Introduction
It is clear from the presentations at this symposium that Assisted Reproductive Technologies (ARTs) in nonhuman primates have made substantial progress since 1984, when the first reports appeared of successful births following in vitro fertilization (IVF) [1,2]. It can truly be said that nonhuman primate ARTs have "come of age" because these births occurred 21 years ago (Figure 1). Initial research efforts were almost entirely directed at establishing appropriate culture conditions for in vitro production (IVP) of monkey embryos, and subsequently at devising workable embryo transfer techniques. The latter efforts illustrate one of the significant differences between macaque and human IVP in its broadest sense (embryo production and births). Although several species of nonhuman primate have been used to study ARTs, the great majority of studies have been with the rhesus macaque, Macaca mulatta, because it is (or was) widely available and because of its general similarity to humans. However, with the heavy emphasis on the use of rhesus monkeys for AIDS-related research during the past ten years, limited availability of animals is restricting reproductive research efforts, almost to the point of blocking research in some cases.
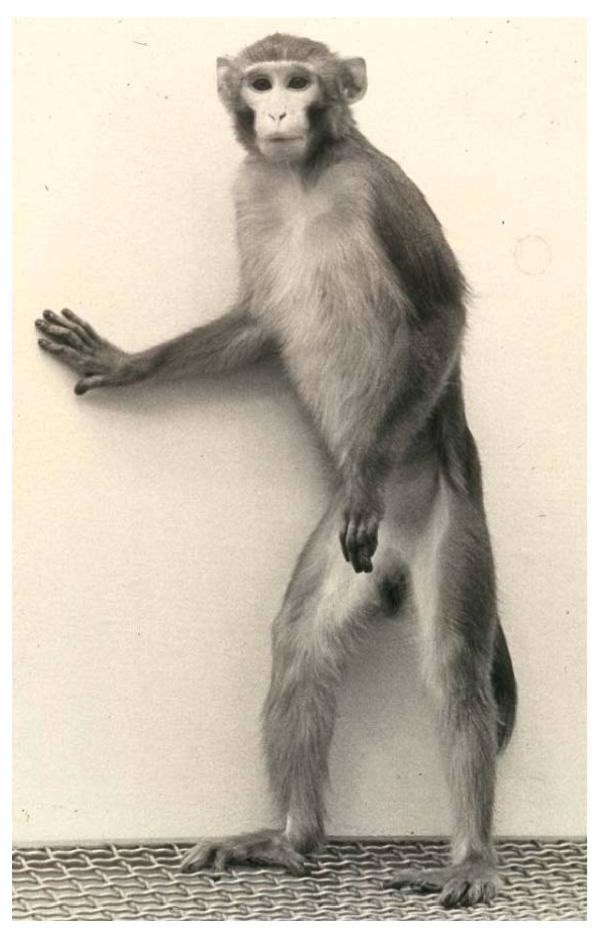
Figure 1.
"Petri," the first IVF macaque monkey, shown here at about 5 years of age. He has since fathered numerous normal offspring, showing that he is healthy and fertile.
Until recently, the primary rationale for ARTs research with nonhuman primates has been to provide information and new technologies that could assist human ARTs. Because basic research, and to some extent the development of new technologies, cannot or should not be done on humans, the nonhuman primate model ought to play a central role in these efforts. Paradoxically, this role to date has been minimal, for several reasons. First, human ART (IVF/IVP/ET) was established before ART in nonhuman primates. Human ART has been developing since 1969, when the first IVF was reported [3], culminating in the birth of Louise Brown in 1978, five years before the first nonhuman primate IVF births. Because of the social importance and commercialization of human ART, it has progressed much faster than nonhuman primate ART. This has made it difficult to present the case for nonhuman primate ART as a model for human ART, because the former is usually perceived as playing "catch-up" to the latter. Second, nonhuman primate ART presently owes more to human ART than vice-versa, e.g., the development and availability of human recombinant gonadotropins, without which monkey ART would be very difficult and perhaps prohibitively expensive. As a result, there has been very little technology transfer from basic research with nonhuman primates to the human clinical arena. Nevertheless, there are several key areas in which progress in human ART has virtually stalled, and quantum improvements in ART success will need new information and technology that can only be obtained using suitable experimental animal models, i.e., nonhuman primates. The efficiency of human ART is rather low – on average, about 12% per embryo transferred, and <5% per embryo produced [4,5]. Improvements could be made, for example, by devising even better culture media for IVP and objective methods for selecting the most viable embryos for transfer. Moreover, as this symposium demonstrates, there is great potential for nonhuman primate ART to make a major contribution to embryonic stem cell biology and technology, avoiding difficult ethical and logistical problems inherent in human ES cell studies and applications.
Because nonhuman primate ART is now well established, and most of the technical problems have been resolved, it is now timely to directly apply it to solving problems in human infertility and stem cell research. That is why this symposium is most opportune.
Gamete collection and processing
Methods for collecting semen from rhesus macaques are well established, and have been in use for the past 20 years at some of the National Primate Centers. The most common method involves penile electrical stimulation, which yields spermatozoa that are highly motile and capable of IVF. One disparity between macaque and human spermatozoa is that the former need chemical activators (caffeine and dbcAMP) to complete capacitation and support functional acrosome reactions, whereas human spermatozoa require no specific activators. The need for chemical stimulation of rhesus monkey spermatozoa allows the acquisition of fertilizing ability to be precisely controlled, which is useful for IVF and for basic research, but it also makes macaque spermatozoa less useful as a model for human spermatozoa.
Oocyte collection in nonhuman primates is obviously more labor-intensive than semen collection. Collection of oocytes is done routinely after ovarian stimulation, usually with human recombinant gonadotropins. Availability of these hormones has revolutionized nonhuman primate ART because each female can usually be stimulated four or five times before becoming refractory. Previously, when using natural hormones (e.g., human urinary FSH, human chorionic gonadotropin, equine chorionic gonadotropin) animals became refractory after only one cycle of stimulation [6], which meant that a fresh female had to be used for every cycle, and this made nonhuman primate ART prohibitively expensive. Most primate centers still use laparoscopic aspiration of stimulated follicles, which is quite effective, but it is a tedious procedure and sometimes follicles are difficult to access. A faster and more efficient route is by ultrasound-guided aspiration, as in women, but this requires a much higher level of skill by the operator. At present, it appears that only one primate center is using this procedure routinely, and its use should be adopted in other centers.
The term "controlled ovarian stimulation" was used by some investigators, but this raised the question: is it really controlled? The doses of gonadotropins, especially of FSH, given to rhesus monkeys are very high, about 2–10 times the dose administered to women on a body weight basis. The possibility that such high gonadotropin doses interfere with the proper development of follicles and oocytes needs investigation. It seems likely that some defective follicles and oocytes that may be destined for atresia are being recruited. The standard "one ampoule per day" regimen of FSH given to a monkey has not been adequately examined to find if lower doses might be effective. It is possible that lower doses might produce acceptable outcomes, perhaps with fewer oocytes having a higher overall quality.
Another important question is the number of cycles of ovarian stimulation allowed on each monkey, which is up to the IACUC at each primate center. There does not appear to be any objective rationale for the number(s) of stimulation cycles allowed. Some Animal Use Committees permit six or more cycles, while others are more conservative. It would be helpful if guidance could be obtained from NIH and/or USDA to determine what is a reasonable number of cycles per donor, and to standardize this across the primate centers. It does not appear that repeated ovarian stimulation with exogenous gonadotropins harms the females' fertility or capacity to bear offspring. Raising the number of cycles permitted could significantly reduce the numbers of animals needed for a research study, and thereby substantially lower the costs of nonhuman primate ART research.
Preservation of gametes
Protocols for cryopreserving macaque semen appear to be satisfactory insofar as they allow IVF to occur with frozen/thawed spermatozoa. Several methods are in use, including pelleting on dry ice and equilibrium freezing in straws [7]. However, there is clearly substantial individual donor variability. The old animal science adage that "some bulls [semen!] don't freeze" applies also to nonhuman primates, and perhaps to humans as well. This indicates that current methods for semen cryopreservation are suboptimal, and perhaps need to be customized so that semen from virtually any individual can be cryopreserved. The impact of genetic variation on sperm cryopreservability needs further investigation, from the perspectives of both basic science and practical applications of technology.
In contrast, current success with oocyte cryopreservation in primates (nonhuman and human) is poor. Much more work is needed on this topic. The metaphase spindle in primate oocytes is very sensitive to cooling, which causes spindle disassembly and chromosome dispersion [8,9]. There is an urgent need to devise efficient protocols for primate oocyte cryopreservation, because of its importance to ARTs in both nonhuman primates (breeding, gene banking, production of research materials) and in humans (PCOS patients, postponing childbearing, etc.). Such protocols can be developed empirically in human clinical laboratories but more basic science is needed to optimize these procedures, and here is a major opportunity for research efforts with nonhuman primates. As well as studying the effectiveness and reliability (preservation of viability) of oocyte cryopreservation protocols, the genetic consequences must also be examined. This will involve the production and destructive analysis of embryos from cryopreserved oocytes, so once again the nonhuman primate model is indicated.
In vitro fertilization and embryo production
Several of the National Primate Research Centers have established IVF programs in macaques, mostly using rhesus monkeys. Present technology for macaque IVF appears to be adequate, with rates of fertilization and subsequent embryo development, about the same as for human ART. However, production of cleavage stage embryos or blastocysts does not necessarily mean that they are all competent. Some of them are viable, as evidenced by births of offspring after transfer of IVF embryos. Several NPRCs reported ART success (production of live offspring) rates of up to 50%. However, as in human ART, this is accomplished by judicious selection of embryos for transfer. The overall ART process is inefficient, because many embryos stop developing during cleavage or especially at the morula-blastocyst transition. The reason for this is unknown, but either defective oocytes are responsible and/or present embryo culture media are suboptimal for supporting normal development. This situation mirrors that in human ART, where it is difficult to reconcile research on embryo development with the primary goal of achieving pregnancy in the patient. Thus, here there is a major opportunity for research in nonhuman primates to help improve human ART outcomes.
Embryo transfer
While the rhesus monkey in several ways is an excellent model for development of ARTs, it suffesr from the disadvantage that the tortuous cervical canal is hard to cannulate, making uterine embryo transfer difficult. As a result, in most studies involving embryo transfer, IVP embryos were inserted into the oviducts, either by a "mini-laparotomy" approach [10] or by laparoscopy [11]. Remarkably, blastocysts have been inserted into rhesus oviducts with production of live offspring [12], indicating that ectopic pregnancy in this species is not a concern and also that transportation of embryos into the uterus by this route is efficient and rapid. Moreover, this and similar studies show that the rhesus macaque is capable of carrying twins to term, unlike with natural breeding, and this offers some significant advantages for ARTs including the production of identical twins, which almost never occurs naturally. A major advantage with nonhuman primates is that embryo transfers are usually done using surrogate females, so adverse effects of ovarian stimulation on the recipient's endocrine status and uterine physiology, as documented in humans, e.g. [13], are avoided.
Because nonhuman primate ART is primarily a research area, there is much less emphasis on embryo transfers as the objective, just the opposite of the situation in humans. As a result, a total of only ~100 monkeys are reported to have been born by ART vs. >1 million humans worldwide.
Specialized models for disease research
A key goal that so far has been elusive is the production of identical macaque monkeys, which occurs naturally hardly ever, if at all. Availability of identical monkeys would help disease research and vaccine production efforts by allowing controls and treatments (e.g., infected animals) to be compared directly, avoiding the usual between-animal variations. Use of identical monkeys would reduce the numbers of animals normally required for a comparative research study, thus lowering the cost. Several approaches for making identical monkeys have been tried. Nuclear transfer using embryonic cells (blastomeres) is restricted because so few donor cells are available from each embryo. Somatic nuclear transfer (SCNT) seems unlikely to work routinely because in other animals large numbers of oocytes are required to overcome the low efficiency of SCNT and this is not an option in monkeys. Two potentially viable approaches are morula or blastocyst splitting, which has been moderately successful in domesticated animals, and blastomere disaggregation/reaggregation. A report at this symposium revealed an inherent flaw in the latter approach that will most likely preclude success. When pairs of identical rhesus monkey embryos were produced by blastomere disaggregation, the number of inner cell mass cells was halved. Although this number was probably still adequate for viability, production of identical twin offspring would require 100% survival following embryo transfer, which is unlikely to happen given present success rates. If instead of two, four identical embryos were produced by this technique, then only two of them need survive to term to produce identical offspring, but unfortunately the number of ICM cells in each blastocyst (1/4 normal) was most probably too low to develop into a viable fetus.
Instead of relying so heavily on the rhesus macaque for research into human infertility and disease, it was pointed out that some other nonhuman primates are also being used or should be developed as models for ART studies. While rhesus monkeys are good models for implantation and pregnancy immunology, embryological studies could also be done with other macaque species or with vervets (African green monkeys). Advantages of vervets are that they are relatively free of dangerous pathogens compared to rhesus monkeys, and less expensive. The baboon is excellent for studying normal physiology of pregnancy and disease (e.g., endometriosis). It would be useful to develop IVP protocols for this animal so that preimplantation events could also be examined. In any research study, the importance was emphasized of integrating cellular, endocrine and molecular approaches. It was also very clear from the symposium presentations that the great strength of using an experimental animal like a nonhuman primate is that it allows hypothesis testing, unlike most clinical ART studies in humans.
There is also considerable interest in creating transgenic nonhuman primate models for disease studies. This approach would allow creation of models with a specific disease, or amplification of existing models, e.g., nonhuman primates with Krabbé disease. Research could then identify genes responsible for the disease process, leading to better understanding of mechanisms, and possibly development of specific treatments. With respect to gene therapy, nonhuman primate research should play a critically important role before human clinical trials are undertaken. Nonhuman primate ARTs would play a key role in creation of such disease models, e.g., by transfection of embryos. However, several difficulties inherent with transgenic nonhuman primates were discussed. Because nonhuman primates are outbred, genetic variability will influence the effects of transgenes. This could be avoided by making identical animals, as described above. Also, it takes several years before macaques reach puberty, making it difficult to study an adult onset diseases. This drawback could be partly offset by targeting X chromosome genes. Particular problems in gene targeting have been encountered in nonhuman primates but creative solutions are being applied to overcome these. The potential importance of "knockout" rhesus monkeys was emphasized, as availability of such animals would help "level the playing field" with mouse genetic models.
I think it is important to recognize that, if ARTs are used to generate nonhuman primates with specific disease traits, then care of the resulting animals may become a pressing issue because they may need more medical attention, special housing, etc., than normal animals.
Contraceptive development
This area offers a major role for nonhuman primate ART, not only for assessing contraceptive effectiveness but also for establishing new approaches to contraception, by controlling the process of embryogenesis. It is also an area in which studies with non-primate species are much less likely to be useful or informative because of the wide differences in reproductive strategies (physiology and endocrinology) among mammals. Several research opportunities for nonhuman primates are presented: contraceptive research efforts could focus on spermatozoa, oocytes and fertilization, embryo development or attachment and implantation. The problem of human over-population, like that of infertility, is global but much more of a challenge because of the repercussions for the entire planet. The point was made that there is an urgent need for new contraceptive approaches, and it is clear that this is a vastly underemphasized problem. The case was also made that contraception research is likely to increase understanding of normal reproductive physiology and embryology in primates.
Embryonic stem cells in nonhuman primates
Monkey ES cells can provide huge opportunities for studying basic properties of these primordial cells, and for developing techniques for directing their differentiation. These efforts can be sustained without the controversy that surrounds use of human ES cells, which is restricting research progress. Several elegant presentations at this symposium described the remarkable progress being made with macaque ES cells. Diabetes was described as a "world wide epidemic" of increasing proportions. There is an urgent need to develop technology to replace the pancreatic beta cells that are defective or lost in diabetic patients. Using monkey ES cells as a model, it should be possible to derive beta cells from them in culture, both to understand the biology of these cells and to devise ways of creating new pancreatic endocrine tissue. The twin problems of ES cell technology were described: how to prevent their spontaneous differentiation in culture, and how to direct their terminal differentiation into specific phenotypes, such as functional neuronal cells. Mouse feeder cell layers have frequently been used to support ES cell cultures, which raises a concern about introducing viruses into the ES cell products.
One aspect of ES cell production and technology that appears to be in need of more attention is their cytogenetics. Human ES cell lines have been derived from IVP blastocysts that came from infertile patients and were rejected for embryo transfer. Moreover, it is well known that 50% or even more of IVP human embryos are aneuploid to some degree [14]. Aneuploidy frequencies in macaque blastocysts have hardly been examined, if at all. Therefore, there should be considerable concern about the normality of primate ES cells: if they are cytogenetically abnormal, then it is hardly likely that they will produce functionally normal organs and tissues. Appropriate markers also need to be identified to discriminate cells that are functionally competent from those that are not. The major issue was also raised of how to avoid immune rejection following transplantation of organs generated from ES cells. It seems that all of these issues could well be, and perhaps should be, addressed by thorough research in nonhuman primates prior to efforts in humans. The quality of information on monkey ES cells presented at this symposium, including the high level of homology between monkey genes and human gene chips, certainly validates this approach.
One intriguing approach is to use parthenogenetic ES cells, which appear to be pluripotent. They can differentiate into progenitors, express appropriate markers, and exhibit some functional properties characteristic of "true" ES cells. It is questionable whether this useful approach could be used in humans in the present climate. Even though parthenogenetic embryos have not been fertilized, they may still be viewed as "human embryos" and therefore still controversial. If so, then the case for using nonhuman primate ES cells generated by ART is further strengthened.
Summary – remaining needs and the future
Several key issues in nonhuman primate ARTs were highlighted by this symposium, or arose during discussions. In addition, as requested by the organizers, I have included a few of my own thoughts for consideration. It was claimed that nonhuman primate ARTs "are ready for propagation of selected genotypes." Certainly, there have been large improvements in ART success rates, but implantation rates after embryo transfer are still only about 20%, which is the same as for human ART [5], so there is considerable room for increases in primate ART efficiency.
• The production of identical twins in rhesus monkeys remains problematic. Success would provide a boost to biomedical research involving nonhuman primates. There needs to be continued extension of nonhuman primate ARTs into addressing human disease problems, not only human infertility.
• We need continued development of technologies supporting these studies, i.e., ES cell derived cells and tissues, gene chips, etc.
• I think it is very desirable to support cooperative training and collaborations among primate researchers, especially those not located at the National Primate Research Centers. Supplying materials for those investigators, e.g., cryopreserved IVP embryos, will increase the amount of research that can be conducted with nonhuman primates without large increases in cost, so it becomes more cost-effective.
• I would encourage the provision of collaborative grants, using (e.g.) the Cooperative Agreement UO1 mechanism, to support and stimulate interactive ART research projects with nonhuman primates. This could be via a joint NCRR/NICHD/GMS program to share the cost and broaden the research scope.
• There is a great need for increased emphasis on funding for nonhuman primate ARTs. Most of the available research funding during the past two decades has gone to support studies with mice, and although much basic information has been generated in this way, very little has been accomplished that can be directly helpful to human ART.
• Meetings like this symposium are invaluable and cost-effective. They bring together researchers from different areas of nonhuman primate biology and encourage collaborations. It would be productive to hold such meetings regularly, with NIH support.
• There are a number of important research needs that remain to be addressed, some of which were not directly addressed in the symposium, including:
(i) Development of protocols for in vitro maturation (IVM) of primate oocytes; this would be useful for ARTs in monkeys and for humans, e.g., PCOS patients. This approach could also avoid excessive ovarian stimulation that may impact oocyte quality and can disturb the reproductive cycle.
(ii) Identification of non-invasive markers for oocyte and embryo quality.
(iii) Development of chemically defined embryo culture media, i.e., without serum or serum proteins, which would avoid the potential introduction of serum-derived pathogenic organisms. This could be critically important for culture of ES cells.
(iv) Obtaining genetic and physiological data on in vivo produced embryos to establish a normal database for improving IVP embryo quality; because this is not, and will not be, available for humans, use of the nonhuman primate can provide critically important information.
(v) Unless there is a sudden reduction in the AIDS research emphasis on rhesus macaques, which appears unlikely, we urgently need to establish other nonhuman primate models for ARTs. This should be a priority both for scientists involved in ARTs and for the NIH.
Finally, I suggest that we need to make greater efforts to educate the general public as well as the federal government about the value of nonhuman primates as models for human disease. This could make our work more appreciated and encourage more support for this important research area.
References
- Bavister BD, Boatman DE, Collins K, Dierschke DJ, Eisele SG. Birth of rhesus monkey infant after in vitro fertilization and non surgical embryo transfer. Proc Natl Acad Sci USA. 1984;81:2218–2222. doi: 10.1073/pnas.81.7.2218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clayton O, Kuehl TJ. The first successful in vitro fertilization and embryo transfer in a nonhuman primate. Theriogenology. 1984;21:228 [abstract]. doi: 10.1016/0093-691X(84)90328-5. [DOI] [Google Scholar]
- Edwards RG, Bavister BD, Steptoe PC. Early stages of fertilization in vitro of human oocytes matured in vitro. Nature (Lond) 1969;221:632–635. doi: 10.1038/221632a0. [DOI] [PubMed] [Google Scholar]
- Bavister BD. Influences of culture media on embryo development. In: DeJonge CJ, Barrett CLR, editor. In ART – Today and Beyond. Cambridge University Press; 2002. pp. 127–143. [Google Scholar]
- Wright VC, Schieve LA, Reynolds MA, Jeng G. Assisted reproductive technology surveillance – United States, 2000. MMWR Surveill Summ. 2003;52:1–16. [PubMed] [Google Scholar]
- Bavister BD, Dees HC, Schultz RD. Refractoriness of rhesus monkeys to repeated ovarian stimulation by exogenous gonadotropins is caused by non-precipitating antibodies. Am J Reprod Immunol Microbiol. 1986;11:11–16. doi: 10.1111/j.1600-0897.1986.tb00021.x. [DOI] [PubMed] [Google Scholar]
- Si W, Zheng P, Tang X, He C, Wang H, Bavister BD, Ji W. Cryopreservation of rhesus monkey (Macaca mulatta) spermatozoa and their functional assessment by in vitro fertilization. Cryobiology. 2000;41:232–240. doi: 10.1006/cryo.2000.2283. [DOI] [PubMed] [Google Scholar]
- Zenzes MT, Bielecki R, Casper RF, Leibo SP. Effects of chilling to 0 degrees C on the morphology of meiotic spindles in human metaphase II oocytes. Fertil Steril. 2001;75:769–777. doi: 10.1016/S0015-0282(00)01800-8. [DOI] [PubMed] [Google Scholar]
- Songsasen N, Yu IJ, Ratterree MS, VandeVoort CA, Leibo SP. Effect of chilling on the organization of tubulin and chromosomes in rhesus monkey oocytes. Fertil Steril. 2002;77:818–825. doi: 10.1016/S0015-0282(01)03240-X. [DOI] [PubMed] [Google Scholar]
- Wolf DP, Vandevoort CA, Meyer-Haas GR, Zelinski-Wooten MB, Hess DL, Baughman WL, Stouffer RL. In vitro fertilization and embryo transfer in the rhesus monkey. Biol Reprod. 1989;41:335–346. doi: 10.1095/biolreprod41.2.335. [DOI] [PubMed] [Google Scholar]
- Boatman DE. In vitro growth of non-human primate pre- and peri-implantation embryos. In: Bavister BD, editor. In The Mammalian Preimplantation Embryo. Plenum Press, New York; 1987. pp. 273–308. [Google Scholar]
- Yeoman RR, Gerami-Naini B, Mitalipov S, Nusser KD, Widmann-Browning AA, Wolf DP. Cryoloop vitrification yields superior survival of Rhesus monkey blastocysts. Hum Reprod. 2001;16:1965–1969. doi: 10.1093/humrep/16.9.1965. [DOI] [PubMed] [Google Scholar]
- Kolb BA, Najmabadi S, Paulson RJ. Ultrastructural characteristics of the luteal phase endometrium in patients undergoing controlled ovarian hyperstimulation. Fertil Steril. 1997;67:625–630. doi: 10.1016/S0015-0282(97)81356-8. [DOI] [PubMed] [Google Scholar]
- Munne S, Cohen J. Chromosome abnormalities in human embryos. Hum Reprod Update. 1998;4:842–855. doi: 10.1093/humupd/4.6.842. [DOI] [PubMed] [Google Scholar]