Abstract
Non–ST-segment elevation myocardial infarctions (NSTEMI) are common and cause significant morbidity and mortality. Following evidence-based medicine (EBM) guidelines is one way to ensure that these patients are cared for appropriately. This pilot study examined data from patients with NSTEMI to assess both documentation quality and use of EBM across multiple teams. Medical records were reviewed for significant differences in documentation quality in areas including history and physical exam, treatment, and inpatient mortality. While total documentation quality and mortality were not significantly different between groups, cardiology teams adhered to evidence-based recommendations more often than other teams.
Lack of proper documentation has been associated with poor patient outcomes. Cox et al found that documentation of cardiac risk factors was quite poor when reviewing history and physical documentation for patients hospitalized for myocardial infarction and congestive heart failure. It was even worse in the elderly and females (1). The absence of documented cardiovascular risk factors has led to higher mortality in non–ST-segment elevation myocardial infarctions (NSTEMI) (2). It was unknown locally how well physicians at Scott & White Memorial Hospital, part of the Baylor Scott & White Health system, document in these situations. This quality improvement study examined medical record documentation associated with three types of inpatient medicine treatment teams to determine if there were differences in documentation and use of evidence-based medicine (EBM) across provider teams.
METHODS
This study was approved by the institutional review board at Scott & White Healthcare. This was a retrospective chart review designed to examine the following questions: 1) In a comparison of cardiology, nonteaching, and teaching teams, which team scored higher in the quality of the medical record documentation and EBM use? 2) Does better physician documentation translate into a decrease in patient mortality at our institution?
The study took place at Scott & White Memorial Hospital in Temple, Texas, a 636-bed hospital part of an integrated health care system in Central Texas. Medical records of patients aged 18 to 99 with a primary diagnosis of NSTEMI who were admitted to our teaching, nonteaching, or cardiology teams between January 1, 2006, and December 31, 2009, were eligible for inclusion. Inclusion dates were chosen by the research team based upon when team structure, guidelines, and medical record systems were the most stable. After this timeframe, many changes in the institution occurred that did not allow for a long enough period of stability. Exclusion criteria included sepsis, demand infarction, NSTEMI as a secondary diagnosis, admission to a non–internal medicine team, and a troponin level <0.04 ng/mL. Based upon these criteria, 442 patients with a diagnosis of NSTEMI were initially included in this study.
Teaching teams comprised internal medicine residents and a hospitalist attending; nonteaching teams comprised a midlevel provider and a hospitalist; and cardiology teams comprised residents, fellows, and cardiology attendings.
As part of a mentored research grant at Scott & White/Texas A&M Health Sciences Center College of Medicine, the first author, who was an internal medicine resident at the time, conducted a retrospective chart review to examine the quality of medical record documentation and use of EBM across teams that cared for NSTEMI patients. The authors compared teams' use of EBM and documentation in the history, physical exam, lab findings, and tests performed. The purpose of this quality improvement project was to determine which team (cardiology, teaching, nonteaching inpatient team) needed the most improvement in documentation and EBM use.
The history and physical checklist used in this study was based upon a 20-point rating scale developed by Dunlay et al (3). The scale was modified to include 25 items evaluating the history and physical, as well as five items designed to evaluate the use of EBM. The modified scale included an expanded history and physical checklist, with a maximum score of 30, compared to 20 in the Dunlay study. The additional items covered were EBM, history of present illness, chief complaint, type and duration of pain, past medical history including lipids or previous cardiac imaging, family history, social history including drug and activity, and adding electrocardiogram and chest x-ray to studies. We excluded creatinine from labs and removed the problem list. Unlike the Dunlay study, partial credit for items was not given in this quality improvement study.
Charts were reviewed and scored using the initial history and physical. Each chart was reviewed and the history and physical was evaluated using the 30-point checklist described above. Use of EBM was determined on a 5-point scale and inpatient mortality was recorded. Patient team data (teaching, nonteaching, cardiology) and demographics were also recorded for each patient. For patients who were admitted overnight by hospitalists, the team recorded was the team to which they were assigned.
Specific criteria were used when examining each variable within the history and physical. For example, the chief complaint must have been listed specifically. A description of the type and duration of the complaint must have been listed, as well as any associated symptoms. The history of present illness was also inspected for mention of prior events like the current one. The medical history was reviewed for mention of current medical problems, recent lipid panels or hemoglobin A1C, or previous stress tests or angiograms or lack thereof. In the family history, the physician must have discussed the age at which a relative had a myocardial infarction, and other family history was counted as a separate item. Documentation of social history must have contained a positive or negative response to any drug, which includes alcohol, tobacco, and illegal drugs. A separate point was given if physical activity was included. Individual portions of the physical exam included vital signs, cardiovascular exam, respiratory exam, and peripheral vascular exam (peripheral pulses). For labs and studies, we concentrated on cardiac enzymes, electrocardiogram, chest x-ray, and hemoglobin. We also examined lipid, glucose, and hemoglobin A1C values.
The assessment and plan were reviewed for a differential diagnosis, five specific evidence-based therapies for NSTEMI, and treatments of other comorbidities. We reviewed for the following five specific therapies: aspirin, beta-blockers, heparin or a heparinoid, statin on discharge, and glycoprotein IIb/IIIa inhibitors. One point each was given if these were mentioned in the assessment and plan by documenting use or reason for not using. Angiotensin-converting enzyme inhibitors were not included due to specific requirements about ejection fraction. Clopidogrel was not included on the checklist since eptifibatide was the preferred agent when providers anticipated invasive management during this time period.
All variables, including 30 checklist items, overall checklist scores, and patient demographics, were summarized according to care team using descriptive statistics: mean for continuous variables and frequency for categorical variables. The three care teams were compared utilizing analysis of variance or Kruskal-Wallis test for continuous variables. Chi-square test or Fisher's exact test was used to compare groups of categorical variables. Pairwise comparisons utilized Bonferroni adjustment or Tukey's pairwise comparison when significant differences were detected. A P value of <0.05 was the threshold for statistical significance. SAS version 9.2 (SAS Institute Inc., Cary, NC) was used for data analysis.
RESULTS
Based upon a retrospective review of 442 charts of patients with a diagnosis of NSTEMI and a troponin level >0.04 ng/mL, 252 (57.0%) were NSTEMI cases that had been treated by one of the three teams. Excluded were 91 cases (20.6%) with ST-elevation myocardial infarctions, 59 cases (12%) treated by teams not in the study, and 40 cases (9%) wherein myocardial infarction was a secondary diagnosis.
Among patients with NSTEMI as a primary diagnosis (N = 252), 151 cases (60%) were treated by a cardiology team, 60 cases (24%) were treated by a teaching team, and 41 cases (16%) were treated by a nonteaching team. Based on pairwise comparisons, the nonteaching team had older patients than the cardiology team, who had significantly more male patients than the teaching team. There were no significant differences in other demographics across teams (Table 1).
Table 1.
Patient characteristics of the entire cohort and according to care team
| Variable | Cardiology (N = 151) | Teaching (N = 60) | Nonteaching (N = 41) | Entire cohort (N = 252) | P value* |
|---|---|---|---|---|---|
| Age (years), mean ± SD | 64 ± 13 | 67 ± 13 | 72 ± 14 | 66 ± 14 | 0.01b |
| Female | 50 (33%) | 32 (53%) | 21 (51%) | 103 (41%) | 0.009a |
| Male | 101 (67%) | 28 (47%) | 20 (49%) | 149 (59%) | |
| Race | |||||
| Black | 16 (11%) | 11 (18%) | 5 (12%) | 32 (13%) | 0.63 |
| Hispanic | 18 (12%) | 9 (15%) | 4 (10%) | 31 (12%) | |
| Unknown | 3 (2%) | 0 (0%) | 0 | 3 (1%) | |
| White | 114 (76%) | 40 (67%) | 32 (78%) | 186 (74%) | |
| Comorbidity | |||||
| Diabetes mellitus | 63 (42%) | 27 (45%) | 21 (51%) | 111 (44%) | 0.55 |
| Hypertensione | 106 (70%) | 50 (83%) | 33 (80%) | 189 (75%) | 0.09 |
| Coronary artery diseasee | 83 (55%) | 26 (43%) | 22 (54%) | 131 (52%) | 0.30 |
| Congestive heart failure | 25 (17%) | 11 (18%) | 7 (17%) | 43 (17%) | 0.95 |
| Hyperlipidemiae | 92 (61%) | 35 (58%) | 22 (54%) | 149 (59%) | 0.70 |
| Sleep apnea | 4 (3%) | 4 (7%) | 3 (7%) | 11 (4%) | 0.20 |
| Current smoker | 44 (29%) | 19 (32%) | 7 (17%) | 70 (28%) | 0.23 |
| Current drug used | 3 (2%) | 1 (2%) | 0 | 4 (2%) | 1.00 |
| Inpatient death | 3 (2%) | 3 (5%) | 0 | 6 (2%) | 0.35 |
Significant difference between Cardiology vs. Teaching.
Significant difference between Cardiology vs. Nonteaching.
Significant difference between Teaching vs. Nonteaching.
Current drug use is defined as the use of any illegal drugs found in the history and physical.
Hypertension, hyperlipidemia, and coronary artery disease are defined as a history of these diagnoses in their medical chart.
The three teams differed significantly on EBM use (P < 0.0001). Based on Bonferroni-adjusted pairwise comparisons, cardiology had a significantly higher mean EBM score than the other teams. No significant differences were detected among the three teams in total history and physical score (0–25) or the 30-item total score (Table 2, Figure 1).
Table 2.
Score comparison according to care team
| Score (mean ± SD) | Cardiology (N = 151) | Teaching (N = 60) | Nonteaching (N = 41) | Entire cohort (N = 252) | P value |
|---|---|---|---|---|---|
| History and physical (25 items) | 17.7 ± 2.9 | 18.2 ± 2.6 | 17.2 ± 2.6 | 17.7 ± 2.8 | 0.20 |
| Evidence-based medicine (5 items) | 4.3 ± 1.0 | 3.8 ± 1.1 | 3.7 ± 0.9 | 4.1 ± 1.0 | <.0001a,b |
| Total (30 items) | 21.9 ± 3.4 | 22.0 ± 2.9 | 20.9 ± 2.8 | 21.8 ± 3.2 | 0.08 |
Significant difference between Cardiology vs. Teaching.
Significant difference between Cardiology vs. Nonteaching.
Significant difference between Teaching vs. Nonteaching.
Figure 1.
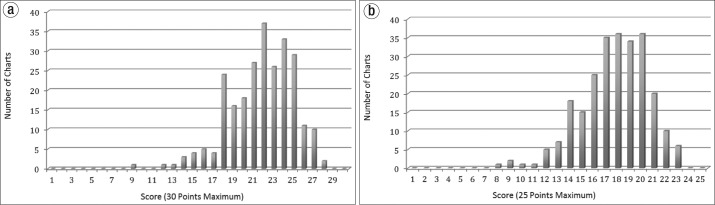
Distribution of history and physical scores (a) with and (b) without the evidence-based medicine score added.
Significant differences were also found on eight of 30 history and physical checklist items (Table 3). Teams differed significantly on documentation of the following items: type and duration of pain; whether the pain had ever occurred before; social history of activity; chest x-ray results; whether lipids, glucose, or A1C were mentioned; differential diagnosis; treatment of other comorbidities; and the use of glycoprotein IIb/IIIa inhibitors. No significant differences were detected across teams on other items. Social history of activity and differential diagnosis were found in only 45 subjects (18%), and those items were documented least often. Pulmonary exam was listed for all subjects in the cohort, and it was most often documented.
Table 3.
Inclusion of each item according to care team
| Variable | Cardiology (N = 151) | Teaching (N = 60) | Nonteaching (N = 41) | Entire cohort (N = 252) | P value |
|---|---|---|---|---|---|
| Chief complaint | 119 (79%) | 53 (88%) | 29 (71%) | 201 (80%) | 0.09 |
| Type and duration of pain | 128 (85%) | 46 (77%) | 28 (68%) | 202 (80%) | 0.05b |
| Associated symptoms | 124 (82%) | 51 (85%) | 33 (80%) | 208 (83%) | 0.82 |
| Previous occurrence | 78 (52%) | 22 (37%) | 10 (24%) | 110 (44%) | 0.004b |
| Past medical history | 149 (99%) | 59 (98%) | 40 (98%) | 248 (98%) | 0.79 |
| Recent lipids or A1C | 27 (18%) | 19 (32%) | 11 (27%) | 57 (23%) | 0.08 |
| Previous stress test or angiogram | 52 (34%) | 18 (30%) | 9 (22%) | 79 (31%) | 0.30 |
| Medications | 149 (99%) | 59 (98%) | 40 (98%) | 248 (98%) | 0.79 |
| Allergies | 145 (96%) | 55 (92%) | 40 (98%) | 240 (95%) | 0.41 |
| Family history of CAD | 88 (58%) | 34 (57%) | 22 (54%) | 144 (57%) | 0.87 |
| Other family history | 79 (52%) | 37 (62%) | 20 (49%) | 136 (54%) | 0.36 |
| Social history of any drugs | 145 (96%) | 54 (90%) | 38 (93%) | 237 (94%) | 0.23 |
| Social history of activity | 34 (23%) | 8 (13%) | 3 (7%) | 45 (18%) | 0.046a,b |
| Vitals documented | 147 (97%) | 60 (100%) | 40 (98%) | 247 (98%) | 0.55 |
| Cardiovascular exam | 150 (99%) | 60 (100%) | 41 (100%) | 251 (100%) | 1.00 |
| Pulmonary exam | 151 (100%) | 60 (100%) | 41 (100%) | 252 (100%) | – |
| Peripheral vascular exam | 115 (76%) | 41 (68%) | 28 (68%) | 184 (73%) | 0.39 |
| Cardiac enzymes | 146 (97%) | 57 (95%) | 41 (100%) | 244 (97%) | 0.45 |
| Electrocardiogram | 137 (91%) | 55 (92%) | 34 (83%) | 226 (90%) | 0.29 |
| Chest x-ray | 80 (53%) | 43 (72%) | 27 (66%) | 150 (60%) | 0.03a |
| Hemoglobin | 118 (78%) | 52 (87%) | 37 (90%) | 207 (82%) | 0.12 |
| Lipids, glucose, or A1C | 93 (62%) | 47 (78%) | 31 (76%) | 171 (68%) | 0.03a,b |
| Differential diagnosis | 19 (13%) | 14 (23%) | 12 (29%) | 45 (18%) | 0.02b |
| Other comorbidities and treatment | 120 (79%) | 59 (98%) | 34 (83%) | 213 (85%) | 0.003a,c |
| TIMI score done | 75 (50%) | 27 (45%) | 15 (37%) | 117 (46%) | 0.32 |
| Aspirin | 140 (93%) | 57 (95%) | 36 (88%) | 233 (92%) | 0.44 |
| Beta-blocker | 141 (93%) | 55 (92%) | 37 (90%) | 233 (92%) | 0.71 |
| Statin on discharge | 140 (93%) | 54 (90%) | 40 (98%) | 234 (93%) | 0.40 |
| Anticoagulation | 133 (88%) | 49 (82%) | 31 (76%) | 213 (85%) | 0.12 |
| Glycoprotein IIb/IIIa inhibitors | 90 (60%) | 14 (23%) | 9 (22%) | 113 (45%) | <.0001a,b |
Significant difference between Cardiology vs. Teaching.
Significant difference between Cardiology vs. Nonteaching.
Significant difference between Teaching vs. Nonteaching.
CAD indicates coronary artery disease; TIMI, Thrombolysis in Myocardial Infarction.
DISCUSSION
The Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the American College of Cardiology/American Heart Association Guidelines (CRUSADE) initiative is being conducted at multiple institutions across the country and deals with the care of patients with unstable angina and NSTEMI. Several studies that referenced the CRUSADE database analyzed the quality of medical record documentation and EBM use within their own institutions (4).
Dunlay et al utilized CRUSADE data to evaluate the quality of documentation, use of EBM, and mortality rates when comparing academic versus nonacademic hospitals, and cardiologists versus noncardiologists. Results showed that academic institutions and cardiologists scored higher than their counterparts, and these higher scores demonstrated better use of EBM and improved mortality rates (3). Patel et al (5) and O'Brien et al (6) found that academic institutions were better at following guidelines than nonacademic institutions, but they did not examine specific history and physical exam documentation. Bottorff et al (7) found that academic institutions were better at prescribing antiplatelet agents in the hospital than nonacademic institutions. Mehta et al (8) reported that once groups were in the CRUSADE trial and were notified of their own results, adherence to guidelines drastically improved. One study showed that institutions that were accredited by the Society of Chest Pain Centers had better outcomes due to an improved use of EBM (9). These studies inspired us to assess documentation and EBM use within our institution and compare outcomes across care teams.
Based upon the results of our study, cardiology teams performed better than teaching and nonteaching teams in giving glycoprotein IIb/IIIa inhibitors. However, teaching teams performed better in discussing the results of chest x-rays and evaluating other comorbidities in the assessment and plan. Findings also indicated that nonteaching teams scored lower than cardiology teams in discussing the symptom type and duration, if the symptoms had ever occurred before, and use of glycoprotein IIb/IIIa inhibitors. Nonteaching teams performed better than cardiology teams at documenting a differential diagnosis. The only difference noted between teaching and nonteaching teams was the discussion of other comorbidities in the assessment and plan.
The present study design differed from previous studies in that we compared different teams within the same hospital to determine if there were differences in quality of care and documentation. Also, while CRUSADE studies included patients with unstable angina, transient ST elevations, and NSTEMI who presented within 24 hours, our study included only NSTEMI whenever it presented.
Our results differed from other studies (10–12) in that we found no difference in medical record total scores or mortality among groups. Detecting differences in mortality between groups was difficult due to the small total number of deaths (N = 6). While other studies have found that teaching hospitals adhere to guidelines more frequently than nonteaching hospitals (5, 13, 14), our findings indicated there was no significant difference between our teaching and nonteaching teams in EBM use. Overall documentation did not seem to influence EBM use. The quality of documentation on medicine teams at our institution appears to be similar to that reported in the Dunlay study (3). In our facility, mean scores were 17.7/25 (70.8%) for the history and physical score and 21.8/30 (72.6%) for history and physical score with EBM added. Dunlay et al (3) reported a mean score of 12.5/20 (62.5%).
Our findings appear to mirror those of Dunlay et al (3) in that cardiology teams adhered to EBM guidelines significantly more than other teams. However, this difference appears to be due to the use of glycoprotein IIb/IIIa inhibitors, which was also found in another study (7). The reason may be lack of knowledge of this particular guideline or a discomfort in prescribing additional blood thinners. We also found that patients treated by the cardiology team were significantly younger and more often male than those served by noncardiology teams, which is similar to demographics seen in other studies (5, 11, 12).
Differences from the Dunlay study include that this retrospective study was performed at one site with a small population. Only NSTEMI patients confirmed with a troponin level >0.04 ng/mL were included in our study. The small sample size could inhibit our ability to detect differences among the teams. Another factor is that other teams in our facility had patients with NSTEMI, but these were excluded in order to compare only medicine teams. Our rating scale was based upon a scale used in the Dunlay study, but was not validated, which could be a limitation.
In an attempt to improve the overall quality of patient care, medicine teams have been notified of the results, and we will reevaluate the documentation and use of EBM across provider teams. Since the onset of the study, the use of certain medications upon admission to the hospital for NSTEMI patients has changed. The frequency of glycoprotein IIb/IIIa inhibitor use decreased during the study period, and it will be removed from future checklists. We believe this may be related to results of the ACUITY Timing trial (15) and EARLY ACS study (16), as well as the increasing use of bivalirudin in the catheterization lab. Most NSTEMI patients at our institution undergo an early invasive strategy and now receive clopidogrel, ticagrelor, or prasugrel as a second antiplatelet agent. Use of these medications will be tracked in future studies. To enhance generalizability of findings, we hope to collaborate with other teaching institutions.
Our quality improvement study demonstrated that cardiology teams at Scott & White/Texas A&M adhered to EBM guidelines more frequently than other medicine teams. Statistically significant differences in mortality rates or documentation were not found. This study appears to be only the second to examine the influence of documentation on patient care in myocardial infarction (3). A small improvement in mortality in a disease this common can translate to a large effect. Studies with an increased sample size may find a difference related to documentation alone. Recent events in our institution have included the integration of a new electronic health record and the merger between Scott & White and Baylor Health Care Systems. These two changes will allow for a larger study to be performed and likely an intervention including a standardized history and physical with order set to ensure appropriate use of EBM.
References
- 1.Cox JL, Zitner D, Courtney KD, MacDonald DL, Paterson G, Cochrane B, Mathers J, Merry H, Flowerdew G, Johnstone DE. Undocumented patient information: an impediment to quality of care. Am J Med. 2003;114(3):211–216. doi: 10.1016/s0002-9343(02)01481-x. [DOI] [PubMed] [Google Scholar]
- 2.Roe MT, Halabi AR, Mehta RH, Chen AY, Newby LK, Harrington RA, Smith SC, Jr, Ohman EM, Gibler WB, Peterson ED. Documented traditional cardiovascular risk factors and mortality in non-ST-segment elevation myocardial infarction. Am Heart J. 2007;153(4):507–514. doi: 10.1016/j.ahj.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 3.Dunlay SM, Alexander KP, Melloni C, Kraschnewski JL, Liang L, Gibler WB, Roe MT, Ohman EM, Peterson ED. Medical records and quality of care in acute coronary syndromes: results from CRUSADE. Arch Intern Med. 2008;168(15):1692–1698. doi: 10.1001/archinte.168.15.1692. [DOI] [PubMed] [Google Scholar]
- 4.Ohman EM, Roe MT, Smith SC, Jr, Brindis RG, Christenson RH, Harrington RA, Gibler WB, Peterson ED. CRUSADE Investigators Care of non-ST-segment elevation patients: insights from the CRUSADE national quality improvement initiative. Am Heart J. 2004;148(5 Suppl):S34–S39. doi: 10.1016/j.ahj.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Patel MR, Chen AY, Roe MT, Ohman EM, Newby LK, Harrington RA, Smith SC, Jr, Gibler WB, Calvin JE, Peterson ED. A comparison of acute coronary syndrome care at academic and nonacademic hospitals. Am J Med. 2007;120(1):40–46. doi: 10.1016/j.amjmed.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 6.O'Brien E, Subherwal S, Roe MT, Holmes DN, Thomas L, Alexander KP, Wang TY, Peterson ED. Do patients treated at academic hospitals have better longitudinal outcomes after admission for non-ST-elevation myocardial infarction? Am Heart J. 2014;167(5):762–769. doi: 10.1016/j.ahj.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Bottorff MB, Nutescu EA, Spinler S. Antiplatelet therapy in patients with unstable angina and non-ST-segment-elevation myocardial infarction: findings from the CRUSADE national quality improvement initiative. Pharmacotherapy. 2007;27(8):1145–1162. doi: 10.1592/phco.27.8.1145. [DOI] [PubMed] [Google Scholar]
- 8.Mehta RH, Roe MT, Chen AY, Lytle BL, Pollack CV, Jr, Brindis RG, Smith SC, Jr, Harrington RA, Fintel D, Fraulo ES, Califf RM, Gibler WB, Ohman EM, Peterson ED. Recent trends in the care of patients with non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE initiative. Arch Intern Med. 2006;166(18):2027–2034. doi: 10.1001/archinte.166.18.2027. [DOI] [PubMed] [Google Scholar]
- 9.Chandra A, Glickman SW, Ou FS, Peacock WF, McCord JK, Cairns CB, Peterson ED, Ohman EM, Gibler WB, Roe MT. An analysis of the Association of Society of Chest Pain Centers Accreditation to American College of Cardiology/American Heart Association non-ST-segment elevation myocardial infarction guideline adherence. Ann Emerg Med. 2009;54(1):17–25. doi: 10.1016/j.annemergmed.2009.01.025. [DOI] [PubMed] [Google Scholar]
- 10.Allison JJ, Kiefe CI, Weissman NW, Person SD, Rousculp M, Canto JG, Bae S, Williams OD, Farmer R, Centor RM. Relationship of hospital teaching status with quality of care and mortality for Medicare patients with acute MI. JAMA. 2000;284(10):1256–1262. doi: 10.1001/jama.284.10.1256. [DOI] [PubMed] [Google Scholar]
- 11.Casale PN, Jones JL, Wolf FE, Pei Y, Eby LM. Patients treated by cardiologists have a lower in-hospital mortality for acute myocardial infarction. J Am Coll Cardiol. 1998;32(4):885–889. doi: 10.1016/s0735-1097(98)00325-8. [DOI] [PubMed] [Google Scholar]
- 12.Jollis JG, DeLong ER, Peterson ED, Muhlbaier LH, Fortin DF, Califf RM, Mark DB. Outcome of acute myocardial infarction according to the specialty of the admitting physician. N Engl J Med. 1996;335(25):1880–1887. doi: 10.1056/NEJM199612193352505. [DOI] [PubMed] [Google Scholar]
- 13.Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL, Brindis RG, Smith SC, Jr, Pollack CV, Jr, Newby LK, Harrington RA, Gibler WB, Ohman EM. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;295(16):1912–1920. doi: 10.1001/jama.295.16.1912. [DOI] [PubMed] [Google Scholar]
- 14.Tricoci P, Peterson ED, Roe MT. CRUSADE Quality Improvement Initiative Patterns of guideline adherence and care delivery for patients with unstable angina and non-ST-segment elevation myocardial infarction (from the CRUSADE Quality Improvement Initiative) Am J Cardiol. 2006;98(12A):30Q–35Q. doi: 10.1016/j.amjcard.2006.09.022. [DOI] [PubMed] [Google Scholar]
- 15.Stone GW, Bertrand ME, Moses JW, Ohman EM, Lincoff AM, Ware JH, Pocock SJ, McLaurin BT, Cox DA, Jafar MZ, Chandna H, Hartmann F, Leisch F, Strasser RH, Desaga M, Stuckey TD, Zelman RB, Lieber IH, Cohen DJ, Mehran R, White HD. ACUITY Investigators Routine upstream initiation vs deferred selective use of glycoprotein IIb/IIIa inhibitors in acute coronary syndromes: the ACUITY Timing trial. JAMA. 2007;297(6):591–602. doi: 10.1001/jama.297.6.591. [DOI] [PubMed] [Google Scholar]
- 16.Giugliano RP, White JA, Bode C, Armstrong PW, Montalescot G, Lewis BS, van 't Hof A, Berdan LG, Lee KL, Strony JT, Hildemann S, Veltri E, Van de Werf F, Braunwald E, Harrington RA, Califf RM, Newby LK. EARLY ACS Investigators Early versus delayed, provisional eptifibatide in acute coronary syndromes. N Engl J Med. 2009;360(21):2176–2190. doi: 10.1056/NEJMoa0901316. [DOI] [PubMed] [Google Scholar]


