Abstract
Posterior fossa emissary veins are valveless veins that pass through cranial apertures. They participate in extracranial venous drainage of the posterior fossa dural sinuses. The mastoid emissary vein, condylar veins, occipital emissary vein, and petrosquamosal sinus are the major posterior fossa emissary veins. We believe that posterior fossa emissary veins can be detected by radiologists before surgery with a thorough understanding of their anatomy. Describing them using temporal bone computed tomography (CT), CT angiography, and cerebral magnetic resonance (MR) venography examinations results in more detailed and accurate preoperative radiological interpretation and has clinical importance. This pictorial essay reviews the anatomy of the major and clinically relevant posterior fossa emissary veins using high-resolution CT, CT angiography, and MR venography images and discusses the clinical importance of reporting these vascular variants.
Posterior fossa emissary veins pass through cranial apertures and participate in extracranial venous drainage of the posterior fossa dural sinuses. These emissary veins are usually small and asymptomatic in healthy people. They protect the brain from increases in intracranial pressure in patients with lesions of the neck or skull base and obstructed internal jugular veins (1). They also help to cool venous blood circulating through cephalic structures (2). Emissary veins may be enlarged in patients with high-flow vascular malformations or severe hypoplasia or aplasia of the jugular veins. They are associated with craniofacial syndromes (1, 3). Dilated emissary veins may cause tinnitus (4, 5).
We aim to emphasize the importance of reporting posterior fossa emissary veins prior to surgeries that are related to the posterior fossa and mastoid region. Here, we review their embryology and anatomy based on high-resolution computed tomography (CT), CT angiography, and magnetic resonance (MR) venography images.
Posterior fossa emissary veins
The development of intracerebral veins and their extracranial drainage is complex in humans. The primary capillary plexus of the early embryo develops in three layers. The superficial vessels drain into the external jugular vein, whereas the middle and deep vessels drain into the internal jugular vein. Emissary veins, in the third trimester, consist of residual connections between the superficial and middle layers (1). During growth of the jugular sinuses, most of them disappear, but some persist and enlarge. The cause may be related to failure of normal maturation of the sigmoid-jugular complexes (6).
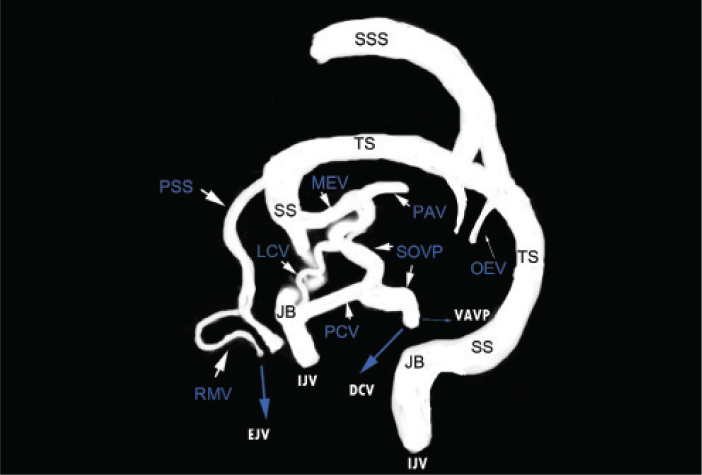
The mastoid emissary vein (MEV), posterior condylar vein, occipital emissary vein, and petrosquamosal sinus (PSS) are the major posterior fossa emissary veins of clinical importance (Fig. 1).
Figure 1.
Schematic representation of posterior fossa emissary veins in a patient with a hypoplastic sigmoid sinus and internal jugular vein. External connections of emissary veins are indicated by the blue arrows and bold white letters. DCV, deep cervical vein; EJV, external jugular vein; IJV, internal jugular vein; JB, jugular bulb; LCV, lateral condylar vein; MEV, mastoid emissary vein; OEV, occipital emissary vein; PAV, posterior auricular vein; PCV, posterior condylar vein; PSS, petrosquamosal sinus; RMV, retromandibular vein; SOVP, suboccipital venous plexus; SS, sigmoid sinus; SSS, superior sagittal sinus; TS, transverse sinus; VAVP, vertebral artery venous plexus.
Mastoid emissary vein
The MEV runs between the sigmoid sinus and posterior auricular or occipital vein by crossing the mastoid foramen. The posterior auricular and occipital veins drain into the suboccipital venous plexus or external jugular vein (Fig. 2). The suboccipital venous plexus drains into the anterior vertebral vein or deep cervical vein (7).
Figure 2. a, b.
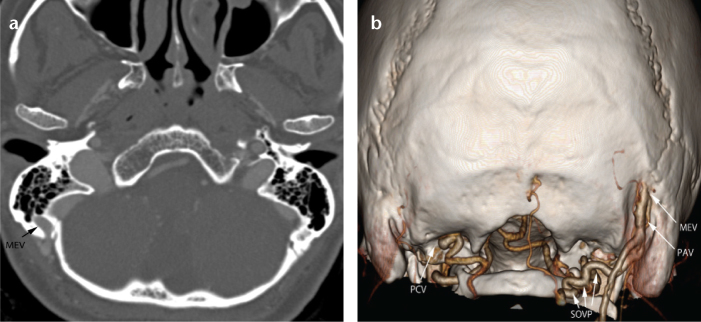
Axial multiplanar reformatted image (a) shows a mastoid emissary vein (MEV). A three-dimensional volume-rendered image (posterior view) (b) shows the MEV draining into the posterior auricular vein (PAV) and PAV draining into the suboccipital venous plexus on the left side. A posterior condylar vein emerges from its canal on the right side.
The MEV may change in size, and there may be multiple MEVs (1, 7). The diameter of MEV is important because this vessel could be a potential target for endovascular procedures (Fig. 3). Endovascular treatment of dural arteriovenous fistulas is difficult due to limited access. It has been reported that MEV can be used to access an isolated or inaccessible transverse or sigmoid sinus system in these patients (8). It would be valuable to determine the diameter of the MEV preoperatively to choose the appropriate cannula.
Figure 3.

Sagittal oblique reformatted image of CT angiography shows the entire course of the mastoid emissary vein along the canal. The diameter of the mastoid emissary vein is very important when it is being considered for endovascular procedures (arrow).
The MEV is a potential source of life-threatening bleeding during surgical procedures. Furthermore, surgical materials for achieving hemostasis of the MEV may predispose one to complications. A previous study reported migration of bone wax into a sigmoid sinus that caused thrombosis (9). Air embolism is another postoperative complication of the MEV during lateral suboccipital approaches (10).
The MEV can be the source of thrombosis of the sigmoid sinus after middle ear surgery. Most importantly, it may be the main outflow pathway of the posterior fossa dural sinuses in some cases, and ligation could lead to venous ischemic and hemorrhagic consequences (8). Two cases of cerebellar infarction and one death resulting from coagulation of the MEV during skull base surgery have been reported (11). Assessing this vein preoperatively would allow one to modify the surgical procedure to reduce complications.
The MEV may constitute a potential risk for spreading infectious processes from extracranial to intracranial areas. It may be thrombosed as a complication of acute otomastoiditis. The MEV thrombosis causes edema and tenderness of the postauricular soft tissues overlying the mastoid process (Griesinger’s sign).
Posterior, anterior, and lateral condylar veins
The posterior condylar vein courses between the superior bulb of the internal jugular vein and deep cervical vein. It also communicates with the horizontal portion of the vertebral artery venous plexus (Fig. 4).
Figure 4. a–c.
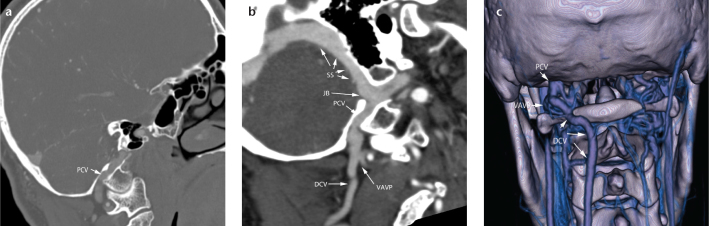
A sagittal multiplanar reformatted image (a), curved planar reformation image (b), and three-dimensional volume-rendered image (posterior view) (c) show the posterior condylar vein (PCV) arising from the superior bulb of the internal jugular vein and draining into the deep cervical vein (DCV). It also communicates with the horizontal portion of the vertebral artery venous plexus (VAVP). JB, jugular bulb; SS, sigmoid sinus.
The posterior condylar vein and deep cervical vein may be very large, particularly regarding jugular vein thrombosis (7, 12). Dilatation of these veins should be known before performing surgery on the posterior fossa and/or posterior cervical region. Dilatation may also change the surgical approach and makes the surgeon more cautious during surgery. A dilated MEV or condylar emissary vein can be a rare cause of tinnitus. Posterior condylar veins may be localized very closely with tumors in the skull base or neck (Fig. 5).
Figure 5.
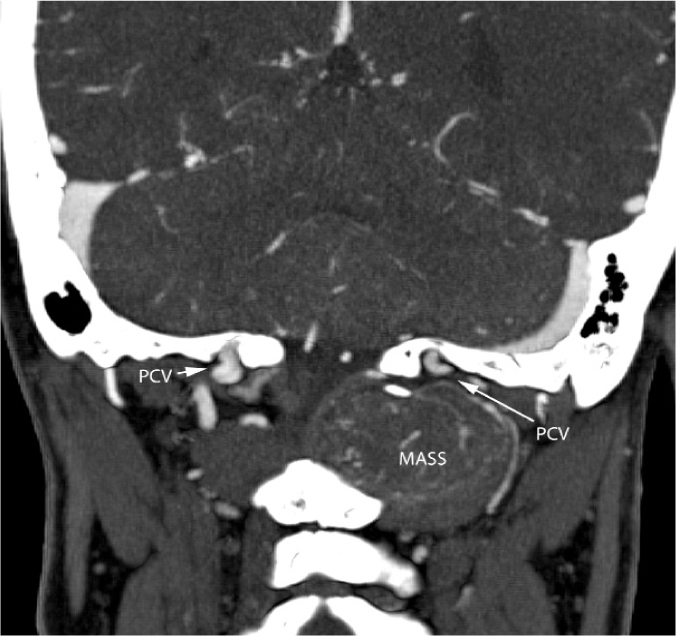
Coronal multiplanar reformatted image shows bilateral posterior condylar veins (PCV) with the left one very close to a hypervascular neck mass.
Lateral and anterior condylar veins also contribute to the venous drainage from the posterior fossa dural sinuses to the vertebral venous system, particularly in cases of thrombosis of the jugular system (12). However, these veins are plexiform connections, and it is difficult to distinguish among these veins with imaging.
Petrosquamosal sinus
The PSS arises from the transverse sinus before its junction with the sigmoid sinus and drains either into the retromandibular vein through the post-glenoid foramen or into the pterygoid venous plexus through the foramen ovale. Its main drainage pathway is the external jugular vein (Figs. 6, 7) (1, 13).
Figure 6. a, b.
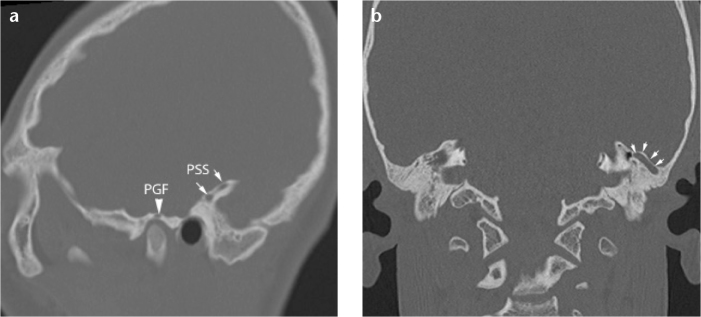
Sagittal (a) and coronal multiplanar reformatted (b) temporal CT images show a petrosquamosal sinus (PSS) sulcus on the left, located on the upper portion of the petrous bone (arrows) and ending in the postglenoid foramen (PGF).
Figure 7.
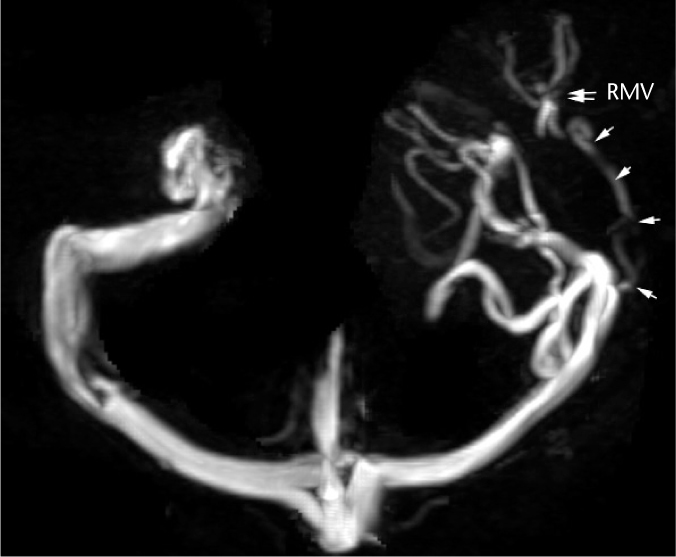
Axial maximum intensity projection image from a three-dimensional phase-contrast MR venography shows the petrosquamosal sinus on the left side (arrows) draining into the retromandibular vein (RMV).
The PSS is rarely found in humans (13). In contrast to anatomical studies, radiological identification of the PSS is quite uncommon (14). In animals that have a smaller degree of telencephalic growth, the PSS is the major outflow pathway of the transverse sinus, and the external jugular vein is the dominant encephalic venous drainage pathway. However, in humans, internal jugular veins and the vertebral venous system are the major cerebral venous outflow pathways. Venous drainage of the brain differs depending on the position of the body. The outflow is through the internal jugular veins in the prone position, whereas most of the encephalic drainage transfers to the internal and external vertebral venous system in the upright position (12, 15).
The PSS is mostly found in patients with congenital malformations of the skull base. It has been reported to be associated with semicircular canal aplasia (16). Both semicircular canal aplasia and PSS may be a component of CHARGE syndrome (17). In these patients, the PSS is generally very large, and it represents a risk for cochlear implant surgery.
The PSS may be the main outflow pathway of the transverse sinus in some cases, and particular care should be taken during surgical procedures because sacrificing this outflow pathway could lead to catastrophic venous ischemic and hemorrhagic consequences.
The PSS and other emissary veins may accompany syndromic craniosynostosis, and they should be assessed before surgeries, particularly when posterior decompression is being considered (3, 17).
Occipital emissary vein
The occipital emissary vein is present in the midline. Its multiple presentation may be seen rarely (Fig. 8). It drains from the confluens sinuum (torcula) to the internal vertebral plexus (3). It may be very large and may also constitute a potential hazard during surgery.
Figure 8.
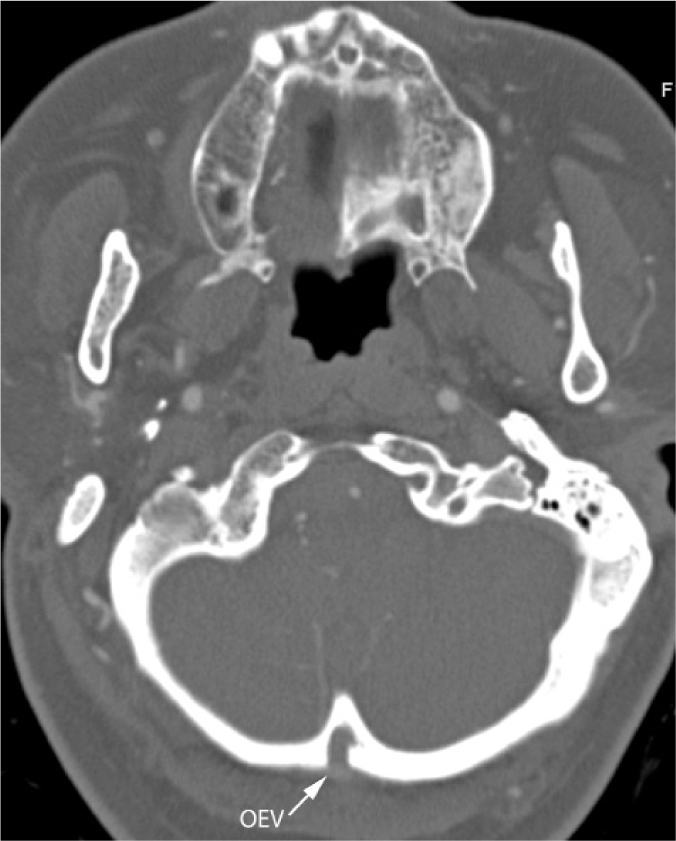
Axial multiplanar reformatted image showing a large central occipital emissary vein (OEV).
Conclusion
Posterior fossa emissary veins should be reported by a radiologist before surgeries to avoid complications, particularly when related to the posterior fossa and mastoid region.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Marsot-Dupuch K, Gayet-Delacroix M, Elmaleh-Bergès M, Bonneville F, Lasjaunias P. The petrosquamosal sinus: CT and MR findings of a rare emissary vein. Am J Neuroradiol. 2001;22:1186–1193. [PMC free article] [PubMed] [Google Scholar]
- 2.Louis RG, Jr, Loukas M, Wartmann CT, et al. Clinical anatomy of the mastoid and occipital emissary veins in a large series. Surg Radiol Anat. 2009;31:139–144. doi: 10.1007/s00276-008-0423-5. [DOI] [PubMed] [Google Scholar]
- 3.Jeevan DS, Anlsow P, Jayamohan J. Abnormal venous drainage in syndromic craniosynostosis and the role of CT venography. Childs Nerv Syst. 2008;24:1413–1420. doi: 10.1007/s00381-008-0667-8. [DOI] [PubMed] [Google Scholar]
- 4.Forte V, Turner A, Liu P. Objective tinnitus associated with abnormal mastoid emissary vein. J Otolaryngol. 1989;18:232–235. [PubMed] [Google Scholar]
- 5.Lambert PR, Cantrell RW. Objective tinnitus in association with an abnormal posterior condylar emissary vein. Am J Otol. 1986;7:204–207. [PubMed] [Google Scholar]
- 6.Chauhan NS, Sharma YP, Bhagra T, Sud B. Persistence of multiple emissary veins of posterior fossa with unusual origin of left petrosquamosal sinus from mastoid emissary. Surg Radiol Anat. 2011;33:827–831. doi: 10.1007/s00276-011-0822-x. [DOI] [PubMed] [Google Scholar]
- 7.Reis CV, Deshmukh V, Zabramski JM, et al. Anatomy of the mastoid emissary vein and venous system of the posterior neck region: neurosurgical implications. Neurosurgery. 2007;61:193–200. doi: 10.1227/01.neu.0000303217.53607.d9. [DOI] [PubMed] [Google Scholar]
- 8.Rivet DJ, Goddard JK, 3rd, Rich KM, Derdeyn CP. Percutaneous transvenous embolization of a dural arteriovenous fistula through a mastoid emissary vein. Technical note. J Neurosurg. 2006;105:636–639. doi: 10.3171/jns.2006.105.4.636. [DOI] [PubMed] [Google Scholar]
- 9.Hadeishi H, Yasui N, Suzuki A. Mastoid canal and migrated bone wax in the sigmoid sinus: technical report. Neurosurgery. 1995;36:1220–1223. doi: 10.1227/00006123-199506000-00028. [DOI] [PubMed] [Google Scholar]
- 10.An YH, Wee JH, Han KH, Kim YH. Two cases of petrosquamosal sinus in the temporal bone presented as perioperative finding. Laryngoscope. 2011;121:381–384. doi: 10.1002/lary.21369. [DOI] [PubMed] [Google Scholar]
- 11.Hoshi M, Yoshida K, Ogawa K, Kawase T. Hypoglossal neurinoma--two case reports. Neurol Med Chir. 2000;40:489–493. doi: 10.2176/nmc.40.489. [DOI] [PubMed] [Google Scholar]
- 12.San Millán Ruíz D, Gailloud P, Rüfenacht DA, Delavelle J, Henry F, Fasel JH. The craniocervical venous system in relation to cerebral venous drainage. Am J Neuroradiol. 2002;23:1500–1508. [PMC free article] [PubMed] [Google Scholar]
- 13.San Millán Ruíz D, Gailloud P, Yilmaz H, et al. The petrosquamosal sinus in humans. J Anat. 2006;209:711–720. doi: 10.1111/j.1469-7580.2006.00652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koesling S, Kunkel P, Schul T. Vascular anomalies, sutures and small canals of the temporal bone on axial CT. Eur J Radiol. 2005;54:335–343. doi: 10.1016/j.ejrad.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Valdueza JM, von Munster T, Hoffman O, et al. Postural dependency of the cerebral venous outflow. Lancet. 2000;355:200–201. doi: 10.1016/s0140-6736(99)04804-7. [DOI] [PubMed] [Google Scholar]
- 16.Giesemann AM, Goetz GF, Neuburger J, Lenarz T, Lanfermann H. Persistent petrosquamosal sinus: high incidence in cases of complete aplasia of the semicircular canals. Radiology. 2011;259:825–833. doi: 10.1148/radiol.11101466. [DOI] [PubMed] [Google Scholar]
- 17.Morimoto AK, Wiggins RH, 3rd, Hudgins PA, et al. Absent semicircular canals in CHARGE syndrome: radiologic spectrum of findings. Am J Neuroradiol. 2006;27:1663–1671. [PMC free article] [PubMed] [Google Scholar]