Abstract
Setting:
Gitega Fistula Centre (GFC), a dedicated obstetric fistula repair centre providing comprehensive care at the Gitega District Hospital, rural Burundi.
Objectives:
To describe 1) the proportion who returned for scheduled 3- and 6-month follow-up visits and 2) outcomes (fistula closure rates and continence status) at discharge from hospital and after 3 and 6 months among patients who underwent fistula repair surgery.
Design:
Retrospective cohort analysis using programme data from April 2010 to December 2011.
Results:
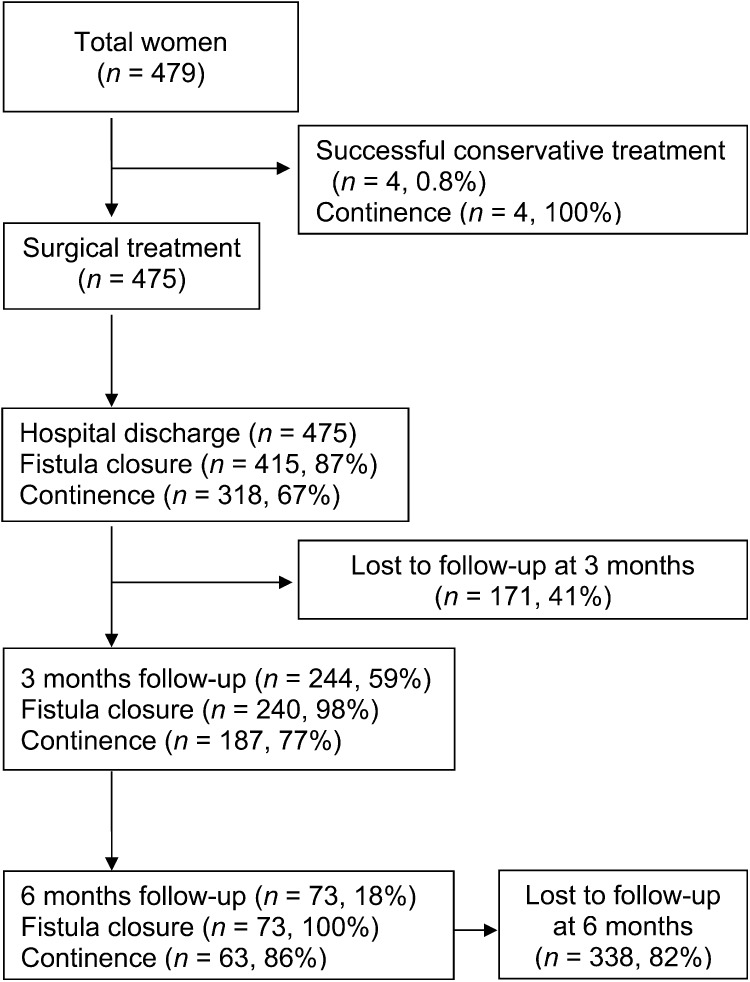
A total of 475 women with obstetric fistula underwent surgical repair. At discharge from hospital, 415 (87%) had a closed fistula, of whom 318 (77%) were continent of urine and/or faeces, while 97 (23%) remained incontinent despite closure. Of the 415 patients with closed fistula, only 244 (59%) were followed up at 3 months and 73 (18%) at 6 months (χ2 for linear trend 576, P < 0.0001). This indicates progressive loss to follow-up, reaching 82% by 6 months.
Conclusion:
Women undergoing obstetric fistula repair surgery at GFC achieve good hospital exit outcomes. Thereafter, substantial and progressive loss to follow-up hinder the ability to judge programme success over time. Steps to address this operational problem are discussed.
Keywords: loss to follow-up, obstetric fistula, operational research, Burundi
Abstract
Contexte:
Le Centre des Fistules de Gitega (GFC), un centre dédié aux réparations des fistules obstétricales fournissant des soins globaux à l’hôpital de district à Gitega, Burundi rural.
Objectifs:
Décrire 1) la proportion d’entre les patientes qui ont subi une réparation chirurgicale des fistules qui sont revenues pour leurs visites de suivi programmées à 3 et à 6 mois, et 2) les résultats (taux de fermeture des fistules et statut de continence) à la sortie de l’hôpital ainsi qu’après 3 et 6 mois parmi elles.
Schéma:
Analyse rétrospective de cohorte utilisant les données du programme entre avril 2010 et décembre 2011.
Résultats:
Au total, une réparation chirurgicale des fistules obstétricales a concerné 475 femmes. A la sortie de l’hôpital, la fistule était fermée chez 415 femmes (87%), parmi lesquelles 318 (77%) étaient continentes au point de vue urinaire ou fécal alors que 97 (23%) restaient incontinentes en dépit de la fermeture. Le suivi à 3 mois n’a été réalisé que chez 244 des 415 patientes (59%) et le suivi à 6 mois chez 73 (18% ; χ2 pour une tendance linéaire = 576, P < 0,0001). Ceci indique une perte progressive de suivi atteignant 82% à 6 mois.
Conclusion:
Les résultats à la sortie de l’hôpital sont bons chez les femmes subissant une réparation chirurgicale d’une fistule obstétricale au GFC. Ensuite, des pertes substantielles et progressives de suivi freinent les moyens de juger les succès du programme à plus long terme. Des étapes visant à répondre à ce problème opérationnel font l’objet d’une discussion.
Abstract
Marco de referencia:
El Centro de fistulas Gitega (GFC) es un establecimiento especializado en la reparación de las fistulas obstétricas y presta una atención integral en el Hospital Distrital de Gitega en una zona rural de Burundi.
Objetivos:
Determinar 1) la proporción de las pacientes que se sometieron a una cirugía de reparación de fistula que acudió a las citas de control programadas 3 y 6 meses después de la cirugía y 2) evaluar los desenlaces clínicos (tasa de cierre de fistulas y estado de continencia) en el momento del alta hospitalaria y a los 3 y los 6 meses.
Métodos:
Se llevó a cabo un análisis de cohortes retrospectivo a partir de los datos del programa, desde abril del 2010 hasta diciembre del 2011.
Resultados:
Cuatrocientas setenta y cinco mujeres que presentaban fístulas obstétricas se sometieron a una reparación quirúrgica. En el momento del alta hospitalaria, en 415 mujeres (87%) la fistula estaba cerrada y de ellas, 318 (77%) presentaban continencia urinaria, continencia fecal o ambas y 97 (23%) permanecían incontinentes pese al cierre de la fístula. A la consulta de seguimiento de los 3 meses solo acudieron 244 de las 415 pacientes (59%) y a la consulta de los 6 meses se presentaron 73 mujeres (18%; tendencia linear χ2 576; P < 0,0001). Estos resultados indican una pérdida progresiva durante el seguimiento, que alcanza un máximo de 82% a los 6 meses.
Conclusión:
Las mujeres que acuden al GFC con el fin de obtener la reparación quirúrgica de una fistula obstétrica presentaron desenlaces favorables en el momento del alta hospitalaria. En adelante, las pérdidas progresivas durante el seguimiento fueron considerables y obstaculizaron la evaluación de la eficacia del programa en el transcurso del tiempo. En el artículo se discuten las medidas que permitirían responder a este problema operativo.
Obstetric or vaginal fistula is a severe medical condition in which a fistula (hole) develops usually between either the rectum and vagina (recto-vaginal fistula [RVF]) or between the bladder and vagina (vesico-vaginal fistula [VVF]) after prolonged labour.1 A fistula most often develops when compression of the birth canal by the unborn child leads to tissue necrosis. More rarely, the injury can be caused by genital cutting, poorly performed abortions or pelvic fractures.2 The condition has been eradicated in the industrialised world, but remains a common complication of childbirth in developing countries, affecting about three million women worldwide.3
In Burundi, the incidence of obstetric fistula is estimated at 0.2–0.5% of all deliveries.4 However, the national capacity for identifying and managing the condition is very limited, and for this reason Médecins Sans Frontières (MSF) set up a dedicated fistula facility, the Gitega Fistula Centre (GFC), for the management of women with obstetric fistula.
Immediate post-surgical closure rates for obstetric fistula can be as high as 90%.5,6 However, late breakdown of the repair has been reported to occur during the 6-month post-operative period, with possible reasons including sexual intercourse resulting in tissue stretching in the first 3 months, wound infection and heavy work.7 While continence is not always achieved immediately after surgical repair, incontinence can improve or resolve in time post-operatively.8 All patients at GFC are thus required to attend 3- and 6-month follow-up visits to assess fistula closure and continence status.
To our knowledge, there are very few published data on the proportion of patients actually followed up and their follow-up outcomes. Such information would be useful to assess outcomes over time, as these are dynamic and could inform policy and practice both in Burundi and elsewhere.
Using data from a dedicated fistula repair centre in rural Burundi, we aimed to describe 1) the proportion of patients who were followed up at their scheduled 3- and 6-month appointments, and 2) surgical outcomes at discharge from hospital and at 3 and 6 months.
METHODS
Study design
This was a retrospective cohort study using routine programmatic data.
Study setting and population
Burundi, a small East African country (population approximately 8 million) is one of the poorest countries in the world, with very poor health indicators, including a maternal mortality rate of 800 per 100 000 live births—among the highest in the world.9 In 2010, the MSF set up a dedicated fistula repair centre (GFC) at the Gitega District Hospital in Central Burundi. GFC is staffed with one fistula specialist and two support doctors (in training), 10 nurses, three social assistants, one health promoter and five professional care givers. The centre has an average capacity for reconstructive repair of 50 cases per month, and all services are offered free-of-charge.
The study population included all women who underwent surgical repair for the first time at GFC between April 2010 and December 2011. All patients were followed up for 6 months.
Recruitment of patients with fistula
Community awareness campaigns on the availability of fistula repair are regularly conducted using mass media (radio) and through religious groups and information leaflets. A free telephone hotline is also available for patients or relatives for information about available services. Patients with fistula generally present at the specialised centre either on their own or by referral after screening at a district hospital.
On arrival, psychological assessment and supportive counselling is performed by trained counsellors and the patient is admitted to the centre. Each patient receives a hospitalisation kit comprising a mosquito net, a blanket, two pieces of cotton cloth, a piece of soap, toothpaste and a toothbrush.
One care giver is allocated for every 15 patients admitted; the care givers are present 24 h a day to support the patients during their pre- and post-operative stay.
Surgical management and post-operative care
Patients are examined by the specialist surgeon at GFC who classifies their fistula according to the Waaldijk classification.10 Patients undergo surgical repair, pre- and post-operative physiotherapy to enhance pelvic muscle tone and to retrain the bladder, and psychosocial counselling. A urinary catheter is inserted after surgery and left for 2–4 weeks. Patients are discharged from GFC 3–7 days after catheter removal after receiving recommendations, including prohibition of sexual intercourse and heavy labour such as cultivating in the field, for at least 3 months. Women are also strongly advised to use a modern method of contraception for at least 1 year.
Follow-up and outcomes
Follow-up visits are scheduled for 3 and 6 months post-discharge to assess fistula closure and continence status. To support the follow-up process, a telephone hotline was set up in May 2011 to trace more patients. Those found with leakage or any other complication were asked to return to GFC for further assessment. If patients remain untraced, they are declared as being lost to follow-up.
Surgical outcomes (fistula closure and continence status) are assessed at hospital discharge and at 3 and 6 months. Fistula closure is assessed using dye and water tests. For VVF cases, this involves inserting a urinary catheter, filling the bladder with dye, clamping the catheter and observing if the dye leaks through the vagina via the fistula. For RVF cases, this involves filling the vagina with water, filling the rectum with air and observing to see if air passes from the rectum to form bubbles on the vaginal side of the passage. Successful fistula closure is defined as assessed by absence of leakage (urine or faeces). Failure of surgical management is classified as 1) non-closure of the fistula or 2) breakdown of fistula repair within 6 months of surgical intervention. Continence is defined as no leakage of urine or faeces.
Data collection and statistical analysis
Patient data on socio-demographic characteristics and follow-up outcomes were sourced from patient files, in-patient registers and surgical registers, and entered into an electronic database which was used for the analysis. The following variables were collected: date of presentation at GFC, age, marital status, occupation, parity, type of fistula (VVF, RVF or both), site of causal delivery, mode of causal delivery, neonatal outcome of causal delivery, and outcome (fistula closure, continence status) at hospital discharge, and at 3 and 6 months follow-up.
The χ2 test for trend was used to assess linear trends in proportions. The level of significance was set at P = 0.05 and 95% confidence intervals were used throughout. Data were analysed using STATA 8.2 software (Stata Corporation, College Station, TX, USA).
Ethics approval
This study satisfied the ethics criteria of the MSF Ethics Review Board (Geneva, Switzerland) and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France, for studies using routinely collected programme data.
RESULTS
Characteristics of the study population
Between April 2010 and December 2011, 475 women underwent surgical fistula repair for the first time at GFC. Table 1 shows the demographic and obstetric characteristics of these women. The median age was 31 years (interquartile range [IQR] 25–40), most (n = 412, 87%) had a VVF and 45% were primiparous. In 74% of cases, the baby was stillborn during the causal delivery. The median duration of stay at GFC was 39 days (IQR 31–51).
TABLE 1.
Socio-demographic and obstetric characteristics of women undergoing surgical fistula repair at Gitega Fistula Centre, central Burundi, April 2010–December 2011
| Variable | n (%) |
| Total | 475 |
| Age, years | |
| <15 | 0 |
| 15–29 | 192 (40) |
| 30–39 | 140 (29) |
| ≥40 | 142 (30) |
| Unknown | 1 (0.2) |
| Median [IQR] | 31 [25–40] |
| Marital status | |
| Single | 57 (12) |
| Married | 259 (55) |
| Separated | 108 (23) |
| Widow | 48 (9) |
| Unknown | 3 (0.6) |
| Occupation | |
| Peasant | 472 (99) |
| Employed | 0 |
| Business | 3 (0.6) |
| Geographical distribution | |
| Urban | 7 (1) |
| Rural | 468 (99) |
| Parity | |
| 1 birth | 214 (45) |
| 2 births | 74 (16) |
| ≥3 births | 187 (39) |
| Site of causal delivery* | |
| Home | 72 (15) |
| Health centre | 72 (15) |
| Hospital | 327 (69) |
| Unknown | 4 (1) |
| Mode of causal delivery | |
| Vaginal | 256 (54) |
| Caesarean section | 209 (44) |
| Not recorded | 10 (2) |
| Neonatal outcome of causal delivery | |
| Alive | 120 (25) |
| Stillborn | 351 (74) |
| Not recorded | 4 (1) |
| Type of obstetric fistula | |
| VVF | 412 (87) |
| RVF | 43 (9) |
| VVF and RVF | 19 (4) |
| Not recorded | 1 (0) |
Delivery associated with the fistula.
IQR = interquartile range; VVF = vesico-vaginal fistula; RVF = recto-vaginal fistula.
Patient follow-up
Of 475 patients who underwent surgical repair, 171 (41%) were lost to follow-up at 3 months and 338 (82%) were lost at 6 months (χ2 for linear trend 576, P < 0.0001, Figure).
FIGURE.
Patient flow and follow-up at Gitega Fistula Centre, Burundi, April 2010–December 2011.
Surgical outcomes at hospital discharge and at 3 and 6 months
Table 2 shows surgical fistula closure and continence status stratified by fistula type at hospital discharge and at 3 and 6 months follow-up. Of the 475 women who underwent surgical repair, fistula closure at hospital discharge was achieved in 415 (87%), in whom urinary and/or faecal continence was achieved in 318 (67%). In the remaining 97 (20%), continence was not yet achieved.
TABLE 2.
Treatment outcomes for women undergoing surgical repair for obstetric fistula according to type of fistula at hospital discharge, and at 3 and 6 months follow-up, Gitega, Burundi, April 2010–December 2011
| Fistula type | Hospital discharge |
3 months follow-up |
6 months follow-up |
||||||
| Fistula closed* | Continent* | Presented† | Fistula closed‡ | Continent‡ | Presented§ | Fistula closed¶ | Continent¶ | ||
| All types (n = 475) | 415 (87) | 318 (67) | 244 (59) | 240 (98) | 187 (77) | 73 (18) | 73 (100) | 63 (86) | |
| VVF (n = 412) | 364 (88) | 269 (65) | 213 (58) | 209 (98) | 156 (73) | 57 (18) | 57 (100) | 47 (82) | |
| RVF (n = 43) | 42 (98) | 40 (93) | 26 (62) | 26 (100) | 26 (100) | 15 (35) | 15 (100) | 15 (100) | |
| VVF and RVF (n = 19) | 9 (47) | 4 (21) | 5 (56) | 5 (100) | 4 (80) | 1 (11) | 1 (100) | 0 | |
Denominator for each row is the total number (n) in the column ‘fistula type’.
Denominator for each row is the total number in the column ‘fistula closed’ at hospital discharge.
Denominator for each row is the total number in the column ‘presented’ at 3 months follow-up.
Denominator for each row is the total number in the column ‘fistula closed’ at hospital discharge minus those broken down at 3 months follow-up.
Denominator for each row is the total number in the column ‘presented’ at 6 months follow-up.
VVF = vesico-vaginal fistula; RVF = recto-vaginal fistula.
DISCUSSION
This is one of the few studies from East Africa to report cumulative and progressive loss to follow-up among women operated on for obstetric fistula. At 3 and 6 months of follow-up, respectively 40% and 80% patients were lost to follow-up. Such high losses seriously compromise the ability to assess programme performance over time.
The study strengths are that 1) data collection at GFC is regularly supervised and monitored, and thus the study data are likely to be robust; 2) a large number of patients with different fistula types were included; and 3) as the data come from a routine setting, they likely reflect operational reality. Furthermore, we followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines11 as well as ethics considerations for operational research.12 The main study limitations are that patients lost to follow-up were not actively traced through home visits, and the study did not investigate the specific reasons for such losses. Data contained in the patient files and registers were also limited, and we were thus only able to examine associations between loss to follow-up and a limited number of specific variables.
The findings of this study raise a number of issues that merit discussion. First, the conventional approach until now has been to report fistula treatment outcomes at the time of hospital discharge only, and not beyond this time. Such outcomes are generally reported to be good, with fistula closure rates of 73–93% reported from various other African settings,13–17 compared to 87% in our setting. However, repair breakdowns are known to occur in the 6-month post-operative period,8 invalidating these hospital discharge outcomes. Given the sequelae that can ensue after fistula repair, we would emphasise the importance of implementing a system of cohort monitoring of all patients who undergo obstetric surgery for fistula.18,19 Other chronic diseases such as tuberculosis and human immunodeficiency virus/acquired immune-deficiency syndrome also require long follow-up periods, and cohort monitoring is routinely used to judge programme success. Quarterly cohort reporting is also advantageous, as it would provide useful operational information on all newly operated cases (disease burden) and their standardised outcomes (such as closed fistula, continence, loss to follow-up, death or transferred out). Such reporting would also provide programme retention and attrition rates, important parameters that can be used to judge overall programme management quality.20,21
The high loss to follow-up rates in our study made it impossible to assess the true outcomes of fistula repair at the 3- and 6-month follow-up intervals. We are only aware of one other published study from Ethiopia that has reported on loss to follow-up rates for post-fistula repair.8 In this study, loss to follow-up at 6 months was just under 40%, which is much lower than in our setting. Possible reasons for the very high losses to follow-up in our setting may be related to access, acceptability and/or financial barriers. GFC is a centralised facility and the only permanent facility in Burundi offering care for women with fistulae, and distance and transport costs may be particularly pertinent. Although the programme offers transport reimbursements to women who attend GFC, individuals have to find the money to get to GFC in the first place, and this may be unaffordable for some. One solution would be to make transport vouchers available at peripheral health centres or decentralised administrative units. In addition, incentives such as buckets, mosquito nets, etc., could be provided to encourage return for follow-up visits. Another operational option would be to decentralise follow-up visits through mobile outreach teams. In the meantime, further research into the reasons underpinning the high losses to follow-up, including specific anthropological studies, would help provide better insight into addressing this problem.
In conclusion, the study shows good outcomes on hospital discharge following fistula repair surgery. However, in the subsequent 6-month period, substantial losses to follow-up hinder the ability to assess overall programme success over time.
Acknowledgments
This research was supported through an operational research course that was jointly developed and run by the Centre for Operational Research, International Union Against Tuberculosis and Lung Disease, Paris, France, and the Operational Research Unit, Médecins Sans Frontières, Brussels-Luxembourg.
Additional support for running the course was provided by the Institute for Tropical Medicine, Antwerp, Belgium; the Center for International Health, University of Bergen, Bergen, Norway; and the University of Nairobi, Nairobi, Kenya.
Funding for the course was from an anonymous donor, the Department for International Development, United Kingdom, and Médecins Sans Frontières, Brussels Operational Center, MSF–Luxembourg.
Conflict of interest: none declared.
References
- 1.Creanga A A, Genadry R R. Obstetric fistulas: a clinical review. Int J Gynaecol Obstet. 2007;99(Suppl 1):S40–S46. doi: 10.1016/j.ijgo.2007.06.021. [DOI] [PubMed] [Google Scholar]
- 2.Miller S, Lester F, Webster M, Cowan B. Obstetric fistula: a preventable tragedy. J Midwifery Womens Health. 2005;50:286–294. doi: 10.1016/j.jmwh.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 3.Donnay F, Weil L. Obstetric fistula: the international response. Lancet. 2004;363:71–72. doi: 10.1016/S0140-6736(03)15177-X. [DOI] [PubMed] [Google Scholar]
- 4.United Nations Population Fund. Evaluation de l’ampleur des fistules obstetricales et traumatiques au Burundi. Bujumbura, Burundi: UNFPA; 2006. [French] [Google Scholar]
- 5.Elkins T E. Surgery for the obstetric vesicovaginal fistula: a review of 100 operations in 82 patients. Am J Obstet Gynecol. 1994;170:1108–1118. doi: 10.1016/s0002-9378(94)70105-9. discussion 1118–1120. [DOI] [PubMed] [Google Scholar]
- 6.Roenneburg M L, Genadry R, Wheeless C.R., Jr Repair of obstetric vesicovaginal fistulas in Africa. Am J Obstet Gynecol. 2006;195:1748–1752. doi: 10.1016/j.ajog.2006.07.031. [DOI] [PubMed] [Google Scholar]
- 7.Hancock B, Browning A. Practical obstetrical fistula surgery. London, UK: Royal Society of Medicine Press; 2009. [Google Scholar]
- 8.Browning A, Member B. Women with obstetric fistula in Ethiopia: a 6-month follow-up after surgical treatment. BJOG. 2008;115:1564–1569. doi: 10.1111/j.1471-0528.2008.01900.x. [DOI] [PubMed] [Google Scholar]
- 9.Maternal Mortality Estimation Interagency Group (MMEIG), WHO, UNICEF, The World Bank, UN Population Division. Trends in maternal mortality 1990–2010. Washington DC, USA: The World Bank, 2012. http://www.unfpa.org/webdav/site/global/shared/documents/publications/2012/Trends_in_maternal_mortality_A4-1.pdf Accessed May 2013.
- 10.Waaldijk K. Surgical classification of obstetric fistula. Int J Gynaecol Obstet. 2005;49:161–163. doi: 10.1016/0020-7292(95)02350-l. [DOI] [PubMed] [Google Scholar]
- 11.von Elm E, Altman D G, Egger M, Pocock S J, Gotzsche P C, Vandenbroucke J P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 12.Edginton M, Enarson D, Zachariah R, Reid T, et al. Why ethics is indispensable for good quality operational research. Public Health Action. 2012:21–22. doi: 10.5588/pha.12.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holme A, Breen M, MacArthur C. Obstetric fistula: a study of women managed at the Monze Mission Hospital, Zambia. BJOG. 2007;114:1010–1017. doi: 10.1111/j.1471-0528.2007.01353.x. [DOI] [PubMed] [Google Scholar]
- 14.Nardos R, Browning A, Chen C C G. Risk factors that predict failure after vaginal repair of obstetric vesicovaginal fistulae. Am J Obstet Gynecol. 2009;200:578. doi: 10.1016/j.ajog.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Goh J T, Browning A, Berhan B, Chang A. Predicting the risk of failure of closure of obstetric fistula and residual urinary incontinence using a classification system. Int Urogynecol J Pelvic Floor Dysfunct. 2008;12:1659–1662. doi: 10.1007/s00192-008-0693-9. [DOI] [PubMed] [Google Scholar]
- 16.Kayondo M, Wassw S, Kabakyenga J, et al. Predictors and outcome of surgical repair of obstetric fistula at a regional referral hospital, Mbarara, western Uganda. BMC Urol. 2011;11:23. doi: 10.1186/1471-2490-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hancock B. First steps in vesico-vaginal fistula repair. London, UK: Royal Society of Medicine Press; 2005. [Google Scholar]
- 18.Harries A D, Zachariah R, Kapur A, Jahn A, Enarson D A. The vital signs of chronic disease management. Trans R Soc Trop Med Hyg. 2009;103:537–540. doi: 10.1016/j.trstmh.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 19.Harries A D, Jahn A, Zachariah R, Enarson D. Adapting the DOTS framework for tuberculosis control to the management of non-communicable diseases in sub-Saharan Africa. PLoS Med. 2008;5:e124. doi: 10.1371/journal.pmed.0050124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khader A, Farajallah L, Shahin Y, et al. Cohort monitoring of persons with diabetes mellitus in a primary healthcare clinic for Palestine refugees in Jordan. Trop Med Int Health. 2012 doi: 10.1111/j.1365-3156.2012.03097.x. Oct 11. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Khader A, Farajallah L, Shahin Y, et al. Cohort monitoring of persons with hypertension: an illustrated example from a primary healthcare clinic for Palestine refugees in Jordan. Trop Med Int Health. 2012;17:1163–1170. doi: 10.1111/j.1365-3156.2012.03048.x. [DOI] [PubMed] [Google Scholar]