Abstract
Aim:
Familial Mediterranean fever (FMF) and inflammatory bowel disease (IBD) carry similar clinical and biological properties. Both are characterized with chronic inflammation attacks and neutrophil migration and impaired apoptosis mechanism are present in the areas of damage in both conditions. In our study, we aimed to determine the frequency of association of FMF in patients with IBD, to compare the demographic, clinical, laboratory and treatment response properties in these patients with the ones in other IBD patients and to determine association of FMF especially in treatment-resistant patients.
Material and Methods:
Fifty-three patients who were being followed up with a diagnosis of IBD aged between 0 and 18 years were included in the study. The patient group included the patients who were diagnosed with IBD according to clinical, serological, endoscopic and histopathological criteria, who were being followed up and whose therapies were continuing. Genetic analysis in terms of MEFV gene mutations was performed in all patients with a diagnosis of IBD. Acute phase reactants, complete blood count, immunoglobulin levels, stool analysis, “perinuclear anti-neutrophil cytoplasmic antibodies” (pANCA) and “anti-Saccharomyces cerevisiae antibodies” (ASCA) were studied at the time of diagnosis. The diagnosis of FMF was made according to detailed history, physical examination findings, laboratory tests and the results of genetic analyses in terms of MEFV gene mutations in accordance with the criteria defined in 2009.
Results:
We found that FMF accompanied in 14 (26.4%) of the patients who had a diagnosis of IBD. 3 of these 14 patients in whom FMF accompanied were being followed up with a diagnosis of Crohn disease and 11 were being followed up with a diagnosis of ulcerative colitis. All of these patients had MEFV gene mutation. These mutations included M694V (50%), K695R (21.4%), M680I (14.3%) and R202Q (14.3%) in order of frequency. When the laboratory data were compared between the patients who had a diagnosis of IBD alone and who had a diagnosis of IBD plus FMF, it was observed that the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) values were statistically significantly higher in the IBD+FMF group.
Conclusions:
FMF is a common condition in the Turkish population and M694V mutation is found most commonly. In our study, this status did not change in cases where FMF accompanied IBD, but K695R mutation was found more frequently compared to FMF alone. We think that it should be kept in mind that other inflammatory conditions including mainly FMF may accompany IBD, if a case of IBD does not have an expected course or is resistant to treatment.
Keywords: Familial Mediterranean fever, inflammatory bowel disease, MEFV
Introduction
Three main diseases including Crohn disease (CD), ulcerative colitis (UC) and indeterminate colitis (IC) constitute inflammatory bowel diseases (IBD) which are a chronic and repetetive disease group. The differentiation of these three diseases is made according to the differences in clinical, endoscopic, radiological and histopathological findings (1). Inflammation which may involve any part from the mouth to the anus and all wall layers of the intestines without continuance in the gastrointestinal system is found in Crohn disease, while ulcerative colitis is limited to the colonic mucosa, its distribution shows continuance, involves the rectum and shows a variable invasion from the rectum proximally (2).
Familial Mediteranean fever (FMF) is an inflammatory disease which occurs as a result of uncontrolled inflammatory response. The frequency of FMF in the Turkish population is higher compared to the Western populations. The disease is characterized with acute fever attacks and inflammatory abdominal, chest and joint pain. MEVF gene encoding pyrin which regulates neutrophil activity is the gene responsible of FMF and is found on chromosome 16p13 (3–5). In many studies, pyrin has been shown to have antiinflammatory property. However, all functions of pyrin are still not known completely (6, 7).
Both epidemiological and clinical data suggest that MEFV may be a potential IBD gene. Familial mediteranean fever and IBD carry very similar clinical and biological properties. Both are characterized with chronic inflammation attacks and neutrophil migration and disrupted apopitosis mechanism are present in the areas of damage in both conditions (8, 9). Other inflammatory diseases including IBD accompany FMF with a gradually increasing frequency. In addition, the frequency of other inflammatory diseases (including juvenile rheumatoid arthritis) increases in conditions where IBD accompanies FMF (10–12). The fact that MEFV gene mutations are found with an increasing frequency in these inflammatory diseases supports this (13). In previous studies, it was found that MEFV gene mutations were observed with a higher rate in patients with a diagnosis of IBD compared to the population and molecular analysis of the MEFV gene may be considerably beneficial in terms of clinical practices (13, 14).
In our study, it was aimed to investigate the frequency of accompaniment of FMF in patients with a diagnosis of IBD, to compare the demographic, clinical, laboratory properties and treatment response of these patients with other patients with a diagnosis of IBD and to investigate if there was an association of FMF in patients who were resistant to treatment.
Material and Methods
Patients and definitions
Fifty-three patients between the ages of 0 and 18 years were included in the study after obtaining consent from the patients and families. The patient group included the patients who were diagnosed with IBD according to clinical, serological, endoscopic and histopathological criteria, who were being followed up and whose therapies were continuing. The files of the patients included in the study were examined and birth dates, dates and findings of esophagoduodenoscopy/colonoscopy, laboratory findings at the time of the first diagnosis and during the follow-up, complaints and times of complaints, current and previous therapies and presence of accompanying morbidity were investigated. Familial history of IBD, FMF and autoimmune disease was interrogated and recorded.
Fifty-three patients who were being followed up with a diagnosis of IBD and who were being treated were evaluated in terms of presence of FMF by a pediatric rheumatologist according to the FMF criteria established in 2009 (15). The diagnosis of FMF was made in accordance with with the criteria mentioned above considering detailed history, physical examination findings, laboratory findings and genetic analysis results in terms of MEFV gene mutations.
Laboratory tests
Genetic analysis was performed in all subjects with a diagnosis of IBD in terms of MEFV gene mutations. At the time of diagnosis, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), components of complete blood count (CBC) (hemoglobin, hematocrit, white blood cells, platalets), immunoglobulin levels, fecal tests results (parasites, amoeba, culture), total protein and albumin, “perinuclear anti-neutrophil cytoplasmic antibodies” (pANCA), “anti-Saccharomyces cerevisiae antibodies” (ASCA) results were examined. In the subjects who were in the attack period, fecal clostridium difficile toxin A and B, blood cytomegalovirus IgM and DNA analyses were performed and recorded.
Invasive procedures
Colonoscopy under sedation was performed in all subjects for a diagnosis of IBD. Multiple biopsy samples were taken for histopathological examination during the procedure. Following examination of the biopsy samples by the pathologist the subjects who were diagnosed with IBD were included in the study. In addition, esophagoduodenoscopy was also performed in all subjects who were diagnosed with IBD and the findings were recorded.
Statistical analyses
Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) 16.0 was used for analysis of the data. Independent statistical variables were calculated using Mann-Whitney U test and dependent statistical variables were calculated using, Wilcoxon test. Variables with anormal distribution were expressed as mean ± standard deviation. Variables which did not show a normal distribution were expressed as median (the lowest-the highest) values. The demographic and antropometric measurements of the patient group were done using ANOVA and chi-square tests. The data which did not show a normal distribution were analyzed using Kruskall-Wallis test. Laboratory variables were analyzed using ANOVA and Kruskall-Wallis tests. Chi-square test was used for comparison of the data. A p value of <0,05 was considered statistically significant.
Patient informed consent and ethics committee approval
Verbal and written informed consent was obtained from all the subjects included in the study and from their parents. After the study was completed, the study result of each subject was reported to his/her own parents. Ethics committee approval for the study was given by İstanbul University Cerrahpaşa Medical Faculty Clinical Research Ethics Committee with the article number of 13418 and with the date of 04.14.2012.
Results
The mean age of 53 patients with a diagnosis of IBD whom we included in the study was 105.07±52.2 months. The demographic properties of the subjects are presented in Table 1.
Table 1.
Demographic properties of the patients with inflammatory bowel disease
| Ulcerative colitis (n=35) | Crohn disease (n=18) | Total (n=53) | |
|---|---|---|---|
| Mean age (months) | 111.82±50.4 | 82.12±40.2 | 105.07±52.2 |
| Mean age at the begining of complaints | 76.89±36.42 | 50.42±24.8 | 67.89±33.7 |
| Gender (F/M) | 22/13 | 4/14 | 19/34 |
| Member of family with IBD (%) | 11.4 | 33.3 | 18.9 |
| Consanguineous marriage (%) | 34.3 | 44.4 | 37.7 |
IBD: inflammatory bowel disease; F: female; M: male
We found that FMF accompanied in 14 (26.4%) of our patients who were being followed up with a diagnosis of IBD. MEFV gene mutation was present in all of these 14 subjects and these mutations included homozygous p.M694V (50%), heterozygous p.K695R and p.M694V (14.3%), homozygous p.K695R (7.14%), homozygous p.M680I (7.14%), heterozygous p.M680I and p.M694V (7.14%), homozygous p.R202Q (7.14%) and heterozygous p.R202Q and p.M694V (7.14%) with order of frequency (Figure 1).
Figure 1.
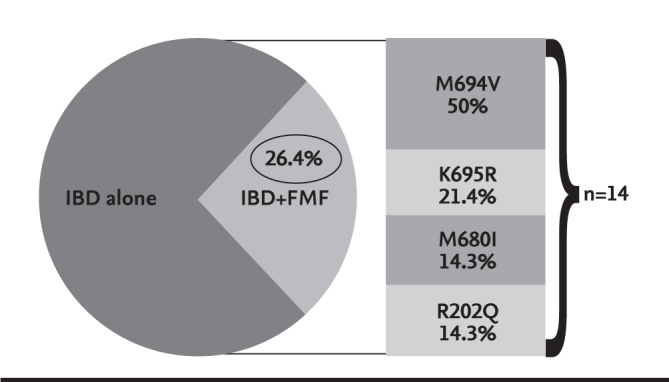
FMF mutations found when FMF accompanied IBD
IBD: inflammatory bowel disease; FMF: familial Mediterranean fever
In our study, three of 14 subjects in whom FMF accompanied IBD was being followed up with a diagnosis of Crohn disease (CD) and 11 were being followed up with a diagnosis of ulcerative colitis (UC). The age at the time of diagnosis was found to be 78.07±14.3 months in the group in which FMF accompanied IBD and 64.230±12.8 months in the group in which FMF did not accompany IBD. The most frequent complaints in the group in which FMF did not accompany IBD included diarrhea, bleeding and abdominal pain in order of frequency, while diarrhea, abdominal pain and bleeding were the most common complaints in order of frequency in the group in which FMF accompanied IBD (Table 2). Again, the most commonly observed complaints in the group in which FMF did not accompany UC included diarrhea, abdominal pain and weight loss in order of frequency, while abdominal pain, diarrhea and weight loss were the most common complaints in order of frequency in the group in which FMF accompanied UC (Table 3).
Table 2.
Comparison of the complaints in UC alone and in UC-FMF association
| UC alone (n=24) | UC+FMF (n=11) | |
|---|---|---|
| Diarrhea, n (%) | 21 (87.5) | 9 (81.8) |
| Abdominal pain, n (%) | 12 (50) | 7 (63.6) |
| Bleeding, n (%) | 21 (87.5) | 6 (54.5) |
UC: ulcerative colitis; FMF: familial Mediterranean fever
Table 3.
Comparison of the complaints in CD alone and in CD-FMF association
| CD alone (n=15) | CD+FMF (n=3) | |
|---|---|---|
| Diarrhea, n (%) | 15 (100) | 3 (100) |
| Abdominal pain, n (%) | 12 (80) | 3 (100) |
| Weight loss, n (%) | 10 (66.7) | 2 (66.7) |
CD: Crohn disease; FMF: familial Mediterranean fever
When the laboratory data of the patients with a diagnosis of IBD solely and the patients with a diagnosis of IBD+FMF were compared, it was observed that ESR and CRP values were statistically significantly higher in the IBD+FMF group. Again, it was observed that both ASCA and P-ANCA were found to be positive with a higher rate when the two conditions accompanied each other (Table 4).
Table 4.
Comparison of the tests in IBD alone and IBD+FMF association
| IBD alone (n=39) | IBD+FMF (n=14) | p | |
|---|---|---|---|
| WBC (count/mm3) | 12 636±6 315 | 8 177±4 080 | 0.025 |
| Hb (g/dL) | 10.44±5.2 | 10.85±5.4 | 0.820 |
| Platelets (count/mm3) | 348 845±174 420 | 294 928±147 450 | 0.07 |
| ESR (mm/h) | 38.03±18.62 | 54±28.2 | 0.04 |
| CRP (mg/dL) | 2.15±1.06 | 3.71±1.85 | 0.04 |
| pANCA (+) n (%) | 15 (38.5) | 14 (64.3) | 0.025 |
| ASCA (+) n (%) | 9 (23.1) | 5 (35.7) | 0.04 |
A p value of <0.05 was considered significant according to Mann-Whitney U test.
Values which showed a normal distribution were expressed as mean±standard deviation
Values which did not show a normal distribution were expressed as median; the lowesr-the highest value.
FMF: familial Mediterranean fever; IBD: inflammatory bowel diseases
Discussion
Since both epidemiological and clinical data suggest that MEFV may be a potential IBD gene, FMF and IBD carry very similar clinical and biological properties and IBD frequently accompanies FMF (16). FMF accompanied IBD in 14 (26.4%) of our patients. In another study in which we investigated the prevalence of IBD in patients with FMF, we found M694V mutation in 5 (41.7%) of 12 patients with IBD, M680I mutation in 3 (25%), K695R mutation in 3 (25%) and E148Q mutation in 1 (8.3%) (17). When compared with this study, it was found that M694V was the most common mutation when FMF accompanied IBD. K695R mutation was observed to be found with a higher rate compared to the past.
In our study, three (21.4%) of 14 subjects in whom FMF accompanied IBD was being followed up with a diagnosis CD and 11 (78.6%) were being followed up with a diagnosis of UC. Association of Crohn disease and FMF has been elucidated better with genetic studies conducted in years and the mutations found. In a study in which 33 patients with IBD (16 UC, 14 CD and 3 indeterminate colitis), a diagnosis of FMF was made in 21.2% of the patients and it was found that FMF accompanied CD with a higher rate (28.6%) (16).
Although it appeared that the same was not true for UC, UC was found with the highest rate when IBD accompanied FMF both in the study we conducted in 2012 (17) and in the study of Giaglis et al. (14). The fact that we found that UC accompanied FMF with a high rate of 78.6% in our study supports these points.
The age at the time of diagnosis was found to be 78.07±14.3 months when FMF accompanied IBD and 64.230±12.8 months when FMF did not accompany IBD. Considering that both conditions are characterized with attacks of inflammation, we think that accompaniment of FMF may delay the diagnosis of IBD because of similar clinical properties.
In our study, abdominal pain was the prominent complaint in presence of association of FMF in both UC and CD. Considering that the most common complaint in FMF is abdominal pain associated with attacks, this result is compatible with this.
In all of the 14 patients in whom FMF accompanied IBD, ESR values at the time of diagnosis were above 20 mm/h, while ESR was high in 20 (51.3%) of 39 patients in whom FMF did not accompany IBD. CRP was found to be higher than normal in 13 (92.9%) of 14 patients in whom FMF accompanied IBD, while CRP was found to be high in 33 (84.6%) of 39 patients in whom FMF did not accompany IBD. CRP and ESR are good markers in defining exacerbations and follow-up of treatment response in both IBD and FMF. In cases where both conditions accompany each other, this values are found to be higher.
p-ANCA positivity was present at the time of diagnosis in 15 (38.5%) of 39 patients in whom FMF did not accompany IBD, while p-ANCA was found to be positive in 9 (64.3%) of 14 patients in whom FMF accomapnied IBD. Again, ASCA was found to be positive in 9 (23.1%) of 39 patients in whom FMF did not accompany IBD, while it was found to be positive in 6 (35.7%) of 14 patients in whom FMF accompanied IBD. We found that both p-ANCA and ASCA values were higher in the group in which FMF accompanied IBD compared to the group in which FMF did not accompany IBD. Comparing with the data of our study we conducted in 2012 in which we investigated the frequency of IBD in FMF (17), we think that these high values of both p-ANCA and ASCA in case of accompaniment of FMF to IBD are compatible.
FMF is a common condition in the Turkish population and M694V mutation is found with the highest rate. Altough this status did not change when FMF accompanied IBD in our study, K695R mutation was found with a higher rate compared to the status of presence of only FMF. In many studies, the course of IBD appeared as CD in case of association of IBD and FMF, whereas the course of IBD appeared as UC with a higher rate in our study. We think that it should be kept in mind that other inflammatory diseases may accompany IBD including mainly FMF in cases where the disease has an unexpected course in patients who are being followed up with a diagnosis of IBD and when there is resistance to treatment.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of İstanbul Üniversity Cerrahpaşa Faculty of Medicine, Clinical Research Ethics Committee (14.04.2012, Approval Number: 13418).
Informed Consent: Written informed consent was obtained from the parents of the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - Ö.F.B., T.E.; Design - Ö.F.B., T.E., T.K., F.Ç.Ç.; Supervision - T.E., T.K., F.Ç.Ç., Ö.K.; Funding - Ö.F.B., D.G.; Materials - Ö.F.B., D.G.; Data Collection and/or Processing -Ö.F.B.; Analysis and/or Interpretation - Ö.F.B., T.E.; Literature Review - Ö.F.B., D.G.; Writer - Ö.F.B.; Critical Review - T.E., T.K., F.Ç.Ç, Ö.K.; Other - E.E.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Bamias G, Nyce MR, De La Rue SA, Cominelli F. New concepts in the pathophysiology of inflammatory bowel disease. Ann Intern Med. 2005;143:895–904. doi: 10.7326/0003-4819-143-12-200512200-00007. http://dx.doi.org/10.7326/0003-4819-143-12-200512200-00007. [DOI] [PubMed] [Google Scholar]
- 2.Potzi R, Walgrm M, Lochs H, Holzner H, Gangl A. Diagnostic significance of endoscopic biopsy in Crohn’ s disease. Endoscopy. 1989;21:60–2. doi: 10.1055/s-2007-1012901. http://dx.doi.org/10.1055/s-2007-1012901. [DOI] [PubMed] [Google Scholar]
- 3.Livneh A, Langevitz P, Zemer D, et al. Criteria for the diagnosis of familial Mediterranean fever. Arthritis Rheum. 1997;40:1879–85. doi: 10.1002/art.1780401023. http://dx.doi.org/10.1002/art.1780401023. [DOI] [PubMed] [Google Scholar]
- 4.Savic S, Dickie LJ, Battellino M, McDermott MF. Familial Mediterranean fever and related periodic fever syndromes/autoinflammatory diseases. Curr Opin Pheumatol. 2012;24:103–12. doi: 10.1097/BOR.0b013e32834dd2d5. http://dx.doi.org/10.1097/BOR.0b013e32834dd2d5. [DOI] [PubMed] [Google Scholar]
- 5.Lachmann HJ, Sengül B, Yavuzs, et al. Clinical and subclinical inflammation in patients with familial Mediterranean fever and in heterozygous carriers of MEFV mutations. Rheumatology (Oxford) 2006;45:746–50. doi: 10.1093/rheumatology/kei279. http://dx.doi.org/10.1093/rheumatology/kei279. [DOI] [PubMed] [Google Scholar]
- 6.Chae JJ, Komarow HD, Cheng J, et al. Targeted disruption of pyrin, the FMF protein, causes heightened sensitivity to endotoxin and a defect in macrophage apoptosis. Mol Cell. 2003;11:591–604. doi: 10.1016/s1097-2765(03)00056-x. http://dx.doi.org/10.1016/S1097-2765(03)00056-X. [DOI] [PubMed] [Google Scholar]
- 7.McDermott MF, Aksentijevich I. The autoinflammatory syndromes. Curr Opin Allergy Clin Immunol. 2002;2:511–6. doi: 10.1097/00130832-200212000-00006. http://dx.doi.org/10.1097/00130832-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Lichtenberger GS, Flavell RA, Alexopoulou L. Innate immunity and apoptosis in IBD. Inflamm Bowel Dis. 2004;10:58–62. doi: 10.1097/00054725-200402001-00012. http://dx.doi.org/10.1097/00054725-200402001-00012. [DOI] [PubMed] [Google Scholar]
- 9.McDermott MF. A common pathway in periodic fever syndromes. Trends Immunol. 2004;25:457–60. doi: 10.1016/j.it.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Ayaz NA, Ozen S, Bilginer Y, et al. MEFV mutations in systemic onset juvenile idiopathic arthritis. Rheumatology. 2009;48:23–5. doi: 10.1093/rheumatology/ken409. http://dx.doi.org/10.1093/rheumatology/ken409. [DOI] [PubMed] [Google Scholar]
- 11.Yurtcu E, Gokcan H, Yilmaz U, Sahin FI. Detection of MEFV gene mutations in patients with inflammatory bowel disease. Genet Test Mol Biomarkers. 2009;13:87–90. doi: 10.1089/gtmb.2008.0094. http://dx.doi.org/10.1089/gtmb.20048.009. [DOI] [PubMed] [Google Scholar]
- 12.Sari S, Egritas O, Dalgic B. The familial Mediterranean fever (MEFV) gene may be a modifier factor of inflammatory bowel disease in infancy. Eur J Pediatr. 2006;167:391–3. doi: 10.1007/s00431-007-0508-x. http://dx.doi.org/10.1007/s00431-007-0508-x. [DOI] [PubMed] [Google Scholar]
- 13.Akyuz F, Besisik F, Ustek D, et al. Association of the MEFV gene variations with inflammatory bowel disease in Turkey. J Clin Gastroenterol. 2013;47:23–7. doi: 10.1097/MCG.0b013e3182597992. http://dx.doi.org/10.1097/MCG.0b013e3182597992. [DOI] [PubMed] [Google Scholar]
- 14.Giaglis S, Mimidis K, Papadopoulos V, et al. Increased frequency of mutations in the gene responsible for familial Mediterranean fever (MEFV) in a cohort of patients with ulcerative colitis: evidence for a potential disease-modifying effect? Dig Dis Sci. 2006;51:687–92. doi: 10.1007/s10620-006-3192-1. http://dx.doi.org/10.1007/s10620-006-3192-1. [DOI] [PubMed] [Google Scholar]
- 15.Yalçinkaya F, Ozen S, Ozçakar ZB, et al. A new set of criteria for the diagnosis of familial Mediterranean fever in childhood. Rheumatology (Oxford) 2009;48:395–8. doi: 10.1093/rheumatology/ken509. http://dx.doi.org/10.1093/rheumatology/ken509. [DOI] [PubMed] [Google Scholar]
- 16.Uslu N, Yüce A, Demir H, et al. The association of inflammatory bowel disease and mediterranean fever gene (MEFV) mutations in Turkish children. Dig Dis Sci. 2010;55:3488–94. doi: 10.1007/s10620-010-1178-5. http://dx.doi.org/10.1007/s10620-010-1178-5. [DOI] [PubMed] [Google Scholar]
- 17.Beşer OF, Kasapçopur O, Cokuğraş FC, Kutlu T, Arısoy N, Erkan T. Association of inflammatory bowel disease with familial Mediterranean fever in Turkish children. J Pediatr Gastroenterol Nutr. 2013;56:498–502. doi: 10.1097/MPG.0b013e31827dd763. [DOI] [PubMed] [Google Scholar]


