Abstract
Aim:
To study the health-care needs of the patients with severe mental disorders as perceived by their family caregivers and the treating psychiatrists.
Materials and Methods:
Caregivers of patients with severe mental disorders and their treating psychiatrists were assessed using Camberwell Assessment of Need-Research Version (CAN-R) scale and indigenously designed Supplementary Assessment of Needs Scale (SNAS).
Results:
The study included 1494 patients recruited from 15 centers. The mean needs as per the CAN-R, perceived by the caregivers were 7.8 and treating psychiatrists were 8.1. About one-third of needs were unmet. On SNAS, both caregivers and treating psychiatrists reported a mean of 7.9 needs, of which more than half were unmet as per the caregivers. As per the treating psychiatrists, 45.5% of the needs as assessed on SNAS were unmet. There was a high level of correlation between needs perceived by the patients, caregivers and the treating psychiatrists. On CAN-R, main domains of needs as reported by the caregivers were those of money, relief of psychological distress, information about the illness and treatment, welfare benefits, transport, company and food. As per the treating psychiatrists, the most common total needs identified were those of relief of psychological distress, welfare benefits, information about the illness and treatment, money, transport, company self-care and physical health. The most common domains of needs as assessed on SNAS as per the caregivers were those of free treatment, medical reimbursement, psychoeducation, financial help, social support, insurance, more time from the clinicians and travel concession. The treating psychiatrists identified dealing with caregiver's stress as the most common need.
Conclusions:
According to the family caregivers and treating psychiatrists, about one-third of the needs of the patients as assessed using CAN-R and about half of the needs as assessed using SNAS are unmet.
Keywords: Caregivers, needs, outcome, psychiatrists, severe mental disorders
INTRODUCTION
In India, most patients with psychiatric disorders are treated on an outpatient basis. The psychiatric care mostly involves addressing the acute symptoms, and there is little emphasis on the rehabilitation of the patients with disabilities.
Due to various cultural reasons, family takes major responsibility for the care of the patient. When a patient is acutely ill, family members take on the responsibilities of the work being carried out by the patient. Additionally, the family members take the responsibility of supervising the medications, making the treatment decisions like whom to consult, what medications to take, bringing the patient to the hospital and re-integrating the patient in the society. In the absence of the day care and rehabilitation facilities, family tries to accommodate the patient in traditional family professions. Therefore, the family members form an integral part of the treatment of patients with mental illnesses. Family is also a major source of support information.
Many studies across the world have assessed the needs of patients with severe mental disorders.[1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16] Most of these studies have evaluated the “needs” of patients with schizophrenia.[1,2,3,4,5,6,7,8,9,10,11,12,13,14] However, these studies have mainly focused on the needs of the patients from their own perspective. Very fewer studies have focused on the needs from the perspective of other staff providing health-care or the mental health professionals. In the studies that have assessed the needs from both the patients and the staff, there is no consistent pattern. Staff reported more needs than the patients in some studies[1,2] while in others patients reported more needs than the staff.[5] In these studies, however, there was no difference in the number of met needs reported by the staff and the patients.[1,2,5] A previous study from India evaluated the needs of patients with schizophrenia from the family members too and reported good correlation of needs of patients as perceived by patients themselves and their caregivers.[17] However, none of the studies from India have evaluated the needs of the patients with severe mental disorders from the perspective of mental health professionals.
Accordingly the aim of this study was to assess the health-care needs of the patients with serious mental illnesses as perceived by their family members and the mental health professionals through a multi-site study.
MATERIALS AND METHODS
This Indian Psychiatric Society (IPS) funded multicentric study followed a cross-sectional design in which participants (patients and their primary caregivers) were assessed only once. During the same time, treating mental health professionals also completed their own assessment of health-care needs of the patients as perceived by them. Details of the methodology of the study have been described in another paper wherein data of needs of the patients with severe mental disorder is reported. Those interested in the details of the methodology can refer to the previous paper.[18]
The study was approved by the IPS Ethical Review Board and/or by the local Institutional Ethics Committees. Participants were recruited after obtaining written informed consent. The study included remitted and clinically stable patients with one of the following mental disorders: Schizophrenia or other psychotic disorders, bipolar disorder, recurrent depressive disorder, major depressive disorder or obsessive compulsive disorder (OCD) as per Diagnostic and Statistical Manual of Mental Disorders-IV Edition criteria.[19]
Needs were assessed using Camberwell Assessment of Need-Research version (CAN-R). Besides CAN-R, needs of the patients were assessed using Supplementary Assessment of Need Scale (SNAS) Questionnaire.[20] The time frame for assessment of needs on both the scales was past 1 month. Besides these instruments, patients were also rated on Global Assessment of Functioning Scale (GAF) and residual psychopathology using appropriate scales.[21]
Statistical Package for the Social Sciences version 14 (SPSS version 14; Chicago, IL, USA) was used to analyze the data. For the continuous variables, means and standard deviations with a range were calculated. Frequencies and percentages were calculated for ordinal or nominal variables. Chi-square test, t-test, Mann–Whitney U-test and analysis of variance with post hoc analysis using Scheffe's test were used for comparison. Pearson's correlation coefficient and Spearman's rank correlation coefficient were used to study the association of needs with sociodemographic and clinical variables. In view of multiple correlations and comparisons, only P ≤ 0.01 was considered as significant.
RESULTS
The study included 1494 patients recruited across the 15 centers.
Sociodemographic profile
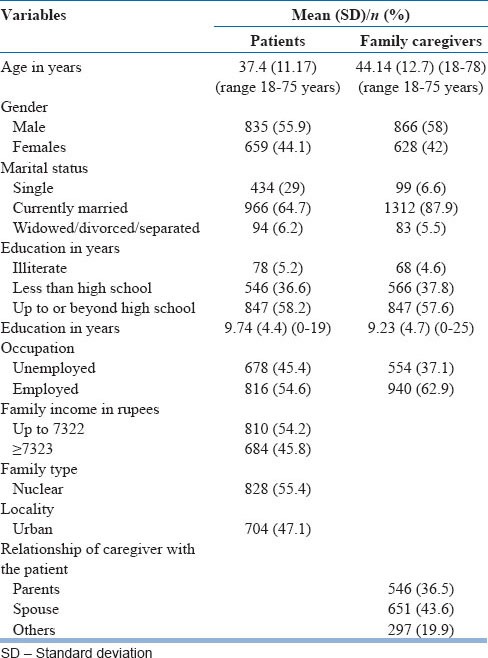
Table 1 shows the sociodemographic profile of the patients and their caregivers. The mean age of the caregivers was more than the patients. In terms of the relationship of caregivers with the patients, most of the caregivers were either the spouse or the parents of patients.
Table 1.
Sociodemographic profile of patients and the family caregivers (n=1494)
Clinical profile
Patients with affective disorders (n = 826; 55.3%) outnumbered patients with psychotic disorders (n = 561; 37.6%). Patients with OCD formed a small group (n = 107; 7.2%).
Needs of the patients as assessed reported by the family caregivers and the treating psychiatrist) are shown in Tables 2 and 3.
Table 2.
Health-care needs as per CAN-R
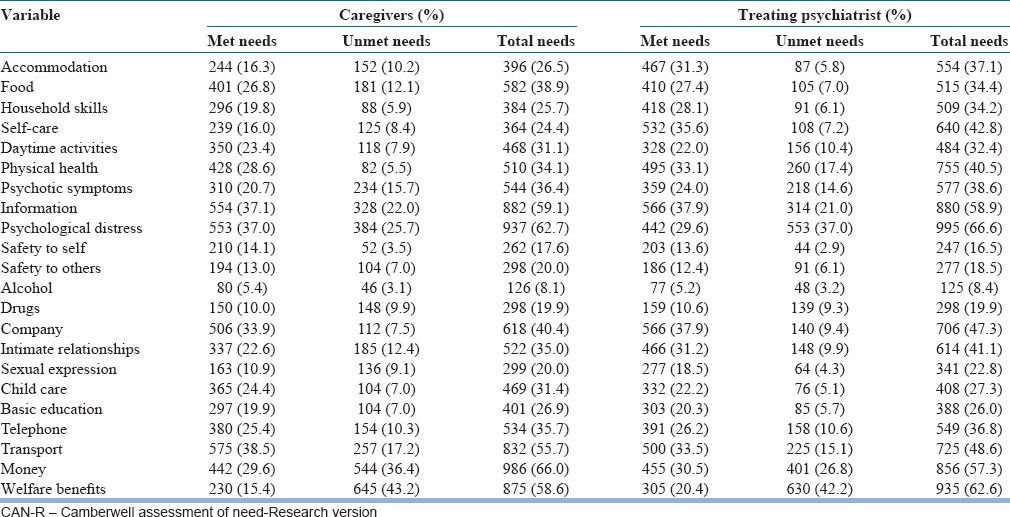
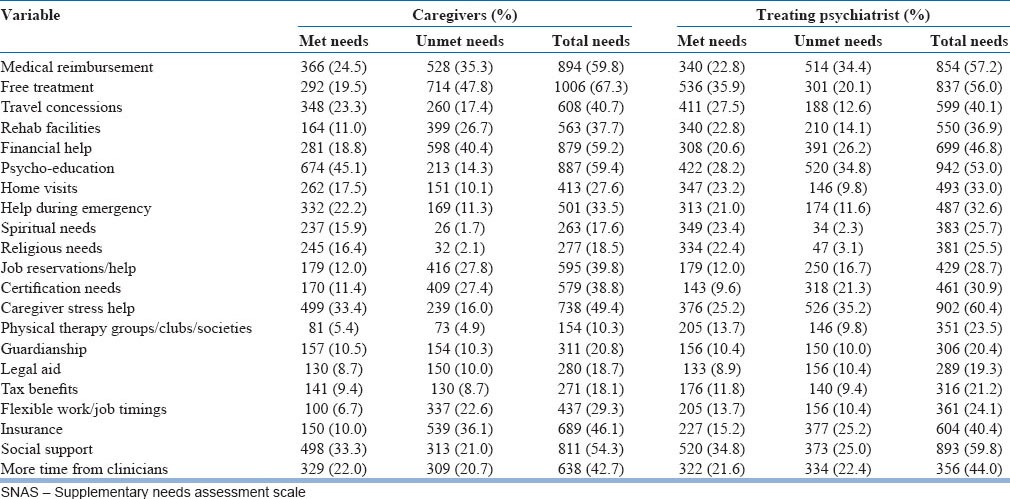
Table 3.
Health-care needs as per SNAS
Needs as per Camberwell Assessment of Need
As per the caregivers of patients with mental disorders, the most commonly reported needs were in the area of money (66%), relief of psychological distress (62.7%), information about the illness and treatment (59.1%), welfare benefits (58.6%), transport (55.7%) company (40.4%), food (38.9%), relief from psychotic symptoms (36.4%) and telephone. In terms of met needs, most commonly reported met needs by the caregivers were those of transport, information about illness and treatment, relief from psychological distress, company, physical health and food. The commonly reported unmet needs were those of welfare benefits, money, relief of psychological distress, information about the illness and treatment, transport, food and intimate relationships.
As per the mental health professionals, the most common total needs identified were those of relief of psychological distress (66.6%), welfare benefits (62.6%), information about the illness and treatment (58.9%), money (57.3%), transport (48.6%), company (47.3%), self-care (42.8%) and physical health (42.8%). The commonly identified areas of met needs by the mental health professionals were those of information about the illness, company, self-care, transport, physical health, intimate relationship and accommodation. In terms of unmet needs, the commonly identified areas included those of welfare benefits, relief of psychological distress, money, information about the illness and treatment, physical health and money.
Needs as per Supplementary Assessment of Needs Scale
The most commonly identified needs by the caregivers of patients were free treatment (67.3%), medical reimbursement (59.8%), psychoeducation (59.4%), financial help (59.2%), social support (54.3%), insurance (46.1%), more time from the clinicians (42.7%) and travel concession (40.7%). Commonly reported met needs were in the area of psychoeducation, dealing with caregiver stress, social support, medical reimbursement, travel concession, help during emergency and more time from clinicians. Majority of the unmet needs were identified in the area of free treatment, financial help, insurance, medical reimbursement, job reservation/help, certification, rehabilitation facilities and flexible work/job timings.
The treating psychiatrists identified dealing with caregiver's stress (60.4%) as the most common need. Other common needs identified by the treating psychiatrists were in the area of social support (59.8%), medical reimbursement (57.2%), free treatment (56%), psychoeducation (53%), financial help (46.8%), more time from clinicians (44%) and flexible work/job timing (40.4%). The most commonly identified met needs were those of free treatment, social support, psychoeducation, travel concession, dealing with caregiver's stress, spiritual needs, religious needs and more time from the clinicians. The commonly identified areas of unmet needs were those of dealing caregiver's stress, psychoeducation, medical reimbursement, financial help, insurance, social support, more time from clinicians and certification.
Total needs as per Camberwell Assessment of Need and Supplementary Assessment of Needs Scale
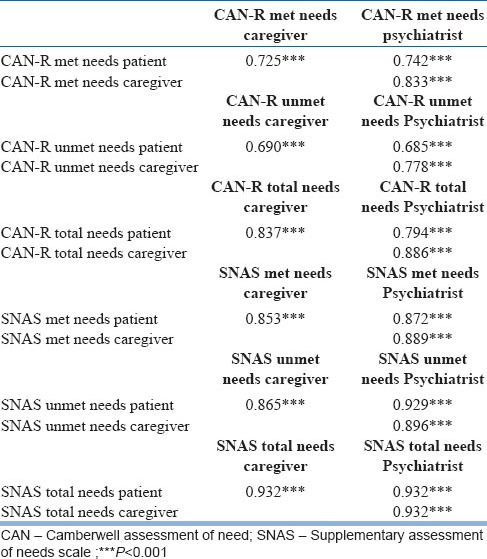
As shown in Table 4, the mean number of needs on CAN-R identified by patients, caregivers and treating psychiatrist varied from 7.6 to 8.3 with more needs reported by the treating psychiatrist. As assessed from the patients, caregivers and treating psychiatrist, about two-third of the needs were met, and one-third needs were unmet. On SNAS, the mean number of needs identified varied from 7.6 to 7.9 with 46% to 52% of needs remaining unmet. As assessed from patients and clinicians, the percentage of met needs exceeded unmet needs; however as per caregivers unmet needs exceeded the met needs. Further, as it is evident from Table 5, there was a high level of correlation between the mean number of needs reported by patients, caregivers and treating psychiatrist.
Table 4.
Mean number of needs as reported by patients, caregivers and professionals
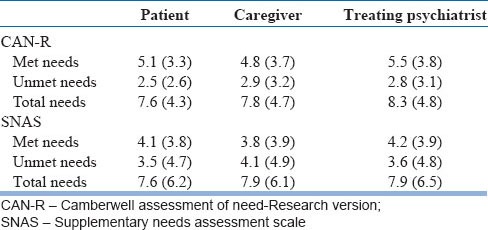
Table 5.
Correlation between the mean number of needs as reported by patients, caregivers and professionals
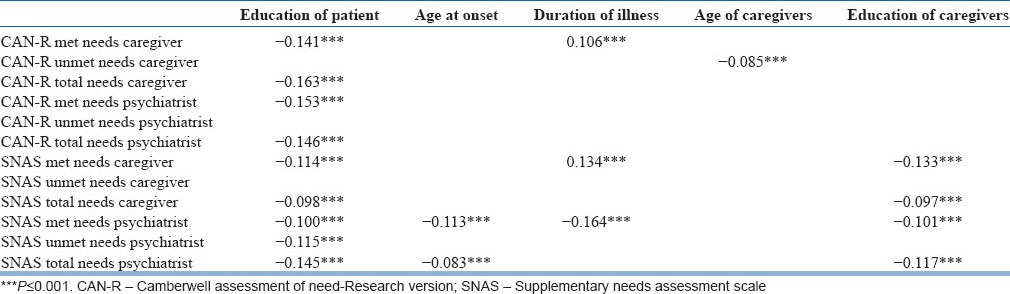
Sociodemographic and clinical factors associated with needs
As shown in Table 6, maximum numbers of correlations were seen between the needs and the education in years of the patient and the needs as perceived by caregivers. Those caregivers having lower level of education reported higher number of needs. Some correlations were also seen between needs and age of onset, duration of illness and age of the caregivers. No correlation was seen between the age of patient and the needs.
Table 6.
Association of sociodemographic variables with needs
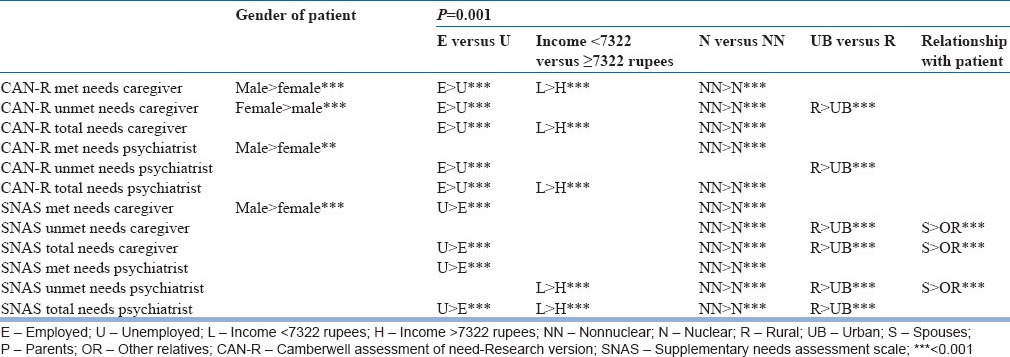
As per the caregivers and treating psychiatrist, males had more met needs [Table 7]. Additionally, caregivers as per the CAN-R reported significantly higher number of unmet needs for females. Those patients who were employed had more needs as per CAN-R but more unmet needs as per SNAS as per both, caregivers and the treating psychiatrists. Greater number of needs was reported for patients from lower family income, from nonnuclear families and rural background by both the caregivers as well as the psychiatrists. On SNAS, when the accompanying relative was a spouse, higher unmet and total needs were reported by the caregivers. Similarly, treating psychiatrist too reported higher unmet needs when the accompanying relative was a spouse.
Table 7.
Association of categorical sociodemographic variables with needs
Association of psychopathology and needs [Table 8]
Table 8.
Association of psychopathology with needs
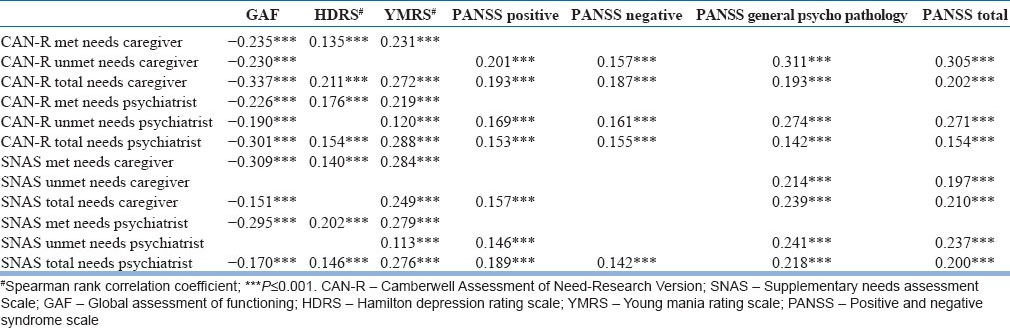
Both family caregivers and treating psychiatrist reported association of higher level of functioning as assessed by GAF and the lower number of needs as assessed on CAN-R and SNAS. In the affective disorder group, higher level of residual psychopathology was associated with more needs. In the psychotic group, higher level of residual psychopathology was associated with more unmet and total needs. There was no relationship of Yale Brown Obsessive Compulsive Scale score with needs.
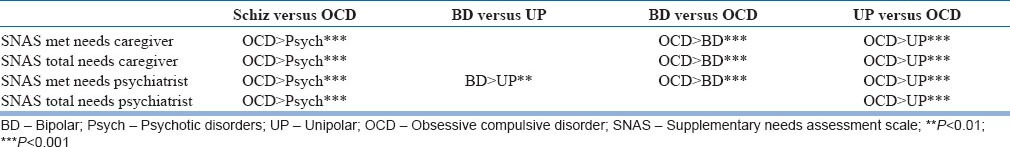
Comparison of needs across different diagnostic groups
When the mean number of needs as per the caregivers and psychiatrists were compared across the different broad diagnostic groups, no significant differences emerged on the number of needs on CAN-R. No significant difference was seen on CAN-R when the psychotic disorder, bipolar disorder, unipolar disorder and OCD groups were compared with each other. On SNAS, there was no difference between the needs of patients with schizophrenia and bipolar disorder as perceived by their caregivers and treating psychiatrist. In general, caregivers of patients of OCD and their treating psychiatrist reported higher number of needs on SNAS compared to patients of schizophrenia, bipolar disorder and unipolar disorder. Details of the results are shown in Table 9.
Table 9.
Comparison of needs across different diagnostic groups
DISCUSSION
This multicentric study evaluated the needs of 1494 patients as perceived by their caregivers and the treating psychiatrists.
Needs as per Camberwell Assessment of Need
In the present study, the mean number of needs on CAN-R identified by patients, caregivers and treating psychiatrists varied from 7.6 to 8.3. Of these about two-third of the needs were met, and one-third were unmet needs.
In the present study, psychiatrists identified somewhat higher number of needs as compared to the patients. Previous studies that have assessed the needs as per both the patients and the staff, have come up with inconsistent findings.[1,2,5] Our findings are in line with those studies that have reported higher number of needs identified by the staff.[1,2]
Studies from the West, which have assessed the needs from the staff have identified management of psychotic symptoms, company, daytime activities, house upkeep, food and information[1,2,22] to be the most commonly reported needs. However, the commonly reported needs as per psychiatrists in the present study were those of relief of psychological distress, welfare benefits, information about the illness and treatment, money, transport, company, self-care and physical health. These differences are possibly due to the kind of services provided to the patients. In the present study, majority of the patients were recruited from the medical college setups where usually the outpatients are overcrowded, and there is poor doctor-patient ratio. Resultantly there is poor time allocation to address the psychological needs of the patients and provide adequate information about the illness. Welfare benefits being the common area of need reflects the lack of provision of rehabilitation services and social security.
Only two previous studies from India using CAN-R have assessed needs as perceived by the caregivers. Both demonstrated that patients report a higher number of needs when compared to caregivers.[17,20] In the present study, the number of needs reported by the patients and the caregivers were comparable.
Studies reporting on the needs of patients with schizophrenia and bipolar disorder as per their caregivers have documented perceived needs in the areas of welfare benefits, information about the condition, psychological distress, money, company, daytime activities, physical health and intimate relationships.[17,20] The present study supports the profile of needs reported by the caregivers in these earlier studies conducted in India. In the index study, as per the caregivers the most commonly reported needs were in the area of money, relief of psychological distress, information about the illness and treatment, welfare benefits, transport and company. In terms of met needs, most commonly reported met needs by the caregivers were those of transport, information about illness and treatment, relief from psychological distress and physical health. The commonly reported unmet needs were those of welfare benefits, money, relief of psychological distress and information about the illness and treatment.
In the present study, there was a high level of correlation between the needs as reported by the patients, caregivers and the mental health professionals. Previous studies, which have assessed the needs as per the patients, the staff and caregivers have reported good level of agreement between rating of patients and the staff[1,2,5] and that between caregivers/relatives and the patients.[17] Thus, it can be said that caregivers are an importance source of information about the needs of their patients and they must be regarded as a reliable partner in the management of patients with severe mental disorders. Further, while formulating any policies and laws related to patients with severe mental disorders, caregivers must be considered as important stake holders, and their concerns must also be taken into account.
Needs as per Supplementary Needs Assessment Scale
Findings of the present study suggest that there is a lot of similarity in the needs identified by the patients, caregivers and treating psychiatrists. On SNAS, both caregivers and treating psychiatrists reported a mean of 7.9 needs, of which more than half were unmet as per the caregivers. Slightly less than half (45.5%) of the needs as assessed by clinicians were unmet. The common areas of needs include financial help, medical reimbursement, psychoeducation, free treatment, certification of mental illness, flexible work/job timings, addressing the caregiver stress, social support, insurance, more time from the clinicians and travel concession. These findings amplify the deficiencies in the state of health-care services available in India. The governmental scheme and policies must address the unmet needs of the patients. Like in many Western countries, there is a need for providing free treatment. There is a need for development of policies for reservation for jobs and flexibility in job timings, to help the patients re-integrate with the society. Further, these findings suggest that although there are certain government schemes to address some of the unmet needs of the patients, yet there is lack of knowledge about the same or there are difficulties in availing the same. Accordingly, information about government schemes like travel concession and certification must be widely advertised and the procedures to avail these facilities must be simplified.
In a country like India, where there is lack of adequate organized health-care system and social security schemes coupled with overburdened health care system, family caregivers of patients with mental illnesses are doing a great service to the patient, society at large and even to the government. In the absence of the family caregivers, patients with mental health problems can become a major burden on the state. Since the caregivers put in unlimited number of hours in caring for their mentally sick members of family, there is a need to evolve government policies that can at least provide travel benefits and extra leaves to the caregivers. Developing a network of day care centers and rehabilitation centers can help in providing some respite from the caregiving responsibility and resultantly may result in a reduction of the caregiver distress.
It is a well-known fact that there is a severe shortage of mental health professionals in this country. To address the unmet treatment needs like those of psychoeducation, and more time from the professionals, increase in the number of mental health training facilities is urgently required in this country to address the acute shortage of staff.
Correlates of needs
This study suggests the association of the higher number of needs with lower educational level of the patients and the caregivers, lower family incomes and being from the rural background. Taken together, these three variables indicate social disadvantage for the patients with mental illnesses. Spouses of the patients reported higher number of unmet and total needs of the patients compared to the other relatives. Many hypotheses can explain this association. First, because of their close association with the patient, spouses are better able to identify all the possible unmet needs of patients. Second, spouses end up taking the caregiver role, particularly when the patient belongs to a nuclear family set-up or when other relatives are not readily available. More commonly, the spouse has to play the role of caregiver and also that of the breadwinner. Resultantly, they are not able to fulfill many needs of patients. Thus, patients are left with more of unmet and total needs.
In terms of clinical variables, higher age of onset was associated with a lower number of met and total needs as per the psychiatrists. Longer duration of illness was associated with a higher number of met needs as per the caregivers, whereas the psychiatrists reported negative correlation between duration of illness and number of met needs as assessed on SANS. May be that in the initial part of the illness, all the attention is focused on the symptom amelioration and family is more worried about the symptom relief. However, as the illness becomes chronic, the focus is not only on the treatment related needs, but also on the social and emotional needs, and caregivers try to fulfill these. Accordingly longer duration of illness is associated with more met needs.
Better functioning of the patients was associated with a lower number of met, unmet and total needs, both as per the family caregivers and treating psychiatrists. Presence of residual psychopathology in patients with schizophrenia was associated with a higher number of unmet and total needs of the patients. Similar associations were also seen in patients with affective disorders. Thus, adequate symptom control should be given paramount importance in the management of patients with severe mental disorders. The relationship of level of functioning and number of needs indicates that meeting the needs of patients can improve the level of functioning or vice versa.
Limitations of the study
This study was limited to the patients attending the mental health services. They may not truly reflect the needs of the patients with severe mental disorders in the community. This study followed a cross-sectional design, assessed patients in remission and who were clinically stable and free of comorbid disorders. However, many patients with severe mental disorders do not achieve remission, continue to remain clinically unstable and present with comorbidities. Therefore, the findings of this study cannot be generalized to all patients. Attempt must be made to overcome these limitations by designing studies assessing the needs of the patients, living in the community at multiple time points.
Implications of the study
This study demonstrates that there is a high level of correlation between the needs of the patients as perceived by patients themselves, their family caregivers and the treating psychiatrists. Further, this study suggests that the majority of the unmet needs are in the social, emotional and treatment related areas.
Taking this into account, it can be concluded that caregivers are an importance source of information about the needs of their patients. Hence, their concerns about their patients must be addressed. Further, at the level of formulation of any policies and laws related to patients with severe mental disorders, government and other agencies must consider caregivers as important stake holders in the management of the patients with severe mental disorders. Government should also come up with clear policies for the family caregivers of the patients with mental illness who devote a significant proportion of their time and resources in caring for the ill members of the family. In terms of service orientation, there is a need to have rehabilitation facilities to help patients learn skills to function independently.
ACKNOWLEDGMENTS
We are thankful to Prof. Subho Chakrabarti for allowing us to use the SNAS.
Footnotes
Source of Support: Indian Psychiatric Society (Funded amount-3.04 lakhs)
Conflict of Interest: None declared
REFERENCES
- 1.Ochoa S, Haro JM, Usall J, Autonell J, Vicens E, Asensio F, et al. Needs and its relation to symptom dimensions in a sample of outpatients with schizophrenia. Schizophr Res. 2005;75:129–34. doi: 10.1016/j.schres.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Ochoa S, Haro JM, Autonell J, Pendàs A, Teba F, Màrquez M, NEDES Group Met and unmet needs of schizophrenia patients in a Spanish sample. Schizophr Bull. 2003;29:201–10. doi: 10.1093/oxfordjournals.schbul.a006998. [DOI] [PubMed] [Google Scholar]
- 3.Wiersma D, Nienhuis FJ, Giel R, Slooff CJ. Stability and change in needs of patients with schizophrenic disorders: A 15 -and 17-year follow-up from first onset of psychosis, and a comparison between ‘objective’ and ‘subjective’ assessments of needs for care. Soc Psychiatry Psychiatr Epidemiol. 1998;33:49–56. doi: 10.1007/s001270050022. [DOI] [PubMed] [Google Scholar]
- 4.Bengtsson-Tops A, Hansson L. Clinical and social needs of schizophrenic outpatients living in the community: The relationship between needs and subjective quality of life. Soc Psychiatry Psychiatr Epidemiol. 1999;34:513–8. doi: 10.1007/s001270050169. [DOI] [PubMed] [Google Scholar]
- 5.Slade M, Phelan M, Thornicroft G. A comparison of needs assessed by staff and by an epidemiologically representative sample of patients with psychosis. Psychol Med. 1998;28:543–50. doi: 10.1017/s0033291798006564. [DOI] [PubMed] [Google Scholar]
- 6.Foldemo A, Bogren L. Need assessment and quality of life in outpatients with schizophrenia: A 5-year follow-up study. Scand J Caring Sci. 2002;16:393–8. doi: 10.1046/j.1471-6712.2002.00107.x. [DOI] [PubMed] [Google Scholar]
- 7.Grinshpoon A, Ponizovsky AM. The relationships between need profiles, clinical symptoms, functioning and the well-being of inpatients with severe mental disorders. J Eval Clin Pract. 2008;14:218–25. doi: 10.1111/j.1365-2753.2007.00836.x. [DOI] [PubMed] [Google Scholar]
- 8.Slade M, Phelan M, Thornicroft G, Parkman S. The Camberwell Assessment of Need (CAN): Comparison of assessments by staff and patients of the needs of the severely mentally ill. Soc Psychiatry Psychiatr Epidemiol. 1996;31:109–13. doi: 10.1007/BF00785756. [DOI] [PubMed] [Google Scholar]
- 9.Slade M, Leese M, Cahill S, Thornicroft G, Kuipers E. Patient-rated mental health needs and quality of life improvement. Br J Psychiatry. 2005;187:256–61. doi: 10.1192/bjp.187.3.256. [DOI] [PubMed] [Google Scholar]
- 10.McNulty SV, Duncan L, Semple M, Jackson GA, Pelosi AJ. Care needs of elderly people with schizophrenia. Assessment of an epidemiologically defined cohort in Scotland. Br J Psychiatry. 2003;182:241–7. doi: 10.1192/bjp.182.3.241. [DOI] [PubMed] [Google Scholar]
- 11.Nakanishi M, Setoya Y, Kodaka M, Makino H, Nishimura A, Yamauchi K, et al. Symptom dimensions and needs of care among patients with schizophrenia in hospital and the community. Psychiatry Clin Neurosci. 2007;61:495–501. doi: 10.1111/j.1440-1819.2007.01698.x. [DOI] [PubMed] [Google Scholar]
- 12.Usall J, Haro JM, Ochoa S, Márquez M, Araya S, Needs of Patients with Schizophrenia group Influence of gender on social outcome in schizophrenia. Acta Psychiatr Scand. 2002;106:337–42. doi: 10.1034/j.1600-0447.2002.01351.x. [DOI] [PubMed] [Google Scholar]
- 13.Middelboe T, Mackeprang T, Hansson L, Werdelin G, Karlsson H, Bjarnason O, et al. The Nordic Study on schizophrenic patients living in the community. Subjective needs and perceived help. Eur Psychiatry. 2001;16:207–14. doi: 10.1016/s0924-9338(01)00566-1. [DOI] [PubMed] [Google Scholar]
- 14.McCrone P, Leese M, Thornicroft G, Schene A, Knudsen HC, Vázquez-Barquero JL, et al. A comparison of needs of patients with schizophrenia in five European countries: The EPSILON Study. Acta Psychiatr Scand. 2001;103:370–9. doi: 10.1034/j.1600-0447.2001.00207.x. [DOI] [PubMed] [Google Scholar]
- 15.Goossens PJ, Knoppert-van der Klein EA, Kroon H, van Achterberg T. Self-reported care needs of outpatients with a bipolar disorder in the Netherlands. J Psychiatr Ment Health Nurs. 2007;14:549–57. doi: 10.1111/j.1365-2850.2007.01127.x. [DOI] [PubMed] [Google Scholar]
- 16.Pollack LE. Informational needs of patients hospitalized for bipolar disorder. Psychiatr Serv. 1995;46:1191–4. doi: 10.1176/ps.46.11.1191. [DOI] [PubMed] [Google Scholar]
- 17.Kulhara P, Avasthi A, Grover S, Sharan P, Sharma P, Malhotra S, et al. Needs of Indian schizophrenia patients: An exploratory study from India. Soc Psychiatry Psychiatr Epidemiol. 2010;45:809–18. doi: 10.1007/s00127-009-0126-1. [DOI] [PubMed] [Google Scholar]
- 18.Grover S, Avasthi A, Shah S, Lakdawala B, Chakraborty K, Nebhinani N, et al. Indian Psychiatric Society multicentric study on assessment of health-care needs of patients with severe mental illnesses. Indian J Psychiatry. 2015;57:43–50. doi: 10.4103/0019-5545.148520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.4th ed. Washington, DC: American Psychiatric Association; 1994. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 20.Neogi R. Chandigarh: 2009. Health Care Needs of Euthymic patients with Bipolar disorder. MD Thesis, submitted to PGIMER. [Google Scholar]
- 21.Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–71. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- 22.Phelan M, Slade M, Thornicroft G, Dunn G, Holloway F, Wykes T, et al. The Camberwell Assessment of Need: The validity and reliability of an instrument to assess the needs of people with severe mental illness. Br J Psychiatry. 1995;167:589–95. doi: 10.1192/bjp.167.5.589. [DOI] [PubMed] [Google Scholar]


