Abstract
Setting:
All tuberculosis (TB) registration sites in Bhutan.
Design:
Cross-sectional study involving a retrospective review of TB registers and TB treatment cards.
Objectives:
To determine: 1) the number and proportion of all TB cases registered as extra-pulmonary TB (EPTB) from 2001 to 2010, 2) the age and sex of the patients and the categories and types of EPTB registered in 2010, and 3) their treatment outcomes.
Results:
The proportion of all TB cases registered as EPTB over a period of 10 years varied from 30% to 40%. In 2010, 505 patients were registered with EPTB, of whom 50% were male, 21% were children, and 96% were new EPTB cases. TB lymph node enlargement and pleural effusion were the two most common types of EPTB, accounting for 67%, followed by abdominal TB and spinal/bone/kidney disease. The overall treatment success rate was 90%, and was generally similar with respect to sex, age and different types of EPTB.
Conclusion:
Bhutan has a high proportion of patients registered as having EPTB, for whom treatment outcomes are satisfactory. Further work is needed to better understand how EPTB is diagnosed throughout the country.
Keywords: Bhutan, tuberculosis, EPTB, treatment outcomes
Abstract
Contexte:
Tous les sites d’enregistrement de la tuberculose (TB) au Bhutan.
Schéma:
Etude transversale comportant une revue rétrospective des registres TB et des cartes de traitement TB.
Objectifs:
Déterminer : 1) le nombre et la proportion de l’ensemble des cas de TB enregistrés comme TB extra-pulmonaire (EPTB) entre 2001 et 2010, 2) l’âge et le sexe des patients et les catégories et types de EPTB enregistrées en 2010, et 3) les résultats de leur traitement.
Résultats:
La proportion de l’ensemble des cas TB enregistrés comme EPTB a varié au cours des 10 années de 30% à 40%. En 2010, 505 patients ont été enregistrés comme EPTB, dont 50% étaient de sexe masculin, 21% étaient des enfants et 96% des nouveaux cas d’EPTB. Les hypertrophies des ganglions lymphatiques TB et les épanchements pleuraux ont constitué les deux types les plus courants d’EPTB (67%), suivis par la TB abdominale et la TB de la colonne vertébrale, des os ou des reins. Le taux global de succès du traitement a été de 90% et a été généralement similaire quels que soient le sexe, l’âge et les différents types d’EPTB.
Conclusion:
Il existe au Buthan une proportion élevée de patients enregistrés comme EPTB pour lesquels les résultats du traitement sont bons. Il y a lieu de veiller à l’avenir à mieux comprendre la façon dont le diagnostic d’EPTB est assuré dans l’ensemble du pays.
Abstract
Marco de referencia:
Todos los centros de registro de la tuberculosis (TB) en Bután.
Método:
Fue este un estudio transversal en el cual se llevó a cabo un examen retrospectivo de los registros y las tarjetas de tratamiento de la TB.
Objetivos:
Determinar: 1) el número y la proporción de todos los casos de TB que se registraron como TB extra-pulmonar (EPTB) entre el 2001 y el 2010, 2) analizar la edad y el sexo de los pacientes y las categorías y tipos de EPTB registrados en el 2010, y 3) describir los desenlaces terapéuticos.
Resultados:
La proporción de EPTB en todos los casos de TB registrados en los 10 años osciló entre 30% y 40%. En el 2010, se registraron 505 pacientes con EPTB, de los cuales el 50% eran de sexo masculino, el 21% eran niños y el 96% se trataba de casos nuevos de EPTB. Las presentaciones clínicas más frecuentes fueron las adenomegalias y el derrame pleural de origen tuberculoso en un 67% de los casos, seguidos por la TB abdominal, medular, ósea y renal. La tasa global de éxito terapéutico fue 90% sin variaciones evidentes con respecto al sexo, la edad ni a los diferentes tipos de enfermedad.
Conclusión:
Bután presenta una alta proporción de pacientes registrados con EPTB que alcanzan desenlaces terapéuticos favorables. Se precisan nuevos estudios con el fin de comprender mejor la forma como se establece este diagnóstico en todo el territorio nacional.
Bhutan is a small, mountainous landlocked country, bordered in the north by the Tibetan autonomous region of China and by India in the south. Although Bhutan was once considered one of the low tuberculosis (TB) burden countries in South-East Asia, TB has become one of the main public health concerns in the country.1
The TB epidemic has affected all age groups in Bhutan, particularly adults aged 15–64 years.1 The Bhutan’s National Tuberculosis Control Programme (NTCP) was established in 1986, and the internationally recommended DOTS strategy for TB control was introduced in 1997.1 There has been steady progress, and through the NTCP’s efforts the country has achieved global targets of case detection and treatment success rates (cured plus treatment completed).1
While the number of TB case notifications has remained fairly constant in the last 10 years, there have been concerns for some time about the large proportion of TB patients registered with extra-pulmonary TB (EPTB).1,2 There is no published information to date from Bhutan on the age and sex of EPTB patients, EPTB types commonly registered and their specific treatment outcomes. A study was therefore undertaken to document the burden and treatment outcomes of EPTB cases registered under Bhutan’s NTCP.
Specific objectives were to determine: 1) the trend in the number and proportion of all TB cases registered as EPTB over the 10-year period from 2001 to 2010; 2) the age and sex of the patients as well as the categories and types of EPTB registered under the NTCP in 2010; and 3) TB treatment outcomes of patients with different types of EPTB registered in 2010.
METHODS
Study design
This was a cross-sectional study involving a retrospective review of TB registers and TB treatment cards.
Setting
Bhutan is a small country that covers a geographic area of 38 394 km2, and has a population of around 708 265, with a population density of 18.4/km2.3 The Royal Government of Bhutan provides free primary health care services to all its citizens. There is no private sector in Bhutan for any form of health care, including for TB.
TB control in the country is the sole responsibility of the NTCP and other relevant partners. In 2011, the reported TB case notification rate was 174 per 100 000 population, and the treatment success rate in new smear-positive pulmonary TB (PTB) was 90% (NTCP, Bhutan).4 Bhutan has a low national prevalence (0.1%) of human immunodeficiency virus infection/acquired immunodeficiency syndrome (HIV/AIDS); there are currently 270 HIV/AIDS patients in the country (135 males and 135 females).5 HIV prevalence among TB patients has been reported as zero in Bhutan.6,7 In 2012, a cross-sectional study on the prevalence of HIV among 150 sampled TB patients conducted by the Bhutan NTCP also reported that there were no cases of HIV infection (TJ, personal observation).
The Bhutan NTCP is a nationwide programme integrated into the general health care system. Bhutan follows a three-tiered health care system, with 181 basic health units (BHUs) at the local level, 29 hospitals and three regional referral hospitals, of which one operates as a national referral hospital. Most BHUs are staffed by trained health assistants. Four BHUs graded as BHU-I are staffed with a medical doctor; these, along with each district hospital and the three regional referral hospitals, act as TB Registration Units. There are 32 such units in Bhutan. Patients with presumptive TB are referred to the TB Registration Units for diagnosis, registration and initial treatment, and all follow national TB control guidelines, which are based on World Health Organization guidelines.8 Each TB Registration Unit is run by a District TB Officer.
PTB is diagnosed by sputum smear microscopy, and chest radiography is performed in those with negative sputum smears. Patients with EPTB are diagnosed on clinical grounds, using X-ray or ultrasound, examination of fluids (e.g., pleural or cerebrospinal fluid), histology when available and circumstantial evidence. Patients are registered with one type of TB: patients diagnosed with PTB and EPTB are registered as having PTB. For those with EPTB, only one site of disease is usually recorded; however, patients with multiple sites of infection are registered as ‘disseminated disease’.
After diagnosis and registration, TB patients are treated for the first 2 weeks in hospital, followed by referral back to the community to receive the remaining treatment from either the BHU or the TB Registration Unit. All new patients, including those with EPTB, are generally treated with a 6-month regimen consisting of rifampicin throughout (Category I), while patients with recurrent TB are treated with a standardised retreatment regimen (Category II).1,8 All such patients are registered in TB registers maintained in the TB Registration Units. Age, sex, category and type of TB are recorded in the TB registers and TB treatment cards. Patients are monitored throughout treatment using the TB treatment cards, and information on final treatment outcomes is recorded on the TB treatment cards. This information is subsequently recorded in the TB patient register.
Study participants
The numbers of TB patients (all types, including EPTB) diagnosed and registered in Bhutan were documented between 2001 and 2010. For patients registered with EPTB in 2010, detailed information was collected on age, sex, category and type of EPTB and treatment outcomes.
Data variables
Data variables were collected between July and August 2012 in relation to the three objectives of the study into a structured proforma by the primary investigator (TJ) assisted by five staff members from the Ministry of Health. Three teams, comprising two members each, were trained over one day and travelled to the three assigned regions for data collection (this included 30 of the 32 TB Registration Units, because two were not yet fully functional in 2010).
Data variables were collected as follows: 1) the number of TB and EPTB patients registered between 2001 and 2010 was obtained from annual health bulletins held in the Health Management and Information System (HMIS) and TB reports from the NTCP; and 2) data on EPTB patients were collected from the TB patient registers and TB treatment cards at each of the TB Registration Units.
The variables included district name, TB Registration Unit, TB registration number (unique), age, sex, type and category of TB, different types of EPTB, TB treatment regimens and TB treatment outcomes. Patients with disseminated disease and those with rare types of EPTB, such as pericardial effusion, ocular TB and TB epididymitis, were classified under ‘other’.
Data entry, analysis and statistics
The data in the structured proforma were extracted and double-entered into the electronic database EpiData, version 3.1 (EpiData Association, Odense, Denmark), and validated for data verification. The analysis was performed using the statistical package STATA version 11.1 (Stata Corporation, College Station, TX, USA). Categorical variables were analysed using the χ2 test, with differences at 5% accepted as statistically significant. Odds ratios (OR), their 95% confidence intervals (CI) and P values were calculated as appropriate.
Ethics
Ethical approval for the study was obtained from the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France, and from the Research Ethics Board of Health, Bhutan. Permission to conduct the study was accorded by the NTCP, Ministry of Health, Bhutan.
RESULTS
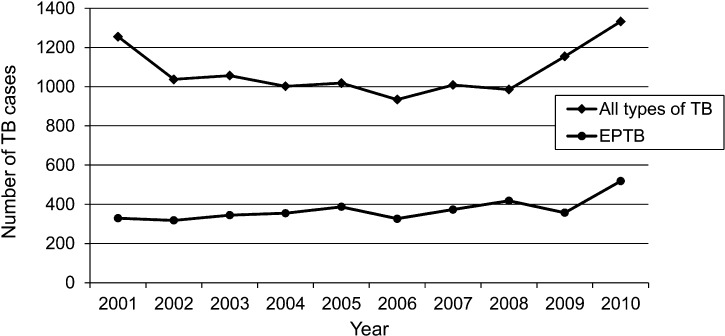
The number and proportion of all TB cases and those registered as EPTB cases from 2001 to 2010 are shown in the Figure. In 2001, there were a total of 1255 TB patients, after which the number decreased and levelled out until 2008, when the number of cases increased to 1332 in 2010. In 2001, 26% of TB patients had EPTB; in the intervening years, the proportion varied from 31% to 42%, and in 2010 it was 39%.
FIGURE.
Trend in reported numbers of all types of TB and EPTB in Bhutan, 2001–2010. TB = tuberculosis; EPTB = extra-pulmonary tuberculosis.
In 2010, a total of 505 patients were registered with EPTB: this number excludes 30 children with TB pneumonia who had been incorrectly classified as having EPTB from the registers and national reports. The different types of EPTB are shown in Table 1. TB lymph node disease and pleural effusion were responsible for 67% of all EPTB cases; other common types were abdominal TB/ascites and spinal/bone and kidney disease.
TABLE 1.
Types of EPTB among all registered cases in Bhutan, 2010
| Type of EPTB | n (%) |
| Lymph node | 195 (39) |
| Pleural effusion | 143 (28) |
| Abdominal TB/TB ascites | 46 (9) |
| Spinal/bone | 14 (3) |
| Kidney disease | 14 (3) |
| Miliary | 7 (1) |
| Meningitis | 7 (1) |
| Skin | 3 (1) |
| Disseminated disease and other sites* | 40 (8) |
| Site not recorded | 36 (7) |
| Total | 505 (100) |
Disseminated TB, i.e., TB in more than one extra-pulmonary site. Other sites: pericardial TB, eye disease/ocular TB, epididymitis, empyema/lung abscess, arthritis TB, rhinitis TB, etc.
EPTB = extra-pulmonary tuberculosis; TB = tuberculosis.
Patient characteristics such as sex, age and category of TB in relation to the different types of EPTB are shown in Table 2. In 2010, the mean age of EPTB patients was 28 years (±17). For all types of EPTB, the male:female ratio was similar, 21% were children aged ≤14 years, and most were new cases of EPTB. Among patients with the two main types of EPTB (lymph node disease and pleural effusion), significantly more females (OR 1.87, 95%CI 1.2–2.9, P < 0.01) and children (OR 3.0, 95%CI 1.6–5.4, P < 0.001) had lymph node disease compared with pleural effusion. Comparisons of characteristics of other types of EPTB were either not significant or were not made (for example, with patients categorised as ‘other’, which included a mix of different types of diseases).
TABLE 2.
Sex, age and category of disease in relation to different types of EPTB in Bhutan, 2010
| Variable | All patients n (%) | Type of EPTB |
Site not recorded n (%) | ||||
| Lymph node n (%) | Pleural effusion n (%) | Abdominal/ascites n (%) | Spinal/bone/renal n (%) | Other n (%)* | |||
| Total | 505 | 195 | 143 | 46 | 28 | 57 | 36 |
| Sex | |||||||
| Male | 251 (50) | 87 (45) | 86 (60) | 26 (57) | 12 (43) | 19 (33) | 21 (58) |
| Female | 254 (50) | 108 (55) | 57 (40) | 20 (43) | 16 (57) | 38 (67) | 15 (42) |
| Age group, years | |||||||
| 0–4 | 38 (8) | 23 (12) | 5 (4) | 0 | 0 | 7 (12) | 3 (8) |
| 5–14 | 67 (13) | 33 (17) | 12 (8) | 7 (15) | 1 (3) | 7 (12) | 7 (19) |
| 15–49 | 339 (67) | 130 (67) | 99 (69) | 34 (74) | 22 (79) | 35 (61) | 20 (56) |
| ≥50 | 61 (12) | 9 (4) | 27 (19) | 5 (11) | 5 (18) | 9 (15) | 6 (17) |
| Category | |||||||
| New | 485 (96) | 182 (93) | 141 (98) | 45 (98) | 27 (96) | 55 (96) | 35 (97) |
| Recurrent | 5 (1) | 4 (2) | 0 | 0 | 1 (4) | 0 | 0 |
| Not specified† | 15 (3) | 9 (5) | 2 (2) | 1 (2) | 0 | 2 (4) | 1 (3) |
Miliary tuberculosis (TB), meningitis, skin, disseminated disease and other organ involvement.
A patient for whom there is no information about TB category.
EPTB = extra-pulmonary tuberculosis.
The variation in the number and proportion of EPTB cases in 2010 across different types of health facilities is shown in Table 3. The national referral hospital registered the highest number of cases, followed by the regional referral hospitals, other district hospitals and BHUs.
TABLE 3.
Number and proportion of EPTB patients by health facility type in Bhutan, 2010 (N = 505)
| TB Registration Unit | n (%) |
| National referral hospital (n = 1)* | 208 (41) |
| Regional referral hospitals (n = 2)† | 115 (23) |
| Phuentsholing Hospital | 39 (8) |
| Trashigang Hospital | 24 (5) |
| Lungtenphu RBA Hospital | 23 (4) |
| Samtse Hospital | 15 (3) |
| Other district hospitals (n = 19)‡ | 74 (15) |
| BHU-I (n = 4)§ | 7 (1) |
Jigme Dorji Wangchuck National Referral Hospital.
Monggar Eastern Regional Referral Hospital and Gelephu Central Regional Referral Hospital.
Bumthang, Damphu, Deothang, Dagana, Dagapela, Gedu, Gidakom, Gomtu, Lhuentse, Paro, Pemagatshel, Punakha, Reserboo, Sipsoo, Samdrup Jongkhar, Trongsa, Tsimalakha, Trashiyangtse, Yebilaptsa.
Bajo, Bali, Gasa and Lhamoizingkha.
EPTB = extra-pulmonary tuberculosis; TB = tuberculosis; RBA = Royal Bhutan Army; BHU-I = basic health unit grade I.
TB treatment outcomes in patients by sex, age, type of EPTB and category of disease are shown in Table 4. The treatment success rate was 90% overall, and was similar in relation to age, sex, type and category of EPTB. The only significant and clinically important difference was that the death rate in patients with pleural effusion was higher than in those with lymph node disease (OR 7.2, 95%CI 1.6–34.0, P < 0.05).
TABLE 4.
Treatment outcomes in relation to sex, age, type and category of EPTB in Bhutan, 2010
| Variable | Starting TB treatment n | Treatment success n (%) | Died n (%) | Lost to follow-up n (%)* | Unknown outcome n (%)† |
| All patients | 505 | 456 (90) | 19 (4) | 13 (2) | 17 (4) |
| Sex | |||||
| Male | 251 | 231 (92) | 13 (5) | 3 (1) | 4 (2) |
| Female | 254 | 225 (89) | 6 (2) | 10 (4) | 13 (5) |
| Age group, years | |||||
| 0–4 | 38 | 35 (92) | 1 (3) | 2 (5) | 0 |
| 5–14 | 67 | 65 (97) | 1 (2) | 0 | 1 (1) |
| 15–49 | 339 | 308 (91) | 11 (3) | 8 (2) | 12 (4) |
| ≥50 | 61 | 48 (79) | 6 (10) | 3 (5) | 4 (6) |
| Type of EPTB | |||||
| Lymph node | 195 | 181 (93) | 2 (1) | 7 (4) | 5 (2) |
| Pleural effusion | 143 | 127 (89) | 10 (7) | 2 (1) | 4 (3) |
| Abdominal/ascites | 46 | 45 (98) | 1 (2) | 0 | 0 |
| Spinal/bone/renal | 28 | 26 (92) | 1 (4) | 0 | 1 (4) |
| Other‡ | 57 | 46 (81) | 5 (9) | 2 (3) | 4 (7) |
| Site not recorded | 36 | 31 (86) | 0 | 2 (6) | 3 (8) |
| Category | |||||
| New | 485 | 437 (90) | 18 (4) | 13 (3) | 17 (3) |
| Recurrent | 5 | 4 (80) | 1 (20) | 0 | 0 |
| Not specified§ | 15 | 15 (100) | 0 | 0 | 0 |
Defaulted.
A patient for whom there is no information about the treatment outcome.
Miliary TB, meningitis, skin and other organ involvement.
A patient for whom there is no information about TB category.
EPTB = extra-pulmonary tuberculosis; TB = tuberculosis.
DISCUSSION
This is the first study in Bhutan to systematically analyse registered trends in EPTB, different types of EPTB and their treatment outcomes. The proportion of all TB cases registered as EPTB was high, at between 30% and 40%, with notification rates having particularly increased in the last 2 years. We did not compute case notification rates per 100 000 population, as accurate numbers were available only from 2005. Although the number and proportion of EPTB cases in our study were high, these findings are not inconsistent with published studies from elsewhere, where similar observations have been made.9,10
The precise reasons for the high proportion of EPTB cases in Bhutan are not known and no in-depth studies have addressed this issue. Possible reasons include over-diagnosis of EPTB by medical doctors or specialists, an increasing number of medical specialists in the country and better equipped facilities over the study period using diagnostic tools such as fine needle aspiration cytology, X-ray, ultrasound, histology services and computerised tomography scanning facilities in the main referral hospital. These reasons are in line with observations in 2010, which showed that the majority of EPTB cases were diagnosed in the national or regional referral hospitals.
The varying trends in notifications of PTB and EPTB over the 10-year period could also be due to more focus being placed on PTB as the more infectious type of disease,11 and a high turnover in trained TB staff during the same time period. Support from the Bhutan’s Global Fund to Fight AIDS, Tuberculosis and Malaria Round 4 grant from 2004, which targeted better case detection, might also have helped to increase TB notifications from 2008 onwards.
An in-depth analysis for the year 2010 showed that the most common types of EPTB were TB lymph node disease and pleural effusion, and that these were responsible for two thirds of EPTB cases. These findings are consistent with other published studies.9–15 Similarly, the findings that more females and more children had lymph node disease compared with pleural effusion are in line with other reports.9–14,16
Overall treatment outcomes in EPTB patients, stratified by type of disease were good, with treatment success rates of ≥90% being documented. The treatment success rates were similar between males and females and across the different age groups. Those with recurrent TB did not fare as well as those with new TB, but the numbers were too small for a proper analysis. Higher death rates in those with pleural effusion compared with lymph node disease may be due to the fact that patients with pleural effusion sometimes have associated underlying pulmonary disease, which can influence the prognosis.
The strengths of this study were that we obtained a full national sample of patients and that the study design, methodology and report followed the recommendations from the STROBE (strengthening the reporting of observational studies in epidemiology) guidelines.17 The limitations are those related to any operational research study, and include inaccuracies and incompleteness of register and treatment card reviews. It would have been useful to assess EPTB in relation to patients’ residence (urban or rural settings), but this variable was incompletely recorded and also may not have been reliable in the registers and treatment cards. Furthermore, patients seeking treatment outside the country or across the border in neighbouring areas were not included in the study.
As this was a register and treatment card review, we have no information as to how EPTB was diagnosed. For example, although the national guidelines recommend that TB lymph node disease be diagnosed with fine needle aspiration and/or histology and TB pleural effusion on the basis of pleural fluid examination for cells, protein and acid-fast bacilli, we do not know if these recommendations were followed by health care staff. Abdominal TB and TB ascites are also notoriously difficult to diagnose, and this warrants further assessment.18,19 Other studies on EPTB from other parts of the world suggest that guidelines are not always followed and that diagnoses are made on the basis of clinical examination or circumstantial evidence only.20–23
This study has some important implications. First, it will be necessary to conduct a survey to assess how EPTB is diagnosed across the country, and this is likely to vary depending on the health facility, its infrastructure, laboratory and radiographic services and trained health care personnel. Second, in the registers and quarterly reports, TB pneumonia had been incorrectly included in the diagnosis of EPTB, especially in children. It will be important to train clinicians and TB officers responsible for registration to ensure these mistakes do not happen in the future. Third, the high rate of EPTB in Bhutan might be due to poor case detection of PTB; this requires further assessment by examining case detection strategies in the country.
CONCLUSION
Bhutan has a high proportion of patients registered with EPTB. The most common types are lymph node disease and pleural effusion. Overall treatment success rates are good, irrespective of age, sex and type of EPTB. Further work is needed to better understand how EPTB is diagnosed in Bhutan.
Acknowledgments
The authors thank the Royal Government of Bhutan for financial support, especially for data collection. They also thank the District TB Officers for their cooperation and all other personnel from the Ministry of Health, in particular, R S Das, Dopo, T Dendup, P Dorji and P Wangdi for their assistance in data collection.
This research was supported through an operational research course that was jointly developed and run by the Centre for Operational Research, International Union Against Tuberculosis and Lung Disease (The Union); The Union South-East Asia Office, Delhi, India; the Operational Research Unit, Médecins Sans Frontières, Brussels Operational Centre, Luxembourg.
Funding for the course came from an anonymous donor and the Department for International Development, UK.
Conflict of interest: none declared.
References
- 1.National Tuberculosis Control Programme. Guidelines for the management of tuberculosis. 5th ed. Thimpu, Bhutan: Department of Public Health, Ministry of Health, Royal Government of Bhutan, NTCP; 2010. [Google Scholar]
- 2.Health Management and Information System. Annual health bulletin. Ministry of Health, Royal Government of Bhutan, 2001–2011. Thimpu, Bhutan: HMIS; 2001–2011. http://www.health.gov.bt/bulletin.php Accessed February 2013. [Google Scholar]
- 3.National Statistics Bureau, Royal Government of Bhutan. Statistical year book of Bhutan 2011. Thimpu, Bhutan: NSB; 2011. http://www.nsb.gov.bt/index.php?id=13 Accessed February 2013. [Google Scholar]
- 4.World Health Organization. Global tuberculosis report 2012. WHO/HTM/TB/ 2012.6. Geneva, Switzerland: WHO; 2012. http://www.who.int/tb/publications/global_report/en/ Accessed February 2013. [Google Scholar]
- 5.National HIV/AIDS Control Programme, Royal Government of Bhutan. Report on HIV/AIDS epidemic updates. Thimpu, Bhutan: National HIV/AIDS Control Programme; 2011. [Google Scholar]
- 6.National HIV/AIDS Control Programme, Royal Government of Bhutan. National strategic plan for the prevention and control of STIs and HIV and AIDS. Thimpu, Bhutan: National HIV/AIDS Control Programme; 2008. [Google Scholar]
- 7.Jha K K, Salhotra V S, Weerakoon A P. Epidemiology of TB-HIV co-infection in the SAARC region and regional efforts to contain it. Vienna, Austria: International AIDS Conference, AIDS 2010–XVIII. Abstract WEPE0968; http://www.iasociety.org/Abstracts/A200736894.aspx Accessed March 2013. [Google Scholar]
- 8.World Health Organization. Treatment of tuberculosis: guidelines for national programmes. 4th ed, 2010. WHO/HTM/TB/2009.420. Geneva, Switzerland: WHO; 2010. http://www.who.int/tb/publications/tb_treatmentguidelines/en/ Accessed February 2013. [Google Scholar]
- 9.Rock R B, Sutherland W M, Baker C, Williams D N. Extra-pulmonary tuberculosis among Somalis in Minnesota. Emerg Infect Dis. 2006;12:1434–1436. doi: 10.3201/eid1209.050295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kruijshaar M E, Abubakar I. Increase in extra-pulmonary tuberculosis in England and Wales, 1999–2006. Thorax. 2009;64:1090–1095. doi: 10.1136/thx.2009.118133. [DOI] [PubMed] [Google Scholar]
- 11.Arora V K, Gupta R. Trends of extra-pulmonary tuberculosis under revised National Tuberculosis Control Programme: a study from South Delhi. Indian J Tuberc. 2006;53:77–83. [Google Scholar]
- 12.Peto H M, Pratt R H, Harrington T A, et al. Epidemiology of extra-pulmonary tuberculosis in the United States, 1993–2006. Clin Infect Dis. 2009;49:1350–1357. doi: 10.1086/605559. [DOI] [PubMed] [Google Scholar]
- 13.Zhang X, Andersen A B, Lillebaek T, et al. Effect of sex, age, and race on the clinical presentation of tuberculosis: a 15-year population-based study. Am J Trop Med Hyg. 2011;85:285–290. doi: 10.4269/ajtmh.2011.10-0630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gonzalez O Y, Adams G, Teeter L D, Bui T T, Musser J M, Graviss E A. Extra-pulmonary manifestations in a large metropolitan area with a low incidence of tuberculosis. Int J Tuberc Lung Dis. 2003;7:1178–1185. [PubMed] [Google Scholar]
- 15.Kourbatova E V, Leonard M K, Romero J, Kraft C, Rio del C, Blumberg H M. Risk factors for mortality among patients with extra-pulmonary tuberculosis at an academic inner-city hospital in the US. Eur J Epidemiol. 2006;21:715–721. doi: 10.1007/s10654-006-9060-7. [DOI] [PubMed] [Google Scholar]
- 16.Forssbohm M, Zwahlen M, Loddenkemper R, Rieder H L. Demographic characteristics of patients with extra-pulmonary tuberculosis in Germany. Eur Respir J. 2008;31:99–105. doi: 10.1183/09031936.00020607. [DOI] [PubMed] [Google Scholar]
- 17.von Elm E, Altman D G, Egger M, Pocock S J, Gotzsche P C, Vandenbroucke J P. STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85:867–872. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vanhoenacker F M, De Backer A I, Op de Beeck B, et al. Imaging of gastrointestinal and abdominal tuberculosis. Eur Radiol. 2004;14:103–115. doi: 10.1007/s00330-003-2047-9. [DOI] [PubMed] [Google Scholar]
- 19.Rigouts L. Clinical practice: diagnosis of childhood tuberculosis. Eur J Pediatr. 2009;168:1285–1290. doi: 10.1007/s00431-009-0988-y. [DOI] [PubMed] [Google Scholar]
- 20.Richter C, Ndosi B, Mwammy A S, Mbwanbo R K. Extra-pulmonary tuberculosis: a simple diagnosis? Trop Geogr Med. 1991;43:375–378. [PubMed] [Google Scholar]
- 21.Richter C, Perenboom R, Swai A B M, et al. Diagnosis of tuberculosis in patients with pleural effusion in an area of HIV infection and limited diagnostic facilities. Trop Geogr Med. 1994;46:293–297. [PubMed] [Google Scholar]
- 22.Harries A D, Hargreaves N J, Kwanjana J H, Salaniponi F M. The diagnosis of extra-pulmonary tuberculosis in Malawi. Trop Doct. 2003;33:7–11. doi: 10.1177/004947550303300106. [DOI] [PubMed] [Google Scholar]
- 23.Weismuller M M, Graham S M, Claessens N J M, Meijnen S, Salaniponi F M, Harries A D. Diagnosis of childhood tuberculosis in Malawi: an audit of hospital practice. Int J Tuberc Lung Dis. 2002;6:432–438. [PubMed] [Google Scholar]