Abstract
We assessed the relationship of lactation to long-term maternal weight gain among African-American women, who have a lower prevalence of lactation and a higher prevalence of obesity than other US women. A pregnancy cohort of 3,147 African-American women from the Black Women's Health Study who gave birth for the first time between 1995 and 2003 was followed for 8 years postpartum. Participants provided data on weight, lactation, gestational weight gain, education, diet, and exercise. Mean differences in weight gain were estimated in multivariable models. Overall, lactation was not associated with mean weight gain. However, the association was modified by prepregnancy body mass index (BMI; weight (kg)/height (m)2) (P for interaction = 0.03): Among women with BMI <30 prior to the pregnancy, mean weight gain decreased with increasing months of lactation (P for trend < 0.01), whereas among obese women (BMI ≥30), mean weight gain increased with increasing duration of lactation (P for trend = 0.04). Adjusted mean differences for ≥12 months of lactation relative to no lactation were −1.56 kg (95% confidence interval: −2.50, −0.61) among nonobese women and 2.33 kg (95% confidence interval: −0.35, 5.01) among obese women. The differences in postpartum mean weight gain persisted over the 8-year study period. Residual confounding by factors more common in women who breastfeed longer may have influenced the results.
Keywords: African-American women, childbearing, lactation, obesity, weight gain
Editor's note:An invited commentary on this article appears on page 940.
Obesity is epidemic in the United States, and the prevalence is highest in African-American women, with 58% being classified as obese in 2009–2010 (1). Many women experience appreciable weight gain during the years following their first childbirth (2–4). Stuebe and Rich-Edwards (5) have hypothesized that lactation may “reset” a woman's metabolism, leading to increased mobilization of stored fat after delivery and long-term altered glucose homeostasis. Lactation may also play a role in appetite regulation through favorable changes in adipokines such as ghrelin (6). Available data on the relationship of lactation to long-term weight gain and obesity are limited and conflicting (7–13).
The Black Women's Health Study (BWHS), a prospective cohort study of 59,000 African-American women, includes a pregnancy cohort of young women who began childbearing after enrollment (2). Data from the pregnancy cohort were used to assess the relationship of lactation to long-term maternal weight gain, taking into account important potentially confounding factors.
METHODS
Data collection
The BWHS is a prospective cohort study of 59,000 black women from all regions of the mainland United States. Participants, aged 21–69 years at baseline, enrolled in 1995 by completing mailed health questionnaires (2, 14). They have been followed every 2 years since 1995 by means of mailed questionnaires. In each questionnaire cycle, follow-up has been complete for approximately 80% of the baseline cohort. The baseline questionnaire included detailed questions on reproductive factors, including number and timing of births and duration of lactation, and on anthropometric factors, physical activity, diet, and years of education. The study protocol was approved by the Boston University Institutional Review Board.
The 1997, 1999, 2001, and 2003 questionnaires included a set of questions about pregnancies and births that had occurred since the previous questionnaire. Participants who reported having given birth were asked to record the date of birth of the baby and the amount of gestational weight gain, in categories of <10, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, and ≥40 pounds (<4.5, 4.5–6.6, 6.7–8.9, 9.0–11.2, 11.3–13.4, 13.5–15.7, 15.8–17.9, and ≥18.0 kg). With the exception of the 1997 questionnaire, which did not include questions on lactation, participants were also asked whether the baby had been breastfed and for how many months. Specifically, the 1999 and 2001 questionnaires asked, “Did you breastfeed the baby? If yes, how long did you breastfeed?”. Response options were “less than 3 months,” “3–5 months,” and “6 months or more.” If a woman checked “6 months or more” on the 1999 or 2001 questionnaire, we used data from the 2011 questionnaire to classify the duration of lactation for that birth as 6–11 months or ≥12 months. The 2011 questionnaire asked all BWHS participants about their entire lactation experience with the following questions: “How many months in total have you breastfed your children (total for all)?” and “What is the longest you breastfed any child?”. An online supplement to the 2011 questionnaire also asked about duration of lactation for each birth. The 2003 and 2005 questionnaires asked, “Did you breastfeed the baby? If yes, how many months?,” with boxes provided to fill in the exact number of months. Lactation data for women who gave birth during the 2-year interval from 1995 to 1997 were obtained from the 2011 questionnaire.
Participant weight was reported every 2 years, and participant body mass index (BMI) for each 2-year interval was calculated as weight (kg) divided by height (m) squared. Hours per week of vigorous physical activity (e.g., jogging) was ascertained on most follow-up questionnaires. In a validation study conducted among 115 participants, self-reported height and weight were highly correlated with technician-measured height and weight, and self-reported vigorous physical activity was correlated with activity measured by means of ActiGraph monitors (ActiGraph, LLC, Pensacola, Florida) (15, 16).
Diet was ascertained in 1995 with use of the National Cancer Institute–Block short-version food frequency questionnaire (17). As previously reported, a factor analysis identified 2 major dietary patterns based on 35 foods or food groups from the food frequency questionnaires: The “vegetables/fruit” dietary pattern (also called the “prudent” diet) was characterized by high intake of fruits and vegetables, whereas the “meat/fried foods” pattern (also called the “Western” diet) was characterized by high intake of meat, fried foods, and sweets (18).
Analytical cohort
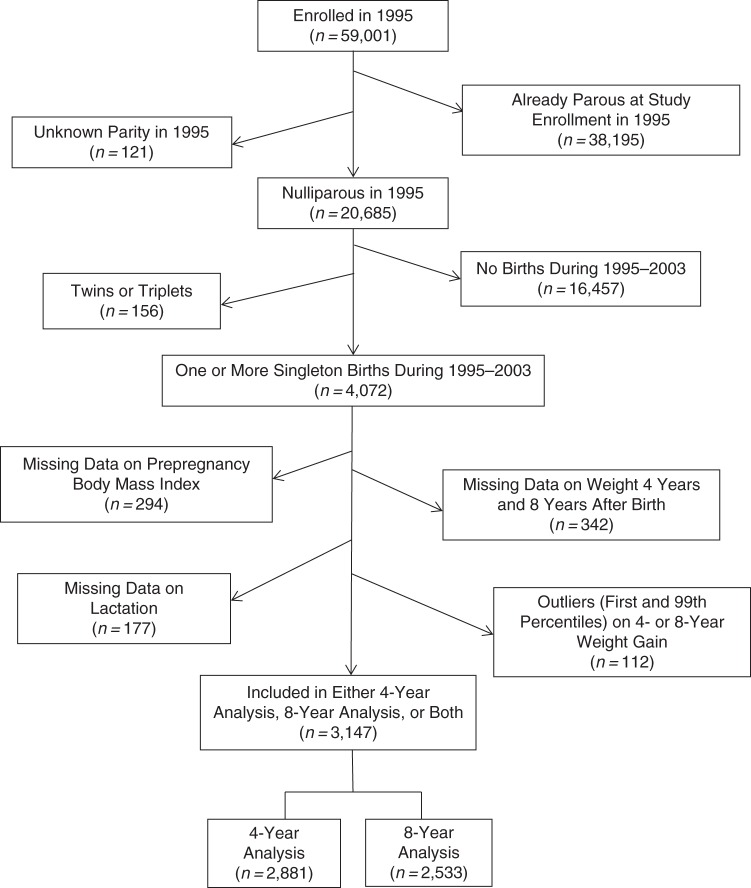
Figure 1 gives details on derivation of the analytical cohort for the present analyses. From among the 59,001 BWHS participants, there were 4,072 women who gave birth for the first time (singleton births only) during the period from 1995 through 2003. Exclusions were as follows: women with missing data on prepregnancy weight, largely because they were currently pregnant when completing the questionnaire from the cycle immediately prior to the cycle in which they reported the birth (n = 294); women who had missing data on weight 4 years and 8 years after the birth (n = 342); women with missing data on lactation (n = 177); and women who were outliers (bottom first percentile and top 99th percentile of 4- or 8-year weight change; n = 112). This left an analytical cohort of 3,147 women.
Figure 1.
Selection of the childbirth cohort from the Black Women's Health Study, 1995–2011. Missing data on prepregnancy body mass index, in most instances, occurred because the woman was pregnant when completing the previous questionnaire.
Statistical analysis
Two outcomes were assessed: weight gain 4 years after baseline and weight gain 8 years after baseline, with “baseline” defined as the year in which the participant first gave birth. Data on weight 4 years after baseline were available for 2,881 of the women, and data on weight 8 years after baseline were available for 2,533. Fewer women were included in the 8-year analyses because women whose first birth occurred in 2003 did not have a chance to attain 8 years of follow-up after the birth by the time data collection ended. Mean weight gain was computed overall and for each category of lactation. Because the data on weight and on new births were collected at 2-year intervals, “4-year” weight gain actually represents approximately 3- to 5-year weight gain, depending on when during a data collection cycle each birth occurred. Similarly, “8-year” weight gain actually represents approximately 7- to 9-year weight gain.
Multiple linear regression was used to estimate adjusted mean differences in weight gain for categories of lactation relative to no lactation, with control for age (<25, 29–29, 30–34, or ≥35 years), gestational weight gain (<20, 20–29, 30–39, or ≥40 pounds (<9.0, 9.0–13.4, 13.5–17.9, or ≥18.0 kg)), whether or not the baby was born preterm, number of additional births during follow-up (0, 1, 2, or 3), mean duration of lactation for the additional births during follow-up, Western dietary pattern (factor analysis score, in quintiles), years of education (<12, 12, 13–15, or ≥16 years), and vigorous exercise (<1, 1–2, or ≥3 hours/week, taken from the first questionnaire completed after the birth). Because the proportion of missing data was less than 2% for each of the covariates, we used the missing indicator method in all multivariable analyses. Tests for trend were conducted by using the median value of each category, with the medians modeled as a continuous variable. Tests for interaction were performed using a likelihood ratio test that compared models with and without interaction terms.
Analyses were carried out overall and within strata of age at first birth and prepregnancy BMI. Interactions by age and prepregnancy BMI were postulated a priori. Age was of interest because excess weight gain in African-American women is greatest in the third decade of life (19). Stratification by prepregnancy BMI was of interest because obese women have difficulty in achieving successful lactation (20) and may also be either more or less likely to gain weight after giving birth.
In a sensitivity analysis, we repeated the analyses in the subset of women who remained uniparous throughout the follow-up period (n = 1,771 for the 4-year period and n = 1,486 for the 8-year period). In this group, confounding by later births and subsequent breastfeeding would be absent. On the other hand, these analyses excluded a considerable proportion of the sample (approximately 38%).
RESULTS
Among the 3,147 women who had their first baby during the period from 1995 through 2003, 77% breastfed the baby for at least 1 month and 14% breastfed for 12 months or more. As shown in Table 1, women who breastfed for 12 or more months were, at baseline, more educated, leaner, more likely to engage in vigorous physical activity, and more likely to have a healthier diet than women who had not breastfed. They were less likely to have a preterm birth.
Table 1.
Baseline Characteristics (Age-Standardized) of Parous Women in the Black Women's Health Study, According to Duration of Lactation, 1995–2011
| Characteristic | Duration of Lactation, monthsa |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 (None) (n = 714) |
<3 (n = 528) |
3–5 (n = 536) |
6–11 (n = 918) |
≥12 (n = 451) |
||||||
| Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | |
| Age at first birth, years | 31.1 (4.6) | 31.0 (4.3) | 30.9 (4.3) | 31.1 (4.2) | 30.8 (4.3) | |||||
| Prepregnancy body mass indexb | 27.5 (6.8) | 27.5 (7.0) | 26.2 (5.6) | 25.2 (5.0) | 25.4 (5.0) | |||||
| >16 years of education | 27 | 26 | 34 | 37 | 50 | |||||
| Western diet (highest quintile) | 21 | 18 | 16 | 16 | 11 | |||||
| ≥35 pounds (≥15.8 kg) of gestational weight gain | 24 | 29 | 27 | 32 | 30 | |||||
| ≥3 hours/week of vigorous exercise | 24 | 27 | 28 | 31 | 37 | |||||
| Preterm birth | 18 | 16 | 14 | 14 | 11 | |||||
| ≥1 additional births | 24 | 31 | 36 | 43 | 47 | |||||
| ≥6 months’ mean lactation duration for additional births | 13 | 14 | 23 | 57 | 72 | |||||
Abbreviation: SD, standard deviation.
a Median year of first birth in each category of lactation: no lactation, 2001; <3 months, 1999; 3–5 months, 1999; 6–11 months, 1999; ≥12 months, 2001.
b Weight (kg)/height (m)2.
Overall, mean 4-year weight gain was 5.72 kg (12.6 pounds). Breastfeeding, including ≥12 months of breastfeeding, was not associated with mean weight gain (Table 2): Compared with no lactation, the adjusted mean differences were −0.28 kg (95% confidence interval (CI): −0.93, 0.37) for ever lactation and −0.87 kg (95% CI: −1.79, 0.05) for ≥12 months of lactation. However, prepregnancy BMI appeared to modify the association between lactation duration and mean weight gain (P for interaction = 0.03): Among women who were not obese, mean weight gain decreased with increasing months of lactation (P for trend < 0.01), whereas among women who were obese prior to the pregnancy, mean weight gain increased with increasing duration of lactation (P for trend = 0.04). The adjusted mean difference for ≥12 months’ lactation was −1.56 kg (95% CI: −2.50, −0.61) among the nonobese women and 2.33 kg (95% CI: −0.35, 5.01) among the obese women. No interaction was observed for age at first birth.
Table 2.
Four-Year Weight Gain in Relation to Lactation History in the Black Women's Health Study, 1995–2011
| No. of Women | Unadjusted Mean Weight Gain, kg | Unadjusted Mean Difference in Weight Gain, kg | Multivariable Mean Difference in Weight Gain, kga | 95% Confidence Interval | P for Trend | |
|---|---|---|---|---|---|---|
| Total | ||||||
| Never lactation | 643 | 6.21 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 2,238 | 5.72 | −0.49 | −0.28 | −0.93, 0.37 | |
| Lactation duration, months | 0.28 | |||||
| <3 | 478 | 5.94 | −0.27 | −0.51 | −1.36, 0.35 | |
| 3–5 | 492 | 6.24 | 0.03 | 0.14 | −0.72, 1.00 | |
| 6–11 | 836 | 5.77 | −0.44 | −0.10 | −0.87, 0.67 | |
| ≥12 | 432 | 4.81 | −1.40 | −0.87 | −1.79, 0.05 | |
| Age <30 years at time of birthb | ||||||
| Never lactation | 167 | 7.60 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 645 | 6.73 | −0.87 | −0.57 | −1.95, 0.80 | |
| Lactation duration, months | 0.61 | |||||
| <3 | 138 | 6.67 | −0.93 | −1.12 | −2.87, 0.62 | |
| 3–5 | 140 | 7.38 | −0.22 | 0.04 | −1.72, 1.81 | |
| 6–11 | 247 | 6.72 | −0.88 | −0.38 | −1.98, 1.22 | |
| ≥12 | 120 | 6.05 | −1.55 | −0.96 | −2.91, 0.98 | |
| Age ≥30 years at time of birthb | ||||||
| Never lactation | 476 | 5.73 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 1,593 | 5.32 | −0.41 | −0.25 | −0.99, 0.49 | |
| Lactation duration, months | 0.27 | |||||
| <3 | 340 | 5.64 | −0.09 | −0.36 | −1.34, 0.62 | |
| 3–5 | 352 | 5.78 | 0.05 | 0.15 | −0.83, 1.14 | |
| 6–11 | 589 | 5.37 | −0.36 | −0.07 | −0.95, 0.81 | |
| ≥12 | 312 | 4.34 | −1.39 | −0.94 | −1.99, 0.10 | |
| Prepregnancy BMIc <30d | ||||||
| Never lactation | 469 | 6.34 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 1,793 | 5.69 | −0.65 | −0.45 | −1.15, 0.25 | |
| Lactation duration, months | <0.01 | |||||
| <3 | 345 | 6.38 | 0.04 | −0.17 | −1.10, 0.76 | |
| 3–5 | 381 | 6.31 | −0.03 | 0.04 | −0.87, 0.95 | |
| 6–11 | 707 | 5.65 | −0.69 | −0.38 | −1.18, 0.42 | |
| ≥12 | 360 | 4.44 | −1.90 | −1.56 | −2.50, −0.61 | |
| Prepregnancy BMI ≥30d | ||||||
| Never lactation | 170 | 5.72 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 440 | 5.88 | 0.16 | 0.30 | −1.37, 1.97 | |
| Lactation duration, months | 0.04 | |||||
| <3 | 131 | 4.77 | −0.95 | −1.35 | −3.43, 0.73 | |
| 3–5 | 111 | 6.00 | 0.28 | 0.78 | −1.44, 3.00 | |
| 6–11 | 126 | 6.49 | 0.77 | 1.00 | −1.16, 3.17 | |
| ≥12 | 72 | 6.68 | 0.96 | 2.33 | −0.35, 5.01 |
Abbreviation: BMI, body mass index.
a Adjusted for age, gestational weight gain, preterm birth, vigorous physical activity, dietary pattern, years of education, number of additional births during follow-up, and mean duration of lactation for the additional births during follow-up.
b P for interaction with age at time of birth = 0.97.
c Weight (kg)/height (m)2. Data on prepregnancy BMI were missing for 9 women.
d P for interaction with prepregnancy BMI = 0.03.
As can be seen by a comparison with the unadjusted mean differences, adjustment for potential confounders generally moved the estimates closer to the null. Education, modeled with terms for <12, 12, 13–15, and ≥16 years, was the covariate that had the strongest association with the estimates. To reduce potential residual confounding by factors related to educational level, we repeated the analyses after restricting the data to women who reported at least some college (education ≥13 years). Results were not materially changed (data not shown). For example, among nonobese women, the adjusted mean difference in weight gain for ≥12 months’ lactation relative to no lactation was −1.67 (95% CI: −2.63, −0.70), and the P value for trend was less than 0.01 for increasing duration of lactation.
Overall mean weight gain 8 years after the first birth was 7.91 kg (17.4 pounds), indicating that the majority of excess weight gain following the first pregnancy occurred in the first 4 years after giving birth. Breastfeeding was not associated with reduced 8-year weight gain overall (Table 3), nor were significant associations observed in either age group. However, effect modification by obesity status was observed (P for interaction < 0.01): Among women with prepregnancy BMI <30, the mean difference in weight gain for ≥12 months’ lactation versus no lactation was −1.53 kg (95% CI: −2.78, −0.27) (P for trend = 0.03), while obese women who had breastfed their babies had an increased mean 8-year weight gain at every level of breastfeeding duration (P for trend < 0.01).
Table 3.
Eight-Year Weight Gain in Relation to Lactation History in the Black Women's Health Study, 1995–2011
| No. of Women | Unadjusted Mean Weight Gain, kg | Unadjusted Mean Difference in Weight Gain, kg |
Multivariable Mean Difference in Weight Gain, kga | 95% Confidence Interval | P for Trend | |
|---|---|---|---|---|---|---|
| Total | ||||||
| Never lactation | 560 | 7.91 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 1,973 | 7.91 | 0.00 | 0.44 | −0.41, 1.29 | |
| Lactation duration, months | 0.31 | |||||
| <3 | 436 | 8.32 | 0.41 | 0.35 | −0.75, 1.46 | |
| 3–5 | 425 | 8.48 | 0.57 | 0.90 | −0.23, 2.02 | |
| 6–11 | 759 | 7.69 | −0.22 | 0.36 | −0.64, 1.35 | |
| ≥12 | 353 | 7.17 | −0.74 | 0.11 | −1.12, 1.33 | |
| Age <30 years at time of birthb | ||||||
| Never lactation | 176 | 10.50 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 635 | 9.06 | −1.44 | −1.16 | −2.82, 0.49 | |
| Lactation duration, months | 0.08 | |||||
| <3 | 141 | 9.58 | −0.92 | −1.12 | −3.24, 1.01 | |
| 3–5 | 144 | 10.20 | −0.30 | −0.02 | −2.13, 2.10 | |
| 6–11 | 239 | 8.53 | −1.97 | −1.69 | −3.62, 0.24 | |
| ≥12 | 111 | 8.03 | −2.47 | −1.94 | −4.31, 0.44 | |
| Age ≥30 years at time of birthb | ||||||
| Never lactation | 384 | 6.72 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 1,338 | 7.36 | 0.64 | 1.14 | 0.15, 2.14 | |
| Lactation duration, months | 0.09 | |||||
| <3 | 295 | 7.71 | 0.99 | 1.01 | −0.28, 2.30 | |
| 3–5 | 281 | 7.60 | 0.88 | 1.30 | −0.03, 2.62 | |
| 6–11 | 520 | 7.31 | 0.59 | 1.22 | 0.06, 2.38 | |
| ≥12 | 242 | 6.78 | 0.06 | 0.97 | −0.46, .40 | |
| Prepregnancy BMIc <30d | ||||||
| Never lactation | 407 | 8.75 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 1,598 | 7.82 | −0.93 | −0.59 | −1.49, 0.32 | |
| Lactation duration, months | 0.03 | |||||
| <3 | 314 | 8.22 | −0.53 | −0.49 | −1.68, 0.71 | |
| 3–5 | 343 | 8.78 | 0.03 | 0.27 | −0.90, 1.44 | |
| 6–11 | 645 | 7.61 | −1.14 | −0.76 | −1.79, 0.27 | |
| ≥12 | 296 | 6.72 | −2.03 | −1.53 | −2.78, −0.27 | |
| Prepregnancy BMI ≥30d | ||||||
| Never lactation | 150 | 5.50 | 0 (Referent) | 0 (Referent) | ||
| Ever lactation | 370 | 8.24 | 2.74 | 3.25 | 1.03, 5.46 | |
| Lactation duration, months | <0.01 | |||||
| <3 | 120 | 8.49 | 2.99 | 2.60 | −0.11, 5.31 | |
| 3–5 | 82 | 7.22 | 1.72 | 2.37 | −0.71, 5.45 | |
| 6–11 | 112 | 8.09 | 2.59 | 3.77 | 0.92, 6.61 | |
| ≥12 | 56 | 9.49 | 3.99 | 5.76 | 2.04, 9.48 |
Abbreviation: BMI, body mass index.
a Adjusted for age, gestational weight gain, preterm birth, vigorous physical activity, dietary pattern, years of education, number of additional births during follow-up, and mean duration of lactation for the additional births during follow-up.
b P for interaction with age at time of birth = 0.42.
c Weight (kg)/height (m)2. Data on prepregnancy BMI were missing for 8 women.
d P for interaction with prepregnancy BMI < 0.01.
Results from sensitivity analyses carried out among women who remained uniparous yielded similar results (see Web Tables 1 and 2, available at http://aje.oxfordjournals.org/). In particular, increasing duration of lactation was significantly associated with lower 4-year and 8-year mean weight gain among women who were not obese when they became pregnant, whereas an opposite association was observed among the obese women.
DISCUSSION
We have previously shown in the BWHS that childbearing is associated with substantial weight gain when compared with continued nulliparity, and that the greatest increase in weight gain occurs after the first birth (2). In the present study, lactation (ever/never) and duration of lactation were not associated with 4-year or 8-year weight gain overall. However, there was statistically significant effect modification of the association by prepregnancy BMI. Among women who were not obese when they became pregnant, increased duration of lactation was associated with decreased weight gain, both 4 years and 8 years after the first birth. Women who reported 12 or more months of lactation were estimated to gain 1.56 kg (3.4 pounds) less in the first 4 years than women with no lactation, and the estimated reduction was maintained over the 8-year study period. By contrast, among women who were obese when they became pregnant, lactation, especially long-duration lactation, was associated with increased weight gain relative to never lactation.
Relatively few previous studies have assessed breastfeeding in relation to long-term weight gain. In data from a population-based survey carried out in Brazil, breastfeeding was associated with lower postpartum weight gain during an average period of 8 years after the first pregnancy among women who were not overweight when they became pregnant and with higher weight gain among women who were already overweight when they became pregnant (8). These results are quite consistent with the present findings. Mothers in the Project Viva cohort who exclusively breastfed for more than 6 months had significantly lower postpartum weight retention at 3 years than did women with shorter durations of exclusive breastfeeding (21). In cross-sectional analyses carried out in a study from England, the Million Women Study, mean BMI was significantly lower among women who had breastfed than among those who had not at every parity level (22). In cross-sectional analyses from the Women's Health Initiative, in which all participants were at least 50 years of age at entry, duration of lactation was weakly associated with lower prevalence of obesity after control for socioeconomic factors, but the association was not statistically significant after further control for physical activity, diet, and other factors (12). In a recent intervention study conducted in Belarus (the Promotion of Breastfeeding Intervention Trial), 11,867 women who had already initiated breastfeeding were randomized to a breastfeeding promotion arm or usual care and were followed for 11.5 years postpartum (13). Compared with less than 3 months of breastfeeding, a longer duration of breastfeeding was not significantly associated with a lower BMI 11.5 years later. There also was no association in observational analyses that ignored intention to treat.
Studies that assessed short-term weight gain have also yielded conflicting results. Among 4,348 participants from Nurses' Health Study II (11), women who had breastfed gained about 1 kg (2.2 pounds) more than women who had not breastfed 2 years after giving birth. In a clinic-based study of 795 women observed through pregnancy and 6 months postpartum, breastfeeding was associated with significantly lower postpartum weight gain (10). By contrast, among 26,846 women in the Danish National Birth Cohort, women who had breastfed had less postpartum weight retention 18 months postpartum (7).
A recent investigation of the relationship of lactation duration to maternal leptin, adiponectin, ghrelin, and peptide YY levels in the Project Viva cohort study supported the biological plausibility of less weight gain among women who have breastfed (6). In this prospective cohort study, long durations of breastfeeding were associated with higher levels of both ghrelin and protein peptide YY 3 years postpartum. These adipokines play a role in metabolism and appetite regulation. The apparent reduction in long-term weight gain observed in our study for nonobese women who breastfed for at least 12 months may be mediated through favorable changes in appetite regulation pathways.
Data on breastfeeding exclusivity were not collected in the present study. An analysis of months of exclusive breastfeeding relative to no breastfeeding might have provided a sharper contrast. Specifically, conflation of exclusive and partial breastfeeding into a single duration category may have contributed to some anomalous findings, such as lack of a monotonic trend in weight gain across durations of breastfeeding. However, breastfeeding exclusivity may be more relevant to studies of short-term weight gain, where the caloric cost of producing milk through exclusive breastfeeding would be important. The longer-term weight gain assessed in the present study may be affected through other mechanisms, as discussed above.
Recent work by Lemay et al. (20) implicated insulin resistance in delayed lactogenesis, suggesting that early weaning may be a marker for maternal metabolic dysfunction. Thus, it is possible that metabolic dysfunction could be a contributing cause of lack of breastfeeding rather than a result. We did not have sufficient data to separate women who tried to breastfeed without success from those who did not intend to breastfeed.
A strength of our study was the availability of weight data collected every 2 years. In addition, we had data on important potential confounders. All estimates of mean difference in weight gain were adjusted for gestational weight gain, age at the time of the first pregnancy, preterm birth status, dietary patterns, and physical activity after the first birth. We also controlled for attained years of education, which is considered to be the best measure of socioeconomic status in US black women (23). Nevertheless, it is an imprecise marker for the many factors linked to socioeconomic status, most of which are difficult to measure. In our analyses, years of education, modeled as <12, 12, 13–15, and ≥16 years, had a greater influence on the association of lactation with weight gain than any other covariate. We repeated the analyses after restricting the data to women with at least some college, among whom there may be fewer differences in lifestyle factors, and the observed associations persisted. Still, it is likely that residual confounding played a role in the observed associations.
BWHS participants come from all socioeconomic strata and educational levels but underrepresent women without a high school diploma. Perhaps because of this, the prevalence of breastfeeding is higher in the BWHS than in the general population of US black women. As can be calculated from Table 1, 77.3% of women in the BWHS pregnancy cohort had breastfed, and 14.3% were still breastfeeding at 12 months. By comparison, in US data on all births among black women (the National Immunization Survey), the prevalence of any lactation was 47.4% in 2000 and 58.9% in 2008, and the prevalence of breastfeeding at 12 months was 6.3% in 2000 and 12.5% in 2008 (24). Results from the present study are probably generalizable to most US black women but may not be generalizable to those without a high school diploma.
Adoption of breastfeeding during the past several decades has been lower among black women than among white women (24, 25). Most US black women of childbearing age must work outside the home, either full-time or part-time, and many employers do not provide a private space or time for expression and storage of breast milk. In addition, social acceptance of breastfeeding and beliefs about the relative benefits of formula and breast milk vary across social/cultural groups (26).
Findings from the present study in black women suggest that for women who are not already obese before their first term pregnancy, prolonged breastfeeding may have a long-term benefit in limiting the excess weight gain that commonly occurs after childbearing. No such benefit was observed for obese women, however, who had a greater mean weight gain if they had breastfed. It is possible that women whose metabolism has already been altered by obesity may be more susceptible to retaining weight from the additional caloric intake that typically occurs during breastfeeding. The present results suggest that mothers themselves may benefit from prolonged breastfeeding, as long as they are not already overweight; however, given the possibility of residual confounding by factors related to socioeconomic status, further research is required to substantiate the observed associations.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Slone Epidemiology Center at Boston University, Boston, Massachusetts (Julie R. Palmer, Kristen Kipping-Ruane, Lauren A. Wise, Jeffrey Yu, Lynn Rosenberg).
This work was supported by grants from the Aetna Foundation (Hartford, Connecticut), the National Cancer Institute (grants R01 CA058420 and UM1 CA164974), and the Centers for Disease Control and Prevention/Association of Schools of Public Health (grant S324-16/18).
The funders played no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, and approval of the manuscript. The content of this article is solely the responsibility of the authors and does not necessarily represent the official view of the National Cancer Institute or the National Institutes of Health.
Conflict of interest: none declared.
REFERENCES
- 1.Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;3075:491–497. [DOI] [PubMed] [Google Scholar]
- 2.Rosenberg L, Palmer JR, Wise LA, et al. A prospective study of the effect of childbearing on weight gain in African-American women. Obes Res. 2003;1112:1526–1535. [DOI] [PubMed] [Google Scholar]
- 3.Smith DE, Lewis CE, Caveny JL, et al. Longitudinal changes in adiposity associated with pregnancy. The CARDIA Study. JAMA. 1994;27122:1747–1751. [PubMed] [Google Scholar]
- 4.Gore SA, Brown DM, West DS. The role of postpartum weight retention in obesity among women: a review of the evidence. Ann Behav Med. 2003;262:149–159. [DOI] [PubMed] [Google Scholar]
- 5.Stuebe AM, Rich-Edwards JW. The reset hypothesis: lactation and maternal metabolism. Am J Perinatol. 2009;261:81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stuebe AM, Mantzoros C, Kleinman K, et al. Duration of lactation and maternal adipokines at 3 years postpartum. Diabetes. 2011;604:1277–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker JL, Gamborg M, Heitmann BL, et al. Breastfeeding reduces postpartum weight retention. Am J Clin Nutr. 2008;886:1543–1551. [DOI] [PubMed] [Google Scholar]
- 8.Coitinho DC, Sichieri R, D'Aquino Benício MH. Obesity and weight change related to parity and breast-feeding among parous women in Brazil. Public Health Nutr. 2001;44:865–870. [DOI] [PubMed] [Google Scholar]
- 9.Gunderson EP, Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev. 2000;222:261–274. [DOI] [PubMed] [Google Scholar]
- 10.Rooney BL, Schauberger CW. Excess pregnancy weight gain and long-term obesity: one decade later. Obstet Gynecol. 2002;1002:245–252. [DOI] [PubMed] [Google Scholar]
- 11.Sichieri R, Field AE, Rich-Edwards J, et al. Prospective assessment of exclusive breastfeeding in relation to weight change in women. Int J Obes Relat Metab Disord. 2003;277:815–820. [DOI] [PubMed] [Google Scholar]
- 12.Schwarz EB, Ray RM, Stuebe AM, et al. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet Gynecol. 2009;1135:974–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oken E, Patel R, Guthrie LB, et al. Effects of an intervention to promote breastfeeding on maternal adiposity and blood pressure at 11.5 y postpartum: results from the Promotion of Breastfeeding Intervention Trial, a cluster-randomized controlled trial. Am J Clin Nutr. 2013;984:1048–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boggs DA, Rosenberg L, Cozier YC, et al. General and abdominal obesity and risk of death among black women. N Engl J Med. 2011;36510:901–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carter-Nolan PL, Adams-Campbell LL, Makambi K, et al. Validation of physical activity instruments: Black Women's Health Study. Ethn Dis. 2006;164:943–947. [PubMed] [Google Scholar]
- 16.Wise LA, Palmer JR, Spiegelman D, et al. Influence of body size and body fat distribution on risk of uterine leiomyomata in U.S. black women. Epidemiology. 2005;163:346–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumanyika SK, Mauger D, Mitchell DC, et al. Relative validity of food frequency questionnaire nutrient estimates in the Black Women's Health Study. Ann Epidemiol. 2003;132:111–118. [DOI] [PubMed] [Google Scholar]
- 18.Boggs DA, Palmer JR, Spiegelman D, et al. Dietary patterns and 14-y weight gain in African American women. Am J Clin Nutr. 2011;941:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis CE, Jacobs DR, Jr, McCreath H, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Am J Epidemiol. 2000;15112:1172–1181. [DOI] [PubMed] [Google Scholar]
- 20.Lemay DG, Ballard OA, Hughes MA, et al. RNA sequencing of the human milk fat layer transcriptome reveals distinct gene expression profiles at three stages of lactation. PLoS One. 2013;87:e67531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stuebe AM, Kleinman K, Gillman MW, et al. Duration of lactation and maternal metabolism at 3 years postpartum. J Womens Health (Larchmt). 2010;195:941–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bobrow KL, Quigley MA, Green J, et al. Persistent effects of women's parity and breastfeeding patterns on their body mass index: results from the Million Women Study. Int J Obes (Lond). 2013;375:712–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith AW. Educational attainment as a determinant of social class among Black Americans. J Negro Educ. 1989;583:416–429. [Google Scholar]
- 24.Centers for Disease Control and Prevention. Progress in increasing breastfeeding and reducing racial/ethnic differences—United States, 2000–2008 births. MMWR Morb Mortal Wkly Rep. 2013;625:77–80. [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Racial and ethnic differences in breastfeeding initiation and duration, by state—National Immunization Survey, United States, 2004–2008. MMWR Morb Mortal Wkly Rep. 2010;5911:327–334. [PubMed] [Google Scholar]
- 26.Ludington-Hoe SM, McDonald PE, Satyshur R. Breastfeeding in African-American women. J Natl Black Nurses Assoc. 2002;131:56–64. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.