Abstract
The incidence of cancer is sharply increasing. Cancer is a leading cause of death as well as a significant burden on society. The incidence of urological cancer has shown a higher than average increase and will become an important concern in the future. Therefore, an overall and accurate understanding of the incidence of urological cancer is essential. In this study, which was based on the Korea National Cancer Incidence Database, annual incident cases, age-standardized incidence rates, annual percentage change (APC), and distribution by age group were examined in kidney, bladder, and prostate cancers, respectively. From 1999 to 2011, the total number of each type of urological cancer was as follows: kidney cancer (32,600 cases, 25.5%), bladder cancer (37,950 cases, 29.7%), and prostate cancer (57,332 cases, 44.8%). The age-standardized incidence rates of prostate cancer showed a significant increase with an APC of 12.3% in males. Kidney cancer gradually increased with an APC of 6.0% for both sexes and became the second most frequent urological cancer after 2008. Bladder cancer showed no significant change with an APC of -0.2% for both sexes and has decreased slightly since 2007. The distribution of kidney cancer according to age showed two peaks in the 50- to 54-year-old and 65- to 69-year-old age groups. Bladder and prostate cancers occurred mostly in the 70- to 74-year-old age group. The proportions of male to female were 2.5:1 in kidney cancer and 5.6:1 in bladder cancer. We have summarized the incidence trends of kidney, bladder, and prostate cancers and have provided useful information for screening and management of these cancers in the future.
Keywords: Incidence, Kidney, Neoplasms, Prostate, Urinary bladder
INTRODUCTION
Cancer is the main cause of death worldwide and is creating a significant burden on society as a result of population growth and aging [1]. Accurate information regarding cancer incidence is important for clinical decision making and appropriate cancer control. Therefore, evaluating trends in cancer incidence nationally is important. However, the incidence of cancer has shown a nonuniform distribution throughout the world [1,2,3].
To date, urological cancer is more prevalent in the West than in the East; however, the incidence of urological cancer has been on the rise and in 2011 accounted for more than 8.0% of all cancers in Korea [2]. Owing to population aging and the consumption of westernized diets, urological cancer is expected to further increase. Therefore, assessment of incidence is necessary to establish a health care policy for the control of urological cancer.
A survey of urological cancer incidence in Korea from 1985 to 1999 was previously reported [4]. In the present study, we summarize the most recent cancer statistics from 1999 to 2011 in Korea and report on the incidence of urological cancer, with a focus on kidney, bladder, and prostate cancers.
SURVEY METHODOLOGY
Data on the incidence of urological cancer from 1999 to 2011 were attained from the Korea National Cancer Incidence Database. The Korea Central Cancer Registry began in the 1980s and data have been collected for the whole population through the Population-Based Regional Cancer Registry program since 1999. As a result, cancer statistics in Korea are released annually [2,5,6,7,8,9]. In this study, urological cancer cases were defined on the basis of the International Classification of Diseases for Oncology, 3rd edition [10], and the International Classification of Disease, 10th edition [11].
To determine trends in urological cancer incidence, annual incident cases were first identified and then age-standardized incidence rates were calculated based on the world standard population. Finally, annual percentage change (APC) was evaluated on the basis of site and sex.
In addition, to examine the urological cancer distribution according to age, the total number of urological cancers was classified according to age group by use of cancer statistics from 2006 to 2010. Change in urological cancer distribution based on age group was evaluated for each year, and site-specific peak age was investigated by combining the 5-year data.
OVERVIEW OF UROLOGICAL CANCER INCIDENCE
In Korea, the incidence of all cancers has increased approximately two folds from 101,032 cases in 1999 to 218,017 cases in 2011. Urological cancer incidence has increased more dramatically compared with the incidence of all cancers combined. For example, the number of kidney, bladder, and prostate cancers was 5,019 in 1999, which was approximately 5% of all cancers, and the incidence increased approximately three folds to 16,490 cases in 2011 (7.6% of all cancers). During the study period, the total number of each type of urological cancer was as follows: kidney cancer (32,600 cases, 25.5%), bladder cancer (37,950 cases, 29.7%), and prostate cancer (57,332 cases, 44.8%). Of the total 127,882 cases, 109,936 cases (86.0%) were in males and 17,946 cases (14.0%) were in females, resulting in a male-to-female ratio of 6.1:1.
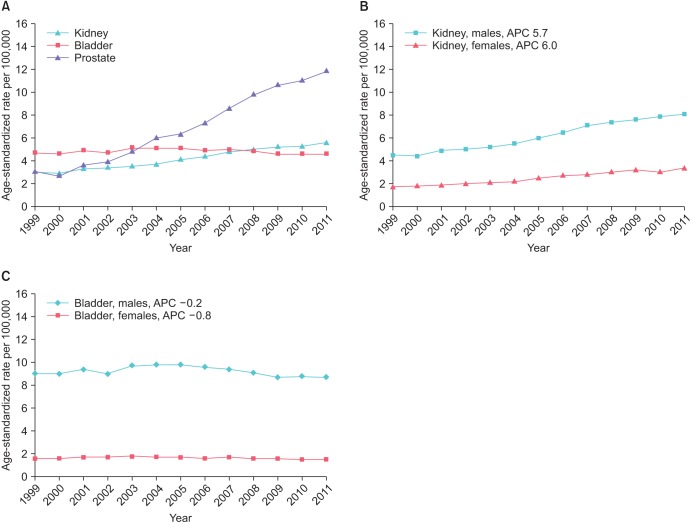
The age-standardized incidence rate of kidney, bladder, and prostate cancers during the study period for both sexes is shown in Fig. 1. The age-standardized incidence rate of prostate cancer showed a steep increase with the highest incidence rates since 2004 (Fig. 1A). The age-standardized incidence rate of kidney cancer showed a gradual increase and became the second most frequent urological cancer since 2008. Bladder cancer showed no significant change and decreased slightly from 2007. When compared according to sex, the age-standardized kidney and bladder cancer incidence rate of males was higher than that of females with a ratio of 2.5-5.6:1. However, the APC pattern differed; in kidney cancer, a greater increase in APC was found in females (6.0) than in males (5.7), whereas for bladder cancer, the APC of females (-0.8) decreased more than in males (-0.4) (Fig. 1B, C).
Fig. 1. Trend in age-standardized cancer incidence rates according to site (A) and sex in kidney (B) and bladder (C). APC, annual percentage change.
INCIDENCE OF KIDNEY CANCER
Reportedly, kidney cancer incidence has increased consistently during the past 30 years [12]. Kidney cancer is the 8th most frequent cancer in Canada [13]. The incidence of kidney cancer shows geographic diversity with a higher incidence rate in North America and Europe than in Asia and South America [14]. In Korea, the number of kidney cancer cases has continued to increase from 1,402 cases in 1999 to 3,989 cases in 2011, a total of 32,600 cases during this period. Of these cases, 22,313 were males and 10,287 were females, resulting in a male-to-female predominance ratio of 2.2:1 (Table 1).
Table 1. Trend in cancer incidence according to site and sex from 1999 to 2011 in Korea.
| Site/gender | Year | APC | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | ||
| Kidney | ||||||||||||||
| Both sexes | 1,402 | 1,433 | 1,659 | 1,756 | 1,903 | 2,089 | 2,376 | 2,655 | 2,955 | 3,248 | 3,487 | 3,648 | 3,989 | 6.0 |
| Male | 965 | 976 | 1,134 | 1,196 | 1,292 | 1,415 | 1,613 | 1,810 | 2,039 | 2,235 | 2,359 | 2,557 | 2,722 | 5.7 |
| Female | 437 | 457 | 525 | 560 | 611 | 674 | 763 | 845 | 916 | 1,013 | 1,128 | 1,091 | 1,267 | 6.0 |
| Bladder | ||||||||||||||
| Both sexes | 2,180 | 2,235 | 2,485 | 2,471 | 2,764 | 2,916 | 3,035 | 3,068 | 3,225 | 3,292 | 3,271 | 3,459 | 3,549 | -0.2 |
| Male | 1,732 | 1,787 | 1,962 | 1,943 | 2,189 | 2,332 | 2,434 | 2,483 | 2,561 | 2,634 | 2,603 | 2,784 | 2,847 | -0.4 |
| Female | 448 | 448 | 523 | 528 | 575 | 584 | 601 | 585 | 664 | 658 | 668 | 675 | 702 | -0.8 |
| Prostate | 1,437 | 1,304 | 1,800 | 2,037 | 2,629 | 3,396 | 3,727 | 4,486 | 5,516 | 6,586 | 7,455 | 8,007 | 8,952 | 12.3 |
APC, annual percentage change.
The age-standardized incidence rate increased from 3.0 per 100,000 in 1999 to 5.6 per 100,000 in 2011 with an APC of 6.0 for both sexes (Table 2). During that time, the average ratio of the age-standardized incidence rate for males to females was 2.5:1, which was similar to the ratio in most other countries [14]. However, the male-to-female ratio declined from 2.6:1 (4.5/1.7) in 1999 to 2.4:1 (8.1/3.4) in 2011. This decline is partly attributed to a greater increase in the APC in females (6.0) than in males (5.7).
Table 2. Trend in age-standardized cancer incidence rates according to site and sex from 1999 to 2011 in Korea.
| Site/gender | Year | APC | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | ||
| Kidney | ||||||||||||||
| Both sexes | 3.0 | 2.9 | 3.3 | 3.4 | 3.5 | 3.7 | 4.1 | 4.4 | 4.8 | 5.0 | 5.2 | 5.3 | 5.6 | 6.0 |
| Male | 4.5 | 4.4 | 4.9 | 5.0 | 5.2 | 5.5 | 6.0 | 6.5 | 7.1 | 7.4 | 7.6 | 7.9 | 8.1 | 5.7 |
| Female | 1.7 | 1.8 | 1.9 | 2.0 | 2.1 | 2.2 | 2.5 | 2.7 | 2.8 | 3.0 | 3.2 | 3.0 | 3.4 | 6.0 |
| Bladder | ||||||||||||||
| Both sexes | 4.7 | 4.6 | 4.9 | 4.7 | 5.1 | 5.1 | 5.1 | 4.9 | 5.0 | 4.8 | 4.6 | 4.6 | 4.6 | -0.2 |
| Male | 9.0 | 9.0 | 9.4 | 9.0 | 9.7 | 9.8 | 9.8 | 9.6 | 9.4 | 9.1 | 8.7 | 8.8 | 8.7 | -0.4 |
| Female | 1.6 | 1.6 | 1.7 | 1.7 | 1.8 | 1.7 | 1.7 | 1.6 | 1.7 | 1.6 | 1.6 | 1.5 | 1.5 | -0.8 |
| Prostate | ||||||||||||||
| Both sexes | 3.1 | 2.7 | 3.6 | 3.9 | 4.8 | 6.0 | 6.3 | 7.3 | 8.6 | 9.8 | 10.6 | 11.0 | 11.8 | 13.8 |
| Male | 8.4 | 7.2 | 9.5 | 10.1 | 12.4 | 15.1 | 15.7 | 17.9 | 20.9 | 23.4 | 25.1 | 25.9 | 27.4 | 12.3 |
APC, annual percentage change.
Age-standardized incidence rates were per 100,000 and calculated based on the world standard population.
The age-standardized incidence rate has increased nearly two folds in recent decades but is relatively low compared with other countries. For example, the age-standardized incidence rate was 3.3 per 100,000 among Koreans compared with 10.6 per 100,000 among Americans in 2001 and 5.3 per 100,000 among Koreans compared with 12.4 per 100,000 among Americans in 2010 [15]. In Japan, the age-standardized incidence rate changed from 7.5 per 100,000 in 2001 to 8.1 per 100,000 in 2007 [16].
The APC, however, was higher in Korean males (5.7) and females (6.0) than in American males (1.9) and females (2.3) [15]. In Japan, the APC was 2.3 in males and 3.1 in females [16]. The higher APC in Koreans may be explained by the more prevalent use of diagnostic imaging tools such as ultrasonography or computerized tomography for the evaluation of a variety of abdominal complaints or routine medical check-ups. The difference could also be explained by changing epidemiology in the risk factors for kidney cancer, such as dietary factors or exposure to other carcinogens, over recent decades [13].
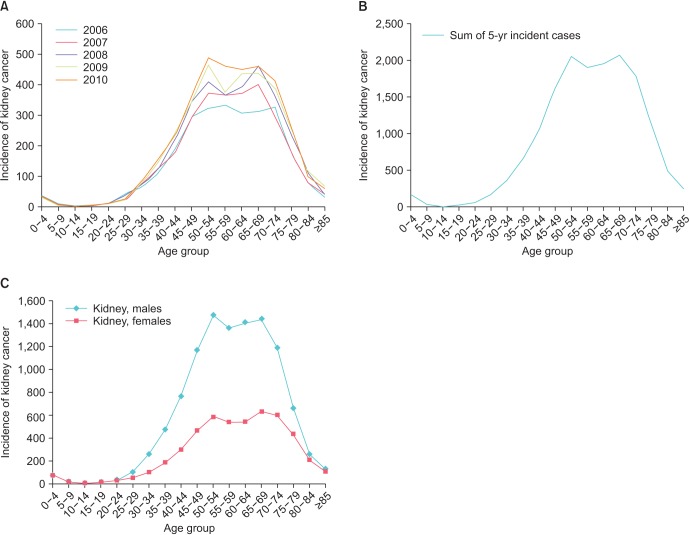
When we analyzed the incidence of kidney cancer according to age, we found that kidney cancer increased rapidly in the 40- to 44-year-old age group and then dropped sharply after 75 to 79 years of age (Fig. 2A). The distribution according to age showed two peaks in the 50- to 54- and 65- to 69-year-old age groups (Fig. 2B). In addition, similar patterns were observed in male and female cases (Fig. 2C). This pattern of distribution is also considered to be a result of medical check-ups, which increased the detection rate of small renal tumors in the 50- to 54-year-old age group.
Fig. 2. The distribution of kidney cancer incidence according to age group. (A) Annual change from 2006 to 2010. (B) Sum of 5-year cancer incidence. (C) Sex comparisons.
INCIDENCE OF BLADDER CANCER
Bladder cancer is the 11th most frequent cancer worldwide [17]. Incidence rates of bladder cancer vary substantially, with high incidence rates occurring in North America and Europe and low incidence rates in South America and Central-South Asia [17]. Smoking is the leading cause of bladder cancer. Schistosoma infection and occupational hazards such as exposure to aromatic amines are other well-known causes of bladder cancer [18]. In Korea, the number of bladder cancer cases continued to increase from 2,180 cases in 1999 to 3,549 cases in 2011, a total of 37,950 cases during this period. Of these cases, 30,291 cases occurred in males and 7,659 cases occurred in females, resulting in a male-to-female predominance ratio of 4.0:1 (Table 1).
The age-standardized incidence rate decreased slightly from 4.7 per 100,000 in 1999 to 4.6 per 100,000 in 2011 with an APC of -0.2 for both sexes (Table 2). The age-standardized incidence rate of bladder cancer was higher than the rate for kidney and prostate cancers in 1999, but was lower than the incidence rate for kidney and prostate cancers since 2008. The average ratio of the age-standardized incidence rate for males to females was 5.6:1, which is slightly higher than that observed in other countries (2-4:1) [19]. This difference is partly attributed to a high rate of smoking in males. However, despite the increased smoking rate in females, the male-to-female ratio was similar during this period, indicating that sex and environmental exposure are also important factors [19,20].
The age-standardized incidence rate was approximately the same over the past few decades, but was relatively low compared with Japan. For example, the age-standardized incidence rate was 4.7 per 100,000 among Koreans compared with 8.1 per 100,000 among Japanese in 1999 and 5.0 per 100,000 among Koreans compared with 6.9 per 100,000 among Japanese in 2007 [16]. However, in addition to Japan, the incidence rate of bladder cancer is decreasing in developed countries in North America as well as in northern and western Europe [17]. This trend reflects the reduction in smoking, which is the most essential risk factor for bladder cancer. For example, in the United States, the rate of smoking decreased from 45% in 1965 to 19% in 2010 [21], and a similar trend was identified in Canada and the United Kingdom [17]. In the case of Korea, the age-standardized incidence rate of bladder cancer has declined since 2007.
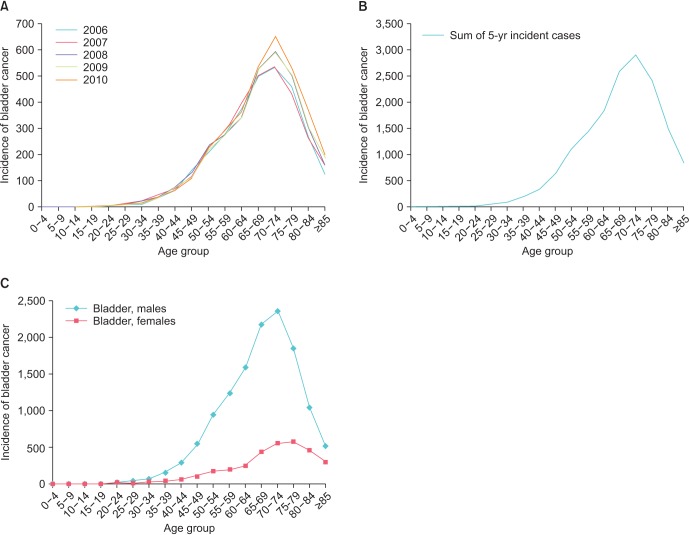
When we analyzed the incidence of bladder cancer by age group, we found that bladder cancer increased rapidly starting in the 50- to 54-year-old age group and peaked in the 70- to 74-year-old age group (Fig. 3A, B). The distribution of bladder cancer according to age differed from the distribution of kidney cancer in that the peak age occurred in one age group and more than 5 years later. This difference is attributed to the evaluation of bladder cancer after microscopic or gross hematuria, or when lower urinary tract symptoms develop, whereas kidney cancer is detected more often as a result of a medical check-up without any symptoms. When the incidence was compared according to sex, a similar pattern was observed (Fig. 3C).
Fig. 3. The distribution of bladder cancer incidence according to age group. (A) Annual change from 2006 to 2010. (B) Sum of 5-year cancer incidence. (C) Sex comparisons.
INCIDENCE OF PROSTATE CANCER
Prostate cancer is the second most commonly diagnosed cancer and the sixth leading cause of death in males worldwide [22]. In developed countries, prostate cancer is the most frequent cancer and the third leading cause of death in males [1]. This cancer also varies geographically, showing high incidence rates in Europe, North America, Japan, and New Zealand/Australia and low incidence rates in Eastern Asia, Central-South Asia, and North Africa [22]. The broad variation in the incidence rate is partly due to the differences in detection practices using the prostate-specific antigen (PSA) test, lifestyle, and treatment. In addition, racial disparities in incidence exist, with black males having a higher incidence rate than white males and Asians [3,23].
In Korea, the number of prostate cancer cases has increased rapidly from 1,437 cases in 1999 to 8,952 cases in 2011, a total of 57,332 cases during this period (Table 1). The number of prostate cancer cases was similar to the number of kidney cancer cases and accounted for two-thirds of bladder cancer in 1999, but became the most frequent urological cancer in 2004 and represented more cases than bladder and kidney cancers combined from 2008 on.
The age-standardized incidence rate sharply increased from 8.4 per 100,000 in 1999 to 27.4 per 100,000 in 2011 with an APC of 12.3 in males (Table 2). The age-standardized incidence rate of prostate cancer was lower than that of bladder cancer during 1999-2000, but showed the highest incidence rate from 2001 on and was more than three folds higher than kidney and bladder cancers in 2011.
Although the age-standardized incidence rate of prostate cancer increased sharply in Korea, it is relatively low compared to other countries. For example, the age-standardized incidence rate was 8.4 per 100,000 among Koreans compared with 24.8 per 100,000 among Japanese in 1999 and 20.9 per 100,000 among Koreans compared with 56.4 per 100,000 among Japanese in 2007 [16]. In the United States, the prostate cancer incidence rate increased significantly with the introduction of serum PSA testing in the 1980s (approximately 12% per year), peaked in 1992, and then stabilized from 1995 to 2005 [24]. Similar to the United States, prostate cancer incidence is expected to increase steadily over the next 10 years in Korea.
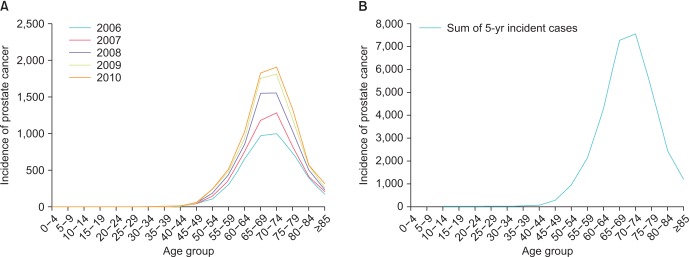
When we analyzed the incidence of prostate cancer according to age, we found that prostate cancer rapidly increased starting with the 55- to 59-year-old age group and peaked with the 70- to 74-year-old age group (Fig. 4A, B). The distribution of prostate cancer according to age was similar to that of bladder cancer in terms of pattern and peak age.
Fig. 4. The distribution of prostate cancer incidence according to age group. (A) Annual change from 2006 to 2010. (B) Sum of 5-year cancer incidence.
CONCLUSIONS
With population growth and aging, urological cancer will continue to increase and become a significant burden on society. In Korea, during the study period, the incidence of prostate and kidney cancers increased at a rapid rate, whereas that of bladder cancer slightly decreased with the reduction in the smoking rate. The peak age of kidney cancer was 50 to 54 and 65 to 69 years. Bladder and prostate cancers commonly peaked in the 70- to 74-year-old age group. When compared according to sex, the male to female ratios were 2.5-5.6:1. Our study will provide useful knowledge for screening and management of urological cancer.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Jung KW, Won YJ, Kong HJ, Oh CM, Lee DH, Lee JS. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2011. Cancer Res Treat. 2014;46:109–123. doi: 10.4143/crt.2014.46.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 4.Cheon J, Kim CS, Lee ES, Hong SJ, Cho YH, Shin EC, et al. Survey of incidence of urological cancer in South Korea: a 15-year summary. Int J Urol. 2002;9:445–454. doi: 10.1046/j.1442-2042.2002.00500.x. [DOI] [PubMed] [Google Scholar]
- 5.Jung KW, Won YJ, Park S, Kong HJ, Sung J, Shin HR, et al. Cancer statistics in Korea: incidence, mortality and survival in 2005. J Korean Med Sci. 2009;24:995–1003. doi: 10.3346/jkms.2009.24.6.995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, et al. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010;25:1113–1121. doi: 10.3346/jkms.2010.25.8.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011;43:1–11. doi: 10.4143/crt.2011.43.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat. 2012;44:11–24. doi: 10.4143/crt.2012.44.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013;45:1–14. doi: 10.4143/crt.2013.45.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fritz A. International classification of diseases for oncology. 3rd ed. Geneva: World Health Organization; 2000. [Google Scholar]
- 11.World Health Organization. International statistical classification of diseases and related health problems. 10th revision ed. Geneva: World Health Organization; 1994. [Google Scholar]
- 12.Tyson MD, Humphreys MR, Parker AS, Thiel DD, Joseph RW, Andrews PE, et al. Age-period-cohort analysis of renal cell carcinoma in United States adults. Urology. 2013;82:43–47. doi: 10.1016/j.urology.2013.02.065. [DOI] [PubMed] [Google Scholar]
- 13.De P, Otterstatter MC, Semenciw R, Ellison LF, Marrett LD, Dryer D. Trends in incidence, mortality, and survival for kidney cancer in Canada, 1986-2007. Cancer Causes Control. 2014;25:1271–1281. doi: 10.1007/s10552-014-0427-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chow WH, Dong LM, Devesa SS. Epidemiology and risk factors for kidney cancer. Nat Rev Urol. 2010;7:245–257. doi: 10.1038/nrurol.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.King SC, Pollack LA, Li J, King JB, Master VA. Continued increase in incidence of renal cell carcinoma, especially in young patients and high grade disease: United States 2001 to 2010. J Urol. 2014;191:1665–1670. doi: 10.1016/j.juro.2013.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katanoda K, Matsuda T, Matsuda A, Shibata A, Nishino Y, Fujita M, et al. An updated report of the trends in cancer incidence and mortality in Japan. Jpn J Clin Oncol. 2013;43:492–507. doi: 10.1093/jjco/hyt038. [DOI] [PubMed] [Google Scholar]
- 17.Chavan S, Bray F, Lortet-Tieulent J, Goodman M, Jemal A. International variations in bladder cancer incidence and mortality. Eur Urol. 2014;66:59–73. doi: 10.1016/j.eururo.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Burger M, Catto JW, Dalbagni G, Grossman HB, Herr H, Karakiewicz P, et al. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol. 2013;63:234–241. doi: 10.1016/j.eururo.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 19.Fajkovic H, Halpern JA, Cha EK, Bahadori A, Chromecki TF, Karakiewicz PI, et al. Impact of gender on bladder cancer incidence, staging, and prognosis. World J Urol. 2011;29:457–463. doi: 10.1007/s00345-011-0709-9. [DOI] [PubMed] [Google Scholar]
- 20.Horstmann M, Witthuhn R, Falk M, Stenzl A. Gender-specific differences in bladder cancer: a retrospective analysis. Gend Med. 2008;5:385–394. doi: 10.1016/j.genm.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Jemal A, Thun MJ, Ries LA, Howe HL, Weir HK, Center MM, et al. Annual report to the nation on the status of cancer, 1975-2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst. 2008;100:1672–1694. doi: 10.1093/jnci/djn389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O, et al. International variation in prostate cancer incidence and mortality rates. Eur Urol. 2012;61:1079–1092. doi: 10.1016/j.eururo.2012.02.054. [DOI] [PubMed] [Google Scholar]
- 23.Cook MB, Rosenberg PS, McCarty FA, Wu M, King J, Eheman C, et al. Racial disparities in prostate cancer incidence rates by census division in the United States, 1999-2008. Prostate. 2015;75:758–763. doi: 10.1002/pros.22958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li J, Djenaba JA, Soman A, Rim SH, Master VA. Recent trends in prostate cancer incidence by age, cancer stage, and grade, the United States, 2001-2007. Prostate Cancer. 2012;2012:691380. doi: 10.1155/2012/691380. [DOI] [PMC free article] [PubMed] [Google Scholar]