SUMMARY
Toxocara canis and T. cati are highly prevalent nematode infections of the intestines of dogs and cats. In paratenic hosts, larvae do not mature in the intestine but instead migrate through the somatic tissues and organs of the body. The presence of these migrating larvae can contribute to pathology. Toxocara larvae can invade the brains of humans, and while case descriptions of cerebral toxocariasis are historically rare, improved diagnosis and greater awareness have contributed to increased detection. Despite this, cerebral or neurological toxocariasis (NT) remains a poorly understood phenomenon. Furthermore, our understanding of cognitive deficits due to toxocariasis in human populations remains particularly deficient. Recent data describe an enhanced expression of biomarkers associated with brain injury, such as GFAP, AβPP, transforming growth factor β1 (TGF-β1), NF-L, S100B, tTG, and p-tau, in mice receiving even low doses of Toxocara ova. Finally, this review outlines a hypothesis to explore the relationship between the presence of T. canis larvae in the brain and the progression of Alzheimer's disease (AD) due to enhanced AD-associated neurodegenerative biomarker expression.
INTRODUCTION
Helminths of the genus Toxocara belong to the class Nematoda, order Ascaroidea, and superfamily Ascaridoidea. Among a total of 21 species within the Toxocara genus, 2 are of significant public health concern, namely, Toxocara canis and T. cati, for which dogs and cats, respectively, are the definitive hosts. After ingestion of food or water contaminated by infective Toxocara eggs, larvae hatch in the small intestine, penetrate the gut wall, and are transported to the liver and lungs via the blood circulation. Subsequently, the larvae undergo a further migration by the tracheal route to mature to adulthood in the small intestine. In general, patent infections occur in dogs 4 to 5 weeks after infection (1, 2) and in cats 8 weeks after infection (3). Dogs and cats may acquire patent infections throughout their lives through accidental ingestion of eggs or via consumption of encapsulated larvae within paratenic hosts. In addition, puppies, unlike kittens, may be infected by the transplacental route (4).
Surveys of T. canis in dogs demonstrate wide ranges of infection prevalences globally, with 86 to 100% prevalence in puppies and 1 to 45% prevalence in adults (5–9). Reports of the prevalence of T. cati infection include 38.3% of Spanish stray cats (10), 79% of stray cats in Denmark, and 91% of feral cats on farms in the United Kingdom (11). A recent study from Japan (12) indicated that in samples from 34 sandpits taken in the Tokyo metropolitan area, 41.2% (14/34 samples) were contaminated with T. cati eggs as examined by PCR analysis. T. cati may play a more important role in human toxocariasis than previously recognized; for example, a number of studies suggest that T. cati is the causative agent of ocular toxocariasis (OT) (11, 13).
Nonembryonated T. canis eggs are shed with the feces, and embryonation occurs in the soil over a period of 2 to 5 weeks, in a process which is influenced by both temperature and humidity (14). Infectivity of eggs occurs within 54 days at 12 to 18°C, whereas the time to attain infectivity is shortened to 14 days at 25 to 30°C. Toxocara eggs are extremely resistant to physical and chemical agents, and in temperate climates, they are able to survive well over winter, for 6 to 12 months. Survivability of eggs under moist, cool conditions may be as long as 2 to 4 years or more (15). However, several factors affect the development and survival of eggs, as well as the availability of eggs to potential hosts, including temperature, light, humidity, pH, the substrate and vegetation cover, and physical dispersal of eggs by definitive hosts or through the actions of birds, rainfall, flies, beetles, earthworms, and slugs. In addition, the potential role of drinking water and the recreational use of water in transmission cannot be ignored (16). Of particular note, Fan et al. (17) utilized T. canis embryonated eggs which had been preserved in 2% formalin for at least 14 months at 4°C to inoculate ICR outbred mice. Larvae recovered from the liver and brain at 469 days postinfection were still alive. Furthermore, these larvae were capable of causing various degrees of Th2-related granulomatous inflammatory injuries to internal organs, such as the liver and lungs, indicating that pathogenicity and infectivity were retained even after long-term storage in 2% formalin.
IMMUNODIAGNOSTICS IN INVESTIGATIVE CLINICAL PRACTICE
The fact that Toxocara larvae do not develop to maturity but remain as larvae within paratenic hosts, such as humans, has implications and challenges for diagnosis (18, 19). In such paratenic hosts, T. canis L3 larvae neither molt, grow, nor replicate and will wander through a number of internal organs in humans so as to cause neurotoxocariasis (NT), ocular toxocariasis (OT), or visceral larva migrans (VLM) (19, 20). Therefore, diagnosis in the context of investigative and clinical practice predominantly depends upon immunological techniques. These include an enzyme-linked immunosorbent assay based on T. canis larval excretory-secretory (TESELISA) antigens or the use of fractionated TES antigens for Western blotting (TESWB), although recombinant antigens used for both serological methods have also been produced and proven to be more specific than TES (21). Although the sensitivity and specificity of TESELISA are reported to be 91% and 86%, respectively, antigenic cross-reactivity greatly reduces accuracy, particularly in subtropical and tropical regions, where polyparasitism is common (19). In contrast, increased specificity can be obtained with TESWB due to reactivity to bands at 24 to 32 kDa that are specific to T. canis infection (19). The detection of IgG subclasses has been found to be more effective for immunodiagnosis of Toxocara sp. infection. In particular, IgG2 antibodies specific to the glycan of Toxocara excretory-secretory antigens yields the highest sensitivity, though at a reduced specificity (22), while the use of IgG4 as the secondary antibody significantly increases specificity (23). Since IgG4 may reflect prolonged antigenic stimulation (24), this antibody subclass could be useful for monitoring larval viability before and after treatment (25).
T. canis larvae can remain viable for prolonged periods in paratenic hosts, maintaining elevated levels of immunoglobulins (26); therefore, determining whether an infection is acute or chronic has remained a significant challenge to date. In toxocariasis, the avidity of specific IgG cannot be determined using specific IgM levels, as IgM antibodies are detected throughout infection (25).
Alternatives to traditional ELISA, such as methods of measuring antibody avidity, have been proposed (26, 27). Methods that measure antibody-binding properties in chronic infections, and their optimization, have been described (28). The avidity of antibodies increases from low to high during the course of infection. Based on this, a method to selectively unbind antibodies by utilizing chaotropic agents, which can disrupt the hydrogen bonding network between macromolecules, i.e., proteins, nucleic acids, and water molecules, by weakening the hydrophobic effect (29), is used to determine the age of a range of infectious diseases (30). This method has been shown to be useful for the diagnosis of toxoplasmosis seroconversion in women during pregnancy (31). Therefore, it seems promising for making a diagnosis of recent Toxocara infections by assessing the IgG avidity. One study has supported the view that high IgG avidity occurs in chronic infections and low IgG avidity in the early phase of infection (26). Furthermore, clinical observations among 11 Polish children suffering from acute toxocariasis described an initially low IgG avidity. Follow-up over a 6- to 12-month period revealed that specific IgG avidity levels increased significantly in all children except one (32). Nevertheless, further studies concerning whether IgG avidity is applicable as a diagnostic index of recent T. canis infection are required for validation of this method. Diagnosis can be reached definitively through biopsy of affected tissue, but biopsy specimens are rarely available. In contrast, in cases where toxocariasis is suspected, PCR detection of Toxocara sp. DNA sampled from affected tissues is applicable (33).
SEROPREVALENCE AND ASSOCIATED RISK FACTORS IN GENERAL POPULATIONS
A Brief Review of Global Seroprevalence
Worldwide seroepidemiological surveys as assessed by IgG antibody level reveal that human toxocariasis is among the most frequently occurring helminthiases. In Western countries, such as the G8 nations (United States, Japan, Canada, Germany, United Kingdom, Italy, France, and Russia), seroprevalence is highest in rural areas, ranging from 35% to 42%, and it falls to 15% to 20% in semirural zones and 2% to 5% in urban areas (25, 34). For example, even in the United States, Toxocara sp. infection is reportedly one of the important childhood zoonotic infections and is more prevalent in African American communities and individuals living in poverty (35). In contrast, higher seroprevalences are reported from developing countries, for example, Nigeria (30%), Brazil (36%), Swaziland (44.6%), Malaysia (58%) Indonesia (63.2%), Nepal (81%), Marshall Islands (86.8%), and La Reunion (93%) (36–39). However, an accurate analysis of seroprevalences between different countries and studies is hindered by the different methodologies used to detect infections (WB or ELISA), different cutoff titers, and the difficulties in linking infection, titers, and symptomatic disease (19, 40). Importantly, seroepidemiological data indicate that exposure to T. canis infection is widespread and, as a potential cause of significant disease, should not be ignored.
Risk Factors
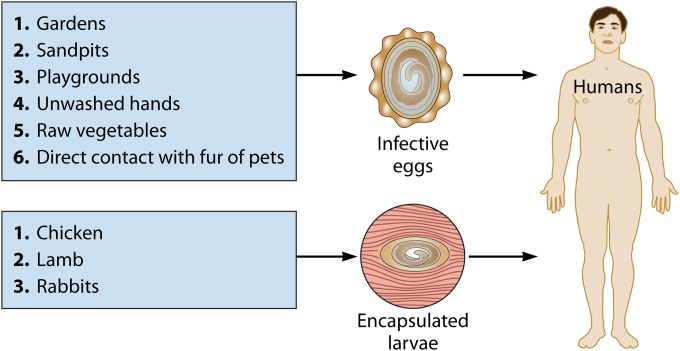
Humans may acquire T. canis infection by several routes, such as accidental ingestion of soil contaminated with eggs (playgrounds, sandpits, and gardens), from unwashed raw vegetables and hands, or from the hair of pet dogs and cats (Fig. 1) (20, 41). Infections caused by ingesting encapsulated larvae in raw or undercooked infected organs or muscle tissues from paratenic hosts, such as chicken, lamb, or rabbit, have been reported from adults in northeastern Asian countries, e.g., Japan or South Korea, albeit rarely (Fig. 1) (20, 42–49). However, successful infection is influenced by a number of exposure- and susceptibility-related factors, including cultural and socioeconomic factors, environmental, geographic, and host immunity, genetics, age, gender, nutrition, coinfection, and the behavior of human and definitive hosts (20, 50, 51). Additionally, international migration and urbanization, with urban areas now containing upward of 50% of the world's population, result in increased interactions between humans and definitive hosts, which contributes to Toxocara/toxocariasis being an ever-changing public health concern (50).
FIG 1.
Potential routes of transmission for Toxocara canis infection to humans via the oral route. Infection through consumption of chicken, lamb, or rabbit is rare.
Companion animals may provide benefits with regard to socialization and physical and mental well-being (52), but potential health hazards of T. canis infection related to pet ownership should be not overlooked (52). A variety of studies from different geographical locations have shown that embryonated T. canis eggs can be recovered from the coats of dogs, suggesting that exposure to dogs may increase the risk of infection to humans (41, 53–56). However, Keegan and Holland (57) demonstrated that owned dogs that had been cared for properly had very few eggs on their hair and that none of these were embryonated, suggesting that direct contact with such dogs is not a high risk factor for infection. Recently, a study from the United States, a country with more than 93 million cats and 77 million dogs (58), showed that both geographic and individual-level risk factors, e.g., pet ownership, are associated with Toxocara sp. seroprevalence (59). Additionally, problems with untreated and uncontrolled definitive hosts result in environments that are heavily contaminated with T. canis ova, which, along with geophagia, poor hygiene, lower education levels, and poverty, provide ideal transmission opportunities, particularly in warmer climates. Host genetics ultimately determines susceptibility or resistance to parasite infection through innate or acquired immunity (60). Therefore, the role of genetic factors and immunological parameters in predisposition to infection with helminths was recently emphasized (61), and the relevance of these observations to Toxocara sp. infection should be explored further.
TYPES OF HUMAN TOXOCARIASIS AND IMMUNOPATHOGENESIS
In human toxocariasis, migrating L3 T. canis larvae are responsible for the clinical syndromes observed. Larvae move through the bloodstream to various organs, including the liver, heart, lungs, kidneys, brain, muscle, and eyes. Symptomatic disease manifestations depend on the infection intensity, the duration of migration, the organs involved, and immune- and age-mediated host responses (20). Currently, both pediatric and adult patients with toxocariasis report a wide variety of inflammation-related conditions, such as asthma, pneumonia, lymphadenopathy, endomyocarditis, granulomatous hepatitis, generalized endophthalmitis, meningoencephalitis, and cutaneous manifestations (33, 62–69). Notably, the focus of much research has been on the role of T. canis in neuropathological disorders, particularly epilepsy (70–73). Quattrocchi et al. (72) demonstrated a highly significant association between people with epilepsy (PWE) and antibodies to Toxocara (see details in “Seizure,” below). However, Magnaval et al. concluded that cerebral invasion by T. canis larvae rarely induces a recognizable neurological syndrome in humans, but instead that infection is correlated with the association of a number of risk factors, including contact with dogs, which may result in repeated infections with small numbers of larvae (74). However, it was noted that a German woman with cerebral toxocariasis also presented with depressive symptoms and cognitive deficits (75). Exploration of the relationship occurring between host and parasite in the brain may elucidate the cryptic symptoms of human toxocariasis, with patients presenting with mental disability, epilepsy, and other central nervous system (CNS) disorders (18).
Due to the range of clinical manifestations of toxocariasis observed over the last 30 years, two main forms of human toxocariasis were established in 1988: VLM and OT (76). A third form, common or covert toxocariasis (CT), was described in 1992 and 1993 for patients who were seropositive and presented with weakness, gastrointestinal disorders, and lethargy (77, 78). Human toxocariasis is currently classified clinically into four types, including VLM, OT, CT, and NT (19, 20, 66). Regarding toxocariasis immunopathogenesis, TES antigens have been found to play a pivotal role in triggering granulomatous inflammation, a manifestation of delayed-type hypersensitivity mediated by Th1 cells, as well as IgE, eosinophilia, and enhanced cytokine expression (e.g., interleukin-13 [IL-13], IL-5, and IL-4) characteristic of Th2-mediated responses (79).
Immunological defenses of the host are influenced by a number of environmental and genetic factors and the interaction between them. Evidence suggests that infection with Toxocara is associated with a polarized CD4+ Th2 response with elevated IgE levels and eosinophilia, mediated by human leukocyte antigen (HLA) class II molecules. HLA class II molecules have been linked to disease severity and host genes affecting exposure-related behaviors (60). A role for Foxp3+ CD4+ CD25+ T regulatory (Treg) cells in the regulation of immunopathology, including granuloma development in murine models of toxocaral hepatitis, and in the enhanced expression of transforming growth factor β1 (TGF-β1) was recently suggested. TGF-β1 is important for the function and local survival of Treg cells during larval migration in the muscle, small intestine, brain, and liver of the mouse (80–82). The potential susceptibility loci of HLA class II molecules are considered to be involved in regulating Th2-dominant immunity (controlled by Foxp3+ CD4+ CD25+ Treg cells by stimulation through TGF-β1), creating an environment that benefits larvae but potentially contributes to organ damage (81). However, the immunological and molecular mechanisms associated with TGF-β1/Th2 responses resulting in protection against or resistance to Toxocara sp. invasion, along with associated pathological changes, need further investigation. Nevertheless, the TGF-β1 Leu10Pro variant has been highlighted as being significantly associated with microfilaria loads in human lymphatic filariasis disease (83), but whether this has a role in toxocariasis disease severity is not known.
Because the Th2-dominated granulomatous inflammatory response and the associated raised antibody titers and eosinophilia do not control or eliminate Toxocara sp. larvae, T. canis larvae per se may be capable of evading host immunological attacks (84). T. canis larvae contain a mucin-rich, highly labile surface coat which is shed when antibodies and/or eosinophils bind, allowing the parasite to escape from attack by the host's immunity (84). Although eosinophilia can frequently be seen in clinical toxocariasis, evidence is lacking for a protective role for eosinophils in toxocariasis, as larvae remain unharmed in mice overexpressing IL-5, to induce a resultant hypereosinophilia. In contrast, the intestinal nematode of mice Nippostrongylus brasiliensis is eliminated (85). Furthermore, when N. brasiliensis is introduced into transgenic IL-5 mice in the presence of TES antigens, the mouse survival rate is greatly enhanced (86). It appears that TES antigens are important in the orchestration of immune evasion/manipulation, which is likely to be a mechanism by which T. canis facilitates its long-term survival in the host (84). In addition, TES antigens are capable of killing T lymphocytes (Th2 cells) by triggering caspase-dependent apoptosis, as evidenced by enhanced caspase-9 expression in TES antigen-cocultured T lymphocytes in vitro (C.-K. Fan, unpublished data).
Visceral Larva Migrans
In 1952, Beaver and colleagues (87) used the term “visceral larva migrans” to describe a group of symptoms associated with eosinophilic granulomas containing Toxocara sp. larvae in the livers of children with anemia, respiratory symptoms, geophagia, enlarged liver, and extreme hypereosinophilia. Later experimental work in mice demonstrated that a high burden of larval infection or repeated infection may result in VLM (79). Although classical VLM typically occurs in young children, the frequency of VLM in adults is relatively high in northeastern Asian countries, e.g., South Korea and Japan, including those patients who became infected by eating raw beef, lamb, chicken, or ostrich liver (47–49).
Infected children may present with a persistent cough which can be treated with anthelminthics (88). However, most pathology associated with VLM occurs in the liver. In Brazil, a study of 24 autopsy cases of granulomatous lesions in the livers of children from the Children's Reference Hospital found that eosinophil-rich granulomas in 10 children (41.7%) stained positive with polyclonal anti-Toxocara serum (89). The pathological findings demonstrated that the hepatic granulomas possessed epithelioid cells and multinucleate giant cells forming a palisade around amorphous eosinophilic material or necrotic debris. Mononuclear cells and eosinophils were frequently observed in granuloma outer layers, and the study showed that the most frequent cause of granulomatous hepatitis in Brazilian children was VLM granulomas (89). In addition, in Poland, Hartleb and Januszewski (90) reported one female patient with chronic liver disease presenting as multiple small mass lesions and fibrous perihepatitis that was immunologically diagnosed to be caused by T. canis infection. Occasionally in toxocaral hepatitis, computed tomography detects low-density lesions as multiple nodules in the liver (67). The other potential clinical findings and symptoms include fatigue, headache, fever, vomiting, diarrhea, asthma, anorexia, weight loss, and abdominal pain (47).
While it is not obvious why symptomatic VLM develops, the involvement of the host immune response to larval antigens is of central importance. The immune response to the larval antigens includes elevated eosinophilia and hypergammaglobulinemia (eosinophils and IgG and IgE antibodies as manifestations of Th2-type cells) and cytokine production, e.g., secretion of IL-4, IL-5, and IL-13 by Th2-type cells. TES antigens are highly likely to prompt the induction of this population of Th2-type cells. The continued production of larval antigens stimulates the immune response, with the accompanying production of IgE antibodies and eosinophils. The main function of eosinophils is antibody-dependent elimination of large parasites through cell-mediated cytotoxicity (91). IL-5 regulates the accumulation of eosinophils in inflammatory tissues and modulates eosinophil maturation, recruitment, and survival. IL-4 induces B-cell class-switch recombination to IgG4 and IgE and upregulates production of major histocompatibility complex (MHC) class II molecules, while reducing production of gamma interferon (IFN-γ), IL-12, Th1 cells, and macrophages, as well as dendritic cell production of IL-12 (92). Tissue macrophages are important in wound repair and chronic inflammation. IL-4 in extravascular tissues induces the alternative, M2 form of macrophage activation and inhibits classical activation of macrophages into M1 cells, which differentiate in response to cytokines and express many characteristics of tissue macrophages (93). An increase in M2 macrophages, along with the simultaneous secretion of IL-10 and TGF-β, reduces damaging inflammation, resulting in further development of wound healing and/or fibrosis (94).
Ocular Toxocariasis
Wilder (95) first described ocular larva migrans (OLM) after detecting lesions containing larvae in the eyes of children with suspected retinoblastoma. OLM, which is currently named OT, is thought to be rare compared to VLM and results from infection with small numbers of T. canis larvae. OT has the highest incidence in young children from the age of 5 to 10 years (96), with damage to vision which is unilateral and accompanied by intermittent strabismus caused by T. canis L3 migration in the eye and resultant immune reactions (20). Accidental ingestion of small numbers of T. canis ova as a result of being consistently exposed to environments that are contaminated with ova may lead to OT, reflecting why Toxocara sp. antibody titers are usually lower in OT cases than VLM cases (96).
Fan et al. (20) reviewed case reports of toxocariasis from PubMed for the period between 1990 and 2012, which included 290 papers and 368 OT cases. The largest number of cases was in Europe (97), followed by Asia (98), North America (62), Latin America (27), Australia (5), and Tunisia (1). Japan, France, Brazil, and the United States had the largest numbers of reported cases in Asia, Europe, Latin America, and North America, respectively.
Although the manifestations of OT range from asymptomatic to severe (99), most reported cases have been accompanied by symptomatology. According to a review paper by Arevalo et al. (96), three major clinical types of OT syndrome have been suggested, based on the severity of manifestations, including diffuse nematode endophthalmitis, the peripheral inflammatory mass type, and the posterior pole granuloma type (100–102). In general, patients with OT have a normal white blood count, normal serum IgE level, and no eosinophilia (96). Substantial clinical evidence indicates that the most common presentation of OT is a granuloma found in the peripheral retina, seen in 50% to 64% of cases, with a posterior pole granuloma seen in 25% to 36% of cases and endophthalmitis seen in <25% of cases (102, 103). Over 50% of cases are unilateral ocular infections presenting with mild ocular inflammation, but if the infection is persistent, bilateral disease may be manifested (104). Stewart et al. (103) analyzed 22 patients from San Francisco with OT between 1977 and 1996, and they reported cases of acute inflammation (36.4%), chronic inflammation (31.8%), and recurrent inflammation (31.8%). Damage to vision occurs over days or weeks, with the location of the larvae, the extent of eosinophilia, and the possible development of a fibrotic granulomatous response determining the level of impairment. The presence of granulomas can result in blindness due to heterotopia and/or detachment of the macula and distortion (98, 105).
Visual impairment can be found in most cases of OT, that is, with a visual acuity of less than 20/40 at presentation (normal vision is commonly referred to as 20/20 vision), with a median between 20/200 and 20/400 in eyes with endophthalmitis, a median of 20/70 in eyes with peripheral granuloma, and a median of 20/50 in eyes with a posterior pole granuloma (103). Larvae are most commonly located in the peripheral retina and vitreous, with larvae occurring in one or both of these sites. An ill-defined, hazy white lesion may be observed in the periphery or posterior pole, with various degrees of vitreous inflammation. After resolution of the inflammatory reaction, the lesion appears as a well-defined elevated mass in the periphery, along with folding in the inner retinal layer which may extend toward the macula. Endophthalmitis does not produce much pain and causes minimal external damage, but it can be accompanied by marked vitritis, a secondary cataract, and a mild anterior chamber reaction (99). Macular detachment may result from uveitis that causes vitreomacular traction or epiretinal membrane and puckering of the macula. Traction may lead to retinal breaks in the atrophic retina, creating a combined tractional rhegmatogenous detachment. An optic papillitis can also occur, usually because of an invasion of the nerve by T. canis larvae or if there is inflammation due to the parasite being situated elsewhere in the eye (106). Gass et al. (107) first described diffuse unilateral subacute neuroretinitis (DUSN) due to Toxocara spp., and another possible presentation of OT, i.e., bilateral DSN, has also been suggested (107, 108). However, in prolonged Toxocara sp. infection, chorioretinitis may be followed by choroidal neovascular membrane formation (14). A recent study from Pennsylvania indicated that 22 of 604 patients within whom pseudoretinoblastomas were identified were found to have OT, indicating that ophthalmologists should avoid misdiagnosing OT as a retinoblastoma (109). A differential diagnosis between OT and retinoblastoma based on morphology, enhancement, calcification, demographics, signs, and complications has been suggested by Small and Schaefer (110) (Table 1). In fact, the diagnosis of OT remains challenging and, in the majority of cases, is only presumptive. Standard diagnostic methods for OT are fundoscopy, imaging, and serologic testing (102). Although the sensitivity and specificity of TESELISA for immunodiagnosis of VLM are fair, the sensitivity for diagnosis of OT syndrome is considerably lower (96). However, the detection of antibodies at any level will support a Toxocara uveitis diagnosis if the possibility complies with the clinical presentation (103, 111). Since establishment of the diagnosis of OT based solely on clinical features and serologic results is considered unreliable, some ophthalmologists recommend the addition of Toxocara sp. Goldman-Witmer coefficient (GW) determination [GW = (level of specific IgG in aqueous humor/level of specific IgG in serum)/(total IgG in aqueous humor/total IgG in serum)] to aid in patient diagnosis of idiopathic focal chorioretinitis or vitritis. A cutoff value of ≥3 for GW is considered to confirm intraocular antibody synthesis related to active Toxocara invasion (96, 104). Imaging studies, particularly ultrasound examination and computed tomography, are also useful (112).
TABLE 1.
Differential diagnosis between ocular toxocariasis and retinoblastomaa
| Parameter | Description |
|
|---|---|---|
| Ocular toxocariasis | Retinoblastoma | |
| Morphology | Centrally located mass with moderate enhancement revealed by MRI | Nodular in contour and lies along the posterior pole of the globe |
| Enhancement | Moderate uveoscleral enhancement or enhancement of a granuloma | Usually characterized by moderate or avid enhancement |
| Calcification | Rare | Punctate or speckled calcification in more than 90% of cases |
| Demographics | Patients usually 5–10 years of age | Observed before 5 years of age in more than 90% of cases, average age at diagnosis is ∼18 months |
| Signs and complications | Usually presents with unilateral visual loss, and pain and redness are common presenting symptoms | Leukocoria in more than half of cases; strabismus is the second most common presentation, occurring in ∼20% of cases |
Based on data from reference 110.
Coinfections with T. canis and other parasites, such as Toxoplasma gondii, may exacerbate impaired vision. As Toxocara spp. and T. gondii share a mode of exposure, i.e., soil ingestion, it was suggested that infections with these parasites may be correlated. A study utilized serum samples obtained during the U.S. Third National Health and Nutrition Examination Survey (NHANES III; 1988–1994), from children aged 12 years and younger, to determine the prevalence of antibodies to Toxocara spp. and T. gondii and to examine coinfection risk factors. After adjusting for risk and demographic factors by multivariate analysis, the results demonstrated that infection with Toxocara spp. was associated with almost twice the risk of infection with T. gondii (odds ratio [OR] = 1.93; 95% confidence limit [CL] = 1.61 to 2.31), and vice versa (OR = 1.91; 95% CL = 1.59 to 2.28) (113).
Risk factors for patients with OT include geophagy, consumption of snails and raw meat, convulsions, and prior ownership of dogs (114). Hayashi et al. (115) observed that the migratory route of T. canis larvae to the eye may be from the brain through the optic nerve, as assessed in one experimental study using a gerbil animal model (although the gerbil is not a natural paratenic host of T. canis). Other researchers postulated that it is more likely that larvae travel in blood vessels rather than by burrowing and that the route by which larvae reach the eye remains to be determined (103).
Treatment options for OT include the anthelmintic drugs albendazole and mebendazole. While data regarding the optimal duration of treatment are lacking, a 5-day course is generally sufficient. In cases where inflammation is present, corticosteroids should be prescribed. This is especially important to prevent scarring in OT patients, which may lead to permanent vision loss; therefore, patients should be monitored closely by an ophthalmologist, and surgery may be required. For example, Woodhall et al. (98) showed that cataracts are the second most common indication for surgical treatment (3 patients were treated with cataract surgery) in patients with ocular toxocariasis.
Covert or Common Toxocariasis
The observation of a high seroprevalence of Toxocara in many countries worldwide but a relatively small number of suspected VLM cases has led to the suggestion that clinical disease entities associated with toxocariasis, other than VLM and OT, are likely to exist (76). Evidence from two cross-sectional community studies, conducted in Ireland and France, resulted in a new clinical type of toxocariasis being described for seropositive adults and children who were asymptomatic or had mild or nonspecific symptoms. This became termed “common or covert toxocariasis” (76, 116, 117). In France, symptoms of toxocariasis in adults included breathing difficulties, rash, pruritus, weakness, and abdominal pain. Those patients showed elevated titers of anti-Toxocara antibodies, eosinophilia, and elevated total IgE levels. The syndrome was termed “common toxocariasis” in adults (117). The subjects were 37 adults living in the Midi-Pyrenees region of France and were age and sex matched with 37 hospital patients who served as controls. In Ireland, symptoms in children infected with Toxocara included pyrexia, loss of appetite, headache, nausea, emesis, lethargy, behavior and sleep disorders, abdominal pain, inflammation of the pharynx, pneumonia, cough, wheeze, itching, rash, limb pains, cervical lymphadenitis, pruritus, rash, and hepatomegaly. Normal blood eosinophil counts were found in 27% of patients exhibiting high anti-Toxocara titers. The syndrome in children was termed “covert toxocariasis” (76). The subjects were patients attending the National Children's Hospital, many of whom had asthma. To date, it remains a challenge to develop convincing diagnostic tests for CT, because most infections go undiagnosed due to less severe systemic manifestations and nonspecific laboratory abnormalities.
Neurotoxocariasis
The sites of CNS invasion by Toxocara larvae include the brain and spinal cord. Neurotoxocariasis (NT) is a CNS manifestation of Toxocara infection that is influenced by multiple factors, such as host genetic factors, the number of ingested ova, and previous exposure, all of which contribute to the complex pathogenesis of NT (20, 118). CNS toxocariasis in humans was first described by Beautyman and Woolf (119) in an autopsy study of a child who died of poliomyelitis, in whom a larva was found in the left thalamus. Beaver et al. (87) proposed the term VLM to account for the disease in children with long-term multisystem disease and eosinophilia. Thereafter, Nichols et al. (120) first identified and gave a full description of the egg, larva, and adult worm morphology of Toxocara spp., the causative agents of toxocariasis.
Magnaval et al. (74) conducted a case-control study and found that T. canis larval invasion of the brain rarely induces recognizable neurological signs, which may be explained by repeated low-dose infections. However, due to improved diagnosis, an increasing number of clinical NT cases due to larval invasion of the brain or spinal cord have been recorded over the last 30 years. Associated neurological damage and consequent epilepsy, neuropsychologic deficits, eosinophilic meningoencephalitis, myelitis, and cerebral vasculitis have been described (18, 33, 121). While our understanding of the mechanisms underlying human NT is incomplete, seroepidemiological surveys demonstrate high levels of exposure to Toxocara in the population, suggesting that NT may be an underestimated public health implication of infection (36). Recently, Toxocara was described as “America's most common neglected infection of poverty and a helminthiasis of global importance” (115, 122); however, the number of cases of NT will tend to be underestimated due to nonspecific clinical signs compared with VLM, as well as due to a lack of availability of appropriate testing, thus leading to possible underdiagnosis (18, 122).
Nevertheless, examination of cerebrospinal fluid (CSF) samples is worthwhile in the exploration of suspected CNS toxocariasis with abnormal neurological symptoms, since many NT cases show negative antibody levels in blood but positivity in CSF (123). The rule appears to be lower serum antibody titers than CSF antibody titers, particularly in the more common toxocaral myelopathy form of the disease (124–126). It should be noted that an antibody reaction in the serum is an unreliable indicator for evaluating disease activity in the CNS, as reactivity persists after clinical recovery (63). Some studies have outlined diagnostic criteria for NT that include high titers of antibodies to T. canis in the serum (evaluated by TESELISA or TESWB), eosinophilia in CSF or blood, intrathecal production of antibodies to T. canis, and a history of exposure to dogs (123).
However, the possibility of baylisascaris as a differential diagnosis for cerebral toxocariasis must not be overlooked. The nematode Baylisascaris procyonis infects the raccoon (Procyon lotor) and may rarely cause neural larva migrans (NLM), which can be devastating neurologically, or even fatal, in young children (127). B. procyonis larvae, unlike those of Toxocara, continue to grow within inappropriate hosts, e.g., humans (127). Patients with B. procyonis NLM often present with an eosinophilic meningoencephalitis that is severe and acute, with severe seizures that are frequent and difficult to control. Visual impairment and blindness often occur, with the majority of patients requiring complete nursing care. Diagnosis of CT versus B. procyonis NLM may include at least two diagnostic criteria. The first criterion is the the larger size of B. procyonis larvae (average length in the 2nd stage, 300 μm) and their capacity for continued growth and development during migration through the host, with B. procyonis larvae reaching lengths of 1,500 to 1,900 μm and diameters of 60 to 80 μm in the 3rd stage. In contrast, T. canis larvae reach lengths of 350 to 445 μm and a diameter of 20 μm, and notably, larvae in paratenic hosts undergo no growth (127). Second, antibodies generated against B. procyonis infection appear to selectively recognize periodate-resistant (protein) epitopes of larval ES antigens with molecular masses of 33 kDa to 45 kDa, which are not recognized by T. canis antibody-positive or normal sera (128). Additionally, several studies have confirmed that sera and CSF of children infected with B. procyonis test positive for antibodies to Baylisascaris while consistently being negative for anti-Toxocara antibodies (129–131).
Clinical drug trials for CNS toxocariasis treatment are lacking (126). Albendazole's lower toxicity than that of other anthelmintics and its good penetration of nervous tissues make it the medication of choice (123). Nevertheless, anthelmintic therapy may have side effects due to inflammatory reactions and edema resulting from Herxheimer's reaction (a rapid response to endotoxins released by the death of T. canis larvae within the body), and corticosteroids may be required from the beginning of the treatment. There have not been any studies that have proven that combined treatment with albendazole and corticosteroids is superior to single therapy (125). Corticoids may be considered in the case of immune vasculitis, though this condition is quite rare and difficult to identify (132).
GLOBAL CASES OF HUMAN CEREBRAL TOXOCARIASIS WITH VARIOUS NEUROLOGICAL DISORDERS FROM 1985 TO 2014
Since the accuracy of various diagnostic approaches for the detection of NT cases has improved greatly over the last 30 years, we undertook a search using some keywords, e.g., “T. canis,” “toxocariasis,” “brain,” and “CNS,” to determine the number of NT cases recorded in PubMed from 1985 to June 2014, and we found that 86 patients with various neurological manifestations have been recorded (Table 2).
TABLE 2.
Neurological manifestations in neurotoxocariasis cases from 1985 to June 2014a
| CNS involvement | Neurological manifestation; patient description | Diagnostic tests and findings | Medication | Country | Reference |
|---|---|---|---|---|---|
| Brain | Cerebral vasculitis; 66-year-old woman | 11% eosinophils in CSF; anti-T. canis IgG antibody in the blood and CSF (ELISA, WB) | Improved spontaneously without any anthelmintic treatment | France | 230 |
| Cerebral vasculitis; 75-year-old woman | 50% eosinophils in blood; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA, WB) | Albendazole plus dexamethasone | Austria | 231 | |
| Cerebral vasculitis; 45-year-old man | Anti-T. canis IgE antibody in the blood and CSF (ELISA); cerebral angiography | Unknown | France | 144 | |
| Cerebral vasculitis; 49-year-old man | Anti-T. canis IgE antibody in the blood and CSF (ELISA) | Anthelmintic treatment | France | 144 | |
| Eosinophilic meningitis; 11-year-old girl | 30% eosinophils in CSF; anti-T. canis IgG antibody in the blood (ELISA) | Diethylcarbamazine | Britain | 232 | |
| Eosinophilic meningitis; 17-year-old boy | 75% eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Albendazole | South Korea | 49 | |
| Eosinophilic meningitis; 54-year-old man | Computed tomography; anti-T. canis IgG antibody in blood (WB) and Toxocara DNA in CSF | Albendazole plus corticosteroids | Italy | 33 | |
| Eosinophilic encephalitis; 48-year-old woman | 57% eosinophils in blood; MRI; computed tomography; indirect immunofluorescence test; IQ of 90 reduced to 55 (WIP) | Diethylcarbamazine plus fenbendazole plus prednisone | Germany | 132 | |
| Eosinophilic meningoencephalitis; 18-year-old man | Eosinophilia in blood; computed tomography; anti-T. canis IgG antibody in the blood (ELISA) | Thiabendazole plus dexamethasone | Brazil | 233 | |
| Eosinophilic meningoencephalitis; 2-year-old boy | 58% eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Albendazole plus dexamethasone | Brazil | 63 | |
| Eosinophilic meningoencephalitis; 54-year-old woman | 36% eosinophils in CSF; computed tomography; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Albendazole plus methylprednisolone | Greece | 118 | |
| Eosinophilic meningoencephalitis; 5-year-old girl | 57% eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Albendazole | Brazil | 234 | |
| Eosinophilic meningoencephalitis; 45-year-old man | 70% eosinophils in blood; computed tomography | Albendazole plus prednisolone | France | 235 | |
| Eosinophilic meningoencephalitis; 54-year-old woman | 10% eosinophils in CSF; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Albendazole plus methylprednisolone | USA | 236 | |
| Bilateral subdural hematoma and a small subarachnoid hemorrhage; 2.5-year-old infant autopsy | NA | NA | Britain | 143 | |
| Fibrotic arachnoidea; 53-year-old woman | Granulomatous mass with Toxocara larva identified by histopathology | Surgery | Italy | 237 | |
| Cerebral meningoradiculitis | Eosinophilia in the CSF; anti-T. canis IgG antibody in the blood and CSF (immunodiagnostic) | Unclear | France | 238 | |
| Seizure; 1-year-old boy | 58% eosinophils in blood; computed tomography; anti-T. canis IgG antibody in the blood (ELISA) | Thiabendazole plus prednisolone | USA | 182 | |
| Seizure; 26-year-old woman | 6% eosinophils in blood; computed tomography; cranial MRI; anti-T. canis IgG antibody in the blood (ELISA) | Diethylcarbamazine | Germany | 137 | |
| Epileptic seizure; 7-year-old girl | 9% eosinophils in blood; computed tomography scan and MRI; T. canis larva identified in histological section | Mebendazole | Poland | 239 | |
| Seizures; 13-year-old girl | Computed tomography scan, MRI, histopathology | Albendazole | India | 181 | |
| Epileptic seizure; 11-year-old girl | 9.5% eosinophils in blood; computed tomography scan, MRI; anti-T. canis IgG antibody in the blood (ELISA) | Albendazole | Switzerland | 70 | |
| Cognitive impairments and dementia; 65-year-old woman | Eosinophilia in CSF; computed tomography; EEG; anti-T. canis IgG antibody in the CSF (ELISA) | Albendazole | Germany | 75 | |
| Cognitive impairments; 45-year-old man | Normal eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (WB) | Albendazole plus prednisolone | Germany | 2 | |
| Spinal cord | Myelitis; 43-year-old woman | 8% eosinophils in blood; T. canis larva detected in CSF | Thiabendazole | China | 124 |
| Myelitis; young woman | Eosinophilia in blood and CSF; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Diethylcarbamazine | France | 147 | |
| Myelitis; 23-year-old woman | 11% eosinophils in CSF; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Thiabendazole plus mebendazole plus dexamethasone | USA | 145 | |
| Myelitis; 58-year-old man | 50% eosinophils in blood; MRI; anti-T. canis IgG antibody in the blood (ELISA) | Mebendazole plus methylprednisolone | Belgium | 240 | |
| Myelitis; 54-year-old woman | 40% eosinophils in CSF; spinal MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Mebendazole plus methylprednisolone | Belgium | 125 | |
| Transverse myelitis; 5-year-old boy | 57% eosinophils in CSF; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Thiabendazole for 15 days | Brazil | 234 | |
| Transverse myelitis; 5-year-old girl | 15% eosinophils in blood, 57% eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Thiabendazole for 14 days plus albendazole for 10 days | Brazil | 234 | |
| Myelitis; 32-year-old woman | 50% eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Mebendazole | France | 241 | |
| Myelitis; 37-year-old woman | 11% eosinophils in CSF; brain MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Albendazole | Japan | 134 | |
| Myelitis; 40-year-old woman | 10% eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA, WB) | Albendazole plus prednisolone | Japan | 134 | |
| Myelitis; 8 men (mean age, 48.5 yr) | MRI; anti-T. canis IgG antibody in the blood (ELISA) | Albendazole plus steroid/no improvement | South Korea | 114 | |
| Myelitis; 14 men (42.8 ± 11.0 yr) and 3 women (31.0 ± 9.9 yr) | 47.1% of patients with eosinophilia in blood; MRI | Albendazole plus steroids | Lebanon | 138 | |
| Lower motor neuron disease; 51-year-old man | Normal eosinophil counts in blood and CSF; anti-T. canis IgG antibody in the blood and CSF (ELISA, WB) | Albendazole plus diethylcarbazine (LMND remained in progress) | Austria | 242 | |
| Eosinophilic meningoencephalomyelitis; 21-year-old woman | 30% eosinophils in CSF; anti-T. canis IgG antibody in the blood and CSF (ELISA, WB) | Diethylcarbamazine plus prednisolone | Japan | 148 | |
| Meningomyelitis; 49-year-old man | 37% eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Albendazole plus steroids | Germany | 146 | |
| Eosinophilic meningomyelitis; 39-year-old man | >40% eosinophils in CSF; MRI | Albendazole plus prednisolone | Germany | 123 | |
| Encephalomyelitis; 2-year-old girl | 11% eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Thiabendazole plus prednisolone | Brazil | 243 | |
| Intracranial and intraspinal abscesses; 38-year-old man | 26% eosinophils in blood; MRI; computed tomography scan; Toxocara larva was identified | Lost to follow-up | India | 244 | |
| Encephalomyelitis; 45-year-old man | 21% eosinophils in blood and 9% eosinophils in CSF; MRI; anti-T. canis IgG antibody in the blood and CSF (ELISA) | Albendazole plus methylprednisolone | Belgium | 135 | |
| Chronic Viliuisk encephalomyelitis; 3 males and 17 females (51.9 ± 14.0 yr) | 13 patients had eosinophilia in blood; MRI; anti-T. canis IgG antibody in the blood and CSF (WB) | No treatment records described | Sakha Republic | 151 |
NA, not available; WIP, a shortened form of the Wechsler intelligence test; LMND, lower motor neuron disease.
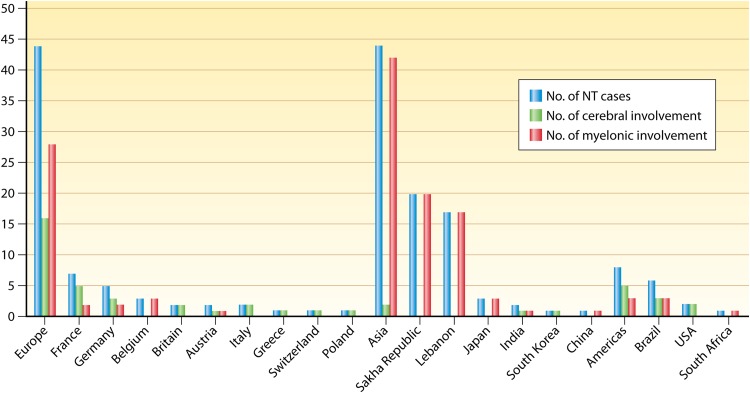
Cerebral injury was recorded for a total of 24 clinical cases (28%), including 6 cases of eosinophilic meningoencephalitis, 5 cases of seizure, 4 cases of cerebral vasculitis, 3 cases of eosinophilic meningitis, 2 cases of cognitive impairment, and 1 case each of eosinophilic encephalitis, fibrotic arachnoidea, bilateral subdural hemorrhage with subarachnoid hemorrhage, and cerebral meningoradiculitis (Table 2). With respect to manifestations of spinal cord involvement, a total of 62 clinical cases (72%) have been reported, including 35 cases of myelitis, 20 cases of Viliuisk encephalomyelitis (VE) (see details in “Myelitis,” below), 5 cases of (meningo)encephalomyelitis, and 1 case each of lower motor neuron disease and spinal abscess (Table 2). Note that some cases of myelopathy, urinary retention, and bowel dysfunction were reported, because T. canis larvae may cause compressive and noncompressive pressure to the spinal cord, resulting in myelopathy (133–135). Further analysis of the clinical NT cases listed in Table 2 demonstrated that Europe and Asia had the same number of cases (44 cases), followed by the Americas, with 8 cases. Only one case was reported from Africa (South Africa) (Fig. 2). Distribution by country revealed that Sakha Republic, Lebanon, and France reported the largest numbers of NT cases (20, 17, and 7 cases, respectively) (Fig. 2). The number of cases with cerebral involvement revealed that Europe had the largest number (16 cases), followed by 5 cases in the Americas and 2 cases in Asia (Fig. 2). In contrast, cases with myelonic involvement were highest in Asia (42 cases), Europe (28 cases), and the Americas (3 cases), with only 1 case reported from Africa (Fig. 2). These patients with NT, with either cerebral or myelonic involvement, were predominantly adults. The average age for 86 patients with NT was 41.3 ± 16.7 years, and males (41.6 ± 14.6 years) and females (41.0 ± 18.7 years) had similar ages. The average age of patients with cerebral involvement was 34.7 ± 23.6 years, and female patients (37.5 ± 25.7 years) were older than male patients (30.7 ± 21.1 years); in patients with myelonic involvement, the average age was 43.7 ± 12.8 years, and male patients (44.7 ± 9.4 years) were older than female patients (42.6 ± 14.8 years).
FIG 2.
Numbers of neurotoxocariasis (NT) cases—totals and those with cerebral and myelonic involvement—analyzed among 86 clinical NT cases in the PubMed database from 1985 to 2014, by continent and country distributions, ranked from the largest to the smallest number (within each continent distribution). Sakha Republic is one of the 10 autonomous Turkic Republics within the Russian Federation.
As shown in Table 2, 41% (35/86 cases) and 24% (21/86 cases) of NT cases had eosinophilia detected in blood and CSF, respectively, emphasizing the importance of eosinophilia as a diagnostic criterion for NT (121). Moreover, most NT cases can be detected by medical imaging techniques. Imaging techniques such as computed tomography and magnetic resonance imaging (MRI) are very useful tools for detecting and localizing lesions caused by migrating Toxocara sp. larvae in neural tissues, thus supporting a tentative diagnosis of NT (134–137). In fact, the more sensitive MRI method can reveal granulomas as hyperintensities on T2-weighted MRI sequences, located mainly cortically or subcortically in brain areas (134, 137, 138).
To conclude, although there are clearly increasing numbers of reports of cerebral or myelonic injury cases caused by T. canis, it remains perplexing that the exact prevalence of CNS involvement in toxocariasis is currently unknown, and information on the impact of NT on human neuropsychology remains sorely lacking (18, 121).
Eosinophilic Meningoencephalitis, Meningitis, and Encephalitis
Of the NT cases listed in Table 2, there are 5 cases of eosinophilic meningoencephalitis, 3 cases of eosinophilic meningitis, and 1 case of eosinophilic encephalitis, and all of them presented with eosinophilia in the blood or CSF. Clinical cerebral toxocariasis disease is associated with the severity of inflammation and damage caused to the CNS and with the number of larvae invading the brain (139). The symptoms of eosinophilic meningitis were described by Vidal et al. (63) for a 2-year-old boy who presented with mental confusion, fever, headache, tachycardia, hyperreflexia, dyspnoea, lethargy, irritability, motor weakness, and nuchal rigidity. Initial lumbar puncture revealed 23% eosinophils in the CSF (the level is <1% under healthy conditions), and thereafter, an eosinophilic pleocytosis persisted in the CSF. Both IgG antibodies in CSF and serum were reactive to T. canis. MRI of the brain identified a single hyperintense lesion, and an electroencephalogram (EEG) showed severe diffuse cerebral involvement. Treatment in the form of albendazole combined with corticosteroids was given, and the general condition of the boy at a 3-month follow-up was improved, though he showed some motor weakness and poor muscle tone in the lower limbs, as well as moderate paralysis and uncontrolled spasms in the right arm.
Xinou et al. (118) described a woman aged 54 years presenting with gait disturbance, clumsiness in the left arm, behavioral disorders, and an eosinophilia of 36%. EEG showed a diffusely, mildly slowed background and focal slow activity in and from the left hemisphere. T2-weighted MRI showed multiple hyperintense lesions in the occipital and right frontal lobes, which computed tomography examination showed as hypodense areas in the white matter. The serum was positive for IgG antibodies against T. canis, but the CSF was negative. The patient's condition improved rapidly after an initial treatment scheme combining albendazole and methylprednisolone, except for some residual clumsiness and weakness of the left arm.
Cerebral T. canis infections may rarely manifest as eosinophilic encephalitis. Sommer et al. (132) reported a 48-year-old patient with T. canis encephalitis presenting with ataxia, rigor, and disturbances of memory and concentration. Imaging revealed both localized and diffuse white matter lesions and middle cerebral artery branch occlusion. Anthelmintic therapy was effective initially, but due to progression of CNS symptoms, immunosuppressive therapy and corticosteroids were given.
In addition to serological or molecular diagnostic methods, medical imaging techniques, such as computed tomography and MRI, are important for the detection and localization of lesions caused by migrating Toxocara sp. larvae in neural tissues (134–138). MRI images of the brain may show clearly defined, multifocal lesions with strong contrast enhancement or, for persistent infections, both diffuse and circumscribed changes, but these are nonspecific findings. Several reports provided descriptions of imaging of cerebral toxocariasis cases, including numerous cortical, subcortical, or white matter lesions that were hyperintense on T2-weighted MRI images, hypoattenuating on computed tomography scans, and homogeneously enhancing. It was noted that the center of one occipital lobe lesion was hyperattenuating on computed tomography scans and hyperintense on both T1- and T2-weighted MRI images, which was suggestive of microhemorrhages or cortical necrosis due to cerebral infarction. Granulomas on the initial MRI also showed strong homogeneous enhancement, possibly due to a localized disruption of the blood-brain barrier (BBB) as a result of inflammation (118, 135, 138).
There is no general agreement on the usefulness of corticosteroids for the treatment of CNS toxocariasis. Prednisolone was shown to have a beneficial effect on eosinophilic meningitis due to the nematode Angiostrongylus cantonensis, suggesting a role for corticosteroids in the treatment of T. canis eosinophilic meningitis (140). In addition, Jung et al. (141) demonstrated that the efficacy of albendazole could be increased approximately 50% by simultaneous administration of dexamethasone. Some studies have indicated that patients with intense inflammatory responses causing serious neurologic symptoms benefit from corticosteroid therapy (142), although some case reports of toxocariasis symptoms, e.g., granulomatous lesions or meningitis (without encephalitis), have described spontaneous remission with anthelmintic treatment alone (143). Since numerous clinical NT case reports describe eosinophilia in the blood or CSF, the role of eosinophils in tissue larval killing and elimination is currently unclear.
Cerebral Vasculitis
A total of four cases of cerebral vasculitis are described in Table 2. However, only one case was documented by cerebral angiography, revealing multiple small branch occlusions in the middle cerebral artery, with multiple consecutive cerebral infarcts (144). In another case, Xinou et al. (118) detected cerebral infarction near cerebral granulomas. Cerebral vasculitis can develop during anthelmintic treatment, and whether infarctions are caused by a type IV (delayed) hypersensitivity to anthelmintic therapy or an acute inflammatory response to the antigen remains to be elucidated (118).
Myelitis
The effects of Toxocara larvae on the spinal cord have been reported repeatedly, and the injury is not limited to myelitis alone (125, 145) but is also concomitant with encephalitis or meningitis (146) (Table 2). Sellal et al. (147) described a young French woman presenting with recurrent myelitis. Eosinophilia and anti-T. canis IgG antibodies were detected in serum and CSF, and VLM was suspected. There was a good response to treatment with diethylcarbamazine. Another report concerned a 21-year-old Japanese woman who had a history of dog ownership and presented with eosinophilic meningoencephalomyelitis manifesting as epilepsy, pyrexia, frontal headache, ataxia, pleocytosis, and meningeal irritation (148). A T2-weighted MRI showed numerous hyperintense cortical and subcortical lesions. IgG antibodies against the T. canis antigen showed positivity in the CSF and serum. The manifestations were resolved successfully after treatment with diethylcarbamazine and corticosteroids. Furthermore, a 40-year-old Belgian woman presented with eosinophilic myelitis causing dermatomal dysesthesia and right leg weakness (148). Investigations revealed an elevated eosinophil count in the cerebrospinal fluid, and a spinal cord MRI showed abnormal hyperintensities. After treatment with mebendazole, the neurological abnormalities were resolved completely. In several meningomyelitis cases, MRI of the spine showed solitary or multiple hyperintense lesions on T2-weighted images, with strong homogeneous enhancement (125, 136, 146).
In a particularly unusual set of clinical cases, evidence for T. canis brain invasion was reported for patients who suffered from chronic Viliuisk encephalomyelitis (VE). VE is a neurological disease occurring only in the Sakha (Iakut/Yakut) population in Northeast Siberia (149). Goldfarb and Gajdusek (150) analyzed the phenotype and showed an acute phase with encephalitis and meningism progressing to a chronic pan-encephalitic syndrome. Clinical features of chronic VE consisted of ataxia, lower limb spasticity, predominant sensory gait apraxia, bladder dysfunction, and cognitive impairment. Most patients suffered an acute phase with meningitis-like symptoms before the chronic phase, and laboratory investigations showed a short-lived eosinophilia in the acute phase. In addition, eosinophilic infiltrations were confirmed through histological analyses of brain specimens from subacute/subchronic VE patients, which suggested an eosinophilic meningitis (150).
Recently, Storch and colleagues (151) used clinical, neuroimaging, and serological data in a cross-sectional study of 20 patients suffering chronic VE to explore hypotheses relating to the pathophysiology and cause of chronic VE. The clinical phenotype of chronic VE patients consisted of dementia in 57% of patients, urge incontinence in 70%, dysarthria in 80%, lower-limb spasticity in 90%, gait apraxia in 95%, and sensory ataxia in 100% of patients. Two-thirds of patients had acute-onset meningitis with cranial nerve deficits which subsided over the disease course. Blood hematology data were retrospectively analyzed from controls and chronic VE patients, revealing that in the subacute/acute phase, 65% of patients had transient, moderately to mildly raised eosinophils, compared to 0% of controls. The discovery of acute-phase eosinophilia prompted the investigators to consider neurotropic infectious agents linked to eosinophilic meningitis, such as viruses (varicella-zoster virus, rubella virus, measles virus, herpes simplex viruses 1 and 2 [HSV-1 and -2], cytomegalovirus, tick-borne encephalitis virus [FSME], and lymphocytic choriomeningitis virus [LCMV]), bacteria (such as Borrelia burgdorferi and Treponema pallidum), and nematodes (T. canis and A. cantonensis). Immunodiagnostic results were similar between VE patients and controls for various neurotropic bacteria and viruses, although a high prevalence of elevated antibody indexes (AIs) was found for HSV-1, HSV-2, and varicella-zoster virus, though this was considered unlikely to be a specific cause of VE and was attributed to endemic infection (152).
In contrast, 70% of chronic VE patients had anti-T. canis antibodies, compared to 13% of controls (no difference was found for A. cantonensis). Although Storch and colleagues (151) claimed that chronic VE was triggered by eosinophilic meningitis, which might have been caused previously by T. canis infection, definitive proof of this relationship is still lacking. Nevertheless, the evidence published by Storch et al. (151) at least provided the first indication that Viliuisk encephalomyelitis is perhaps an endemic form of rare cerebral complications combined with cerebral and myelonic symptoms of Toxocara sp. infection; however, further parasitological exploration within the Viliuiski area is warranted in order for a comprehensive elucidation to be made.
Seizure
Seizures are paroxysmal events resulting from excessive, hypersynchronous electrical discharge of neurons causing a number of behavioral and clinical manifestations, e.g., dramatic convulsions. Recent advances in experimental neuroscience have revealed that inflammation can facilitate seizures or sustain seizure activity. Neuroinflammation occurs in the epileptic brain and can intensify seizures or increase seizure frequency, because neuroinflammation may directly affect neurovascular and glial function. Moreover, the effects of systemic inflammation can be mediated or facilitated by a loss of BBB function due to activation of circulating leukocytes and release of molecular mediators that increase vascular permeability (153).
It is estimated that 65 million people are affected by epilepsy worldwide, particularly in sub-Saharan Africa (SSA), whereas specific seizure-causing parasitic infections are largely absent in industrialized countries (154). Early reports have suggested that people with epilepsy (PWE) have a high rate of exposure to T. canis (155, 156). Woodruff et al. (155) found that a higher percentage of PWE (7.5%) reacted positively to a toxocariasis skin test than the case for apparently healthy controls (2.1%). They also found that a positive skin test in PWE was significantly associated with exposure to dogs. Arpino et al. (157) conducting a case-controlled study of more than 300 children and found a significant relationship between seizures and a positive serum reaction to T. canis antibodies. The relationship was strongest in children under the age of 5 years.
Owing to an improved specificity and sensitivity of serodiagnosis, the association between T. canis seropositivity and epilepsy was further investigated in various populations and suggested that toxocariasis may be a cofactor in the occurrence of epilepsy in areas where the helminth is endemic (70, 158). A large, case-controlled, cross-sectional study across five SSA countries found that risk factors for active convulsive epilepsy in children included head injury and difficulties in crying, breathing, or feeding after birth. In adults (≥18 years), epilepsy risk factors included malaria or pyrexia, exposure to T. gondii, Onchocerca volvulus, Taenia solium, or T. canis, and hypertension (73). A meta-analysis and systematic review of available data, including seven case-control studies, provided 1,867 subjects, including 1,017 people without epilepsy (PWOE) and 850 PWE, at ages ranging from 1 year to 17 years, while children below 10 years of age were excluded from one study (72). The studies were undertaken in Bolivia, the United States, Turkey, Italy, Tanzania, and Burundi, in urban and rural settings, to evaluate the relationship between epilepsy and T. canis seropositivity. The findings of these studies supported the existence of a positive association between T. canis seropositivity and epilepsy.
Recently, Kamuyu et al. (159) investigated the association between epilepsy and parasitic infections at five SSA sites. Their findings also revealed an association between exposure to T. canis as well as elevated levels of T. canis antibodies and the prevalence of active convulsive epilepsy. One major limitation concerning these various studies is the heterogeneity in the immunodiagnostic techniques employed, i.e., WB or ELISA. In addition, Kamuyu et al. (159) mentioned that a commercial kit which was employed to detect serum anti-T. canis IgG antibodies by using TESELISA had a 97% sensitivity and 78.6% specificity. Even though Quattrocchi et al. (72) stipulated that TESWB has a reasonable sensitivity and superior specificity compared to commercial or in-house TESELISA, it remains unavoidable that cross-reactivity will be caused by other soil-transmitted helminths with this assay. This limitation has already been revealed, i.e., sera from individuals with intestinal helminthiasis, e.g., ascariasis, trichuriasis, or schistosomiasis, can also cross-react with TES antigens as assessed by TESWB (160).
However, the evidence outlined above for an association between epilepsy and T. canis seropositivity does not prove causality between epilepsy and infection with T. canis. For causality to be definitively established, it is necessary to show that exposure to T. canis occurred before the onset of epilepsy. Although evidence is accumulating to suggest that infection with T. canis is implicated in epilepsy (71, 72), the exact etiological connection still requires more comprehensive investigation, i.e., the association needs to be established in cases where epilepsy has just developed (161), especially in regions where Toxocara occurs sympatrically with other epilepsy-causing infections (50).
Schizophrenia
Schizophrenia is a severe, debilitating mental disorder with devastating impacts on patients, their families, and society (162). Schizophrenia is a heterogeneous disorder characterized by a range of clinical features, such as positive symptoms, referring to psychotic behaviors, including hallucinations, and negative symptoms, associated with disruption of normal behavior, such as lack of motivation. The prevalence of schizophrenia has been reported to be 1% of the adult population, with development in late adolescence or early adulthood, and most patients suffer from the disease throughout their lifetime (163). Cognitive deficits affect sensory processing, episodic memory, processing speed, attention inhibition, working memory, and language and executive functions (164).
The invasion of the CNS by T. canis larvae may result in psychiatric and neurological disorders that could contribute to schizophrenia. However, compared to the case for Toxoplasma, the link between schizophrenia and T. canis infection has received much less attention (165). According to the “original dopamine hypothesis,” hyperactive dopamine (DP) transmission is responsible for schizophrenic symptoms. Carlsson and Lindqvist (166) developed the hypothesis after demonstrating DP's role as a neurotransmitter. DP is produced in several areas of the brain, including the ventral tegmental region, prefrontal cortex, striatum, substantia nigra, and hippocampus, and changes in DP are linked to schizophrenia (167).
Positive symptoms, such as delusions and hallucinations, result from an excess of DP in the subcortical region, which hyperstimulates D2 receptors and is thought to result from disruption of the cortical pathway. Negative symptoms include anhedonia (loss of the capacity to experience pleasure) (97), lack of speech, and lack of motivation resulting from reduced prefrontal cortex D1 receptor stimulation (168). The “revised dopamine hypothesis” proposes hyperdopaminergia in the mesolimbic pathway and hypodopaminergia in the prefrontal cortex in patients with schizophrenia (169). In particular, hippocampal dysregulation of the DP system occurs in schizophrenia patients (169).
Using a murine model, Othman et al. (170) found that DP levels significantly decreased over time in the brains of mice infected with Toxocara larvae. In contrast, another study found enhanced expression of tyrosine hydroxylase (TH), which is capable of catalyzing the conversion of the amino acid l-tyrosine to l-3,4-dihydroxy-phenylalanine (l-DOPA), a precursor for DP (171; Fan et al., unpublished data). TH is present in the adrenal medulla, the peripheral sympathetic neurons, and the CNS (171). Substantial studies have indicated that an alteration of TH activity is related to disorders such as Parkinson's disease and schizophrenia (172). However, the role of the DP system in a schizophrenia disorder in NT remains to be elucidated comprehensively.
Di Fiore et al. (173) investigated the seroprevalence of T. canis infection in 335 Italian human sera and found a prevalence of 13% among psychiatric patients, compared with 9.4% of farmers, 1.9% of children, and 1.2% of blood donors. Richartz and Buchkremer (75) reported a case of a German woman who tested positive for T. canis antibodies in the CSF and who had cognitive deficits and symptoms of depression. In Turkey, Kaplan et al. (174) found that 45 of 98 patients with schizophrenia had a higher seroprevalence of T. canis infection than healthy individuals (45.9% versus 2%). Furthermore, in Egypt, El-Sayed and Ismail (175) found that toxocariasis was detected at a higher rate in patients with schizophrenia disorder (23.3% [21/90 patients]) than in controls (2.2% [1/45 patients]). In Mexico, Alvarado-Esquivel (176) found IgG antibodies to Toxocara in 4.7% of 128 psychiatric patients, compared to 1.1% of 276 healthy controls.
In India, Khademvatan et al. (177) also found that patients with schizophrenia disorders had a statistically higher seroprevalence of T. canis infection than healthy individuals (14% [14/100 individuals] versus 4.3% [4/95 individuals]), and schizophrenic women and men did not differ in their T. canis seroprevalence. Meanwhile, Cong et al. (178) undertook a seroepidemiological investigation of infection with T. canis in Shandong Province in eastern China, and they also found an insignificantly higher seroprevalence in schizophrenia patients (14.0% [33/235 patients]) than in clinically normal subjects (13.1% [187/1,431 subjects]) and pregnant women (9.2% [91/990 subjects]). From this range of epidemiological studies with a wide geographical variation, we can postulate either that the greater prevalence of Toxocara in patients with psychiatric disorders than in controls reflects a role for T. canis infection in the etiology of psychiatric diseases or that psychiatric patients have a higher risk of infection due to abnormal behavioral changes, such as poor hygiene and self-care skills as well as a propensity to eat inappropriate things (175).
Substantial studies have indicated that people with T. gondii infection may be highly susceptible to schizophrenia development (165). Since infection with T. canis would increase the risk for T. gondii infection and vice versa (113), we cannot completely exclude the possibility that schizophrenia syndrome in T. canis-seropositive patients is truly triggered by T. gondii rather than T. canis infection. However, this is still unclear, since the studies mentioned above did not reveal the status of T. gondii infection among schizophrenia patients. Clearly, further research on the possible mechanistic relationship between Toxocara brain involvement and schizophrenia, depressive, and cognitive disorders is required.
Cognitive Deficits
Substantial studies have indicated a correlation between CNS inflammation and cognitive impairment in a number of neurological diseases, e.g., Alzheimer's disease (AD), because CNS inflammation has been confirmed to be implicated in the development of amyloid neuritic plaques, one of the hallmarks of AD (179, 180). The impact of T. canis infection on cognitive development in humans is sorely lacking, with very few clinical or population-based studies having examined the relationship between neuropsychological parameters and T. canis seropositivity (18, 181). Some clinical studies have described various cognitive deficits associated with infection, including a lack of developmental progress and speech (181), depressive symptoms and cognitive deficits possibly indicative of dementia (75), mental confusion and cognitive impairment (66, 182), impairments of mental fluency and short-term and working memory spans, and slowed information processing (2).
At the population level, Worley et al. (183) first reported an association between T. canis seropositivity and poor reading achievement, distractibility, and lower intelligence in kindergarten children, but the effects of social class were not considered in the analysis. Later, Marmor et al. (184) undertook neuropsychological tests on children aged 1 to 15 years and found significant cognitive deficits in T. canis-seropositive children compared with seronegative controls adjusted for race, socioeconomic status, and blood lead concentrations. Thereafter, Nelson et al. (185) evaluated cognitive function in children aged 1 to 4 years and identified lower mental development scores and IQ levels in T. canis-seropositive children; however, blood lead levels, which have been linked with cognitive impairment, were not assessed in these subjects (186).
Jarosz et al. (181) undertook a study of more than 200 students of 14 to 16 years of age in rural Poland. The authors investigated the relationship between toxocariasis and the students' physical fitness and developmental age, and they demonstrated that boys who were seropositive performed significantly worse academically than students who were seronegative. However, the authors acknowledged that behavioral factors increasing exposure to infection, such as more time spent playing outdoors instead of studying, could have explained the relationship.
In a significant advance, Walsh and Haseeb (187) sampled 3,949 children living in the United States, using data from the Third National Health and Nutrition Examination Survey (NHANES III; 1988–1994). They reported statistically lower cognitive scores on both the Wechsler Intelligence Scale for Children, Revised (WISC-R), and the Wide Range Achievement Test, Revised (WRAT-R), for seropositive children than for children who were seronegative. This finding controlled for ethnicity, socioeconomic status, gender, infection with cytomegalovirus, blood lead levels, and rural residence. Nevertheless, the need for additional longitudinal data to elucidate an etiological relationship between diminished cognitive function and toxocariasis warrants further comprehensive investigations (187).
Data from murine models exploring the effect of T. canis infection on memory and learning are particularly relevant to human infection (18). Cox and Holland (188) used spatial learning tasks to assess information-gathering ability and memory in mice. Initial experiments utilized infected and control LACA mice. These were exposed to a particular resource, a water tube, in a novel environment to test the latency required for mice to relocate the resource after a period of deprivation, an indication of memory capacity in mice. Mice classified as having large and moderate numbers of larvae in the brain took longer to perform tasks than control mice and mice with low-level infections. The experiments were repeated using BALB/c mice, which are susceptible to Toxocara cerebral infection, and resistant NIH mice. BALB/c mice required significantly more time to complete tasks than NIH mice, suggesting the occurrence of memory loss, which may be attributable to where the larvae were located in the brain (189). Studies have reported larvae in the telencephalon (190) and cerebellum (191), both of which are regions of the brain linked to memory and learning as well as control of voluntary movement and coordination.
Idiopathic Parkinson's Disease
Idiopathic Parkinson's disease (IPD) is a common neurodegenerative disorder characterized by a progressive degeneration of midbrain dopamine neurons of the substantia nigra, resulting in a variety of motor symptoms, e.g., rigidity, akinesia, and resting tremor. The molecular pathways leading to clinical alterations require comprehensive elucidation but may be the result of either environmental factors, genetic influences, or a combination of these (192). Degeneration of neurons in IPD may result from several pathogenic mechanisms, including neuroinflammatory processes, oxidative stress, excitatory amino acids, mitochondrial abnormalities, elevated intracytoplasmic free calcium, apoptotic processes, and cytokines. Recently, studies have suggested a fundamental role for microglia-driven neuroinflammation and the neurotoxic products (nitric oxide, proinflammatory cytokines, and reactive oxygen species) of infiltrated peripheral immune cells in the pathological process of IPD (193). The impact of infectious agents on IPD patients and the relationship between infections and pathogenesis or clinical findings for IPD are unclear. A few studies have indicated that infectious agents, e.g., influenza virus, may play a role in IPD (194).
T. canis larval invasion into the CNS may cause neurological manifestations resulting in some neurological and psychiatric disorders that may include IPD; however, a potential relationship between infection with T. canis and IPD has received little attention. The primary symptoms of IPD result from a greatly reduced activity of DP-secreting cells caused by a loss of cells in the substantia nigra pars compacta, thus possibly leading to insufficient formation and activity of DP produced in certain neurons within parts of the midbrain (192). Recently, Çelik et al. (195) found that although the T. canis infection seroprevelance was higher in IPD patients (6.0%) than in controls (0%), no statistical difference was found in the seropositivity rate between IPD and control groups.
Using a murine model, Othman et al. (170) found that mice infected with Toxocara showed increased gene expression of nitric oxide and proinflammatory cytokines, particularly in the chronic stage. While proinflammatory cytokines are neuroprotective, prolonged or elevated levels can cause neuronal damage (170). In particular, compared with uninfected mice, T. canis-infected mice showed significant decreases in DP, monoamine, GABA, and serotonin levels. In contrast, as discussed in “Schizophrenia,” above, our study found that DP expression increased in the brains of Toxocara-infected outbred ICR mice (Fan et al., unpublished data). This difference in DP expression between two animal studies warrants further investigation to further elucidate the possibility of DP-related IPD occurring with neurotoxocariasis.
Dementia
The causes of dementia, a decline in cognitive function severe enough to affect social or occupational functioning, are complex and may be due to AD or vascular dementia (196). The pathogenesis of dementia is postulated to be very similar to that of cognitive dysfunction (196), indicating that CNS inflammation is implicated in this neurodegenerative disease due to the development of amyloid neuritic plaques (179, 180).
Higher T. canis seroprevalences have been found for various patient groups with neuropsychiatric disorders, e.g., seizure, cognitive deficits, IPD, and schizophrenia, than for control groups (159, 175, 187, 195); however, clinical case reports concerning the status of T. canis infection among dementia patients are rare. Among the cases shown in Table 2, only one NT patient who exhibited dementia and depression was reported (75). In this case, a 65-year-old woman with a long history of cognitive decline and depression was described. Laboratory examination revealed eosinophilia as well as reactive antibodies against T. canis antigen in the CSF. The infection was possibly attributable to her occupation as a shepherdess, with a high frequency of close contact with dogs. Cognitive deficits were improved by treatment with albendazole.
Nevertheless, dementia cases caused by T. canis are rarely reported and may be overlooked due to the fact that most humans with cerebral toxocariasis do not present significantly clinical neurological signs as a consequence of light parasitic burdens (18). This, along with the longevity of T. canis larvae resident in the internal organs, including the brain (20), demonstrates the need for more extensive investigation of the link between dementia and NT. A summary of potential linkages between T. canis infections and neuropsychiatric disorders is shown in Table 3.
TABLE 3.
Potential linkages between T. canis infections and neuropsychiatric disorders
| Neuropsychiatric disorder | Possible mechanisms | Type of studies | Possible causal relationships | References |
|---|---|---|---|---|
| Seizure | Increased proinflammatory cytokine expression and BBB dysfunction | Human/animal studies | Three large-scale studies provided evidence for a positive association between T. canis seropositivity and seizure. | 71–73, 153–159, 200, 208 |
| Schizophrenia | Increased or decreased dopamine expression | Animal studies | Epidemiological studies indicated that the schizophrenia group had a higher seroprevalence of T. canis infection than healthy individuals. Increased or decreased dopamine expression was observed in the T. canis-infected mouse brain. | 97, 166–170, 173–178 |
| Cognitive deficits | CNS inflammation causes amyloid neuritic plaque formation | Human/animal studies | Several epidemiological studies indicated significant cognitive deficits in T. canis-seropositive children compared with seronegative controls. | 170, 179–189, 199 |
| Idiopathic Parkinson's disease (IPD) | CNS inflammation causes dopaminergic neuronal degeneration | Animal studies | Insignificantly higher seroprevalence of T. canis infection in patients with IPD than in controls. Significantly decreased GABA and DP levels were found in T. canis-infected mice compared with uninfected mice. | 170, 192–195 |
| Dementia | CNS inflammation causes amyloid neuritic plaque formation | Human studies | An elderly German woman with a long history of depression and cognitive decline showed reactive antibodies against T. canis antigen in CSF. | 75, 179, 180 |
| Alzheimer's disease | CNS inflammation causes amyloid neuritic plaque formation | Human/animal studies | Significantly increased proinflammatory cytokines and insoluble β-amyloid levels were found in brains of T. canis-infected mice compared with uninfected mice. | 170, 196, 200, 208 |
MURINE MODELS OF NEUROLOGICAL INFLAMMATION, UBIQUITIN-PROTEASOME IMPAIRMENT, AND COGNITIVE DEFECTS IN CEREBRAL TOXOCARIASIS
Humans are known to harbor Toxocara larvae in their brains, but the number of cases of cerebral infection described in the literature is still small. Additionally, the cryptic nature of the effects of brain involvement are not easily explained or observed in humans with CT. The choice of an appropriate animal model to explore the behavioral and pathological implications of cerebral toxocariasis is therefore important. Furthermore, our and other researchers' experience of methodological and ethical challenges associated with studies of geohelminth infections and cognitive development in human subjects (197) highlights the necessity of useful laboratory animal model systems to investigate the relationship between learning deficits and cerebral toxocariasis. Holland and Hamilton (18) outlined the advantages of mouse models for toxocariasis, including ease of manipulation and larval detection in small organs, the selective choice of inbred or knockout strains, and, importantly, the role of Mus musculus and other small rodents in the natural Toxocara life cycle under field conditions.
The mouse model has been useful for exploring the impact of Toxocara infection on murine behavior. Infected mice tend to be less explorative and active and less responsive to novelty, and they show lower levels of aversion to predator stimuli and open areas than control animals (188, 198). These abnormal behavioral changes are likely related to the site where T. canis larvae are located in the brain, the immune response directed against T. canis larvae, and, more importantly, pathological effects rather than parasite-altered host behavior (199). Therefore, mice are useful animal models for exploration of the impact of T. canis on the biology of the brain and behavior as well as the pathogenesis of neurotoxocariasis.
Experimental work in mice has established evidence that may have implications for human health, such as the following: larvae recovered from the murine brain differ in number between genetically different inbred mice inoculated with the same dose (189), the distribution of larvae may not be random in the brain (190, 191), behavioral alterations are dose dependent (198), cerebral infection can lead to deficits in memory and learning (189), and infection in the brain induces an inflammatory immune response (82, 200). Given the central role of cytokines in the brain under normal or disease conditions, prolonged exposure to proinflammatory cytokines that promote neural injuries, e.g., tumor necrosis factor alpha (TNF-α), IL-6, and IL-1β, may aggravate neurodegenerative progression and compromise vulnerable neurons (201). Our knowledge of the systemic immune response to T. canis greatly exceeds that of the brain's immune response (202). Evidence from other brain-inhabiting parasites, such as those causing malaria (203), trypanosomiasis (204), toxoplasmosis (205), and neurocysticercosis (206), demonstrates that cytokines produced in response to neurotropic parasites can contribute to CNS diseases that often lead to pathological injuries in the brain.
Experiments conducted by Hamilton et al. (200) showed that T. canis-infected BALB/c mice exhibited significantly raised mRNA levels for IFN-γ, IL-5, IL-10, and inducible nitric oxide synthase (iNOS) compared to infected NIH mice. Furthermore, these levels were particularly raised at 35 and 42 days postinfection, times that coincide with observed behavioral alterations, most notably memory impairment. Dantzer et al. (207) proposed a “sickness behavior” that was triggered by proinflammatory cytokines involved in an array of behavioral symptoms, e.g., decreased exploration, reduced memory and learning, and depression of locomotor activity, in humans and mice. In particular, memory and learning impairments were linked to elevated levels of IL-1β, revealing an interference of memory storage by an increase in cytokine production. Moreover, Liao et al. (82) observed biomarkers (BIABs) associated with brain injury, including glial fibrillary acidic protein (GFAP), TGF-β1, S100B, tissue transglutaminases (tTG), AβPP, NF-L, and p-tau, in brains of ICR outbred Toxocara-infected mice given a single-dose inoculation of 250 eggs. They also observed injury to the BBB in a similar cerebral toxocariasis experiment, as assessed by pathological changes, GFAP expression, and Evans blue (EB) dye concentration. In addition, abnormal BBB permeability and cerebral injury increased over the duration of the infection, though the changes appeared to be unrelated to larval numbers in the brain (208).
The issue of infective dose and the resultant larval burden (and the relationship between observed behavioral and immunological changes) in the brain for murine animal models is an important one. In contrast to Hamilton et al. (189, 200), who utilized doses of 1,000 ova, Fan et al. (209) used a single dose of 250 T. canis eggs to infect ICR outbred mice and reported larval recovery rates ranging from 2.9% to 3.8% from the murine brain. This larval recovery is close to that of 4.4% recorded by Cox and Holland (188), who used an inoculum of 100 ova given to outbred LACA mice. Good et al. (190) assessed the larval distribution in the brains of CD1-ICR outbred mice, and they found that brain region and dose were significant factors contributing to the observed distribution. Cox and Holland (188) suggested that the provision of a low-dose inoculation, with a resultant low T. canis larval burden, more realistically reflects cerebral toxocariasis infection in wild rodents and humans.
These observations underline an urgent need to further elucidate the link observed between enhanced BIAB expression or abnormal BBB permeability and behavioral alterations in experimental cerebral toxocariasis. Liao et al. (82) also indicated that enhanced expression of BIABs, which may be deleterious to the brain, might be explained by a ubiquitin-proteasome system (UPS) dysfunction that is unable to degrade misfolded, damaged, or unwanted proteins with the potential to form toxic aggregates in the brains of mice infected with T. canis. It has been hypothesized that the presence of deposits consisting of ubiquitylated proteins in diseased neurons (found in many hereditary and sporadic neurodegenerative diseases) is suggestive of a link between pathogenesis and UPS dysfunction, e.g., in AD (210), and whether cerebral infection by T. canis has damaging effects that increase the risk of cerebral toxocariasis progressing to neurodegenerative disorders should not be completely disregarded.
Furthermore, Othman et al. (170) showed that elevations of proinflammatory cytokines, such as iNOS, TNF-α, and IL-6, as well as changes in neurotransmitter profiles in T. canis-infected mouse brains were greatest during chronic infection, as indicated by enhanced GFAP expression. Of particular importance was their novel observation that the normal patterns of neurotransmitters, e.g., GABA, dopamine, and serotonin, were disrupted as a result of T. canis infection. Since changes in neurotransmitter patterns in humans are related to a variety of perturbations, including behavioral disturbances and seizures, these observations, along with those on enhanced proinflammatory cytokine expression, could provide explanations for the cognitive and behavioral deficits seen in CT in mice and humans (170) (Table 3).
CEREBRAL TOXOCARIASIS VERSUS ALZHEIMER'S DISEASE: A SILENT PROGRESSION
AD is the most common form of dementia worldwide. Two major neuropathological hallmarks characterize the condition: extracellular plaques largely consisting of insoluble beta-amyloid (Aβ) peptide aggregates and the presence of intracellular neurofibrillary tangles (NFTs) comprised of the hyperphosphorylated form of microtubule-associated protein tau (211). Animal and clinical studies have indicated that insoluble Aβ42 peptide accumulation is crucial for development of AD; this is thought to derive from aberrantly processed or overproduced AβPP, and dysregulation of AβPP production may be important in the etiology of Alzheimer's disease (211). Generation of the soluble Aβ40 peptide or insoluble Aβ42 peptide requires sequential cleavages of AβPP. Extracellular cleavage by beta-secretase 1 (beta-site AβPP-cleaving enzyme 1 [BACE 1]) leaves a membrane-bound fragment, referred to as AβPP-C99, and a large soluble extracellular fragment. Cleavage of AβPP-C99 within its transmembrane domain by γ-secretase releases the intracellular domain of AβPP and produces the insoluble Aβ42 peptide, which is the primary etiology of AD. In contrast, α-secretase cleaves AβPP closer to the cell membrane than BACE1 does, resulting in production of the soluble Aβ40 peptide, which may be removed from the brain (211). NFTs are made up of paired helical filaments (PHFs); tau in these PHFs is abnormally phosphorylated (212).
In addition to hypotheses about the Aβ cascade and tauopathy, the pathological mechanism of AD is complicated and remains unclear; however, some cytokines, i.e., TGF-β1 (213) and S100B (214), glial proteins, i.e., GFAP (215) and NF-L (216), and enzymes, i.e., tTG (217) and ubiquitin (210), have been characterized as being highly associated with or involved in not only acute injury of cerebral toxocariasis but also AD. In particular, TGF-β1, a multifunctional cytokine, plays a significant role in regulating brain responses to inflammation and injury, and experimental and clinical studies have indicated that it is highly involved in initiating or promoting amyloidogenesis (218, 219).
Under normal circumstances, S100B promotes neurite outgrowth, stimulates proliferation of astroglial cells, and increases intracellular concentrations of free calcium in astrocytes and neurons. It has been reported that overexpression of S100B may have deleterious consequences, including dystrophic changes in neurons and neuritis, which characterize the neuritic Aβ plaques used in AD diagnosis (220). Some intermediate filament proteins, such as GFAP and NFs, have also been proposed to be associated with AD. In CNS injury, elevated expression of GFAP was associated with astrocyte activation, modulated by TGF-β1, during neural responses to injury (221). NFs, which are comprised of neurofilament light (NF-L), neurofilament medium (NF-M), and neurofilament heavy (NF-H) subunits, are intermediate filaments found specifically in neurons and are considered to convey tensile strength, structural rigidity, and intracellular transport guidance to dendrites and axons, while abnormal accumulation of NF-L is detected in AD (216, 222). Evidence also indicates that some enzymes, such as tTG and ubiquitin, are potent mediators of the pathogenesis of AD. By facilitating the formation of one or both of two insoluble neurotoxic proteins, Aβ and tau, tTG may be involved in AD pathogenesis (211). The UPS functions in cellular quality control by degrading misfolded, unwanted, or defective proteins. The UPS also serves as the primary route for degradation of thousands of normal short-lived and regulatory proteins and thus contributes to the regulation of a variety of cellular processes. Failure to detect and eliminate misfolded proteins, or the UPS itself, may contribute to or be a target for toxic proteins involved in the pathogenesis of neurodegenerative diseases, including AD (223). Elevated accumulation of the insoluble Aβ42 peptide is considered to compromise neuronal function and viability through dysregulation of intracellular Ca2+ homeostasis and impairment of mitochondrial activity and to stimulate proapoptotic signaling through interaction with neuroreceptors. The increased activation of kinases results in dendritic spine loss, tau hyperphosphorylation, cytoskeletal compromise, and accumulation of NFTs. A number of factors are released by damaged neurons and induce the generation of free radicals and inflammation, whose effects are intensified by proinflammatory cytokine release (224).
Our preliminary data showed that T. canis-infected ICR outbred mice exhibited significant expression of biomarkers associated with AD, such as GFAP, total Tau (T-tau), TGF-β1, TG2, S100B, and NF-L, with 2- to 4-fold increases in the brain compared to the levels in age-matched uninfected controls at 20 weeks postinfection. BACE1, AβPP-C99, and Aβ42 were observed to have 3- to 13-fold, 3- to 3.5-fold, and 3- to 5-fold increases, respectively, within the brains of mice infected with T. canis compared to age-matched uninfected mice at 20 weeks postinfection (Fig. 3A to C).
FIG 3.
Increased expression of Alzheimer's disease-associated neurodegenerative proteins, including TGF-β1, S100B, T-tau, GFAP, NF-L, tTG, and BACE1 (A), β-secretase-derived AβPP fragment C99 (AβPP-C99) (B), and β-amyloid peptides of 42 amino acids (Aβ42) (C), and UPS dysfunction (D) in the brains of Toxocara canis-infected mice inoculated with a single dose of 250 infective eggs, at 3 days (D3), 4 weeks (W4), 12 weeks (W12), and 20 weeks (W20) postinfection, as assessed by Western blotting. (E) T. canis larva (longer arrow) found in an area close to the choroid plexus (shorter arrow) at 12 weeks postinfection. GAPDH, glyceraldehyde-3-phosphate dehydrogenase; W1-C and W20-C, uninfected control mice at 1 week and 20 weeks postinfection; (+)Aβ, the Aβ42 peptide was run by SDS-PAGE and then transferred to the membrane, and it was recognized by a mouse anti-Aβ42 monoclonal antibody which is regarded as a positive control. These data are our unpublished observations.
UPS dysfunction initially occurred early, at 3 days postinfection, became abnormal at 4 weeks postinfection (Fig. 3D), and then continued until 20 weeks postinfection (Fig. 3D). Pathological findings indicated that one T. canis larval section was found in an area close to the choroid plexus (Fig. 3E). It seemed probable that AD-associated protein aggregation caused the dysfunction of the UPS, as a number of studies have proposed that intracellular deposition of ubiquitylated and aggregated proteins, as well as an increase in ubiquitin, is a cytopathological aspect of AD (225, 226), and this was confirmed by direct impairment of UPS function caused by aggregation of proteins (223). The animal use protocol in this experiment was reviewed and approved by the Institutional Animal Care and Use Committee, Taipei Medical University (approval no. LAC-99-0010). All animal experiments were carried out in accordance with institutional policies and guidelines for the care and use of laboratory animals, and all efforts were made to minimize animal suffering. Taken together with our previous study that revealed the impairment of the BBB in murine brains invaded by T. canis larvae (208), these preliminary, unpublished results provide fresh insights to better understand the possible role of T. canis larval invasion in the potential development of AD due to enhanced AD-associated neurodegenerative biomarker expression.
CONCLUSIONS
Based upon the high levels of exposure to Toxocara worldwide but the relatively small numbers of human cerebral toxocariasis cases reported in the literature, most cases of human toxocaral brain involvement are likely to involve small numbers of larvae that do not present with significant clinical neurological signs. However, experimental data obtained from monkeys (227) and mice (228) confirm that T. canis larvae may accumulate in the brain and remain there for extended periods. This longevity may contribute to cerebral pathogenesis, and clinically, cerebral toxocariasis patients do indeed present with various neuropsychiatric disorders, e.g., seizure, cognitive deficits, and, rarely, dementia. Epidemiological observations also find a higher seroprevalence of T. canis in patients with schizophrenia and IPD than in controls.
However, for ethical and methodological reasons, the complex relationship between cerebral toxocariasis, neuropathogenesis, and observed behavioral deficits needs to be explored in a suitable animal model in order to definitively outline the mechanistic relationships. Care needs to be exercised in controlling for potential confounding variables in murine models, such as genetic status, infective dose, duration of infection, refinement of behavioral testing, and the challenge of measuring behavioral alterations in tandem with complex pathophysiological, biochemical, and immunological measures (18).
Our preliminary data from a murine model hypothesize that cerebral toxocariasis may exhibit a silent progression to AD (Fig. 4). Certainly, the enhanced expression of GFAP indicates that the very few T. canis larvae that had migrated to the brains of ICR outbred mice fed a low dose of infective ova were capable of causing brain injury (82, 208). Furthermore, BBB impairment (208) and UPS dysfunction can occur simultaneously in mice with cerebral toxocariasis. The expression of AD-associated biomarkers also significantly increased with infection duration, and in addition, expression of BACE1, AβPP-C99, and Aβ42 (which represent apparent amyloidogenesis), which is also believed to be an important cause of AD, was enhanced in mice with cerebral toxocariasis (Fig. 4). We thus postulate that cerebral toxocariasis may progress to AD due to an impaired UPS that cannot degrade the unwanted or nerve-deleterious proteins, e.g., AD-associated proteins. Combined with a compromised BBB, the UPS cannot perform its normal function to balance the cerebral environment by transporting harmful molecules out of the brain, thus leading to nerve-deleterious materials accumulating in the brain and the disease gradually progressing to AD (229). To conclude, the underlying molecular pathogenesis associated with cerebral toxocariasis that may progress to AD is complex; however, we provide an animal model and a hypothesis to further elucidate the possible pathogenic mechanism.
FIG 4.
Illustration of the hypothesis that cerebral toxocariasis may progress to Alzheimer's disease.
ACKNOWLEDGMENT
We are grateful to the National Science Council, Taiwan, for its support of our experimental cerebral toxocariasis study (grant NSC 99-2628-B-038-001-MY3).
Biographies

Chia-Kwung Fan received his Ph.D. from the Graduate Institute of Microbiology, National Taiwan University College of Medicine. Currently, he is working as a full-time Professor in the Department of Molecular Parasitology and Tropical Diseases, School of Medicine, Taipei Medical University, and he also works as an Expert Consultant for the Centers for Disease Control, Ministry of Health and Welfare, Taiwan. His current administrative job is as Department Chair. His research has included the study of zoonotic parasitoses, particularly the epidemiology, molecular pathogenesis, and immunopathogenesis of toxocariasis and toxoplasmosis, since 1990. Since 2009, he has led his research team to undertake epidemiological investigations with associated risk factor analysis of T. canis infection among school children in Africa (Swaziland and Sao Tome and Principe) as well as the Republic of Marshall Islands. He has authored 54 research articles from 2003 to the present, as well as 3 book chapters.

Celia Holland, B.Sc., Ph.D., M.R.I.A., is a Professor of Parasitology at Trinity College Dublin. Her main research interests are in the epidemiology and control of the soil-transmitted helminths, including Ascaris and Toxocara. She was elected to the Fellowship of Trinity College and as a member of the Royal Irish Academy in recognition of her research. Professor Holland is an Invited Expert on the WHO Advisory Panel on Parasitic Diseases and is currently Secretary General of the European Federation of Parasitology. She is an Editor of the journal Parasitology. She is the author of 108 publications, including peer-reviewed journal articles, books, and book chapters on parasitology and related topics, including the senior editorship of Toxocara: the Enigmatic Parasite and The Geohelminths: Ascaris, Trichuris and Hookworm, as part of the World Class Parasites series. In 2013, she was the sole editor of a book entitled Ascaris: the Neglected Parasite, published by Elsevier.

Karen Loxton received a B.Sc. in ecology from University College Cork and received her Ph.D. from Trinity College Dublin. Her current research interests involve the role of parasites in species invasions, particularly those of small mammals.

Ursula Barghouth obtained her M.S. in public health from the School of Public Health and Tropical Medicine at Tulane University in 2012, with a focus on tropical medicine and parasitology. She conducted her practicum at the Taipei Medical University Department of Parasitology under the supervision of Ted Fan, with a focus on inhibition of inflammatory mediators to lessen pulmonary injury caused by T. canis. She is currently a student at the A. T. Still University School of Osteopathic Medicine in Arizona, obtaining her medical degree and a second master's degree, in health administration.
APPENDIX
DEFINITIONS
- Aβ
β-Amyloid
- AD
Alzheimer's disease
- AβPP
β-Amyloid precursor proteins
- BACE1
Beta-site AβPP-cleaving enzyme 1
- DP
Dopamine
- DUSN
Diffuse unilateral subacute neuroretinitis
- GFAP
Glial fibrillary acidic protein
- IPD
Idiopathic Parkinson's disease
- l-DOPA
l-3,4-Dihydroxyphenylalanine
- NF-L
Neurofilament light chain
- NFTs
Neurofibrillary tangles
- NLM
Neural larva migrans
- TGF-β1
Transforming growth factor β1
- TH
Tyrosine hydroxylase
- tTG
Tissue transglutaminases
- UPS
Ubiquitin-proteasome system
- VE
Viliuisk encephalomyelitis
REFERENCES
- 1.Parsons JC. 1987. Ascarid infections of cats and dogs. Vet Clin North Am Small Anim Pract 17:1303–1307. [DOI] [PubMed] [Google Scholar]
- 2.Scheid R, Tina Jentzsch R, Schroeter ML. 2008. Cognitive dysfunction, urinary retention, and a lesion in the thalamus—beware of possible toxocariasis of the central nervous system. Clin Neurol Neurosurg 110:1054–1057. doi: 10.1016/j.clineuro.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 3.Sprent JFA. 1956. The life history and development of Toxocara cati (Shrank 1788) in the domestic cat. Parasitology 46:54–78. [PubMed] [Google Scholar]
- 4.Overgaauw PA, van Knapen F. 2013. Veterinary and public health aspects of Toxocara spp. Vet Parasitol 193:398–403. doi: 10.1016/j.vetpar.2012.12.035. [DOI] [PubMed] [Google Scholar]
- 5.Barriga OO. 1988. A critical look at the importance, prevalence and control of toxocariasis and the possibilities of immunological control. Vet Parasitol 29:195–234. doi: 10.1016/0304-4017(88)90126-4. [DOI] [PubMed] [Google Scholar]
- 6.Habluetzel A, Traldi G, Ruggieri S, Attili AR, Scuppa P, Marchetti R, Menghini G, Esposito F. 2003. An estimation of Toxocara canis prevalence in dogs, environmental egg contamination and risk of human infection in the Marche region of Italy. Vet Parasitol 113:243–252. doi: 10.1016/S0304-4017(03)00082-7. [DOI] [PubMed] [Google Scholar]
- 7.Dai RS, Li ZY, Li F, Liu DX, Liu W, Liu GH, He SW, Tan MY, Lin RQ, Liu Y, Zhu XQ. 2009. Severe infection of adult dogs with helminths in Hunan Province, China poses significant public health concerns. Vet Parasitol 160:348–350. doi: 10.1016/j.vetpar.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Soriano SV, Pierangeli NB, Roccia I, Bergagna HF, Lazzarini LE, Celescinco A, Saiz MS, Kossman A, Contreras PA, Arias C, Basualdo JA. 2010. A wide diversity of zoonotic intestinal parasites infects urban and rural dogs in Neuquén, Patagonia, Argentina. Vet Parasitol 167:81–85. doi: 10.1016/j.vetpar.2009.09.048. [DOI] [PubMed] [Google Scholar]
- 9.Schär F, Inpankaew T, Traub RJ, Khieu V, Dalsgaard A, Chimnoi W, Chamnan C, Sok D, Marti H, Muth S, Odermatt P. 2014. The prevalence and diversity of intestinal parasitic infections in humans and domestic animals in a rural Cambodian village. Parasitol Int 63:597–603. doi: 10.1016/j.parint.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Waap H, Gomes J, Nunes T. 2014. Parasite communities in stray cat populations from Lisbon, Portugal. J Helminthol 88:389–395. doi: 10.1017/S0022149X1300031X. [DOI] [PubMed] [Google Scholar]
- 11.Fisher M. 2003. Toxocara cati: an underestimated zoonotic agent. Trends Parasitol 19:167–170. doi: 10.1016/S1471-4922(03)00027-8. [DOI] [PubMed] [Google Scholar]
- 12.Macuhova K, Akao N, Fujinami Y, Kumagai T, Ohta N. 2013. Contamination, distribution and pathogenicity of Toxocara canis and T. cati eggs from sandpits in Tokyo, Japan. J Helminthol 87:271–276. doi: 10.1017/S0022149X12000314. [DOI] [PubMed] [Google Scholar]
- 13.Sakai R, Kawashima H, Shibui H, Kamata K, Kambara C, Matsuoka H. 1998. Toxocara cati-induced ocular toxocariasis. Arch Ophthalmol 116:1686–1687. [PubMed] [Google Scholar]
- 14.Despommier D. 2003. Toxocariasis: clinical aspects, epidemiology, medical ecology, and molecular aspects. Clin Microbiol Rev 16:265–272. doi: 10.1128/CMR.16.2.265-272.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Azam D, Ukpai OM, Said A, Abd-Allah GA, Morgan ER. 2012. Temperature and the development and survival of infective canis larvae. Parasitol Res 110:649–656. doi: 10.1007/s00436-011-2536-8. [DOI] [PubMed] [Google Scholar]
- 16.Beer SA, Novosil'tsev GI, Mel'nikova LI. 1999. The role of the water factor in the dissemination of Toxocara eggs and the spread of toxocariasis in a megalopolis. Parazitologiia 33:129–135. [PubMed] [Google Scholar]
- 17.Fan CK, Lin YH, Du WY, Su KE. 2003. Infectivity and pathogenicity of 14-month-cultured embryonated eggs of Toxocara canis in mice. Vet Parasitol 113:145–155. doi: 10.1016/S0304-4017(03)00046-3. [DOI] [PubMed] [Google Scholar]
- 18.Holland CV, Hamilton CM. 2013. The significance of cerebral toxocariasis: a model system for exploring the link between brain involvement, behaviour and the immune response. J Exp Biol 216:78–83. doi: 10.1242/jeb.074120. [DOI] [PubMed] [Google Scholar]
- 19.Smith H, Holland C, Taylor M, Magnaval JF, Schantz P, Maizels R. 2009. How common is human toxocariasis? Towards standardizing our knowledge. Trends Parasitol 25:182–188. doi: 10.1016/j.pt.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 20.Fan CK, Liao CW, Cheng YC. 2013. Factors affecting disease manifestation of toxocarosis in humans: genetics and environment. Vet Parasitol 193:342–352. doi: 10.1016/j.vetpar.2012.12.030. [DOI] [PubMed] [Google Scholar]
- 21.Yamasaki H, Araki K, Lim PK, Zasmy N, Mak JW, Taib R, Aoki T. 2000. Development of a highly specific recombinant Toxocara canis second-stage larva excretory-secretory antigen for immunodiagnosis of human toxocariasis. J Clin Microbiol 38:1409–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watthanakulpanich D, Smith HV, Hobbs G, Whalley AJ, Billington D. 2008. Application of Toxocara canis excretory-secretory antigens and IgG subclass antibodies (IgG1–4) in serodiagnostic assays of human toxocariasis. Acta Trop 106:90–95. doi: 10.1016/j.actatropica.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 23.Noordin R, Smith HV, Mohamad S, Maizels RM, Fong MY. 2005. Comparison of IgG-ELISA and IgG4-ELISA for Toxocara serodiagnosis. Acta Trop 93:57–62. doi: 10.1016/j.actatropica.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 24.Obwaller A, Jensen-Jarolim E, Auer H, Huber A, Kraft D, Aspöck H. 1998. Toxocara infestations in humans: symptomatic course of toxocarosis correlates significantly with levels of IgE/anti-IgE immune complexes. Parasite Immunol 20:311–317. doi: 10.1046/j.1365-3024.1998.00146.x. [DOI] [PubMed] [Google Scholar]
- 25.Fillaux J, Magnaval JF. 2013. Laboratory diagnosis of human toxocariasis. Vet Parasitol 193:327–336. doi: 10.1016/j.vetpar.2012.12.028. [DOI] [PubMed] [Google Scholar]
- 26.Hubner J, Uhlikova M, Leissova M. 2001. Diagnosis of the early phase of larval toxocariasis using IgG avidity. Epidemiol Mikrobiol Imunol 50:67–70. [PubMed] [Google Scholar]
- 27.Förstl M, Buchta V, Psohlavec J, Cermák P, Cermáková Z, Urban J, Chrzová M. 2004. Diagnostics of larval toxocariasis. Klin Mikrobiol Infekc Lek 10:181–185. [PubMed] [Google Scholar]
- 28.Nossal GJV. 1992. The molecular and cellular basis of affinity maturation in the antibody response. Cell 68:1–2. doi: 10.1016/0092-8674(92)90198-L. [DOI] [PubMed] [Google Scholar]
- 29.Sinha R, Khare SK. 2014. Structural changes in halophilic and non-halophilic proteases in response to chaotropic reagents. Protein J 33:394–402. doi: 10.1007/s10930-014-9571-0. [DOI] [PubMed] [Google Scholar]
- 30.Hedman L, Söderlund-Venermo M, Jartti T, Ruuskanen O, Hedman K. 2010. Dating of human bocavirus infection with protein-denaturing IgG-avidity assays—secondary immune activations are ubiquitous in immunocompetent adults. J Clin Virol 48:44–48. doi: 10.1016/j.jcv.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Fricker-Hidalgo H, Cimon B, Chemla C, Darde ML, Delhaes L, L'Ollivier C, Godineau N, Houze S, Paris L, Quinio D, Robert-Gangneux F, Villard O, Villena I, Candolfi E, Pelloux H. 2013. Toxoplasma seroconversion with negative or transient immunoglobulin M in pregnant women: myth or reality? A French multicenter retrospective study. J Clin Microbiol 51:2103–2111. doi: 10.1128/JCM.00169-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dziemian E, Zarnowska H, Kolodziej-Sobocinska M, Machnicka B. 2008. Determination of the relative avidity of the specific IgG antibodies in human toxocariasis. Parasite Immunol 30:187–190. doi: 10.1111/j.1365-3024.2007.01010.x. [DOI] [PubMed] [Google Scholar]
- 33.Caldera F, Burlone ME, Genchi C, Pirisi M, Bartoli E. 2013. Toxocara encephalitis presenting with autonomous nervous system involvement. Infection 41:691–694. doi: 10.1007/s15010-012-0342-6. [DOI] [PubMed] [Google Scholar]
- 34.Magnaval JF, Glickman LT, Dorchies P, Morassin B. 2001. Highlights of human toxocariasis. Korean J Parasitol 39:1–11. doi: 10.3347/kjp.2001.39.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barry MA, Weatherhead JE, Hotez PJ, Woc-Colburn L. 2013. Childhood parasitic infections endemic to the United States. Pediatr Clin North Am 60:471–485. doi: 10.1016/j.pcl.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 36.Smith HV, Noordin R. 2006. Diagnostic limitations and future trends in the serodiagnosis of human toxocariasis, p 89–112. In Holland CV, Smith HV (ed), Toxocara: the enigmatic parasite. CABI Publishing, Cambridge, MA. [Google Scholar]
- 37.Liao CW, Sukati H, D'Lamini P, Chou CM, Liu YH, Huang YC, Chung MH, Mtsetfwa JS, Jonato J, Chiu WT, Chang PW, Du WY, Chan HC, Chu TB, Cheng HC, Su WW, Tu CC, Cheng CY, Fan CK. 2010. Seroprevalence of Toxocara canis infection among children in Swaziland, southern Africa. Ann Trop Med Parasitol 104:73–80. doi: 10.1179/136485910X12607012373795. [DOI] [PubMed] [Google Scholar]
- 38.Rubinsky-Elefant G, Hirata CE, Yamamoto JH, Ferreira MU. 2010. Human toxocariasis: diagnosis, worldwide seroprevalences and clinical expression of the systemic and ocular forms. Ann Trop Med Parasitol 104:3–23. doi: 10.1179/136485910X12607012373957. [DOI] [PubMed] [Google Scholar]
- 39.Fu CJ, Chuang TW, Lin HS, Wu CH, Liu YC, Langinlur MK, Lu MY, Hsiao Wesley WW, Fan CK. 2014. Seroepidemiology of Toxocara canis infection among primary schoolchildren in the capital area of the Republic of the Marshall Islands. BMC Infect Dis 14:261. doi: 10.1186/1471-2334-14-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alderete JM, Jacob CM, Pastorino AC, Elefant GR, Castro AP, Fomin AB, Chieffi PP. 2003. Prevalence of Toxocara infection in schoolchildren from the Butanta Region, Sao Paulo, Brazil. Mem Inst Oswaldo Cruz 98:593–597. doi: 10.1590/S0074-02762003000500002. [DOI] [PubMed] [Google Scholar]
- 41.Wolfe A, Wright IP. 2003. Human toxocariasis and direct contact with dogs. Vet Rec 152:419–422. doi: 10.1136/vr.152.14.419. [DOI] [PubMed] [Google Scholar]
- 42.Nagakura K, Tachibana H, Kaneda Y, Kato Y. 1989. Toxocariasis possibly caused by ingesting raw chicken. J Infect Dis 160:735–736. doi: 10.1093/infdis/160.4.735. [DOI] [PubMed] [Google Scholar]
- 43.Stürchler D, Weiss N, Gassner M. 1990. Transmission of toxocariasis. J Infect Dis 162:571. doi: 10.1093/infdis/162.2.571-a,10.1093/infdis/162.2.571. [DOI] [PubMed] [Google Scholar]
- 44.Salem G, Schantz P. 1992. Toxocaral visceral larva migrans after ingestion of raw lamb liver. Clin Infect Dis 15:743–744. doi: 10.1093/clind/15.4.743. [DOI] [PubMed] [Google Scholar]
- 45.Hill SL, Cheney JM, Taton-Allen GF, Reif JS, Bruns C, Lappin MR. 2000. Prevalence of enteric zoononotic organisms in cats. J Am Vet Med Assoc 216:687–692. doi: 10.2460/javma.2000.216.687. [DOI] [PubMed] [Google Scholar]
- 46.Robertson ID, Thomson RC. 2002. Enteric parasitic zoonoses of domesticated dogs and cats. Microbes Infect 4:867–873. doi: 10.1016/S1286-4579(02)01607-6. [DOI] [PubMed] [Google Scholar]
- 47.Akao N, Ohta N. 2007. Toxocariasis in Japan. Parasitol Int 56:87–93. doi: 10.1016/j.parint.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 48.Yoshikawa M, Nishiofuku M, Moriya K, Ouji Y, Ishizaka S, Kasahara K, Mikasa K, Hirai T, Mizuno Y, Ogawa S, Nakamura T, Maruyama H, Akao N. 2008. A familial case of visceral toxocariasis due to consumption of raw bovine liver. Parasitol Int 57:525–529. doi: 10.1016/j.parint.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 49.Noh Y, Hong ST, Yun JY, Park HK, Oh JH, Kim YE, Jeon BS. 2012. Meningitis by Toxocara canis after ingestion of raw ostrich liver. J Korean Med Sci 27:1105–1108. doi: 10.3346/jkms.2012.27.9.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Macpherson CN. 2013. The epidemiology and public health importance of toxocariasis: a zoonosis of global importance. Int J Parasitol 43:999–1008. doi: 10.1016/j.ijpara.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 51.Viney ME, Graham AL. 2013. Patterns and processes in parasite co-infection. Adv Parasitol 82:321–369. doi: 10.1016/B978-0-12-407706-5.00005-8. [DOI] [PubMed] [Google Scholar]
- 52.Paul M, King L, Carlin EP. 2010. Zoonoses of people and their pets: a US perspective on significant pet-associated parasitic diseases. Trends Parasitol 26:153–154. doi: 10.1016/j.pt.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 53.Aydenizoz-Ozkayhan M, Yagci BB, Erat S. 2008. The investigation of Toxocara canis eggs in coats of different dog breeds as a potential transmission route in human toxocariasis. Vet Parasitol 152:94–100. doi: 10.1016/j.vetpar.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 54.Roddie G, Stafford P, Holland C, Wolfe A. 2008. Contamination of dog hair with eggs of Toxocara canis. Vet Parasitol 152:85–93. doi: 10.1016/j.vetpar.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 55.Amaral HL, Rassier GL, Pepe MS, Gallina T, Villela MM, Nobre MO, Scaini CJ, Berne ME. 2010. Presence of Toxocara canis eggs on the hair of dogs: a risk factor for visceral larva migrans. Vet Parasitol 174:115–118. doi: 10.1016/j.vetpar.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 56.El-Tras WF, Holt HR, Tayel AA. 2011. Risk of Toxocara canis eggs in stray and domestic dog hair in Egypt. Vet Parasitol 178:319–323. doi: 10.1016/j.vetpar.2010.12.051. [DOI] [PubMed] [Google Scholar]
- 57.Keegan JD, Holland CV. 2010. Contamination of the hair of owned dogs with eggs of Toxocara spp. Vet Parasitol 173:161–164. doi: 10.1016/j.vetpar.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 58.Esch KJ, Petersen CA. 2013. Transmission and epidemiology of zoonotic protozoal diseases of companion animals. Clin Microbiol Rev 26:58–85. doi: 10.1128/CMR.00067-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Congdon P, Lloyd P. 2011. Toxocara infection in the United States: the relevance of poverty, geography and demography as risk factors, and implications for estimating county prevalence. Int J Public Health 56:15–24. doi: 10.1007/s00038-010-0143-6. [DOI] [PubMed] [Google Scholar]
- 60.Quinnell RJ. 2003. Genetics of susceptibility to human helminth infection. Int J Parasitol 33:1219–1231. doi: 10.1016/S0020-7519(03)00175-9. [DOI] [PubMed] [Google Scholar]
- 61.Dold C, Holland CV. 2011. Investigating the underlying mechanism of resistance to Ascaris infection. Microbes Infect 13:624–631. doi: 10.1016/j.micinf.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 62.Chan PW, Anuar AK, Fong MY, Debruyne JA, Ibrahim J. 2001. Toxocara seroprevalence and childhood asthma among Malaysian children. Pediatr Int 43:350–353. doi: 10.1046/j.1442-200X.2001.01421.x. [DOI] [PubMed] [Google Scholar]
- 63.Vidal JE, Sztajnbok J, Seguro AC. 2003. Eosinophilic meningoencephalitis due to Toxocara canis: case report and review of the literature. Am J Trop Med Hyg 69:341–343. [PubMed] [Google Scholar]
- 64.Gavignet B, Piarroux R, Aubin F, Millon L, Humbert P. 2008. Cutaneous manifestations of human toxocariasis. J Am Acad Dermatol 59:1031–1042. doi: 10.1016/j.jaad.2008.06.031. [DOI] [PubMed] [Google Scholar]
- 65.López ML, Bojanich MV, Jacobacci JM, Sercic C, Michelini A, Alonso JM. 2010. Toxocara canis and bronchial asthma. Medicina (B Aires) 70:75–78. [PubMed] [Google Scholar]
- 66.Salvador S, Ribeiro R, Winckler MI, Ohlweiler L, Riesgo R. 2010. Pediatric neurotoxocariasis with concomitant cerebral, cerebellar, and peripheral nervous system involvement: case report and review of the literature. J Pediatr (Rio J) 86:531–534. doi: 10.1590/S0021-75572010000600015. [DOI] [PubMed] [Google Scholar]
- 67.Stoicescu RM, Mihai CM, Giannakopoulou AD. 2011. Marked hypereosinophilia in a toddler: a case report. J Med Life 4:105–108. [PMC free article] [PubMed] [Google Scholar]
- 68.Damasceno EF, Damasceno NA. 2012. Anterior uveitis after treatment of hepatitis C with alpha interferon: the recurrence of a previous inflammatory process due to presumed ocular toxocariasis. Ocul Immunol Inflamm 20:53–55. doi: 10.3109/09273948.2011.615448. [DOI] [PubMed] [Google Scholar]
- 69.Ranasuriya G, Mian A, Boujaoude Z, Tsigrelis C. 2014. Pulmonary toxocariasis: a case report and literature review. Infection 42:575–578. doi: 10.1007/s15010-014-0587-3. [DOI] [PubMed] [Google Scholar]
- 70.Bachli H, Minet JC, Gratzl O. 2004. Cerebral toxocariasis: a possible cause of epileptic seizure in children. Childs Nerv Syst 20:468–472. doi: 10.1007/s00381-004-0963-x. [DOI] [PubMed] [Google Scholar]
- 71.Nicoletti A, Bartoloni A, Sofia V, Mantella A, Nsengiyumva G, Frescaline G, Preux PM. 2007. Epilepsy and toxocariasis: a case-control study in Burundi. Epilepsia 48:894–899. doi: 10.1111/j.1528-1167.2007.01104.x. [DOI] [PubMed] [Google Scholar]
- 72.Quattrocchi G, Nicoletti A, Marin B, Bruno E, Druet-Cabanac M, Preux PM. 2012. Toxocariasis and epilepsy: systematic review and meta-analysis. PLoS Negl Trop Dis 6:e1775. doi: 10.1371/journal.pntd.0001775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ngugi AK, Bottomley C, Kleinschmidt I, Wagner RG, Kakooza-Mwesige A, Ae-Ngibise K, Owusu-Agyei S, Masanja H, Kamuyu G, Odhiambo R, Chengo E, Sander JW, Newton CR, SEEDS Group . 2013. Prevalence of active convulsive epilepsy in sub-Saharan Africa and associated risk factors: cross-sectional and case-control studies. Lancet Neurol 12:253–263. doi: 10.1016/S1474-4422(13)70003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Magnaval JF, Galindo V, Glickman LT, Clanet M. 1997. Human Toxocara infection of the central nervous system and neurological disorders: a case-control study. Parasitology 115:537–543. doi: 10.1017/S0031182097001558. [DOI] [PubMed] [Google Scholar]
- 75.Richartz E, Buchkremer G. 2002. Cerebral toxocariasis: a rare cause of cognitive disorders. A contribution to differential dementia diagnosis. Nervenarzt 73:458–462. [DOI] [PubMed] [Google Scholar]
- 76.Taylor MR, Keane CT, O'Connor P, Mulvihill E, Holland C. 1988. The expanded spectrum of toxocaral disease. Lancet i:692–695. [DOI] [PubMed] [Google Scholar]
- 77.Nathwani D, Laing RB, Currie PF. 1992. Covert toxocariasis—a cause of recurrent abdominal pain in childhood. Br J Clin Pract 46:271. [PubMed] [Google Scholar]
- 78.Rasmussen LN, Dirdal M, Birkebaek NH. 1993. “Covert toxocariasis” in a child treated with low-dose diethylcarbamazine. Acta Paediatr 82:116–118. doi: 10.1111/j.1651-2227.1993.tb12537.x. [DOI] [PubMed] [Google Scholar]
- 79.Kayes SG. 1997. Human toxocariasis and the visceral larva migrans syndrome: correlative immunopathology. Chem Immunol 66:99–124. doi: 10.1159/000058667. [DOI] [PubMed] [Google Scholar]
- 80.Fan CK, Hung CC, Lin YH, Li MH, Su KE. 2004. Enhanced expression of transforming growth factor-β1 in inflammatory cells and secretory granules in Paneth cells in the small intestine of mice infected with Toxocara canis. Parasitol Res 94:397–404. doi: 10.1007/s00436-004-1233-2. [DOI] [PubMed] [Google Scholar]
- 81.Wu MS, Liao CW, Du WY, Kao TC, Su KE, Lin YH, Chang CC, Fan CK. 2008. Enhanced expression of transforming growth factor beta1 in inflammatory cells, alpha-smooth muscle actin in stellate cells, and collagen accumulation in experimental granulomatous hepatitis caused by Toxocara canis in mice. Acta Trop 105:260–268. doi: 10.1016/j.actatropica.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 82.Liao CW, Fan CK, Kao TC, Ji DD, Su KE, Lin YH, Cho WL. 2008. Brain injury-associated biomarkers of TGF-beta1, S100B, GFAP, NF-L, tTG, AbetaPP, and tau were concomitantly enhanced and the UPS was impaired during acute brain injury caused by Toxocara canis in mice. BMC Infect Dis 8:84. doi: 10.1186/1471-2334-8-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Debrah AY, Batsa L, Albers A, Mand S, Toliat MR, Nurnberg P, Adjei O, Hoerauf A, Pfarr K. 2011. Transforming growth factor-β1 variant Leu10Pro is associated with both lack of microfilariae and differential microfilarial loads in the blood of persons infected with lymphatic filariasis. Hum Immunol 72:1143–1148. doi: 10.1016/j.humimm.2011.07.305. [DOI] [PubMed] [Google Scholar]
- 84.Maizels RM. 2013. Toxocara canis: molecular basis of immune recognition and evasion. Vet Parasitol 193:365–374. doi: 10.1016/j.vetpar.2012.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dent LA, Daly CM, Mayrhofer G, Zimmerman T, Hallett A, Bignold LP, Creaney J, Parsons JC. 1999. Interleukin-5 transgenic mice show enhanced resistance to primary infections with Nippostrongylus brasiliensis but not primary infections with Toxocara canis. Infect Immun 67:989–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Giacomin PR, Cava M, Tumes DJ, Gauld AD, Iddawela DR, McColl SR, Parsons JC, Gordon DL, Dent LA. 2008. Toxocara canis larval excretory/secretory proteins impair eosinophil dependent resistance of mice to Nippostrongylus brasiliensis. Parasite Immunol 30:435–445. doi: 10.1111/j.1365-3024.2008.01040.x. [DOI] [PubMed] [Google Scholar]
- 87.Beaver PC, Snyder CH, Carrera GM, Dent JH, Lafferty JW. 1952. Chronic eosinophilia due to visceral larva migrans. Report of three cases. Pediatrics 9:7–19. [PubMed] [Google Scholar]
- 88.Bede O, Szenasi Z, Danka J, Gyurkovits Nagy KD. 2008. Toxocariasis associated with chronic cough in childhood: a longitudinal study in Hungary. J Helminthol 82:357–363. doi: 10.1017/S0022149X0804827X. [DOI] [PubMed] [Google Scholar]
- 89.Musso C, Castelo JS, Tsanaclis AM, Pereira FE. 2007. Prevalence of Toxocara-induced liver granulomas, detected by immunohistochemistry, in a series of autopsies at a Children's Reference Hospital in Vitória, ES, Brazil. Virchows Arch 450:411–447. doi: 10.1007/s00428-007-0388-5. [DOI] [PubMed] [Google Scholar]
- 90.Hartleb M, Januszewski K. 2001. Severe hepatic involvement in visceral larva migrans. Eur J Gastroenterol Hepatol 13:1245–1249. doi: 10.1097/00042737-200110000-00020. [DOI] [PubMed] [Google Scholar]
- 91.Giembycz MA, Lindsay MA. 1999. Pharmacology of the eosinophil. Pharmacol Rev 51:213–340. [PubMed] [Google Scholar]
- 92.Hosoyama T, Aslam MI, Abraham J, Prajapati SI, Nishijo K, Michalek JE, Zarzabal LA, Nelon LD, Guttridge DC, Rubin BP, Keller C. 2011. IL-4R drives dedifferentiation, mitogenesis, and metastasis in rhabdomyosarcoma. Clin Cancer Res 17:2757–2766. doi: 10.1158/1078-0432.CCR-10-3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jelachich ML, Bramlage C, Lipton HL. 1999. Differentiation of M1 myeloid precursor cells into macrophages results in binding and infection by Theiler's murine encephalomyelitis virus and apoptosis. J Virol 73:3227–3235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Luo H, Hao Y, Tang B, Zeng D, Shi Y, Yu P. 2012. Mouse forestomach carcinoma cells immunosuppress macrophages through transforming growth factor-β1. Mol Med Rep 5:988–992. doi: 10.3892/mmr.2012.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wilder HC. 1950. Nematode endophthalmitis. Trans Am Acad Ophthalmol Otolaryngol 55:99–109. [PubMed] [Google Scholar]
- 96.Arevalo JF, Espinoza JV, Arevalo FA. 2013. Ocular toxocariasis. J Pediatr Ophthalmol Strabismus 50:76–86. doi: 10.3928/01913913-20120821-01. [DOI] [PubMed] [Google Scholar]
- 97.Treadway MT, Zald DH. 2013. Parsing anhedonia: translational models of reward-processing deficits in psychopathology. Curr Dir Psychol Sci 22:244–249. doi: 10.1177/0963721412474460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Woodhall D, Starr MC, Montgomery SP, Jones JL, Lum F, Read RW, Moorthy RS. 2012. Ocular toxocariasis: epidemiologic, anatomic, and therapeutic variations based on a survey of ophthalmic subspecialists. Ophthalmology 119:1211–1217. doi: 10.1016/j.ophtha.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 99.Sabrosa NA, de Souza EC. 2001. Nematode infections of the eye: toxocariasis and diffuse unilateral subacute neuroretinitis. Curr Opin Ophthalmol 12:450–454. doi: 10.1097/00055735-200112000-00010. [DOI] [PubMed] [Google Scholar]
- 100.Wilkinson CP, Welch RB. 1971. Intraocular Toxocara. Am J Ophthalmol 71:921–930. doi: 10.1016/0002-9394(71)90267-4. [DOI] [PubMed] [Google Scholar]
- 101.Yokoi K, Goto H, Sakai J, Usui M. 2003. Clinical features of ocular toxocariasis in Japan. Ocul Immunol Inflamm 11:269–275. doi: 10.1076/ocii.11.4.269.18266. [DOI] [PubMed] [Google Scholar]
- 102.Do Lago A, Andrade R, Muccioli C, Belfort R Jr. 2006. Optical coherence tomography in presumed subretinal Toxocara granuloma: case report. Arq Bras Oftalmol 69:403–405. doi: 10.1590/S0004-27492006000300022. [DOI] [PubMed] [Google Scholar]
- 103.Stewart JM, Cubillan LD, Cunningham ET Jr. 2005. Prevalence, clinical features, and causes of vision loss among patients with ocular toxocariasis. Retina 25:1005–1013. doi: 10.1097/00006982-200512000-00009. [DOI] [PubMed] [Google Scholar]
- 104.Cortez RT, Ramirez G, Collet L, Giuliari GP. 2011. Ocular parasitic diseases: a review on toxocariasis and diffuse unilateral subacute neuroretinitis. J Pediatr Ophthalmol Strabismus 48:204–212. doi: 10.3928/01913913-20100719-02. [DOI] [PubMed] [Google Scholar]
- 105.Centers for Disease Control and Prevention. 2011. Ocular toxocariasis—United States, 2009–2010. MMWR Morb Mortal Wkly Rep 60:734–736. [PubMed] [Google Scholar]
- 106.Arevalo JF, Garcia-Amaris RA. 2008. The role of vitreo-retinal surgery in children with uveitis. Int Ophthalmol Clin 48:153–172. doi: 10.1097/IIO.0b013e31817d7fc1. [DOI] [PubMed] [Google Scholar]
- 107.Gass JD, Gilbert WR, Guerry RK, Scelfo R. 1978. Diffuse unilateral subacute neuroretinitis. Ophthalmology 85:521–545. doi: 10.1016/S0161-6420(78)35645-1. [DOI] [PubMed] [Google Scholar]
- 108.de Souza EC, Nakashima Y. 1995. Diffuse unilateral subacute neuroretinitis. Report of transvitreal surgical removal of a subretinal nematode. Ophthalmology 102:1183–1186. [DOI] [PubMed] [Google Scholar]
- 109.Shields CL, Schoenberg E, Kocher K, Shukla SY, Kaliki S, Shields JA. 2013. Lesions simulating retinoblastoma (pseudoretinoblastoma) in 604 cases: results based on age at presentation. Ophthalmology 120:311–316. doi: 10.1016/j.ophtha.2012.07.067. [DOI] [PubMed] [Google Scholar]
- 110.Small J, Schaefer PW. 2012. Neuroradiology: key differential diagnoses and clinical questions. Saunders, Philadelphia, PA. [Google Scholar]
- 111.Taylor MR. 2001. The epidemiology of ocular toxocariasis. J Helminthol 75:109–118. doi: 10.1079/JOH200175. [DOI] [PubMed] [Google Scholar]
- 112.Vitale AT, Foster CS. 2005. Uveitis affecting infants and children: infectious causes, p 250–289. In Hartnett ME, Trese M, Capone A Jr, Bronya JBK, Scott MS (ed), Pediatric retina. Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 113.Jones JL, Kruszon-Moran D, Won K, Wilson M, Schantz PM. 2008. Toxoplasma gondii and Toxocara spp. co-infection. Am J Trop Med Hyg 78:35–39. [PubMed] [Google Scholar]
- 114.Lee IH, Kim ST, Oh DK, Kim HJ, Kim KH, Jeon P, Byun HS. 2010. MRI findings of spinal visceral larva migrans of Toxocara canis. Eur J Radiol 75:236–240. doi: 10.1016/j.ejrad.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 115.Hayashi E, Akao N, Fujita K. 2003. Evidence for the involvement of the optic nerve as a migration route for larvae in ocular toxocariasis of Mongolian gerbils. J Helminthol 77:311–315. doi: 10.1079/JOH2003186. [DOI] [PubMed] [Google Scholar]
- 116.Taylor MR, Keane CT, O'Connor P, Girdwood RW, Smith H. 1987. Clinical features of covert toxocariasis. Scand J Infect Dis 19:693–696. doi: 10.3109/00365548709117206. [DOI] [PubMed] [Google Scholar]
- 117.Glickman LT, Magnaval JF, Domanski LM, Shofer FS, Lauria SS, Gottstein B, Brochier B. 1987. Visceral larva migrans in French adults: a new disease syndrome? Am J Epidemiol 125:1019–1034. [DOI] [PubMed] [Google Scholar]
- 118.Xinou E, Lefkopoulos A, Gelagoti M, Drevelegas A, Diakou A, Milonas I, Dimitriadis AS. 2003. CT and MR imaging findings in cerebral toxocaral disease. Am J Neuroradiol 24:714–718. [PMC free article] [PubMed] [Google Scholar]
- 119.Beautyman W, Woolf AL. 1951. An ascaris larva in the brain in association with acute anterior poliomyelitis. J Pathol Bacteriol 63:635–647. doi: 10.1002/path.1700630410. [DOI] [PubMed] [Google Scholar]
- 120.Nichols RL. 1956. The etiology of visceral larva migrans. Diagnostic morphology and infective second stage. J Parasitol 42:349–362. [PubMed] [Google Scholar]
- 121.Finsterer J, Auer H. 2007. Neurotoxocarosis. Rev Inst Med Trop Sao Paulo 49:279–287. doi: 10.1590/S0036-46652007000500002. [DOI] [PubMed] [Google Scholar]
- 122.Hotez PJ, Wilkins PP. 2009. Toxocariasis: America's most common neglected infection of poverty and a helminthiasis of global importance? PLoS Negl Trop Dis 3:e400. doi: 10.1371/journal.pntd.0000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Eberhardt O, Bialek R, Nagele T, Dichgans J. 2005. Eosinophilic meningomyelitis in toxocariasis: case report and review of the literature. Clin Neurol Neurosurg 107:432–438. doi: 10.1016/j.clineuro.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 124.Wang C, Huang CY, Chan PH, Preston P, Chau PY. 1983. Transverse myelitis associated with larva migrans: finding of larva in cerebrospinal fluid. Lancet i:423. [DOI] [PubMed] [Google Scholar]
- 125.Goffette S, Jeanjean AP, Duprez TP, Bigaignon G, Sindic CJ. 2000. Eosinophilic pleocytosis and myelitis related to Toxocara canis infection. Eur J Neurol 7:703–706. doi: 10.1046/j.1468-1331.2000.00123.x. [DOI] [PubMed] [Google Scholar]
- 126.Graeff-Teixeira C, da Silva AC, Yoshimura K. 2009. Update on eosinophilic meningoencephalitis and its clinical relevance. Clin Microbiol Rev 22:322–348. doi: 10.1128/CMR.00044-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gavin PJ, Kazacos KR, Shulman ST. 2005. Baylisascariasis. Clin Microbiol Rev 18:703–718. doi: 10.1128/CMR.18.4.703-718.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Boyce WM, Asai DJ, Wilder JK, Kazacos KR. 1989. Physiochemical characterization and monoclonal and polyclonal antibody recognition of Baylisascaris procyonis larval excretory-secretory antigens. J Parasitol 75:540–548. doi: 10.2307/3282903. [DOI] [PubMed] [Google Scholar]
- 129.Gavin PJ, Kazacos KR, Tan TQ, Brinkman WB, Byrd SE, Davis AT, Mets MB, Shulman ST. 2002. Neural larval migrans caused by the raccoon roundworm Baylisascaris procyonis. Pediatr Infect Dis J 21:971–975. doi: 10.1097/00006454-200210000-00017. [DOI] [PubMed] [Google Scholar]
- 130.Moertel CL, Kazacos KR, Butterfield JH, Kita H, Watterson J, Gleich GJ. 2001. Eosinophil-associated inflammation and elaboration of eosinophil-derived proteins in two children with raccoon roundworm (Baylisascaris procyonis) encephalitis. Pediatrics 108:e93. doi: 10.1542/peds.108.5.e93. [DOI] [PubMed] [Google Scholar]
- 131.Park SY, Glaser C, Murray WJ, Kazacos KK, Rowley HA, Fredrick DR, Bass N. 2000. Raccoon roundworm (Baylisascaris procyonis) encephalitis: case report and field investigation. Pediatrics 106:e56. doi: 10.1542/peds.106.4.e56. [DOI] [PubMed] [Google Scholar]
- 132.Sommer C, Ringelstein EB, Biniek R, Glöckner WM. 1994. Adult Toxocara canis encephalitis. J Neurol Neurosurg Psychiatry 57:229–231. doi: 10.1136/jnnp.57.2.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Osoegawa M. 2004. Diagnosis and treatment of CNS parasite infection with special reference to parasitic myelitis. Rinsho Shinkeigaku 44:961–964. [PubMed] [Google Scholar]
- 134.Umehara F, Ookatsu H, Hayashi D, Uchida A, Douchi Y, Kawabata H, Goto R, Hashiguchi A, Matsuura E, Okubo R, Higuchi I, Arimura K, Nawa Y, Osame M. 2006. MRI studies of spinal visceral larva migrans syndrome. J Neurol Sci 249:7–12. doi: 10.1016/j.jns.2006.05.057. [DOI] [PubMed] [Google Scholar]
- 135.Helsen G, Vandecasteele SJ, Vanopdenbosch LJ. 2011. Toxocariasis presenting as encephalomyelitis. Case Rep Med 2011:503913. doi: 10.1155/2011/503913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Dupas B, Barrier J, Barre P. 1986. Detection of Toxocara by computed tomography. Br J Radiol 59:518–519. doi: 10.1259/0007-1285-59-701-518. [DOI] [PubMed] [Google Scholar]
- 137.Rüttinger P, Hadidi H. 1991. MRI in cerebral toxocaral disease. J Neurol Neurosurg Psychiatry 54:361–362. doi: 10.1136/jnnp.54.4.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Jabbour RA, Kanj SS, Sawaya RA, Awar GN, Hourani MH, Atweh SF. 2011. Toxocara canis myelitis: clinical features, magnetic resonance imaging (MRI) findings, and treatment outcome in 17 patients. Medicine 90:337–343. doi: 10.1097/MD.0b013e31822f63fb. [DOI] [PubMed] [Google Scholar]
- 139.Rowley HA, Uht RM, Kazacos KR, Sakamari J, Wheaton WV, Barkovich AJ, Bollen AW. 2000. Radiologic-pathologic findings in raccoon roundworm (Bayliscaris procyonis) encephalitis. Am J Neuroradiol 21:415–420. [PMC free article] [PubMed] [Google Scholar]
- 140.Chotmongkol V, Sawanyawisuth K, Thavornpitak Y. 2000. Corticosteroid treatment of eosinophilic meningitis. Clin Infect Dis 31:660–662. doi: 10.1086/314036. [DOI] [PubMed] [Google Scholar]
- 141.Jung H, Hurtado M, Medina MT, Sanchez M, Sotelo J. 1990. Dexamethasone increases plasma levels of albendazole. J Neurol 273:279–280. [DOI] [PubMed] [Google Scholar]
- 142.Mimoso MG, Pereira MC, Estevao MH, Barroso AA, Mota HC. 1993. Eosinophilic meningoencephalitis due to Toxocara canis. Eur J Pediatr 152:783–784. doi: 10.1007/BF01954007. [DOI] [PubMed] [Google Scholar]
- 143.Hill IR, Denham DA, Scholtz CL. 1985. Toxocara canis larvae in the brain of a British child. Trans R Soc Trop Med Hyg 79:351–354. doi: 10.1016/0035-9203(85)90378-5. [DOI] [PubMed] [Google Scholar]
- 144.Lompo LD, Kamdem FK, Revenco E, Allibert R, Medeiros E, Vuillier F, Moulin T. 2012. Toxocara canis cerebral vasculitis revealed by iterative strokes. Rev Neurol 168:533–537. doi: 10.1016/j.neurol.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 145.Kumar J, Kimm J. 1994. MR in Toxocara canis myelopathy. Am J Neuroradiol 15:1918–1920. [PMC free article] [PubMed] [Google Scholar]
- 146.Strupp M, Pfister HW, Eichenlaub S, Arbusow V. 1999. Meningomyelitis in a case of toxocariasis with markedly isolated CSF eosinophilia and MRI documented thoracic cord lesion. J Neurol 246:241–244. [DOI] [PubMed] [Google Scholar]
- 147.Sellal F, Picard F, Mutschler V, Marescaux C, Collard M, Magnaval JF. 1992. Myelitis caused by Toxocara canis (larva migrans). Rev Neurol 148:53–55. [PubMed] [Google Scholar]
- 148.Ota S, Komiyama A, Johkura K, Hasegawa O, Kondo K. 1994. Eosinophilic meningo-encephalo-myelitis due to Toxocara canis. Rinsho Shinkeigaku 34:1148–1152. [PubMed] [Google Scholar]
- 149.Stone R. 2002. Infectious disease. Siberia's deadly stalker emerges from the shadows. Science 296:642–645. doi: 10.1126/science.296.5568.642. [DOI] [PubMed] [Google Scholar]
- 150.Goldfarb LG, Gajdusek DC. 1992. Viliuisk encephalomyelitis in the Iakut people of Siberia. Brain 115:961–978. doi: 10.1093/brain/115.4.961. [DOI] [PubMed] [Google Scholar]
- 151.Storch A, Kassubek J, Tumani H, Vladimirtsev VA, Hermann A, Osakovsky VL, Baranov VA, Krivoshapkin VG, Ludolph AC. 2014. Communicating hydrocephalus following eosinophilic meningitis is pathogenic for chronic Viliuisk encephalomyelitis in northeastern Siberia. PLoS One 9:e84670. doi: 10.1371/journal.pone.0084670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Storch A, Vladimirtsev VA, Tumani H, Wellinghausen N, Haas A, Krivoshapkin VG, Ludolph AC. 2008. Viliuisk encephalomyelitis in northeastern Siberia is not caused by Borrelia burgdorferi infection. Neurol Sci 29:11–14. doi: 10.1007/s10072-008-0852-2. [DOI] [PubMed] [Google Scholar]
- 153.Marchi N, Granata T, Janigro D. 2014. Inflammatory pathways of seizure disorders. Trends Neurosci 37:55–65. doi: 10.1016/j.tins.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Newton CR, Garcia HH. 2012. Epilepsy in poor regions of the world. Lancet 380:1193–1201. doi: 10.1016/S0140-6736(12)61381-6. [DOI] [PubMed] [Google Scholar]
- 155.Woodruff AW, Bisseru B, Bowe JC. 1966. Infection with animal helminths as a factor in causing poliomyelitis and epilepsy. Br Med J 1:1576–1579. doi: 10.1136/bmj.1.5503.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Critchley EM, Vakil SD, Hutchinson DN, Taylor P. 1982. Toxoplasma, Toxocara, and epilepsy. Epilepsia 23:315–321. doi: 10.1111/j.1528-1157.1982.tb06197.x. [DOI] [PubMed] [Google Scholar]
- 157.Arpino C, Gattinara GC, Piergili D, Curatolo P. 1990. Toxocara infection and epilepsy in children: a case-control study. Epilepsia 31:33–36. doi: 10.1111/j.1528-1157.1990.tb05356.x. [DOI] [PubMed] [Google Scholar]
- 158.Zibaei M, Firoozeh F, Bahrami P, Sadjjadi SM. 2013. Investigation of anti-Toxocara antibodies in epileptic patients and comparison of two methods: ELISA and Western blotting. Epilepsy Res Treat 2013:156815. doi: 10.1155/2013/156815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kamuyu G, Bottomley C, Mageto J, Lowe B, Wilkins PP, Noh JC, Nutman TB, Ngugi AK, Odhiambo R, Wagner RG, Kakooza-Mwesige A, Owusu-Agyei S, Ae-Ngibise K, Masanja H, Osier FH, Odermatt P, Newton CR, Study of Epidemiology of Epilepsy in Demographic Sites (SEEDS) Group. 2014. Exposure to multiple parasites is associated with the prevalence of active convulsive epilepsy in sub-Saharan Africa. PLoS Negl Trop Dis 8:e2908. doi: 10.1371/journal.pntd.0002908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Magnaval JF, Fabre R, Maurières P, Charlet JP, de Larrard B. 1991. Application of the western blotting procedure for the immunodiagnosis of human toxocariasis. Parasitol Res 77:697–702. doi: 10.1007/BF00928685. [DOI] [PubMed] [Google Scholar]
- 161.Garcia HH, Modi M. 2008. Helminthic parasites and seizures. Epilepsia 49(Suppl 6):25–32. doi: 10.1111/j.1528-1167.2008.01753.x. [DOI] [PubMed] [Google Scholar]
- 162.Perez SM, Lodge DJ. 2014. New approaches to the management of schizophrenia: focus on aberrant hippocampal drive of dopamine pathways. Drug Des Dev Ther 8:887–896. doi: 10.2147/DDDT.S42708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Brisch R, Saniotis A, Wolf R, Bielau H, Bernstein HG, Steiner J, Bogerts B, Braun AK, Jankowski Z, Kumaritlake J, Henneberg M, Gos T. 2014. The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue. Front Psychiatry 5:47. doi: 10.3389/fpsyt.2014.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Barch DM, Ceasar A. 2012. Cognition in schizophrenia: core psychological and neural mechanisms. Trends Cogn Sci 16:27–34. doi: 10.1016/j.tics.2011.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Fabiani S, Pinto B, Bruschi F. 2013. Toxoplasmosis and neuropsychiatric diseases: can serological studies establish a clear relationship? Neurol Sci 34:417–425. doi: 10.1007/s10072-012-1197-4. [DOI] [PubMed] [Google Scholar]
- 166.Carlsson A, Lindqvist M. 1963. Effect of chlorpromazine or haloperidolon formation of 3 methoxytyramine and normetanephrine in mouse brain. Acta Pharmacol Toxicol 20:140–144. [DOI] [PubMed] [Google Scholar]
- 167.Wang YC, Ho UC, Ko MC, Liao CC, Lee LJ. 2012. Differential neuronal changes in medial prefrontal cortex, basolateral amygdale and nucleus accumbens after postweaning social isolation. Brain Struct Funct 217:337–351. doi: 10.1007/s00429-011-0355-4. [DOI] [PubMed] [Google Scholar]
- 168.Shen LH, Liao MH, Tseng YC. 2012. Recent advances in imaging of dopaminergic neurons for evaluation of neuropsychiatric disorders. J Biomed Biotechnol 2012:259349. doi: 10.1155/2012/259349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Pogarell O, Koch W, Karch S, Dehning S, Müller N, Tatsch K, Poepperl G, Möller HJ. 2012. Dopaminergic neurotransmission in patients with schizophrenia in relation to positive and negative symptoms. Pharmacopsychiatry 45:S36–S41. doi: 10.1055/s-0032-1306313. [DOI] [PubMed] [Google Scholar]
- 170.Othman AA, Abdel-Aleem GA, Saied EM, Mayah WW, Elatrash AM. 2010. Biochemical and immunopathological changes in experimental neurotoxocariasis. Mol Biochem Parasitol 172:1–8. doi: 10.1016/j.molbiopara.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 171.Dickson PW, Briggs GD. 2013. Tyrosine hydroxylase: regulation by feedback inhibition and phosphorylation. Adv Pharmacol 68:13–21. doi: 10.1016/B978-0-12-411512-5.00002-6. [DOI] [PubMed] [Google Scholar]
- 172.Thibaut F, Ribeyre JM, Dourmap N, Meloni R, Laurent C, Campion D, Ménard JF, Dollfus S, Mallet J, Petit M. 1997. Association of DNA polymorphism in the first intron of the tyrosine hydroxylase gene with disturbances of the catecholaminergic system in schizophrenia. Schizophr Res 23:259–264. doi: 10.1016/S0920-9964(96)00118-1. [DOI] [PubMed] [Google Scholar]
- 173.Di Fiore M, Virga A, Usticano V, Di Rosa S, Rini GB. 1989. Antibodies against Toxocara canis in human serum from western Sicily. Boll Ist Sieroter Milan 68:93–96. [PubMed] [Google Scholar]
- 174.Kaplan M, Kalkan A, Kuk S, Demirdag K, Ozden M, Kilic SS. 2008. Toxocara seroprevalence in schizophrenic patients in Turkey. Yonsei Med J 49:224–229. doi: 10.3349/ymj.2008.49.2.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.El-Sayed NM, Ismail KA. 2012. Relationship between Toxocara canis infection and schizophrenia. Rawal Med J 37:155–161. [Google Scholar]
- 176.Alvarado-Esquivel C. 2013. Toxocara infection in psychiatric inpatients: a case control seroprevalence study. PLoS One 8:e62606. doi: 10.1371/journal.pone.0062606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Khademvatan S, Khajeddin N, Izadi S, Yousefi E. 2014. Investigation of anti-Toxocara and anti-Toxoplasma antibodies in patients with schizophrenia disorder. Schizophr Res Treatment 2014:230349. doi: 10.1155/2014/230349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Cong W, Zhang XX, Zhou N, Yu CZ, Chen J, Wang XY, Li B, Qian AD, Zhu XQ. 2014. Toxocara seroprevalence among clinically healthy individuals, pregnant women and psychiatric patients and associated risk factors in Shandong Province, eastern China. PLoS Negl Trop Dis 8:e3082. doi: 10.1371/journal.pntd.0003082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Gorelick PB. 2010. Role of inflammation in cognitive impairment: results of observational epidemiological studies and clinical trials. Ann N Y Acad Sci 1207:155–162. doi: 10.1111/j.1749-6632.2010.05726.x. [DOI] [PubMed] [Google Scholar]
- 180.Wallin MT, Pretell EJ, Bustos JA, Caballero M, Alfaro M, Kane R, Wilken J, Sullivan C, Fratto T, Garcia HH. 2012. Cognitive changes and quality of life in neurocysticercosis: a longitudinal study. PLoS Negl Trop Dis 6:e1493. doi: 10.1371/journal.pntd.0001493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Jarosz W, Mizgajska-Wiktor H, Kirwan P, Konarski J, Rychlicki W, Wawrzyniak G. 2010. Developmental age, physical fitness and Toxocara seroprevalence amongst lower-secondary students living in rural areas contaminated with Toxocara eggs. Parasitology 137:53–63. doi: 10.1017/S0031182009990874. [DOI] [PubMed] [Google Scholar]
- 182.Fortenberry JD, Kenney RD, Younger J. 1991. Visceral larval migrans producing static encephalopathy in an infant. Pediatr Infect Dis J 10:403–406. doi: 10.1097/00006454-199105000-00011. [DOI] [PubMed] [Google Scholar]
- 183.Worley G, Green JA, Frothingham TE, Sturner RA, Walls KW, Pakalnis VA, Ellis GS Jr. 1984. Toxocara canis infection: clinical and epidemiological associations with seropositivity in kindergarten children. J Infect Dis 149:591–597. doi: 10.1093/infdis/149.4.591. [DOI] [PubMed] [Google Scholar]
- 184.Marmor M, Glickman L, Shofer F, Faich LA, Rosenberg C, Cornblatt B, Friedman S. 1987. Toxocara canis infection of children: epidemiologic and neuropsychologic findings. Am J Public Health 77:554–559. doi: 10.2105/AJPH.77.5.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Nelson S, Greene T, Ernhart CB. 1996. Toxocara canis infection in preschool age children: risk factors and the cognitive development of preschool children. Neurotoxicol Teratol 18:167–174. doi: 10.1016/0892-0362(95)02018-7. [DOI] [PubMed] [Google Scholar]
- 186.Lidsky TI, Schneider JS. 2003. Lead neurotoxicity in children: basic mechanisms and clinical correlates. Brain 126:5–19. doi: 10.1093/brain/awg014. [DOI] [PubMed] [Google Scholar]
- 187.Walsh MG, Haseeb MA. 2012. Reduced cognitive function in children with toxocariasis in a nationally representative sample of the United States. Int J Parasitol 42:1159–1163. doi: 10.1016/j.ijpara.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 188.Cox DM, Holland CV. 2001. Relationship between three intensity levels of Toxocara canis larvae in the brain and effects on exploration, anxiety, learning and memory in the murine host. J Helminthol 75:33–41. doi: 10.1079/JOH200028. [DOI] [PubMed] [Google Scholar]
- 189.Hamilton CM, Stafford P, Pinelli E, Holland CV. 2006. A murine model for cerebral toxocariasis: characterization of host susceptibility and behaviour. Parasitology 132:791–801. doi: 10.1017/S0031182006009887. [DOI] [PubMed] [Google Scholar]
- 190.Good B, Holland CV, Stafford P. 2001. The influence of inoculum size and time post-infection on the number and position of Toxocara canis larvae recovered from the brains of outbred CD1 mice. J Helminthol 75:175–181. doi: 10.1079/JOH200178. [DOI] [PubMed] [Google Scholar]
- 191.Burren CH. 1971. The distribution of Toxocara larvae in the central nervous system of the mouse. Trans R Soc Trop Med Hyg 65:450–453. doi: 10.1016/0035-9203(71)90155-6. [DOI] [PubMed] [Google Scholar]
- 192.Shulman JM, De Jager PL, Feany MB. 2011. Parkinson's disease: genetics and pathogenesis. Annu Rev Pathol 6:193–222. doi: 10.1146/annurev-pathol-011110-130242. [DOI] [PubMed] [Google Scholar]
- 193.Tufekci KU, Genc S, Genc K. 2011. The endotoxin-induced neuroinflammation model of Parkinson's disease. Parkinsons Dis 2011:487450. doi: 10.4061/2011/487450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Takahashi M, Yamada T. 1999. Viral etiology for Parkinson's disease—a possible role of influenza A virus infection. Jpn J Infect Dis 52:89–98. [PubMed] [Google Scholar]
- 195.Çelik T, Kaplan Y, Ataş E, Öztuna D, Berilgen S. 2013. Toxocara seroprevalence in patients with idiopathic Parkinson's disease: chance association or coincidence? Biomed Res Int 2013:685196. doi: 10.1155/2013/685196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Sun Y, Lee HJ, Yang SC, Chen TF, Lin KN, Lin CC, Wang PN, Tang LY, Chiu MJ. 2014. A nationwide survey of mild cognitive impairment and dementia, including very mild dementia, in Taiwan. PLoS One 9:e100303. doi: 10.1371/journal.pone.0100303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Bundy DA, Kremer M, Bleakley H, Jukes MC, Miguel E. 2009. Deworming and development: asking the right questions, asking the questions right. PLoS Negl Trop Dis 3:e362. doi: 10.1371/journal.pntd.0000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Cox DM, Holland CV. 1998. The relationship between numbers of larvae recovered from the brain of Toxocara canis-infected mice and social behaviour and anxiety in the host. Parasitology 116:579–594. doi: 10.1017/S0031182098002649. [DOI] [PubMed] [Google Scholar]
- 199.Holland CV, Cox DM. 2001. Toxocara in the mouse: a model for parasite-altered host behaviour? J Helminthol 75:125–135. doi: 10.1079/JOH200169. [DOI] [PubMed] [Google Scholar]
- 200.Hamilton CM, Brandes S, Holland CV, Pinelli E. 2008. Cytokine expression in the brains of Toxocara canis-infected mice. Parasite Immunol 30:181–185. doi: 10.1111/j.1365-3024.2007.01002.x. [DOI] [PubMed] [Google Scholar]
- 201.González H, Elgueta D, Montoya A, Pacheco R. 2014. Neuroimmune regulation of microglial activity involved in neuroinflammation and neurodegenerative diseases. J Neuroimmunol 274:1–13. doi: 10.1016/j.jneuroim.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 202.Pinelli E, Brandes S, Dormans J, Fonville M, Hamilton CM, der Giessen JV. 2007. Toxocara canis: effect of inoculum size on pulmonary pathology and cytokine expression in BALB/c mice. Exp Parasitol 115:76–82. doi: 10.1016/j.exppara.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 203.Lacerda-Queiroz N, Rodrigues DH, Vilela MC, Miranda AS, Amaral DC, Camargos ER, Carvalho LJ, Howe CL, Teixeira MM, Teixeira AL. 2010. Inflammatory changes in the central nervous system are associated with behavioral impairment in Plasmodium berghei (strain ANKA)-infected mice. Exp Parasitol 125:271–278. doi: 10.1016/j.exppara.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Quan N, He Lai LW. 2003. Intraventricular infusion of antagonists of IL-1 and TNF alpha attenuates neurodegeneration induced by the infection of Trypanosoma brucei. J Neuroimmunol 138:92–98. doi: 10.1016/S0165-5728(03)00122-X. [DOI] [PubMed] [Google Scholar]
- 205.Aviles H, Stiles J, O'Donnell P, Orshal J, Leid J, Sonnenfeld G, Monroy F. 2008. Kinetics of systemic cytokine and brain chemokine gene expression in murine toxoplasma infection. J Parasitol 94:1282–1288. doi: 10.1645/GE-1309.1. [DOI] [PubMed] [Google Scholar]
- 206.Gundra UM, Mishra BB, Wong K, Teale JM. 2011. Increased disease severity of parasite-infected TLR2−/− mice is correlated with decreased central nervous system inflammation and reduced numbers of cells with alternatively activated macrophage phenotypes in a murine model of neurocysticercosis. Infect Immun 79:2586–2596. doi: 10.1128/IAI.00920-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Dantzer R, O'Connor JC, Freund GG, Johnson RW, Kelley KW. 2008. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Liao CW, Cho WL, Kao TC, Su KE, Lin YH, Fan CK. 2008. Blood-brain barrier impairment with enhanced SP, NK-1R, GFAP and claudin-5 expressions in experimental cerebral toxocariasis. Parasite Immunol 30:525–534. doi: 10.1111/j.1365-3024.2008.01048.x. [DOI] [PubMed] [Google Scholar]
- 209.Fan CK, Chung WC, Su KE, Tsai YJ. 1998. Larval distribution in different organs of ICR strain mice infected with Toxocara canis. Kaohsiung J Med Sci 14:315–320. [PubMed] [Google Scholar]
- 210.Wang H, Saunders AJ. 2014. The role of ubiquitin-proteasome in the metabolism of amyloid precursor protein (APP): implications for novel therapeutic strategies for Alzheimer's disease. Discov Med 18:41–50. [PubMed] [Google Scholar]
- 211.Taylor JP, Hardy J, Fischbeck KH. 2002. Toxic proteins in neurodegenerative disease. Science 296:1991–1995. doi: 10.1126/science.1067122. [DOI] [PubMed] [Google Scholar]
- 212.Cook C, Stankowski JN, Carlomagno Y, Stetler C, Petrucelli L. 2014. Acetylation: a new key to unlock tau's role in neurodegeneration. Alzheimers Res Ther 6:29. doi: 10.1186/alzrt259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Martinez-Canabal A, Wheeler AL, Sarkis D, Lerch JP, Lu WY, Buckwalter MS, Wyss-Coray T, Josselyn SA, Frankland PW. 2013. Chronic over-expression of TGFβ1 alters hippocampal structure and causes learning deficits. Hippocampus 23:1198–1211. doi: 10.1002/hipo.22159. [DOI] [PubMed] [Google Scholar]
- 214.Mori T, Koyama N, Arendash GW, Horikoshi-Sakuraba Y, Tan J, Town T. 2010. Over-expression of human S100B exacerbates cerebral amyloidosis and gliosis in the Tg2576 mouse model of Alzheimer's disease. Glia 58:300–314. doi: 10.1002/glia.20924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Korolainen MA, Auriola S, Nyman TA, Alafuzoff I, Pirttila T. 2005. Proteomic analysis of glial fibrillary acidic protein in Alzheimer's disease and aging brain. Neurobiol Dis 20:858–870. doi: 10.1016/j.nbd.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 216.Liu Q, Xie F, Siedlak SL, Nunomura A, Honda K, Moreira PI, Zhua X, Smith MA, Perry G. 2004. Neurofilament proteins in neurodegenerative diseases. Cell Mol Life Sci 61:3057–3075. doi: 10.1007/s00018-004-4268-8. [DOI] [PubMed] [Google Scholar]
- 217.Lesort M, Tucholski J, Miller ML, Johnson GV. 2000. Tissue transglutaminase: a possible role in neurodegenerative diseases. Prog Neurobiol 61:439–463. doi: 10.1016/S0301-0082(99)00052-0. [DOI] [PubMed] [Google Scholar]
- 218.Zetterberg H, Andreasen N, Blennow K. 2004. Increased cerebrospinal fluid levels of transforming growth factor-beta1 in Alzheimer's disease. Neurosci Lett 367:194–196. doi: 10.1016/j.neulet.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 219.Hoshino T, Suzuki K, Matsushima T, Yamakawa N, Suzuki T, Mizushima T. 2013. Suppression of Alzheimer's disease-related phenotypes by geranylgeranylacetone in mice. PLoS One 8:e76306. doi: 10.1371/journal.pone.0076306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Griffin WS. 2006. Inflammation and neurodegenerative diseases. Am J Clin Nutr 83:470S–474S. [DOI] [PubMed] [Google Scholar]
- 221.Krohn K, Rozovsky I, Wals P, Teter B, Anderson CP, Finch CE. 1999. Glial fibrillary acidic protein transcription responses to transforming growth factor-beta1 and interleukin-1beta are mediated by a nuclear factor-1-like site in the near-upstream promoter. J Neurochem 72:1353–1361. [DOI] [PubMed] [Google Scholar]
- 222.Rudrabhatla P, Jaffe H, Pant HC. 2011. Direct evidence of phosphorylated neuronal intermediate filament proteins in neurofibrillary tangles (NFTs): phosphoproteomics of Alzheimer's NFTs. FASEB J 25:3896–3905. doi: 10.1096/fj.11-181297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Bence NF, Sampat RM, Kopito RR. 2001. Impairment of the ubiquitin-proteasome system by protein aggregation. Science 292:1552–1555. doi: 10.1126/science.292.5521.1552. [DOI] [PubMed] [Google Scholar]
- 224.Gu L, Guo Z. 2013. Alzheimer's Aβ42 and Aβ40 peptides form interlaced amyloid fibrils. J Neurochem 126:305–311. doi: 10.1111/jnc.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Mori H, Kondo J, lhara Y. 1987. Ubiquitin is a component of paired helical filaments in Alzheimer's disease. Science 235:1641–1644. doi: 10.1126/science.3029875. [DOI] [PubMed] [Google Scholar]
- 226.Wang GP, Khatoon S, Iqbal K, Grundke-Iqbal I. 1991. Brain ubiquitin is markedly elevated in Alzheimer disease. Brain Res 566:146–151. doi: 10.1016/0006-8993(91)91692-T. [DOI] [PubMed] [Google Scholar]
- 227.Glickman LS, Summers BA. 1983. Experimental Toxocara canis infection in cynomolgus macaques (Macaca fascicularis). Am J Vet Res 44:2347–2354. [PubMed] [Google Scholar]
- 228.Bardon R, Cuellar C, Guillen JL. 1994. Larval distribution of Toxocara canis in BALB/c mice at nine weeks and one year post-inoculation. J Helminthol 68:359–360. doi: 10.1017/S0022149X00001644. [DOI] [PubMed] [Google Scholar]
- 229.Gosselet F, Saint-Pol J, Candela P, Fenart L. 2013. Amyloid-β peptides, Alzheimer's disease and the blood-brain barrier. Curr Alzheimer Res 10:1015–1033. doi: 10.2174/15672050113106660174. [DOI] [PubMed] [Google Scholar]
- 230.Hamidou MA, Fradet G, Kadi AM, Robin A, Moreau A, Magnaval JF. 2002. Systemic vasculitis with lymphocytic temporal arteritis and Toxocara canis infection. Arch Intern Med 162:1521–1524. doi: 10.1001/archinte.162.13.1521. [DOI] [PubMed] [Google Scholar]
- 231.Helbok R, Brenneis C, Engelhardt K, Beer R, Lackner P, Brössner G, Pfausler B, Schmutzhard E. 2007. A rare case of Toxocara canis cerebral vasculitis. Eur J Neurol 14:e49. doi: 10.1111/j.1468-1331.2006.01564.x. [DOI] [PubMed] [Google Scholar]
- 232.Gould IM, Newell S, Green SH, George RH. 1985. Toxocariasis and eosinophilic meningitis. Br Med J 291:1239–1240. doi: 10.1136/bmj.291.6504.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Barra LA, dos Santos WF, Chieffi PP, Bedaque EA, Salles PS, Capitão CG, Vianna S, Hanna R, Pedretti L Jr. 1996. Visceral larva migrans: a mixed form of presentation in an adult. The clinical and laboratory aspects. Rev Soc Bras Med Trop 29:373–376. doi: 10.1590/S0037-86821996000400011. [DOI] [PubMed] [Google Scholar]
- 234.Moreira-Silva SF, Rodrigues MG, Pimenta JL, Gomes CP, Freire LH, Pereira FE. 2004. Toxocariasis of the central nervous system: with report of two cases. Rev Soc Bras Med Trop 37:169–174. doi: 10.1590/S0037-86822004000200011. [DOI] [PubMed] [Google Scholar]
- 235.Mrissa R, Battikh R, Ben Abdelhafidh N, Jemli B, Azzouz O, Zaouali J, Louzir B, M'sadek F, Ben Abdallah N, Gargouri S, Yedeas M, Othmani S. 2005. Toxocara canis encephalitis: case report. Rev Med Interne 26:829–832. doi: 10.1016/j.revmed.2005.04.025. [DOI] [PubMed] [Google Scholar]
- 236.Keller M, Pavia AT, Byington CL. 2008. Possible intrafamilial transmission of Toxocara causing eosinophilic meningitis in an infant. Pediatr Infect Dis J 27:849–850. doi: 10.1097/INF.0b013e3181719bd1. [DOI] [PubMed] [Google Scholar]
- 237.Villano M, Cerillo A, Narciso N, Vizioli L, Del Basso De Caro M. 1992. A rare case of Toxocara canis arachnoidea. J Neurosurg Sci 36:67–69. [PubMed] [Google Scholar]
- 238.Robinson A, Tannier C, Magnaval JF. 2002. Toxocara canis meningoradiculitis. Rev Neurol 158:351–353. [PubMed] [Google Scholar]
- 239.Kazek B, Jamroz E, Mandera M, Bierzyńska-Macyszyn G, Kluczewska E, Marszał E. 2006. The cerebral form of toxocarosis in a seven-year-old patient. Folia Neuropathol 44:72–76. [PubMed] [Google Scholar]
- 240.Duprez TPJ, Bigaignon G, Delgrange E, Desfontaines P, Hermans M, Vervoort T, Sindic CJM, Buysschaert M. 1996. MRI of cervical cord lesions and their resolution in Toxocara canis myelopathy. Neuroradiology 38:792–795. doi: 10.1007/s002340050350. [DOI] [PubMed] [Google Scholar]
- 241.Dauriac-Le Masson V, Chochon F, Demeret S, Pierrot-Deseilligny C. 2005. Toxocara canis meningomyelitis. J Neurol 252:1267–1268. doi: 10.1007/s00415-005-0688-0. [DOI] [PubMed] [Google Scholar]
- 242.Finsterer J, Kallab V, Auer H. 2010. Neurotoxocariasis associated with lower motor neuron disease. Report of one case. Neuro Rev Med Chil 138:483–486. [PubMed] [Google Scholar]
- 243.Marx C, Lin J, Masruha MR, Rodrigues MG, da Rocha AJ, Vilanova LC, Gabbai AA. 2007. Toxocariasis of the CNS simulating acute disseminated encephalomyelitis. Neurology 69:806–807. doi: 10.1212/01.wnl.0000267664.53595.75. [DOI] [PubMed] [Google Scholar]
- 244.Moiyadi A, Mahadevan A, Anandh B, Shivashankar RS, Chickabasavaiah YT, Shankar SK. 2007. Visceral larva migrans presenting as multiple intracranial and intraspinal abscesses. Neuropathology 27:371–374. doi: 10.1111/j.1440-1789.2007.00775.x. [DOI] [PubMed] [Google Scholar]