Abstract
This cross-sectional multi-centric study compared the yield of and potential benefit for detecting smear-positive pulmonary tuberculosis (PTB) by bleach sedimentation (2% sodium-hypochlorite) versus direct microscopy under programme conditions in India. Among 3168 PTB suspects, 684 (21.6%) were detected by bleach sedimentation vs. 625 (19.7%) by direct microscopy, with a proportional overall agreement of 96% (κ = 0.88). While 594 patients were smear-positive with both methods, 31 patients detected by direct microscopy were missed and an additional 90 patients were detected by bleach sedimentation. Overall, bleach sedimentation increased the yield of smear-positive TB detection; however; it also increased the time to results.
Keywords: bleach sedimentation, bleach smears, direct smears, TB diagnosis, conventional microscopy
Abstract
Cette étude transversale multicentrique a comparé, dans les conditions du programme en Inde, le rendement et les avantages potentiels de la détection des tuberculoses pulmonaires (TBP) à frottis positif par la sédimentation à l’eau de Javel (2% d’hypochlorite de sodium) par comparaison avec l’examen microscopique direct. Parmi 3168 sujets suspects de TBP, 684 (21,6%) ont été détectés par la sédimentation à l’eau de Javel par rapport à 625 (19,7%) par l’examen microscopique direct, avec donc une proportion de 96% de concordance globale (κ = 0,88). Alors que les résultats des frottis étaient positifs chez 594 patients par les deux méthodes, l’examen microscopique direct a raté la détection chez 31 patients et la sédimentation à l’eau de Javel a détecté 90 patients de plus. Au total, la sédimentation à l’eau de Javel a augmenté le rendement de la détection des TB à frottis positif, mais a prolongé la durée avant obtention des résultats.
Abstract
En un estudio transversal multicéntrico se comparó el rendimiento y la posible utilidad de la detección de la tuberculosis (TB) con baciloscopia positiva mediante la concentración del esputo con hipoclorito de sodio (2%) y se comparó esta técnica con el examen microscópico directo, en las condiciones del programa nacional de la India. En los 3168 pacientes con presunción clínica de TB se detectaron 684 casos (21,6%) por el método de la sedimentación con lejía y 625 casos (19,7%) mediante la microscopia directa, lo cual ofrece una concordancia global del 96% (índice κ = 0,88). Quinientos noventa y cuatro pacientes presentaron baciloscopias positivas con ambas técnicas; con la técnica de sedimentación se pasaron por alto 31 de los pacientes diagnosticados por microscopia directa y la concentración con lejía permitió el diagnóstico de 90 pacientes suplementarios. En términos generales, la sedimentación con lejía aumentó el rendimiento de la detección de casos de tuberculosis con baciloscopia positiva, pero prolongó el lapso hasta la obtención de los resultados.
Sputum microscopy is the most widely used test for the diagnosis of pulmonary tuberculosis (PTB) globally. Although alternative diagnostic methods such as culture and molecular tests are more sensitive and specific, they are expensive and often difficult to implement in resource-limited settings.1
Direct smear microscopy has been used as the primary tool for diagnosis of PTB in India for more than a decade.2 Its sensitivity ranges between 20% and 80%, and it requires two specimens collected over 1–2 days.3 It can only detect bacilli when there are ≥104 bacilli/ml of sputum,4 and according to the Global Plan to Stop TB 2006–2015 the method needs optimisation.5
Previous studies have demonstrated that concentration of sputum by various methods significantly increases the yield of PTB cases by conventional light and light-emitting diode fluorescence microscopy (LED-FM).6,7 Most studies used varying chemical methods and sedimentation methods, were based on a small sample, or were conducted at specialised centres.7 While studies on optimising microscopy have been performed in reference laboratories, no studies have been reported under routine programme conditions in India. One method, the bleach (2% sodium-hypochlorite [NaOCl]) sedimentation technique for concentration of sputum, has been reported to be simple, cost-effective and safe.8,9
This study compared the yield of and potential benefit for detecting smear-positive PTB by bleach sedimentation versus direct microscopy under programme conditions in India.
METHODS
This was a cross-sectional, multi-centric study conducted in 10 conveniently selected designated microscopy centres (DMCs), five each in Andra Pradesh and Madhya Pradesh. All PTB suspects presenting at study DMCs, staggered over a 3–5 month period from January to July 2011, were enrolled in the study. Per national guidelines, two specimens containing ≥2 ml of sputum, one spot and the other collected overnight, were processed for direct smear microscopy.2 The remnants were blinded by a neutral officer and further processed by Bonnet’s technique to homogenise each specimen with an equal volume of 2% NaOCl* (manual inversion for 30 s and overnight gravity sedimentation at room temperature for 15–18 h).9,10
An external quality assurance protocol was fol-lowed in each DMC, including cross-verification of sample slides and random blinded repeat slide reading per Revised National Tuberculosis Control Programme (RNTCP) guidelines.2 Both direct and sedimented smears were examined by conventional Ziehl-Neelsen (ZN) microscopy.
Sputum smear-positive TB was defined as at least one specimen with acid-fast bacilli (AFB) detected by ZN microscopy. Only PTB suspects with results available for all four smears (i.e., two direct and two sedimented) were included in the study. The number of smear-positive TB cases diagnosed from direct and sedimentation methods were compared for the level of agreement, along with the number of patients obtained in addition or lost if only the sedimented smears were used, using κ statistic.
The study was implemented under routine programmatic settings to assess the feasibility of this intervention under field conditions. The protocol was approved by the ethics committee of the National Tuberculosis Institute of India and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease.
RESULTS
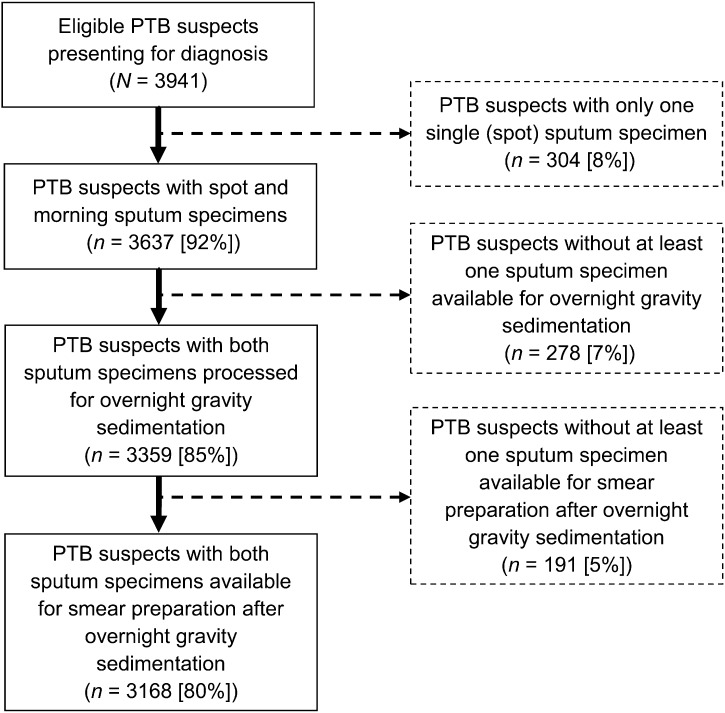
Of 3941 PTB suspects enrolled, 304 (8%) were excluded due to non-availability of a second sample, 278 (7%) due to an inadequate remnant (<2 ml), and 191 (5%) due to lost sediments or lysed samples (Figure).
FIGURE.
Study inclusion criteria for PTB suspects in select designated microscopy centres in Andhra Pradesh and Madhya Pradesh, India, January–July 2011. PTB = pulmonary tuberculosis.
Of 3168 PTB suspects included in the study, 715 smear-positive TB cases were detected by either method. We found case positivity concordance with 594 cases and case negativity concordance with 2453 cases, with overall agreement in 96% of the results (κ = 0.88; Table). While sedimented smears detected an additional 90 (12.6%) cases, direct smears detected 31 (4.3%) cases missed by sedimented smears. In terms of effort, the number of PTB suspects needed to screen to detect one smear-positive case was reduced from 5.1 by the direct smear method to 4.6 by the sedimentation method. This reduction came at a cost, however, as the time to result increased by 15–18 h. There was no difference in laboratory performance: the results of external quality assurance at each site were within national standards.
TABLE.
Matched pair comparison of direct smear and bleach-sedimented smear among pulmonary tuberculosis suspects in select designated microscopy centres, Andhra Pradesh and Madhya Pradesh, India, January–July 2011
| Methodology | Bleach-sedimented smear |
Proportion of overall agreement (κ)* | Continuity-corrected χ2 (P value) | ||
| Positive | Negative | Total | |||
| Direct smear | |||||
| Positive | 594 | 31 | 625 | ||
| Negative | 90 | 2453 | 2543 | 0.96 (0.88) | 27.8 (<0.0001) |
| Total | 684 | 2484 | 3168 | ||
Proportion of overall agreement ( p0 = a + d/a + b + c + d ).
DISCUSSION
Bleach sedimentation improves case detection by ∼10% compared to direct smear using conventional light microscopy. This was comparable with other World Health Organization endorsed methods for optimisation of sputum examination.5 This increase in case detection may be important in high-burden countries such as India, where even nominal increases could translate into large absolute numbers.
However, the bleach sedimentation method increased the workload of the laboratory technicians as well as the time to result, due to an inherent procedural delay of 15–18 h, despite adding negligible material expense. It remains unclear if bleach sedimentation, when combined with other techniques, such as LED-FM, could yield a higher smear-positive detection rate, shorten the examination time and lower the unit examination cost as compared to traditional ZN microscopy. At the conclusion of this study, the RNTCP revealed a plan to distribute 2600 LED-FM microscopes by 2015. It should be noted, however, that it may take several more years for LED-FM to completely replace conventional light microscopy in the >13 000 DMCs throughout India. More research is needed to determine if LED-FM may be an alternative to ZN as a cost-effective method for detecting AFB in peripheral laboratories of India.
The study was conducted in peripheral diagnostic centres with existing staff and minimal infrastructure, training and supervision. As the DMCs did not have access to culture methods, the sensitivity and specificity of sedimentation could not be studied. Because the study was carried out as part of a time-bound operational research course, we were unable to follow patients through time and ascertain reasons for loss of sediments and lyses of samples. It remains unclear if the smear-positive cases were missed by sedimented smears due to overexposure to bleach by overnight sedimentation in 2% bleach and/or lack of specific skills of peripheral staff.
CONCLUSION
Bleach sedimentation improved the overall detection of smear-positive TB cases compared to direct microscopy. However, staff workload, time to results, procedural difficulties and the proportion of PTB cases missed by bleach sedimentation needs to be considered, especially when other simple optimisation techniques are available.
Acknowledgments
The authors are grateful to the state TB programme managers of Andhra Pradesh and Madhya Pradesh, the District TB programme managers of all study Designated Microscopy Centres (DMCs), all the nodal officers and the laboratory technicians of the study DMCs for their useful contributions to the study.
The study was conducted as a part of the ‘TB Operations Research Training Project’ aimed to build operational research capacity within the Government of India’s RNTCP. This training project was conceived and implemented jointly by the Central TB Division (Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India), The National TB Institute (Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India, Bangalore, India), the World Health Organization (WHO; India Country Office), the International Union Against Tuberculosis and Lung Disease (The Union; South-East Asia Regional Office, New Delhi, India) and the US Centers for Disease Control and Prevention (CDC; Division of TB Elimination, Atlanta, GA, USA). Funding support was provided in part by The Union from Global Fund Round 9 India TB Project funds and by WHO-India from United States Agency for International Development funds.
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the CDC or the WHO.
Conflict of interest: none declared.
Footnotes
A pilot study of 128 specimens determined a 2% NaOCl solution with distilled water prepared daily to be optimal under field conditions (unpublished data, Hyderabad, India).
References
- 1.Ling D I, Flores L L, Riley L W, Pai M. Commercial nucleic-acid amplification tests for diagnosis of pulmonary tuberculosis in respiratory specimens: meta-analysis and meta-regression. PLoS ONE. 2008;3:e1536. doi: 10.1371/journal.pone.0001536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Directorate General of Health Services. Ministry of Health and Family Welfare, Revised National Tuberculosis Control Programme Laboratory Network. New Delhi, India: RNTCP; 2005. Guidelines for quality assurance of smear microscopy for diagnosing tuberculosis. http://www.tbcindia.nic.in/pdfs/RNTCP%20Lab%20Network%20Guidelines.pdf Accessed March 2013. [Google Scholar]
- 3.Urbanczik R. Present position of microscopy and of culture in diagnostic mycobacteriology. Zentralbl Bakteriol Mikrobiol Hyg A. 1985;260:81–87. doi: 10.1016/s0176-6724(85)80101-2. [DOI] [PubMed] [Google Scholar]
- 4.Behr M A, Warren S A, Salamon H, et al. Transmission of Mycobacterium tuberculosis from patients smear-negative for acid-fast bacilli. Lancet. 1999;353:444–449. doi: 10.1016/s0140-6736(98)03406-0. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. The Global Plan to Stop TB, 2011–2015. Geneva, Switzerland: WHO; 2011. http://www.stoptb.org/assets/documents/global/plan/TB_GlobalPlanToStopTB2011-2015.pdf Accessed March 2013. [Google Scholar]
- 6.Habtamu M, van den Boogaard J, Ndaro A, et al. Light-emitting diode with various sputum smear preparation techniques to diagnose tuberculosis. Int J Tuberc Lung Dis. 2012;16:402–407. doi: 10.5588/ijtld.10.0762. [DOI] [PubMed] [Google Scholar]
- 7.Steingart K R, Ng V, Henry M, et al. Sputum processing methods to improve the sensitivity of smear microscopy for tuberculosis: a systematic review. Lancet Infect Dis. 2006;6:664–674. doi: 10.1016/S1473-3099(06)70602-8. [DOI] [PubMed] [Google Scholar]
- 8.Cameron G M, Castles R. Clorox digestion: a comparison of clorox digestion and three other methods for finding acid-fast organisms in sputum. Am Rev Tuberc. 1945;52:530–533. doi: 10.1164/art.1945.52.6.530. [DOI] [PubMed] [Google Scholar]
- 9.Miörner H, Ganlov G, Yohannes Z, Adane Y. Improved sensitivity of direct microscopy for acid-fast bacilli: sedimentation as an alternative to centrifugation for concentration of tubercle bacilli. J Clin Microbiol. 1996;34:3206–3207. doi: 10.1128/jcm.34.12.3206-3207.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonnet M, Ramsay A, Githui W, Gagnidze L, Varaine F, Guérin P J. Bleach sedimentation: an opportunity to optimize smear microscopy for tuberculosis diagnosis in settings of high prevalence of HIV. Clin Infect Dis. 2008;46:1710–1716. doi: 10.1086/587891. [DOI] [PubMed] [Google Scholar]