Abstract
OBJECTIVES:
Fixed-dose combination formulations, which simplify the administration of drugs and prevent the development of drug resistance, have been recommended as a standard anti-tuberculosis treatment regimen. However, the composition and dosage recommendations for fixed-dose combination formulations differ from those for separate formulations. Thus, questions about the effectiveness and side effects of combination formulations remain. The aim of this study was to compare the safety and efficacy of these two types of anti-tuberculosis regimens for pulmonary tuberculosis treatment.
METHOD:
A prospective, randomized controlled study was conducted using the directly observed treatment short-course strategy. Patients were randomly allocated to one of two short-course regimens. One year after completing the treatment, these patients' outcomes were analyzed. ClinicalTrials.gov: NCT00979290.
RESULTS:
A total of 161 patients were enrolled, 142 of whom were evaluable for safety assessment. The two regimens had a similar incidence of adverse effects. In the per-protocol population, serum bilirubin concentrations at the peak level, at week 4, and at week 8 were significantly higher for the fixed-dose combination formulation than for the separate formulations. All patients had negative sputum cultures at the end of the treatment, and no relapse occurred after one year of follow-up.
CONCLUSIONS:
In this randomized study, transient higher serum bilirubin levels were noted for the fixed-dose combination regimen compared with the separate formulations during treatment. However, no significant difference in safety or efficacy was found between the groups when the directly observed treatment short-course strategy was used.
Keywords: Pulmonary Tuberculosis, Fixed-Dose Combination, Adverse Effect, Efficacy
INTRODUCTION
Tuberculosis (TB) is one of the major causes of death from a curable infectious disease. The standard short-course treatment for adult TB is a regimen of isoniazid (INH, H), rifampicin (RIF, R), pyrazinamide (PZA, Z), and ethambutol (EMB, E) for the two-month initial phase, followed by a four-month phase of continuation of treatment with INH and RIF or with INH, RIF, and EMB (if there are high levels of INH resistance or if INH drug susceptibility testing results are unavailable before the continuation phase begins) 1. Despite the availability of effective anti-TB drugs, poor drug adherence may lead to treatment failure and may promote drug resistance. Additionally, inadequate doses may also lead to treatment failure and to the emergence of drug resistance if the anti-TB drugs are given in an unsupervised manner 2. The use of fixed-dose combinations (FDCs) of anti-TB drugs and a directly observed treatment short-course strategy (DOTS), as recommended by the World Health Organization (WHO) and other organizations, helps to ensure adequate treatment 3–5. The efficacy, tolerability, and acceptability of FDCs have been described in several studies 6–8. Although FDC formulations simplify TB therapy, current evidence does not indicate that these formulations improve treatment outcomes among patients with active TB 9. The dosages of the different FDC components are therefore not consistent, so higher risks of drug toxicity and adverse reactions should also be considered.
A previous study revealed that a three-drug FDC (3-FDC) regimen resulted in fewer drug-related adverse events than separate formulations (SFs) of anti-TB drugs did; however, the study method was self-administered treatment and was did not implement the DOTS 10. Additionally, the available 3-FDC formulation in Taiwan had a higher ratio of INH to RIF and PZA. Since 2006, however, the DOTS has been fully implemented in Taiwan. The aim of the present study was to compare the adverse effects and efficacy of a short-course regimen between an FDC and SFs of anti-TB drugs in the treatment of pulmonary TB and to examine the benefits of the DOTS.
METHODS
A prospective, open-label, randomized controlled study was performed at E-DA hospital, which is a 1,000-bed teaching hospital, from October 2008 to November 2009. The study protocol was approved by the hospital's ethics committee (EMRP-097-081), and all involved participants signed informed consent forms. ClinicalTrials.gov: NCT00979290
Eligibility criteria
Patients aged 18 years and older with suspected pulmonary TB (at least two sputum specimens positive for acid-fast bacilli [AFB] on direct smear microscopy or one positive specimen and a chest X-ray or chest computed tomography [CT] scan consistent with pulmonary TB), as determined by a clinician, were initially included in the study. The pulmonary TB diagnosis was confirmed histologically, microbiologically, or based on improvements in clinical status and imaging after completing the full course of treatment.
Patients were excluded from the study if they had a history of receiving anti-TB treatment, had a life expectancy of less than six months, had abnormal baseline liver function (alanine aminotransferase [ALT] or aspartate aminotransferase [AST] values greater than three times the upper limit of normal [ULN] and/or total bilirubin [BIL] values greater than 2 mg/dL), or had received immunosuppressive treatment.
Study regimens
The patients were randomly and sequentially assigned to either the FDC group or the SF group according to a randomization table created using Microsoft Word 2007 software. The FDC group received Rifater® (Gruppo Lepetit SPA, Lainate, Italy) and EMB (Veterans Pharmaceutical, Taoyuan County, Taiwan) for the first two months, followed by Rifinah® (Gruppo Lepetit SPA, Lainate, Italy) and EMB for an additional four months or longer. The daily dosage of Rifater® (INH/RIF/PZA: 80/120/250 mg per tablet) consisted of three tablets for patients weighing 30–39 kg, four tablets for patients weighing 40–49 kg, and five tablets for patients weighing 50 kg or more. Meanwhile, the daily dosage of Rifinah® consisted of three tablets of Rifinah(150)® (INH/RIF 100/150 mg per tablet) for patients weighing less than 50 kg and two tablets of Rifinah(300)® (INH/RIF 150/300 mg per tablet) for patients weighing 50 kg or more. The SF group received INH (Genuine Chemical Pharmaceutical, Taiwan), RIF (Swiss Pharmaceutical, Taiwan), PZA (Pei Li Pharmaceutical Industrial, Taiwan), and EMB for the first two months, followed by HRE (INH, RIF, EMB) for an additional four months or longer. The daily dosages of the SFs were selected based on published recommendations 11,12. The HRE was administered in the continuation phase because of a high prevalence of primary resistance to INH and because approximately 25% of patients in Taiwan are diagnosed with pulmonary TB based on their clinical presentation 13–15.
Sputum collection and culture methods
Sputum was collected from the patients at two and four months of treatment and at the end of treatment. Three sets of sputum samples were obtained at each collection time point. The sputum specimens were expectorated by the patients, and the standardized procedures for sputum storage, sputum smear preparation, and acid-fast staining were conducted in accordance with WHO recommendations 16. All specimens were processed and cultured on Lowenstein-Jensen medium using an MGIT 960 system. Drug susceptibility tests were performed using the proportion method with 7H10 medium. If specimen collection was inadequate and culture results revealed contamination, repeat specimens were collected.
Adverse effects and efficacy assessments
Clinical information was obtained from a questionnaire provided to the patients during consultation or after interviewing the patients' family members. Adverse effects, including symptoms and altered laboratory results, were closely assessed at each visit during the first and second weeks of the first month of treatment and were then assessed monthly over the next four months. Hepatotoxicity was defined as functional disturbance (AST/ALT <3×ULN and total BIL <3 mg/dL), hepatitis (AST/ALT >3×ULN with symptoms or AST/ALT >5×ULN and total BIL >3 mg/dL), or severe hepatotoxicity (persistent hepatitis after re-challenge with INH, RIF, and PZA and permanent modification of the anti-TB drug regimen). Anti-microbial efficacy was assessed by monitoring the bacteriological response rate (the negative proportion) at two and four months and at the end of treatment. The negative sputum proportion was defined as the earliest time at which the sputum culture became negative for TB, combined with the requirement that it remain negative thereafter.
Treatment response was based on the WHO definition, as follows 1. Cure was defined by a sputum smear or culture that was positive at the beginning of treatment but negative in the last month of treatment. Failure was defined by a sputum smear or culture that was positive at five months of treatment or later. Treatment completion was defined by completion of treatment without fulfillment of the criteria to be classified as either a cure or a failure. Treatment success was defined as the sum of treatment cure and completion. The assessment of relapse focused on the patients who completed treatment and follow-up without interruption, and relapse was defined as a positive culture at any time up to one year after completion of treatment.
Patient populations and DOTS
The randomized patients who received at least one dose of medication were considered as the intent-to-treat (ITT) population. All ITT patients who had completed treatment and one year of follow-up, who had received the correct daily dosage and who had not violated the protocol in any way that might influence the efficacy outcome were considered as the per-protocol (PP) population. Additionally, all patients randomized in the study who received at least one dose of medication and who had at least one element of adverse effect information were considered as evaluable for safety analysis. All patients were treated under the direct supervision of health workers and were regularly followed up at the clinic during treatment. The total duration of the studied treatment was at least six months, depending on the clinician's evaluation. After completing treatment, the patients were followed up for one year. Chest X-rays were arranged at one, two, and six months during treatment and at three, six, and 12 months after completion of treatment or at any time when the patients presented with respiratory symptoms. If any abnormalities were noted, sputum was collected for AFB smear and culture.
Since 2006, the DOTS has been recommended by the Taiwan CDC as the optimal treatment strategy 15. In the current study, a trained supervisor observed the patient during medication administration 5 days/week, whereas weekend doses were self-administered. However, treatment intake was still checked by the supervisor by unplanned visits to patients' homes and by pill counting 17.
Statistical analysis
The sample size was determined based on the reported incidence of hepatitis induced by the SFs and by the same anti-TB drug components in the form of an FDC 18,19. The expected success rate in the SF group was estimated to be 80%. With α=0.05, P1=0.03, and P2=0.21, it was estimated that 66 evaluable patients per group were included, considering an expected drop-out rate of 20%.
Inter-group differences in demographic data, clinical characteristics, diagnostic methods, drug-related adverse effects, disease severity, and laboratory data were examined using two-sided Fisher's exact tests or chi-square tests for categorical variables and independent-samples Student's t tests for continuous variables. Statistical software (SPSS version 13.0; SPSS; Chicago, IL, USA) was used for all statistical analyses. A p-value of <0.05 was considered to be statistically significant.
RESULTS
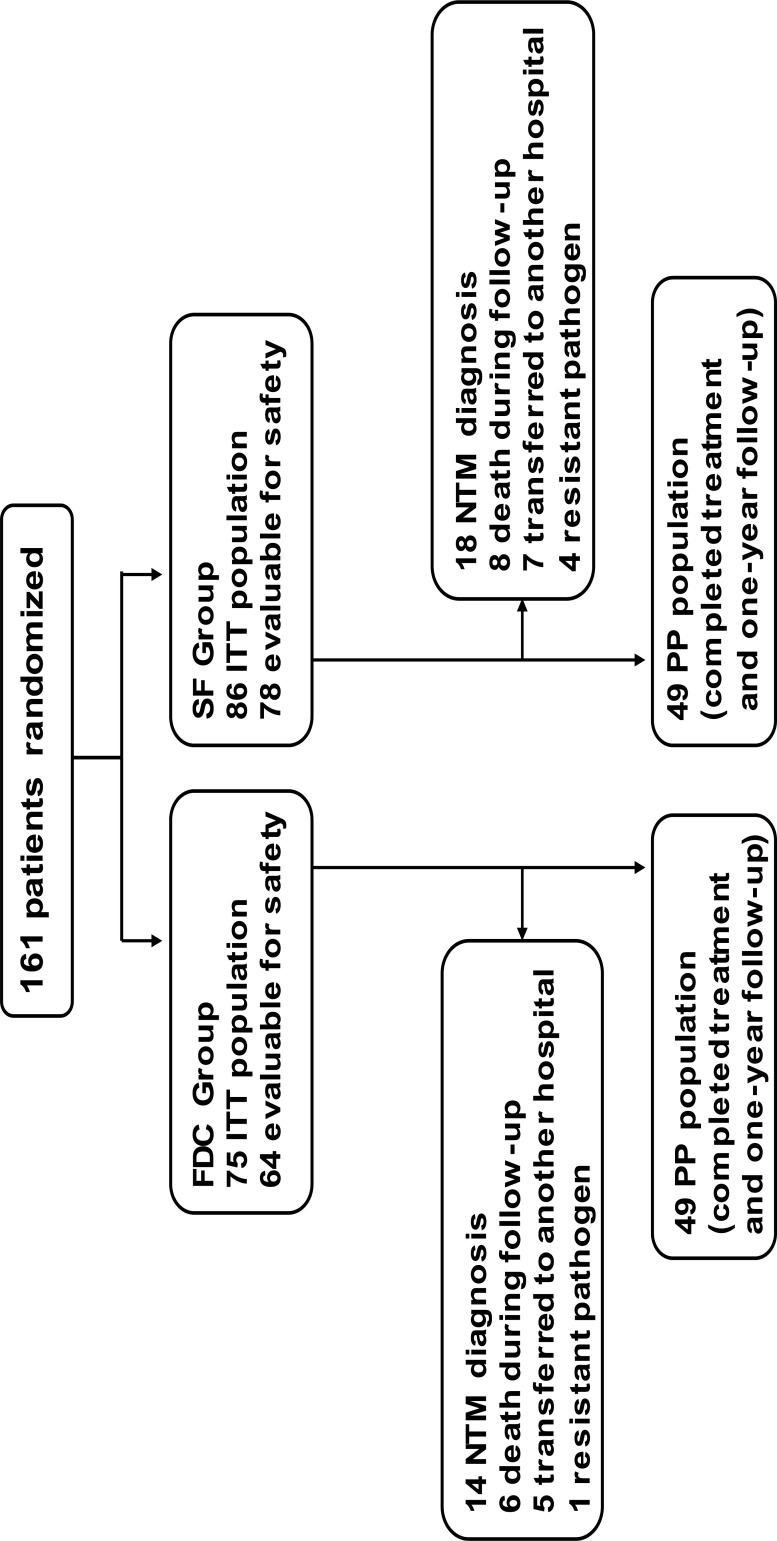
Of a total of 210 patients who were diagnosed with suspected pulmonary TB by physicians from October 2008 to November 2009, 161 patients agreed to enroll in this study. The enrolled patients were randomly assigned to either the FDC group or the SF group, and both groups were treated using the DOTS. The baseline demographic characteristics of the ITT and PP populations are presented in Table 1. No significant differences were found between the two groups in terms of demographic or clinical characteristics. Diabetes mellitus was the most common underlying disease. Of the 161 randomized patients, 63 were excluded from the analysis for the following reasons: 32 had non-tuberculous mycobacteria (NTM) (19.9%), 14 died from non-TB-related causes (8.7%), 12 were transferred to another hospital (7.5%), and 5 had resistant pathogens (3.1%) (3 with pathogens resistant to INH and 2 with pathogens resistant to INH and streptomycin). No significant difference was found between the groups in terms of the reasons for exclusion from the PP analysis (Figure 1).
Table 1.
Demographic and clinical characteristics of the study patients.
| ITT | PP | |||||
|---|---|---|---|---|---|---|
| FDC Group | SF Group | p-Value | FDC Group | SF Group | p-value | |
| Patient number | 75 | 86 | 49 | 49 | ||
| Age (years), mean ± SD | 59.2±16.7 | 64.9±17.2 | 0.04 | 57.8±17.2 | 62.3±17.3 | 0.23 |
| BW (kg), mean ± SD | 57.5±9.6 | 55.4±11.3 | 0.19 | 56.9±10.1 | 56.2±11.5 | 0.89 |
| BMI (kg/m2), mean ± SD | 21.0±3.2 | 23.2±4.4 | 0.41 | 20.6±3.3 | 20.8±3.5 | 0.79 |
| Gender (male) | 50(66.7) | 59(68.6) | 0.81 | 33(67.3) | 35(71.4) | 0.66 |
| Co-morbid conditions | ||||||
| Diabetes mellitus | 10(13.3) | 14(16.3) | 0.60 | 10(20.4) | 14(28.6) | 0.35 |
| Hepatitis carrier (HBV/HCV) | 11(14.7) | 8(9.3) | 0.29 | 10(20.4) | 7(14.3) | 0.42 |
| COPD | 4(5.3) | 9(10.5) | 0.23 | 2(4.1) | 7(14.3) | 0.16 |
| Malignancy | 4(5.3) | 3(3.5) | 0.57 | 3(6.1) | 2(4.1) | 1.0 |
| Renal insufficiency | 3(4.0) | 3(3.5) | 0.86 | 2(4.1) | 2(4.1) | 1.0 |
| Alcohol consumption | 13(17.3) | 18(20.9) | 0.56 | 8(16.3) | 7(14.3) | 0.78 |
| Smoking | 26(34.7) | 32(37.2) | 0.74 | 18(36.7) | 19(38.8) | 0.84 |
The data are presented as n(%) or as the mean ± standard deviation (SD). ITT=intent-to-treat; PP=per-protocol; FDC=fixed-dose combination; SF=separate formulation; BW=body weight; BMI=body mass index; HBV=hepatitis B virus; HCV=hepatitis C virus; COPD=chronic obstructive pulmonary disease; CXR= chest roentgenography; PCR=polymerase chain reaction
Figure 1.
Study profile. ITT=intent-to-treat; PP=per-protocol; NTM=non-tuberculous mycobacteria; FDC=fixed-dose combination; SF=separate formulation
A total of 142 patients were evaluable for safety assessment. No significant differences between the two regimens were found with regard to adverse effects (Table 2). The most frequently reported symptoms were similar between the two groups, including skin disorders (56.3% in the FDC group and 41.0% in the SF group), subjectively reported blurred vision (46.9% in the FDC group and 47.43% in the SF group), and peripheral neuropathy (39.1% in the FDC group and 30.8% in the SF group). The most frequently reported system/organ-related adverse reaction detected by laboratory examinations was hyperuricemia (>8 mg/dL: 89.1% in the FDC group and 89.7% in the SF group; >13 mg/dL: 20.3% in the FDC group and 23.1% in the SF group). Functional disturbance in hepatic enzymes was more frequent in the FDC group (42.2%) than in the SF group (39.7%), but this difference was not significant. Moreover, one patient in the FDC group and one patient in the SF group had severe hepatotoxicity that required permanent modification of their anti-TB treatment regimen. Four patients in the FDC group and two patients in the SF group required unscheduled hospitalization because of adverse effects related to the anti-TB treatment (three cases of hepatitis and one case of drug-induced fever in the FDC group and one case each of severe vomiting and urticaria in the SF group).
Table 2.
Adverse effects in the patients evaluable for safety.
| FDC Group | SF Group | p-value | |
|---|---|---|---|
| Total patients</emph> | 64 | 78 | |
| Symptoms | |||
| Arthralgia | 13(20.3) | 19(24.4) | 0.56 |
| Peripheral neuropathy | 25(39.1) | 24(30.8) | 0.30 |
| Skin disorders (rash, itching) | 36(56.3) | 32(41.0) | 0.07 |
| Blurred vision | 30(46.9) | 37(47.4) | 0.95 |
| Gastrointestinal disorders (anorexia, | 17(26.6) | 20(25.6) | 0.90 |
| Fatigue | 14(21.9) | 15(19.2) | 0.69 |
| Systemic organ laboratory reaction | |||
| Hepatotoxicity | 0.87 | ||
| Functional disturbance | 27(42.2) | 31(39.7) | |
| Hepatitis | 6(9.4) | 5(6.4) | |
| Severe hepatotoxicity | 1(1.6) | 1(1.3) | |
| Hyperuricemia | |||
| >8 mg/dL | 57(89.1) | 70(89.7) | 0.89 |
| >13 mg/dL | 13(20.3) | 18(23.1) | 0.69 |
| Thrombocytopenia (<150×103/L) | 12(18.8) | 12(15.4) | 0.59 |
| Leukopenia (<3.5×103/L) | 5(7.8) | 5(6.4) | 0.74 |
| Unscheduled hospitalization | 4(6.3) | 2(2.6) | 0.28 |
*The data are presented as n(%). FDC=fixed-dose combination; SF=separate formulation
In the PP population, we analyzed liver function fluctuation during anti-TB drug treatment. The results revealed that serum total BIL levels at the peak level and at weeks four and eight were significantly higher in the FDC group compared with the SF group (p=0.03, 0.04, and 0.03, respectively) (Table 3).
Table 3.
Liver function tests in the PP population during anti-TB drug treatment.
| FDC Group (n=49) | SF Group (n=49) | p-value | |
|---|---|---|---|
| Baseline AST level (U/L) | 31(28–56) | 23(18–37) | 0.6 |
| Peak AST level (U/L) | 67(45–102) | 55(33–60) | 0.86 |
| 1st week | 35(23–43) | 24(19–31) | 0.83 |
| 2nd week | 36(28–57) | 27(24–37) | 0.41 |
| 4th week | 38(21–43) | 30(25–49) | 0.42 |
| 8th week | 36(31–57) | 30(25–58) | 0.41 |
| 12th week | 33(29–54) | 29(25–37) | 0.93 |
| 16th week | 40(29–45) | 25(23–36) | 0.20 |
| Baseline ALT level (U/L) | 20(17–41) | 18(14–30) | 0.79 |
| Peak ALT level (U/L) | 63(46–97) | 46(26–102) | 0.41 |
| 1st week | 16(11–35) | 15(12–26) | 0.65 |
| 2nd week | 24(17–66) | 19(16–37) | 0.19 |
| 4th week | 21(16–37) | 26(21–44) | 0.93 |
| 8th week | 23(19–46) | 28(19–62) | 0.55 |
| 12th week | 39(20–47) | 33(21–58) | 0.97 |
| 16th week | 24(21–39) | 23(16–27) | 0.26 |
| Baseline T-BIL level (mg/dl) | 0.85(0.59–.093) | 0.6(0.45–1.22) | 0.22 |
| Peak T-BIL level (mg/dl) | 1.21(0.98–1.54) | 0.93(0.73–1.29) | 0.03 |
| 1st week | 0.76(0.55–0.99) | 0.61(0.43–0.7) | 0.28 |
| 2nd week | 0.64(0.42–0.82) | 0.66(0.36–0.84) | 0.11 |
| 4th week | 0.87(0.66–1.10) | 0.72(0.57–0.89) | 0.04 |
| 8th week | 1.06(0.70–1.43) | 0.57(0.44–0.97) | 0.03 |
| 12th week | 0.89(0.54–1.15) | 0.77(0.46–1.07) | 0.21 |
| 16th week | 0.95(0.76–1.21) | 0.65(0.47–1.08) | 0.15 |
The data are presented as the median(range). AST=aspartate aminotransferase; ALT=alanine aminotransferase; T-BIL=total bilirubin; FDC=fixed-dose combination; SF=separate formulation
The severity of disease was not significantly different between the two regimens (Table 4). In particular, 17 (34.7%) patients in FDC group and 18 (36.7%) patients in the SF group were sputum smear positive. After two months of treatment, four patients (two in the FDC group and two in the SF group) were smear positive. Only one patient in the FDC group was still sputum smear and culture positive after two months of treatment, whereas all other patients were culture negative. The negative sputum proportion rate after two months of treatment was 93.5% in the FDC group and 100% in the SF group. All patients in the FDC and SF groups were sputum culture negative after four and six months of treatment, respectively No relapse occurred in either group after one year of follow-up.
Table 4.
The severity of disease and the distribution of diagnostic methods.
| FDC Group (n=49) | SF Group (n=49) | |
|---|---|---|
| Severity of disease | ||
| Cavitation on CXR | 8(16.3) | 5(10.2) |
| Smear positive | 17(34.7) | 18(36.7) |
| Diagnosis | ||
| Culture | 29(59.2) | 34(69.4) |
| Pathology | 1(2) | 0 |
| PCR | 1(2) | 0 |
| Clinically diagnosed | 18(36.7) | 12(30.6) |
*The data are presented as n(%). FDC=fixed-dose combination; SF=separate formulation; CXR=chest roentgenography; PCR=polymerase chain reaction
DISCUSSION
FDCs, which simplify the administration of drugs and prevent the development of drug resistance 20, have been recommended as a standard anti-TB treatment regimen 4,5. However, the composition and dosage recommendations for FDCs differ from those for SFs, which is a major concern for clinicians. We found that when treatment with anti-TB medications was supervised using the DOTS, the incidence rates of adverse effects and efficacy were not significantly different between the FDC and the SF regimens in a safety population analysis. Only the occurrence of transient hyperbilirubinemia was significantly different in the patients treated with the FDC regimen compared with those treated with the SF regimen during the course of treatment in the PP population.
In the current study, the negative sputum proportion rate after two months of treatment was 93.5% for the FDC regimen and 100% for the SF regimen, which are values comparable to those in previous reports 10,19,21. No treatment failures after six months of treatment and no relapse after one year of follow-up were observed for either regimen. The treatment success in this study is comparable to that in previous reports 10,19,22. In fact, nearly all work comparing the efficacy of FDCs and single-drug regimens has reported similar results (i.e., no significant differences), regardless of the FDC formulation, when patients were enrolled in DOTS-based studies 23.
Comparisons of safety between FDC and SF regimens have been reported in previous studies, and most randomized studies have revealed that adverse events did not significantly differ between the groups 24,25. In contrast, Su et al. 10 reported fewer drug-related adverse events among patients receiving an FDC regimen compared with an SF regimen; however, the study was not supervised using the DOTS, and the dosages of the components of Rifater® were different from those of the current FDCs in Taiwan. Additionally, the recommended dosage of Rifater® based on body weight is higher than the recommended dosage of INH (e.g., 400 mg/day vs. 300 mg/day in 50 kg patients, which is higher than the maximum of 300 mg daily), so the higher dosage of INH in those receiving FDC, which has a greater risk of inducing liver dysfunction, should be considered. In the current study, we found that in the PP population, the average peak levels of AST, ALT, and total BIL in the patients receiving the FDC regimen were higher than those in the patients receiving the SF regimen during the course of treatment. However, hepatotoxicity (including functional disturbance and severe hepatotoxicity) did not significantly differ between the two regimens in the safety population study. Cholestasis is thought to be an adverse effect of RIF treatment that may be insidious and that may be resolved without discontinuing the drug 26. The combined use of RIF and INH has been reported to pose an increased risk of hepatotoxicity 27, which may explain the transient, statistically significant hyperbilirubinemia observed in the FDC group (receiving a higher dosage of INH) compared with the SF group in the present study.
In the current study, the mean age of the enrolled patients was approximately 60 years. The safety evaluation among these patients was based on symptoms and laboratory examinations. The major adverse effects were skin reactions, overall hepatotoxicity, and non-symptomatic hyperuricemia. However, no significant differences were found between the two study groups. However, a higher occurrence of adverse effects was observed in this study compared with other studies 28, which may have been due to differences in the age and ethnicity of the study populations 15.
FDC treatment has the advantages of increased acceptance and adherence, an increased success rate, a lower cost, and increased prevention of prescription errors and drug resistance 6,10,19,20,24. These benefits are based on patient adherence to treatment. Indeed, previous studies have suggested that when the DOTS is deficient, the increased adherence that is expected with an FDC regimen may compensate for the small difference in efficacy between SF and FDC regimens 23,24. In the present randomized study, FDC and SF regimens were objectively compared using the DOTS standard, and the results revealed that the potential disadvantages of SFs appeared to be overcome if TB patients are treated using the DOTS.
Based on the higher price of FDCs at current market rates in Taiwan, we estimate that the cost of an FDC-based regimen (233 US$) is approximately 1.7 times higher than that of an SF regimen (135 US$) for a six-month treatment course. These estimated costs must be carefully interpreted because they only include the product cost and were determined based on standardized DOTS programs. These findings differ from those in previous reports, which predicted that FDC prices will drop as competition and production volume increase 4,29. In resource-limited countries, DOTS-based programs have not been successfully implemented for TB care 30, but the use of FDCs is likely to play a relevant role in increasing cure rates and also in decreasing the cost of managing the drug supply system due to simplification of formulations, ordering, procurement, distribution, and storage 31.
There are certain limitations to the present study. First, the prevalence of NTM is increasing in Taiwan 32, and the fact that the clinical presentation of NTM was difficult to differentiate from that of TB at initial enrollment resulted in nearly 20% of the patients being excluded from the analysis. Second, more elderly TB patients were included in this study compared with other studies 22,28, and their higher rates of co-morbidities may have influenced their ability to complete the one year of follow-up. Third, patients with drug-resistant strains were also excluded to avoid the influence of efficacy assessment between regimens. All of these factors limited the number of cases that were analyzed at the end of the study, which could have led to these findings being inconclusive. However, although only few patients who completed this study were analyzed, the patients included in the analysis had multiple underlying diseases that are typical in daily clinical practice. In any case, a larger randomized study is warranted to confirm the findings of this study.
In conclusion, the present study demonstrated that DOTS-based TB treatment with an FDC or SF regimen shows no significant differences in terms of efficacy or adverse events. Although the components of the FDC and their recommended dosages were not consistent with those for SFs of anti-TB drugs, only transiently increased serum levels of BIL were noted in the FDC group.
ACKNOWLEDGMENTS
This study was funded by a grant (EDAHP99037) from E-DA hospital/I-Shou University, Kaohsiung, Taiwan.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.World Health Organization. Tuberculosis Programme Treatment of tuberculosis: guidelines for national programmes. 4th ed. WHO/HTM/TB/2009.420. Geneva, Switzerland: WHO; 2009. [Google Scholar]
- 2.Mitchison DA. How drug resistance emerges as a result of poor compliance during short course chemotherapy for tuberculosis. Int J Tuberc Lung Dis. 1998;2((1)):10–15. [PubMed] [Google Scholar]
- 3.Moulding T, Dutt AK, Reichman LB. Fixed-dose combinations of anti-tuberculous medications to prevent drug resistance. Ann Intern Med. 1995;122((12)):951–4. doi: 10.7326/0003-4819-122-12-199506150-00010. [DOI] [PubMed] [Google Scholar]
- 4.Blomberg B, Spinaci S, Fourie B, Laing R. The rationale for recommending fixed-dose combination tablets for treatment of tuberculosis. Bull World Health Organ. 2001;79((1)):61–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: Treatment of tuberculosis. Am J Respir Crit Care Med. 2003;167((4)):603–62. doi: 10.1164/rccm.167.4.603. [DOI] [PubMed] [Google Scholar]
- 6.Hong Kong Chest Service/British Medical Research Council. Acceptability, compliance, and adverse reactions when isoniazid, rifampin, and pyrazinamide are given as a combined formulation or separately during three-times-weekly anti-tuberculosis chemotherapy. Am Rev Respir Dis. 1989;140((6)):1618–22. doi: 10.1164/ajrccm/140.6.1618. [DOI] [PubMed] [Google Scholar]
- 7.Blomberg B, Fourie B. Fixed-dose combination drugs for tuberculosis: application in standardised treatment regimens. Drugs. 2003;63((6)):535–53. doi: 10.2165/00003495-200363060-00002. [DOI] [PubMed] [Google Scholar]
- 8.Lienhardt C, Cook SV, Burgos M, Yorke-Edwards V, Rigouts L, Anyo G, et al. Efficacy and Safety of a 4-Drug Fixed-Dose Combination Regimen Compared With Separate Drugs for Treatment of Pulmonary Tuberculosis. The Study C Randomized Controlled Trial. JAMA. 2011;305((14)):1415–23. doi: 10.1001/jama.2011.436. [DOI] [PubMed] [Google Scholar]
- 9.Albanna AS, Smith BM, Cowan D, Menzies D. Fixed-dose combination antituberculosis therapy: a systematic review and meta-analysis. Eur Respir J. 2013;42((3)):721–32. doi: 10.1183/09031936.00180612. [DOI] [PubMed] [Google Scholar]
- 10.Su WJ, Perng RP. Fixed-dose combination chemotherapy (Rifater®/Rifinah®) for active pulmonary tuberculosis in Taiwan: a two-year follow-up. Int J Tuberc Lung Dis. 2002;6((11)):1029–32. [PubMed] [Google Scholar]
- 11.Infectious Diseases Society of the Republic of China; Society of Tuberculosis, Taiwan; Medical Foundation in Memory of Dr. Deh-Lin Cheng; Foundation of Professor Wei-Chuan Hsieh for Infectious Diseases Research and Education; C Y Lee's Research Foundation for Pediatric Infectious Diseases and Vaccines. Guidelines for chemotherapy of tuberculosis in Taiwan. J Microbiol Immunol Infect. 2004;37((6)):382–4. [PubMed] [Google Scholar]
- 12.Taiwan Guidelines for TB Diagnosis and Treatment. (Taiwan): Centers for Disease Control, Department of Health, R.O.C.; (2008). 3rd Ed. [Google Scholar]
- 13.Jiang JR, Yen SY, Wang JY. Increased prevalence of primary drug-resistant pulmonary tuberculosis in immunocompromised patients. Respirology. 2011;16:308–13. doi: 10.1111/res.2011.16.issue-2. [DOI] [PubMed] [Google Scholar]
- 14.Yu CC, Chang CY, Liu CE, Shih LF, Hsiao JH, Chen CH. Drug Resistance Pattern of Mycobacterium Tuberculosis Complex at a Medical Center in Central Taiwan, 2003–2007. J Microbiol Immunol Infect. 2010;43((3)):285–90. doi: 10.1016/S1684-1182(10)60045-X. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control, Republic of China (Taiwan) Department of health, The Executive Tuan, Taiwan. (Available at http://www.cdc.gov.tw) (date of access: May. 3, 2013). [Google Scholar]
- 16.World Health Organization. Laboratory services in tuberculosis control. Part II:microscopy. WHO/TB/98.258. Geneva, Switzerland: WHO; 1998. [Google Scholar]
- 17.Taiwan Centers for Disease Control and Prevention. Nov, 2013. [Promulgated defi nitions of TB]. Taipei, Taiwan: CDC, 2009. http://203.65.72.83/ch/dt/upload/QC/QC_index.htm. Accessed. [Google Scholar]
- 18.Sun HY, Chen IL, Gau CS, Chang SC, Luh KT. A prospective study of hepatitis during antituberculous treatment in Taiwanese patients and a review of the literature. J Formos Med Assoc. 2009;108((2)):102–11. doi: 10.1016/S0929-6646(09)60040-1. [DOI] [PubMed] [Google Scholar]
- 19.Zhang L-X, Kan G-Q, Tu D-H, Wan L-Yet, Faruqi AR. Fixed-dose combination chemotherapy versus multiple, single-drug chemotherapy for tuberculosis. Curr Therap Research. 1996;57((11)):849–56. doi: 10.1016/S0011-393X(96)80018-X. [DOI] [Google Scholar]
- 20.Moulding TS, Le HQ, Rikleen D, Davidson P. Preventing drug-resistant tuberculosis with a fixed dose combination of isoniazid and rifampin. Int J Tuberc Lung Dis. 2004;8((6)):743–8. [PubMed] [Google Scholar]
- 21.Bellabas M, Khaled S, Khaled NA, Boulahbal F, Chaulet P. Therapeutic trial of a combination of isoniazid, rifampicin and pyrazinamide in the first 2 months of treatment of pulmonary tuberculosis. Rev Mal Respir. 1989;6((1)):59–64. [PubMed] [Google Scholar]
- 22.Agounitestane D, Chiheb M, Khaled S, Ait Khaled N, Boulahbal F, Chaulet P. A therapeutic trial of a combination of 3 essential drugs in a short course of chemotherapy in tuberculosis. Results 6months after the end of treatment. Rev Mal Respir. 1990;7((3)):209–13. [PubMed] [Google Scholar]
- 23.Monedero I, Caminero JA. Evidence for promoting fixed-dose combination drugs in tuberculosis treatment and control: a review. Int J Tuberc Lung Dis. 2011;15((4)):433–9. doi: 10.5588/ijtld.09.0439. [DOI] [PubMed] [Google Scholar]
- 24.Teo SK. Assessment of a combined preparation of isoniazid, rifampicin and pyrazinamide (Rifater®) in the initial phase of chemotherapy in three 6-month regimens for smear-positive pulmonary tuberculosis: a five-year follow-up report. Int J Tuberc Lung Dis. 1999;3((2)):126–32. [PubMed] [Google Scholar]
- 25.Bartacek A, Schutt D, Panosch B, Borek M. Rimstar® 4-FDC Study Group. Comparison of a four-drug fixed-dose combination regimen with a single tablet regimen in smear-positive pulmonary tuberculosis. Int J Tuberc Lung Dis. 2009;13((6)):760–6. [PubMed] [Google Scholar]
- 26.Girling DJ. Adverse reactions to rifampicin in antituberculosis regimens. J Antimicrob Chemother. 1977;3((2)):115–32. doi: 10.1093/jac/3.2.115. [DOI] [PubMed] [Google Scholar]
- 27.Steele MA, Burk RF, DesPrez RM. Toxic hepatitis with isoniazid and rifampin. A meta-analysis. Chest. 1991;99((2)):465–71. doi: 10.1378/chest.99.2.465. [DOI] [PubMed] [Google Scholar]
- 28.Marra F, Marra CA, Bruchet N, Richardson K, Moadebi S, Elwood RK, et al. Adverse drug reactions associated with first-line anti-tuberculosis drug regimens. Int J Tuberc Lung Dis. 2007;11((8)):868–75. [PubMed] [Google Scholar]
- 29.Laing RO, McGoldrick KM. Tuberculosis drug issues: prices, fixed-dose combinatsion products and second-line drugs. Int J Tuberc Lung Dis. 2000;4((12 Suppl 2)):S194–207. [PubMed] [Google Scholar]
- 30.Uplekar M, Pathania V, Raviglione M. Private practitioners and public health: weak links in tuberculosis control. Lancet. 2001;358((9285)):912–6. doi: 10.1016/S0140-6736(01)06076-7. [DOI] [PubMed] [Google Scholar]
- 31.Norval PY, Blomberg B, Kitler ME, Dye C, Spinaci S. Estimate of the globalmarket for rifampicin-containing fixed-dose combination tablets. Int J Tuberc Lung Dis. 1999;3((11 Suppl 3)):S292–300. [PubMed] [Google Scholar]
- 32.Tsai CF, Shiau MY, Chang YH, Wang YL, Huang TL, Liaw YC, et al. Trends of mycobacterial clinical isolates in Taiwan. Trans R Soc Trop Med Hyg. 2011;105((3)):148–52. doi: 10.1016/j.trstmh.2010.11.005. [DOI] [PubMed] [Google Scholar]