Abstract
A case of trichilemmoma in continuity with a pigmented basal cell carcinoma is presented with dermatoscopy and dermatopathology. The distinction between the two lesions was evident dermatoscopically and was confirmed dermatopathologically. While trichilemmoma has been reported in association with basal cell carcinoma and dermatoscopy images of four previous cases of trichilemmoma have been published, no previous dermatoscopy image has been published of trichilemmoma associated with basal cell carcinoma.
Keywords: trichilemmoma, pigmented basal cell carcinoma, dermatoscopy, dermoscopy, dermatopathology
Case report
A 75-year-old male farmer presented to a primary care skin cancer practice in West Australia with a 6-month history of an enlarging painless lesion on his left cheek with no history of any possible precursor lesion. The patient was of Italian parentage with Fitzpatrick skin photo-type 3. There was a past history of treatment of two separate squamous cell carcinomas in-situ, one on the forehead and the other on an ear, in the previous two years. Other comorbidities included asthma, coronary heart disease, chronic obstructive pulmonary disease and arthritis. There was no history of nevus sebaceous and there was neither history nor clinical signs suggestive of Cowden’s syndrome.
Examination showed a single small non-pigmented nodular lesion located on the left cheek in continuation with a small, pigmented macular lesion (Figure 1).
Figure 1.

Clinical image of a focally pigmented nodular lesion on the left cheek of a 75-year-old man. [Copyright: ©2015 Al Kaptan et al.]
Dermatoscopy (Figure 2) revealed a raised pink lesion, 3.5 mm in diameter, with a radial arrangement of vessels peripherally, with centered blood vessels in the middle of the lesion, these vessels being centered in skin-colored clods. No keratin structures (keratin scale, white structureless areas or white circles) were seen. At one edge of this lesion, in direct contact with it, was a heavily pigmented flat lesion, 1 mm in diameter with a pattern of pigmented lines radial, converging (Figure 2).
Figure 2.
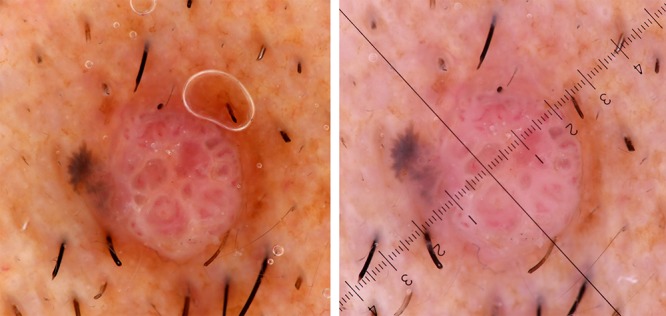
Dermatoscopy images (polarized left, non-polarized right) of the lesion shown in Figure 1. There is a focal pigmented macular component with lines radial converging and a larger non-pigmented nodule with a radial arrangement of vessels peripherally and a centered arrangement of vessels centrally. [Copyright: ©2015 Al Kaptan et al.]
The lesion was subjected to an excision biopsy with a 4 mm peripheral margin and submitted for dermatopathological evaluation.
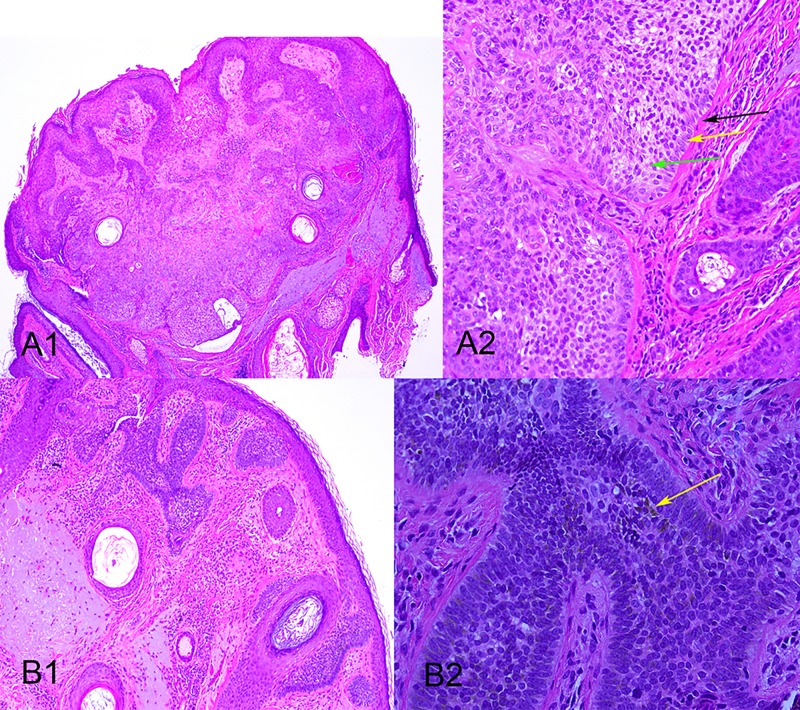
Dermatopathology (Figure 3) showed both the trichilemmoma and BCC (basal cell carcinoma) components. The trichilemmoma (Figure 3 A1 and A2) was a well-circumscribed, sharply demarcated lesion with surface papillomatosis, horn cysts and a degree of central desmoplasia. Under high power an eosinophilic mantle of thickened basement membrane, mimicking the outer root sheath of the hair follicle infundibulum, was seen. Peripheral palisading was evident adjacent to the basement membrane and extending from that there were clear cells which were banal cytologically, lacked mitosis or individual cell necrosis (apoptosis) and contained an abundant amount of glycogen within their cytoplasm.
Figure 3A and B.
Dermatopathology images of the lesion shown in figures 1 and 2. A1: Low power view of the trichilemmoma component showing a well-circumscribed, sharply demarcated lesion with surface papillomatosis, three horn cysts and a degree of desmoplasia centrally. A2: Higher power view) shows a thickened basement membrane (black arrow), peripheral palisading (yellow arrow) and clear cells (green arrow). B1: Low power view of the BCC component showing superficial BCC at the dermo-epidermal junction. B2: Higher power view of the BCC with low light, showing melanin pigment (arrow). [Copyright: ©2015 Al Kaptan et al.]
The BCC component (Figure 3 B1 and B2) showed superficial BCC at the dermo-epidermal junction. In the high power view melanin pigment could be seen.
Conclusions
Trichilemmoma is a benign tumor derived from the external sheath cells of pilosebaceous units [1] and desmoplastic trichilemmoma is a rare variant, which can present clinically with features suggesting invasive malignancy [2]. There has been controversy as to whether trichilemmomas are actually aged warts, this belief being proposed by well-known dermatopathologist Bernie Ackerman [3] but vigorously opposed by others including Marty Brownstein [4].
Basal cell carcinoma is a malignant tumor, of trichoblast differentiation but uncertain origin, although it is probably of follicular derivation [5], predilection for non-glabrous skin being consistent with this.
Trichilemmoma has previously been reported in association with BCC in the context of lesions arising in a preexisting nevus sebaceous [6,7]. In addition, three cases of desmoplastic trichilemmoma arising in association with BCC without a preexisting nevus sebaceous have been reported [8].
The dermatoscopy of four trichilemmomas has been reported [9,10] with images being presented for three of them [10]. In the first case reported, without a photograph, the dermatoscopic features were described as “keratin masses; perivascular whitish halos” [9]. The other three were reported together, with the first two described as having a hyperkeratotic central area with peripheral erythematous radial lines, the third having a “peripheral radiated red area.” All three were then presented as depicting what the authors called a “red iris like structure.” Examination of the photographs published in fact displayed a non-pigmented lesion in each case with a radial arrangement of vessels peripherally and structureless white centrally with some centred vessels [11].
In the case we report, the clinician interpreted the lesion as a pigmented lesion and assessed it using the chaos and clues decision-algorithm [12]. The lesion was regarded as chaotic (asymmetrical) with the clues of an eccentric structureless (pink) area as well as lines radial segmental, which lead to a clear decision to do an excision biopsy. The pathologist, as is often the case with esoteric lesions, was able to deliver the answer to which particular type of malignancy this was.
The dermatoscopic features of the trichilemmoma presented here are consistent with those published previously, with a radial pattern of vessels peripherally and centred vessels centrally. Association with a BCC is a previously reported, unusual variation, consistent with both lesions having hair-follicle derivation.
This case demonstrates the utility of using a decision algorithm in esoteric cases with the final diagnosis to be delivered by the gold standard of dermatopathology.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
All authors have contributed significantly to this publication.
References
- 1.Tsai J-H, Huang W-C, Jhuang J-Y, et al. Frequent activating HRAS mutations in trichilemmoma. Br J Dermatol. 2014;171(5):1073–77. doi: 10.1111/bjd.13143. [DOI] [PubMed] [Google Scholar]
- 2.Sano DT, Yang JJH, Tebcherani AJ, Bazzo LA de PM. A rare clinical presentation of Desmoplastic Trichilemmoma mimicking Invasive Carcinoma. An Bras Dermatol. 2014;89(5):796–98. doi: 10.1590/abd1806-4841.20143095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ackerman AB. Trichilemmoma. Arch Dermatol. 1978;114(2):286. [PubMed] [Google Scholar]
- 4.Brownstein MH. Trichilemmoma. Benign follicular tumor or viral wart? Am J Dermatopathol. 1980;2(3):229–31. doi: 10.1097/00000372-198000230-00006. [DOI] [PubMed] [Google Scholar]
- 5.Sellheyer K. Basal cell carcinoma: cell of origin, cancer stem cell hypothesis and stem cell markers. Br J Dermatol. 2011;164(4):696–711. doi: 10.1111/j.1365-2133.2010.10158.x. [DOI] [PubMed] [Google Scholar]
- 6.Wang Y, Bu W-B, Chen H, Zhang M-L, et al. Basal cell carcinoma, syringocystadenoma papilliferum, trichilemmoma, and sebaceoma arising within a nevus sebaceus associated with pigmented nevi. Dermatol Surg. 2011;37(12):1806–10. doi: 10.1111/j.1524-4725.2011.02163.x. [DOI] [PubMed] [Google Scholar]
- 7.Yoon DH, Jang IG, Kim TY, Kim HO, Kim CW. Syringocystadenoma papilliferum, basal cell carcinoma and trichilemmoma arising from nevus sebaceus of Jadassohn. Acta Derm Venereol. 1997;77(3):242–43. doi: 10.2340/0001555577242243. [DOI] [PubMed] [Google Scholar]
- 8.Crowson AN, Magro CM. Basal cell carcinoma arising in association with desmoplastic trichilemmoma. Am J Dermatopathol. 1996;18(1):43–8. doi: 10.1097/00000372-199602000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Lallas A, Moscarella E, Argenziano G, et al. Dermoscopy of uncommon skin tumours. Australas J Dermatol. 2014;55(1):53–62. doi: 10.1111/ajd.12074. [DOI] [PubMed] [Google Scholar]
- 10.Horcajada-Reales C, Avilés-Izquierdo JA, Ciudad-Blanco C, et al. Red iris-like structure. J Am Acad Dermatol. 2015;72(1 Suppl):S30–2. doi: 10.1016/j.jaad.2014.04.064. [DOI] [PubMed] [Google Scholar]
- 11.Rosendahl C, Cameron A, Tschandl P, et al. Prediction without Pigment: a decision algorithm for non-pigmented skin malignancy. Dermatol Pract Concept. 2014;4(1):9. doi: 10.5826/dpc.0401a09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosendahl C, Cameron A, McColl I, Wilkinson D. Dermatoscopy in routine practice— “chaos and clues”. Aust Fam Physician. 2012;41(7):482–87. [PubMed] [Google Scholar]