Abstract
Setting:
The National Tuberculosis Programme in Singapore where, among resident cases, higher tuberculosis (TB) rates have been reported in ethnic Malays.
Objective:
To describe the socio-demographic and clinical characteristics of resident TB cases by ethnicity, and to assess whether Malays differ from other groups in terms of the above parameters.
Design:
Cross-sectional review of records from the tuberculosis registry’s electronic database.
Results:
Among 15 622 resident cases notified, 72.2% were Chinese, 18.7% Malay, 5.8% Indian and 2.9% were from other minorities. Compared to other ethnicities, Malays were more likely to be incarcerated at the time of notification (odds ratio [OR] 3.70, 95%CI 3.03–4.52) and clustered at the same residential address (OR 1.65, 95%CI 1.44–1.89), but were less likely to be aged ≥65 years (OR 0.61, 95%CI 0.54–0.70) or to reside in high-cost housing (OR 0.11, 95%CI 0.07–0.17). In terms of disease characteristics, more Malays had diabetes mellitus (OR 1.54, 1.37–1.73), a highly-positive acid-fast bacilli smear (OR 1.64, 95%CI 1.47–1.83) and cavitary disease on chest X-ray (OR 1.41, 95%CI 1.28–1.55).
Conclusion:
Compared to other ethnicities, reported TB cases among Malays were more severe and were likely to be more infectious. Increased vigilance in case management and contact investigations, as well as an improvement in the socio-economic conditions of this community, are required to reduce TB rates in this ethnic group.
Keywords: TB, Singapore, ethnic group, characteristics, operational research
Abstract
Contexte:
Programme National de la Tuberculose à Singapour, où parmi les cas chez les résidents, des taux plus élevés de tuberculose (TB) ont été signalés chez les sujets d’ethnie malaise.
Objectif:
Décrire les caractéristiques socio-démographiques et cliniques des cas de TB chez les résidents en fonction de leur ethnie et évaluer dans quelle mesure les Malais diffèrent des autres groupes en ce qui concerne ces paramètres.
Schéma:
Révision transversale des dossiers de la base de données électroniques du registre de la tuberculose.
Résultats:
Parmi 15 622 cas déclarés chez les résidents, 72,2% étaient Chinois, 18,7% Malais, 5,8% Indiens et 2,9% originaires d’autres minorités. Par comparaison avec les autres ethnies, les Malais sont plus susceptibles d’être emprisonnés au moment de la déclaration (OR 3,70 ; IC95% 3,03–4,52) et de se retrouver en grappes à la même adresse de résidence (OR 1,65 ; IC95% 1,44–1,89), mais sont moins susceptibles d’avoir un âge ≥65 ans (OR 0,61 ; IC95% 0,54–0,70) et de résider dans des habitats à coût élevé (OR 0,11 ; IC95% 0,07–0,17). En termes de caractéristiques de la maladie, chez les Malais le diabète sucré est plus fréquent (OR 1,54 ; IC95% 1,47–1,73), les frottis à la recherche de bacilles acido-résistants sont plus fortement positifs et une excavation est plus fréquente au cliché thoracique (OR 1,41 ; IC95% 1,28–1,55).
Conclusions:
Par comparaison avec ceux d’autres ethnies, les cas de TB signalés chez les Malais sont plus graves et plus susceptibles d’être contagieux. Si l’on veut réduire les taux de TB dans cette ethnie, il faut veiller à une vigilance accrue dans la prise en charge des cas et dans les investigations des contacts ainsi qu’à une amélioration des conditions socio-économiques de cette collectivité.
Marco de referencia:
El Programa Nacional contra la Tuberculosis en Singapur, donde las tasas más altas de tuberculosis (TB) en los residentes se notifican en la población de etnia malaya.
Abstract
Objetivo:
Describir las características sociodemográficas y clínicas de los casos de TB en residentes en función de la etnia de los pacientes y evaluar si los malayos se diferencian de otros grupos con respecto a estos criterios.
Métodos:
Se llevó a cabo un estudio transversal con examen de las historias clínicas a partir de la base de datos electrónica del registro de TB.
Resultados:
De los 15 622 casos residentes notificados, el 72,2% correspondió a chinos, el 18,7% a malayos, el 5,8% a indios y el 2,9% a pacientes pertenecientes a otras minorías. En comparación con otras etnias, fue más frecuente que los malayos estuviesen reclusos en el momento de la notificación (OR 3,70; IC95% 3,03–4,52) y que se encontrasen agrupados en una misma dirección domiciliaria (OR 1,65; IC95% 1,44–1,89); fue menos frecuente que tuviesen ≥65 años de edad (OR 0,61; IC95% 0,54–0,70) y que habitasen en viviendas de alto costo (OR 0,11; IC95% 0,07–0,17). Con respecto a las características de la enfermedad, más malayos tenían un diagnóstico de diabetes (OR 1,54; IC95% 1,37–1,73), obtuvieron una baciloscopia positiva de alto grado (OR 1,64; IC95% 1,47–1,83) y presentaron imágenes de cavernas en la radiografía de tórax (OR 1,41; IC95% 1,28–1,55).
Conclusión:
En comparación con otras etnias, los casos de TB notificados en la población malaya fueron más graves y con mayor frecuencia eran contagiosos. Sería oportuno prestar mayor atención al manejo de los casos y a la investigación de los contactos en esta comunidad, a fin de disminuir las tasas de TB en las personas de etnia malaya.
Singapore is a multi-ethnic country with a total population of about 5.1 million: 3.8 million residents and 1.3 million non-residents.1 Among the 3.8 million residents, 86% are Singaporean citizens, and 14% are permanent residents, i.e., foreigners who have been granted permanent residency in Singapore. The remaining 1.3 million non-residents comprise foreigners who have been granted permits to study or work in Singapore, as well as dependents of either Singapore residents or those permit holders who have been granted long-term residency in Singapore.
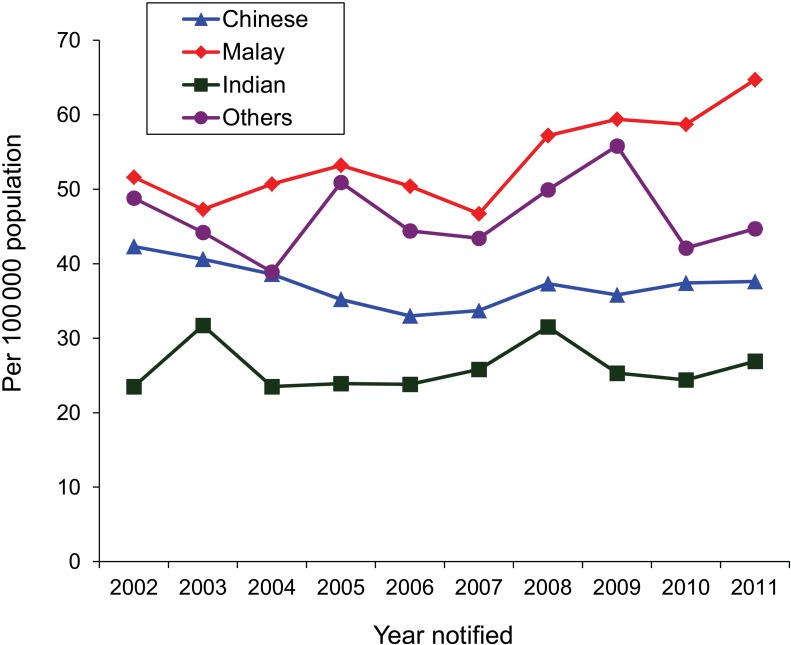
The resident population of Singapore comprises about 75% Chinese, 15% Malays, 8% Indians, and 2% from other ethnic groups.1 Of the 3032 new tuberculosis (TB) cases reported in 2011, 1533 were among Singapore residents, giving a notification rate of 40.5 cases per 100 000 resident population.2 However, the notification rates vary across ethnic groups. As shown in the Figure, based on ethnic group specific TB notification rates from 2002 to 2011,2–10 Malays had consistently higher TB incidence rates than other ethnicities. Although the Malay ethnic group comprises only about 15% of the resident population,1 they make up 21% of TB cases.2 This suggests that Malay ethnicity is disproportionately represented, and that the risk of TB may be higher among Malays than other ethnicities.
FIGURE.
Tuberculosis notification trends among Singapore residents by ethnicity, 2002–2011.
It is well established that certain socio-demographic characteristics and co-morbidities are associated with an increased risk of TB infection and disease. However, it is not known whether ethnic Malays in Singapore differ from other ethnic groups in these aspects, as there are few published reports on this subject. Two articles have reported that non-Chinese ethnicity was a strong predictor of treatment default,11 and that Chinese ethnicity was found to be more strongly associated with treatment completion.12 Recent publications on TB control in Singapore have since touched on issues such as the emergence of multidrug-resistant TB,13,14 the impact of diagnostic delay,15 treatment non-adherence,16 and TB among foreign migrants.17 However, no studies have focused on the topic of TB across the various ethnicities.
The aim of this study was to describe, for each ethnic group, the socio-demographic and clinical characteristics of resident TB patients, and to assess whether Malays differed from other ethnicities in terms of these parameters.
METHODS
Design
This was a descriptive analysis of routinely collected TB programme data.
Setting
The Singapore TB Elimination Programme (STEP) Registry is the epidemiological arm of Singapore’s National TB Control Programme. The clinical arm of STEP is the TB Control Unit (TBCU), which acts as the national treatment centre and primary referral centre for the management of difficult cases. The TBCU treats about 65–70% of Singapore’s TB cases, while the remaining cases are seen primarily at public hospitals and by private respiratory physicians. DOTS is the standard of care at TBCU, and TB drugs are provided free of charge for patients treated under DOTS. Due to issues with monitoring DOTS adherence, the DOTS programme is only administered at TBCU.
The notification of TB in Singapore is mandatory under the Infectious Diseases Act, which requires any physician who diagnoses or suspects active TB to notify the TB registry within 72 hours. This can be done by submitting a TB notification form (MD532) by fax or post or by electronic submission through the Ministry of Health’s website. The notification records are entered manually (for hardcopy submissions) or uploaded electronically (for online submissions) into the registry’s electronic database.
In Singapore, Mycobacterium tuberculosis culture is performed only at the Central TB Laboratory, located at Singapore General Hospital, and the microbiology laboratory at the National University Hospital. Acid-fast bacilli (AFB) smear microscopy, on the other hand, is performed at both of these laboratories and at a number of others in both the public and private sector.
The STEP Registry is electronically linked to the two culture laboratories, as well as to three others in public hospitals that perform AFB smear microscopy. The registry thus captures the results of all TB culture examinations performed in Singapore, and the majority of AFB smear examinations.
Study population
The study population comprised new and retreatment TB cases among Singapore residents notified to the STEP Registry from 2002 to 2011. All required data pertaining to the TB case records were extracted from the STEP Registry’s electronic database. Sampling was not required, as it involved the use of data from a national registry, which has nationwide coverage.
Study variables
The socio-demographic variables included National Registration Identity Card number, sex, ethnic group, date of birth, residential address, marital status, housing type, country of birth, residential status, and incarceration in a correctional facility.
‘Housing type’ was stratified into three subgroups: ‘government flat (one to two rooms)’, ‘government flat (three to five rooms)’, and ‘private housing’. Housing type was used as a proxy for socio-economic status: 1- to 2-room government flats represent the cheapest forms of housing; 3- to 5-room government flats are mid-range; and private housing refers to private apartments and any form of landed property, which represent the most expensive forms of housing.
Residential address was used to determine the number and proportion of cases with the same residential address. This was a proxy for comparing transmission within households across ethnic groups. Patients whose address had no floor and unit number were considered as residing in a landed property; for these cases, matching for identical addresses was based on postal code, as every landed property in Singapore has a unique postal code. The addresses for all other patients living in government flats and private apartments were matched on the basis of postal codes as well as floor and unit numbers.
Variables pertaining to disease characteristics included site of disease, TB category, human immunodeficiency virus diagnosis (from 2008), presence or absence of diabetes mellitus (DM), cough characteristics, chest X-ray (CXR) results, baseline sputum smear results and baseline sputum culture results, with the last four clinical characteristics being applicable for notified cases of pulmonary TB (PTB) only. Cases with both pulmonary and extra-pulmonary sites were considered as PTB cases.
Data validation
Data captured in the STEP Registry’s electronic database were routinely double-checked to ensure good data quality. No further validation was performed upon data extraction.
Data analysis
Age at date of TB notification was calculated from patient’s date of birth. For each ethnic group, the mean age of the notified cases and the proportion by age group (0–14, 15–64 and ≥65 years) were calculated. The socio-demographic and clinical characteristics of each ethnic group were described in terms of absolute numbers and proportion (%), as well as odds ratios (OR) and their 95% confidence intervals (95%CI; Malays vs. non-Malays), using EpiData Version 3.1 (EpiData Association, Odense, Denmark) analysis. Multiple logistic regression was done using SPSS Statistics version 17 (SPSS Inc, Chicago, IL, USA).
Ethics approval
Permission to conduct the study was obtained from the Ministry of Health, Singapore. Ethics approval was obtained from the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease.
RESULTS
A total of 15 622 resident TB cases were notified from 2002 to 2011. Among these, 11 353 (72.7%) were of Chinese ethnicity, 2919 (18.7%) were Malay, 900 (5.8%) were Indian, and 450 (2.9%) were from ‘other’ ethnicities.
Table 1 describes the socio-demographic characteristics of each ethnicity. More Chinese (73%) were male, compared to about 66% of Malay and Indian patients. The latter two ethnic groups also had a younger age distribution: about 20% of the cases were aged ≥65 years compared to 36% of Chinese cases. Malay patients had the lowest proportion of foreign-born cases and permanent residents (7.5%, 2%), while those of ‘other’ ethnicities had the highest proportion, at 79% and 63.8%, respectively. In terms of marital status, the proportion of those divorced ranged from 2% of ‘others’ to 6.5% of Malay cases. With regard to housing, the majority of patients resided in 3- to 5-room government flats (about 70–75%). However, a lower proportion of Malays were living in private properties (0.7%). The Malays had the highest proportion of subjects incarcerated in a correctional facility at time of notification (6.6% vs. 1.6–3.9% in the other groups). Malays also had the highest proportion of patients living at the same residential address.
TABLE 1.
Baseline socio-demographic characteristics of TB cases among Singapore residents by ethnicity, 2002–2011
| Characteristic | Chinese (n = 11353) n (%) | Malay (n = 2919) n (%) | Indian (n = 900) n (%) | Others (n = 450) n (%) |
| Sex | ||||
| Male | 8 286 (73.0) | 1921 (65.8) | 596 (66.2) | 200 (44.4) |
| Age, years, mean ± SD | 59.9 ± 18.7 | 48.3 ± 18.5 | 48.6 ± 17.5 | 39.9 ± 17.2 |
| 0–14 | 80 (0.7) | 65 (2.2) | 11 (1.2) | 13 (2.9) |
| 15–39 | 2 089 (18.4) | 901 (30.9) | 282 (31.3) | 259 (57.6) |
| 40–64 | 5 065 (44.6) | 1370 (46.9) | 438 (48.7) | 132 (29.3) |
| ≥65 | 4 119 (36.3) | 583 (20.0) | 169 (18.8) | 46 (10.2) |
| Marital status | ||||
| Divorced | 447 (3.9) | 190 (6.5) | 52 (5.8) | 9 (2.0) |
| Other | 10 090 (88.9) | 2572 (88.1) | 789 (87.7) | 424 (94.2) |
| Unknown | 816 (7.2) | 157 (5.4) | 59 (6.6) | 17 (3.8) |
| Housing type* | ||||
| Government flat (1–2 room) | 832 (7.3) | 247 (8.5) | 68 (7.6) | 22 (4.9) |
| Government flat (3–5 room) | 7 818 (68.9) | 2146 (73.5) | 617 (68.6) | 341 (75.8) |
| Private housing | 711 (6.2) | 23 (0.7) | 41 (4.6) | 40 (8.9) |
| Unknown | 2 703 (23.8) | 526 (18.0) | 215 (23.9) | 87 (19.3) |
| Local-born | ||||
| Yes | 9 767 (86.0) | 2697 (92.4) | 583 (64.8) | 93 (20.7) |
| No | 1 523 (13.0) | 219 (7.5) | 309 (34.3) | 356 (79.1) |
| Unknown | 63 (1.0) | 3 (0.1) | 8 (0.9) | 1 (0.2) |
| Residential status | ||||
| Citizen | 10 946 (96.4) | 2861 (98.0) | 726 (80.7) | 163 (36.2) |
| Permanent resident | 407 (3.6) | 58 (2.0) | 174 (19.3) | 287 (63.8) |
| Incarceration in a correctional facility at point of TB notification† | 195 (1.7) | 192 (6.6) | 35 (3.9) | 7 (1.6) |
| Clustered by home address (n = 14 109)‡ | 794 (7.8) | 321 (11.9) | 56 (6.9) | 17 (4.1) |
1- to 2-room government flats represent the cheapest forms of housing, while 3- to 5-room government flats are mid-range; private housing refers to private apartments and any forms of landed property, the most expensive forms of housing.
Includes 61 inmates from drug rehabilitation centres and 326 prison inmates.
Does not include patients residing in congregate settings such as prisons, nursing homes, sheltered homes, halfway houses, etc.
TB = tuberculosis; SD = standard deviation.
Disease characteristics and co-morbidities among the cohort are described in Table 2: 88.7% of the Chinese patients had PTB, compared to 83.9% of Malays, 71.2% of Indians, and 74.2% of ‘others’. Malays had the highest proportion of cases with AFB smear 3–4+ (28%), while more Chinese and Malays were baseline culture-positive (about 75%). The proportion of cases without AFB smear or TB culture performed was similar for all ethnicities, at ≤10%. More Malays presented with cough (73.2% vs. 60% of Chinese and 69% of Indians) and cavitary disease on CXR (33% vs. 24–30%).
TABLE 2.
Baseline clinical characteristics and co-morbidities of TB cases among Singapore residents by ethnicity, 2002–2011
| Characteristic | Chinese (n = 11 353) n (%) | Malay (n = 2919) n (%) | Indian (n = 900) n (%) | Others (n = 450) n (%) |
| Site of disease | ||||
| Pulmonary | 10 070 (88.7) | 2448 (83.9) | 641 (71.2) | 334 (74.2) |
| Extra-pulmonary | 1 283 (11.3) | 471 (16.1) | 259 (28.8) | 116 (25.8) |
| AFB smear* | ||||
| Negative | 4 411 (43.8) | 918 (37.5) | 262 (40.9) | 188 (56.3) |
| 1–2+ | 2 508 (24.9) | 601 (24.6) | 160 (25.0) | 50 (15.0) |
| 3–4+ | 2 016 (20.0) | 686 (28.0) | 143 (22.3) | 57 (17.1) |
| Not performed | 1 135 (11.3) | 243 (9.9) | 76 (11.9) | 39 (11.7) |
| TB culture* | ||||
| Negative | 1 901 (18.9) | 462 (18.9) | 146 (22.8) | 90 (26.9) |
| Positive | 7 556 (75.0) | 1859 (75.9) | 448 (69.9) | 209 (62.6) |
| Not performed† | 613 (6.1) | 127 (5.2) | 47 (7.3) | 35 (10.5) |
| Presence of cough* | ||||
| Yes | 6 634 (65.9) | 1793 (73.2) | 411 (68.8) | 200 (59.9) |
| No | 3 436 (34.1) | 655 (26.8) | 200 (31.2) | 134 (40.1) |
| Cough duration, weeks, median [IQR]* | 4 [2–12] | 4 [2–8] | 4 [2–8] | 4 [2–12] |
| CXR showing cavitary disease* | ||||
| No | 7 315 (72.6) | 1600 (65.4) | 444 (69.3) | 246 (73.3) |
| Yes | 2 600 (25.8) | 809 (33.0) | 189 (29.5) | 79 (23.7) |
| Not performed/unknown | 155 (1.5) | 39 (1.6) | 8 (1.2) | 9 (2.7) |
| Presence of DM | ||||
| Yes | 2 215 (19.5) | 752 (25.8) | 253 (28.1) | 45 (10.0) |
| No | 9 138 (80.5) | 2167 (74.2) | 647 (71.9) | 405 (90.0) |
| Presence of HIV | ||||
| Yes | 128 (3.8) | 28 (2.8) | 7 (2.4) | 3 (1.6) |
| No | 2 339 (70.1) | 749 (75.2) | 202 (70.1) | 134 (72.0) |
| Test not performed | 941 (27.6) | 219 (22.0) | 79 (27.4) | 49 (26.3) |
PTB cases only.
Includes eight Chinese and two Malay patients with ‘contaminated’ results.
TB = tuberculosis; AFB = acid-fast bacilli; IQR = interquartile range; CXR = chest X-ray; DM = diabetes mellitus; HIV = human immunodeficiency virus.
We also compared the socio-demographic and clinical characteristics of Malays patients vs. all non-Malay patients (Table 3). Compared to non-Malays, Malay ethnicity was more strongly associated with incarceration in a correctional facility at the time of TB notification (OR 4.00, 95%CI 2.87–5.66), and not living in private housing (OR 0.18, 95%CI 0.11–0.29), based on adjusted OR.
TABLE 3.
Baseline clinical and socio-demographic characteristics of TB cases among Singapore residents, 2002–2011 (Malay vs. non-Malay)*
| Characteristic | Malay (n = 2919) n (%) | Non-Malay (n = 12 703) n (%) | Univariate analysis |
Multivariate analysis |
||
| OR (95%CI) | P value | OR (95%CI) | P value | |||
| Sex, male | 1921 (65.8) | 9 082 (71.5) | 0.77 (0.70–0.84) | <0.01 | 0.59 (0.52–0.66) | <0.01 |
| Age, >65 years | 583 (20.0) | 4 119 (36.3) | 0.44 (0.40–0.48) | <0.01 | 0.61 (0.54–0.70) | <0.01 |
| Singapore-born, No | 219 (7.5) | 2 188 (17.2) | 0.39 (0.34–0.45) | <0.01 | 0.36 (0.29–0.43) | <0.01 |
| Marital status | ||||||
| Divorced/separated | 190 (6.5) | 508 (4.0) | 1.64 (1.38–1.96) | <0.01 | 1.10 (0.93–1.40) | 0.21 |
| Other | 2572 (88.1) | 11 303 (89.0) | Reference | Reference | ||
| Residing in private housing | 23 (1.0) | 792 (8.2) | 0.11 (0.07–0.17) | 0.01 | 0.18 (0.11–0.29) | <0.01 |
| Incarceration in a correctional facility at moment of notification | 192 (6.6) | 237 (1.9) | 3.70 (3.03–4.52) | <0.01 | 4.00 (2.87–5.66) | <0.01 |
| Clustered by home address† | 321 (11.9) | 867 (7.6) | 1.65 (1.44–1.89) | <0.01 | 1.40 (1.16–1.62) | <0.01 |
| Retreatment | 276 (9.5) | 1 397 (11.0) | 0.85 (0.74–0.97) | 0.02 | 0.95 (0.80–1.14) | 0.60 |
| Pulmonary TB | 2448 (83.9) | 11 045 (86.9) | 0.78 (0.70–0.87) | <0.01 | 0.62 (0.50–0.78) | <0.01 |
| Baseline sputum smear‡ | ||||||
| Negative | 918 (37.5) | 4 861 (44.0) | Reference | Reference | ||
| 1 to 2+ | 601 (24.6) | 2 718 (24.6) | 1.17 (1.05–1.31) | <0.01 | 1.11 (0.96–1.28) | <0.01 |
| 3 to 4+ | 686 (28.0) | 2 216 (20.1) | 1.64 (1.47–1.83) | <0.01 | 1.32 (1.13–1.53) | <0.01 |
| CXR showing cavitary disease‡ | 809 (33.0) | 2 868 (26.0) | 1.41 (1.28–1.55) | <0.01 | 1.14 (1.01–1.28) | 0.04 |
| Presence of cough‡ | 1793 (73.2) | 7 275 (65.9) | 1.42 (1.29–1.56) | <0.01 | 1.13 (0.99–1.30) | 0.07 |
| Presence of DM | 752 (25.8) | 2 513 (19.8) | 1.41 (1.28–1.55) | <0.01 | 1.54 (1.37–1.73) | <0.01 |
The analysis presented in this table is based only on those records where data is available; details of records with unknown data can be found in Tables 1 and 2.
Does not include patients residing in congregate settings such as prisons, nursing homes, sheltered homes, halfway houses, etc.
Pulmonary TB cases only.
TB = tuberculosis; OR = odds ratio; CI = confidence interval; CXR = chest X-ray; DM = diabetes mellitus.
DISCUSSION
The findings from this study suggest that among diagnosed and reported cases of TB, Malay patients were more likely to have known risk factors for TB transmission and more severe disease than patients of other ethnicities. For example, more Malays had a highly positive AFB smear and CXR indicative of cavitary disease. These findings suggest that Malays had a higher bacillary burden and were thus potentially more infectious. This may be attributed to delayed diagnosis; however, whether the more severe disease presentation in this ethnic group could be due to genetic factors that influence host immune responses merits further study.
It has been well documented that DM increases the risk of active TB.18 Our study findings showed that the Malays were more likely to have DM than Chinese and ‘other’ ethnicities. This trend in DM prevalence also mirrors that of the general resident population.19 The Malays therefore have an increased risk of active TB compared to most non-Malays. We did, however, observe that Indian patients, who have the lowest rate of TB among all ethnicities, have the highest prevalence of DM, both in this study as well as among the general resident population. The reasons for this reverse trend are unclear and warrant further investigation.
Previous reports on molecular epidemiology have shown that clustering (and therefore recent transmission) was more likely in the younger age groups,20,21 presumably due to increased mobility, compared to those of post-retirement age. Our study findings reported a higher proportion of cases among the Malays aged ≤65 years compared to non-Malays. This suggests that a higher proportion of reported cases among Malays were due to recent transmission rather than reactivation of an old infection.
The association between lower socio-economic status and higher TB incidence has been reported elsewhere.22 In this study, we used housing type as a proxy for socio-economic status. Our findings showed that Malays were less likely to reside in private properties, suggesting that they were generally less affluent than other ethnicities. A previous report also associated low socio-economic status with diagnostic delay,23 which in turn delays the prompt treatment of active cases required to break the chain of transmission. In Singapore, newly diagnosed TB patients are routinely counselled prior to treatment commencement (using the patient’s preferred language), to educate the patient on treatment adherence issues as well as to evaluate the need for any financial or social assistance. However, we have observed that it is not uncommon for inherent issues to be uncovered only when the patient becomes non-adherent to treatment, and when probed further on the reason for default. It is therefore worthwhile to ensure that Malay patients are financially assessed more proactively and, if necessary, provided with the required assistance as early as possible to prevent disruption to treatment.
Compared to the other ethnic groups, a higher proportion of Malays shared the same residential address, suggesting that a higher proportion of transmission took place in Malay households. This could be a reflection of more crowded living conditions in Malay households, which concurs with our finding that more Malays reside in 1- or 2-room government flats compared to other ethnicities. The 2010 Singapore Census reported the largest average household size among Malays (4.2 persons vs. 3.5 in non-Malays).1
In the experience of our TB Contact Clinic, identified contacts of Malay index cases were less likely than those of other ethnic groups to attend for screening.24 The reasons for this are unclear, but may be due to educational or cultural factors, which in turn influence beliefs and attitudes towards health and health-seeking behaviour. It appears that, despite national guidelines that prioritise screening for close household contacts, opportunities to detect active disease and latent tuberculous infection among high-risk individuals in this ethnic group have been missed, resulting in further disease transmission in this close-knit community. This warrants further studies to evaluate the comprehensiveness of the current contact investigations and how to formulate strategies to address barriers to early case detection and disease prevention via contact screening and acceptance of preventive therapy.
It is well established that the risk of TB is high in congregate settings such as correctional facilities.25,26 Data from this study show that a significantly higher number of Malays were incarcerated in a correctional facility at the moment of notification. However, using available data, it cannot be ascertained whether more Malay inmates had TB, or whether the proportion of Malays was the same among inmates with TB and among all inmates in Singapore. It would be useful to know the ethnic distribution among all correctional facility inmates, but this information is not available.
A study from Singapore published in 2011 reported increased proportions of foreign-born persons among all notified cases in the country since 2005.17 Data from this study have shown that the Malay group had a substantially lower proportion of foreign-born persons compared to the other ethnic groups. This suggests that foreign-born Malays do not contribute to the observed increase in this ethnic group. However, further studies are required —possibly using molecular epidemiology—to determine the transmission dynamics between Malay Singapore residents and foreign-born persons.
The strengths of this study lie in the fact that it utilises nationwide, high quality data, ensuring the representativeness and validity of the reported findings. It is also the first study of Singapore resident TB cases to address the subject of ethnicity. It provides an insight into previously unknown socio-epidemiological and clinical differences, some of which are related to TB transmission, across the various ethnic groups among Singapore residents with a reported diagnosis of TB.
However, a number of limitations are recognised. Information on a number of known risk factors for TB (such as smoking history, history of substance abuse and chronic alcoholism) were not available for the study, as they were not routinely collected during TB notification. Consideration should be given to including these as part of the information required for TB notification, as they can be predictors of good adherence to treatment.27,28 Another concern was the high proportion of ‘unknown’ data (about 20% across all ethnic groups) for housing type, possibly due to the fact that this information is not mandatory for TB notification. However, this inadequacy is uniform across ethnic groups, and there is no reason to suspect that the ‘unknowns’ were more likely to relate to a particular housing type. Finally, although this study found a higher prevalence of known TB risk factors among reported TB cases among Malays, it does not definitively attribute the higher observed rate to any of these risk factors.
In conclusion, this study shows that among reported TB cases in Singapore residents, Malays, who have the highest TB incidence rates among the ethnic groups, have increased socio-economic risk factors for TB transmission and more severe disease. In addition to increased vigilance in case management and contact tracing, it is likely that interventions to improve socio-economic conditions in this community, as well as an assessment of their attitudes towards health (to highlight any needs for intervention), are required to reverse the increasing trend of TB rates in this ethnic group.
Acknowledgments
This research was supported by an operational research course that was jointly developed and run by the Centre for Operational Research, the International Union Against Tuberculosis and Lung Disease (The Union), Paris, France; The Union South-East Asia Office, New Delhi, India; and the Operational Research Unit (LUXOR), Médecins Sans Frontières, Brussels-Luxembourg. Additional support for running the course was provided by the Centre for International Health, University of Bergen, Bergen, Norway.
Funding for the course was from an anonymous donor and the Department for International Development, UK.
Conflict of interest: none declared.
References
- 1.Singapore Department of Statistics, Singapore. Census of Population 2010. Singapore: Singstat; 2011. http://www.singstat.gov.sg/Publications/population.html#census_of_population Accessed October 2013. [Google Scholar]
- 2.Ministry of Health, Singapore. Communicable Diseases Surveillance in Singapore 2011. Singapore: MoH; 2012. [Google Scholar]
- 3.Ministry of Health, Singapore. Communicable Diseases Surveillance in Singapore 2010. Singapore: MoH; 2011. [Google Scholar]
- 4.Ministry of Health, Singapore. Communicable Diseases Surveillance in Singapore 2009. Singapore: MoH; 2010. [Google Scholar]
- 5.Ministry of Health, Singapore. Communicable Diseases Surveillance in Singapore 2008. Singapore: MoH; 2009. [Google Scholar]
- 6.Ministry of Health, Singapore. Communicable Diseases Surveillance in Singapore 2007. Singapore: MoH; 2008. [Google Scholar]
- 7.Ministry of Health, Singapore. Communicable Diseases Surveillance in Singapore 2006. Singapore: MoH; 2007. [Google Scholar]
- 8.Ministry of Health, Singapore. Communicable Diseases Surveillance in Singapore 2005. Singapore: MoH; 2006. [Google Scholar]
- 9.Ministry of Health, Singapore. Communicable Diseases Surveillance in Singapore 2004. Singapore: MoH; 2005. [Google Scholar]
- 10.Communicable Disease Centre, Singapore. HIV/STI and TB surveillance report 2003. Singapore: CDC; 2004. [Google Scholar]
- 11.Chee C B E, Boudville I C, Chan S P, Zee Y K, Wang Y T. Patient and disease characteristics, and outcome of treatment defaulters from the Singapore TB control unit—a one-year retrospective survey. Int J Tuberc Lung Dis. 2000;4:496–503. [PubMed] [Google Scholar]
- 12.Chee C B E, Wang Y T, Teleman M D, Boudville I C, Chew S K. Treatment outcome of Singapore residents with pulmonary tuberculosis in the first year after introduction of a computerized treatment surveillance module. Singapore Med J. 2006;47:529–533. [PubMed] [Google Scholar]
- 13.Chee C B E, Hsu L Y, Sng L H, Leo Y S, Cutter J, Wang Y T. MDR TB transmission, Singapore. Emerg Infect Dis. 2013;19:1151–1152. doi: 10.3201/eid1907.120372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chee C B E, Kyin Win K M, Cutter J, Wang Y T. The imminent threat of multi-drug resistant TB in Singapore. Singapore Med J. 2012;53:238–240. [PubMed] [Google Scholar]
- 15.Chee C B E, Gan S H, Chua P G, Wang Y T. TB control in Singapore: the high price of diagnostic delay. Singapore Med J. 2012;53:505. [PubMed] [Google Scholar]
- 16.Wang Y T, Gan S H, Chee C B E. Non-adherence to TB treatment: who cares. Singapore Med J. 2012;53:782–783. [PubMed] [Google Scholar]
- 17.Kyi Win K M, Chee C B E, Shen L, Cutter J, Wang Y T. Tuberculosis among foreign-born persons, Singapore, 2000–2009. Emerg Infect Dis. 2011;17:517. doi: 10.3201/eid1703.101615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Christie Y J, Megan B M. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Med. 2008;5:e152. doi: 10.1371/journal.pmed.0050152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epidemiology and Disease Control Division. National Health Survey 2010. Singapore: MoH; 2011. Ministry of Health, Singapore. [Google Scholar]
- 20.Kamper-Jorgensen Z, Andersen A B, Kok-Jensen A, et al. Clustered tuberculosis in a low-burden country: nationwide genotyping through 15 years. J Clin Microbiol. 2012;50:2660–2667. doi: 10.1128/JCM.06358-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cattamanchi A, Hopewell P C, Gonzales L C, et al. A 13-year molecular epidemiological analysis of tuberculosis in San Francisco. Int J Tuberc Lung Dis. 2006;10:297–304. [PubMed] [Google Scholar]
- 22.Tanrikulu A C, Acemoglu H, Palanci Y, Dagli C E. Tuberculosis in Turkey: high altitude and other socio-economic risk factors. Public Health. 2008;122:613–619. doi: 10.1016/j.puhe.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 23.French C E, Kruijshaar M E, Jones J A, Abubakar I. The influence of socio-economic deprivation on tuberculosis treatment delays in England, 2000–2005. Epidemiol Infect. 2009;137:591–596. doi: 10.1017/S0950268808001118. [DOI] [PubMed] [Google Scholar]
- 24.Ministry of Health, Singapore. Missed opportunities for tuberculosis contact screening in Singapore—a retrospective case-control study. Epidemiol News Bull. 2008;34:34–40. [Google Scholar]
- 25.Moges B, Amare B, Asfaw F, et al. Prevalence of smear positive pulmonary tuberculosis among prisoners in North Gondar Zone Prison, northwest Ethiopia. BMC Infect Dis. 2012;15:352. doi: 10.1186/1471-2334-12-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Banu S, Hossain A, Uddin M K, et al. Pulmonary tuberculosis and drug resistance in Dhaka central jail, the largest prison in Bangladesh. PLOS ONE. 2010;5:e10759. doi: 10.1371/journal.pone.0010759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kulkarni P, Akarte S, Mankeshwar R, Bhawalkar J, Banerjee A, Kulkarni A. Non-adherence of new pulmonary tuberculosis patients to anti-tuberculosis treatment. Ann Med Health Sci Res. 2013;3:67–74. doi: 10.4103/2141-9248.109507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oeltmann J E, Kammerer J S, Pevzner E S, Moonan P K. Tuberculosis and substance abuse in the United States, 1997–2006. Arch Intern Med. 2009;169:189–197. doi: 10.1001/archinternmed.2008.535. [DOI] [PubMed] [Google Scholar]