Abstract
Setting:
Childhood obesity is of growing public health concern in Fiji. The study setting was primary schools in Fiji’s Western Division.
Objective:
1) To assess primary schools’ compliance with national school canteen guidelines, 2) to understand reasons for non-compliance, and 3) to assess the relationship between compliance with the guidelines and students’ body mass index (BMI).
Design:
Cross-sectional analysis of data collected in 2010 by public health dieticians of the Ministry of Health on annual visits to primary schools.
Results:
Among 230 schools, 33 (14%) had no canteen data. Of the 197 schools with data, only 31 (16%) were fully compliant with national school canteen guidelines, while the remaining 166 (84%) did not fully comply with the guidelines. This was irrespective of school location or whether the canteen was school or commercially operated. In a random sample (n = 44 schools), overweight and obesity were more common among children in non-compliant schools than in fully compliant schools (40% vs. 32%, P < 0.001).
Conclusion:
Most primary schools in Fiji’s Western Division did not comply with school canteen guidelines, which is worrying given the increasing rates of overweight children. Given the association between non-compliance and student overweight/obesity, further action is needed to ensure that these guidelines are implemented.
Keywords: Fiji, primary school, canteen guidelines, compliance
Abstract
Contexte:
L’obésité infantile représente une préoccupation croissante de santé publique aux Iles Fiji. Cette étude a été menée dans les écoles primaires de la Division Ouest des Iles Fiji.
Objectif:
1) Evaluer l’observance des écoles primaires concernant les directives nationales sur les cantines scolaires, 2) comprendre les raisons de non-observance et 3) évaluer les relations entre l’observance des directives et l’index de masse corporelle (BMI) des élèves.
Schéma:
Analyse transversale des données recueillies en 2010 par les diététiciens du Service de Santé Publique du Ministère de la Santé lors de leurs visites annuelles dans les écoles primaires.
Résultats:
Parmi 230 écoles, les données concernant la cantine faisaient défaut dans 33 (14%). Sur les 197 écoles avec données, 31 seulement (16%) observaient totalement les directives nationales concernant les cantines scolaires, alors que les 166 restantes (84%) n’adhéraient pas complètement à ces directives. Ceci ne dépend pas de la localisation de l’école ni du fait que la cantine soit gérée par l’école ou par une firme commerciale. Dans un échantillon aléatoire (n = 44 écoles), le surpoids et l’obésité étaient plus courants chez les enfants dans les écoles avec une manque d’observance que dans les écoles avec une bonne observance (40% vs. 32%, P < 0,001).
Conclusion:
Dans la Division Ouest des Iles Fiji, la plupart des écoles primaires ne respectent pas les directives sur les cantines scolaires, ce qui constitue une préoccupation vu les taux croissants de surpoids chez les enfants. Donné l’association entre la non-observance et le surpoids ou l’obésité des élèves, des actions complémentaires s’imposent pour garantir la mise en œuvre effective de ces directives.
Abstract
Marco de referencia:
La obesidad en la infancia constituye un problema creciente de salud pública en Fiji. Se llevó a cabo un estudio en las escuelas primarias de la división occidental del país.
Objetivo:
1) Evaluar el cumplimiento de las normas nacionales en materia de funcionamiento de las cafeterías escolares en las escuelas primarias; 2) investigar las razones de la falta de conformidad; y 3) estudiar la correlación entre el cumplimiento con las normas nacionales y el índice de masa corporal de los alumnos.
Métodos:
Se llevó a cabo un análisis transversal de los datos recogidos por los nutricionistas del Ministerio de Salud Pública en el 2010, en el marco de las visitas anuales a las escuelas primarias.
Resultados:
De las 230 escuelas analizadas, 33 carecían de datos con respecto a la cafetería (14%). De los 197 establecimientos que contaban con la información, solo 31 cumplían a cabalidad con las normas nacionales sobre las cafeterías escolares (16%) y las 166 escuelas restantes (84%) no las cumplían integralmente. Esta observación fue independiente de la localización de la escuela y del tipo de administración de la cafetería por la propia escuela o por una entidad lucrativa. En una muestra aleatoria (n = 44 escuelas), el sobrepeso y la obesidad fueron más frecuentes en los niños que acudían a las escuelas que contravenían las normas que en los niños de las escuelas que las observaban (40% contra 32%; P < 0,001).
Conclusión:
La mayoría de las escuelas primarias de la división occidental de Fiji no cumplía con las normas sobre las cafeterías escolares, lo cual es fuente de inquietud, al considerar las tasas crecientes de sobrepeso en los niños. Dada la asociación demostrada entre la falta de conformidad con estas normas y el sobrepeso o la obesidad de los alumnos, es necesario tomar medidas que favorezcan la aplicación de las pautas nacionales.
Childhood overweight and obesity are of growing public health concern globally. The number of overweight children was estimated at over 42 million in 2010, with >80% of the burden in developing countries.1
A small Pacific island nation of 837 000 people, with 39% aged <20 years,2 Fiji is no exception. Studies have shown that the prevalence of overweight and obese children in Fiji is increasing: The 2004 Fiji National Nutrition Survey reported that 14.5% of children (aged <18 years) were obese,3 10% more than in the 1993 survey. A recent community-based obesity prevention project conducted in Fiji, the Obesity Prevention in Community (OPIC) Project, concluded that rates of overweight and obesity among children aged 12–18 years were high, and identified related indicators such as poor diet, lack of physical activity and unfavourable school and household environments as factors that need to be tackled.4
Almost all schools in Fiji have canteens that are operated directly by the schools or outsourced to commercial caterers. Many students regularly purchase food and beverages from these canteens.4 In 2005, the Fiji Ministry of Education, Ministry of Health and the National Food and Nutrition Centre developed school canteen guidelines5 providing direction on the sale of healthy foods and drinks. Mandatory compliance with these guidelines was stipulated by the Minister of Education from early 2009.6 However, according to the Consumer Council of Fiji, school canteens continue to sell unhealthy foods, snacks and carbonated beverages.7
The present study was undertaken 1) to assess the extent to which primary schools in Fiji’s Western Division comply with the canteen guidelines, 2) to better understand the reasons for non-compliance, and 3) to assess the relationship between compliance with the canteen guidelines and students’ weights.
METHODS
Study design
The study was a cross-sectional analysis of routinely collected data.
Setting and population
The study sites were all of the 230 primary schools in Fiji’s Western Division, one of four administrative regions in Fiji comprising four districts covering the mainland western coastal area, interior and offshore islands. The primary schools are attended by approximately 55 000 students aged 5–12 years. In urban areas, schools are larger, averaging 125 students per school, whereas schools in rural areas average only 55 students.
In Fiji, all primary schools are visited annually by public health dieticians employed by the Ministry of Health who, as part of their role, collect data on canteen food and child health. Health inspectors also undertake annual school visits to ensure adherence to hygiene and safety standards generally. They inspect school canteens, awarding a licence to operate if the standards are met. Data collected on these school visits are kept at each of the four district hospitals.
Data variables and collection
Data pertaining to this study were obtained from the 2010 records collected by public health dieticians and health inspectors, and from individual student records held at the schools. Using a structured proforma, we collected the following variables: school location (urban or rural, using Department of Education categories), name of canteen operator (school-led or outsourced to a commercial operator), the presence of a health inspector’s licence to operate, compliance with the school canteen guidelines, and the height and weight of the children. We defined a fully compliant school as one meeting all four goals of the canteen menu section of the guidelines and a non-compliant school as not meeting all four of these goals. The four goals are as follows: 1) schools should provide healthy meals in their canteens and practise good hygiene; 2) all canteens should sell food items at a reasonable price so that students can afford them; 3) foods that are detrimental to the health of schoolchildren should be taken off the shelves; 4) canteen owners should have nutritional knowledge that can guide them in selling only healthy foods in the canteen.
The body mass index (BMI) was calculated by dividing an individual’s weight (in kg) by the square of the individual’s height (m2), and categorised according to US Centers for Disease Control and Prevention criteria for children: underweight (BMI <13.5), healthy (BMI 13.5–<17.5), overweight (BMI 17.5–<18.5) and obese (BMI ≥18.5).8
School compliance with canteen guidelines was assessed among all 230 schools, while the relationship between compliance with the guidelines and student BMI status was assessed among 44 (30%) schools randomly selected from each of the four Western Division districts. This involved stratifying the schools by district to ensure equal representation, and randomly selecting schools using random number tables. With only four stratification units, a sample of 30% was deemed to be both appropriate for generating a representative sample and feasible in terms of study resources.
Data analyses
Simple descriptive and comparative analyses were undertaken. To assess the relationship between compliance with the guidelines and student BMI status, we stratified the schools according to compliance level (fully compliant or not fully compliant) and then calculated the mean proportion of children in each of the BMI categories for each level of compliance. χ2 tests were used to compare proportions, with differences considered to be significant at the 5% level (P < 0.05). Data were analysed using EpiData, version 2.2.1.171 (EpiData Association, Odense, Denmark).
Ethics
Ethics approval for the study was obtained from the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, the Fiji National Research Ethics Review Committee and the Fiji National University College Research Committee. Permission to access data was also obtained from the Fiji Ministry of Health, Divisional Office West and the Ministry of Education, Divisional Office West.
RESULTS
Of the 230 primary schools in Fiji’s Western Division, 33 (14%) had no canteen data and these schools were thus excluded from the analysis. The Table shows the characteristics of the 197 primary schools included in the study and their compliance with the canteen guidelines: 31 (14%) schools were fully compliant with the guidelines, while 166 (84%) were not. While compliance with the guidelines was not found to be associated with school location (urban or rural) or canteen operator status, a significantly greater proportion of fully compliant schools had a current health inspector licence compared to non-compliant schools (65% vs. 39%; P = 0.007).
TABLE.
Characteristics of schools in Fiji’s Western Division in relation to their compliance with the school canteen guidelines, 2010
| School factors | Full compliance |
P value* | |
| Yes n (%) | No n (%) | ||
| Total | 31 (16) | 166 (84) | — |
| School location | |||
| Urban | 4 (13) | 21 (13) | 0.65 |
| Rural | 27 (87) | 144 (87) | |
| Unknown | 0 | 1 (0.6) | |
| Canteen operator | |||
| School-led | 16 (52) | 78 (47) | 0.64 |
| Outsourced | 15 (48) | 88 (53) | |
| Health inspector licence | |||
| Yes | 20 (65) | 64 (39) | 0.007 |
| No | 11 (35) | 102 (61) | |
χ2 test comparing fully compliant and non-fully compliant schools for each variable, excluding any unknown records.
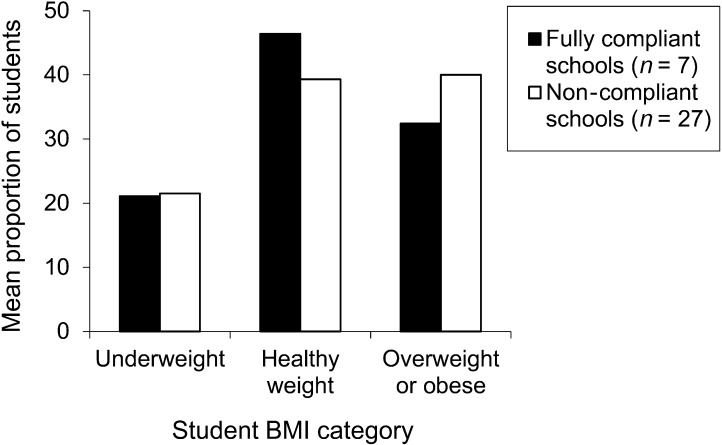
Among the 44 schools randomly selected to assess the relationship between compliance with the guidelines and student BMI status, 10 did not have canteen data and were therefore not included in the analysis. Among the 33 schools with canteen data, 3791 student records were retrieved to assess student BMI. The Figure shows the association between school compliance with canteen guidelines and student BMI status. Fully compliant schools (n = 7) had a higher proportion of children of healthy weight than non-compliant schools (n = 27; 46% vs. 39%, P < 0.001), and overweight and obesity were more common among children in non-compliant schools than in fully compliant schools (40% vs. 32%, P < 0.001).
FIGURE.
The relationship between student BMI and school compliance with canteen guidelines among a random sample of primary schools in Fiji’s Western Division, 2010. BMI = body mass index.
DISCUSSION
This study found that the majority of primary schools in the Western Division did not comply with Fiji’s national school canteen guidelines. While school canteens should encourage healthy eating by selling nutritious foods, foods of low nutritional value were the predominant food type offered. Contrary to our expectations, there was no association between compliance with the guidelines and either canteen operator status or school location (urban or rural). Compared with non-compliant schools, fully compliant schools had a significantly higher proportion of children of healthy weight and a significantly lower proportion of overweight and obese children.
This is the first study to examine compliance with the canteen guidelines since the implementation of these guidelines. The findings provide useful baseline data for the Ministries of Health and Education and the National Food and Nutrition Centre. As the study used routine data collected by trained health professionals, we believe that the data are relatively robust. Our study also adhered to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) Guidelines.9 Ethical approval was also obtained in addition to the primary recommendation.10
There are a number of study limitations. First, it is possible that our findings are not fully applicable to other regions of Fiji. The Western Division is less urbanised than the Southern Division, and the Northern Division is predominantly rural. However, as school location (urban or rural) was not associated with compliance with the guidelines, this may not be an issue. Second, any children who were absent at the time the individual anthropometric data were collected would not have been included. We were not able to quantify the incompleteness of these anthropometric data, although we do not believe that student absence was high enough to significantly bias the results. Third, a proportion of the schools (14%) did not have canteen data. This may have been because they had no canteen or because no data on their canteen were available. We were unable to differentiate between these two factors for each of the schools, and reasons for the absence of canteen data were not investigated. Finally, the associations we drew between compliance with the guidelines and BMI are speculative at best: children access food outside of school canteens, on the journey to and from school and at home, and not all children use school canteens for their lunches; we did not have access to data on physical activity or data on any proxy activity, such as the degree of participation in school sports; and we were unable to measure socio-economic status or other determinants of nutritional status or food consumption.
Possible reasons for non-compliance with the canteen guidelines include lack of awareness of the importance of implementing the guidelines by school heads and teachers. We had hypothesised that outsourcing canteen catering to commercial operators would lead to poorer quality food and drink being available, but the threat of licence withdrawal may be sufficient to ensure this does not occur. We had also hypothesised that urban schools would be more likely to sell poor quality food and drinks due to demand from urbanised children who might consume these foods every day outside of school due to their wide availability in other stores. However, neither of these hypotheses was supported by the findings.
Nonetheless, given the association between non-compliance of schools with canteen guidelines and student overweight and obesity, our findings make the case for the following recommendations: 1) national authorities should ensure strong and regular provision of guidance for schools on implementing the school canteen guidelines; 2) implementation of the canteen guidelines should be rigorously monitored; 3) compliance with canteen guidelines should be made mandatory for continued accreditation of schools with the Ministry of Health and Ministry of Education and for being granted a health inspector licence to operate.
Further research in this area should include surveying head teachers of non-compliant and compliant schools about the barriers or enablers to successful guideline implementation, and investigating the link between school canteens and healthy weight in students.
In conclusion, the majority of primary schools in Fiji’s Western Division failed to adhere to school canteen guidelines. An association between non-compliance with the guidelines and student overweight is of concern, and highlights the need for action to ensure that the guidelines are implemented by the schools.
Acknowledgments
The authors thank the dietician and the district dieticians of the Western Division for allowing them to access their routinely collected data for 2010. The authors also thank W Snowdon, Co-Coordinator, Pacific Research Centre for the Prevention of Obesity and NCDs, College of Medicine, Nursing and Health Sciences, Tamavua Campus, Suva, for her advice and guidance.
This research was supported through an operational research course that was jointly developed and run by the Fiji National University; the Centre for Operational Research, International Union Against Tuberculosis and Lung Disease; the Operational Research Unit, Médecins Sans Frontières, Brussels; the University of Auckland, Auckland, New Zealand; the Woolcock Institute of Medical Research, Sydney, NSW, Australia; and the Centre for International Child Health, University of Melbourne, Melbourne, VIC, Australia.
Funding for this course came from the Global Fund to Fight AIDS, Tuberculosis and Malaria, the International Union Against Tuberculosis and Lung Disease and the World Health Organization.
Conflict of interest: none declared.
References
- 1.World Health Organization. Global strategy on diet, physical activity and health. Childhood overweight and obesity. Geneva, Switzerland: WHO; 2010. http://www.who.int/dietphysicalactivity/childhood/en/ Accessed December 2012. [Google Scholar]
- 2.Fiji Bureau of Statistics. Key statistics. Population by age, sex and province of enumeration, Fiji: 2007 census. Suva, Fiji: Bureau of Statistics; 2011. http://www.statsfiji.gov.fj/Key%20Stats/Population/1.5%20%20Pop%20by%20age0.pdf Accessed December 2012. [Google Scholar]
- 3.National Nutrition Survey. Main report. Suva, Fiji: National Food and Nutrition Centre; 2004. http://www.nutrition.gov.fj/pdf/reports/2004%20NATIONAL%20NUTRITION%20SURVEY.pdf Accessed December 2012. [Google Scholar]
- 4.Tuiketei T, Snowdon W, Waqa G, Kremer P, Schultz J. Vanualailai; on behalf of the OPIC Team. Obesity Prevention in Community (OPIC) Project: Fiji report 2004–2008. Suva, Fiji: OPIC; 2010. http://www.fsm.ac.fj/files/Country%20OPIC%20Fiji%20report%20with%20cover%20FINAL.pdf Accessed December 2012. [Google Scholar]
- 5.National Food & Nutrition Centre. School canteen guidelines. Suva, Fiji: National Food & Nutrition Centre; 2005. [Google Scholar]
- 6.Bole F. School canteen guidelines. Fiji Food & Nutrition Newsletter. 2008;33(2) http://www.nutrition.gov.fj/pdf/nfnc_newsletter/Fiji%20Food%20and%20Nutrition%20newsletter%20Issue%202%202008.pdf Accessed December 2012. [Google Scholar]
- 7.Kumar P. School canteens play a role. Suva, Fiji: Consumer Council of Fiji, 2012. Fiji Times Online 2012; http://www.fijitimes.com/story.aspx?ref=archive&id=176813 Accessed December 2012. [Google Scholar]
- 8.Centers for Disease Control and Prevention. BMI for children and teens. Atlanta, GA, USA: CDC; http://m.cdc.gov/en/HealthSafetyTopics/HealthyLiving/HealthyWeight/AssessingYourWeight/BodyMassIndex/BMIChildrenTeens Accessed December 2012. [Google Scholar]
- 9.Von Elm E, Altman D G, Egger M, Pocock S J, Gøtzsche P C, Vandenbroucke J P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85:867–872. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edginton M, Enarson D, Zachariah R, et al. Why ethics is indispensable for good-quality operational research. Public Health Action. 2012;2:21–22. doi: 10.5588/pha.12.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]