Abstract
Objectives.
This study investigates how health- and disability-based need factors and enabling factors (e.g., socioeconomic and family-based resources) relate to nursing home admission among 3 different racial and ethnic groups.
Method.
We use Cox proportional hazard models to estimate differences in nursing home admission for non-Hispanic whites, non-Hispanic blacks, and Hispanics from 1998 to 2010 in the Health and Retirement Study (N = 18,952).
Results.
Racial–ethnic differences in nursing home admission are magnified after controlling for health- and disability-based need factors and enabling factors. Additionally, the degree to which specific factors contribute to risk of nursing home admission varies significantly across racial–ethnic groups.
Discussion.
Our findings indicate that substantial racial and ethnic variations in nursing home admission continue to exist and that Hispanic use is particularly low. We argue that these differences may demonstrate a significant underuse of nursing homes for racial and ethnic minorities. Alternatively, they could signify different preferences for nursing home care, perhaps due to unmeasured cultural factors or structural obstacles.
Key words: Hispanic ethnicity, Long-term care, Nursing homes, Race.
Studies find that older Hispanic and non-Hispanic black adults are less likely than non-Hispanic white adults to enter nursing homes (Akamigbo & Wolinsky, 2007; Angel, Angel, Aranda, & Miles, 2004; Cagney & Agree, 1999; Smith, Feng, Fennell, Zinn, & Mor, 2007; U.S. Census Bureau, 2010b; Wallace, Levy-Storms, Kington, & Andersen, 1998). However, previous estimations of racial- and ethnic-based differences in nursing home admission are limited. Studies of Hispanics’ use of nursing homes tend to rely on small samples, be geographically limited, and/or examine only Hispanics (Angel & Angel, 1997; Angel, Angel, McClellan, & Markides, 1996; Baxter, Bryant, Scarbro, & Shetterly, 2001; Wallace et al., 1998). Further, many studies that compare non-Hispanic blacks, non-Hispanic whites, and Hispanics are not based on individual-level data but rather overall rates of nursing home admission. Thus, they are unable to examine the constellation of factors that account for any racial and ethnic group differences (Feng, Fennell, Tyler, Clark., & Mor, 2011). Because of this deficiency, the implications of these racial- and ethnic-based differences in long-term care are complex and poorly understood. We draw on Andersen’s model of medical care utilization to examine what factors contribute to racial and ethnic differences in nursing home admission, focusing on need-based factors (e.g., physical health and disability) and enabling factors (e.g., socioeconomic resources, social and family ties) (Andersen, McCutcheon, Aday, Chiu, & Bell, 1983). To explore the importance of these factors, the first goal of our study is to examine nursing home admission by race and ethnicity using nationally representative longitudinal data, paying attention to how need and enabling factors alter the association between race/ethnicity and nursing home admission.
Relatedly, the factors that increase non-Hispanic white Americans’ risk of nursing home admission are not necessarily also relevant to non-Hispanic black and Hispanic Americans. With the increase in Hispanic and non-Hispanic black adults in nursing homes (Feng et al., 2011), it is increasingly important to investigate whether nursing home admission models based on levels of need and enabling factors are applicable across different racial and ethnic groups. Because the majority of past studies do not test for differences by race and/or ethnicity (Angel & Angel, 1997; Cagney & Agree, 1999; Dunlop, Manheim, Song, & Chang, 2002; Friedman, Steinwachs, Rathouz, Burton, & Mukamel, 2005; Wallace et al., 1998), we know little about how vulnerability for nursing home admission varies within racial and ethnic groups. Thus, the second goal of our study is to test interactions between race and Hispanic ethnicity and need and enabling factors in order to identify whether these factors have moderating relationships with nursing home admission.
Background
Prior studies demonstrate that disability and poor health increase the risk of nursing home admission (Friedman et al., 2005; Gaugler, Duval, Anderson, & Kane, 2007; Miller & Weissert, 2000). In line with Andersen’s model (1983), we categorize poor health and high levels of disability as indicators of nursing home need. Because older Hispanic and non-Hispanic black adults report worse health and higher levels of disability compared with non-Hispanic white adults (Angel, Angel, & Hill, 2009; Ottenbacher et al., 2009) yet exhibit lower overall rates of nursing home admission than non-Hispanic white adults (Akamigbo & Wolinsky, 2007; Feng et al., 2011), health and disability may serve to suppress the relationship between nursing home admission and race/ethnicity.
Differences in nursing home admission may also be due to fewer enabling resources (i.e., means available for the use of particular health care services) among some groups compared with others (Andersen et al., 1983). Socioeconomic resources make up one important category of enabling factors, as income, wealth, and health insurance are all important predictors of nursing home admission (Friedman et al., 2005; Himes, Wagner, Wolf, Aykan, & Dougherty, 2000). This association is complicated, however, as some studies find that socioeconomic resources are associated with decreased risk of nursing home admission (Martikainen et al., 2009; McCann, Grundy, & O’Reilly, 2012), perhaps because socioeconomic resources afford access to nursing home substitutes like home health care. Non-Hispanic black and Hispanic adults report fewer socioeconomic resources, reflective of discrimination and marginalization processes (DeNavas-Walt, Proctor, & Smith, 2009). Therefore, taking the fewer socioeconomic resources of racial and ethnic minorities into account is important for estimating the extent of racial and ethnic differences in nursing home admissions.
Family and social resources represent a second important category of enabling resources (Andersen et al., 1983). Family and social ties, including marital status and living arrangements, are key predictors of nursing home admission (Freedman, 1996; Freedman, Berkman, Rapp, & Ostfeld, 1994; Friedman et al., 2005; Noël-Miller, 2010; Soldo, Wolf, & Agree, 1990). Hispanics report strong family and social ties (Angel et al., 2004; Angel & Hogan, 2004; Herrera, George, Angel, Markides, & Torres-Gil, 2012; Scharlach, Giunta, Chow, & Lehning, 2008). Thus, it may be that these strong social and family ties among Hispanics, which include close geographic proximity to children, serve as substitutes for nursing home care and potentially reduce nursing home admissions. We expect that family and social ties may be a more important resource for Hispanics compared with other groups due to strong cultural imperatives to care for older adults and an emphasis on familism, defined as a cultural mandate that privileges family members’ needs over individual interests (Angel et al., 2004; Burton, Bonilla-Silva, Ray, Buckelew, & Hordge Freeman, 2010; Ibarra, 2003). Non-Hispanic black adults are more likely to live alone (U.S. Census Bureau, 2010a) and less likely to be married (Elliott, Krivickas, Brault, & Kreider, 2012) than Hispanic or non-Hispanic white adults. Family care and nursing home care are not necessarily mutually exclusive—one study found that non-Hispanic black adults do not substitute nursing home care for family care but are more likely to supplement nursing home care with family care (Miner, 1995). Thus, we expect family and social ties to be less important for understanding non-Hispanic black adults’ nursing home admissions than non-Hispanic white or Hispanic adults’.
We propose that not taking health and disability, socioeconomic resources, and family and social ties into account leads to poor estimations of racial–ethnic differences in nursing home admissions. Further, if large racial and ethnic differences in nursing home admission persist among those who are the most vulnerable (e.g., worst health, most disability, least socioeconomic resources, fewest family and social ties), then these differences may demonstrate a potential underuse of nursing homes for racial and ethnic minorities. This may be due to discrimination or structural reasons (e.g., few nursing homes in areas with high concentrations of racial and ethnic minorities), which should be a cause for public policy concern. Conversely, racial and ethnic differences in nursing home admission could also be due to aversion to nursing homes, perhaps due to cultural preferences or structural obstacles (e.g., no Spanish spoken by nursing home staff).
Drawing on the reviewed literature, in this study, we propose to test two hypotheses:
Hypothesis 1: The risk of nursing home admission will be higher for non-Hispanic white adults than for non-Hispanic black adults and Hispanics, with the lowest risk among Hispanics, controlling for predisposing characteristics (birth year, gender, foreign born) and need (health and disability) and enabling factors (socioeconomic resources and social and family ties).
Hypothesis 2: Need and some enabling factors—specifically socioeconomic resources—will be more important for predicting non-Hispanic white adults’ nursing home admission than for non-Hispanic black or Hispanic adults, while other enabling factors—specifically social and family ties—will be more important for predicting Hispanic adults’ nursing home admission than for non-Hispanic blacks or non-Hispanic whites and will be least important for predicting non-Hispanic black adults’ nursing home admission.
Method
Data come from the Health and Retirement Study (HRS), a nationally representative biennial survey of persons over the age of 50, first interviewed in 1992 (Juster & Suzman, 1995). We employ this data set because it oversamples non-Hispanic black and Hispanic adults, documents nursing home admission, and investigates health, economic resources, and family and social ties in older ages. For this study, we use seven waves of the HRS (1998–2010) and limit the analytic sample to the population ages 65 and older. We exclude respondents who do not self-report as non-Hispanic white, non-Hispanic black, or Hispanic (n = 369). We also exclude respondents missing data on three or more variables (n = 1,301). These respondents do not differ from non-missing respondents on risk of nursing home admission or racial or ethnic identity. The final sample size is 18,952.
Measures
Nursing home admission.
Time to first nursing home admission is our primary outcome. Previous research suggests that the timing of first nursing home admission marks the beginning of reliance on the formal long-term care system (Freedman, 1996). Respondents are asked whether, since the last wave (or, for first time respondents, in the last 2 years), they have been overnight patients in a nursing home, convalescent home, or other long-term health care facility. This includes all respondents who have been admitted into a nursing home during the study period, regardless of length of stay. We drop respondents who entered a nursing home before 1998 or before age 65 (n = 553). Thus, what we code as “nursing home” throughout this study includes any long-term health care facility. We construct a measure of age at first nursing home admission, subtracting the year and month of nursing home admission from the respondent’s birth year and month. In total, 2,798 respondents entered a nursing home during the study period.
Race/ethnicity.
The primary predictor variable is race/ethnicity. We use the following mutually exclusive categories: non-Hispanic white, non-Hispanic black, and Hispanic. Those who identify as Hispanic are excluded from the non-Hispanic white and non-Hispanic black categories, regardless of how they identify their race.
Need (health and disability factors).
Our health and disability measures consist of number of activities of daily living (ADL), instrumental activities of daily living (I-ADL), and mobility activities that the respondents report any difficulty performing; number of cognitive impairments; any incontinence in past year; and previous hospitalization. The ADL index, which ranges from 0 to 6, includes any difficulty with bathing, eating, dressing, walking across a room, getting in or out of bed, or using the toilet. The I-ADL index ranges from 0 to 3 and measures any difficulty performing three household tasks (using a telephone, taking medication, and handling money). The mobility index asks about any difficulty walking one block, walking several blocks, walking across a room, climbing one flight of stairs, and climbing several flights of stairs; this ranges from 0 to 5. For all three measures, higher scores represent greater disability. We also include an index of the respondent’s cognitive impairments. Respondents were given several tests, specifically immediate and delayed word recall, the serial 7’s test, counting backward, naming tasks, and vocabulary questions. This results in a score from 0 to 35. The original variable was coded so that higher scores demonstrate more cognitive abilities (e.g., ability to recall all of the words from a set of words). We recode this score so that higher values indicate more cognitive impairments. We use the imputations provided by the RAND HRS data file for missing values (RAND HRS Data, 2010). For incontinence, respondents were asked, “During the last 12 months, have you lost any amount of urine beyond your control?” For previous hospitalization, respondents were asked if they had any overnight hospital stays in the past 2 years.
Enabling (socioeconomic resources and family and social ties).
We assess socioeconomic resources with questions about educational attainment, total non-housing net worth, homeownership, Medicaid participation, and household income. Educational attainment is coded into two categories: less than high school and more than high school. Total non-housing net worth is the sum of household non-housing asset amounts minus total debt, as reported by respondents. We use the net worth imputations provided by the RAND HRS data file for missing net worth values (RAND HRS Data, 2010). Furthermore, we transform the net worth values using inverse hyperbolic sine transformation (Burbidge, Magee, & Robb, 1988). This transformation is very similar in properties and interpretation to more common log transformations but is defined for zero and negative values. We use the same technique for household income. Homeownership and Medicaid participation are both dichotomous variables.
Family and social ties include number of living children, any living siblings, marital status, proximity of adult children, and future help availability. Number of living children is continuous, and the indicator for any living siblings is dichotomous. The marital status variable includes four categories: married, widowed, divorced, and never married. For proximity of adult children, we code three mutually exclusive categories: child lives within 10 miles, child lives with respondent, and child does not live within 10 miles of respondent. For the future help variable, respondents were asked: “Suppose in the future, you needed help with basic personal care activities like eating or dressing. Do you have relatives or friends (besides your husband/wife/partner/…) who would be willing and able to help you over a long period of time?” Respondents who reported having a non-spousal helper were not asked this question. We code this categorically, with respondents who said “no” or “don’t know” as the reference category, respondents who said “yes” as the first group, and respondents who reported using non-spousal helpers as the second.
Controls (predisposing factors).
Predisposing factors include gender (woman or man), year of birth, and whether the respondent is foreign born or U.S. born. We include year of birth instead of age because age is the analysis time used in the hazard models.
Analysis
We begin our analysis with descriptive statistics by race and Hispanic ethnicity. We then use appropriate tests to statistically compare non-Hispanic white respondents with non-Hispanic black and Hispanic respondents for each variable. We utilize Cox proportional hazards regression models, and time to first nursing home admission is our primary outcome. Age is our analytic unit of time. The Cox regression model is useful when time dependence in the baseline hazard is unknown (Vuchinich, Teachman, & Crosby, 1991). We include respondents in models as at risk for nursing home admission when they are at least 65. We right-censor respondents who did not enter a nursing home by the end of the study period (n = 7,011) or died before the end of the study without entering a nursing home (n = 9,143). Of those who died before the end of the study without entering a nursing home, 78.5% were non-Hispanic white, 14.5% were non-Hispanic black, and 7% were Hispanic. We report hazard ratios, which are exponentiated coefficients: a hazard ratio greater than one indicates an increasing risk of nursing home admission for an increase in the independent variable at any event time, whereas less than one indicates a decreasing risk.
In the multivariate analysis to test Hypothesis 1, we first estimate five models. In the baseline model, we include race/ethnicity, gender, birth year, and foreign or U.S. born. In the second model, we add the health and disability variables; in the third model, we add socioeconomic resources to the baseline model; and in the fourth model, we add family and social ties to the baseline model. In the fifth model, we include all variables (full model).
To test Hypothesis 2, we examine whether these same variables across the three categories—predisposing factors, need-based factors, and enabling factors—serve as moderators for the relationship between racial–ethnic identity and nursing home admission. To test moderators, we interact each variable of interest with the race/ethnicity variables. We fit a full model with each of these interactions simultaneously. We only present significant interactions from this full model. As a test for robustness, and because of concerns of small sample sizes especially for Hispanics, we also examine descriptive statistics of those who entered nursing homes compared with those who did not, stratified by race and ethnicity, and we examine our conceptual models separately by racial–ethnic groups. These results confirm our interaction findings.
We create missing flags for those respondents missing information on any variables, thus we retain these respondents. Those missing on more than three variables are excluded. We do not present coefficients for these missing flags, but they are available upon request. All analyses are conducted using Stata (StataCorp, 2009).
Results
Descriptive Statistics
Table 1 presents descriptive statistics of variables by race/ethnicity. A higher proportion of non-Hispanic white respondents (0.16) enter a nursing home during our study period than any other racial–ethnic group. Notably, however, the proportion of non-Hispanic black adults (0.13) who enter a nursing home is not significantly different than the proportion of non-Hispanic white adults. A significantly lower proportion of Hispanics (0.09) enters nursing homes, indicating this group is least at risk for nursing home admission.
Table 1.
Descriptive Statistics, HRS 1998–2010 (N = 18,952)
| Non-Hispanic whites (n = 14,828) | Non-Hispanic blacks (n = 2,653) | Hispanics (n = 1,471) | |
|---|---|---|---|
| Entered nursing home | 0.16 | 0.13 | 0.09*** |
| Predisposing factors (sociodemographics) | |||
| Women (ref = man) | 0.57 | 0.62*** | 0.58* |
| Birth year | 1927.58 | 1928.71*** | 1929.37*** |
| Foreign born | 0.05 | 0.05 | 0.55*** |
| Need (health and functioning) | |||
| ADL difficulties (0–6) | 0.48 | 0.74*** | 0.76*** |
| I-ADL difficulties (0–3) | 0.19 | 0.30*** | 0.31*** |
| Mobility difficulties (0–5) | 1.29 | 1.54*** | 1.49*** |
| Number of cognitive impairments (0–35) | 12.91 | 16.17*** | 15.62*** |
| Incontinence | 0.26 | 0.20*** | 0.20*** |
| Previous hospitalization | 0.33 | 0.32 | 0.29*** |
| Enabling (socioeconomic resources) | |||
| Less than high school education | 0.22 | 0.51*** | 0.67*** |
| Non-housing wealth ($10,000s) | 49.49 | 10.84*** | 12.45*** |
| Homeownership | 0.82 | 0.67*** | 0.64*** |
| Any Medicaid | 0.05 | 0.22*** | 0.35*** |
| Income ($10,000s) | 5.05 | 2.71*** | 2.21*** |
| Enabling (social and family ties) | |||
| Number of living children | 3.13 | 3.80*** | 4.19*** |
| Any living siblings | 0.78 | 0.78 | 0.88*** |
| £Marital status | |||
| Married (reference) | 0.60 | 0.40*** | 0.54*** |
| Widowed | 0.30 | 0.40*** | 0.29 |
| Divorced | 0.08 | 0.16*** | 0.13*** |
| Never married | 0.02 | 0.04*** | 0.04*** |
| £Proximity of children | |||
| Lives farther than 10 miles from child (reference) | 0.39 | 0.31*** | 0.28*** |
| Child lives within 10 miles | 0.47 | 0.39*** | 0.35*** |
| Lives with child | 0.14 | 0.30*** | 0.37*** |
| £Future help availability | |||
| No help available (reference) | 0.35 | 0.22*** | 0.30*** |
| Help available | 0.50 | 0.55*** | 0.48*** |
| Currently using help | 0.15 | 0.23*** | 0.22*** |
Notes. ADL = activities of daily living; HRS = Health and Retirement Study; I-ADL = instrumental activities of daily living.
*p < .05. **p < .01. ***p < .001.
Hazard Models: Risk of Entering Nursing Home During Study Period
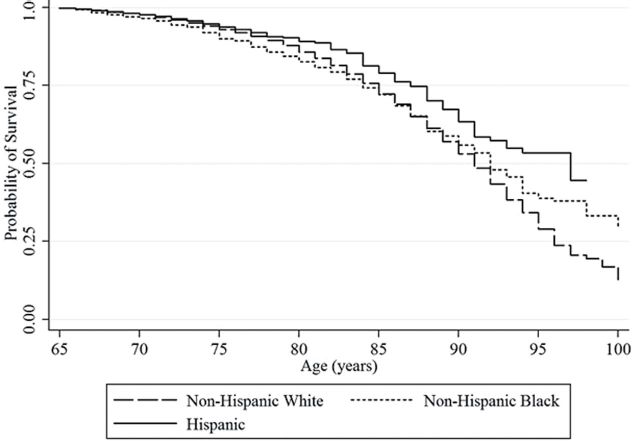
The baseline model is reported in Model 1 in Table 2. Hispanics have a 34% lower risk of entering nursing homes during the study period compared with non-Hispanic white adults (p < .001). Non-Hispanic black and non-Hispanic white respondents have statistically similar risks of nursing home admission. Figure 1 shows the baseline Kaplan–Meier survival estimates for entering a nursing home during the study period by race/ethnicity. This figure demonstrates that the risk of nursing home admission is significantly lower for Hispanics compared with the other groups.
Table 2.
Hazard Ratios for Entry into Nursing Home, HRS 1998–2010 (N = 18,952)
| Model 1 (baseline) | Model 2 (need) | Model 3 (enabling) | Model 4 (family-based alternatives) | Model 5 (full) | Model 6a (full with interactions) | |
|---|---|---|---|---|---|---|
| Predisposing (sociodemographics) | ||||||
| Race/ethnicity | ||||||
| Non-Hispanic white (reference) | ||||||
| Non-Hispanic black | 0.95 | 0.73*** | 0.61*** | 0.76*** | 0.70*** | 2.04 |
| Hispanic | 0.66*** | 0.53*** | 0.37*** | 0.56*** | 0.52*** | 1.03 |
| Women (ref = man) | 1.42*** | 1.26*** | 1.18*** | 1.09 | 1.06 | 1.11* |
| Woman × Non-Hispanic black | 0.69* | |||||
| Woman × Hispanic | 0.94 | |||||
| Birth year | 1.15*** | 1.14*** | 1.15*** | 1.13*** | 1.13*** | 1.13*** |
| Foreign born | 0.89 | 0.87 | 0.75*** | 0.85* | 0.79** | 0.90 |
| Foreign born × Non-Hispanic Black | 0.78 | |||||
| Foreign born × Hispanic | 0.58* | |||||
| Need (health and functioning) | ||||||
| ADL difficulties (0–6) | 1.18*** | 1.12*** | 1.12*** | |||
| I-ADL difficulties (0–3) | 1.41*** | 1.22*** | 1.20*** | |||
| Mobility difficulties (0–5) | 1.15*** | 1.06*** | 1.07*** | |||
| Number of cognitive impairments (0–35) | 1.02*** | 1.01* | 1.01** | |||
| Incontinence | 1.02 | 1.07 | 1.07 | |||
| Previous hospitalization | 3.68*** | 4.98*** | 5.14*** | |||
| Enabling (socioeconomic resources) | ||||||
| Less than high school education | 0.97 | 0.87** | 0.89* | |||
| Non-housing wealth (transformation) | 0.98*** | 1.00 | 1.01 | |||
| Non-housing wealth × non-Hispanic black | 0.97** | |||||
| Non-housing wealth × Hispanic | 1.01 | |||||
| Homeownership | 0.59*** | 0.69*** | 0.69*** | |||
| Any Medicaid | 2.50*** | 1.34*** | 1.39*** | |||
| Income (transformation) | 0.93*** | 0.95** | 0.94** | |||
| Enabling (social and family ties) | ||||||
| Number of living children | 0.97** | 0.97** | 0.97* | |||
| Any living siblings | 0.96 | 0.95 | 0.97 | |||
| Marital status | ||||||
| Married (reference) | ||||||
| Widowed | 1.56*** | 1.25*** | 1.22*** | |||
| Divorced | 1.83*** | 1.32*** | 1.36*** | |||
| Never married | 2.10*** | 1.51*** | 1.71*** | |||
| Never married × non-Hispanic black | 0.50* | |||||
| Never married × Hispanic | 1.06 | |||||
| Proximity of children | ||||||
| Lives farther than 10 miles from child (reference) | ||||||
| Child lives within 10 miles | 0.95 | 0.96 | 0.95 | |||
| Lives with child | 0.69*** | 0.68*** | 0.68*** | |||
| Future help availability | ||||||
| No help available (reference) | ||||||
| Help available | 0.79** | 0.84* | 0.86 | |||
| Help available × Non-Hispanic Black | 1.20 | |||||
| Help available × Hispanic | 0.37* | |||||
| Currently using help | 6.47*** | 2.20*** | 2.19*** | |||
| Log likelihood | −22231.737 | −20392.244 | −21835.873 | −21008.35 | −19943.711 | −18293.213 |
Notes. ADL = activities of daily living; HR = hazard ratio; HRS = Health and Retirement Study; I-ADL = instrumental activities of daily living.
aModel 6 adjusts for interactions between race–ethnicity categories and birth year, health and functioning variables, educational attainment, homeownership, Medicaid coverage, income, number of living children, any living siblings, being widowed, being divorced, proximity of children, and whether currently using help.
*p < .05. **p < .01. ***p < .001.
Figure 1.
Kaplan–Meier survival estimates for entering nursing homes after age 65 by race/ethnicity (N = 18,952; adjusted for birth year and gender).
In the next steps, we test whether need-based factors and enabling factors mitigate or suppress these racial–ethnic differences in nursing home admission. In Model 2 in Table 2, we fit the baseline models and the health and disability variables. As shown in Table 1, in general, Hispanics and non-Hispanic blacks report worse health and more disability than non-Hispanic whites. However, controlling for these differences magnifies the difference in nursing home admission risk between these groups. Including the need variables, which are overall positively associated with the risk of nursing home admission, modifies Hispanics’ risk of nursing home use such that Hispanics have almost a 50% lower risk of entering nursing homes compared with non-Hispanic whites. Non-Hispanic black respondents, who exhibit a similar risk of nursing home admission as non-Hispanic white respondents in the baseline model, have a 27% lower risk of entering nursing homes than non-Hispanic white respondents when health and disability variables are considered. The χ2 difference between these models is significant (p < .001).
In Model 3 in Table 2, we fit the baseline models and the enabling factors related to socioeconomic resources. There are mixed results in terms of how socioeconomic resources relate to nursing home admission: homeownership and lower levels of non-housing wealth and income significantly decrease the risk of nursing home admission, whereas being on Medicaid increases the risk. As with the need variables, adding socioeconomic resources to the model substantially increases the difference in risk of nursing home admission by race/ethnicity. This suppressor effect is even greater than it was when the need variables are added, as now Hispanics have a 63% lower risk of nursing home admission compared with non-Hispanic white respondents and non-Hispanic black respondents have a 39% lower risk. The χ2 difference between Model 3 and the baseline model is significant (p < .001).
In Model 4, we add the enabling factors related to social and family ties to the baseline model. Social and family ties, specifically number of living children, being married, living with a child, and having future help available if needed, lowers risk of nursing home admission, and currently having an informal caregiver increases risk of nursing home admission. Additional analysis demonstrates that this trend is mostly driven by the collinear association between worse health and disability and having a caregiver. In this model, as with the need-based model and the socioeconomic resources model, the inclusion of social and family ties exacerbates the gap between non-Hispanic whites’ risk of nursing home admission and non-Hispanic blacks’ and Hispanics’ risk of nursing home admission. The χ2 difference between Model 4 and the baseline model is significant (p < .001).
Overall, the models in Table 2 demonstrate that need and enabling variables serve as suppressors. Not including them in our models leads to underestimations of Hispanics’ and non-Hispanic blacks’ reduced risk of nursing home admission compared with non-Hispanic whites’. This is consistent with Hypothesis 1.
In the next step of our analyses to test Hypothesis 2, we examine whether the factors that place older persons at greater or lesser risk of nursing home admission differ across racial–ethnic groups. By interacting each variable across all categories with the race/ethnicity variables, we identify five variables with statistically significant interactions (gender, foreign born, non-housing wealth, never married, and future help available), indicating that the risk of nursing home admission based on these factors differs across racial and ethnic groups. These interactions are shown in Model 6 in Table 2. This model controls for all other possible interactions, although we only present significant interactions.
Interaction between gender and non-Hispanic black is significant (p < .05). This interaction demonstrates that gender relates to risk of nursing home admission among non-Hispanic whites and Hispanics, with women having an 11% higher risk of entering nursing homes in the full model compared with men, but among non-Hispanic blacks, there is an opposite pattern. Models stratified by race/ethnicity (not shown) indicate that non-Hispanic black women are actually 24% less likely to enter nursing homes than non-Hispanic black men, net of other variables. In regard to foreign-born status, there is a statistically significant interaction between being foreign born and Hispanic ethnicity (p < .001). Stratified models demonstrate that foreign-born Hispanics have a 41% lower risk of entering nursing homes than U.S.-born Hispanics. However, being foreign born does not predict nursing home admission for non-Hispanic white or non-Hispanic black respondents.
There are no significant interactions between need variables and race/ethnicity in estimating nursing home risk. Among enabling variables related to socioeconomic resources, we find that non-housing wealth does not predict nursing home risk for Hispanics or non-Hispanic whites in the full model. Stratified models demonstrate that among non-Hispanic blacks, there is a 3% lower risk of entering nursing homes during the study period for every extra transformed unit of non-housing wealth. Regarding enabling factors related to social and family ties, marital status also seems to matter differently for non-Hispanic blacks compared with Hispanics and non-Hispanic whites. In particular, although being never married increases risk of nursing home admission by about 70% for Hispanics and non-Hispanic whites compared with being currently married, for non-Hispanic blacks, there is no difference in nursing home risk between these two categories. Interactions further demonstrate that future help availability functions differently for Hispanics compared with non-Hispanic whites and non-Hispanic blacks. Among non-Hispanic whites and non-Hispanic blacks, having future help available does not affect nursing home risk compared with not having future help available. But among Hispanics, as found in the stratified models, having future help available decreases risk of nursing home admission by about 70% compared with not having help available.
Most variables are consistently significant across all racial and ethnic groups. Older age, ADL, I-ADL, mobility difficulties, cognitive impairments, previous hospitalization, any Medicaid, being widowed or divorced, and relying on a caregiver increase risk of nursing home use for all groups. Less than high school education, homeownership, higher income, more living children, and living with a child decreases nursing home risk similarly for all groups. In sum, we find some support for Hypothesis 2.
Discussion
This study contributes to our understanding of racial and ethnic differences in nursing home admission. Nursing home admission among non-Hispanic blacks and Hispanics is lower than we expected based on their physical need and relative to non-Hispanic whites. This is consistent with lower preferences for nursing home care among racial and ethnic minorities, perhaps due to cultural aversion or structural obstacles, but it could also indicate an underuse of nursing homes due to racial and ethnic health care inequity. Caring for older minorities is a major policy concern, as they face significant challenges stemming from features unique to their history, including immigration experiences and institutional and individual discrimination (Angel, Angel, Lee, & Markides, 1999; Angel, Torres-Gil, & Markides, 2012; Williams, 2012). As late-life Hispanic and non-Hispanic black families demographically shift and encounter new pressures (e.g., declining fertility, increases in women’s labor force participation, and geographic mobility) (Angel et al., 2012; Wallace et al., 1998), their members may be less able or willing to provide care for older relatives or face higher opportunity costs for engaging in this care, making increased access to formal long-term care a key issue. In our investigation, we take advantage of a nationally representative longitudinal sample to estimate the nursing home admission profiles for three racial–ethnic groups—non-Hispanic whites, non-Hispanic blacks, and Hispanics—that are rarely included within the same study.
Because we use an individual-level longitudinal data set, we go beyond past studies and examine whether racial–ethnic differences in need-based and enabling factors explain or confound the racial–ethnic differences in nursing home admission. We replicate previous work by demonstrating that Hispanics enter nursing homes less often than non-Hispanic whites (Baxter et al., 2001; Feng et al., 2011), and we expand current understandings of racial–ethnic disparities in nursing home admission by showing that Hispanics also use nursing homes less often than non-Hispanic blacks. These findings indicate that current nursing home admission by Hispanics is far below that of other groups especially when need-based and enabling variables are taken into account, suggesting that racial and ethnic differences in nursing home admissions persist. This draws attention to the necessity of examining Hispanic and non-Hispanic black adults as separate groups with distinctive nursing home admission profiles. We also find clear differences between non-Hispanic black and non-Hispanic white adults in terms of nursing home admission, with non-Hispanic black adults much less likely to enter nursing homes than non-Hispanic white adults. This trend occurs despite the fact that recent research has concluded that the racial gap in nursing home admission has closed (Miller & Weissert, 2000; Ness, Ahmed, & Aronow, 2004; Smith, Feng, Fennell, Zinn, & Mor, 2008). Our study demonstrates that unadjusted rates of nursing home admissions from these studies mask the reality that a profound racial difference in nursing home admission still exists.
We find these need-based factors suppress the full extent of racial–ethnic differences in nursing home admission. Non-Hispanic blacks and Hispanics have worse health and more disability than non-Hispanic whites (Angel et al., 2009; Ottenbacher et al., 2009), which would seem to indicate greater need for nursing homes among non-Hispanic blacks and Hispanics especially based on Andersen’s model (Andersen et al., 1983; Himes et al., 2000). However, our analysis demonstrates that taking the worse health and disability of non-Hispanic blacks and Hispanics into account only widens the differences in nursing home admission between non-Hispanic whites, non-Hispanic blacks, and Hispanics. Socioeconomic resources similarly suppress the full extent of racial–ethnic differences in nursing home admission. Non-Hispanic blacks and Hispanics have fewer socioeconomic resources than non-Hispanic whites (Mor, Zinn, Angelelli, Teno, & Miller, 2004), but rather than explaining nursing home differences across these groups, including socioeconomic resources magnifies these nursing home differences.
Put simply, these finding suggest two possibilities: (a) racial and ethnic minorities have similar preferences for nursing homes as non-Hispanic whites, but due to objective obstacles in access (e.g., geographic proximity), there is an underuse of nursing homes by non-Hispanic blacks and Hispanics based on their health profile, suggesting potential inequities or (b) racial and ethnic minorities have different preferences for nursing homes than non-Hispanic whites and either cultural differences (e.g., greater preference for family care) or structural obstacles (e.g., language barriers) make nursing home less desirable to them. We are unable to test these explanations with our data and call for future studies to examine these pathways.
As support for the possibility that our results demonstrate inequity in access to nursing homes, previous studies find that Hispanics and non-Hispanic blacks are being excluded from nursing homes due to institutional and individual discrimination, which may be more salient for some groups than others (Falcone & Broyles, 1994; Fennell et al., 2012). For instance, Hispanics who do not speak English may not be able to find a nursing home with Spanish language proficiency or may have trouble discussing nursing care options with a monolingual physician (Fennell et al., 2012). Additionally, nursing homes available to Hispanics and non-Hispanic blacks, as the result of geographic location, socioeconomic resources, and/or informal segregation, may be of lower quality than nursing homes for non-Hispanic whites, making them less viable options, which would lower rates of nursing home admission for racial–ethnic minority groups (Fennell et al., 2012; Mor et al., 2004).
Alternatively, racial–ethnic minorities may prefer informal care to nursing homes to a greater extent than non-Hispanic whites due to cultural norms encouraging family care and discouraging institutionalization (Frank, 2006). This sentiment may be shifting, though, because of new economic pressures. Increasingly, Hispanic women are working outside of the home (Dubeck & Borman, 1996), making caring for older family members a difficult task and possibly contributing to the rising rates of nursing home admission by Hispanics (Feng et al., 2011). This could mean that Hispanic families bear a disproportionate burden of care compared with other racial–ethnic groups, which will become more challenging as the population continues to age (Brown, Herrera, & Angel, 2013; Villa, Wallace, Bagdasaryan, & Aranda, 2012), contributing to increased caregiver strain for family members (Feng et al., 2011; Frank, 2006).
Beyond considering overall racial and ethnic differences in nursing home admission, as the second key contribution of this study, we test for interactions between individual variables and race/ethnicity. Most prior models of nursing home admission focus exclusively on non-Hispanic white Americans, at most including a control variable for race and/or ethnicity, assuming that the characteristics that increase non-Hispanic white Americans’ risk of nursing home admission also increase Hispanics’ and non-Hispanic blacks’ risks (Angel & Angel, 1997; Cagney & Agree, 1999; Dunlop et al., 2002; Friedman et al., 2005; Wallace et al., 1998). By testing interactions, we demonstrate that although most resources similarly structure nursing home admission across various racial and ethnic groups, there are important across-group differences in regard to other variables, specifically gender, being foreign born, non-housing wealth, never being married, and having future help available. Our preliminary analysis does demonstrate that evaluating nursing home admission with samples of only non-Hispanic whites or with all racial–ethnic groups pooled together could lead to poor estimates and demographic projections of future nursing home admission.
Previous studies conclude that women tend to enter nursing homes more than men (Friedman et al., 2005; Himes et al., 2000), but our study provides an important modification to this point. Among non-Hispanic blacks, nursing home admission risk is highest among men, once controlling for other factors. Future research should replicate this point to confirm its robustness and examine why gender differences are opposite for non-Hispanic blacks compared with non-Hispanic whites and Hispanics. Although older women are certainly overrepresented in nursing homes compared with older men, our study demonstrates that there may be some important differences across racial/ethnic groups in this feminization of nursing homes trend. We further find that U.S.-born Hispanics are much more likely to enter nursing homes than foreign-born Hispanics. Foreign-born Hispanics may face more discrimination and have more cultural aversion to nursing homes than U.S.-born Hispanics; thus, it makes sense that their nursing home admission is lower. Future analysis should examine how nursing home admission relates to both time spent in the United States and country of origin among a sample of Hispanics.
We find that only one component of socioeconomic resources, non-housing wealth, operates differently in how it is related to nursing home use for non-Hispanic whites and Hispanics compared with non-Hispanic blacks. Non-housing wealth is not related to nursing home admission for non-Hispanic whites and Hispanics, though it is a significant predictor for non-Hispanic blacks. For non-Hispanic blacks, non-housing wealth may signify an ability to stay in the community (e.g., ability to pay for home health care) (Martikainen et al., 2009; McCann et al., 2012), but for non-Hispanic whites and Hispanics, non-housing wealth may not carry these same meanings.
In terms of alternatives to nursing home admission, we observe larger families and households do not account for the difference between a higher need and lower nursing home admission for Hispanics as we and others have hypothesized (Akamigbo & Wolinsky, 2007; Lum, 2005; Scharlach et al., 2008) but that social and family ties suppress this association. Being divorced or widowed carries a similar nursing home risk for non-Hispanic blacks and the other racial–ethnic groups. Among non-Hispanic blacks, non-Hispanic whites, and Hispanics, divorce and widowhood are marital disruptions that increase nursing home risk, in line with the marital crisis hypothesis that focuses on the consequences from the stress involved with the ending of a marriage (Liu & Umberson, 2008). Among non-Hispanic whites and Hispanics, marriage itself seems to serve as a resource above and beyond representing the absence of marital dissolution, as demonstrated by the lower risk of nursing home admission for the married compared with the never married. But for non-Hispanic blacks, there is no difference between these groups, suggesting that for non-Hispanic blacks, there is no added benefit of being married compared with being never married, supporting previous research that finds that marriage is less protective for black adults than white adults against nursing home admission (Akamigbo & Wolinsky, 2007). This may result from the fact that kin (i.e., friends and family) serve as a functional substitute for marriage among the never married non-Hispanic blacks, in contrast with non-Hispanic whites and Hispanics, who accrue more protection against nursing home admission from a spouse than from other kin. Additionally, family care may occur within the context of nursing home care, and it is not necessarily the case that family care implies an underuse of nursing home care.
Our findings reveal important differences in how having future help available is related to nursing home admission across racial and ethnic groups—having future help available reduces risk of nursing home admission for Hispanics but not for non-Hispanic whites or non-Hispanic blacks when accounting for other variables. This is consistent with the idea that family and friends may be more important for Hispanics than non-Hispanics, especially when it comes to providing alternate care to nursing homes (Angel et al., 2004; Burton et al., 2010; Ibarra, 2003). Though about half of each racial–ethnic group expect that they will have help available if they need it, this help may be more substantial and salient for Hispanics compared with other groups, as indicated by its association with a statistical reduction in nursing home admission for Hispanics only.
This study’s unique contributions to understanding race–ethnicity and nursing home admission should be considered within the context of study limitations. Although this analysis is among the first to compare nursing home admission and factors predicting nursing home admission across three racial–ethnic groups using representative data, other racial–ethnic groups are notably absent, including Asian Americans and Native Americans. Further, because of sample size limitations, we do not examine country of origin among Hispanics, but rather combine Mexican-origin, Puerto Rican-origin, Cuban-origin, and other groups despite important between-group differences. Due to data limitations, we also do not include measures of discrimination, cultural aversion, or other factors that could explain differences in nursing home admission across racial and ethnic groups. We also do not examine whether those who do not enter nursing homes are receiving care from alternative sources (e.g., home health care). Differences in nursing home admission may signify use of this alternative care rather than unmet health care needs. Additionally, we do not examine length of stay in nursing homes and reason for nursing home visit (e.g., short-term rehabilitation, long-term care). Further, under the assumption that, on average, individuals and their families make the best and the most rational decisions about their health care, given the constraints they face, we certainly recognize the possibility that in many cases family care is better than the available nursing home care, and future studies should consider quality and availability of nursing homes as explanations for fewer nursing home admissions among particular groups.
Current and projected demographic shifts in age and racial–ethnic structure make this research, and other studies addressing racial–ethnic differences in nursing home admission, critically important. According to population projections, nursing home admission will increase over the next several decades, with one study predicting that the number of 65-year olds entering nursing homes will double by 2020 (Spillman and Lubitz, 2002; see also Lakdawalla et al., 2003). Much of this increase will likely be among Hispanics and non-Hispanic blacks, groups that are currently experiencing a rapid increase in their nursing home admission (Feng et al., 2011; Smith et al., 2008). Yet if fewer nursing home admissions by racial–ethnic minorities continue as we identify in our study, if racial–ethnic disparities in health and socioeconomic resources continue to grow (Kramarow, Lubitz, Lentzner, & Gorina, 2007), and if family size, living arrangements, and work patterns (e.g., women’s labor force participation) among minorities, Hispanics in particular, continue to change and become more similar to patterns observed for non-Hispanic whites (Dubeck & Borman, 1996), then it is likely that a sizeable number of Hispanic and black adults will be without formal, and possibly even informal, long-term care. This potential unmet need could create financial and emotional strain for family members and make those without kin particularly vulnerable. Additionally, aging adults living with their family members may receive suboptimal care, as families often lack knowledge and resources to help effectively navigate the medical system. Future research and policies should address these disparities and continue to highlight the unique health care needs of aging racial–ethnic minorities.
Funding
The research was supported by the NIH National Institute of Minority Health and Health Disparities grant (1 R01 MD005894-01).
Acknowledgments
M. B. Thomeer led data analysis and interpretation, wrote the paper, and participated in the conceptualization of the study. S. Mudrazija participated in the conceptualization of the study and contributed to statistical analysis, data interpretation, and manuscript writing. J. L. Angel originated the study and participated in its conceptual model, data interpretation, and manuscript writing.
References
- Akamigbo A. B., Wolinsky F. D. (2007). New evidence of racial differences in access and their effects on the use of nursing homes among older adults. Medical Care, 45, 672–679. 10.1097/MLR.0b013e3180455677 [DOI] [PubMed] [Google Scholar]
- Andersen R. M., McCutcheon A., Aday L. A., Chiu G. Y., Bell R. (1983). Exploring dimensions of access to medical care. Health Services Research, 18, 49–74. [PMC free article] [PubMed] [Google Scholar]
- Angel J., Hogan D. (2004). Population aging and diversity in a new era. In Whitfield K. (Ed.), Closing the gap: Improving the health of minority elders in the new millennium (pp. 1–12). Washington, DC: Gerontological Society of America. [Google Scholar]
- Angel J. L., Angel R. J., Aranda M. P., Miles T. P. (2004). Can the family still cope? Social support and health as determinants of nursing home use in the older Mexican-origin population. Journal of Aging and Health, 16, 338–354. 10.1177/0898264304264203 [DOI] [PubMed] [Google Scholar]
- Angel J. L., Angel R. J., McClellan J. L., Markides K. S. (1996). Nativity, declining health, and preferences in living arrangements among elderly Mexican Americans: Implications for long-term care. The Gerontologist, 36, 464–473. 10.1093/geront/36.4.464 [DOI] [PubMed] [Google Scholar]
- Angel J. L., Torres-Gil F., Markides K. (2012). Aging, health, and longevity in the Mexican-origin population. New York: Springer. [Google Scholar]
- Angel R. J., Angel J. L. (1997). Health services use and long-term care among Hispanics. In Markides K. S., Miranda M. R. (Eds.), Minorities, aging and health (pp. 343–366). Newbury Park, CA: Sage Publications. [Google Scholar]
- Angel R. J., Angel J. L., Hill T. D. (2009). Subjective control and health among Mexican-origin elders in Mexico and the United States: Structural considerations in comparative research. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64, 390–401. 10.1093/geronb/gbn029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angel R. J., Angel J. L., Lee G. Y., Markides K. S. (1999). Age at migration and family dependency among older Mexican immigrants: Recent evidence from the Mexican American EPESE. The Gerontologist, 39, 59–65. 10.1093/geront/39.1.59 [DOI] [PubMed] [Google Scholar]
- Baxter J., Bryant L. L., Scarbro S., Shetterly S. M. (2001). Patterns of rural Hispanic and non-Hispanic white health care use: The San Luis Valley Health and Aging Study. Research on Aging, 23, 37–60. 10.1177/0164027501231003 [Google Scholar]
- Brown H. S., III, Herrera A. P., Angel J. L. (2013). Opportunity costs associated with caring for older Mexican-Americans. Journal of Cross-Cultural Gerontology, 28, 375–389. 10.1007/s10823-013-9208-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burbidge J. B., Magee L., Robb A. L. (1988). Alternative transformations to handle extreme values of the dependent variable. Journal of the American Statistical Association, 83, 123–127. 10.1080/01621459.1988.10478575 [Google Scholar]
- Burton L. M., Bonilla-Silva E., Ray V., Buckelew R., Hordge Freeman E. (2010). Critical race theories, colorism, and the decade’s research on families of color. Journal of Marriage and Family, 3, 440–459. 10.1111/j.1741-3737.2010.00712.x [Google Scholar]
- Cagney K. A., Agree E. M. (1999). Racial differences in skilled nursing care and home health use: The mediating effects of family structure and social class. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54, 223–236. 10.1093/geronb/54B.4.S223 [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C., Proctor B. D., Smith J. C. (2009). Income, poverty, and health insurance coverage in the United States: 2009. Current population reports. Washington, DC: U.S. Census Bureau. [Google Scholar]
- Dubeck P. J., Borman K. M. (1996). Latinas in the U.S. labor force. In DuBeck P., Borman K. (Eds.), Women and work: A reader (pp. 38–41). New Brunswick, NJ: Rutgers University Press. [Google Scholar]
- Dunlop D. D., Manheim L. M., Song J., Chang R. W. (2002). Gender and ethnic/racial disparities in health care utilization among older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 57, 221–233. 10.1093/geronb/57.4.S221 [DOI] [PubMed] [Google Scholar]
- Elliott D. B., Krivickas K., Brault M. W., Kreider R. M. (2012). Historical marriage trends from 1890–2010: A focus on race differences. Washington, DC: United States Census Bureau. [Google Scholar]
- Falcone D., Broyles R. (1994). Access to long-term care: Race as a barrier. Journal of Health Politics, Policy and Law, 19, 583–595. 10.1215/03616878-19-3-583 [DOI] [PubMed] [Google Scholar]
- Feng Z., Fennell M. L., Tyler D. A., Clark M., Mor V. (2011). The Care Span: Growth of racial and ethnic minorities in US nursing homes driven by demographics and possible disparities in options. Health Affairs, 30, 1358–1365. 10.1377/hlthaff.2011.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fennell M., Clark M., Feng Z., Mor V., Smith D. B., Tyler D. A. (2012). Separate and unequal access and quality of care in nursing homes: Transformations of the research program for aging Hispanics. In Angel J. L., Torres-Gil F., Markides K. (Eds.), Aging, health and longevity in the Mexican-origin population (pp. 207–225). New York: Springer. [Google Scholar]
- Frank D. (2006). Hispanics shun nursing homes. The Hispanic Outlook in Higher Education, 16, 24–26. [Google Scholar]
- Freedman V. A. (1996). Family structure and the risk of nursing home admission. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 51, 61–69. 10.1093/geronb/51B.2.S61 [DOI] [PubMed] [Google Scholar]
- Freedman V. A., Berkman L. F., Rapp S. R., Ostfeld A. M. (1994). Family networks: Predictors of nursing home entry. American Journal of Public Health, 84, 843–845. 10.2105/AJPH.84.5.843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman S. M., Steinwachs D. M., Rathouz P. J., Burton L. C., Mukamel D. B. (2005). Characteristics predicting nursing home admission in the program of all-inclusive care for elderly people. The Gerontologist, 45, 157–166. 10.1093/geront/45.2.157 [DOI] [PubMed] [Google Scholar]
- Gaugler J. E., Duval S., Anderson K. A., Kane R. L. (2007). Predicting nursing home admission in the U.S: A meta-analysis. BMC Geriatrics, 7, 13. 10.1186/1471-2318-7-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrera A. P., George R., Angel J. L., Markides K., Torres-Gil F. (2012). Variation in Older Americans Act caregiver service use, unmet hours of care, and independence among Hispanics, African Americans, and Whites. Home Health Care Services Quarterly, 32, 35–56. 10.1080/01621424.2012.755143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himes C. L., Wagner G. G., Wolf D. A., Aykan H., Dougherty D. D. (2000). Nursing home entry in Germany and the United States. Journal of Cross-Cultural Gerontology, 15, 99–118. 10.1023/A1006797731500 [DOI] [PubMed] [Google Scholar]
- Ibarra M. L. (2003). The tender trap: Mexican immigrant women and the ethics of elder care work. Aztlan: A Journal of Chicano Studies, 28, 87–113. [Google Scholar]
- Juster F. T., Suzman R. (1995). An overview of the Health and Retirement Study. The Journal of Human Resources, 30, S7–S56. 10.2307/146277 [Google Scholar]
- Kramarow E., Lubitz J., Lentzner H., Gorina Y. (2007). Trends in the health of older Americans, 1970-2005. Health Affairs, 26, 1417–1425. 10.1377/hlthaff.26.5.1417 [DOI] [PubMed] [Google Scholar]
- Lakdawalla D., Goldman D. P., Bhattacharya J., Hurd M. D., Joyce G. F., Panis C. W. A. (2003). Forecasting the nursing home population. Medical Care, 41, 8–20. 10.1097/00005650-200301000-00003 [DOI] [PubMed] [Google Scholar]
- Liu H., Umberson D. J. (2008). The times they are a changin’: Marital status and health differentials from 1972 to 2003. Journal of Health and Social Behavior, 49, 239–253. 10.1177/002214650804900301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lum T. Y. (2005). Understanding the racial and ethnic differences in caregiving arrangements. Journal of Gerontological Social Work, 45, 3–21. 10.1300/J083v45n04_02 [DOI] [PubMed] [Google Scholar]
- Martikainen P., Moustgaard H., Murphy M., Einiö E. K., Koskinen S., Martelin T., Noro A. (2009). Gender, living arrangements, and social circumstances as determinants of entry into and exit from long-term institutional care at older ages: A 6-year follow-up study of older Finns. The Gerontologist, 49, 34–45. 10.1093/geront/gnp013 [DOI] [PubMed] [Google Scholar]
- McCann M., Grundy E., O’Reilly D. (2012). Why is housing tenure associated with a lower risk of admission to a nursing or residential home? Wealth, health and the incentive to keep ‘my home’. Journal of Epidemiology and Community Health, 66, 166–169. 10.1136/jech-2011-200315 [DOI] [PubMed] [Google Scholar]
- Miller E. A., Weissert W. G. (2000). Predicting elderly people’s risk for nursing home placement, hospitalization, functional impairment, and mortality: A synthesis. Medical Care Research and Review, 57, 259–297. 10.1177/107755870005700301 [DOI] [PubMed] [Google Scholar]
- Miner S. (1995). Racial differences in family support and formal service utilization among older persons: A nonrecursive model. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 50, 143–153. 10.1093/geronb/50B.3.S143 [DOI] [PubMed] [Google Scholar]
- Mor V., Zinn J., Angelelli J., Teno J. M., Miller S. C. (2004). Driven to tiers: Socioeconomic and racial disparities in the quality of nursing home care. The Milbank Quarterly, 82, 227–256. 10.1111/j.0887-378X.2004.00309.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ness J., Ahmed A., Aronow W. S. (2004). Demographics and payment characteristics of nursing home residents in the United States: A 23-year trend. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 59, 1213–1217. 10.1093/gerona/59.11.1213 [DOI] [PubMed] [Google Scholar]
- Noël-Miller C. (2010). Spousal loss, children, and the risk of nursing home admission. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65, 370–380. 10.1093/geronb/gbq020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottenbacher K. J., Graham J. E., Al Snih S., Raji M., Samper-Ternent R., Ostir G. V., Markides K. S. (2009). Mexican Americans and frailty: Findings from the Hispanic established populations epidemiologic studies of the elderly. American Journal of Public Health, 99, 673–679. 10.2105/AJPH.2008.143958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- RAND HRS Data. (2010). Santa Monica, CA: Rand Center for the Study of Aging. [Google Scholar]
- Scharlach A. E., Giunta N., Chow J. C., Lehning A. (2008). Racial and ethnic variations in caregiver service use. Journal of Aging and Health, 20, 326–346. 10.1177/0898264308315426 [DOI] [PubMed] [Google Scholar]
- Smith D. B., Feng Z., Fennell M. L., Zinn J., Mor V. (2008). Racial disparities in access to long-term care: The illusive pursuit of equity. Journal of Health Politics, Policy and Law, 33, 861–881. 10.1215/03616878-2008-022 [DOI] [PubMed] [Google Scholar]
- Smith D. B., Feng Z., Fennell M. L., Zinn J. S., Mor V. (2007). Separate and unequal: Racial segregation and disparities in quality across U.S. nursing homes. Health Affairs, 26, 1448–1458. 10.1377/hlthaff.26.5.1448 [DOI] [PubMed] [Google Scholar]
- Soldo B. J., Wolf D. A., Agree E. M. (1990). Family, households, and care arrangements of frail older women: A structural analysis. Journal of Gerontology, 45, S238–S249. 10.1093/geronj/45.6.S238 [DOI] [PubMed] [Google Scholar]
- Spillman B. C., Lubitz J. (2002). New estimates of lifetime nursing home use: Have patterns of use changed? Medical Care, 40, 965–975. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2009). Stata statistical software: Release 11. College Station, TX: Author. [Google Scholar]
- U.S. Census Bureau. (2010a). America’s families and living arrangements: 2010. Washington, DC: U.S. Department of Commerce. [Google Scholar]
- U.S. Census Bureau. (2010b). S2601A, characteristics of the group quarters population Retrieved from http://factfinder2.census.gov/legacy/aff_sunset.html
- Villa V. M., Wallace S. P., Bagdasaryan S., Aranda M. P. (2012). Hispanic Baby Boomers: Health inequities likely to persist in old age. The Gerontologist, 52, 166–176. 10.1093/geront/gns002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuchinich S., Teachman J., Crosby L. (1991). Families and hazard rates that change over time: Some methodological issues in analyzing transitions. Journal of Marriage and Family, 53, 898–912. 10.2307/352996 [Google Scholar]
- Wallace S. P., Levy-Storms L., Kington R. S., Andersen R. M. (1998). The persistence of race and ethnicity in the use of long-term care. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 53, 104–112. 10.1093/geronb/53B.2.S104 [DOI] [PubMed] [Google Scholar]
- Williams D. R. (2012). Miles to go before we sleep: Racial inequities in health. Journal of Health and Social Behavior, 53, 279–295. 10.1177/0022146512455804 [DOI] [PMC free article] [PubMed] [Google Scholar]