Abstract
Background:
The treatment of tinea capitis using radiotherapy was introduced at the beginning of the twentieth century. A variety of cancers including basal cell carcinoma (BCC) are seen years after this treatment.
Objective:
We sought to determine the clinical characteristics of BCCs among irradiated patients.
Methods:
The clinical records of all patients with BCC in a clinic in north of Iran were reviewed.
Results:
Of the 58 cases of BCC, 29 had positive history for radiotherapy in their childhood. Multiple BCCs were seen in 79.3% and 10.3% of patients with history and without history of radiotherapy, respectively.
Conclusions:
X-ray radiation is still a major etiologic factor in developing BCC in northern Iran. Patients with positive history for radiotherapy have higher rate of recurrence.
Keywords: basal cell carcinoma, radiotherapy, tinea capitis, Iran, Rasht
Introduction
“Primum no nocere!”—Hippocrates
Tinea capitis was a common disease in northern Iran, where the majority of population still resides in rural areas. The first effective antifungal agent, i.e., Griseofulvin, was introduced in 1959. Up that time, there was no therapy available for patients with tinea capitis except radiation therapy (RT).
It has been estimated that approximately 200,000 children worldwide received RT for tinea capitis [1]. There is no clear data on the number and method patients were treated in Iran, but regarding the poor hygienic status of people, it can be imagined that probably thousands of patients, mostly children, have been treated with radiotherapy. Unfortunately, many did not even have this privilege and were left untreated or had underwent non-efficient remedies. Here, I will take a historical look at the issue followed by analyzing the clinical characteristics of BCCs in irradiated patients.
Materials and methods
In a retrospective study, the clinical records of all patients with BCC were reviewed. Demographic details as well as clinical details and history of RT for treating tinea capitis was analyzed. Data were analyzed using SPSS and P-values less than 0.05 were considered significant.
Results
A total number of 69 patients with BCC were studied. The youngest one was a 27 years old man with Gorlin’s syndrome that was excluded from the study. Also, in 10 cases, the history for radiotherapy was not clear and therefore they were excluded from the study. Of the remaining 58 patients, there were 23 women and 35 men with an age range from 34 to 85 years (mean age 60 years). Twenty-nine out of 58 patients (50%) had positive history for RT in their childhood for treatment of tinea capitis. The demographic data of patients is shown in Table 1.
TABLE 1.
Demographic and clinical characteristics of patients.
| RT+ | RT− | P. Value | |
|---|---|---|---|
| Gender, no (%) | 29 | 29 | 0.104 |
| Female | 9 (31.0) | 14 (48.3) | |
| Male | 20 (69.0) | 15 (51.7) | |
|
| |||
| Age (mean) | 60.31±7.85 | 59.57±9.86 | 0.87 |
|
| |||
| Number of lesions | 0.0001 | ||
| Solitary, no (%) | 6 (20.7) | 26 (89.7) | |
| Multiple, no (%) | 23 (79.3) | 3 (10.3) | |
RT: Radiotherapy.
Statistical analysis using chi-square test and t-test showed no significant difference from the point of gender and age between those who had history of RT and those who had not such history. In those who had positive history for RT, 23 out of 29 (79.3%) had multiple BCCs. In 27 of them (93.1%), the site of involvement was scalp. Fifteen out of 29 (51.7%) had recurrent lesions in this group. In contrast, in the group with negative history for RT, only three patients (10.3%) had multiple BCCs, in only seven patients (24.1%), scalp was involved and only five patients (17.2%) had recurrent BCCs.
Discussion
Non-melanoma skin cancers are the most common malignancies in Iran, with an incidence of around 10–15 new cases per 100,000 of the population. BCC is the most common skin cancer and constitutes about three forth of all skin cancers in Iran [2,3]. Skin cancer, particularly BCC, presents a major problem for patients who have undergone irradiation for the treatment of tinea capitis. While ultraviolet radiation is the most common risk factor in BCC development, a significant number of the patients with BCC in northern Iran, are still those who had radiation therapy for treating their tinea capitis.
A bit of history!
Guilan is a province located in northern Iran, nowadays with a population of around three million. Guilan, with its humid climate and heavy rainfalls, is the center of rice and tea farms in Iran. During the early years of twentieth century, this province and its capital, Rasht, were the battlefield of civil wars and invasions by Russians and the British. At that time, diseases such as malnutrition, cholera, tuberculosis, malaria, typhoid, leprosy and skin infections were common in this region.
The American Presbyterian mission started its mission in Guilan in 1905, and the American Christian Hospital that was founded by this group was among the first hospitals made in Northern Iran circa 1917 and maybe the first hospital with X-ray facility (Figure 1). The major figure in this hospital was Dr. John Davidson Frame (1880–1942) who established the hospital and worked as a physician and surgeon in Rasht for about 37 years (Figure 2) [4,5].
Figure 1.

Medallion of American Mission Hospital in Iran [5] (Reproduced with permission).
Figure 2.

Dr. John Davidson Frame and nurses in front of American Hospital in Rasht [5] (Reproduced with permission).
The exact number of patients with tinea capitis who have been treated with radiotherapy in the American Christian Hospital and other centers in Guilan is unknown, but we as dermatologists are still seeing signs of radiotherapy-induced tumors today. Also, the dosage of RT was not clear, but the target dose was the induction of total depilation.
The cutaneous symptoms after radiation exposure are based on a combination of inflammatory processes and alteration of cellular proliferation as a result of a specific pattern of transcriptionally activated pro-inflammatory cytokines and growth factors. The entire complex is referred to as cutaneous radiation syndrome and its severity depends on several factors such as the radiation dose, radiation quality, individual radiation sensitivity, the extent of contamination and absorption and amount of skin exposed [6]. Clinical manifestations usually include a combination of hyper- and hypopigmentations, epidermal thinning and sclerosis (Figure 3).
Figure 3.
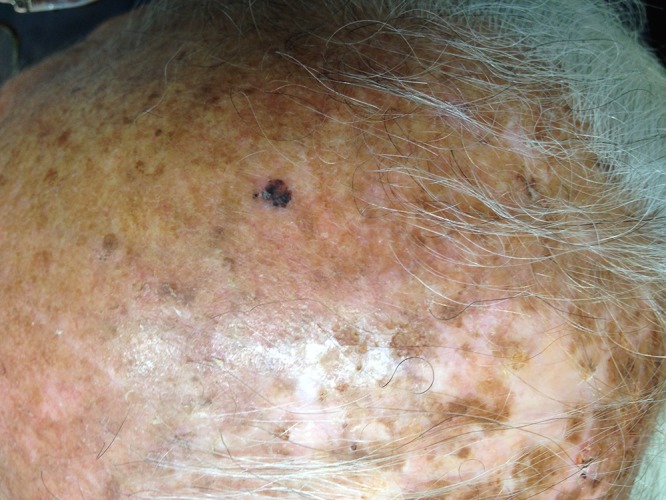
Basal cell carcinoma on the background of old radiodermatitis. [Copyright: ©2015 Zargari.]
In a study done by Shore et al on more than 2,000 children given X-ray therapy for tinea capitis at New York University Hospital, they found a relative risk (RR) of 3.6 for developing BCC in irradiated children [7], in 40% of whom the BCCs were multiple. Also, they found an inverse association between BCC risk and age of radiation exposure [7]. In another study, Ron et al compared 10,834 patients irradiated for tinea capitis in their childhood in Israel to a control group of 16,226, demonstrating an RR of 4.9 (95 % CI = 2.6–8.9) for BCC in the irradiated group [8].
The predominant type of BCC in our study was nodular type, which was in concordance with the study done in Tunis [9].
BCCs have been stratified as low-risk or high-risk according to their propensity for recurrence [10]. Our study revealed a greater risk for recurrence among those who have had history for radiation. Hassanpour et al compared the management and treatment characteristics of patients previously irradiated for tinea capitis as well as unexposed patients and found that the previously irradiated patients proved to be more difficult to treat, with more hospital admissions (P = 0.008), more operations (P = 0.01), and longer hospitalization period (P = 0.01) [11]. Risk factors considered include histologic subtype, horizontal diameter, anatomic location, and patient health status.
We believe that history of radiation should be considered as another independent risk factor for basal cell carcinoma in Iran. The reason for higher recurrence rate and more aggressive natural history of these tumors is as yet unexplained. A recent study has revealed that mitochondrial D-Loop instability is significantly higher in irradiated BCCs than in the nonirradiated ones [12]. On the other hand, a genetic study failed to demonstrate any genetic differences (specifically, difference in p53 and PTCH) between BCC in irradiated patients and BCC in non-irradiated patients [13]. Therefore, it seems that the natural history is more host-related than tumor-related. An interesting question is whether UV radiation and ionizing radiation have a synergistic effect.
This study is subject to several limitations. In addition to the problems inherent in any retrospective analysis, the sample size was small and lacking data on skin phototypes of patients and had no histopathologic comparison between the irradiated and non-irradiated patients.
Conclusions
This study shows that X-ray radiation for treating tinea capitis is a significant cause of BCC development in northern Iran. BCCs in those who had history of radiation have a more aggressive behavior with higher rate of recurrence.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
All authors have contributed significantly to this publication.
References
- 1.Cipollaro AC, Brodey A. Control of tinea capitis. NY State J Med. 1950;15:1931–4. 50. [PubMed] [Google Scholar]
- 2.Iraji F, Arbaby N, Asilian A, et al. Incidence of non-melanoma skin cancers in Isfahan. Iranian J of Dermatology. 2007;38:330–4. [Google Scholar]
- 3.Noorbala MT, Kafaie P. Analysis of 15 years of skin cancer in central Iran (Yazd) Dermatol Online J. 2007;13(4):1. 13. [PubMed] [Google Scholar]
- 4.Frame MA. Passage to Persia—Writings of an American Doctor During Her Life in Iran, 1929–1957. England: Summertime Publisher; 2014. [Google Scholar]
- 5.Taeb H. The Hospitals of Rasht. Iran: Nashr-e farhang-e Ilia; 2005. [Google Scholar]
- 6.Gottlöber P, Krähn G, Peter RU. Cutaneous radiation syndrome: clinical features, diagnosis and therapy. Hautarzt. 2000;51(8):567–74. doi: 10.1007/s001050051173. [DOI] [PubMed] [Google Scholar]
- 7.Shore RE, Moseson M, Xue X, et al. Skin cancer after X-ray treatment for scalp ringworm. Radiat Res. 2002;157(4):410–8. doi: 10.1667/0033-7587(2002)157[0410:scaxrt]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 8.Ron E, Modan B, Preston D, Alfandary E, et al. radiation-induced skin carcinomas of the head and neck. Radiat Res. 1991;125(3):318–25. [PubMed] [Google Scholar]
- 9.Mseddi M, Bouassida S, Marrekchi S, et al. Basal cell carcinoma of the scalp after radiation therapy for tinea capitis: 33 patients. Cancer Radiother. 2004;8(4):270–3. doi: 10.1016/j.canrad.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Sloane JR. The value of typing basal cell carcinomas in predicting recurrence after surgical excision. Br J Dermatol. 1977;96(2):127–33. doi: 10.1111/j.1365-2133.1977.tb12533.x. [DOI] [PubMed] [Google Scholar]
- 11.Hassanpour SE, Kalantar-Hormozi A, Motamed S, Moosavizadeh SM, Shahverdiani R. Basal cell carcinoma of scalp in patients with history of childhood therapeutic radiation: a retrospective study and comparison to nonirradiated patients. Ann Plast Surg. 2006;57(5):509–12. doi: 10.1097/01.sap.0000229002.09605.5d. [DOI] [PubMed] [Google Scholar]
- 12.Boaventura P, Pereira D, Mendes A, et al. Mithocondrial D310 D-Loop instability and histological subtypes in radiation-induced cutaneous basal cell carcinomas. J Dermatol Sci. 2014;73(3):31–9. doi: 10.1016/j.jdermsci.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Tessone A, Amariglio N, Weissman O, et al. Radiotherapy-induced basal cell carcinomas of the scalp: are they genetically different? Aesthetic Plast Surg. 2012;36(6):1387–92. doi: 10.1007/s00266-012-9969-z. [DOI] [PubMed] [Google Scholar]


