016/j.jpsychores.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 11.Asgari P, Pasha R, Aminiyan M. Relationship between emotion regulation, mental stresses and body image with eating disorders of women. AndishehVaRaftar. 2009;4:65–78. [Google Scholar]
- 12.ShamsaldinSaeed N, Aziz zadehForouzi M, Mohammad Alizadeh S, Haghdoost AA, Gharousi Relationship between body image and eating disorders. Iran J Nurs Res. 2010;4:33–43. [Google Scholar]
- 13.Brannan ME. Texas, USA: University of NorthTexas; 2010. The relationship between body dissatisfaction and eatingdisorder symptomatology: An examination of moderatingvariables. [Google Scholar]
- 14.Coker S, Roger D. The Construction and preliminary validation of a scale for measuring eating disorders. J Psycosom Res. 1990;34:223–31. doi: 10.1016/0022-3999(90)90056-a. [DOI] [PubMed] [Google Scholar]
- 15.Valizade A, Ariapooran S. Prevalence of Eating Disorders and their Role in Psychological Signs among Women with Sport Activities. J Med Facu Guilan Univ Med Sci. 2011;20:15–23. [Google Scholar]
- 16.Conboy Croff R. Philadelphia: DrexelUniversity; 2005. Development of a cancer specific body-image instrument. [Google Scholar]
- 17.Jones J. Canada: University of Toronto; 2000. Eating disorders in adolescent females with type 1 diabetes mellitus: A controlled three-site. [Google Scholar]
- 18.Markowitz JT. Pennsylvania, USA: DrexelUniversity; 2008. Body mass index and disordered eating in adolescent females with type 1 diabetes. [Google Scholar]
- 19.Shragge JE. Edmonton: Universityof Alberata; 2006. Shifting to conscious control-psychosocial and diatery management of anorexia by patients with advanced cancer. [DOI] [PubMed] [Google Scholar]
- 20.Peeters CA. Canada: University of Ottawa; 2009. Body image concerns in men with localized prostate cancer [PhD Dissertation] [Google Scholar]
- 21.Rhondali W, Chisholm GB, Daneshmand M, Allo J. Canada: University of Alberta; 2012. Association between body image dissatisfaction and weight loss among patients with advanced cancer and their caregivers: A preliminary report. [DOI] [PubMed] [Google Scholar]
- 22.Harrington JM, Badger TA. Body image and quality of life in men with prostate cancer. Cancer Nurs. 2009;32:E1–7. doi: 10.1097/NCC.0b013e3181982d18. [DOI] [PubMed] [Google Scholar]
- 23.Erol O, Can G, Aydıner A. Effects of alopecia on body image and quality of life of Turkish cancer women with or without head scarf. Support Care Cancer. 2012;20:2349–56. doi: 10.1007/s00520-011-1338-y. [DOI] [PubMed] [Google Scholar]
- 24.Iredale R, Brain K, Williams B, France E, Gray J. The experiences of men with breast cancer in the United Kingdom. Eur J Cancer. 2006;42:334–4. doi: 10.1016/j.ejca.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 25.Holly P, Kennedy P, Taylor A, Beedie A. Immediate breast reconstruction and psychological adjustment in women who have undergone surgery for breast cancer: A preliminary study. Psychol Health Med. 2003;4:441–52. doi: 10.1080/1354850310001604586. [DOI] [PubMed] [Google Scholar]
- 26.Falk Dahl CA, Reinertsen KV, Nesvold IL, Fosså SD, Dahl AA. A Study of Body Image in Long Term Breast Cancer Survivors. Cancer. 2010;13:3549–57. doi: 10.1002/cncr.25251. [DOI] [PubMed] [Google Scholar]
- 27.Bahrami M. Why differences exist? An interpretive approach to nurses’ perceptions of cancer patients’ quality of life. Iran J Nurs Midwifery Res. 2011;16:117–24. [PMC free article] [PubMed] [Google Scholar]


