Abstract
Intraductal papillary mucinous neoplasms (IPMNs) of the pancreas are neoplasms that are characterized by ductal dilation, intraductal papillary growth, and thick mucus secretion. This relatively recently defined pathology is evolving in terms of its etiopathogenesis, clinical features, diagnosis, management, and treatment guidelines. A PubMed database search was performed. All the relevant abstracts in English language were reviewed and the articles in which cases of IPMN could be identified were further scrutinized. Information of IPMN was derived, and duplication of information in several articles and those with areas of persisting uncertainties were excluded. The recent consensus guidelines were examined. The reported incidence of malignancy varies from 57% to 92% in the main duct-IPMN (MD-IPMN) and from 6% to 46% in the branch duct-IPMN (BD-IPMN). The features of high-risk malignant lesions that raise concern include obstructive jaundice in a patient with a cystic lesion in the pancreatic head, the findings on radiological imaging of a mass lesion of >30 mm, enhanced solid component, and the main pancreatic duct (MPD) of size ≥10 mm; while duct size 5-9 mm and cyst size <3 mm are considered as “worrisome features.” Magnetic resonance imaging (MRI) and endoscopic ultrasound (EUS) are primary investigations in diagnosing and following up on these patients. The role of pancreatoscopy and the analysis of aspirated cystic fluid for cytology and DNA analysis is still to be established. In general, resection is recommended for most MD-IPMN, mixed variant, and symptomatic BD-IPMN. The 5-year survival of patients after surgical resection for noninvasive IPMN is reported to be at 77-100%, while for those with invasive carcinoma, it is significantly lower at 27-60%. The follow-up of these patients could vary from 6 months to 1 year and would depend on the risk stratification for invasive malignancy and the pathology of the resected specimen. The understanding of IPMN has evolved over the years. The recent guidelines have played a role in this regard.
Keywords: Carcinoma of pancreas, Cystic tumors of pancreas, Intraductal papillary mucinous neoplasm (IPMN), Magnetic resonance cholangiopancreatography (MRCP)
Introduction
Intraductal papillary mucinous neoplasm (IPMN) of the pancreas is characterized by papillary growths within the pancreatic ductal system with thick mucin secretion, and is at risk for undergoing malignant transformation.[1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29] The first few cases of IPMN were reported in 1970s and then in 1980s.[20,21] In 1990s, the term IPMN was coined and the tumor was established as a special entity among the pancreatic neoplasms.[22] The incidence of IPMN appears to have risen since the initial reports, but this may reflect the combined effects of new diagnostic techniques and the progress in recognition of the pathology, its classification, and the management of this disease.[1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66] Although most reports of IPMN were from Japan,[2,8,19] an increasing number of cases of IPMN of the pancreas have been reported in recent years from around the world.[1,3,4,5,6,7,9,10,11,12,13,14,15,16,17,18] IPMN is characterized by cystic dilatation of the main and/or branches of the main pancreatic duct (MPD).[2,3,4,5,9,10,13,16] The disease originates from the epithelium of the pancreatic duct and the latest evidence suggests that if untreated, IPMN will follow the dysplasia-carcinoma sequence undergoing malignant transformation.[2,4,13,28] The World Health Organization has classified cystic mucin-producing neoplasms of the pancreas into two distinct entities: IPMN and mucinous cystic neoplasms (MCNs).[23] IPMN, which in the past was classified into four categories based on the degree of epithelial dysplasia (adenoma, borderline, carcinoma in situ, and invasive carcinoma), is presently classified as low-grade dysplasia (adenoma), intermediate-grade dysplasia (borderline), and high-grade dysplasia (carcinoma in situ).[27] It occurs mainly in the sixth and seventh decades of life, affecting males slightly more frequently than females.[3,13] The incidence of IPMN is reported to be approximately one-thirtieth to that of typical ductal adenocarcinoma and accounts for 0.5% of all the pancreatic neoplasms found at autopsy, 7.5% of the clinically diagnosed pancreatic neoplasms, 16.3-25% of the surgically resected pancreatic neoplasms, and 50% of the incidentally detected pancreatic cysts.[2,3,4,13,19,24,25,26,27,28,29] Majority of IPMN occurs in the head of the pancreas.[2,3,19] Clinically, the diagnosis of IPMN is often delayed due to its similarity to pancreatitis or cystic tumors of the pancreas.[2,4,13] In addition, the differentiation of benign and malignant IPMN is often difficult to be established preoperatively, despite the advances in imaging studies.[1,4,13] The prognosis after resection of the noninvasive neoplasms such as adenoma or noninvasive carcinoma is favorable.[2,3,4,13,15] On the contrary, the presence of an invasive component may be associated with poor survival even after surgical resection and in some cases, despite complete curative resection.[2,3,4,5,6,13,15] This article reviews the pathology, clinical presentation, classification, investigations, management, outcomes, and the recent consensus guidelines of this evolving condition. The literature was reviewed by searching the PubMed database for articles on IPMN. All the relevant abstracts in English language were reviewed and the articles in which cases of IPMN could be identified were further analyzed. Information on IPMN was derived, and duplication of information in several articles and those with areas of persisting uncertainties were excluded. In addition, two recent guidelines, the International consensus guidelines and the European consensus guidelines, were examined.
Etiology and Pathogenesis
There is no clarity regarding the etiology IPMN. There is, however, no definite genetic or familial tendency although an association has been described with familial adenomatous polyposis.[2,3,4,13,23,26,53] The genetic changes attributed to the progression of IPMN adenoma to IPMN invasive carcinoma have not been entirely established but are thought to be distinct from those associated with the development of pancreatic ductal carcinoma.[2,3,23] A leading feature of many IPMN is excessive mucin production. It has been demonstrated that most IPMN produce mucin 2 (MUC2) while mucin 1 (MUC1) is not expressed, except in those cases that showed an invasive tubular component resembling ductal carcinoma.[53] A mixed type of IPMN, coexpressing both MUCI and MUC2, has been reported.[13,23,53] Additional findings observed are the expressions of proliferating cell nuclear antigen (PCNA), tumor protein p53 (p53), and vascular endothelial growth factor (VEGF). This is particularly seen in those tumors where the malignant potential increases.[2,13,26] GTPase KRas (KRAS) mutation is considered to be the key event leading to subsequent genetic alteration in the development of IPMN, including inactivation of the tumor suppressor cyclin-dependent kinase inhibitor 2A (p16) and tumor protein p53 (p53) genes or the gene products.[2,4,23,26,53]
Pathology
IPMN is a pancreatic exocrine tumor composed of intraductal papillary growth of mucin containing neoplastic cells in the MPD or its major branches. The main duct-IPMN (MD-IPMN) is characterized by segmental or diffuse dilation of the MPD of >5 mm and in the absence of dilation due to another cause of obstruction. According to the recent consensus guidelines, a low threshold for MPD dilation (5 mm) is adopted. This increases the sensitivity for radiologic diagnosis of MD-IPMN without losing its specificity.[2] In the revised guidelines proposed, MPD dilation of 5-9 mm is considered as a “worrisome feature” while an MPD diameter of ≥10 mm is one of the “high-risk stigmata.”[2] Pancreatic cysts >5 mm in diameter that communicate with the MPD is considered as the branch duct-IPMN (BD-IPMN). In such patients, pseudocyst is considered in the differential diagnosis when there is a past history of pancreatitis in them. Those with both MD-IPMN and BD-IPMN features are categorized as mixed type.[2,4]
IPMN accounts for less than 10% of all pancreatic neoplasms. The reported locations of IPMN include the head (50%), the tail (7%), and the uncinate process (4%), with the remainder (39%) spread throughout the pancreas.[4,13,25,26,27] The present international classification system for IPMN separates noninvasive from invasive carcinoma. Noninvasive carcinoma is further categorized on the basis of the degree of dysplasia into low-grade and moderate dysplasia (their distinction has no clinical significance) and high-grade dysplasia or carcinoma in situ.[2,4,5,27] Even though the molecular steps of progression of IPMN to malignancy in the form of adenoma-carcinoma sequence is not well established, it is generally believed to occur.[2,3,5,13,28,29] Presently, most authors agree that their evolution toward the carcinoma stage is slow and estimated to be 3-6.4 years.[4,13,25,26,28] Malignant IPMN is associated with lower incidence (22%) of lymph node metastasis than ductal adenocarcinoma[30] and are found to be more favorable.[2,4,13,25,26]
Histological Aspect
Histological variant of invasive carcinoma has major prognostic implications, and is therefore a significant part during the reporting of IPMN.[51,52,53,54,55,56,57] IPMN is classified into four histopathological types based on the cytoarchitectural features and immunophenotypes. They include intestinal (18-36%), gastric (49-63%), pancreaticobiliary (7-18%), and oncocytic (1-8%) types [Figures 1 and 2].[27] A significant portion of MD-IPMN, which are of intestinal type, show diffuse expression of caudal type homeobox 2 (CDX2) and MUC2.[52,53] It is well established that the colloid carcinoma variant has a better prognosis than the tubular carcinoma.[2,3,5,13] The cell lineage of the “papillary component” of IPMN has clinicopathologic significance. The vast majority of BD-IPMN, that is, of the gastric type is mucin 5AC (MUC5AC) positive but MUC1 negative.[52,54] The gastric type is typically of low grade, with only a small percentage developing into carcinoma [Figure 1].[52,53] Although carcinoma may develop in them, it is usually of tubular type and behaves more like the conventional pancreatic ductal adenocarcinoma (PDAC).[52,53] On the contrary, the pancreaticobiliary type is not well characterized and is uncommon [Figure 2].[57] It is regarded by some as a high-grade version of the gastric type.[57] Invasive carcinoma associated with this type is usually tubular and aggressive.[51,52] Oncocytic type is another variant and is characterized by complex aborising papillae with delicate cores, oncocytic cells, intraepithelial lumina formation, and common mucin 6 (MUC6) expression.[55] These lesions are uncommon and have limited invasion capability and tend to be large with obscure intraductal appearance. With the present advances in endoscopic ultrasound (EUS)-guided biopsy, it is possible to subtype these lesions preoperatively, provided the papillae are sampled in the biopsy.[56]
Figure 1.
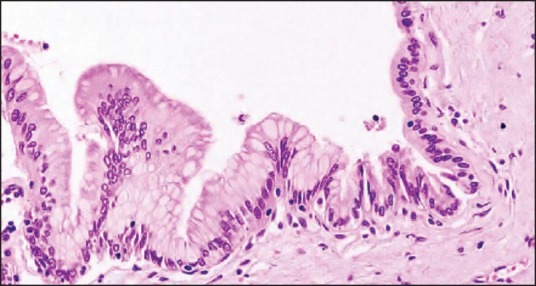
Low-grade (gastric IPMN) showing uniform monolayer of columnar cells with basal nuclei exhibiting no or minimal atypia
Figure 2.
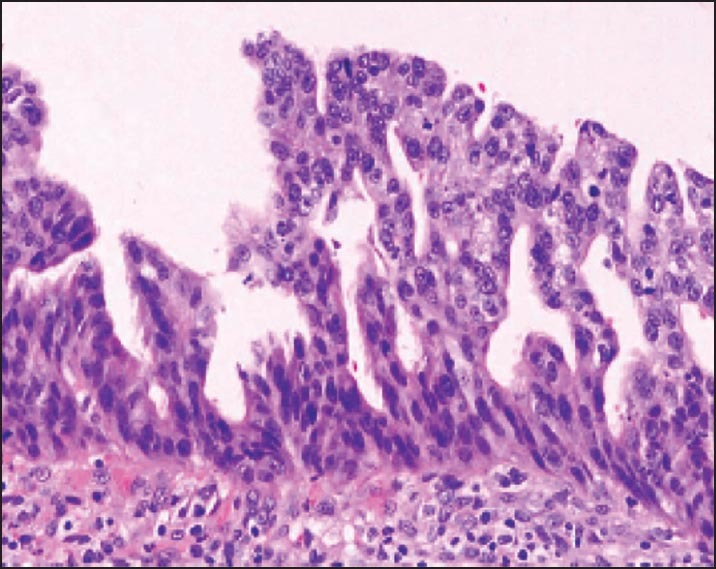
High-grade (pancreaticobiliary IPMN) showing marked cytological atypia and complex architecture with cribriform groups and the budding of neoplastic cells into the lumen
Differential diagnoses of IPMN that should be histopathologically differentiated include other mucinous cystic lesions, retention cysts, pancreatic intraepithelial neoplasm (PanIN), and intraductal tubulopapillary neoplasm (ITPN).[27] MCN can be differentiated from IPMN by the presence of ovarian type of stroma in MCN and by the absence of communication with the ducts.[2,27,33] Cystic mucin-producing lesions, without either IPMN histological features or ovarian type of stroma, are termed as indeterminate mucin-producing neoplasms. Retention cysts, which result due to obstruction of the pancreatic duct, are usually unilocular and are lined by normal or flattened duct epithelium without atypia but are occasionally described with slight papillary or mucinous change.[63] PanINs, which are premalignant lesions, are flat micropapillary or papillary lesions but unlike IPMN, these are not macroscopically visible and hence are microscopic entities.[63,64] They typically arise from the smaller ducts and then involve the larger ducts. The histological distinction between PanIN and BD-gastric type of IPMN may not always be possible because of its peripheral location, similar cytohistological appearance, and immunohistochemical profile (MUC2 negative and MUC5AC positive).[63,64] PanIN is generally less than 0.5 cm while IPMN is over 1 cm.[63,64] ITPN is a rare lesion and is characterized by a more solid intraductal growth without visible mucin secretion and with less cystic features than IPMN.[65] Histologically, ITPN is characterized by a complex proliferation of tubules and variable extension of papillary architecture.[65] The neoplastic cells show scanty cytoplasmic mucin and uniform high-grade dysplasia. Solid areas and necrotic foci are frequently seen.[65]
Classification
According to the site and extent of involvement, IPMN is usually classified into the following three types: MD, BD, and combined.[1,2,4,13,25,26,31] The morphological pattern of duct dilatation is dependent on both the tumor location and the mucus production.[4,24,30,31] The following four patterns have been recognized:
Diffuse MD ectasia,
Segmental MD ectasia,
Side branch ectasia, and
Multifocal cysts with pancreatic duct communication. Each pattern has its clinical implications, which is related to significant differences in the prevalence of cancer and therefore, the extent of resection.
The reported incidence of malignancy could vary from 57% to 92%[2,6,13,25,26,27] in MD-IPMN and from 6% to 46% in BD-IPMN.[1,2,3,4,5,6,13,25,26,27,28,29,30,31,32] Surgical specimen of BD-IPMN, when histologically examined, may reveal some degree of the MD involvement; this may lead to many BD-IPMN patients being reported as mixed type.[4,13]
MD type
MD-IPMN is characterized by diffusely or partially dilated MPD, filled with excessive mucin. Diffuse MD ectasia may be due to obstruction by neoplasm growth, mucus production by a tumor in the head of the gland, or a neoplasm diffusely involving the pancreatic duct.[2,3,4,5,6,13,25,26,27,28,29,30,31] MD-IPMN occurs predominately in the head of the pancreas and occasionally in the tail.[2,25,26,27,28,29,30,31] Segmental MD ectasia, however, usually involves the body and the tail of the pancreas. Obstruction of MD with viscid mucin or mural nodules over several years may lead to chronic pancreatitis, in which case the entire pancreas may be fibrotic.[3,13,33] The probability of malignancy increases when the MPD is >1 cm and shows mural nodules.[2] However, the predictive value of malignancy is reported to reach 91% in the presence of the following three factors: Mural nodules, tumor size ≥30 mm, and MD size ≥12 mm.[16] Once the invasive carcinoma develops from a preexisting IPMN and involves the MD, it may be difficult to demonstrate the presence of IPMN in such cases.[2,4,6,13]
BD type
Side branch ectasia is usually recognized in the head or the uncinate process, and is known to cause the most diagnostic uncertainty.[9,14,18,23] This pattern is often seen in asymptomatic patients and a precise preoperative diagnosis is generally recommended before embarking on a major resection.[2,3,4,13,18] The branch type affects one or more branches of the pancreatic duct, which consequently show cystic dilatation. These may be filled with solitary or multiple tumors and/or viscid mucin.[2,18,22,23,24,25,26,27] They are often confused with pseudocysts, simple cysts, and serous cystadenoma, as they may appear similar on imaging.[3,6,13] The presence of large mural nodules increases the likelihood of malignancy.[2,14,16,23,24,25,26,27] Large IPMN may cause compression of the MPD and the bile duct, resulting in jaundice. The BD, however, is less often associated with invasive carcinoma in comparison to MD-IPMN.[2,3,4,6,16,23,27]
Combined type
This type of IPMN is a combination of the above two types.[2,3,4,6,9,16,23,24,25,26,27,28,29] This may be an outcome of an advanced form of the branch type, in which IPMN has spread to the MPD or an end result of the MPD type involving the BD as well. In the combined type, the MPD contains papillary growth of columnar epithelia of various degrees of dysplasia that produce excessive mucin.[2,3,6,13] Caution, however, is required in classifying a BD-IPMN as a mixed type merely because the MPD is dilated due to excessive mucin production by the branch type.[3,4,13]
Clinical Presentation
Patients with IPMN complain of epigastric discomfort or pain (70-80%), nausea and vomiting (11-21%), backache (10%), weight loss (20-40%), diabetes, and jaundice.[13,25,26,27,33] The patients in whom invasive carcinoma coexists with IPMN (40% of patients), a symptom profile similar to that of PDAC (jaundice, pain, weight loss, and malaise) may be present.[4,13,25,26,27,28,29,33] Weight loss is seen in these patients, which may be due to reasons related to the stage of the disease. In the early phase, the hyperproduction of mucin obstructs normal pancreatic secretion, causing pain related to meals.[3,13] Hence, the patient stops eating to avoid pain. In the more advanced stage, loss of appetite is related to neoplastic factors responsible for cachexia. Jaundice is a consequence of obstruction of the common bile duct (CBD) by viscid mucin, mural nodules, or direct compression by the size of IPMN. Persistent occlusion of the MPD with viscid mucin may result in exocrine and/or endocrine pancreatic insufficiency, and some may have persistent hyperamylasemia for many years.[3,4,13,26,29] However, a significant number of patients with inactive mucin production or involvement of the body/tail of the pancreas may be asymptomatic. Approximately, 20% of the patients with IPMN present with acute pancreatitis of mild to moderate severity.[3,4,25,26] Some of them may appear to have idiopathic pancreatitis in view of the dilated pancreatic duct or chronic pancreatitis. However, patients with IPMN are older and have no history of prolonged pancreatopathy.[3,25] Infrequently, IPMN can fistulate into the adjoining organs including the stomach, the duodenum, the choledochus, the colon, and the small intestine.[27] The fistula may be related to benign IPMN (low-grade dysplasia). This fistula may occur as a consequence of mechanical penetration as a result of excessive pressure by the mucin-filled ducts or due to inflammation or autodigestion by the enzyme-rich fluids,[27] or it could be a result of direct invasion due to malignancy, as in malignant IPMN (high-grade dysplasia).[27]
Diagnosis
Detection of cystic lesion in the pancreas on ultrasonography performed for abdominal pain may require further analysis with computed tomography (CT) scan or magnetic resonance imaging (MRI) to reduce the number of differential diagnosis.[60] While in the past, CT scan was considered as the primary imaging modality in detecting and evaluating IPMN, of late magnetic resonance cholangiopancreatography (MRCP) is found to be more reliable and when available, would be an initial investigation of choice.[2,3,4,5,9,10,12,13,16,30,60] CT scan, however, may reveal one or more cystic dilatations in the pancreas (branch type) or diffuse or segmental dilatation of the MPD (main duct type) with or without polypoidal lesion in patients with IPMN [Figure 4]. While duct dilatation can be appreciated even in noncontrast CT scan, distending the duodenal lumen with water will facilitate recognition of the protruding papilla.[2,3,10,16] Deposits of calcium in mucin may appear as calcification. Significant ductal dilatation with normal or increased parenchymal thickness may indicate the presence of malignancy, which is supported by the presence of papillary proliferations. The presence of cystic ectasia of collateral ducts, along with the protruding papilla, makes diagnosis of the diffuse forms easier.[3,10,16] In segmental forms, the CT image is nonspecific.[10,16] However, if a communication of the cystic mass to pancreatic duct is established, then IPMN diagnosis is most likely. The following CT scan signs are useful in differentiating a benign IPMN from a malignant IPMN:[2,3,10,16]1) the presence or absence of mural nodules, 2) focal size of the lesion: A lesion greater than 30 mm, with mural nodules that strongly suggest malignancy, 3) enlargement and metastasis of the lymph nodes, and 4) MPD dilatation of >10 mm.
Figure 4.
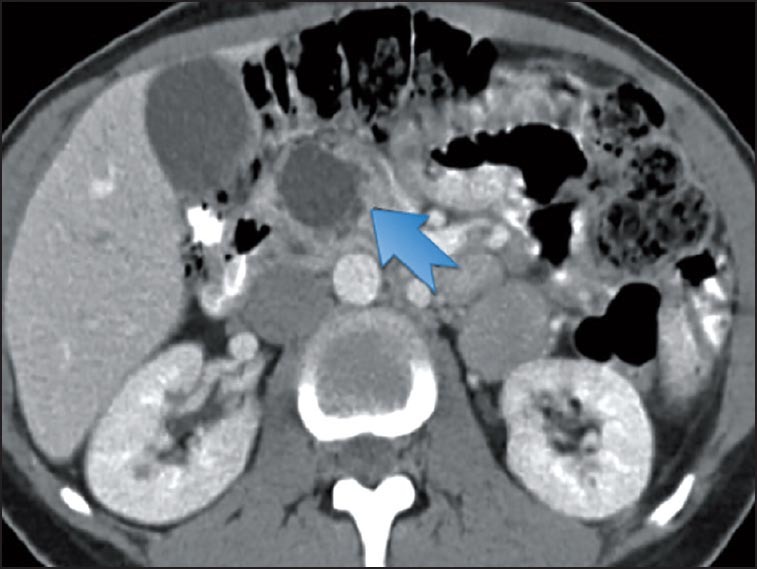
CT scan showing a large cystic lesion in the head of the pancreas in a patient with MD-IPMN
However, the ductal system and its communication with cystic masses are better appreciated on endoscopic retrograde cholangiopancreatography (ERCP).[34,35,36] The features that may be well noted include dilatation of the MPD or its branches, filling defects due to the presence of either mural nodules or mucin, and communication of the duct with cystic masses.[2,3,13,34,35,36] Moreover, the diagnostic features like the gaping ampulla with extrusion of mucin (fish-mouth appearance) may be observed.[2,3,13] Further improvement in the ERCP technique, including the balloon catheter ERCP-compression study (ERCP-CS), may facilitate better quality pancreatograms by spot film compression, thereby demonstrating localized stenosis and ductal communications.[35] The diagnostic ability of the balloon catheter ERCP-CS in MD-IPMN and BD-IPMN is reported to have a sensitivity of 100% and 73%, specificity of 40% and 86%, and accuracy of 84% and 82%, respectively.[2,3,34,35,36] However, due to its invasive nature, of late it has been superseded by MRCP as an initial investigation of choice and is used only in those patients with uncertain diagnosis.[60]
MRCP is reported to be more sensitive than ERCP,[2,3,9,12,13,60] the distinct advantage being that it is not operator dependent and noninvasive. Moreover, due to its high signal intensity, the dilated ductal system and complex cystic mass associated with the side-branch IPMN is better demonstrated [Figure 3].[9,12] MRCP visualizes the entire outline of either MD-IPMN or BD-IPMN, which may not be feasible in ERCP, particularly in the presence of ductal obstruction by mucin or mural nodules. MRCP is also found to be useful in postoperative follow-ups.[2,3,13,60]
Figure 3.
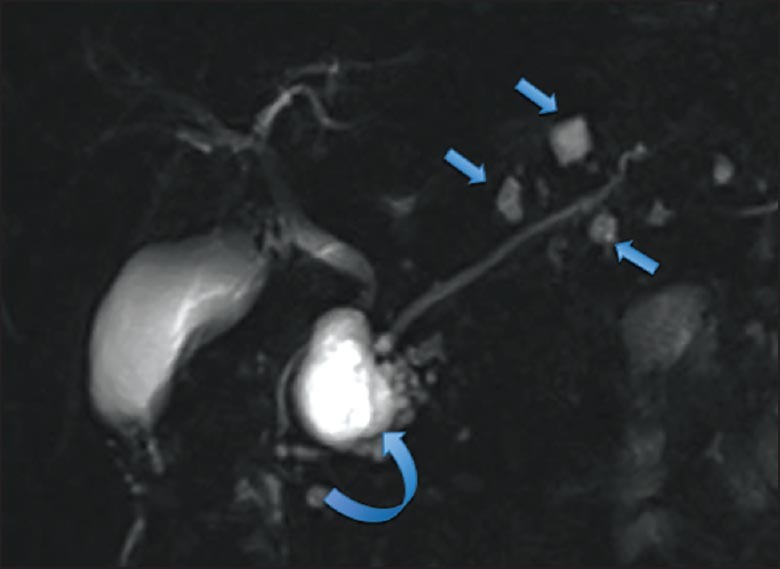
MRI coronal T2 weighted images of BD-IPMN. Multiple cystic dilations of the side branches with the largest lesion in the head (curved arrow) and smaller lesions in the body and the tail (straight arrows)
EUS adds a further dimension in the diagnosis of IPMN by improving the accuracy of the assessment of pancreatic parenchyma.[66] The features that are diagnostic of IPMN in EUS include dilatation of the MPD, hypoechoic thickening of the duct wall, mural nodules or papillary projections, and pancreatic atrophy.[37,66] EUS is generally considered to be reliable in identifying lesions that merit resection than in clarifying the exact type of cystic lesion present.[60] A recent report has proposed an EUS scoring system using seven points, which has been reported to predict malignancy in BD-IPMN more accurately than the Sendai criteria with 75% sensitivity and 94% specificity.[63]
Recently, some centers have used peroral pancreatoscopy in evaluating IPMN.[40] Assessment of mucin secretion, and the nature and location of mural nodules and their biopsy can be established by peroral pancreatoscopy.[40] In MD-IPMN, peroral pancreatoscopy may demonstrate the fish-egg appearance of papillary neoplasm, granular or polypoidal mucosa, or rough mucosa while in BD-IPMN, it may reveal mucin in the MPD.[27,40] The drawback, however, is that the expertise is limited to a few centers; it is operator dependent and it may be impossible to assess the tumor located at a side branch.[37,40] Presently, its role in evaluating IPMN is not well established and its use is restricted to those few centers where it may be useful in differentiating between benign (chronic pancreatitis) lesion and premalignant lesion in MD-IPMN.[60]
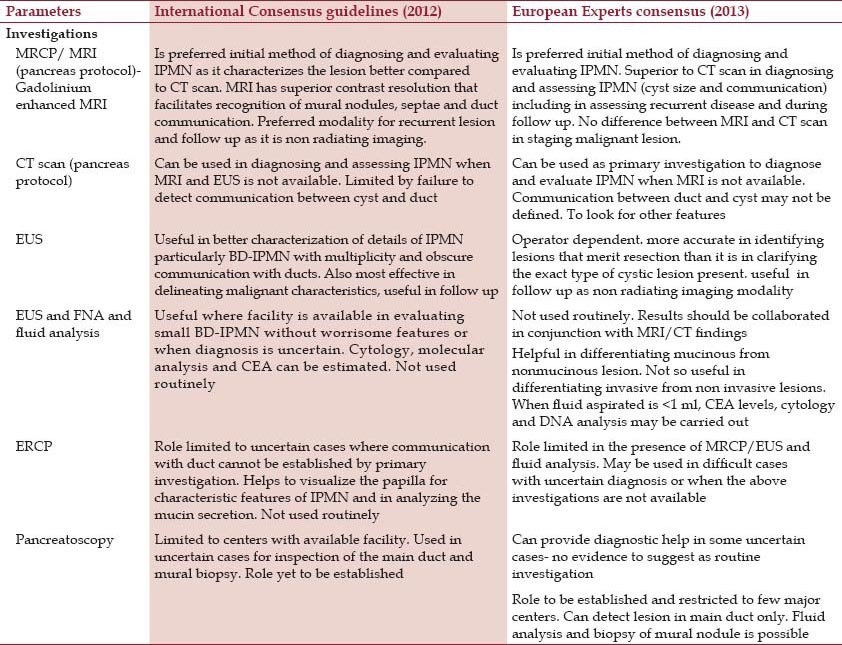
In a recent report, fludeoxyglucose (18F)-positron emission tomography (FDG-PET)/CT scan was found to be superior to contrast enhanced CT scan in differentiating between benign and malignant IPMN with mural nodules.[8] With a cutoff value of 2.3-mm-sized mural nodules, the sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were found to be 77.8%, 100%, 100%, 77.8%, and 87.5%, respectively.[8] However, its role in routine management of IPMN is still to be established.[60] The role of the various investigations based on the two recent guidelines are summarized in Table 1. To summarize, the initial investigation of choice in evaluating IPMN should be pancreatic protocol MRI/MRCP (CT only when MRI is not available) or EUS. ERCP, cystic fluid analysis, and pancreatoscopy are considered in cases where there is difficulty in establishing the diagnosis or in ruling out malignancy.[2,60] The staging of the invasive carcinoma is by using the conventional staging protocols of the American Joint Committee on Cancer/TNM Classification of Malignant Tumors (AJCC/TNM) and a further substage of the T1 category (those with invasive carcinoma of <2 cm) is included. These are subdivided into T1a for those that are ≤0.5 cm, T1b for those that are >0.5 cm and ≤1 cm, and T1c for those that are 1-2 cm.[2]
Table 1.
Comparison of the role of investigations between the International consensus guidelines and the European experts’ consensus statement
Preoperative predictors of malignancy
Despite the advances made in radiological investigations to facilitate the diagnosis of IPMN, the concern remains in differentiating a benign IPMN from a malignant lesion. Several reports that have appeared have described the preoperative variables common in patients with IPMN and the abnormal findings on investigations (particularly radiological), and its correlation with subsequent histological findings or survival outcomes.[2,3,5,13,24,26,29,46]
Clinical variables
The clinical variables studied include age (>70 years), sex of patient, diabetes mellitus, pancreatitis, steatorrhea, abdominal mass, tumor size, weight loss, serum carbohydrate antigen (CA) 19-9 level, and serum carcinoembryonic antigen (CEA) levels.[2,3,4,13,24,25,26,27,32] Salvia et al.[25] and Weisenauer et al.[41] have suggested jaundice and its worsening form, or the new onset of diabetes mellitus as the preoperative predictors of malignant IPMN. Cytological findings and CEA levels in pure pancreatic juice are reported to correlate to the risk of malignancy. In recent reviews, elevated CEA is reported to be a marker that distinguishes mucinous from nonmucinous cysts, but not benign from malignant cysts.[2,38,39] A cutoff value of ≥192-200 ng/mL is approximately 80% accurate for diagnosis of a mucinous cyst.[2,38,39] An increase in the cutoff value improves specificity at the expense of the sensitivity.[42] In a recent study, the risk factors of malignancy developing in BD-IPMN were studied. Seven significant predictors were noted in univariate analysis of 134 patients and included the following: Jaundice, tumor occupying the pancreatic head, MPD size >5 mm, mural nodules >5 mm, serum CA 19-9 level, positive cytology in pancreatic juice, and CEA levels in pancreatic juice >30 ng/mL.[14] In a multivariate analysis, a mural nodule size >5 mm and CEA levels in pancreatic juice of >30 ng/mL were the independent factors associated with malignancy. The positive predictive value of a mural nodule size >5 mm and CEA level in the pancreatic juice >30 ng/mL was 100% with a negative predictive value of 96.3%.[14]
Radiological investigations
Abnormal radiological findings suggestive of malignant IPMN include the appearance of mural nodules, abnormal contrast enhancement of the ductal walls, mural nodules larger than 3 mm, cyst size greater than 3 cm, and the dilated MPD.[2,3,4,13,16,30,34,46] The MPD is reported to be wider in patients with malignant IPMN, compared to benign lesion.[2,60] MPD diameter of >10 mm is found to be associated with malignancy with a specificity of 92%.[43,44] Tumors, with the MPD dilatation greater than 10-15 mm, are reported to be statistically (P < 0.05) of poorer prognosis than those that cause less dilatation. Several other findings suggestive of malignancy include large side branch tumors, papillary bulging, CBD dilatation, large number of tumors, solid components, calcified ductal content, invasion to adjacent organs, enlarged peripancreatic lymph nodes, and presence of liver lesions that are suggestive of metastasis.[2,3,4,5,6,13,16,24,25,26,27,28,29,32,34] Taouli et al. reported the specificity of the association of malignancy in the presence of solid mass, multifocal involvement, and intraluminal calcified content to be 96%, 77%, and 77%, respectively.[44] Kawamoto et al. noted that the size of the tumor in the BD type and the combined type, and the caliber of the MPD were significantly larger in patients with invasive carcinoma when compared with those without invasive carcinoma (4.7 ± 1.7 cm vs 2.6 ± 1.4 cm) [P = 0.0007] and (9.3 ± 5.5 mm vs 4.6 ± 4.1 mm) [P = 0.006].[43,45] However, a recent study analyzing the International consensus guidelines[2,60] using parameters like “worrisome feature” and “high-risk stigmata,” observed that these parameters carry unequal weight and are not cumulative in the predication of risk of malignancy or invasiveness of IPMN.[61]
Differential diagnosis
Several lesions of the pancreas could be considered in the differential diagnosis of IPMN, based on the age of the patient, clinical presentation, and radiological findings.[2,3,4,13,16,26,29,33,35,41,46] The most likely among them include chronic pancreatitis, mucinous cystadenoma, serous cystadenoma, simple cysts, and pseudocysts.[3,35] Side branch ectasia is usually recognized in the head and the uncinate process, and is the pattern that causes most diagnostic uncertainty.[2,3,6,13,16] This pattern is often seen in asymptomatic patients and on imaging, may appear similar to pseudocyst, simple cyst, or serous cystadenoma.[3,6,13] EUS performed to demonstrate the presence of mural nodules and analysis of the cyst fluid for cytology, extracellular mucin, and CEA levels may help in establishing the diagnosis.[38,39,42] In the presence of ductal dilatation, calcification, and some degree of parenchymal atrophy, differentiating IPMN from chronic pancreatitis becomes important.[2,3,13] Demographic data (sex and age) and lifestyle habits (alcohol consumption and smoking) may suggest chronic pancreatitis, while the presence of jaundice and diabetes is suggestive of malignancy.[3,35] IPMN differentiation from MCN could be challenging.[30,33] This is compounded by the fact that the tumor cells of MCN have the same cytological features as those of IPMN.[2,25,26] However, the features that would point to a diagnosis of MCN include patients who are usually asymptomatic and this occurs almost exclusively in young women; however, patients with malignant variant may be a few years older. IPMN, which occurs more commonly in the pancreatic head, can be single or multifocal and is seen more commonly in men.[3,13] The location of side branch IPMN is mainly in the uncinate process unlike MCN, which is seen usually in the body and the tail of the pancreas.[3,13,16]
Workup for cystic lesions of the pancreas
Investigations of pancreatic disorders by imaging studies have led to increased detection of cystic lesions of the pancreas. The frequency of pancreatic cyst detection by MRI (19.9%) is higher than that of CT.[2,60] However, according to a recent guideline, when the cysts are <10 mm in size, the risk of malignancy is low and therefore no further workup may be needed at that point, although follow-up is recommended.[2] However, when the cysts are >10 mm, better characterization of the lesions is required and this is best achieved by gadolinium-enhanced MRI, with MRCP or pancreatic protocol CT scan.[2,9,13,60] The general consensus suggests that dedicated MRI is the procedure of choice for evaluating pancreatic cysts, based on its superior contrast resolution that facilitates recognition of septa, nodules, and duct communication.[2,9,12] Moreover, patients who require frequent imaging during follow-up are better served by MRI, as radiation exposure is avoided and their images are superior.[2,9,12]
“Worrisome features” on imaging include cyst of ≥3 cm, thickened enhanced cyst walls, MPD size of 5-9 mm, nonenhanced mural nodule, abrupt change in the MPD caliber with distal pancreatic atrophy, and lymphadenopathy.[2] The cysts with obvious “high-risk stigmata” on CT or MRI (i.e., obstructive jaundice in a patient with a cystic lesion of the pancreatic head, enhanced solid component, and MPD size ≥10 mm) should undergo resection without further testing.[2] A smaller cyst with “worrisome features” is evaluated by EUS to further stratify the risk of a malignant lesion. Patients with cysts of >3 cm and no “worrisome features” are considered for EUS to verify the absence of thickened walls or mural nodules, particularly when the patient is elderly.[2] All the patients with cysts ≤3 cm in size and without “worrisome features” undergo surveillance, according to the risk of malignancy.[2,60] When the patients present with symptomatic cystic lesions, they would require further evaluation and resection to relieve their symptoms, and to alleviate the concern of higher risk of malignancy.[2,60]
Distinction of BD-IPMN from MCN and other pancreatic cysts are achieved by a combination of the clinical history, sex, imaging characteristics, cytology, cyst fluid, and chemical analysis of CEA and amylase.[3,4,6,13,16] This would facilitate not only in characterizing the pancreatic cysts into mucinous and nonmucinous but possibly their specific subtypes as well.[3,4,26,29] The initial preoperative diagnosis of the cyst type may be established by a combination of clinical and imaging characteristics. The primary imaging modality for the diagnosis of BD-IPMN are multidetector CT (MDCT) and MRCP, which would define the morphology, location, multiplicity, and communication with the MPD.[2,3,13,16] The reliable distinguishing features of BD-IPMN include multiplicity and visualization of a connection to the MPD, although such a connection is not always observed.[2,60] In such instances, EUS can be used for detecting mural nodules and invasion, and is most effective for delineating the malignant characteristics, although it has limitation of operator dependency.[2,60] While the cyst fluid can be further analyzed for CEA and amylase levels as well as cytology, it may not be always possible to distinguish MCN and IPMN. A more recent study reported the usefulness of molecular analysis for GNAS complex locus (GNAS) mutations to distinguish between MCN and BD-IPMN.[50]
Association with other malignancies
An interesting observation made by some researchers is the likely association of IPMN with synchronous or metachronous malignancy in various other organs.[2,3,5,47,48] The rate of association of IPMN with malignant extrapancreatic organs has been reported to range 10-40%.[2,3,5,47,48] Nonpancreatic malignancy was noted in patients with benign and malignant IPMN, and included tumors like colorectal, gastric, and bile duct tumors. These were seen before surgery 78/92 (80.4%), at surgery 14/92 (14.4%), or after surgery for IPMN 5/92 (5.2%) of the patients.[5] In a multicenter cohort study of 92 patients with IPMN, extrapancreatic malignancy was found in 23.6% of the patients.[5] These included colorectal cancer [2.26; confidence interval (CI) 95% 1.17-3.96], renal cell carcinoma (6.0; CI 95% 2.74-11.39), and thyroid cancer (5.56; CI 95% 1.80-12.96).[5] The frequency and the location of extrapancreatic malignancies differ from one country to another.[2] Gastrointestinal cancer is common in Asia,[47] while skin, breast, and prostate cancers are frequent in the United States.[48] Increased age, heavy cigarette smoking, alcohol consumption, and first degree family history of gastric cancer were seen as the significant risk factors while first degree family history of colorectal cancer was a borderline risk factor.[5] The relationship between the types of IPMN and the extrapancreatic malignancies is controversial.[2] While some authors report that extrapancreatic malignancies occur in all types of IPMN,[5,47,48] others have related it to the transcription of MUC2.[49] There are no screening recommendations for detecting extrapancreatic malignancies at present, but it is prudent to look for these lesions based on the frequency of malignancies in the general population of the country or region.[2] Reports have recommended the screening of colorectal polyps and cancer in the United States.[48]
Management
Surgical outcome of IPMN has been widely accepted to be better than that of ductal adenocarcinoma of the pancreas. This stems from the fact that IPMN has indolent biological behavior, including slow growth and late metastasis. The recommendations of consensus guidelines in the management of IPMN in general include resection of most MD-IPMN, mixed variant, and symptomatic BD variant.[1,2,3,4,5,6,13,26,29,60] This is summarized in Table 2.
Table 2.
Comparison between the International consensus guidelines and the European experts’ consensus statement in the management of IPMN
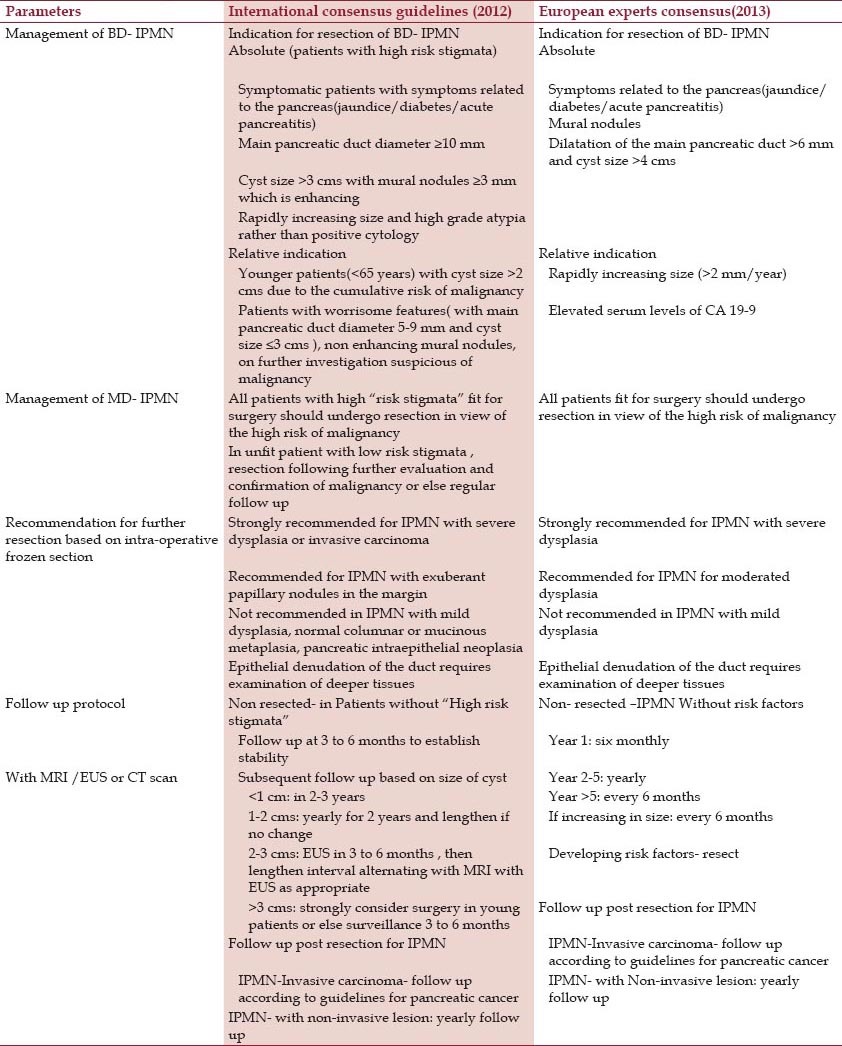
Indication for resection of MD-IPMN
MD-IPMN shows invasive proliferation and may progress rapidly with a poor prognosis.[2,60] The mean frequency of malignancy in MD-IPMN is 61.6% (range 36-100%) and the mean frequency of invasive IPMN is 43.3% (range 11-81%).[1,2,3,4,5,6,13,26,27,28,29,30,31,32,33,60] Considering these high incidences of malignant/invasive lesions and the low 5-year survival rates (31-54%), surgical resection with lymphadenectomy is strongly recommended for all surgically fit patients with invasive MD-IPMN, while patients with benign IPMN may be observed.[1,2,3,4,5,6,13,26,27,28,29,30,31,32,33,60] Therefore, it is essential to select the appropriate treatment strategy for IPMN by accurately differentiating malignant IPMN from benign IPMN. The patients having MD-IPMN with MPD dilatation of 5-9 mm are considered to have “worrisome features” and as in the case of BD-IPMN, are recommended for evaluation without immediate resection;[2] however, others would consider resection of all the MD-IPMN patients with MPD >6 mm in a fit patient.[60] Asymptomatic benign MD-IPMN are strictly followed up without resection.[2] They generally progress slowly, occur in elderly patients, and are sometimes multifocal.[2,3,5,13] To date, there are no consistent predictive factors for malignancy;[2,5,25,30] however, some have recommended resection under certain criteria. These include the presence of symptoms, MD, or combined type with dilatation of MPD >10 mm, presence of mural nodules >5 mm in size, cytological findings of classes 1V and V in the pancreatic juice, and CEA concentration in pancreatic juice >110 ng/mL. While in segmental ectatic type or diffuse type with focal lesions (mural nodules etc.), it is relatively easy to decide on the site and extent of resection, those with diffuse dilatation type without focal lesions need careful evaluation including ERCP, EUS, and pancreatoscopy (when available), as some of them may be due to chronic pancreatitis rather than IPMN.[1,2,3,13,26,33,43,60]
Indication for resection of BD-IPMN
The mean frequency of malignancy in resected BD-IPMN is 25.5% (range 6.3-46.5%) and the mean frequency of cancer is 17.7% (range 1.4-36.7%).[1,2,3,4,5,6,7,8,26,27,28,29,60] Hence, although resection of BD-IPMN warrants consideration, these lesions mostly occur in elderly patients with an annual malignancy rate of 2-3%.[2,58,59] These factors support a conservative management with follow-up in patients who do not have the risk factors predicting malignancy.[2,3,4,5,13,26,43,60] New high-risk factors proposed include a rapidly increasing cyst size and high-grade atypia[2,58,60] rather than “positive cytology.”[67,68] Controversy, however, exists in dealing with patients who are younger (<65 years) with a cyst size >2 cm and they may be the candidates for resection owing to the cumulative risk of malignancy [Table 2].[69,70] BD-IPMN size >3 cm is a weaker indicator of malignancy than the presence of mural nodules and positive cytology; thus, BD-IPMN >3 cm without these signs may be observed without immediate resection, particularly in the elderly patients.[2,60] The recommendations of the two recent guidelines are summarized in Table 2.
Extent of resection
Resection is based on the location and extent of IPMN. In general, pancreaticoduodenectomy with lymphadenectomy is indicated for invasive MD-IPMN of the head, the neck, or the uncinate process,[1,2,3,4,5,6,13,14,15,25,26,33] and distal pancreatectomy is indicated for IPMN of the body and tail of the pancreas. Total pancreatectomy is carried out in exceptional cases when IPMN diffusely involves the whole gland or when a proximal IPMN extends through the body and the tail.[1,2,3,4,5,6,13,14,15,25,26,30,33] With each partial pancreatectomy, an assessment of the margin by frozen section is carried out to allow further resection of positive margin when either high-grade dysplasia or invasive carcinoma is reported [Table 2].[2,3,13] Total pancreatectomy is not commonly recommended as it results in obligate insulin-dependent diabetes, predictable malabsorption requiring pancreatic enzyme supplements, and other metabolic complications.[2,60,71] Despite being a possible curative operation for extensive noninvasive IPMN, it does not universally prevent recurrence for invasive lesion.[2] Thus, total pancreatectomy is not necessary for the majority of the patients.[2,3,13,25,26,29,30,33] Following total pancreatectomy for invasive IPMN, the overall disease recurrence rate is 12-68%.[1,2,3,4,5,6,13,24,25,26,30,33] The recurrence in the form of disseminated disease (3.4-44%) is higher than isolated pancreatic remnant recurrence (0-15%).[1,2,3,4,5,6,13,24,25,26,30,33] Thus, prophylactic total pancreatectomy may not solve the problem of high incidence of disseminated disease recurrence.[1,2,3,4,5,6,13,26,30,33] Based on the present evidence, the patients with IPMN should receive segmental pancreatectomy as far as negative ductal margin can be obtained in order to preserve as much exocrine and endocrine pancreatic functions as possible.[2,60] Total pancreatectomy is reserved for patients with resectable but extensive IPMN involving the whole pancreas.[2,3,13,25,26,30,33]
Limited resection or focal nonanatomic resection includes excision, enucleation, and uncinectomy, and are considered for BD-IPMN without clinical, radiological, cytopathological, or serological suspicion of malignancy.[71,72,73] However, the concern is that it may be associated with rare but possible leakage of mucin, resulting in pseudomyxoma peritonei. In addition, the risk of developing pancreatic fistulae and recurrence from potential residual neoplasms exists.[74]
Role of laparoscopic resection
The patients with low-grade or high-grade dysplasia of IPMN may be good candidates for laparoscopic surgery.[75,76] However, conversion to a standard resection with lymphadenectomy is carried out if intraoperative findings raise concern of malignancy or frozen section pathology reveals high-grade dysplasia or invasive disease.[75,76] A reoperation would be required in surgically fit patients, in the event the final pathology reveals invasion or positive margin for high-grade dysplasia, undetected on frozen section.[2]
On table assessment of extent of resection
One of the major concerns of a surgeon is to estimate on table the extent of the disease and thus, the extent of resection. After resection, the tumor involved ductal margin for both benign and malignant pathology and is reported to range 23-52%.[13] Diffuse dilatation of the MPD seen on preoperative imaging can be due to mucus plugs, tumor obstruction of the MPD, or diffuse tumor involvement of the pancreatic duct.[2,3,4,5,13,26,29,33] The various options employed by the surgeon to determine the extent of disease and facilitate the extent of resection include intraoperative ultrasonography[77,78] and pancreatoscopy.[13,40] However, it is intraoperative frozen section that is often used to decide on the extent of resection.[2,60] This is despite the concern that the diagnosis by frozen section is not always accurate as it is considered a suboptimal method of analyzing tissue morphology.[79] The resection should be extended if the ductal margin shows malignant invasive disease.[17,43,80] The management of the ductal resection margin with benign and noninvasive diseases such as the various degrees of atypia or dysplasia is a controversial issue.[43,81] In general, the presence of lesser grades of dysplasia (moderate or low-grade) may not require any further therapy.[2,3,5,13,82] On the other hand, if clear high-grade dysplasia or invasive carcinoma is present at the margin, further resection is warranted.[2,3,4,5,6,13,26,29,33] If exuberant papillary nodules are present at the margin, there may be abundant residual tumor in the pancreas.[83] The recommendations of two recent guidelines regarding this are summarized in Table 2. While some would not resect further, others would recommend total pancreatectomy.[2,3,4,5,6,13,25,26,29,33,43] Such an aggressive treatment, however, should be balanced against the long-term postoperative consequences.[2,60]
Role of mucosal ablation by ethanol injection under EUS guidance in the management of IPMN
There are reports of EUS guided ablation of pancreatic cysts/IPMN by ethanol or ethanol followed by paclitaxel.[84,85,86] The patients suitable for these include those with cystic lesions that show no communication with the MPD and IPMN in those who refuse surgery or are high-risk surgical candidates.[86,87] While significant success has been reported in patients with CT-defined cyst resolution (33-79%), concerns remain.[84,85,86,87] These include insufficient ethanol infiltration and impossible imaging surveillance after cyst collapse.[88] In addition, recent studies have shown that PDAC occurs quite frequently as a malignant transformation of IPMN in some sites, and not related to IPMN at others.[89] More light needs to be thrown into the applicability of this modality of treatment with regard to the technique, materials, long term outcome, and its adequacy. Presently, it is only part of the closely monitored research protocol.[2]
Role of adjuvant therapy in invasive IPMN
In a recent report, the patients with resected invasive IPMN showed better survival rate when treated with gemcitabine-based adjuvant chemotherapy.[7] Significant disease-free survival benefit was seen in both node positive and node negative subgroups, with significant overall survival benefit in patients with node involvement.[7] Further studies on the role of adjuvant therapy should clarify its role in the armamentarium of management, after resection of invasive IPMN.
Prognosis, recurrence and surveillance
The overall 5-year survival is reported to be 36-77%.[1,2,3,4,5,6,13,16,18,25,26,28,29,31,33,43] The 5-year survival of surgical resection for noninvasive IPMN was reported from 77% to 100%. However, the 5-year survival rate following surgical resection for IPMN with invasive carcinoma has been reported to range 27-60%.[1,2,3,4,5,6,13,16,18,25,26,29,33,43] The presence of invasive carcinoma, the type of invasive component (tubular is worse than colloid), lymph node involvement, the presence of vascular invasion, surgical margin involvement, and the presence of jaundice are poor prognostic factors for patients with IPMN after resection.[1,2,3,4,5,13,29,43] It has been reported that the malignant IPMN acquire aggressive behavior similar to that of common type pancreatic carcinoma, once it has invaded the pancreatic parenchyma.[2,43]
The patients with resected benign IPMN have a risk of recurrence in the remaining pancreas and if it occurs, can benefit by further resection. The overall recurrence rate for IPMN varies from 7% to 43%.[1,2,3,4,5,6,13,16,18,25,26,29,33,43] There is a risk of recurrence in both invasive and noninvasive IPMN, making follow-up mandatory. Good results have been seen in patients who undergo repeat resection for isolated recurrence in the pancreatic remnant.[2,3,13,43]
In a recent systematic review and meta-analysis comparing the surgical outcome of IPMN with PDAC, IPMN was significantly more likely to present at an earlier stage and was less likely to demonstrate nodal involvement, perineural invasion, and vascular invasion.[90] The likelihood of IPMN tumor extending beyond the pancreas compared to PDAC was 27.6% versus 94.3% (T4 vs T1), nodal metastasis was 45.4% versus 62.9%, positive margin was 14.2% versus 28.3%, perineural invasion was 49.2% versus 76.5%, and vascular invasion was 25.2% versus 45.7%.[90] The overall 5-year survival was significantly better at 34.5% versus 12.4%.[90]
Follow-up (surveillance)
There is no adequate evidence in the literature to define the frequency and type of surveillance that is required to detect recurrences. The decision to follow up an IPMN is a matter of clinical judgment based on the patient's age, family history, symptoms, comorbidities, perceived pancreatic cancer risk, and the patient's preference.[2,31,60] The follow-up would include history/physical examination, MRI/MRCP (or pancreatic CT scan) surveillance,[1,2,3,4,5,6,12,13,14,17,25,60] and EUS when the presence of a mural nodule is suspected.[60] If expertise is available, consideration is given for EUS with cytopathology,[62,63,64,65,66,67,68,69] CEA,[39] and molecular analysis.[89,90] However, molecular analysis is evolving. Studies show that the detection of KRAS mutation is likely to support the diagnosis of mucinous cyst more accurately rather than malignant cyst.[91,92] A recent study indicates that GNAS mutation may be helpful in distinguishing a mucinous cyst from an indolent cyst that can be managed conservatively.[50]
Frequency of surveillance
The frequency of surveillance, as suggested by the two recent consensus guidelines,[2,60] is summarized in Table 2. The patients with “high-risk stigmata” are recommended to undergo short interval (3-6 months) follow-ups with pancreatic protocol MRI/MRCP (or CT scan) to establish the stability, if prior imaging is not available.[2,60]
One study suggests only clinical follow-up with imaging being considered, if the symptoms appear.[91] A regimen consisting of yearly follow-up with nonradiating images like MRI or EUS is most widely used for surveillance.[25,26,60,93] There is no good long-term data to indicate whether surveillance can be safely spaced to every 2 years or even discontinued after long-term stability.[2] Some would prefer to continue surveillance at short intervals due to the potential risk of developing PDAC in patients with IPMN.[2,3,4,5,6,25,33,82,88] If surgically fit, the patients with high-risk stigmata detected on surveillance undergo resection.[2] Shorter interval surveillance (3-6 months) is considered in those patients whose IPMN progresses toward these indicators or in those patients who already have high-risk stigmata. In addition, it is also considered in those patients, who for reasons of operative risk or personal preference, have chosen heightened surveillance over resection.[2] The patients who have undergone partial pancreatectomy for IPMN undergo yearly follow-up and those who had resection for invasive IPMN-cancer are followed up, according to the guidance for pancreatic cancer.[60] It has been suggested that pancreaticogastrostomy should be used after pancreaticoduodenectomy that would allow easy access to the pancreatic duct and thus, for disease surveillance with endoscopy and sampling of the pancreatic juice for cytology.[94]
Conclusion
Knowledge of the natural history and pathology of IPMN is still incomplete and our understanding of the disease in terms of its management is evolving. IPMN constitutes less than 10% of pancreatic neoplasms, with MD-IPMN being the commonest. The concern, however, is that if untreated, some of them may follow the dysplasia-carcinoma sequence, thereby progressing into invasive carcinoma. Despite the advances made in radiological investigations, it may still be difficult at times to differentiate IPMNs from other benign lesions. The recent guidelines suggest a lowering of the MPD diameter to >5 mm as a criterion for characterizing MD-MPN, without losing specificity for its radiological diagnosis. IPMN is stratified into “high-risk stigmata” and “worrisome features” as a guide in managing these patients, either those with resection of the lesion or those under surveillance. While the recent guidelines help in managing patients with IPMN, various parameters stratifying the risk for malignancy are being constantly analyzed by the recent reports. In general, management of MD-PMN in surgically fit patients would warrant resection. However, in patients with BD-IPMN, a more conservative approach is practiced. The standard treatment for invasive IPMN would be pancreatectomy with lymph node dissection, while limited resection is appropriate for noninvasive lesions. The role of adjuvant therapy in invasive IPMN is evolving. The interval of surveillance, though controversial, would depend on the risk stratification. The overall 5-year survival of noninvasive IPMN is good, while in invasive carcinoma despite surgical resection, it is moderate. While significant progress has been made in the understanding of this relatively new pathology, with more quality research in the future, we would hopefully be close to achieving our goal in further understanding its pathology and determining the appropriate management.
Footnotes
Source of Support: Nil
Conflict of Interest: No conflict of interest, actual or potential including financial, personal, or for products mentioned in the manuscript.
References
- 1.Lafemena J, Katabi N, Klimstra D, Correa-Gallego C, Gaujoux S, Kingham TP, et al. Malignant progression in IPMN: A cohort analysis of patients initially selected for resection or observation. Ann Surg Oncol. 2013;20:440–7. doi: 10.1245/s10434-012-2702-y. [DOI] [PubMed] [Google Scholar]
- 2.Tanaka M, Fernández-del Castello C, Adsay V, Chari S, Falconi M, Jang JY, et al. International Association of Pancreatology. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–97. doi: 10.1016/j.pan.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Gourgitois S, Ridolfine MP, Germanos S. Intraductal papillary mucinous neoplasms of the pancreas. Eur J Surg Oncol. 2007;33:678–84. doi: 10.1016/j.ejso.2006.11.031. [DOI] [PubMed] [Google Scholar]
- 4.Hwang DW, Jang JY, Lee SE, Lim CS, Lee KU, Kim SW. Clinicopathologic analysis of surgically proven intraductal papillary mucinous neoplasms of the pancreas in SNUH: A 15-year experience at a single academic institution. Langenbecks Arch Surg. 2012;397:93–102. doi: 10.1007/s00423-010-0674-6. [DOI] [PubMed] [Google Scholar]
- 5.Larghi A, Panic N, Capurso G, Leoncini E, Arzani D, Salvia R, et al. Prevalence and risk factors of extrapancreatic malignancies in large cohort of patients with intraductal papillary mucinous neoplasms (IPMN) of the pancreas. Ann Oncol. 2013;24:1907–11. doi: 10.1093/annonc/mdt184. [DOI] [PubMed] [Google Scholar]
- 6.Bae SY, Lee KT, Lee JH, Lee JK, Lee KH, Rhee JC. Proper management and follow up strategy of branch duct intraductal papillary mucinous neoplasms of the pancreas. Dig Liver Dis. 2012;44:257–60. doi: 10.1016/j.dld.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Caponi S, Vasile E, Funel N, De Lio N, Campani D, Ginocchi L, et al. Adjuvant chemotherapy seems beneficial for invasive intraductal papillary mucinous neoplasms. Eur J Surg Oncol. 2013;39:396–403. doi: 10.1016/j.ejso.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Takanami K, Hiraide T, Tsuda M, Nakamura Y, Kaneta T, Takase K, et al. Additional value of FDG PET/CT to contrast-enhanced CT in differentiation between benign and malignant intraductal papillary mucinous neoplasms of the pancreas with mural nodules. Ann Nucl Med. 2011;25:501–10. doi: 10.1007/s12149-011-0494-y. [DOI] [PubMed] [Google Scholar]
- 9.Casteill F, Basetti D, Negrelli R, Di Paola V, Zantedeschi L, Ventriglia A, et al. Multifocal branch-duct intraductal papillary mucinous neoplasms (IPMNs) of the pancreas: Magnetic resonance (MR) imaging pattern and evolution over time. Radiol Med. 2013;118:917–29. doi: 10.1007/s11547-013-0945-8. [DOI] [PubMed] [Google Scholar]
- 10.Zhang J, Wang PJ, Yuan XD. Correlation between CT patterns and pathological classification of intraductal papillary mucinous neoplasm. Eur J Radiol. 2010;73:96–101. doi: 10.1016/j.ejrad.2008.09.035. [DOI] [PubMed] [Google Scholar]
- 11.Inoue H, Tsuchida A, Kawasaki Y, Fujimoto Y, Yamasaki S, Kajiyama G. Preoperative diagnosis of intraductal papillary-mucinous tumors of the pancreas with attention to telomerase activity. Cancer. 2001;91:35–41. doi: 10.1002/1097-0142(20010101)91:1<35::aid-cncr5>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 12.Kang KM, Lee JM, Shin CI, Baek JH, Kim SH, Yoon JH, et al. Added value of diffusion-weighted imaging to MR cholangiopancreatography with unenhanced MR imaging for predicting malignancy or invasiveness of intraductal papillary mucinous neoplasm of the pancreas. J Magn Reson Imaging. 2013;38:555–63. doi: 10.1002/jmri.24022. [DOI] [PubMed] [Google Scholar]
- 13.Jeurnink SM, Vleggaar FP, Siersema PD. Overview of the clinical problem: Facts and current issues of mucinous cystic neoplasms of the pancreas. Dig Liver Dis. 2008;40:837–46. doi: 10.1016/j.dld.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 14.Hirono S, Tani M, Kawai M, Okada K, Miyazawa M, Shimizu A, et al. The carcinoembryonic antigen level in pancreatic juice and mural nodule size are predictors of malignancy for branch duct type intraductal papillary mucinous neoplasms of the pancreas. Ann Surg. 2012;255:517–22. doi: 10.1097/SLA.0b013e3182444231. [DOI] [PubMed] [Google Scholar]
- 15.Piciucchi M, Crippa S, Del Chiaro M, Valente R, Pezzilli R, Falconi M, et al. Outcomes of intraductal papillary mucinous neoplasm with “Sendai-positive” criteria for resection undergoing non-operative management. Dig Liver Dis. 2013;45:584–8. doi: 10.1016/j.dld.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 16.Gupta R, Mortelé KJ, Tatli S, Girshman J, Glickman JN, Levy AD, et al. Pancreatic intraductal mucinous neoplasms: Role of CT in predicting pathologic subtypes. AJR Am J Roentgenol. 2008;191:1458–64. doi: 10.2214/AJR.07.3302. [DOI] [PubMed] [Google Scholar]
- 17.Moriya T, Traverso W. Fate of the pancreatic remnant after resection for an intraductal papillary mucinous neoplasm: A longitudinal level II cohort study. Arch Surg. 2012;147:528–34. doi: 10.1001/archsurg.2011.2276. [DOI] [PubMed] [Google Scholar]
- 18.Rebours V, Couvelard A, Peyroux JL, Sauvanet A, Hammel P, Ruszniewski P, et al. Familial intraductal papillary mucinous neoplasms of the pancreas. Dig Liver Dis. 2012;44:442–6. doi: 10.1016/j.dld.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 19.Furuta K, Watanabe H, Ikeda S. Differences between solid and duct-ectatic types of pancreatic ductal carcinomas. Cancer. 1992;69:1327–33. doi: 10.1002/1097-0142(19920315)69:6<1327::aid-cncr2820690605>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 20.Ohashi K, Murakami Y, Maruyama M, Takekoshi T, Ohta H, Ohashi I. Four cases of mucus-secreting pancreatic cancer. Prog Digest Endosc. 1982;20:348–51. [Google Scholar]
- 21.Itai Y, Ohhashi K, Nagai H, Murakami Y, Kokubo T, Makita K, et al. "Ductectatic" mucinous cystadenoma and cystadenocarcinoma of the pancreas. Radiology. 1986;161:697–700. doi: 10.1148/radiology.161.3.3786719. [DOI] [PubMed] [Google Scholar]
- 22.Sessa F, Solcia E, Capella C, Bonato M, Scarpa A, Zamboni G, et al. Intraductal papillary-mucinous tumours represent a distinct group of pancreatic neoplasms: An investigation of tumour cell differentiation and K-ras, p-53 and c-erbB-2 abnormalities in 26 patients. Virchows Arch. 1994;425:357–67. doi: 10.1007/BF00189573. [DOI] [PubMed] [Google Scholar]
- 23.Longnecker DS, Adler G, Hruban RH, Klo¨ppel G. Intraductal papillary mucinous neoplasms of the pancreas. In: Hamilton SR, Aaltonen LA, editors. World Health Organization Classification of Tumors. Lyon: IARC Press; 2000. pp. 237–41. [Google Scholar]
- 24.Kobari M, Egawa S, Shibuya K, Shimamura H, Sunamura M, Takeda K, et al. Intraductal papillary mucinous tumours of the pancreas comprise 2 clinical subtypes: Differences in clinical characteristics and surgical management. Arch Surg. 1999;134:1131–6. doi: 10.1001/archsurg.134.10.1131. [DOI] [PubMed] [Google Scholar]
- 25.Salvia R, Fernández-del Castillo C, Bassi C, Thayer SP, Falconi M, Mantovani W, et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: Clinical predictors of malignancy and long-term survival following resection. Ann Surg. 2004;239:678–87. doi: 10.1097/01.sla.0000124386.54496.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sohn TA, Yeo CJ, Cameron JL, Hruban RH, Fukushima N, Campbell KA, et al. Intraductal papillary mucinous neoplasms of the pancreas: An updated experience. Ann Surg. 2004;239:788–99. doi: 10.1097/01.sla.0000128306.90650.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Castellano-Megías VM, Andrés CI, López-Alonso G, Colina-Ruizdelgado F. Pathological features and diagnosis of intraductal papillary mucinous neoplasm of the pancreas. World J Gastrointest Oncol. 2014;6:311–24. doi: 10.4251/wjgo.v6.i9.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brat DJ, Lillemoe KD, Yeo CJ, Warfield PB, Hruban RH. Progression of pancreatic intraductal neoplasias to infiltrating adenocarcinoma of the pancreas. Am J Surg Pathol. 1998;22:163–9. doi: 10.1097/00000478-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Longnecker DS. Observations on the etiology and pathogenesis of intraductal papillary-mucinous neoplasms of the pancreas. Hepatogastroenterology. 1998;45:1973–80. [PubMed] [Google Scholar]
- 30.Sugiyama M, Atomi Y. Intraductal papillary mucinous tumors of the pancreas: Imaging studies and treatment strategies. Ann Surg. 1998;228:685–91. doi: 10.1097/00000658-199811000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roch AM, Ceppa EP, Al-Haddad MA, DeWitt JM, House MG, Zyromski NJ, et al. The natural history of main duct-involved, mixed-type intraductal papillary mucinous neoplasm: Parameters predictive of progression. Ann Surg. 2014 Oct;260(4):680–90. doi: 10.1097/SLA.0000000000000927. [DOI] [PubMed] [Google Scholar]
- 32.Kitagawa Y, Unger TA, Taylor S, Kozarek RA, Traverso LW. Mucus is a predictor of better prognosis and survival in patients with intraductal papillary mucinous tumor of the pancreas. J Gastrointest Surg. 2003;7:12–9. doi: 10.1016/S1091-255X(02)00152-X. [DOI] [PubMed] [Google Scholar]
- 33.Tanaka M. Intraductal papillary mucinous neoplasm of the pancreas: Diagnosis and treatment. Pancreas. 2004;28:282–8. doi: 10.1097/00006676-200404000-00013. [DOI] [PubMed] [Google Scholar]
- 34.Palmucci S, Trombatore C, Foti PV, Mauro LA, Milone P, Milazzotto R, et al. The utilization of imaging features in the management of intraductal papillary mucinous neoplasms. Gastroenterol Res Pract. 2014;2014:765451. doi: 10.1155/2014/765451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Inoue K, Ohuchida J, Ohtsuka T, Nabae T, Yokohata K, Ogawa Y, et al. Several localized stenosis and marked dilatation of the main pancreatic duct are indicators of pancreatic cancer instead of chronic pancreatitis on endoscopic retrograde balloon pancreatography. Gastrointest Endosc. 2003;58:510–5. doi: 10.1067/s0016-5107(03)01962-x. [DOI] [PubMed] [Google Scholar]
- 36.Maeshiro K, Nakayama Y, Yasunami Y, Furuta K, Ikeda S. Diagnosis of mucin-producing tumour of the pancreas by balloon-catheter endoscopic retrograde pancreatography - compression study. Hepatogastroenterology. 1998;45:1986–95. [PubMed] [Google Scholar]
- 37.Kubo H, Chijiiwa Y, Akahoshi K, Hamada S, Harada N, Sumii T, et al. Intraductal papillary-mucinous tumours of the pancreas: Differential diagnosis between benign and malignant tumours by endoscopic ultrasonography. Am J Gastroenterol. 2001;96:1429–34. doi: 10.1111/j.1572-0241.2001.03794.x. [DOI] [PubMed] [Google Scholar]
- 38.Park WG, Mascarenhas R, Palaez-Luna M, Smyrk TC, O'Kane D, Clain JE, et al. Diagnostic performance of cyst fluid carcinoembryonic antigen and amylase in histologically confirmed pancreatic cysts. Pancreas. 2011;40:42–5. doi: 10.1097/MPA.0b013e3181f69f36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cizginer S, Turner BG, Bilge AR, Karaca C, Pitman MB, Brugge WR. Cyst fluid carcinoembryonic antigen is an accurate diagnostic marker of pancreatic mucinous cysts. Pancreas. 2011;40:1024–8. doi: 10.1097/MPA.0b013e31821bd62f. [DOI] [PubMed] [Google Scholar]
- 40.Arnelo U, Siiki A, Swahn F, Segersvärd R, Enochsson L, del Chiaro M, et al. Single-operator pancreatoscopy is helpful in the evaluation of suspected intraductal intraductal papillary mucinous neoplasms (IPMN) Pancreatology. 2014;14:510–4. doi: 10.1016/j.pan.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 41.Wiesenauer CA, Schmidt CM, Cummings OW, Yiannoutsos CT, Howard TJ, Wiebke EA, et al. Preoperative predictors of malignancy in pancreatic intraductal papillary mucinous neoplasms. Arch Surg. 2003;138:610–8. doi: 10.1001/archsurg.138.6.610. [DOI] [PubMed] [Google Scholar]
- 42.van der Waaij LA, van Dullemen HM, Porte RJ. Cyst fluid analysis in the differential diagnosis of pancreatic cystic lesions: A pooled analysis. Gastrointest Endosc. 2005;62:383–9. doi: 10.1016/s0016-5107(05)01581-6. [DOI] [PubMed] [Google Scholar]
- 43.Jang JY, Kim SW, Ahn YJ, Yoon YS, Choi MG, Lee KU, et al. Multicenter analysis of clinicopathological features of intraductal papillary mucinous tumour of the pancreas: Is it possible to predict the malignancy before surgery? Ann Surg Oncol. 2005;12:124–32. doi: 10.1245/ASO.2005.02.030. [DOI] [PubMed] [Google Scholar]
- 44.Taouli B, Vilgrain V, Vullierme MP, Terris B, Denys A, Sauvanet A, et al. Intraductal papillary mucinous tumors of the pancreas: Helical CT with histopathologic correlation. Radiology. 2000;217:757–64. doi: 10.1148/radiology.217.3.r00dc24757. [DOI] [PubMed] [Google Scholar]
- 45.Kawamoto S, Horton KM, Lawler LP, Hruban RH, Fishman EK. Intraductal papillary mucinous neoplasms of the pancreas: Can benign lesions be differentiated from malignant lesions with multidetector CT? Radiographics. 2005;25:1451–70. doi: 10.1148/rg.256055036. [DOI] [PubMed] [Google Scholar]
- 46.Baba T, Yamaguchi T, Ishihara T, Kobayashi A, Oshima T, Sakaue N, et al. Distinguishing benign from malignant intraductal papillary mucinous tumors of the pancreas by imaging techniques. Pancreas. 2004;29:212–7. doi: 10.1097/00006676-200410000-00006. [DOI] [PubMed] [Google Scholar]
- 47.Sugiyama M, Atomi Y. Extrapancreatic neoplasms occur with unusual frequency in patients with intraductal papillary mucinous tumors of the pancreas. Am J Gastroenterol. 1999;94:470–3. doi: 10.1111/j.1572-0241.1999.879_h.x. [DOI] [PubMed] [Google Scholar]
- 48.Reid-Lombardo KM, Mathis KL, Wood CM, Harmsen WS, Sarr MG. Frequency of extrapancreatic neoplasms in intraductal papillary mucinous neoplasm of the pancreas: Implications for management. Ann Surg. 2010;251:64–9. doi: 10.1097/SLA.0b013e3181b5ad1e. [DOI] [PubMed] [Google Scholar]
- 49.Lee SY, Choi DW, Jang KT, Lee KT, Choi SH, Heo JS, et al. High expression of intestinal-type mucin (MUC2) in intraductal papillary mucinous neoplasms coexisting with extrapancreatic gastrointestinal cancers. Pancreas. 2006;32:186–9. doi: 10.1097/01.mpa.0000202939.40213.fd. [DOI] [PubMed] [Google Scholar]
- 50.Wu J, Matthaei H, Maitra A, Dal Molin M, Wood LD, Eshleman JR, et al. Recurrent GNAS mutations define an unexpected pathway for pancreatic cyst development. Sci Transl Med. 2011;3:92ra66. doi: 10.1126/scitranslmed.3002543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adsay NV, Merati K, Basturk O, Iacobuzio-Donahue C, Levi E, Cheng JD, et al. Pathologically and biologically distinct types of epithelium in intraductal papillary mucinous neoplasms: Delineation of an “intestinal” pathway of carcinogenesis in the pancreas. Am J Surg Pathol. 2004;28:839–48. doi: 10.1097/00000478-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 52.Sadakari Y, Ohuchida K, Nakata K, Ohtsuka T, Aishima S, Takahata S, et al. Invasive carcinoma derived from the nonintestinal type intraductal papillary mucinous neoplasm of the pancreas has a poorer prognosis than that derived from the intestinal type. Surgery. 2010;147:812–7. doi: 10.1016/j.surg.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 53.Adsay NV, Merati K, Andea A, Sarkar F, Hruban RH, Wilentz RE, et al. The dichotomy in the preinvasive neoplasia to invasive carcinoma sequence in the pancreas: Differential expression of MUC1 and MUC2 supports the existence of two separate pathways of carcinogenesis. Mod Pathol. 2002;15:1087–95. doi: 10.1097/01.MP.0000028647.98725.8B. [DOI] [PubMed] [Google Scholar]
- 54.Mino-Kenudson M, Fernández-del Castillo C, Baba Y, Valsangkar NP, Liss AS, Hsu M, et al. Prognosis of invasive intraductal papillary mucinous neoplasm depends on histological and precursor epithelial subtypes. Gut. 2011;60:1712–20. doi: 10.1136/gut.2010.232272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Adsay NV, Adair CF, Heffess CS, Klimstra DS. Intraductal oncocytic papillary neoplasms of the pancreas. Am J Surg Pathol. 1996;20:980–94. doi: 10.1097/00000478-199608000-00007. [DOI] [PubMed] [Google Scholar]
- 56.Hibi Y, Fukushima N, Tsuchida A, Sofuni A, Itoi T, Moriyasu F, et al. Pancreatic juice cytology and subclassification of intraductal papillary mucinous neoplasms of the pancreas. Pancreas. 2007;34:197–204. doi: 10.1097/MPA.0b013e31802dea0. [DOI] [PubMed] [Google Scholar]
- 57.Lüttges J, Zamboni G, Longnecker D, Klöppel G. The immunohistochemical mucin expression pattern distinguishes different types of intraductal papillary mucinous neoplasms of the pancreas and determines their relationship to mucinous noncystic carcinoma and ductal adenocarcinoma. Am J Surg Pathol. 2001;25:942–8. doi: 10.1097/00000478-200107000-00014. [DOI] [PubMed] [Google Scholar]
- 58.Kang MJ, Jang JY, Kim SJ, Lee KB, Ryu JK, Kim YT, et al. Cyst growth rate predicts malignancy in patients with branch duct intraductal papillary mucinous neoplasms. Clin Gastroenterol Hepatol. 2011;9:87–93. doi: 10.1016/j.cgh.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 59.Lévy P, Jouannaud V, O'Toole D, Couvelard A, Vullierme MP, Palazzo L, et al. Natural history of intraductal papillary mucinous tumors of the pancreas: Actuarial risk of malignancy. Clin Gastroenterol Hepatol. 2006;4:460–8. doi: 10.1016/j.cgh.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 60.Del Chiaro M, Verbeke C, Salvia R, Klöppel G, Werner J, McKay C, et al. European Study Group on Cystic Tumours of the Pancreas. European experts consensus statement on cystic tumours of pancreas. Dig Liver Dis. 2013;45:703–11. doi: 10.1016/j.dld.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 61.Roch AM, Ceppa EP, DeWitt JM, Al-Haddad MA, House MG, Nakeeb A, et al. International Consensus Guidelines parameters for the prediction of malignancy in intraductal papillary mucinous neoplasm are not properly weighted and are not cumulative. HPB (Oxford) 2014;16:929–35. doi: 10.1111/hpb.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Suzuki R, Thosani N, Annangi S, Guha S, Bhutani MS. Diagnostic yield of EUS-FNA-based cytology distinguishing malignant and benign IPMNs: A systematic review and meta-analysis. Pancreatology. 2014;14:380–4. doi: 10.1016/j.pan.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 63.Hruban RH, Takaori K, Klimstra DS, Adsay NV, Albores-Saavedra J, Biankin AV, et al. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2004;28:977–87. doi: 10.1097/01.pas.0000126675.59108.80. [DOI] [PubMed] [Google Scholar]
- 64.Longnecker DS, Adsay NV, Fernandez-del Castillo C, Hruban RH, Kasugai T, Klimstra DS, et al. Histopathological diagnosis of pancreatic intraepithelial neoplasia and intraductal papillary-mucinous neoplasms: Interobserver agreement. Pancreas. 2005;31:344–9. doi: 10.1097/01.mpa.0000186245.35716.18. [DOI] [PubMed] [Google Scholar]
- 65.Yamaguchi H, Shimizu M, Ban S, Koyama I, Hatori T, Fujita I, et al. Intraductal tubulopapillary neoplasms of the pancreas distinct from pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2009;33:1164–72. doi: 10.1097/PAS.0b013e3181a162e5. [DOI] [PubMed] [Google Scholar]
- 66.Lee KH, Lee SJ, Lee JK, Ryu JK, Kim EY, Kim TH, et al. Prediction of malignancy with endoscopic ultrasonography in patients with branch duct-type intraductal papillary mucinous neoplasm. Pancreas. 2014;43:1306–11. doi: 10.1097/MPA.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 67.Pitman MB, Genevay M, Yaeger K, Chebib I, Turner BG, Mino-Kenudson M, et al. High-grade atypical epithelial cells in pancreatic mucinous cysts are a more accurate predictor of malignancy than “positive” cytology. Cancer Cytopathol. 2010;118:434–40. doi: 10.1002/cncy.20118. [DOI] [PubMed] [Google Scholar]
- 68.Genevay M, Mino-Kenudson M, Yaeger K, Konstantinidis IT, Ferrone CR, Thayer S, et al. Cytology adds value to imaging studies for risk assessment of malignancy in pancreatic mucinous cysts. Ann Surg. 2011;254:977–83. doi: 10.1097/SLA.0b013e3182383118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jang JY, Kim SW, Lee SE, Yang SH, Lee KU, Lee YJ, et al. Treatment guidelines for branch duct type intraductal papillary mucinous neoplasms of the pancreas: When can we operate or observe? Ann Surg Oncol. 2008;15:199–205. doi: 10.1245/s10434-007-9603-5. [DOI] [PubMed] [Google Scholar]
- 70.Weinberg BM, Spiegel BM, Tomlinson JS, Farrell JJ. Asymptomatic pancreatic cystic neoplasms: Maximizing survival and quality of life using Markov-based clinical nomograms. Gastroenterology. 2010;138:531–40. doi: 10.1053/j.gastro.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Falconi M, Mantovani W, Crippa S, Mascetta G, Salvia R, Pederzoli P. Pancreatic insufficiency after different resections for benign tumours. Br J Surg. 2008;95:85–91. doi: 10.1002/bjs.5652. [DOI] [PubMed] [Google Scholar]
- 72.Warshaw AL, Rattner DW, Fernández-del Castillo C, Z'graggen K. Middle segment pancreatectomy: A novel technique for conserving pancreatic tissue. Arch Surg. 1998;133:327–31. doi: 10.1001/archsurg.133.3.327. [DOI] [PubMed] [Google Scholar]
- 73.Takeyoshi I, Ohwada S, Nakamura S, Ogawa T, Kawashima Y, Ikeya T, et al. Segmental pancreatectomy for mucin-producing pancreatic tumors. Hepatogastroenterology. 1999;46:2585–8. [PubMed] [Google Scholar]
- 74.Mizuta Y, Akazawa Y, Shiozawa K, Ohara H, Ohba K, Ohnita K, et al. Pseudomyxoma peritonei accompanied by intraductal papillary mucinous neoplasm of the pancreas. Pancreatology. 2005;5:470–4. doi: 10.1159/000086551. [DOI] [PubMed] [Google Scholar]
- 75.Gumbs AA, Grès P, Madureira FA, Gayet B. Laparoscopic vs. open resection of noninvasive intraductal pancreatic mucinous neoplasms. J Gastrointest Surg. 2008;12:707–12. doi: 10.1007/s11605-007-0311-z. [DOI] [PubMed] [Google Scholar]
- 76.Vijan SS, Ahmed KA, Harmsen WS, Que FG, Reid-Lombardo KM, Nagorney DM, et al. Laparoscopic vs open distal pancreatectomy: A single-institution comparative study. Arch Surg. 2010;145:616–21. doi: 10.1001/archsurg.2010.120. [DOI] [PubMed] [Google Scholar]
- 77.Kaneko T, Nakao A, Inoue S, Sugimoto H, Hatsuno T, Ito A, et al. Intraoperative ultrasonography by high-resolution annular array transducer for intraductal papillary mucinous tumors of the pancreas. Surgery. 2001;129:55–65. doi: 10.1067/msy.2001.109118. [DOI] [PubMed] [Google Scholar]
- 78.Cheon YK, Cho YD, Jeon SR, Moon JH, Jeong SW, Hur KY, et al. Pancreatic resection guided by preoperative intraductal ultrasonography for intraductal papillary mucinous neoplasm. Am J Gastroenterol. 2010;105:1963–9. doi: 10.1038/ajg.2010.169. [DOI] [PubMed] [Google Scholar]
- 79.Couvelard A, Sauvanet A, Kianmanesh R, Hammel P, Colnot N, Lévy P, et al. Frozen sectioning of the pancreatic cut surface during resection of intraductal papillary mucinous neoplasms of the pancreas is useful and reliable: A prospective evaluation. Ann Surg. 2005;242:774–80. doi: 10.1097/01.sla.0000188459.99624.a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.White R, D'Angelica M, Katabi N, Tang L, Klimstra D, Fong Y, et al. Fate of the remnant pancreas after resection of noninvasive intraductal papillary mucinous neoplasm. J Am Coll Surg. 2007;204:987–95. doi: 10.1016/j.jamcollsurg.2006.12.040. [DOI] [PubMed] [Google Scholar]
- 81.D'Angelica M, Brennan MF, Suriawinata AA, Klimstra D, Conlon KC. Intraductal papillary mucinous neoplasms of the pancreas: An analysis of clinicopathologic features and outcome. Ann Surg. 2004;239:400–8. doi: 10.1097/01.sla.0000114132.47816.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yamaguchi K, Ohuchida J, Ohtsuka T, Nakano K, Tanaka M. Intraductal papillary-mucinous tumor of the pancreas concomitant with ductal carcinoma of the pancreas. Pancreatology. 2002;2:484–90. doi: 10.1159/000064716. [DOI] [PubMed] [Google Scholar]
- 83.Hawes RH. The evolution of endoscopic ultrasound: Improved imaging, higher accuracy for fine needle aspiration and the reality of endoscopic ultrasound-guided interventions. Curr Opin Gastroenterol. 2010;26:436–44. doi: 10.1097/MOG.0b013e32833d1799. [DOI] [PubMed] [Google Scholar]
- 84.Gan SI, Thompson CC, Lauwers GY, Bounds BC, Brugge WR. Ethanol lavage of pancreatic cystic lesions: Initial pilot study. Gastrointest Endosc. 2005;61:746–52. doi: 10.1016/s0016-5107(05)00320-2. [DOI] [PubMed] [Google Scholar]
- 85.Oh HC, Seo DW, Lee TY, Kim JY, Lee SS, Lee SK, et al. New treatment for cystic tumors of the pancreas: EUS-guided ethanol lavage with paclitaxel injection. Gastrointest Endosc. 2008;67:636–42. doi: 10.1016/j.gie.2007.09.038. [DOI] [PubMed] [Google Scholar]
- 86.DeWitt J, McGreevy K, Schmidt CM, Brugge WR. EUS-guided ethanol versus saline solution lavage for pancreatic cysts: A randomized, double-blind study. Gastrointest Endosc. 2009;70:710–23. doi: 10.1016/j.gie.2009.03.1173. [DOI] [PubMed] [Google Scholar]
- 87.Oh HC, Seo DW, Kim SC, Yu E, Kim K, Moon SH, et al. Septated cystic tumors of the pancreas: Is it possible to treat them by endoscopic ultrasonography-guided intervention? Scand J Gastroenterol. 2009;44:242–7. doi: 10.1080/00365520802495537. [DOI] [PubMed] [Google Scholar]
- 88.Uehara H, Nakaizumi A, Ishikawa O, Iishi H, Tatsumi K, Takakura R, et al. Development of ductal carcinoma of the pancreas during follow-up of branch duct intraductal papillary mucinous neoplasm of the pancreas. Gut. 2008;57:1561–5. doi: 10.1136/gut.2007.145631. [DOI] [PubMed] [Google Scholar]
- 89.Sawhney MS, Devarajan S, O'Farrel P, Cury MS, Kundu R, Vollmer CM, et al. Comparison of carcinoembryonic antigen and molecular analysis in pancreatic cyst fluid. Gastrointest Endosc. 2009;69:1106–10. doi: 10.1016/j.gie.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 90.Koh YX, Chok AY, Zheng HL, Tan CS, Goh BK. Systematic review and meta-analysis comparing the surgical outcomes of invasive intraductal papillary mucinous neoplasms and conventional pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2014;21:2782–800. doi: 10.1245/s10434-014-3639-0. [DOI] [PubMed] [Google Scholar]
- 91.Shen J, Brugge WR, Dimaio CJ, Pitman MB. Molecular analysis of pancreatic cyst fluid: A comparative analysis with current practice of diagnosis. Cancer. 2009;117:217–27. doi: 10.1002/cncy.20027. [DOI] [PubMed] [Google Scholar]
- 92.Khalid A, Zahid M, Finkelstein SD, LeBlanc JK, Kaushik N, Ahmad N, et al. Pancreatic cyst fluid DNA analysis in evaluating pancreatic cysts: A report of the PANDA study. Gastrointest Endosc. 2009;69:1095–102. doi: 10.1016/j.gie.2008.07.033. [DOI] [PubMed] [Google Scholar]
- 93.Chari ST, Yadav D, Smyrk TC, DiMagno EP, Miller LJ, Raimondo M, et al. Study of recurrence after surgical resection of intraductal papillary mucinous neoplasm of the pancreas. Gastroenterology. 2002;123:1500–7. doi: 10.1053/gast.2002.36552. [DOI] [PubMed] [Google Scholar]
- 94.Gigot JF, Deprez P, Sempoux C, Descamps C, Metairie S, Gilneur D, et al. Surgical management of intraductal papillary mucinous tumors of the pancreas: The role of routine frozen section of the surgical margin, intraoperative endoscopic staged biopsies of the Wirsung duct, and pancreaticogastric anastomosis. Arch Surg. 2001;136:1256–62. doi: 10.1001/archsurg.136.11.1256. [DOI] [PubMed] [Google Scholar]


