Abstract
Background
Increased discounting of delayed rewards may be a premorbid characteristic and possible risk factor for alcohol and other drug use disorders; however, previous studies have found no or minimal differences in delay discounting in individuals at risk for substance use disorders based on family history. It is possible that increased delay discounting may be more closely associated with antisocial traits, evident in a subset of individuals with positive family histories of alcohol and drug use disorders, and that previous studies were underpowered for detecting subtle to modest overall group differences.
Methods
In this study, we compared 143 young adults with family histories of alcohol and other drug use disorders (FH+) and 155 young adults with no such histories (FH−) on delay discounting and subsequently examined how delay discounting was related to antisocial traits and other selected psychological and demographic variables.
Results
The FH+ group discounted delayed rewards more than the FH− group. Subsequent analyses revealed that increased delay discounting was correlated with having more parents and grandparents with alcohol and drug use disorders, more antisocial traits, more depressive tendencies and lower IQs, and lower income. After controlling for all these relationships, more antisocial traits and lower IQ still predicted greater delay discounting, and subsequent analysis revealed that the greater delay discounting in the FH+ group was mediated by this group’s greater number of individuals with antisocial traits.
Conclusion
FH+ individuals who discount delayed rewards more may be at increased risk for developing alcohol and other drug use disorders; however, additional descriptive studies and longitudinal studies are needed.
Keywords: Delay Discounting, Impulsivity, Family History, Alcohol Use Disorders, Substance Use Disorders, Antisocial
Heavy drinkers and alcohol dependent individuals have been reported to discount delayed rewards more than healthy controls (Bjork et al., 2004; Field et al., 2007; MacKillop et al., 2010; Mitchell et al., 2005; Petry, 2001a; Vuchinich and Simpson, 1998), meaning they have increased preferences for sooner smaller rewards over delayed larger rewards. Increased delay discounting has also been associated with a variety of other addictions including stimulant, opiate, and tobacco use disorders, binge eating, and problem gambling (Alessi and Petry, 2003; Coffey et al., 2003; Davis et al., 2010; Heil et al., 2006; Hoffman et al., 2006; Madden et al., 1997; Petry, 2001b; Yeomans et al., 2008). Thus, increased delay discounting may be a general, possibly core feature of addictions even though specific relationships to the pathology of addictions are unclear (Bickel et al., 2007; Bretteville-Jensen, 1999; Reynolds, 2006). For instance, increased delay discounting may plausibly be (i) a premorbid characteristic and possible risk factor for addictions, or (ii) a characteristic that emerges as addictions develop, possibly either as result of neurobiological changes caused by excessive substance use or as an adaptive behavioral response to environments associated with addictions where delayed rewards are unlikely (e.g., promises of delayed money may often not be trustworthy or reliable and/or the individual may perceive themselves as likely to be incarcerated, seriously ill, or deceased when delayed money would be available).
Previous studies have examined if increased delay discounting may present before addictions develop by examining delay discounting in individuals with family histories of alcohol and other drug use disorders (FH+), a population at increased risk for developing alcohol and drug use disorders themselves (Finn et al., 1990; Lieb et al., 2002; Merikangas et al., 1998). These studies have found no or minimal differences in delay discounting among FH+ individuals relative to those with no family histories of alcohol or drug use disorders (FH−; Crean et al., 2002; Herting et al., 2010; Petry et al., 2002). However, FH+ young adults have been reported to be more impulsive on go/no go task (Saunders et al., 2008), and impulsive performance on stop signal tasks can predict the development of problem drinking among FH+ adolescents and the development of alcohol dependence among adult heavy drinkers (Nigg et al., 2006; Rubio et al., 2008). These contrasting results may be interpreted in the context of recent theoretical and empirically derived models of impulsivity indicating that delay discounting-related measures assay decision making aspects of impulsivity that are distinct from the response initiation and response inhibition aspects of impulsivity indexed by stop signal and go/no go tasks (Dougherty et al., 2009; Evenden, 1999; Moeller et al., 2001; Reynolds et al., 2006; Winstanley et al., 2006; de Wit and Richards, 2004). Consequently, FH+ appears most robustly associated with increased response initiation and response inhibition impulsivity and not increased delay discounting.
The lack of effects of FH status on delay discounting suggests that increased delay discounting may not be a premorbid characteristic across all individuals at risk for alcohol and drug use disorders based on family histories; however, it is also possible that increased delay discounting may be present in subset of FH+ individuals with additional risk factors. One likely candidate risk factor is the presence of antisocial traits as this is not only a risk for alcohol and drug use disorders (e.g., Enoch, 2006; Moffitt et al., 2002) but also, among individuals with alcohol and drug use disorders, mediates increased delay discounting (Petry, 2002) and greater impairments on a simulated gambling task involving learning, risk taking, and decision making (Cantrell et al., 2008; Dom et al., 2006;Miranda et al., 2009).
In our work comparing FH+ and FH− nondependent young adults in the Oklahoma Family Health Patterns Project, we have characterized antisocial tendencies using Gough’s California Psychological Inventory Socialization Scale (CPI-So) score (Gough, 1994). We have found that impulsive go/no go task performance in FH+ individuals appeared to be mediated by antisocial tendencies as FH status was no longer significantly associated with impulsive task performance after controlling for CPI-So scores (Saunders et al., 2008). FH+ subjects with low CPI-So (more antisocial) scores had higher interference scores on the Stroop test than FH+ subjects with high CPI-So scores or FH− subjects with low or high CPI-So scores (Lovallo et al., 2006), indicating FH+ subjects with antisocial tendencies may be more sensitive to response conflicts and/or have impairments in selective attention. Finally, FH+ males with low CPI-So scores were more attentive to gains on the Iowa Gambling task (Lovallo et al., 2006). Given the cognitive differences observed in FH+ individuals with antisocial tendencies and prior research relating antisocial traits to greater discounting of delayed rewards in other populations, it is plausible that antisocial tendencies may mediate greater discounting of delayed rewards in FH+ individuals.
In this study, we examined delay discounting in a sample of FH+ and FH− young adults large enough to detect subtle to modest effect size differences. To better understand underlying factors contributing to group differences in delay discounting, we also examined how delay discounting related to and was influenced by antisocial traits as well as other relevant variables. These variables included demographic variables previously associated with delay discounting such as socioeconomic status, education and estimated intelligence (de Wit et al., 2007), estimates of lifetime adversities that are thought to increase risks both for alcohol and drug use disorders and antisocial and disinhibited behavioral patterns (Hicks et al., 2009), and individual alcohol and drug use levels.
MATERIALS AND METHODS
Participants
The present sample consisted of 298 healthy young adults (143 FH+ and 155 FH−), 125 men (42%) and 173 women (58%), recruited through community advertisement from the general population of Oklahoma City, OK. Participants had no current Axis I or II disorders (clusters A and C) by DSM-IV-TR (APA, 2000) criteria, including current depression, current drug or alcohol abuse, or any history of drug or alcohol dependence except for nicotine dependence (Table 1). All participants signed a consent form approved by the Institutional Review Board of the University of Oklahoma Health Sciences Center and the Veterans Affairs Medical Center in Oklahoma City, OK.
Table 1.
Sample Characteristics
| Family history | FH− | FH+ | p-Values |
|---|---|---|---|
| N (M/F) | 155 (73/82) | 143 (52/91) | 0.06 |
| Age (years) | 23 (0.2) | 24 (0.3) | |
| Education (years) | 14.8 (0.1) | 14.5 (0.1) | |
| SES | 49 (1.1) | 41 (1.1) | <0.0001 |
| Shipley mental age | 17.2 (0.1) | 17.0 (0.1) | |
| Ethnicity (%) | 0.007 | ||
| Caucasian | 90 | 76 | |
| African American | 6 | 13 | |
| Hispanic | 3 | 2 | |
| Native American | 2 | 6 | |
| Other | 0 | 3 | |
| CPI-So | 33.1 (0.4) | 29.2 (0.4) | <0.0001 |
| BDI | 3.5 (0.3) | 5.9 (0.4) | <0.0001 |
| EPI-neuroticism | 4.8 (0.3) | 6.6 (0.3) | <0.0001 |
| EPI-extraversion | 12.6 (0.3) | 12.1 (0.3) | |
| EPI-impulsivity | 4.1 (0.1) | 4.3 (0.2) | |
| AUDIT | 3.1 (0.2) | 3.8 (0.3) | 0.05 |
| Alcohol intake (standard drinks/month) | 40 (3) | 51 (4) | 0.02 |
| Caffeine (mg/d) | 118 (12) | 122 (11) | |
| Tobacco (% using weekly) | 9 | 18 | 0.02 |
Entries (mean ± SEM) unless given otherwise. SES scores shown are considered “Middle Class.” Variables were compared with between group t-tests. Only ps < 0.10 are shown.
FH−, negative family history; FH+, positive family history; M, male; F, female; SES, Hollingshead & Redlich Socioeconomic Status Score; Shipley mental age, Shipley Institute of Living Mental Age Score; CPISo, California Personality Inventory Sociability Scale; BDI, Beck Depression Inventory; EPI, Eysenck Personality Inventory; AUDIT, Alcohol Use Disorders Identification Test.
Family History of Alcohol and Other Drug Use Disorders
Family history classification was established using the Family History Research Diagnostic Criteria (FH-RDC; Andreasen et al., 1977). The FH-RDC has a high degree of interrater reliability (0.95) for reports of substance use disorders (Andreasen et al., 1977; Zimmerman et al., 1988). All FH+ participants reported at least 1 biological parent met at least 2 of the possible 6 criteria for alcohol or substance abuse. FH− participants reported no alcohol or substance use disorders in their biological parents and grandparents. The participants FH-RDC was confirmed by parent interview in all possible cases (79% of these participants) and parents confirmed FH status in 89% of these cases. FH status could confidently be reassigned in 3% of the cases and 6% were dropped for inconsistent or insufficient information. Of the participants with no parent interview, we assume that 89% are correctly classified, and by extrapolation, that 91% of the total sample remaining in this analysis is correctly classified. Participants were excluded if either they or the parent reported possible fetal exposure to alcohol or other drugs. Family history was also examined using a family density score obtained by counting the number of parents and grandparents meeting criteria for alcohol and/or drug use disorders. Scores ranged from 0 (FH− participants) to a possible 6 (FH+ participants with both parents and all grandparents affected).
Physical Health, Mental Health, and Demographic Assessments
Physical health was assessed using a structured medical history and self-report of current good health. Estimated intelligence (Shipley mental age) was determined from the vocabulary score on the Revised Shipley Institute of Living Scale (Zachary, 1986). Psychological functioning was assessed using the computerized version of the Diagnostic Interview Schedule-IV (DIS-IV; Bucholz et al., 1994) and the Beck Depression Inventory II (BDI; Beck et al., 1996). Alcohol and drug use were assessed through the Cahalan Drinking Habits Questionnaire (Cahalan and Cisin, 1968), the Alcohol Use Disorders Identification Test (Barbor et al., 1992), and a drug use questionnaire (Saunders et al., 2008). Socioeconomic Status Score (SES) was measured using the Hollingshead scale (Hollingshead, 1975) with updated occupational categories and was based on the primary occupation of the main breadwinner in the household in which the participant grew up.
Personality Assessments
Antisocial traits were quantified with the Sociability scale of CPI-So (Gough, 1994), a 46-item self-report measure of norm abiding and pro-social behaviors. Gough (1994) reported that scores ≥30 characterize norm-abiding groups, such as research scientists (32.0) and nursing students (31.5), while scores <30 indicate increasingly deviant, norm-violating groups, such as infrequent and frequent marijuana smokers (28.7 and 26.3), shoplifters (27.9), children of less- and more-severe alcoholics (27.4 and 25.1), alcoholics (22.8), and pathological gamblers (21.3). Other measures of personality included the Tridimensional Personality Questionnaire (TPQ; Cloninger et al., 1991), and the Eysenck Personality Inventory (EPI; Eysenck and Eysenck, 1964).
Lifetime Adversity
Lifetime adversity was assessed from questions on the DIS-IV using 5 items similar to adverse life events assessed in the studies by Caspi and colleagues (2002, 2003): (1) Have you ever been mugged or threatened with a weapon, or experienced a break-in or robbery? (2) Have you ever been raped or sexually assaulted by a relative? (3) Have you ever been raped or sexually assaulted by someone not related to you? (4) Before you were 15, was there a time when you did not live with your biological mother for at least 6 months? (5) Before you were 15, was there a time when you did not live with your biological father for at least 6 months? Possible scores ranged from 0 (endorsing no items) to 5 (endorsing all items).
Delay Discounting
The delay discounting procedure used has been described in detail previously (Kirby, 2009; Kirby et al., 1999) and consisted of 27 choices between smaller, immediate, and larger, delayed amounts of money such as, “Would you prefer (a) $34 today or (b) $50 in 30 days?” 9 of the 27 choices offered small amounts of delayed money ($25 to $35), 9 offered medium amounts of delayed money ($50 to $60), and 9 offered large amounts of delayed money ($75 to $85). Discount rate estimates (k) based on the hyperbolic discounting function of Mazur (1987) were estimated for each participant based on the pattern of choices made across the 9 questions in each money size category. Possible values of k for each money size category ranged from 0.00016 (choosing all 9 delayed options) to 0.25 (choosing all 9 immediate options).
Testing Protocol
Participants took part in 3 laboratory visits. The first was a screening assessment of health status, psychological functioning, temperament characteristics, drinking behavior, and personality. The second 2 visits consisted of 2 days of laboratory testing, controlling for time of day. The first test day primarily consisted of psychophysiological stress testing and the second day included the delay discounting measure and other behavioral tasks. Alcohol and drug abstinence was confirmed on test days by negative expired-air alcohol tests (AlcoMate Prestige, AL-6000; AK Solutions, Palisades Park, NJ) and urine drug screens (icup; Alcopro, Knoxville, TN).
Data Analysis
All data analyses were performed using SAS (SAS System for Windows, version 9.1.3, SAS Institute, Cary, NC). The FH groups were compared on demographic variables, psychological status, and drug and alcohol use with chi-square tests and 2-tailed Student’s t-tests. The k values for the small, medium, and large amounts of delayed money were normalized prior to all analyses using a natural log transform because they were skewed. A mixed factor analysis of variance was conducted (SAS Proc Mixed) to examine the effects of FH on delay discounting for the 3 k values with delayed money amount as a within subject variable and FH status (FH− or FH+) as a between-subject variable. Next, Pearson correlation coefficients were computed between k values, FH density, demographic variables, and personality measures to identify relationships with delay discounting. Following this, a multiple linear regression analysis was performed to model the relationship of the variables significantly correlated with k values, after controlling for FH density. Finally, regression analysis was employed to investigate possible mediators of the relationship between FH density and delay discounting using Arioan’s test of mediation (Sobel, 1982; Baron and Kenny, 1986).
RESULTS
Demographic Characteristics
Participant demographic characteristics are presented in Table 1. Compared with FH−, the FH+ participants had lower SES, lower CPI-So scores, higher BDI scores, higher EPI-Neuroticism Scores, and higher monthly alcohol intake. There were more minorities and smokers in the FH+ group. FH+ and FH− participants did not differ in age, education, estimated intelligence, or AUDIT scores. Among FH+ participants, 79 (56%) had family histories of alcohol use disorders only, 52 (37%) had family histories of alcohol and drug use disorders, and 10 (7%) had family histories of drug use disorders only. Density of affected relatives among FH+ subjects was as follows: 1 relative for 64 (45%), 2 for 43 (30%), 3 for 26 (18%) and 4 for 9 (6%).
Effects of FH Status on Delay Discounting
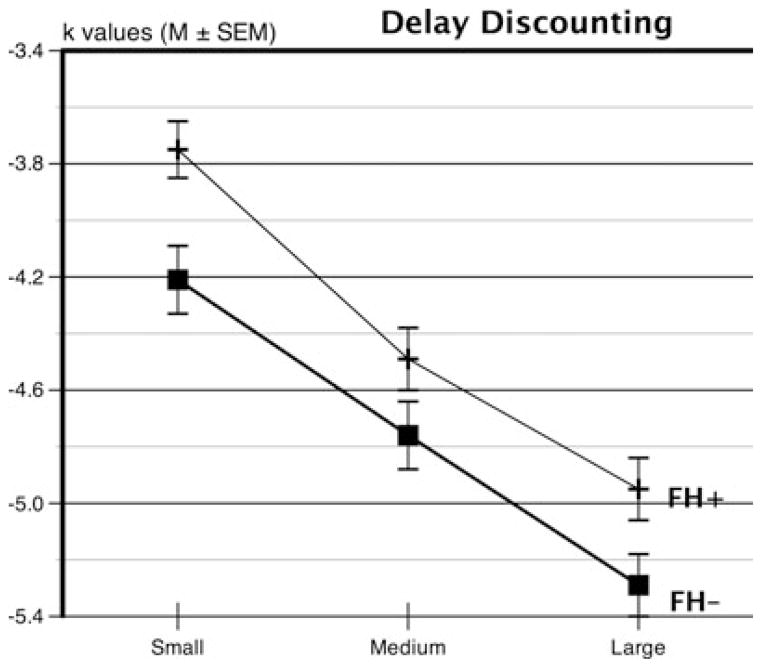
FH+ had smaller k values than FH− participants [main effect of group; F(1, 296) = 5.53, p = 0.019], indicating greater discounting of delayed rewards (Fig. 1). Furthermore, k values declined with increasing amounts of delayed money [main effect of delayed money amount; F(2, 592) = 301.47, p < 0.0001] indicating smaller delayed rewards were discounted more than larger delayed rewards. There was no significant interaction between FH status and reward size.
Fig. 1.
Comparison of delay discounting of small, medium, and large hypothetical monetary rewards in FH+ and FH− individuals, as indexed by natural log transformed k values (mean ± SEM). FH+ participants discounted delayed rewards more impulsively, as indexed by higher k values. FH+ = subjects with a positive parental history of alcohol or drug abuse. FH− = persons with no alcohol or drug abuse in parents or grandparents.
Relationships of Demographic and Personality Variables to Delay Discounting
Pearson correlation coefficients were computed between mean k values and selected demographic variables, personality measures, and alcohol use (Table 2). Of these, FH density, race, and BDI scores were positively correlated with k values, indicating individuals with denser family histories of alcohol and drug use disorders, non-Caucasians, and more depressed individuals discounted delayed rewards more. CPI-So scores, SES, and Shipley mental age were all negatively correlated with k values, indicating individuals with lower sociability, less income, and lower intelligence all discounted delayed rewards more rapidly.
Table 2.
Delay Discounting (Mean k Value) Correlations
| Variable | r | p |
|---|---|---|
| CPI | −0.23 | <0.0001 |
| SES | −0.17 | 0.005 |
| Education (years) | −0.02 | 0.79 |
| AUDIT | −0.01 | 0.87 |
| Race (Caucasion/other)a | 0.21 | 0.0004 |
| BDI | 0.14 | 0.02 |
| Shipley mental age | −0.23 | <0.0001 |
| FH density | 0.15 | 0.01 |
| Life adversity | 0.09 | 0.12 |
| EPI-neuroticism | 0.04 | 0.51 |
| EPI-impulsivity | 0.10 | 0.10 |
| EPI-extraversion | 0.06 | 0.30 |
| Alcohol intake (oz/month) | 0.04 | 0.52 |
| Tobacco (% using weekly)a | 0.08 | 0.15 |
CPI-So, California Personality Inventory Sociability Scale; SES, Hollingshead & Redlich Socioeconomic Status Score; AUDIT, Alcohol Use Disorders Identification Test; BDI, Beck Depression Inventory; Shipley mental age, Shipley Institute of Living Mental Age Score; FH density; number of parents and grandparents meeting criteria for alcohol and/or drug use disorders; EPI, Eysenck Personality Inventory.
Point biserial correlation reported as tobacco and race are binary outcome variables.
Multivariate Prediction of Delay Discounting Rates
A sequential multiple linear regression analysis was performed to build a model predicting delay discounting. Each of the predictor variables was chosen due to a significant (p < 0.01) zero-order correlation with delay discounting. In the first step, FH density was added. This model was statistically significant, F(1, 273) = 5.43, p = 0.02, R2 = 0.02 (Table 3). SES, race, BDI, and mental age were entered simultaneously in the second step to determine whether the personality and demographic characteristics contributed to delay discounting over and above FH density. The addition of these predictors increased the fit of the model to the data, F(4, 269) = 5.95, p < 0.0001, sr2 = 0.08. The resulting model R2 was significantly >0, F(5, 269) = 5.92, p < 0.0001. In the final step, CPI-So was entered to determine whether antisocial tendencies account for additional variability in delay discounting over and above FH density and the other demographic and personality variables. The addition of CPI-So significantly increased the fit of the model, F(1, 268) = 6.51, p = 0.01, sr2 = 0.02. The resulting model R2 was significantly >0, F(6, 268) = 6.12, p < 0.0001, and accounted for 12% of the variability in delay discounting. Each of the predictor variables had a significant (p < 0.01) zero-order correlation with delay discounting, but only the CPI-So and mental age predictors had significant (p < 0.05) partial effects in the full model.
Table 3.
Sequential Regression Predicting Delay Discounting
| Step | Variables | B | se(B) | β | Block ΔR2 | F | p |
|---|---|---|---|---|---|---|---|
| 1 | FH density* | 0.16 | 0.07 | 0.14 | 0.02 | 5.43 | 0.02 |
| 2 | FH density | 0.07 | 0.07 | 0.06 | 0.08 | 5.95 | <0.0001 |
| SES | −0.01 | 0.01 | −0.09 | ||||
| MA* | −0.17 | 0.06 | −0.16 | ||||
| Race* | 0.46 | 0.22 | 0.13 | ||||
| BDI | 0.03 | 0.02 | 0.09 | ||||
| 3 | FH density | 0.02 | 0.07 | 0.02 | 0.02 | 6.51 | 0.01 |
| SES | −0.01 | 0.01 | −0.08 | ||||
| MA* | −0.16 | 0.06 | −0.15 | ||||
| Race | 0.43 | 0.22 | 0.12 | ||||
| BDI | 0.01 | 0.02 | 0.04 | ||||
| CPI-So* | −0.04 | 0.02 | −0.17 |
Full model: R2 = 0.12, F(6, 268) = 6.12, p < 0.0001.
FH density, number of parents and grandparents meeting criteria for alcohol and/or drug use disorders; SES, Hollingshead & Redlich Socioeconomic Status Score; BDI, Beck Depression Inventory; MA, Shipley Institute of Living Mental Age Score; CPI-So, California Personality Inventory Sociability Scale.
p < 0.05.
These results suggested that the increased delay discounting in the FH+ group was mediated by this group’s greater number of individuals with low CPI-So scores as there were no FH differences in IQ. Therefore, we employed a regression analysis to investigate the involvement of CPI-So as a possible mediator of the relationship between FH density and delay discounting. FH density was found to be significantly related to CPI-So (β = −0.34, p < 0.0001). Delay discounting was significantly related to a linear combination of FH density and CPI-So, F(2, 294) = 8.89, p = 0.0002. Only CPI-So (β = −0.2, p = 0.001) had a significant partial effect on delay discounting. Aroian’s test of mediation indicated that CPI-So significantly mediated the relationship between FH density and behavior (TS = 2.91, p = 0.004).
DISCUSSION
In this study, we observed that FH+ individuals discounted delayed rewards more than FH− individuals. Among all participants, increased delay discounting was related to having more parents and grandparents with alcohol and drug use disorders, more antisocial tendencies (lower CPI-So scores), more depressive tendencies, less income, non-Caucasian race, and lower IQs. After controlling for FH density and other relevant demographic and personality variables, greater antisocial tendencies and lower IQs independently predicted greater discounting, indicating that the increased delay discounting in the FH+ group is mediated by this group’s greater number of individuals with low CPI-So scores as there were no FH differences in IQ which was confirmed with subsequent analyses. Consequently, FH+ individuals are more likely to discount delayed rewards more because they are more likely to have antisocial tendencies; however, it is presently unclear how increased delay discounting specifically relates to risk for alcohol and drug use disorders.
The present findings contrast with previous studies that have found no or minimal effects of FH status on delay discounting (Crean et al., 2002; Herting et al., 2010; Petry et al., 2002). This discrepancy is likely due to previous studies being underpowered for detecting the relatively modest difference observed in this study. In this study, we found that increased delay discounting was more directly linked to antisocial traits, which are commonly present in FH+ individuals, rather than simply FH+ status. While the presence of antisocial traits also appears to mediate impulsive performance on a go/no go task in FH+ individuals (Saunders et al., 2008), FH effects on both go/no and stop signal tasks appear to be more readily detected in smaller sample sizes (Nigg et al., 2006; Rubio et al., 2008). These findings indicate that impulsive performances on go/no go and stop signal tasks are more robustly associated with FH+ status than increased delay discounting; however, FH+ individuals with antisocial traits do discount delayed rewards more.
The present results showing that FH+ individuals with lower CPI-So scores are likely to discount delayed rewards more stand in relation to prior findings from the Oklahoma Family History Project that reveal a pattern of impulsive and less well-regulated cognitive and behavioral performance in FH+ individuals who also have low CPI-So scores. We have reported that FH+ individuals with low CPI-So scores have higher interference scores on the Stroop task (Lovallo et al., 2006), and they make more impulsive errors on a go/no go reaction time task (Saunders et al., 2008). The males also show greater attraction to gains in the Iowa Gambling Task (Lovallo et al., 2006), and they also have greater activity in the caudate nucleus while performing this task (Acheson et al., 2009). These findings are consistent with the formulation of Tarter and colleagues (2004) that young persons with a significant diathesis for alcohol and other substance use disorders display a neurobehavioral disinhibition, and they are also consistent with the characterization of Sher and colleagues (1991) that such persons are behaviorally undercontrolled. These results are therefore suggestive of a less tightly regulated prefrontal control over motivated behavior in persons at familial risk for alcoholism.
While the present results indicate that increased delay discounting is present in a subset FH+ individuals who are plausibly most at risk for developing alcohol and drug use disorders, it is unclear what role delay discounting may play in FH+ associated behavioral characteristics and risks for addictions in this population. Increased discounting of delayed rewards or perhaps delayed consequences more generally may be a core vulnerability and underlie not only lack of concern for future consequences but also may play a role in the poor decision making and excessive risk taking observed in this population. These behavioral patterns driven by increased delay discounting could in turn promote more problematic use of alcohol and drugs leading to substance use disorders. Alternatively, increased delay discounting in this population may be a peripheral consequence of a more central characteristic of FH+ individuals such as high reward dependence. Finally, although delay discounting is increased in at least some FH+ individuals, it is still unclear if delay discounting may also be increased by direct or indirect consequences of excessive alcohol or drug use. Additional descriptive studies to more fully characterize FH+ individuals as well as longitudinal studies where causal inferences can be determined are needed to address these issues.
Acknowledgments
This article is dedicated in memory of our colleague Frank Collins, Ph.D., of Oklahoma State University and the University of North Texas, who passed away as this paper was being prepared. Frank initiated the investigation of delay discounting in this project and provided invaluable direction in its early development and interpretation in the context of risk for alcohol and other drug use disorders. This work was supported by the Department of Veterans Affairs Medical Research Service and the National Institutes of Health/NIAAA (R01-AA12207) and NCRR (M01-RR14467, UL1-RR025767 & KL2-RR025766).
References
- Acheson A, Robinson JL, Glahn DC, Lovallo WR, Fox PT. Differential activation of the anterior cingulate cortex and caudate nucleus during a gambling simulation in persons with a family history of alcoholism: studies from the Oklahoma Family Health Patterns Project. Drug Alcohol Depend. 2009;100:17–23. doi: 10.1016/j.drugalcdep.2008.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alessi SM, Petry NM. Pathological gambling severity is associated with impulsivity in a delay discounting procedure. Behav Processes. 2003;64:345–354. doi: 10.1016/s0376-6357(03)00150-5. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Endicott J, Stitzer RL, Winokur G. The family history method using diagnostic criteria. Arch Gen Psychiatry. 1977;34:1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. 4. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Barbor TF, de las Fuentes JR, Saunders JB, Grant M. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines For Use in Primary Health Care. World Health Organization; Geneva, Switzerland: 1992. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Miller ML, Yi R, Kowal BP, Lindquist DM, Pitcock JA. Behavioral and neuroeconomics of drug addiction: competing neural systems and temporal discounting processes. Drug Alcohol Depend. 2007;90(Suppl 1):S85–S91. doi: 10.1016/j.drugalcdep.2006.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjork JM, Hommer DW, Grant SJ, Danube C. Impulsivity in abstinent alcohol-dependent patients: relation to control subjects and type 1-/type 2-like traits. Alcohol. 2004;34:133–150. doi: 10.1016/j.alcohol.2004.06.012. [DOI] [PubMed] [Google Scholar]
- Bretteville-Jensen AL. Addiction and discounting. J Health Econ. 1999;18:393–407. doi: 10.1016/s0167-6296(98)00057-5. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Jr, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Cahalan D, Cisin IH. American drinking practices: summary of findings from a national probability sample: II. Measurement of massed versus spaced drinking. Q J Stud Alcohol. 1968;29:642–656. [PubMed] [Google Scholar]
- Cantrell H, Finn PR, Rickert ME, Lucas J. Decision making in alcohol dependence: insensitivity to future consequences and comorbid disinhibitory psychopathology. Alcohol Clin Exp Res. 2008;32:1398–1407. doi: 10.1111/j.1530-0277.2008.00714.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, McClay J, Moffitt TE, Mill J, Martin J, Craig IW, Taylor A, Poulton R. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297:851–854. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Przybeck TR, Åvrakic DM. The Tridimensional Personality Questionnaire: U.S. normative data. Psychol Rep. 1991;69:1047–1057. doi: 10.2466/pr0.1991.69.3.1047. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Gudleski GD, Saladin ME, Brady KT. Impulsivity and rapid discounting of delayed hypothetical rewards in cocaine-dependent individuals. Exp Clin Psychopharmacol. 2003;11:18–25. doi: 10.1037//1064-1297.11.1.18. [DOI] [PubMed] [Google Scholar]
- Crean J, Richards JB, de Wit H. Effect of tryptophan depletion on impulsive behavior in men with or without a family history of alcoholism. Behav Brain Res. 2002;136:349–357. doi: 10.1016/s0166-4328(02)00132-8. [DOI] [PubMed] [Google Scholar]
- Davis C, Patte K, Curtis C, Reid C. Immediate pleasures and future consequences. A neuropsychological study of binge eating and obesity. Appetite. 2010;54:208–213. doi: 10.1016/j.appet.2009.11.002. [DOI] [PubMed] [Google Scholar]
- Dom G, De Wilde B, Hulstijn W, van den Brink W, Sabbe B. Decisionmaking deficits in alcohol-dependent patients with and without comorbid personality disorder. Alcohol Clin Exp Res. 2006;30:1670–1677. doi: 10.1111/j.1530-0277.2006.00202.x. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh-Richard DM, Furr RM, Nouvion SO, Dawes MA. Disinctions in behavioral impulsivity: implications for substance abuse research. Addict Disord Their Treat. 2009;8:61–73. doi: 10.1097/ADT.0b013e318172e488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enoch MA. Genetic and environmental influences on the development of alcoholism: resilience vs. risk. Ann N Y Acad Sci. 2006;1094:193–201. doi: 10.1196/annals.1376.019. [DOI] [PubMed] [Google Scholar]
- Evenden JL. Varieties of impulsivity. Psychopharmacology (Berl) 1999;146:348–361. doi: 10.1007/pl00005481. [DOI] [PubMed] [Google Scholar]
- Eysenck SB, Eysenck HJ. An improved short questionnaire for the measurement of extraversion and neuroticism. Life Sci. 1964;305:1103–1109. doi: 10.1016/0024-3205(64)90125-0. [DOI] [PubMed] [Google Scholar]
- Field M, Christiansen P, Cole J, Goudie A. Delay discounting and the alcohol Stroop in heavy drinking adolescents. Addiction. 2007;102:579–586. doi: 10.1111/j.1360-0443.2007.01743.x. [DOI] [PubMed] [Google Scholar]
- Finn PR, Kleinman I, Pihl RO. The lifetime prevalence of psychopathology in men with multigenerational family histories of alcoholism. J Nerv Ment Dis. 1990;178:500–504. [PubMed] [Google Scholar]
- Gough HG. Theory, development, and interpretation of the CPI socialization scale. Psychol Rep. 1994;75:651–700. doi: 10.2466/pr0.1994.75.1.651. [DOI] [PubMed] [Google Scholar]
- Heil SH, Johnson MW, Higgins ST, Bickel WK. Delay discounting in currently using and currently abstinent cocaine-dependent outpatients and non-drug-using matched controls. Addict Behav. 2006;31:1290–1294. doi: 10.1016/j.addbeh.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Herting MM, Schwartz D, Mitchell SH, Nagel BJ. Delay discounting behavior and white matter microstructure abnormalities in youth with a family history of alcoholism. Alcohol Clin Exp Res. 2010;34(9):1590–1602. doi: 10.1111/j.1530-0277.2010.01244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks BM, South SC, Dirago AC, Iacono WG, McGue M. Environmental adversity and increasing genetic risk for externalizing disorders. Arch Gen Psychiatry. 2009;66:640–648. doi: 10.1001/archgenpsychiatry.2008.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman WF, Moore M, Templin R, McFarland B, Hitzemann RJ, Mitchell SH. Neuropsychological function and delay discounting in methamphetamine-dependent individuals. Psychopharmacology (Berl) 2006;188(2):162–170. doi: 10.1007/s00213-006-0494-0. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. Yale University; New Haven, CT: 1975. [Google Scholar]
- Kirby KN. One-year temporal stability of delay-discount rates. Psychon Bull Rev. 2009;16:457–462. doi: 10.3758/PBR.16.3.457. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Lieb R, Merikangas KR, Hofler M, Pfister H, Isensee B, Wittchen HU. Parental alcohol use disorders and alcohol use and disorders in offspring: a community study. Psychol Med. 2002;32:63–78. doi: 10.1017/s0033291701004883. [DOI] [PubMed] [Google Scholar]
- Lovallo WR, Yechiam E, Sorocco KH, Vincent AS, Collins FL. Working memory and decision-making biases in young adults with a family history of alcoholism: studies from the Oklahoma family health patterns project. Alcohol Clin Exp Res. 2006;30:763–773. doi: 10.1111/j.1530-0277.2006.00089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Miranda R, Jr, Monti PM, Ray LA, Murphy JG, Rohsenow DJ, McGeary JE, Swift RM, Tidey JW, Gwaltney CJ. Alcohol demand, delayed reward discounting, and craving in relation to drinking and alcohol use disorders. J Abnorm Psychol. 2010;119:106–114. doi: 10.1037/a0017513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, Petry NM, Badger GJ, Bickel WK. Impulsive and self-control choices in opioid-dependent patients and non-drug-using control participants: drug and monetary rewards. Exp Clin Psychopharmacol. 1997;5:256–262. doi: 10.1037//1064-1297.5.3.256. [DOI] [PubMed] [Google Scholar]
- Mazur JE. An adjusting amount procedure for studying delayed reinforcement. In: Commons ML, Mazur JE, Nevin JA, Rachlin H, editors. Quantitative Analysis of Behavior: The Effects of Delay and of Intervening Events on Reinforcement Value. Vol. 5. Lawrence Erlbaum Associates; Hillsdale: 1987. pp. 55–73. [Google Scholar]
- Merikangas KR, Stolar M, Stevens DE, Goulet J, Preisig MA, Fenton B, Zhang H, O’Malley SS, Rounsaville BJ. Familial transmission of substance use disorders. Arch Gen Psychiatry. 1998;55:973–979. doi: 10.1001/archpsyc.55.11.973. [DOI] [PubMed] [Google Scholar]
- Miranda R, Jr, MacKillop J, Meyerson LA, Justus A, Lovallo WR. Influence of antisocial and psychopathic traits on decision-making biases in alcoholics. Alcohol Clin Exp Res. 2009;33:817–825. doi: 10.1111/j.1530-0277.2009.00901.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JM, Fields HL, D’Esposito M, Boettiger CA. Impulsive responding in alcoholics. Alcohol Clin Exp Res. 2005;29:2158–2169. doi: 10.1097/01.alc.0000191755.63639.4a. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158:1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Dev Psychopathol. 2002;14:179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Wong MM, Martel MM, Jester JM, Puttler LI, Glass JM, Adams KM, Fitzgerald HE, Zucker RA. Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. J Am Acad Child Adolesc Psychiatry. 2006;45:468–475. doi: 10.1097/01.chi.0000199028.76452.a9. [DOI] [PubMed] [Google Scholar]
- Petry NM. Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology (Berl) 2001a;154:243–250. doi: 10.1007/s002130000638. [DOI] [PubMed] [Google Scholar]
- Petry NM. Pathological gamblers, with and without substance use disorders, discount delayed rewards at high rates. J Abnorm Psychol. 2001b;110:482–487. doi: 10.1037//0021-843x.110.3.482. [DOI] [PubMed] [Google Scholar]
- Petry NM. Discounting of delayed rewards in substance abusers: relationship to antisocial personality disorder. Psychopharmacology (Berl) 2002;162:425–432. doi: 10.1007/s00213-002-1115-1. [DOI] [PubMed] [Google Scholar]
- Petry NM, Kirby KN, Kranzler HR. Effects of gender and family history of alcohol dependence on a behavioral task of impulsivity in healthy subjects. J Stud Alcohol. 2002;63:83–90. [PubMed] [Google Scholar]
- Reynolds B. A review of delay-discounting research with humans: relations to drug use and gambling. Behav Pharmacol. 2006;17:651–667. doi: 10.1097/FBP.0b013e3280115f99. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Ortengren A, Richards JB, de Wit H. Dimensions of impulsive behavior: personality and behavioral measures. Personality Individ Differ. 2006;40:305–315. [Google Scholar]
- Rubio G, Jimenez M, Rodriguez-Jimenez R, Martinez I, Avila C, Ferre F, Jimenez-Arriero MA, Ponce G, Palomo T. The role of behavioral impulsivity in the development of alcohol dependence: a 4-year follow-up study. Alcohol Clin Exp Res. 2008;32:1681–1687. doi: 10.1111/j.1530-0277.2008.00746.x. [DOI] [PubMed] [Google Scholar]
- Saunders B, Farag N, Vincent AS, Collins FL, Jr, Sorocco KH, Lovallo WR. Impulsive errors on a Go-NoGo reaction time task: disinhibitory traits in relation to a family history of alcoholism. Alcohol Clin Exp Res. 2008;32:888–894. doi: 10.1111/j.1530-0277.2008.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, Walitzer KS, Wood PK, Brent EE. Characteristics of children of alcoholics: putative risk factors, substance use and abuse, and psychopathology. J Abnorm Psychol. 1991;100:427–448. doi: 10.1037//0021-843x.100.4.427. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological Methodology 1982. American Sociological Association; Washington DC: 1982. pp. 290–312. [Google Scholar]
- Tarter RE, Kirisci L, Habeych M, Reynolds M, Vanyukov M. Neurobehavior disinhibition in childhood predisposes boys to substance use disorder by young adulthood: direct and mediated etiologic pathways. Drug Alcohol Depend. 2004;73:121–132. doi: 10.1016/j.drugalcdep.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Vuchinich RE, Simpson CA. Hyperbolic temporal discounting in social drinkers and problem drinkers. Exp Clin Psychopharmacol. 1998;6:292–305. doi: 10.1037//1064-1297.6.3.292. [DOI] [PubMed] [Google Scholar]
- Winstanley CA, Eagle DM, Robbins TW. Behavioral models of impulsivity in relation to ADHD: translation between clinical and preclinical studies. Clin Psychol Rev. 2006;26:379–395. doi: 10.1016/j.cpr.2006.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit H, Flory J, Acheson A, McCloskey M, Manuck SB. IQ and nonplanning impulsivity are independently associated with delay discounting in middle-aged adults. Personality Individ Differ. 2007;42:111–121. [Google Scholar]
- de Wit H, Richards JB. Dual determinants of drug use in humans: reward and impulsivity. Nebr Symp Motiv. 2004;50:19–55. [PubMed] [Google Scholar]
- Yeomans MR, Leitch M, Mobini S. Impulsivity is associated with the disinhibition but not restraint factor from the Three Factor Eating Questionnaire. Appetite. 2008;50:469–476. doi: 10.1016/j.appet.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Zachary RA. Shipley Institute of Living Scale Revised Manual. Western Psychological Services; Los Angeles, CA: 1986. [Google Scholar]
- Zimmerman M, Coryell W, Pfohl B, Stangl D. The reliability of the family history method for psychiatric diagnoses. Arch Gen Psychiatry. 1988;45:320–322. doi: 10.1001/archpsyc.1988.01800280030004. [DOI] [PubMed] [Google Scholar]