Abstract
Pulsed-field gel electrophoresis fingerprints of 98 Campylobacter jejuni isolates from patients (85) and chicken carcasses (13) in Hong Kong in 2002 demonstrated high genetic diversity. The prevalence of quinolone resistance among the isolates was 85.9%, and replacement of the threonine-86 residue in the gyrase subunit A was the major resistance mechanism.
Campylobacter spp. are major diarrhea-causing bacterial pathogens in the industrialized world, with Campylobacter jejuni being the most frequently identified species. In Hong Kong, a recent study by the Emergency Department in a major hospital, Prince of Wales Hospital, ranked it behind Vibrio parahaemolyticus and Salmonella spp. as the most frequently identified etiological agent of acute bacterial gastroenteritis and found that it caused significantly higher morbidity than the other two did (2). Although patients often recover without chemotherapy, in the case of severe or persistent illness, erythromycin or fluoroquinolones are the drugs of choice (3).
In an attempt to investigate if there is any predominant strain in Hong Kong, we employed pulsed-field gel electrophoresis (PFGE) to determine the genetic relatedness of 85 C. jejuni strains isolated from human stools or rectal swabs collected from government outpatient clinics throughout the 12 months of 2002, together with 13 strains obtained by an enrichment culture method (12) from refrigerated chicken carcasses sampled at point of sale before cooking in December 2002. Susceptibilities to nalidixic acid (NAL) and ciprofloxacin (CIP) were determined together with the sequence of the quinolone resistance-determining region (QRDR) of the gyrase subunit A gene (gyrA) in order to assess the prevalence and the major mechanism of resistance.
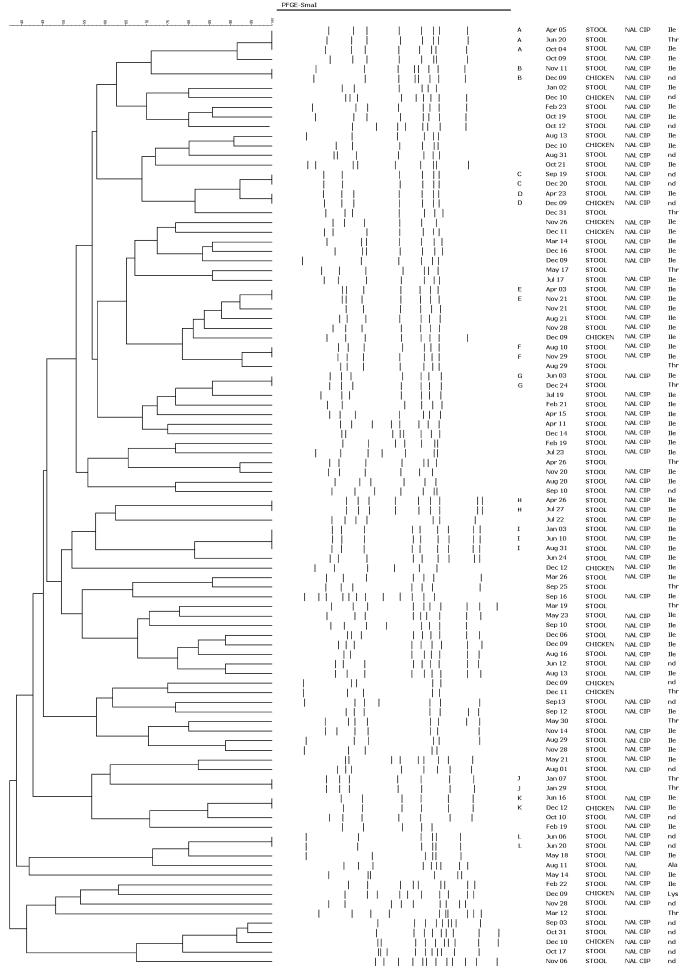
PFGE fingerprints of the 98 isolates were generated according to a protocol described previously (10). A dendrogram with 1.0% band position tolerance was constructed with BioNumerics software (Applied Maths, Ghent, Belgium) with the unweighted pair group method with averages from a Dice coefficient matrix (Fig. 1). Eighty-four different fingerprints were obtained from the 98 isolates. With 80% similarity as the cutoff, the majority of the fingerprints (55 of 98) were separated into 22 clusters and no distinct predominant cluster was observed, suggesting that the greater part of the isolates were genetically diverse. This is also supported by visual examination of the fingerprints. Nonetheless, 12 fingerprints (clusters A to L) were shared by more than one isolate. All of the 25 strains with shared fingerprints were epidemiologically unlinked except for one pair which came from the same patient, who appeared still to shed the same organism 22 days after the first isolation (cluster J, Fig. 1). The time between collections among these 25 strains within their own clusters varied between 12 and 240 days. Three clusters (B, D, and K) each have one isolate from chicken carcasses, suggesting that the sources of infection and contamination may be common. However, the considerable temporal difference between the isolates within each cluster and the significant genetic diversity of the fingerprints suggested the presence of multiple reservoirs rather than single inoculation or contamination.
FIG. 1.
Dendrogram constructed by unweighted pair group method with averages from a Dice coefficient matrix showing the relatedness of the PFGE SmaI fingerprints of 98 C. jejuni strains isolated in 2002 in Hong Kong. The band patterns were digitally represented, and the band position tolerance was 1.0%. The first column is cluster designation, the second is isolation date, the third is specimen type, the fourth is resistance phenotype, and the fifth is the amino acid at residue 86 of the gyrase subunit A. nd, not determined.
Disk diffusion assays for testing susceptibilities to NAL (30 μg/disk) and CIP (5 μg/disk) were performed according to NCCLS guidelines (6). Mueller-Hinton agar used was supplemented with 5% horse blood. Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 were controls. Zone diameters (ZDs) were recorded after incubation (42°C, 24 h) and interpreted according to NCCLS guidelines (7). Seventy-three of the 85 human isolates (85.9%) were found to be resistant to NAL (ZD, ≤13 mm). While 72 of these resistant strains were also resistant to CIP (ZD, ≤15 mm), one was sensitive (ZD, ≥21 mm). This level of quinolone resistance was higher than that in Australia (0%), Taiwan (52%), Germany (45.1%), and Spain (75%) (5, 11, 13, 15). Eleven of the 13 chicken isolates (84.6%) were resistant to both antibiotics.
PCR sequencing of the gyrA QRDR was performed as described by Piddock et al. (9). Seventy-seven strains (69 human and 8 chicken carcass isolates) had their gyrA QRDR successfully characterized. The remaining 21 isolates failed to produce PCR amplicons capable of being sequenced. Replacement of the threonine-86 residue of the gyrase subunit A with isoleucine (56 human and 6 chicken carcass isolates) or lysine (one chicken carcass isolate) correlated perfectly with resistance to NAL and CIP, suggesting that this is the major mechanism of resistance. The stool isolate resistant to only NAL had an alanine as residue 86 of the gyrase subunit A, and this amino acid change was previously reported to be associated with an increased MIC of NAL but not of CIP (1).
Poultry farms are attractive candidates for possible environmental perpetuating sources because C. jejuni may persist there and the use of fluoroquinolones such as enrofloxacin as growth promoters may help to explain the high level of resistance in both clinical and chicken carcass isolates (4). Indeed, previous studies have shown that C. jejuni can persist in a confined geographical area and that broiler houses may be repeatedly infected with a few clones during the life cycles of successive broiler flocks (16). However, measures successfully used to stop Salmonella colonization of broiler flocks are completely ineffective against Campylobacter, suggesting that the mode of transmission and perhaps the ecology of these poultry-borne pathogens are very different (8). Interestingly, isolates in two clusters (A and G, Fig. 1) have different resistance patterns, indicating that PFGE-indistinguishable strains can have different resistance phenotypes. If these strains did come from the same source, their paths to acquisition of the resistance mutations may still be different. Recent laboratory experiments have demonstrated that the rapid emergence of resistance to quinolones in C. jejuni does not necessarily result from horizontal transmission of resistant strains among chickens but could be solely the result of de novo selection of resistance in individual chickens (14). Moreover, this rapid selection of quinolone resistance in C. jejuni is not mirrored in E. coli under the same conditions, reinforcing the idea that Campylobacter has a different ecology from that of other organisms occupying the same niche.
In conclusion, the quinolone resistance rate among clinical isolates in Hong Kong appeared high at 85.9% and was mirrored also in the limited number of chicken carcass isolates. Replacement of the Thr-86 residue of the gyrase subunit A was the major resistance mechanism involved. Although no predominant strain of C. jejuni was detected in 2002 in Hong Kong, the significant genetic diversity and considerable temporal difference between the isolates with indistinguishable PFGE fingerprints suggested the presence of multiple perpetuating environmental sources, and poultry farms are possible candidates. However, the actual route for transmission and quinolone resistance selection is likely to be complex, as exemplified by the PFGE-indistinguishable strains with different resistance phenotypes in this study.
Nucleotide sequence accession number.
The nucleotide sequence of the gyrA QRDR with the alanine substitution at amino acid residue 86 was deposited in GenBank under accession no. AY383720.
Acknowledgments
We thank Stephen Lau, Mike Kwok, and Daniel So of the General Bacteriology Laboratory; Matthew Tsang of the ARS Laboratory; Vivien Tsang and Catherine Law of the Molecular Laboratory; and K. K. Kwok and Susanna Yeung of the Public Health Laboratory for their excellent technical support.
REFERENCES
- 1.Bachoual, R., S. Ouabdesselam, F. Mory, C. Lascols, C. J. Soussy, and J. Tankovic. 2001. Single or double mutational alterations of gyrA associated with fluoroquinolone resistance in Campylobacter jejuni and Campylobacter coli. Microb. Drug Resist. 7:257-261. [DOI] [PubMed] [Google Scholar]
- 2.Chan, S. S., K. C. Ng, D. J. Lyon, W. L. Cheung, A. F. Cheng, and T. H. Rainer. 2003. Acute bacterial gastroenteritis: a study of adult patients with positive stool cultures treated in the emergency department. Emerg. Med. J. 20:335-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DuPont, H. L. 1991. Use of quinolones in the treatment of gastrointestinal infections. Eur. J. Clin. Microbiol. Infect. Dis. 10:325-329. [DOI] [PubMed] [Google Scholar]
- 4.Engberg, J., F. M. Aarestrup, D. E. Taylor, P. Gerner-Smidt, and I. Nachamkin. 2001. Quinolone and macrolide resistance in Campylobacter jejuni and C. coli: resistance mechanisms and trends in human isolates. Emerg. Infect. Dis. 7:24-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li, C.-C., C.-H. Chiu, J.-L. Wu, Y.-C. Huang and T.-Y. Lin. 1998. Antimicrobial susceptibilities of Campylobacter jejuni and coli by using E-test in Taiwan. Scand. J. Infect. Dis. 30:39-42. [DOI] [PubMed] [Google Scholar]
- 6.National Committee for Clinical Laboratory Standards. 2003. Methods for dilution antimicrobial susceptibility tests for bacteria that grows aerobically, 6th ed. Approved standard M7-A6. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 7.National Committee for Clinical Laboratory Standards. 2003. Performance standards for antimicrobial susceptibility testing—13th informational supplement M100-S13. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 8.Newell, D. G., and C. Fearnley. 2003. Sources of Campylobacter colonization in broiler chickens. Appl. Environ. Microbiol. 69:4343-4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piddock, L. J. V., V. Ricci, L. Pumbwe, M. J. Everett, and D. J. Griggs. 2003. Fluoroquinolone resistance in Campylobacter species from man and animals: detection of mutations in topoisomerase genes. J. Antimicrob. Chemother. 51:19-26. [DOI] [PubMed] [Google Scholar]
- 10.Ribot, E. M., C. Fitzgerald, K. Kubota, B. Swaminathan, and T. J. Barrett. 2001. Rapid pulsed-field gel electrophoresis protocol for subtyping of Campylobacter jejuni. J. Clin. Microbiol. 39:1889-1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sáenz, Y., M. Zarazaga, M. Lantero, M. J. Gastañares, F. Baquero, and C. Torres. 2000. Antibiotic resistance in Campylobacter strains isolated from animals, foods and humans in Spain in 1997-1998. Antimicrob. Agents Chemother. 44:267-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scotter, S. L., T. J. Humphrey, and A. Henley. 1993. Methods for the detection of thermotolerant campylobacters in foods: results of an inter-laboratory study. J. Appl. Bacteriol. 74:155-163. [DOI] [PubMed] [Google Scholar]
- 13.Unicomb, L., J. Ferguson, T. V. Riley, and P. Collignon. 2003. Fluoroquinolone resistance in Campylobacter absent from isolates, Australia. Emerg. Infect. Dis. 9:1482-1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Boven, M., K. T. Veldman, M. C. de Jong, and D. J. Mevius. 2003. Rapid selection of quinolone resistance in Campylobacter jejuni but not in Escherichia coli in individually housed broilers. J. Antimicrob. Chemother. 52:719-723. [DOI] [PubMed] [Google Scholar]
- 15.Wagner, J., M. Jabbusch, M. Eisenblatter, H. Hahn, C. Wendt, and R. Ignatius. 2003. Susceptibilities of Campylobacter jejuni isolates from Germany to ciprofloxacin, moxifloxacin, erythromycin, clindamycin, and tetracycline. Antimicrob. Agents Chemother. 47:2358-2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wedderkopp, A., E. M. Nielsen, and K. Pedersen. 2003. Distribution of Campylobacter jejuni Penner serotypes in broiler flocks 1998-2000 in a small Danish community with special reference to serotype 4-complex. Epidemiol. Infect. 131:915-921. [DOI] [PMC free article] [PubMed] [Google Scholar]