Abstract
Setting:
An antenatal clinic serving a population of 47 604 in Nausori, Fiji.
Objective:
1) To estimate the prevalence of anaemia, syphilis and hepatitis B in pregnant women attending their first antenatal visit; and 2) to estimate the uptake of treatment for syphilis and for the prevention of hepatitis B transmission in affected individuals.
Design:
Retrospective review of the clinic register and patient records for the year 2011.
Results:
The prevalence of anaemia, hepatitis B and syphilis were respectively 22%, 2% and 5%. Among women with syphilis, 78% of those for whom data were available received a complete course of three doses of penicillin during their pregnancy, and 83% of babies born to women with hepatitis B received hepatitis B immunoglobulin.
Conclusion:
The prevalence of anaemia in pregnant women has declined but remains high, and further research is required to identify the major causes of this condition in Fiji. The prevalence of syphilis has remained static, while hepatitis B has decreased over the past decade. There are some gaps in the implementation of effective interventions to manage these conditions in pregnant women.
Keywords: antenatal care, community health, maternal and child health, nutrition, sexually transmitted diseases
Abstract
Contexte:
Une polyclinique prénatale au service d’une population de 47 604 personnes à Nausori, Fiji.
Objectif:
Estimer 1) la prévalence de l’anémie, de la syphilis et de l’hépatite B chez les femmes enceintes lors de leur première visite prénatale, et 2) l’adoption du traitement de la syphilis ainsi que le traitement préventif de la transmission de l’hépatite B à partir des individus atteints.
Schéma:
Revue rétrospective du registre clinique et des dossiers des patients pendant l’année 2011.
Résultats:
La prévalence de l’anémie, de l’hépatite B et de la syphilis a été respectivement de 22%, 2% et 5%. Parmi les femmes syphilitiques, 78% de celles dont les données étaient disponibles avaient reçu une cure complète de 3 doses de pénicilline au cours de leur grossesse et 83% des bébés nés de femmes atteintes d’hépatite B avaient reçu l’immunoglobuline de l’hépatite B.
Conclusion:
La prévalence de l’anémie a décliné chez les femmes enceintes, mais reste élevée, et des recherches complémentaires s’imposent pour identifier les causes principales de cette condition aux Iles Fiji. La prévalence de la syphilis est restée tout à fait stable, alors que l’hépatite B devient moins fréquente au cours de la dernière décennie. Il persiste quelques insuffisances dans la mise en œuvre d’interventions efficientes pour la prise en charge de ces affections chez les femmes enceintes.
Abstract
Marco de referencia:
Un consultorio de control prenatal que cubre a una población de 47 604 personas en Nausori, Fiji.
Objetivo:
Se calculó la prevalencia de anemia, sífilis y hepatitis B en las mujeres embarazadas que acudieron a la primera consulta prenatal y se evaluó la aceptación del tratamiento de la sífilis y del tratamiento preventivo de la transmisión de la hepatitis B en las mujeres afectadas.
Método:
Se practicó un examen retrospectivo de los registros médicos y las historias clínicas de las pacientes del año 2011.
Resultados:
La prevalencia de anemia fue 22%, de hepatitis B fue 2% y la prevalencia de sífilis fue 5%. En las mujeres que padecían sífilis, el 78% de aquellas cuyos datos se pudieron consultar recibió un ciclo completo de tres dosis de penicilina durante el embarazo y el 83% de los recién nacidos de mujeres que sufrían hepatitis B recibió la inmunoglobulina contra la hepatitis B.
Conclusión:
En Fiji, la prevalencia de anemia en las mujeres embarazadas ha disminuido, pero sigue siendo alta y se precisan nuevas investigaciones que determinen las principales causas de este problema. Durante el último decenio la prevalencia de sífilis ha permanecido muy estable y la prevalencia de hepatitis B ha disminuido. Existen algunas lagunas en la ejecución de las intervenciones eficaces encaminadas a tratar estas afecciones en las mujeres embarazadas.
Anaemia, hepatitis B and syphilis are serious conditions in pregnant women due to their adverse effects on both maternal and infant health. However, the adverse infant outcomes associated with these conditions are preventable, especially if they are detected and managed appropriately during pregnancy and the neonatal period. It is therefore routine practice to screen pregnant women for anaemia, hepatitis B and syphilis during antenatal care visits.1–3
Recent data on the prevalence and management of these conditions during pregnancy in Fiji are sparse. The prevalence of anaemia among pregnant women in Fiji was 44% in 2004.4 In 2010, the Fiji Ministry of Health (MoH) reported a prevalence of anaemia of 11%.5 However, this is likely to be an underestimate due to under-reporting of cases. In the Western Pacific region as a whole, the prevalence of anaemia was estimated to be 30.7% between 1993 and 2005, slightly lower than the global prevalence of 41.8% during the same period.6 The prevalence of syphilis in Fiji between 1992 and 1995 was 5.9%,7 compared to 0.7% in the Western Pacific region as a whole.8 Of the 1488 babies born to mothers with syphilis in Fiji during this period, 73 died, including 53 whose mothers had not completed treatment for syphilis during their pregnancy. The prevalence of hepatitis B among pregnant women in Fiji was around 5% between 1994 and 1996,9 compared with 3.9% in the Western Pacific region in 2007.10 There is a need for more up-to-date information on the prevalence of these conditions and on the implementation of effective management in order to establish whether current practice is meeting the care needs of pregnant women.
Using routine data from an antenatal clinic in Nausori, Fiji, we carried out this study to determine 1) the prevalence of anaemia, hepatitis B and syphilis in pregnant women, and 2) the proportion of women with syphilis and hepatitis B for whom appropriate management was implemented, to establish an evidence base to inform future policy and practice in Fiji.
METHODS
Setting
Fiji is an island nation located in the south-west Pacific, with a population of approximately 837 000. It consists of approximately 332 islands, covering a total land area of 1833 km2.
The study was conducted at the Nausori Maternity Unit (NMU), an antenatal clinic in Nausori on Viti Levu island, the largest island in Fiji. Situated 19 km from the capital, Suva, Nausori is the fourth largest town in Fiji, with a population of 47 604 (approximately 6% of Fiji’s entire population).11
The NMU is a free, government-run service and the sole maternity unit catering for the population of the Rewa Medical Subdivision; it also covers some surrounding areas. In addition to maternity care, the service provides advice and support for women and their families on family planning, prevention of sexually transmissible infections (STIs), nutritional advice and postnatal care and lactation counselling. The NMU manages 1500–2000 deliveries per year.5
Design
This was a cross-sectional study involving the retrospective review of routine antenatal clinic records. The study included all pregnant women who attended their first antenatal care booking at the NMU between January and December 2011.
Individual data on all pregnant women attending their first antenatal care booking were sourced from the antenatal clinic booking register and included the following variables: ethnicity, age, gestational age, marital status, parity, haemoglobin (Hb) concentration, hepatitis B surface antigen (HbsAg) status and Venereal Disease Research Laboratory (VDRL) serology status. Additional data on Treponema pallidum haemagglutination test status (TPHA) and treatment of syphilis were obtained from a separate serology register. Information on receipt of hepatitis B immunoglobulin among infants born to mothers with hepatitis B was obtained from the clinic records.
Anaemia was defined as Hb concentration < 11 g/dl, in accordance with the standard World Health Organization definition.6 Women who were HbsAg- and TPHA-positive were classified as having respectively hepatitis B and syphilis. Women with syphilis were regarded as having received appropriate treatment if there was evidence that they had received a course of three injections of penicillin. Infants born to women with hepatitis B were regarded as having been managed appropriately if they had received hepatitis B immunoglobulin. We did not attempt to assess the management of anaemia, as all women received iron and folate supplements regardless of Hb level.
Statistical analyses
All data were entered into a data entry file using EpiData Entry software version 3.1 (EpiData Association, Odense, Denmark).
Data were analysed using SAS version 9.3 (SAS Institute, Cary, NC, USA). Continuous variables were described as means and standard deviations (SDs), while categorical variables were described as proportions. Differences between groups were compared using the χ2 test for categorical variables. P < 0.05 was regarded as significant.
Ethics
Ethics approval was obtained from the Fiji Ministry of Health National Health Research Committee and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease.
RESULTS
During 2011, 2168 pregnant women attended a first antenatal clinic booking at the NMU. The majority of the women were aged between 20 and 29 years, were indigenous Fijian, presented in the second trimester of pregnancy and had had one or fewer previous deliveries (Table); 69% were married and a further 18% were in de facto relationships.
TABLE.
Characteristics and prevalence of anaemia, hepatitis B and syphilis among pregnant women attending their first antenatal clinic booking at Nausori Maternity Unit, Fiji, 2011
| Variable | n (%)* | Anaemia n (%)† | Hepatitis B n (%)† | Syphilis n (%)† |
| Total | 2168 | 451 | 47 | 98 |
| Age, years | ||||
| <20 | 191 (9) | 48 (27) | 1 (0.6) | 2 (1) |
| 20–29 | 1341 (62) | 289 (23) | 32 (3) | 70 (6) |
| 30–39 | 579 (27) | 106 (20) | 14 (3) | 25 (5) |
| ≥40 | 46 (2) | 6 (14) | 0 | 1 (2) |
| Unknown | 11 (0.5) | 2 (22) | 0 | 0 |
| Ethnicity | ||||
| Fijian | 1662 (77) | 318 (20) | 44 (3) | 92 (6) |
| Indo-Fijian | 463 (21) | 123 (28) | 0 | 5 (1) |
| Other | 41 (2) | 10 (26) | 3 (3) | 1 (3) |
| Unknown | 2 (0.1) | 0 | 0 | 0 |
| Gestational age | ||||
| First trimester | 161 (7) | 16 (11) | 4 (3) | 6 (4) |
| Second trimester | 709 (33) | 152 (22) | 24 (4) | 31 (5) |
| Third trimester | 157 (7) | 51 (34) | 1 (1) | 11 (8) |
| Unknown | 1141 (53) | 232 (22) | 18 (2) | 50 (5) |
| Parity | ||||
| No previous births | 761 (35) | 179 (25) | 7 (1) | 21 (3) |
| 1 birth | 525 (24) | 91 (18) | 12 (2) | 28 (6) |
| 2 births | 372 (17) | 77 (22) | 12 (3) | 29 (8) |
| 3 births | 230 (11) | 58 (27) | 6 (3) | 8 (4) |
| ≥4 births | 280 (13) | 46 (17) | 10 (4) | 12 (5)w |
*Percentage of pregnant women with this characteristic.
†Percentage of women with this characteristic who had anaemia, hepatitis B or syphilis, respectively. Excludes 115 women in whom Hb was not recorded, 166 in whom HbsAg was not recorded and 123 in whom TPHA was not recorded.
Hb = haemoglobin; HbsAg = hepatitis B surface antigen; TPHA = Treponema pallidum haemagglutination test status.
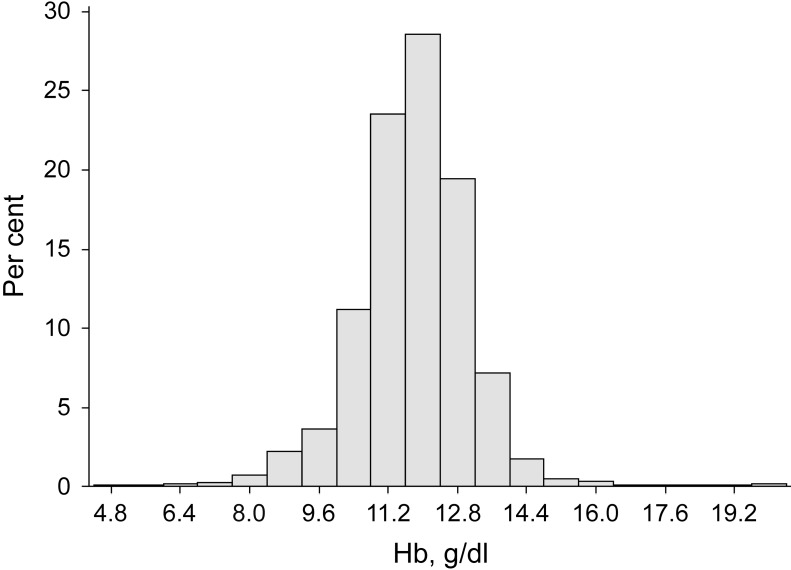
Data for Hb, hepatitis B and syphilis serology were missing for respectively 115 (5%), 166 (8%) and 123 (6%) women. The mean Hb concentration was 11.8 g/dl (standard deviation 1.3). The prevalence of anaemia, hepatitis B and syphilis among those for whom data were available was respectively 22%, 2% and 5%. The frequency distribution of Hb concentration among pregnant women is shown in the Figure. Anaemia was more common in Indo-Fijian than indigenous Fijian women (P = 0.004), and in women who presented in the later stages of pregnancy than those presenting during the first trimester (P < 0.001). In contrast, syphilis and hepatitis B were more common in indigenous Fijian women (P < 0.001), and were not related to gestational age or actual age at the time of first presentation for antenatal care.
FIGURE.
Relative frequency distribution of Hb among pregnant women attending their first antenatal clinic booking at Nausori Maternity Unit, Fiji, 2011. Hb = haemoglobin.
Among 98 women diagnosed with syphilis at the NMU, 39 (40%) did not complete their antenatal care at Nausori. There were no significant differences in age group, ethnicity and gestational age at presentation or parity between women with syphilis managed at Nausori and those managed elsewhere (P > 0.4). Of the 59 who completed their antenatal care at Nausori, 46 (78%) received a course of three doses of penicillin as treatment for syphilis, while the remaining 13 women (22%) had no record of having completed a full course of treatment. There were no significant differences between women who completed a full course of treatment and those who did not in age group, gestational age at first presentation or parity (all P > 0.5). Forty-two (78%) of the 54 Fijian women and all four Indo-Fijian women (100%; P = 0.1) diagnosed with syphilis who did not transfer out of the NMU during their antenatal care had a record of having completed treatment for syphilis at the NMU.
Of the 47 babies born to mothers with hepatitis B, 39 (83%) received hepatitis B immunoglobulin. The remaining eight infants were delivered at other maternity units, and information on the administration of hepatitis B immunoglobulin to these infants was not available.
DISCUSSION
There is a high prevalence of anaemia and a low prevalence of hepatitis B and syphilis among pregnant women presenting for their first antenatal care visit in Nausori, Fiji. A substantial proportion of women with syphilis had no record of having received appropriate antibiotic treatment during their pregnancy. Most infants born to mothers with hepatitis B received hepatitis B immunoglobulin in the postnatal period.
The study strengths are that 1) a relatively large number of individuals were included, 2) data were obtained from a single clinic that provides all antenatal care for a population of 47 000, and the data are therefore representative of the target population, 3) as the study period encompassed a full calendar year, seasonal factors should not have influenced the results, and 4) the antenatal register in this clinic includes near-complete data on Hb concentration and serology of pregnant women.
The main limitations are that some data on demographic and other pregnancy-related variables were missing. However, this differed between registers representing different periods of the year, and is therefore unlikely to result in bias. As data on behavioural and dietary risk factors were not available, it is not possible to draw conclusions about the reasons for the high prevalence of anaemia. Data on foetal and infant outcomes were not available and the consequences of anaemia, hepatitis B and syphilis could therefore not be ascertained in this study.
Our study results indicate that the prevalence of anaemia in pregnant women has decreased substantially since the prevalence estimated in 2004.4 The current prevalence of 22% is lower than in other developing countries, which were in the range of 40% to 60% in 2005.6 We believe that the main reason for this substantial decline in the prevalence of anaemia during pregnancy in Fiji is the programme of iron fortification of flour, which was introduced as a national initiative in 2002 and has been fully implemented nationwide since 2005. Fortification of staple foods is useful as a strategy for tackling widespread deficiencies as it does not require individual compliance and, if well placed, should not require any change in dietary habits. Flour was identified as being the best vehicle for iron fortification in Fiji as it is a food product consumed on a daily basis by all ethnic groups. An evaluation of serum ferritin levels and Hb concentrations among women of childbearing age (15–45 years) in 2004 and 2010 revealed a significant decline in iron deficiency, from 22.9% to 7.9%, and in anaemia, from 40.3% to 27.6%, over this period.12
These findings in Fiji are corroborated by other studies that have demonstrated the success of fortification programmes in reducing iron deficiency and iron deficiency anaemia. In Venezuela, fortification of flour with iron reduced the prevalence of iron deficiency and iron deficiency anaemia in children by almost half.13 A randomised controlled trial in Viet Nam showed that the consumption of fortified fish sauce reduced the prevalence of iron deficiency and iron deficiency anaemia among women aged 17 to 49 years compared to controls.14 There is thus strong support for the view that the observed reduction in anaemia in pregnant women is attributable to the programme of iron fortification of flour.
In addition to the flour fortification initiative, a National Iron & Micronutrient Supplementation Programme was introduced in 2010 for women of childbearing age (15–49 years) and children aged <5 years. This initiative may have further contributed to the decline in anaemia observed among pregnant women. However, while there is evidence that iron supplementation alone results in a substantial reduction in individual women’s risk of anaemia,15 the overall impact of iron supplementation interventions under field conditions has been questioned. Their limited success has been attributed to inadequate infrastructure and poor compliance.16 The impact of the National Iron & Micronutrient Supplementation Programme in Fiji thus needs to be evaluated.
Although the prevalence of anaemia among pregnant women has declined in recent years, it remains unacceptably high and there may be contributing factors other than nutritional deficiency. Other possible causes include abnormal vaginal discharge, intestinal infections and malaria.17 The relevance of these causes varies between settings. For example, although schistosomiasis and malaria were common causes of anaemia in pregnant women in Mali,17 these infections do not occur in Fiji. The Fiji National Nutrition Survey conducted in 2004 identified high intake of processed foods and low intake of fruits and vegetables as a problematic feature of the diets of many Fijians.4 This problem may have been exacerbated in recent years by economic difficulties. There are, however, no data on the causes of anaemia in pregnant women in Fiji, and further research into the causes of anaemia is required so that appropriate additional clinical and public health responses can be initiated.
The prevalence of hepatitis B among 15 113 pregnant women attending the Colonial War Memorial (CWM) Hospital in Suva, Fiji, during the period 1994–1996 was 4.8%.9 These data from Nausori, situated next to Suva, thus show a reduction in the prevalence of hepatitis B in pregnant women over the last 15 years.
The prevalence of syphilis has not declined since it was estimated at 5.9% among pregnant women attending the CWM Hospital in 1995.7 This is higher than reported for Papua New Guinea (2.7%) and Malaysia (0.1%).8 The very low prevalence of syphilis during pregnancy in Malaysia coincides in that country with the expanded coverage of STI interventions through an integrated approach that offers convenient STI services at clinics for sexual and reproductive health.8
The relatively high proportion of children born to mothers with positive syphilis serology who have no record of having received penicillin implies that more attention needs to be paid to the implementation of this effective treatment. The programme of screening for hepatitis B and administration of hepatitis B immunoglobulin to affected infants seems to be more effective, although there remains some uncertainty about the management of pregnant women who transfer care to another centre after initial screening. Efforts to prevent transmission of STIs and to ensure adequate population coverage with hepatitis B vaccine should continue.
In conclusion, the prevalence of anaemia in pregnant women remains high, and further research is required to identify the major causes of this condition in Fiji. While the prevalence of syphilis and hepatitis B has decreased over the past decade, efforts to improve the provision of effective treatments are still needed.
Acknowledgments
The authors thank T Qoriniasi, Sub-Divisional Medical Officer, Rewa, and U Sikivou, Sister-in-Charge Maternity, Rewa, for their assistance in providing access to the data.
This research was supported through an operational research course that was jointly developed and run by the Fiji National University, Suva, Fiji; the Centre for Operational Research, International Union Against Tuberculosis and Lung Disease, Paris, France; the Operational Research Unit, Médecins Sans Frontières, Brussels, Belgium; the University of Auckland, Auckland, New Zealand; the Woolcock Institute of Medical Research, Sydney, NSW, Australia; and the Centre for International Child Health, the University of Melbourne, Melbourne, VIC, Australia.
Funding for this course came from the Global Fund to Fight AIDS, Tuberculosis and Malaria, the International Union Against Tuberculosis and Lung Disease and the World Health Organization.
Conflict of interest: none declared.
References
- 1.Sekhavat L, Davar R, Hosseinidezoki S. Relationship between maternal hemaglobin concentration and neonatal birth weight. Hematology. 2011;16:373–376. doi: 10.1179/102453311X13085644680186. [DOI] [PubMed] [Google Scholar]
- 2.Hawkes S, Matin N, Broutet N, Low N. Effectiveness of interventions to improve screening for syphilis in pregnancy: systematic review and meta-analysis. Lancet Infect Dis. 2011;11:684–691. doi: 10.1016/S1473-3099(11)70104-9. [DOI] [PubMed] [Google Scholar]
- 3.Degli E S, Shah D. Hepatitis B in pregnancy: challenges and treatment. Gastroenterol Clin North Am. 2011;40:355–372. doi: 10.1016/j.gtc.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Schultz J T, Vatucawaqa P, Tuivaga J. 2004 Fiji National Nutrition Survey. Main Report. Suva, Fiji: National Food and Nutrition Centre; 2007. [Google Scholar]
- 5.Ministry of Health. Annual report. Suva, Fiji: MoH; 2010. p. 20. [Google Scholar]
- 6.World Health Organization. Worldwide prevalence of anaemia, 1993–2005. WHO global database on anaemia. Geneva, Switzerland: WHO; 2008. http://whqlibdoc.who.int/publications/2008/9789241596657_eng.pdf Accessed January 2013. [Google Scholar]
- 7.Schramm M. Syphilis in Fiji 1995. Pacific Health Dialog. 1996;3:216–219. [Google Scholar]
- 8.World Health Organization. HIV and sexually transmitted infections in the Western Pacific Region 2000–2010. Manila, Philippines: WHO Western Pacific Region; 2012. [Google Scholar]
- 9.Mathai E, Krishna M. Hepatitis B infection in the Pacific. Pacific Health Dialog. 2012;5:142–146. [Google Scholar]
- 10.Ugbebor O, Aigbirior M, Osazuwa F, Enabudoso E, Zabayo O. The prevalence of hepatitis B and C viral infections among pregnant women. N Am J Med Sci. 2011;3:238–241. doi: 10.4297/najms.2011.3238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiji Islands Bureau of Statistics. Population of towns and urban areas 2007. Suva, Fiji: Bureau of Statistics; 2007. [Google Scholar]
- 12.Schultz J T, Vatucawaqa P. Impact of iron fortified flour in child bearing age (CBA) women in Fiji. 2010 Report. Suva, Fiji: National Food and Nutrition Centre; 2012. [Google Scholar]
- 13.Layrisse M, Garcia-Casal M N, Mendez-Castellano H, et al. Impact of fortification of flours with iron to reduce the prevalence of anaemia and iron deficiency among schoolchildren in Caracas, Venezuela: a follow-up. Food Nutr Bull. 2002;23:384–389. doi: 10.1177/156482650202300412. [DOI] [PubMed] [Google Scholar]
- 14.Van Thuy P, Berger J, Nakanishi Y, Khan N C, Lynch S R, Dixon P. The use of NaFeEDTA-fortified fish sauce is an effective tool for controlling iron deficiency in women of childbearing age in rural Viet Nam. J Nutr. 2005;135:2596–2601. doi: 10.1093/jn/135.11.2596. [DOI] [PubMed] [Google Scholar]
- 15.Villar J, Merialdi M, Gulmezoglu M, et al. Nutritional interventions during pregnancy for the prevention or treatment of maternal morbidity and preterm delivery: an overview of randomized controlled trials. J Nutr. 2003;5(Suppl 2):1606S–1625S. doi: 10.1093/jn/133.5.1606S. [DOI] [PubMed] [Google Scholar]
- 16.Mora J O. Iron supplementation: overcoming technical and practical barriers. J Nutr. 2002;132(Suppl):853S–855S. doi: 10.1093/jn/132.4.853S. [DOI] [PubMed] [Google Scholar]
- 17.Ag Ayoya M, Spiekermann-Brouwer G M, Traor A K, Stoltzfus R J, Garza C. Determinants of anaemia among pregnant women in Mali. Food Nutr Bull. 2006;27:3–11. doi: 10.1177/156482650602700101. [DOI] [PubMed] [Google Scholar]