Abstract
Introduction
Although rare, the atrioesophageal fistula is one of the most feared complications in radiofrequency catheter ablation of atrial fibrillation due to the high risk of mortality.
Objective
This is a prospective controlled study, performed during regular radiofrequency catheter ablation of atrial fibrillation, to test whether esophageal displacement by handling the transesophageal echocardiography transducer could be used for esophageal protection.
Methods
Seven hundred and four patients (158 F/546M [22.4%/77.6%]; 52.8±14 [17-84] years old), with mean EF of 0.66±0.8 and drug-refractory atrial fibrillation were submitted to hybrid radiofrequency catheter ablation (conventional pulmonary vein isolation plus AF-Nests and background tachycardia ablation) with displacement of the esophagus as far as possible from the radiofrequency target by transesophageal echocardiography transducer handling. The esophageal luminal temperature was monitored without and with displacement in 25 patients.
Results
The mean esophageal displacement was 4 to 9.1cm (5.9±0.8 cm). In 680 of the 704 patients (96.6%), it was enough to allow complete and safe radiofrequency delivery (30W/40ºC/irrigated catheter or 50W/60ºC/8 mm catheter) without esophagus overlapping. The mean esophageal luminal temperature changes with versus without esophageal displacement were 0.11±0.13ºC versus 1.1±0.4ºC respectively, P<0.01. The radiofrequency had to be halted in 68% of the patients without esophageal displacement because of esophageal luminal temperature increase. There was no incidence of atrioesophageal fistula suspected or confirmed. Only two superficial bleeding caused by transesophageal echocardiography transducer insertion were observed.
Conclusion
Mechanical esophageal displacement by transesophageal echocardiography transducer during radiofrequency catheter ablation was able to prevent a rise in esophageal luminal temperature, helping to avoid esophageal thermal lesion. In most cases, the esophageal displacement was sufficient to allow safe radiofrequency application without esophagus overlapping, being a convenient alternative in reducing the risk of atrioesophageal fistula.
Keywords: Catheter Ablation, Esophagus, Esophageal Fistula, Atrial Fibrillation
Abstract
Introdução
Apesar de rara, a fístula átrio-esofágica é uma das complicações mais temidas na ablação por radiofrequência da fibrilação atrial pelo alto risco de mortalidade.
Objetivo
Este é um estudo prospectivo controlado, realizado durante a ablação por radiofrequência da fibrilação atrial regular, para testar se o deslocamento do esôfago ao manipular o transdutor de ecocardiografia transesofágica poderia ser usado para a proteção de esôfago.
Métodos
Setecentos e quatro pacientes (158 mulheres e 546 homens [22,4%/77,6%]; 52,8±14 [17-84] anos), com EF média igual a 0,66±0,8 e com fibrilação atrial refratária ao tratamento medicamentoso, foram submetidos à terapia híbrida com ablação por radiofrequência (isolamento convencional das veias pulmonares e ninhos de fibrilação atrial e ablação de taquicardia de background) com deslocamento do esôfago o mais longe possível do alvo da radiofrequência por manuseio do transdutor de ecocardiografia transesofágica. A temperatura luminal esofágica foi monitorada com e sem deslocamento em 25 pacientes.
Resultados
O deslocamento esofágico significativo foi de 4 a 9,1 centímetros (5,9±0,8 cm). Em 680 dos 704 pacientes (96,6%), isso foi o suficiente para permitir a entrega completa e segura de radiofrequência (30W/40ºC/cateter irrigado ou 50W/60ºC/cateter de 8 milímetros) sem sobreposição do esôfago. As alterações médias de temperatura luminal esofágica com e sem deslocamento de esôfago foram de 0,11±0,13ºC versus 1,1±0,4ºC, respectivamente, P<0,01. A radiofrequência teve que ser interrompida em 68% dos pacientes sem deslocamento de esôfago devido ao aumento da temperatura luminal esofágica. Não houve nenhum caso, suspeito ou confirmado, de fístula átrio-esofágica. Foram observados apenas dois sangramentos superficiais causados por inserção do transdutor de ecocardiografia transesofágica.
Conclusão
O deslocamento mecânico do esôfago pelo transdutor de ecocardiografia transesofágico durante a ablação com radiofrequência foi capaz de impedir o aumento da temperatura luminal esofágica, ajudando a evitar lesão térmica. Na maioria dos casos, o deslocamento esofágico foi suficiente para permitir a aplicação segura de radiofrequência sem sobreposição do esôfago, sendo uma alternativa conveniente para reduzir o risco de fístula átrio-esofágica.
| Abbreviations, acronyms & symbols | |
|---|---|
| AF | Atrial fibrillation |
| AEF | Atrioesophageal fistula |
| ED | Esophageal displacement |
| EF | Ejection fraction |
| ELT | Esophageal luminal temperature |
| LA | Left atrium |
| LAO | Left anterior oblique |
| PA | Postero-anterior |
| PV | Pulmonary vein |
| RAO | Right anterior oblique |
| RF | Radiofrequency |
| RFA | Radiofrequency catheter ablation |
| TET | Transesophageal echocardiography transducer |
INTRODUCTION
Radiofrequency (RF) catheter ablation of atrial fibrillation (AF) has been the most widely used method to retrieve sinus rhythm when AF is refractory to drug therapy. During ablation there is a risk of thermal damage of the esophagus due to its proximity and contact with the left atrium[1] (Figure 1). The most feared complication is atrioesophageal fistula[2-4], whose low but worrisome occurrence has been estimated to be <1%[5,6]. However, its true incidence is certainly unknown since there is no systematic report of this complication. A recent study of esophagogastroscopy performed in 28 patients 24 hours after catheter ablation without control of the esophagus position showed that 47% and 18% of the patients had esophageal lesions compatible with superficial thermal injury and necrosis or ulcer, respectively[7].
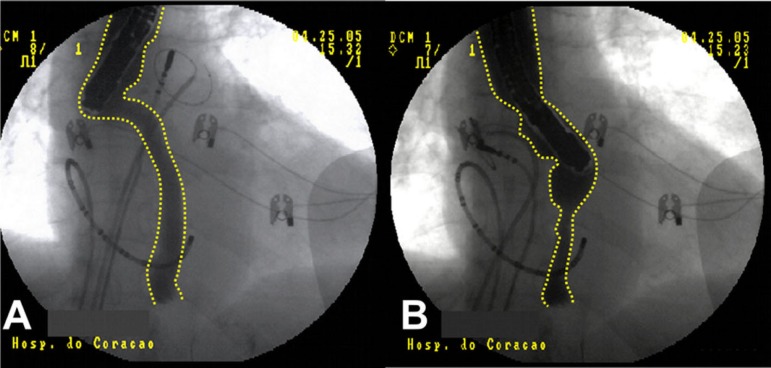
Fig. 1.
Cardiac computed tomography with esophagus visualization in RAO, PA and LAO, respectively, from left to right. There is a large contact area between the esophagus and the left atrium. This anatomical relationship can easily explain the risk of thermal injury of the esophagus during endocardial left atrial ablations. RAO=right anterior oblique; PA=postero-anterior; LAO=left anterior oblique
Technical developments in catheter ablation of AF have seen increasing use of high power large surface catheters (8 mm) and high power transfer systems (irrigated catheters) in left atrium regions that have great contact with the esophagus (pulmonary veins antrum and LA posterior wall). In addition, the use of long and even confluent LA block lines has been a common practice[8]. These aspects make the risk of esophageal injury highly prevalent. The main problem is that atrioesophageal fistula, in spite of being rare, is extremely serious with a high risk of mortality from stroke, mediastinitis, sepsis, and endocarditis. It is caused by conductive heat transfer to the esophagus with trans-mural necrosis[9,10] and possible participation of ischemia because of circulation and damage to esophageal innervation.
These considerations justify extreme caution during catheter ablation of AF in order to avoid esophageal lesion. Cooling esophageal protection systems are being developed to prevent thermal damage during ablation[11]. Several thermal monitoring[12] and esophagus location systems have been described to avoid RF release in risk areas, reducing the power applied in these places. However, energy restriction can lead to incomplete ablation, increasing its risk of failure. On the other hand, as the esophagus has great spontaneous motility, its pre-procedure location has little value and continuous monitoring is required[13,14].
As we regularly use transesophageal echocardiography (TEE) throughout catheter ablation of AF, we proposed that the TEE transducer could be regularly employed to divert the esophagus out of the ablation area and, in January 2005, we started this prospective study to test its possible benefits (Figura 2).
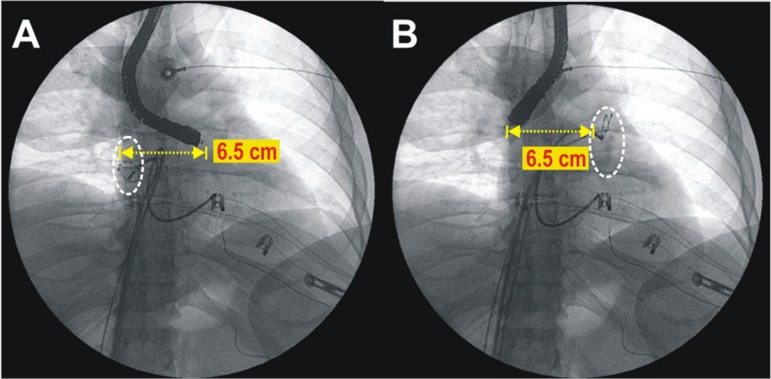
Fig. 2.
Lateral displacement of the esophagus usually obtained during transesophageal echocardiography. In this case the total displacement was 6.5 cm, allowing isolation of the the pulmonary vein (white circles) on each side with a good distance from the esophagus.
Objective
The objective of this study was to test the hypothesis that controlled deflection of the TEE transducer could meet two major aims:
1. Divert the esophagus out of the area to be ablated in order to avoid heating; and
2. Keep the esophagus stable in a well-known fixed position, avoiding an undesirable and unexpected interposition in the ablation area due to its natural motility.
This is a prospective study of regular clinical application. The purpose of this article is to show the results and discuss details and limitations of this technique after 6 years of systematic employment and follow-up.
METHODS
Seven hundred and four patients (158 female and 546 male [22.4%/77.6%]; mean±SD age, 52.8±14 [17 to 84] years) with drug-refractory AF (314 paroxysmal [44.6%], 332 persistent [47.2%], and 58 permanent [8.2%]) and treated by catheter RF endocardial ablation were included. Most patients (425, 60.4%) had no significant heart disease, with mean EF of 0.66±0.8 (0.3 to 0.8). In most cases, the LA diameter was either normal or slightly increased (39.9±6.8 mm) (Table 1).
Table 1.
Main features of 704 patients included in this study.
| N | 704 | Range or % | |
|---|---|---|---|
| Age (years) | 52.8±13.8 | 17 to 84 | |
| Female/Male | 158/546 | 22.4% /77.6% | |
| Weight (Kg) | 82.5±15.8 | 42 to 145 | |
| Atrial Fibrillation | Paroxysmal | 314 | 44.6% |
| Persistent | 332 | 47.2% | |
| Permanent | 58 | 8.2% | |
| With/Without Cardiopathy | 279/425 | 39.6% / 60.4% | |
| Left Atrium diameter (mm) | 39.9±6.8 | 25 to 60 | |
| Ejection fraction | 0.66±0.8 | 0.3 to 0.8 | |
| RF shots | 70.5±18.9 | 40 to 120 | |
| X-ray duration (min) | 60.6±21.1 | 10 to 99 | |
| Number of sessions | 1.16 ±0.4 | 1 to 4 | |
| Max Esophageal displacement (cm) | 5.9±0.8 | 4 to 9.1 |
Methodology
In every cases, catheter RF ablation of AF was performed in both atria, the LA being reached by trans-septal access. A hybrid technique was used with pulmonary veins isolation[8,15,16], AF-Nests ablation[17-19] mapping, and ablation of the background tachycardia[20]. The St Jude Navx System was employed for electroanatomic 3D mapping. Patients using oral anticoagulants had the prothrombin time adjusted before the procedure (target INR ≤ 1.6). Conventional surface ECG monitoring, adhesive defibrillation patches, mechanical ventilation with intravenous or inhalation general anesthesia in addition to the placement of TEE transducer were used. After having confirmed absence of intracardiac thrombus, four right femoral vein punctures were performed and a duodecapolar catheter was placed into coronary sinus. Trans-septal puncture was used in order to introduce both an ablation and a circular catheter in the left atrium. The following additional equipment was used: Cicero anaesthesia system (Dräger); multiparameter HP/Philips M1026A monitor; HP/Philips Sonos-2500 echocardiograph; 32 channels TEB polygraph with software for spectral analysis (Pachón-TEB); computerized spectrometer (Pachón®) for real-time spectral analysis, Siemens digital radioscopy; Medtronic, Biotronik and Irvine RF generator; Philips Heartstart biphasic XL defibrillator with trans-cutaneous pacemaker and cerebral activity spectrometer (BIS). The ablations were carried out by using 8 mm catheter Blazer EPT, Medtronic Conductor and Johnson Irrigated. Activated clotting time was attained between 300 and 400 s by IV Heparin infusion. All the patients included in the study accepted the procedure being made aware of the methodology and potential complications, having signed the written informed consent.
Esophageal Displacement and Ablation
After obtaining a three-dimensional LA model with Navx system by handling the TEE, the esophagus was shifted and kept into the rightmost position before the ablation of the left half of LA (left pulmonary veins isolation and AF-Nests ablation). Afterwards, the TEE transducer was handled again in order to shift the esophagus to the leftmost location. Ablation of the half right of the LA was then performed. All positions were photographed in order to get accurate esophageal displacement measurements. In the final ablation phase, in cases with LA background tachycardia, the esophagus was again shifted far from the ablation sites. At any time, at operator discretion before turning the RF on, the esophagus was manipulated by the TEE transducer in order to keep it as far as possible from the RF delivery point.
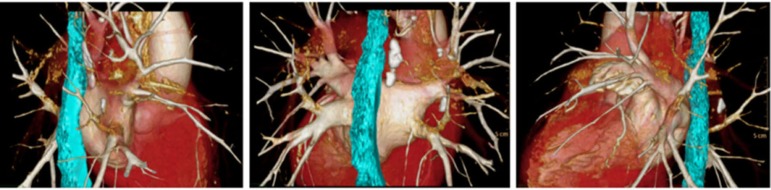
Esophageal Temperature Monitoring versus Displacement
A group of 25 patients were also studied to see the effects of displacement in the esophageal luminal temperature (ELT). They had an esophageal probe and thermometer additionally inserted. In these cases the esophagus was contrasted with barium and ELT was monitored during the ablations, before and after displacements. With the esophagus in the natural position, since the esophageal thermometer was in a good site (Figure 3) and whenever a ≥ 1ºC ELT was observed, the ablation was immediately halted and the esophagus was quickly shifted.
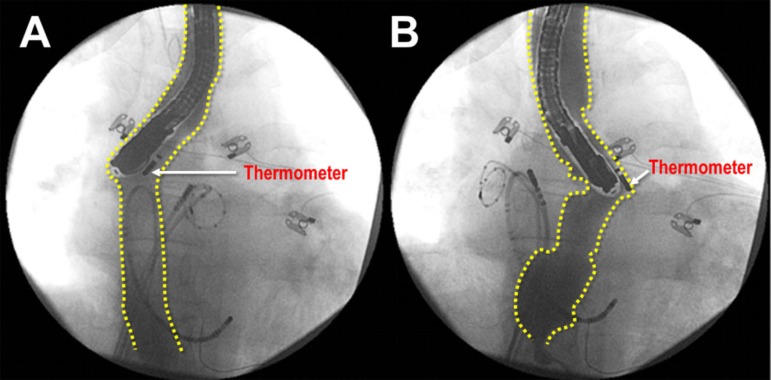
Fig. 3.
Barium esophagography showing esophageal displacement during RF catheter ablation of AF. In A, the thermometer position is satisfactory; however, in B, the thermometer is misplaced and should not be considered for temperature control of the ablation. The yellow dotted lines show the esophageal lumen contour. Enough bilateral esophageal displacement can also be observed, allowing safe ablation. AF=atrial fibrilation; RF=radiofrequency
Esophageal Endoscopy after Ablation
After ablation the patients were kept in the hospital under strict clinical monitoring for two days. Esophageal endoscopy was indicated whenever there was any symptom or sign of esophageal discomfort or lesion.
Medication after Ablation
Proton pump blockers were not used unless the patient was taking it prior to the ablation. During the first 3 months, in all cases, antiarrhythmic medication (amiodarone, propafenone or beta blockers) was used depending on the patient's tolerance. Anticoagulation was strictly established for at least 2-3 months using warfarin (INR = 2 to 3) or dabigatran.
RESULTS
The anatomical course of the esophagus was quite variable. In 22.2% of the patients, it was centralized; however, in 57.5% and 20.3% of the patients, it was diverted near or superimposed onto the left or right pulmonary veins (Figures 4 and 5), respectively. In all cases, it was possible to achieve mechanical esophageal displacement. For safety reasons, the displacement was applied even in cases with centered esophagus. Displacement ranged from 4 to 9.1 cm (5.9±0.8 cm). In 680 of the 704 patients (96.6%), the displacement was large enough to allow RF delivery with reasonable safety, even in the LA posterior wall (30W/40ºC/irrigated catheter or 50W/60ºC/8 mm catheter). For ablation of the LA posterior wall, the TEE transducer depth was modified as needed for each case. In 24 cases (3.4%), the esophagus had reduced and difficult mobility or allowed only one-way displacement, as seen in Figures 4 and 5. However, with stepwise handling, it was possible to obtain reasonable segmental displacement to get safe RF delivery in most areas of the pulmonary veins, although not completely sufficient for extensive treatment of the posterior LA wall.
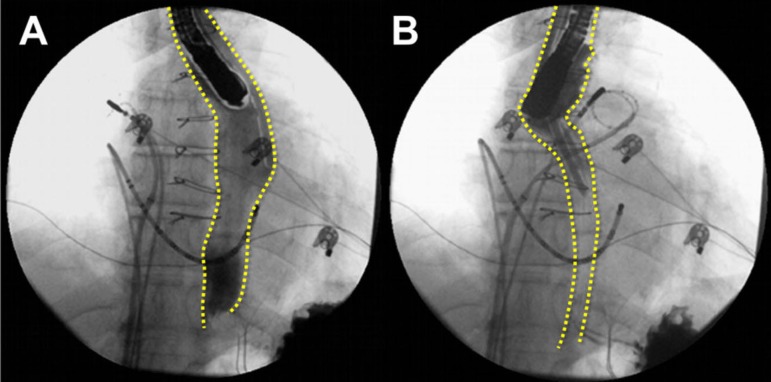
Fig. 4.
Esophagus positioned on the left at rest showing some restriction to be moved. Nevertheless, there was enough displacement for treating left pulmonary vein. In such cases, the barium esophagography is helpful to define the real esophagus boundaries and to show the extension of the displaced segment.
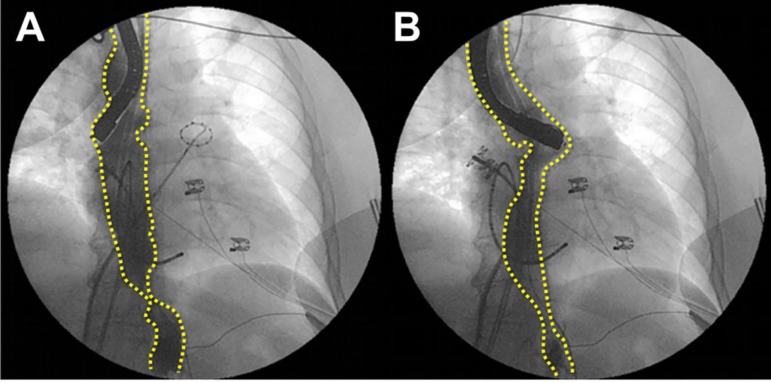
Fig. 5.
This patient had an old phrenic palsy and the esophagus was adhered to the same side showing restriction to be displaced to the left. However, enough displacement was achieved for right pulmonary vein ablation. Again, barium esophagography was helpful to define the real esophagus borders and to show the extension of the displaced segment.
In the whole group there was neither a case nor a suspicion of atrioesophageal fistula (mean follow-up of 37.9±81.9 months). Eight patients underwent esophageal endoscopy due to symptoms, with two of them showing slight bleeding. The investigation revealed normal esophagus in six of the eigh patients. The two cases with bleeding had superficial linear lesions in the high esophagus portion (above the atrial level), without signs of burning or necrosis. They were related to mechanical injury caused by introduction of the TEE transducer. Although small and superficial, the bleeding was certainly increased by anticoagulation. In both cases, the bleeding was promptly stopped with topic 1:1000 adrenaline solution. No cases presented symptoms compatible with injury to the periesophageal nerve plexus. There was no occurrence of ileus palsy or pylori spasm.
Study of Esophageal temperature versus Displacement
The results of 25 patients having ELT monitored without and with mechanical esophageal displacement are displayed in Table 2.
Table 2.
ELT changes with and without esophageal displacement. In 19/25 (76%) patients the RF was interrupted due to ELT increase > 1ºC during one RF delivery at least.
| N | 25 | Range/% | P |
|---|---|---|---|
| Age (years) | 58.5±10.5 | 33 to 73 | |
| Female/Male | 8/17 | 32%/68% | |
| Weight (Kg) | 78.3±14.3 | 52 to 101 | |
| Atrial Fibrillation | Paroxysmal 6 | 24% | |
| Persistent 17 | 68% | ||
| Permanent 2 | 8% | ||
| With/Without Cardiopathy | 9/16 | 36%/64% | |
| Left atrium diameter (mm) | 40.9±8.3 | 29 to 59 | |
| Ejection fraction | 0.66±0.9 | 0.37 to 0.79 | |
| RF shots | 70.1±13.8 | 44 to 99 | |
| X-ray duration (min) | 65.1±16.5 | 28 to 99 | |
| Number of sessions | 1.2±0.5 | 1 to 3 | |
| max Esophageal displacement (cm) | 6.1±1.3 | 4.5 to 9.2 | |
| max ∆ T with displacement (theC) | 0.11±0.13 | 0 to 0.5 | P<0.01 |
| max ∆ T without displacement (theC) | 1.3±0.5 | 0 to 2 | |
| ∆T > 1ºC without displacement | 19/25 | 76% | P<0.01 |
| ∆T > 1ºC with displacement | 0 | 0% |
ELT=esophageal luminal temperature; RF=radiofrequency
DISCUSSION
Several techniques have been proposed for esophageal protection during catheter ablation of AF. Any alternative limiting the amount or the sites of RF delivery increases the rate of ablation failure. Techniques have been used for:
Locating the esophagus before and/or during ablation;
Monitoring esophageal temperature;
Limitating RF energy or sites;
Esophageal cooling; and
Esophageal displacement.
The esophagus location before ablation has been held with barium contrast radiography, computed tomography (Figure 1), MRI or electroanatomical 3D mapping[21]. These techniques allow a fairly accurate location, but with more or less information on the extent of the contact between the LA and the esophagus. The main disadvantages are spontaneous change of esophagus position and the need of reducing the RF energy in overlapping regions that can lead to incomplete ablation.
The esophagus location during ablation has been determinated through contrast with barium, intracardiac echocardiography[22], and electroanatomical 3D mapping[23]. These methods have the great advantage of showing the actual position of the esophagus during ablation, but also limit RF delivery in overlapping areas. Therefore, if a AF relapse occurs due to restriction of RF energy release, the problem will persist in the same area in case of reablation[24].
Esophageal temperature monitoring during ablation[12] is another option, but it does not completely prevent complications because the thermometer can be located outside the point of greatest heat and, in addition, there is the problem of thermal latency of the esophagus[25]. Studies have shown low correlation between the total energy delivered in LA and LET increase[25,26]. Furthermore, heating of the esophagus restricts RF, delivery bringing out the problem of incomplete ablation.
A quite creative technique is placing a cooled balloon irrigated with saline solution inside the esophagus[27,28]. However, more detailed studies need to be conducted to verify whether anterior displacement caused by esophageal balloon insufflation could be an additional problem, thereby reducing its potential benefits.
Several techniques have advocated esophagus protection by reducing the RF power in overlapping areas. So far, there is no evidence based on guidelines defining the limits of RF energy. Speculative recommendations suggest that RF energy in overlapping areas of the esophagus should be <20W for less than 20 seconds and there should be at least 180 sec between two successive RF applications. However, the disadvantage is that even when well-implemented, incomplete and insufficient ablation may predispose to relapse.
In this study, it was possible to demonstrate that the esophagus has a large motility. If on the one hand this feature is a disadvantage due to the risk of unexpected esophageal interposition in the RF focus, on the other hand, it allows it to be mechanically displaced away from the point of RF application reducing the risk of thermal injury and atrioesophageal fistula (Figure 2). Additionally, mechanical esophageal displacement by using the TEE transducer, allows it to keep it stable and far from the RF application site. Since January 2005, we have regularly used this feature in any LA ablation as an indispensable requirement for ablation (Figure 6). Similar experience has been published supporting our observations and strengthening the idea that controlled esophageal displacement could be employed as a protection against thermal lesions[29,30].
Fig. 6.
Good esophageal displacement allowing large bilateral antrum ablation.
The extent of displacement depends on several factors such as constitutional characteristics, thorax size, patient age, presence of adhesions and/or esophageal pathologies, operator experience, transducer mobility, etc. In this study, the displacement of the esophagus ranged from 4 to 9.1 cm (5.9±0.8 cm). This allowed for secured visualized RF application (keeping a safe distance from the RF application site) in 690 patients (98.1%). Only 14 cases (1.9%) had very low esophageal mobility and a careful displacement for each pulmonary vein ablation was needed. In these cases, despite having enough displacement to ablate the pulmonary veins antrum, it was not possible to safely apply RF to the posterior LA wall.
Besides visual control of the esophageal displacement, 25 patients underwent concomitant monitoring of ELT (Figure 3). The RF was then applied with and without esophageal displacement. With displacement, it was not necessary to halt the RF energy whereas without displacement, the RF energy had to be stopped in 17 patients (68%) due to ELT increase of ≥1ºC. In addition, it was found that the esophageal displacement was able to reduce 10.9 times the ELT range (∆ELT = 0.11±0.13ºC with versus 1.2±0.5ºC without displacement, P<0.01) (Table 2). We decided to stop the RF early in case of a slight ELT (<1ºC) increase because of the thermal esophageal that could raise the temperature even after RF interruption[31]. This behavior decreases the ELT control effectiveness in preventing the esophageal thermal lesion. ELT sensitivity to safely detect esophageal warming is questionable because there is low correlation between the total amount of energy released in the left atrium and the final increase of ELT[25,26]. Moreover, the slow cooling of the esophagus is another particularity that cannot be neglected. This feature increases the risk of thermal damage due to the cumulative effect in temperature caused by RF applications in areas relatively near as described by Pappone et al.[4]. These authors identified that ablation confluent line blocks are high-risk critical areas for the formation of atrioesophageal fistulas.
One problem observed in this study was the potential risk of mechanical trauma of the oropharynx and upper esophagus during the introduction of the TEE transducer, causing bleeding that was intensified by anticoagulation. These observed cases were easily treated with topic application of adrenaline solution during diagnostic endoscopy. This complication occurred at the beginning of the learning curve. Based on this experience, the TEE transducer insertion procedure was changed, with more appropriate lubrication and careful handling being applied. As a result, this complication was no longer observed.
The TEE transducer should never be advanced inside the esophagus with pronounced angulation. It is important to move it with extreme care. Its position must be changed often to avoid forcing it in a single point for a long time. It could cause an ischemic injury to the esophageal mucosa.
Study and Method Limitations
Active and controlled esophagus displacement during catheter RF of AF ablation seems to be able to prevent esophageal temperature increase as well as esophageal thermal lesions. However, it depends on the use of the TEE transducer throughout the procedure. This may be considered a limitation for some services, but in our methodology, it becomes an advantage as we regularly use the TEE to replace the useful but more expensive intracardiac echocardiogram.
The insertion of TEE transducer depends on good sedation or general anesthesia, thus many services that perform AF ablation with a conscious patient or with superficial sedation may have difficulty employing this technique. The insertion process must be performed with additional care because since the patient will be anti-coagulated any mucosal trauma may cause significant bleeding.
Due to its significant diameter (11 mm), the TEE transducer may be considered a disadvantage as it forces the esophageal wall to the atrium, reducing the postero-anterior dimension of the LA. This could reduce the space for ablation, favoring esophageal heating. However, the proposal is to bend the transducer in order to maintain the esophagus as far as possible from the ablation site with minimal overlapping of the transducer and the LA.
One limitation of this study is that endoscopy was performed only in a few symptomatic cases. Since this is a prospective study of regular clinical application, though, it would be inconvenient and ethically questionable to perform an additional semi-invasive procedure in asymptomatic patients. This must be achieved through a randomized study. Nevertheless, the high number of cases treated without any occurrence of clinical esophageal lesion is a highly positive finding. Furthermore, the study of 25 patients undergoing ablation with ELT monitoring showed the high efficacy of this method for preventing esophageal temperature increase.
Sometimes, malposition and low mobility of the esophagus may limit the application of this technique; however, the experience of this study shows that these cases are rare.The presence of the TEE transducer and, especially, the barium in the esophagus may reduce the radiological visibility in some degree. Currently, we have used barium only in cases with difficult esophagus displacement.
CONCLUSION
Mechanical esophageal displacement using the TEE transducer during catheter RF ablation of AF was able to prevent a rise in esophageal intraluminal temperature, helping to avoid esophageal thermal lesion. In the absolute majority of cases the displacement of the esophagus was sufficient to allow the RF application in a visually safe condition. The absence of symptoms of esophageal lesions, the absence of injury to the peri-esophageal nerve plexus in a large number of patients, and the simplicity and low cost of the procedure suggest that this technique is a valuable alternative in reducing the risk of atrioesophageal fistula.
| Authors' roles & responsibilities | |
|---|---|
| JCPM | Analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; design and study design; conduct of the operations and/or experiments; writing of the manuscript or critical review of its content |
| EIPM | analysis and/or interpretation of data; statistical analysis; final approval of the manuscript; design and study design; conduct of the operations and/or experiments; writing of the manuscript or critical review of its content |
| TGSP | Conduct of operations and/or experiments |
| TJL | Conduct of operations and/or experiments |
| JCPM | Conduct of operations and/or experiments |
| RNAV | Conduct of operations and/or experiments |
| CTCP | Analysis and/or interpretation of data; conduct of the operations and/or experiments |
| JCZA | Conduct of operations and/or experiments |
Footnotes
This study was carried out at Instituto Dante Pazzanese (IDPC), Hospital do Coração Hcor, University of São Paulo Medical School, São Paulo, SP, Brazil.
No financial support
REFERENCES
- 1.Tsao HM, Wu MH, Higa S, Lee KT, Tai CT, Hsu NW, Chang CY, et al. Anatomic relationship of the esophagus and left atrium: implication for catheter ablation of atrial fibrillation. Chest. 2005;128(4):2581–2587. doi: 10.1378/chest.128.4.2581. [DOI] [PubMed] [Google Scholar]
- 2.Gillinov AM, Pettersson G, Rice TW. Esophageal injury during radiofrequency ablation for atrial fibrillation. J Thorac Cardiovasc Surg. 2001;122(6):1239–1240. doi: 10.1067/mtc.2001.118041. [DOI] [PubMed] [Google Scholar]
- 3.Scanavacca MI, D'ávila A, Parga J, Sosa E. Left atrial-esophageal fistula following radiofrequency catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2004;15(8):960–962. doi: 10.1046/j.1540-8167.2004.04083.x. [DOI] [PubMed] [Google Scholar]
- 4.Pappone C, Oral H, Santinelli V, Lang CC, Manguso F, Torracca L, et al. Atrio-esophageal fistula as a complication of percutaneous transcatheter ablation of atrial fibrillation. Circulation. 2004;109(22):2724–2726. doi: 10.1161/01.CIR.0000131866.44650.46. [DOI] [PubMed] [Google Scholar]
- 5.Ghia KK, Chugh A, Good E, Pelosi F, Jongnarangsin K, Bogun F, et al. A nationwide survey on the prevalence of atrioesophageal fistula after left atrial radiofrequency catheter ablation. J Interv Card Electrophysiol. 2009;24(1):33–36. doi: 10.1007/s10840-008-9307-1. [DOI] [PubMed] [Google Scholar]
- 6.Cummings JE, Schweikert RA, Saliba WI, Burkhardt JD, Kilikaslan F, Saad E, et al. Brief communication: atrial-esophageal fistulas after radiofrequency ablation. Ann Intern Med. 2006;144(8):572–574. doi: 10.7326/0003-4819-144-8-200604180-00007. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt M, Nölker G, Marschang H, Gutleben KJ, Schibgilla V, Rittger H, et al. Incidence of oesophageal wall injury post-pulmonary vein antrum isolation for treatment of patients with atrial fibrillation. Europace. 2008;10(2):205–209. doi: 10.1093/europace/eun001. [DOI] [PubMed] [Google Scholar]
- 8.Pappone C, Rosanio S, Oreto G, Tocchi M, Gugliotta F, Vicedomini G, et al. Circunferential radiofrequency ablation of pulmonary vein ostia: A new anatomic approach for curing atrial fibrillation. Circulation. 2000;102(21):2619–2628. doi: 10.1161/01.cir.102.21.2619. [DOI] [PubMed] [Google Scholar]
- 9.Teplitsky L, Hegland DD, Bahnson TD. Catheter based cryoablation and radiofrequency ablation for atrial fibrillation results in conductive heat transfer from and to the esophagus. Heart Rhythm. 2006;3(5):S242–S242. [Google Scholar]
- 10.Ripley KL, Gage AA, Olsen DB, Van Vleet JF, Lau CP, Tse HF. Time course of esophageal lesions after catheter ablation with cryothermal and radiofrequency ablation: implication for atrio-esophageal fistula formation after catheter ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2007;18(6):642–646. doi: 10.1111/j.1540-8167.2007.00790.x. [DOI] [PubMed] [Google Scholar]
- 11.Arruda MS. Pre clinical "in vivo" evaluation of an esophageal protective system: Implications on esophageal thermal injury during AF ablation. Heart Rhythm. 2008;5:S16–S16. [Google Scholar]
- 12.Redfearn DP, Trim GM, Skanes AC, Petrellis B, Krahn AD, Yee R, et al. Esophageal temperature monitoring during radio frequency ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2005;16(6):589–593. doi: 10.1111/j.1540-8167.2005.40825.x. [DOI] [PubMed] [Google Scholar]
- 13.Good E, Oral H, Lemola K, Han J, Tamirisa K, Igic P, et al. Movement of the esophagus during left atrial catheter ablation for atrial fibrillation. J Am Coll Cardiol. 2005;46(11):2107–2110. doi: 10.1016/j.jacc.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 14.Helms A, West JJ, Patel A, Mounsey JP, DiMarco JP, Mangrum JM, et al. Real-time rotational ICE imaging of the relationship of the ablation catheter tip and the esophagus during atrial fibrillation ablation. J Cardiovasc Electrophysiol. 2009;20(2):130–137. doi: 10.1111/j.1540-8167.2008.01277.x. [DOI] [PubMed] [Google Scholar]
- 15.Haissaguerre M, Jais P, Shah DC, Garrigue S, Takahashi A, Lavergne T, et al. Electrophysiological end point for catheter ablation of atrial fibrillation initiated from multiple pulmonary venous foci. Circulation. 2000;101(12):1409–1417. doi: 10.1161/01.cir.101.12.1409. [DOI] [PubMed] [Google Scholar]
- 16.Morady F. Treatment of paroxysmal atrial fibrillation by pulmonary vein isolation. Circ J. 2003;67(7):567–571. doi: 10.1253/circj.67.567. [DOI] [PubMed] [Google Scholar]
- 17.Pachón M JC, Pachón M EI, Pachon M JC, Lobo TJ, Pachon MZ, Vargas RN, et al. A new treatment for atrial fibrillation based on spectral analysis to guide the catheter RF-ablation. Europace. 2004;6(6):590–601. doi: 10.1016/j.eupc.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 18.Arruda M, Natale A. Ablation of permanent AF: adjunctive strategies to pulmonary veins isolation: targeting AF NEST in sinus rhythm and CFAE in AF. J Interv Card Electrophysiol. 2008;23(1):51–57. doi: 10.1007/s10840-008-9252-z. [DOI] [PubMed] [Google Scholar]
- 19.Huang SY, Lin YJ, Tsao HM, Chang SL, Lo LW, Hu HF, et al. The biatrial substrate properties in different types of paroxysmal atrial fibrillation. Heart Rhythm. 2011;8(7):961–967. doi: 10.1016/j.hrthm.2011.01.046. [DOI] [PubMed] [Google Scholar]
- 20.Mateos JC, Mateos EI, Lobo TJ, Pachón MZ, Mateos JC, Pachón DQ, et al. Radiofrequency catheter ablation of atrial fibrillation guided by spectral mapping of atrial fibrillation nests in sinus rhythm. Arq Bras Cardiol. 2007;89(3):124-34, 140-50. doi: 10.1590/s0066-782x2007001500001. [DOI] [PubMed] [Google Scholar]
- 21.Good E, Oral H, Lemola K, Han J, Tamirisa K, Igic P, et al. Movement of the esophagus during left atrial catheter ablation for atrial fibrillation. J Am Coll Cardiol. 2005;46(11):2107–2110. doi: 10.1016/j.jacc.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 22.Kenigsberg DN, Lee BP, Grizzard JD, Ellenbogen KA, Wood MA. Accuracy of intracardiac echocardiography for assessing the esophageal course along the posterior left atrium: a comparison to magnetic resonance imaging. J Cardiovasc Electrophysiol. 2007;18(2):169–173. doi: 10.1111/j.1540-8167.2006.00699.x. [DOI] [PubMed] [Google Scholar]
- 23.Sherzer AI, Feigenblum DI, Kulkarni S, Pina JW, Casey JL, Salka KA, et al. Continuous nonfluoroscopic localization of the esophagus during radiofrequency catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2007;18(2):157–160. doi: 10.1111/j.1540-8167.2006.00674.x. [DOI] [PubMed] [Google Scholar]
- 24.Kennedy R, Good E, Oral H, Huether E, Bogun F, Pelosi F, et al. Temporal stability of the location of the esophagus in patients undergoing the repeat left atrial ablation procedure for atrial fibrillation or flutter. J Cardiovasc Electrophysiol. 2008;19(4):351–355. doi: 10.1111/j.1540-8167.2007.01051.x. [DOI] [PubMed] [Google Scholar]
- 25.Teplitsky L, Perzanowski C, Durrani S, Berman AE, Hranitzky P, Bahnson TD. Radio frequency catheter ablation for atrial fibrillation produces delayed and long lasting elevation of luminal esophageal temperature independent of lesion duration and power. Heart Rhythm. 2005;2(Suppl):S8–S9. [Google Scholar]
- 26.Cummings JE, Schweikert RA, Saliba WI, Burkhardt JD, Brachmann J, Gunther J, et al. Assessment of temperature, proximity, and course of the esophagus during radiofrequency ablation within the left atrium. Circulation. 2005;112(4):459–464. doi: 10.1161/CIRCULATIONAHA.104.509612. [DOI] [PubMed] [Google Scholar]
- 27.Berjano EJ, Hornero F. A cooled intraesophageal balloon to prevent thermal injury during endocardial radiofrequency surgical ablation of the left atrium: a finite element study. Phys Med Biol. 2005;50(20):N269–N279. doi: 10.1088/0031-9155/50/20/N03. [DOI] [PubMed] [Google Scholar]
- 28.Tsuchiya T, Ashikaga K, Nakagawa S, Hayashida K, Kugimiya H. Atrial fibrillation ablation with esophageal cooling with the cooled water-irrigated intraesophageal balloon: a pilot study. J Cardiovasc Electrophysiol. 2007;18(2):145–150. doi: 10.1111/j.1540-8167.2006.00693.x. [DOI] [PubMed] [Google Scholar]
- 29.Herweg B, Johnson N, Postler G, Curtis AB, Barold SS, Ilercil A. Mechanical esophageal deflection during ablation of atrial fibrillation. Pacing Clin Electrophysiol. 2006;29(9):957–961. doi: 10.1111/j.1540-8159.2006.00470.x. [DOI] [PubMed] [Google Scholar]
- 30.Chugh A, Rubenstein J, Good E, Ebinger M, Jongnarangsin K, Fortino J, et al. Mechanical displacement of the esophagus in patients undergoing left atrial ablation of atrial fibrillation. Heart Rhythm. 2009;6(3):319–322. doi: 10.1016/j.hrthm.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 31.Singh SM, D'ávila A, Doshi SK, Brugge WR, Bedford RA, Mela T, et al. Esophageal injury and temperature monitoring during atrial fibrillation ablation. Circ Arrhythm Electrophysiol. 2008;1(3):162–168. doi: 10.1161/CIRCEP.107.789552. [DOI] [PubMed] [Google Scholar]