Abstract
Nail-patella syndrome is a rare disorder characterized classically by the tetrad of nail hypoplasia or aplasia, aplastic or hypoplastic patellae, elbow dysplasia, and the presence of iliac horns. Iliac horns are considered pathognomonic, and the presence of hypoplastic or aplastic patellae in conjunction with nail abnormalities is a cardinal feature of diagnosis. Elbow dysplasia is present in most cases and can exhibit features typical of the syndrome. Herein we present the radiographic findings of the elbows, knees, and pelvis of a woman with nail-patella syndrome.
Nail-patella syndrome (NPS), a hereditary disorder that occurs in approximately 1 in 50,000 newborns (1), is known by many other names, including hereditary onycho-osteodysplasia (HOOD), Turner-Keiser syndrome, and Fong disease (2). It is characterized by nail hypoplasia or aplasia, aplastic or hypoplastic patellae, elbow dysplasia, and the presence of iliac horns (2). The earliest description of a nail dysplasia being associated with knee and elbow dysplasia dates back to 1820 by Chatelain (3). The familial and hereditary nature of the disorder was recognized by Pye-Smith and Little in 1883 and 1897, respectively (4). A few years after Fong described the incidental finding of “iliac horns” in 1946 during a routine pyelogram, they became associated with the syndrome and are now considered pathognomonic (4, 5). Identifying the common radiographic manifestations of the pelvis, knees, and elbows can aid in establishing the diagnosis of NPS.
CASE STUDY
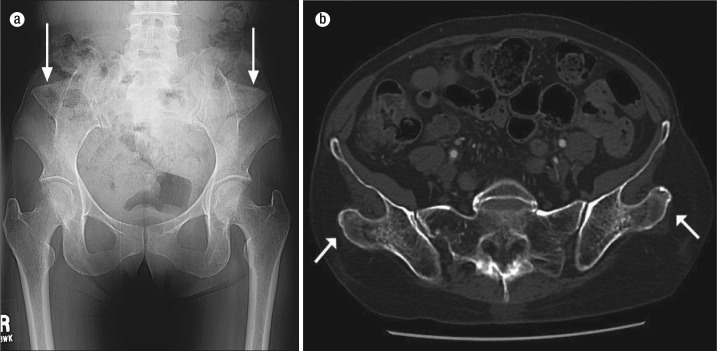
A 70-year-old woman presented to the emergency department complaining of hip pain. An anteroposterior radiograph of the pelvis was obtained and demonstrated no acute abnormality and only mild osteoarthritic degenerative changes of the hips bilaterally. Incidentally, there were bilateral, triangular osseous excrescences extending from the posterior aspect of the ilia (Figure 1a). Review of the patient's prior imaging studies revealed multiple musculoskeletal studies in addition to computed tomography (CT) of the abdomen and pelvis. CT of the abdomen and pelvis showed the bilateral posterior iliac osseous excrescences to involve the origin of the gluteus medius muscles (Figure 1b). An anteroposterior view of the bilateral femurs demonstrated both patellae to be hypoplastic (Figure 2). Anteroposterior and lateral radiographs of the right elbow showed an abnormal configuration of the capitulum, lateral epicondyle, and radial head as well as posterior inferior dislocation of the radial head (Figure 3). Radiographic features of the left elbow were similar though less pronounced, and the left radial head was also posteriorly and inferiorly dislocated. Review of the patient's records revealed a standing diagnosis of NPS.
Figure 1.
Imaging of the pelvis. (a) Radiograph of the anteroposterior pelvis demonstrates the presence of bilateral triangular osseous excrescences from the posterior aspect of the ilia, known as iliac horns (arrows). (b) CT of the pelvis shows the bilateral iliac osseous excrescences (arrows) to emanate from the posterior body of the ilia at the origin of the gluteus medius muscles.
Figure 2.
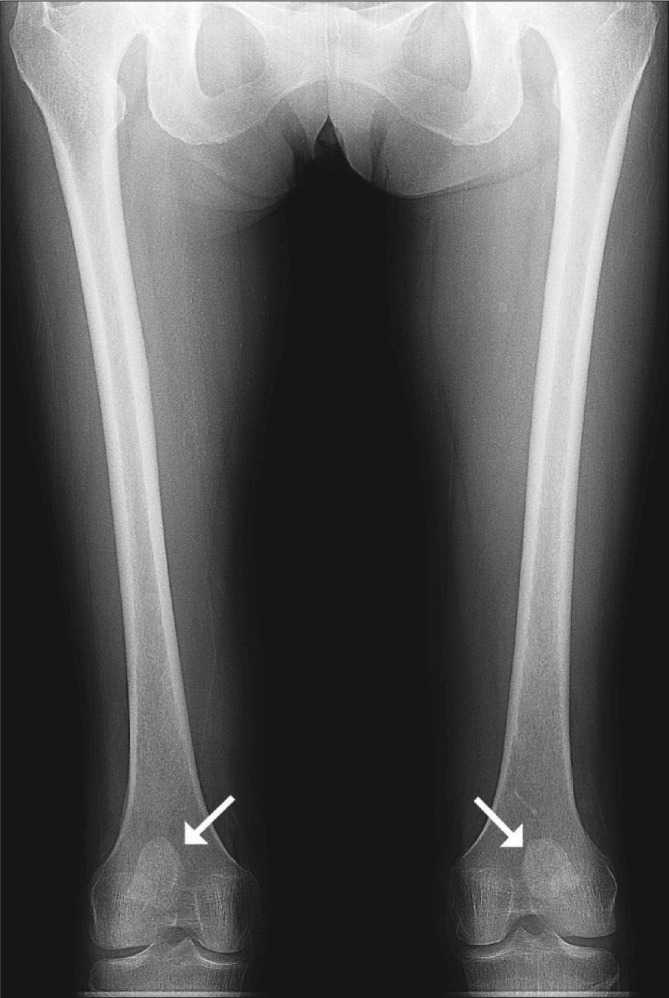
Anteroposterior radiograph of the bilateral femurs shows both patellae to be hypoplastic (arrows).
Figure 3.
Radiograph of the right elbow. (a) Anteroposterior radiograph demonstrates dysplasia of the radial head (arrow), capitulum (asterisk), and lateral epicondyle (arrowhead). (b) Lateral radiograph shows the radial head (arrow) to be inferiorly and posteriorly dislocated.
DISCUSSION
NPS exhibits full genetic penetrance but an unpredictable degree of expression, even within families (1, 6). No clinical diagnostic criteria exist for NPS; however, a combination of clinical and imaging features seen with this condition are characteristic (6). Genetic testing can be performed if findings are ambiguous (6). NPS results from loss of function mutations of transcription factor LMX1B located on chromosome 9, which is a member of the LIM-homeodomain family of transcription factors involved in ventral-dorsal body-pattern formation during development (7).
Nail dysplasia and patellar aplasia or hypoplasia are cardinal features in the diagnosis of NPS (4). Nail anomalies predominantly involve the fingernails, with the thumbs most severely affected. The toenails are rarely involved and the presence of triangular nail lunulae is considered pathognomonic (4). The nails may be absent, hypoplastic, or dystrophic, with some of the various nail dysplasia including horizontal or longitudinal ridging, pitting, or the presence of a longitudinal cleft that separates them in half.
Patellar abnormalities are present in >90% of cases and include aplasia or, more frequently, patellar hypoplasia (4). Recurrent superolateral subluxation or dislocation is common. Even when not displaced, the hypoplastic patellae tend to be positioned more superolateral than normal (6). There can also be hypoplasia of the lateral femoral condyle resulting in a genu valgus deformity.
Elbow dysplasia is also frequently encountered in NPS, having been described in >90% of patients (4). Most frequently the radial heads, lateral epicondyles, and capitula are dysplastic with recurrent, typically posterolateral, displacement of the radial heads occurring in 61% of patients (4). Pterygia (webbing) may also occur across the elbow.
Iliac horns, which are pathognomonic for NPS, only occur in 70% to 80% of patients (2, 5). They are most often bilateral, conical osseous excrescences that typically project dorsolaterally from the posterior ilia and serve as the origin of the gluteus medius muscles (5). On physical exam, these processes may be palpable, although they are typically asymptomatic and have no effect on gait (4). They can be identified as early as the third trimester on a fetal ultrasound (6).
Other frequently encountered orthopedic features of NPS that do not contribute to the diagnosis are shoulder girdle dysplasia, short stature, talipes equinovarus (club foot), calcaneo-valgus feet, dislocation of the hips, Madelung's deformity, and large joint contractures.
Besides physical manifestations, there is also a strong association with open-angle glaucoma and progressive nephropathy (7). Nephropathy is reported to be present in 30% to 60% of patients, with progression to nephrotic syndrome in 20% and renal failure requiring dialysis and/or transplant in approximately 10% (8). Open-angle glaucoma occurs in 10% and ocular hypertension in 7% (4). There is no cure for NPS, and treatment is directed towards addressing the various orthopedic and nonorthopedic manifestations of the disorder.
References
- 1.Levy M, Feingold J. Estimating prevalence in single-gene kidney diseases progressing to renal failure. Kidney Int. 2000;58(3):925–943. doi: 10.1046/j.1523-1755.2000.00250.x. [DOI] [PubMed] [Google Scholar]
- 2.Mankin H. Nail-patella syndrome: hereditary onycho-osteodysplasia. In: Mankin H, editor. Pathophysiology of Orthopaedic Diseases. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2009. pp. 191–196. [Google Scholar]
- 3.Thompson EA, Walker ET, Weens HS. Iliac horns: an osseous manifestation of hereditary arthrodysplasia associated with dystrophy of the fingernails. Radiology. 1949;53(1):88–92. doi: 10.1148/53.1.88. [DOI] [PubMed] [Google Scholar]
- 4.Bongers EM, Gubler MC, Knoers NV. Nail-patella syndrome. Overview on clinical and molecular findings. Pediatr Nephrol. 2002;17(9):703–712. doi: 10.1007/s00467-002-0911-5. [DOI] [PubMed] [Google Scholar]
- 5.Fong EE. Iliac horns (symmetrical bilateral central posterior iliac processes) Radiology. 1946;47(5):517. doi: 10.1148/47.5.517. [DOI] [PubMed] [Google Scholar]
- 6.Sweeney E, Hoover-Fong JE, McIntosh I. Nail-patella syndrome. 2003 [updated 2014 Nov 13] In: Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJH, Bird TD, Dolan CR, Fong CT, Smith RJH, Stephens K, editors. GeneReviews® [Internet] Seattle, WA: University of Washington; 1993–2015. Available at http://www.ncbi.nlm.nih.gov/books/NBK1132/ [PubMed] [Google Scholar]
- 7.McIntosh I, Dunston JA, Liu L, Hoover-Fong JE, Sweeney E. Nail patella syndrome revisited: 50 years after linkage. Ann Hum Genet. 2005;69(Pt 4):349–363. doi: 10.1111/j.1529-8817.2005.00191.x. [DOI] [PubMed] [Google Scholar]
- 8.Granata A, Nori G, Ravazzolo R, Marini M, Castellino S, Sicurezza E, Fiore CE, Mignani R. Nail-patella syndrome and renal involvement. Description of three cases and literature review. Clin Nephrol. 2008;69(5):377–382. doi: 10.5414/cnp69377. [DOI] [PubMed] [Google Scholar]